Abstract
Severe acute respiratory syndrome coronavirus 2 disease 2019 (COVID-19) has rapidly spread worldwide since December 2019. An acute respiratory distress syndrome develops in a relevant rate of patients, who require hospitalization. Among them, a nonnegligible rate of 9.8% to 15.2% of patients requires tracheal intubation for invasive ventilation. We report the case of a pneumomediastinum and subcutaneous emphysema developing in a COVID-19 patient secondary to postintubation tracheal injury. The management of COVID-19 patients can be challenging due to the risk of disease transmission to caregivers and epidemic spread. We performed a bedside tracheal injury surgical repair, after failure of conservative management, with resolution of pneumomediastinum and subcutaneous emphysema and improvement of the patient’s conditions.
Since the first reported case in Wuhan, China,1 novel coronavirus disease 2019 (COVID-19) has quickly spread worldwide. Most patients are asymptomatic or complain of mild respiratory influenza-like symptoms. However, some patients need hospitalization for respiratory support, and a relevant rate of 9.8% to 15.2% require orotracheal intubation (OTI) for invasive ventilation. On April 3, 2020, 28,741 patients in Italy were hospitalized for COVID-19. Among them, 4068 (14.2%) needed intensive care support, and most were intubated for mechanical ventilation support. OTI can rarely lead to tracheal injury, particularly under emergency or in patients with documented airway management difficulty.
We present a case of a COVID-19 patient in whom a postintubation tracheal injury resulted in a massive pneumomediastinum and subcutaneous emphysema. Considering the hemodynamic and respiratory instability after conservative management, a bedside surgical tracheostomy with primary suture of the tracheal lesion was performed.
A 72-year-old man was admitted to our hospital complaining fever (38°C) and cough. In his medical history, the patient reported systemic hypertension and an epidemiologic link with family members who had returned from northern Italy. At admission, his temperature was 37.8°C, oxygen saturation was 95%, and laboratory tests showed an enhanced C-reactive protein (3.02 mg/dL) and normal leukocytes count with lymphopenia (870 cells/μL).
A computed tomographic scan showed multiple ground-glass opacity extensively involving the lungs bilaterally, with associated mild pericardial effusion. The nasopharyngeal swab polymerase chain reaction test confirmed infection by severe acute respiratory syndrome coronavirus 2, confirming the diagnosis of COVID-19.
The patient was immediately isolated in a dedicated COVID-19 ward and was given supplemental oxygen and antiviral and antirheumatic drugs as protocol in our hospital (lopinavir/ritonavir, hydroxychloroquine). However, progressive dyspnea, persistent fever, and deterioration of hemogas oxygenation developed the day after and the patient required continuous positive airway pressure by helmet (positive end-expiratory pressure, 10; fraction of inspired oxygen, 0.5→1).
On day 4, the rapid worsening of respiratory conditions led to an emergency OTI. A fast-track intubation was performed using an 8-mm single-lumen orotracheal tube with the support of video laryngoscopy. The patient was then transferred to a dedicated COVID-19 intensive care unit.
The patient immediately presented progressive subcutaneous emphysema. A flexible bronchoscopy revealed a level II tracheal laceration of approximately 1 cm in the membranous wall and approximately 2 cm distally to the vocal cords. Considering the dimension and characteristics of the rupture, a conservative management was first considered convenient. The orotracheal tube was endoscopically positioned with the cuff located distally to the lesion. However, the subcutaneous emphysema continued to worsen (Figure 1 ), reaching the zygomatic and periorbital region, the whole chest bilaterally, and the arms, accompanied by atrial fibrillation and hemodynamic instability.
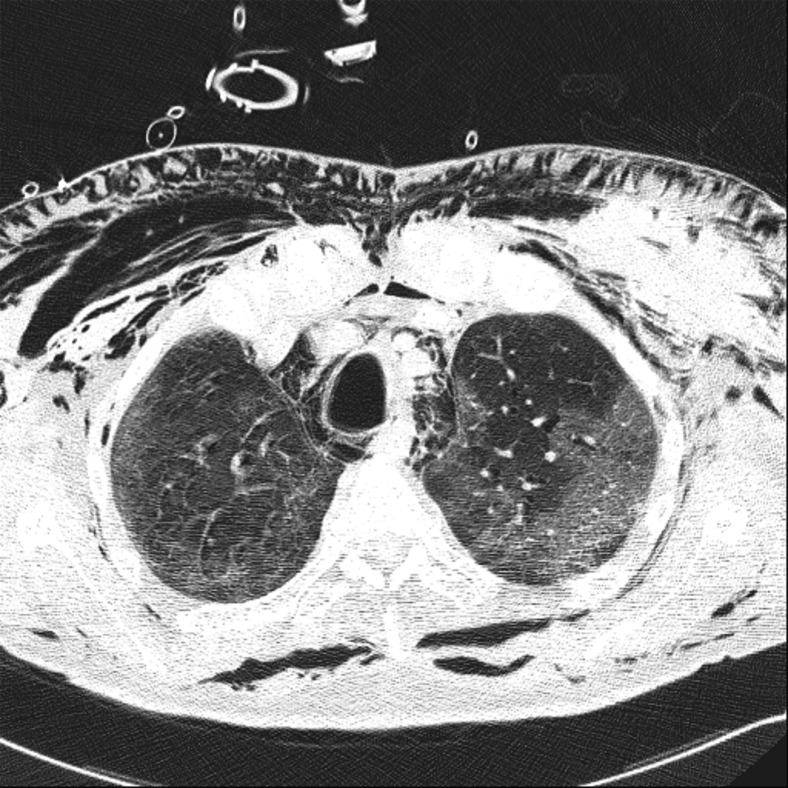
Figure 1.
Computed tomographic scan performed after conservative management of the tracheal lesion shows worsening pneumomediastinum and subcutaneous emphysema.
On day 7, surgical repair of the tracheal injury with tracheostomy was planned. To reduce the risk of epidemic spread and avoid transporting, in absence of a COVID-19–dedicated operating room, the procedure was performed bedside.
Under total intravenous general anesthesia, a transverse cervical incision of approximately 4 cm was performed. Meticulous dissection of the cervical fascia, platysma, and pretracheal muscles allowed the visualization of the anterior tracheal wall. A reverse U-shaped tracheal incision was performed, and the tracheal injury was identified and repaired using a 4-0 absorbable running suture. The tracheotomy was then used to insert an 8-mm cuffed tracheostomy cannula. The procedure from tracheotomy to cannula insertion was rapidly performed in apnea to reduce the aerosol contamination, with the anesthesiologist constantly monitoring the vital signs.
By day 9, the patient’s condition started to improve, with a reduction in subcutaneous emphysema, an increase in gasses exchange and hemodynamic parameters, and no new episodes of tachycardia or atrial fibrillation. The patient was progressively weaned from mechanical ventilation with the improvement of oxygenation and general conditions.
Comment
The incidence of airways injury due to OTI is reported to be approximately 0.005% with a single-lumen tube and occurs more often in a patient with difficult airway management or when performed as an emergency.2 However, some authors believe that it is probably underestimated because these injuries are often unrecognized and underreported.3
Pneumomediastinum and subcutaneous emphysema are the most common clinical manifestations but can lead to more severe conditions such as bilateral pneumothorax, hemodynamic instability, mediastinitis, and sepsis. The treatment options include noninvasive interventions, such positioning the tracheal tube cuff distal to the lesion, and observation. Surgery is indicated in case of large tracheal ruptures, type III A-B lesions,4 ventilatory instability, mediastinitis, or a progressive increase in subcutaneous emphysema.3 For injuries of the proximal one-third of the trachea, a transcervical approach, first proposed by Angelillo-Mackinlay,5 is preferred over traditional right thoracotomy because it is less invasive. More recently, a transcervical-transtracheal approach that includes a T-shaped tracheotomy has been proposed for postintubation tracheal injury.6
Management of COVID-19 patients represents a challenge, especially during invasive airways interventions.2 A negative-pressure operating room, adequate protective equipment, and an experienced team are mandatory to minimize the risk of contagion.
In this case, the precautions used to minimize the epidemic spread were:
-
1.
Bedside approach. The choice for a bedside approach avoids patient transport and disconnection/reconnection to ventilators. Transferring of COVID-19 patients must be always considered a risk of contamination and avoided if possible. The bedside approach avoid risks related to transport and the requirement of a dedicated operating room as previously demonstrated during the outbreaks of severe acute respiratory syndrome and Middle East respiratory syndrome.7
-
2.
Time of aerosol exposure. Intraoperatively, some tricks have been adopted to reduce the time of respiratory secretion exposure. First, the patient remained ventilated through the orotracheal tube, connected to a closed viral-filtered system, until the reverse U-shaped tracheal incision was performed. The adequate length of tracheotomy for surgical repair and subsequent tracheostomy cannula insertion were checked in this phase. Second, the ventilation was stopped and the tube withdrawn to visualize the tracheal injury. Third, the repair was rapidly performed during patient’s apnea. This was possible because the lesion was small; however, an on-field 5-mm tracheal tube was available if ventilation was needed. No suction was needed.
-
3.
General anesthesia. Total intravenous general anesthesia, with infusion of propofol, sufentanil, and rocuronium, guarantees deep curarization to prevent cough or reflexes during the procedure.
Unquestionably, this technique presents some limitations, mainly related to the impossibility in treating large injuries or lesions of the lower-third of the trachea. Moreover, the bedside approach presents some considerations related to the limited space, suboptimal positioning of the patient, and the movement of essential surgical instruments.7 These difficulties can be overcome with rigorous preoperative planning and an experienced team.
In conclusion,an increasing number of patients affected by COVID-19 are requiring OTI for mechanical ventilation. Even if rare, postintubation tracheal injury can occur, especially in an emergency scenario. The bedside transcervical-transtracheal approach is feasible for small to moderate lesions and minimizes contamination risks.
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sorbello M., El-Boghdadly K., Di Giacinto I. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia. 2020;75:724–732. doi: 10.1111/anae.15049. [DOI] [PubMed] [Google Scholar]
- 3.Grewal H.S., Dangayach N.S., Ahmad U., Ghosh S., Gildea T., Mehta A.C. Treatment of tracheobronchial injuries: a contemporary review. Chest. 2019;155:595–604. doi: 10.1016/j.chest.2018.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardillo G., Carbone L., Carleo F. Tracheal lacerations after endotracheal intubation: a proposed morphological classification to guide non-surgical treatment. Eur J Cardiothorac Surg. 2010;7:581–587. doi: 10.1016/j.ejcts.2009.07.034. [DOI] [PubMed] [Google Scholar]
- 5.Angelillo-Mackinlay T. Transcervical repair of distal membranous tracheal laceration. Ann Thorac Surg. 1995;59:531–532. doi: 10.1016/0003-4975(94)00882-8. [DOI] [PubMed] [Google Scholar]
- 6.Mussi A., Ambrogi M.C., Menconi G., Ribechini A., Angeletti C.A. Surgical approaches to membranous tracheal wall lacerations. J Thorac Cardiovasc Surg. 2000;120:115–118. doi: 10.1067/mtc.2000.107122. [DOI] [PubMed] [Google Scholar]
- 7.Tay J.K., Khoo M.L., Loh W.S. Surgical considerations for tracheostomy during the COVID-19 pandemic: lessons learned from the severe acute respiratory syndrome outbreak. JAMA Otolaryngol Head Neck Surg. 2020;146:517–518. doi: 10.1001/jamaoto.2020.0764. [DOI] [PubMed] [Google Scholar]