Abstract
The COVID pandemic of 2020 has emerged as a global threat to patients, health care providers, and to the global economy. Owing to this particular novel and highly infectious strain of coronavirus, the rapid community spread and clinical severity of the subsequent respiratory syndrome created a substantial strain on hospitals and health care systems around the world. The rapid surge of patients presenting over a small period for emergent clinical care, admission to the hospital, and intensive care units with many requiring mechanically assisted ventilators for respiratory support demonstrated the potential to overwhelm health care workers, hospitals, and health care systems. The purpose of this article is to describe an effective system for redeployment of health care supplies, resources, and personnel to hospitals within a suburban academic hospital system to optimize the care of COVID patients, while treating orthopedic patients in an equally ideal setting to maximize their surgical and clinical care. This article will provide a particular focus on the current and future role of a specialty hip and knee hospital and its partnering ambulatory surgery center in the context of an outpatient arthroplasty program.
Keywords: COVID-19, coronavirus, hip artthroplasty, knee arthroplasty, surge, resources
The COVID pandemic is the result of the spread of the SARS-CoV-2 virus, which results in severe acute respiratory syndrome and in the most severe cases, death. Its origin is in Wuhan, People's Republic of China, with the first cases reported there in December of 2019 and has rapidly spread worldwide since that time. In March 2020, the World Health Organization declared COVID-19 a world pandemic and to date, over two million people worldwide have been infected with the SARS-CoV-2 virus and it will continue to spread throughout the world over the coming months to years. Its health and economic consequences have been profound and have affected nearly all countries across the globe [1].
Owing to emerging information and epidemiologic modeling leading up to its rapid spread here in the United States, many institutions were able to prepare and enact a coordinated response in anticipation of what has been termed the “COVID-19 surge,” and the anticipated shortage of personal protection equipment (PPE), intensive care unit beds, and respiratory ventilators. This article will discuss how a suburban hospital region within a large academic health system was able to group COVID patients in hospitals with optimal capability and expertise to care for those patients with severe respiratory illness, while utilizing a smaller orthopedic-focused hospital, Indiana University Hip and Knee Center at Saxony Hospital, to treat the urgent orthopedic cases. This article will discuss the successful resource reallocation methodology with a particular emphasis on the outpatient and ambulatory setting.
COVID-19 Surge Anticipation
Indiana University (IU) Health is the largest health system in the state of Indiana with 2708 total beds and over 118,000 hospital admissions annually and is partnered with the nation’s largest medical school, Indiana University School of Medicine. Through close cooperation with our state government and examination of available epidemiological models, IU Health determined that a surge of patients affected by the novel coronavirus would encounter our health system in late March and within an anticipated peak in mid to late April. Our program made the decision to stop all elective, nonurgent hip and knee arthroplasty surgery on March 17, 2020, and based on evolving data that became clear, the ambulatory aspect of patient care also ceased immediately. From a hip and knee arthroplasty perspective, appropriately triaging patients based on the extent of their clinical condition and acuity was paramount.
Concurrently, with the canceling of all elective surgeries and nonurgent patients in the ambulatory clinic setting, protocols were rapidly being developed to care for the more urgent needed orthopedic hip and knee arthroplasty patients, which included those with infections, fractures, and periprosthetic hip and knee fractures. The Indiana University Hip and Knee Center at Saxony Hospital is part of a four hospital regional health network called the Indianapolis Suburban Region (ISR) and the administrative and clinical leadership immediately developed and enacted a plan to preserve PPE and hospital resources to support the appropriate deployment to the frontline caregivers that included emergency room physicians, pulmonologist, anesthesiologists, and critical care physicians and team members. Simultaneously, PPE and equipment such as ventilators were moved from our orthopedic-focused hospital to the two larger hospitals in the ISR where COVID patients would be treated predominantly.
From an outpatient perspective our ambulatory clinic made a number of significant changes that optimized patient safety as well as preservation of personal protective equipment. Patients and staff members are required to use masks during every patient interaction and patients were seen in person only if the patient’s clinical condition was deemed urgent. All examination rooms in their entirety were thoroughly cleaned with disinfectant between each and every patient. In addition, like many other institutions in the United States and abroad, virtual interaction with existing and potential patients was initiated using HIPAA compliant software. Virtual clinic visits were offered to follow-up and new patients, who consented to that form of clinical interaction.
Unique to the outpatient surgery environment, the ambulatory surgery center facilities played a significant and vital role in terms of contributing resources to accommodate the surge of COVID-19 patients. IU Health has a unique and collaborative partnership with Surgical Care Affiliates (SCA). The partnership between the two entities encompasses 14 discrete ambulatory surgery centers (ASCs) whose operations are run by IU Health with administrative support from SCA. The 14 IU Health ASCs perform approximately 75,000 outpatient surgeries annually, and analogous to the main hospitals, the ASCs stopped all elective surgeries on March 17, 2020. Supplies and staff from the ASCs were redeployed into the hospitals to serve vital roles in the continued health care expansion to accept the medically ill patients within the COVID-19 surge. In fact, approximately 85% of extra supplies and equipment needed for the frontline providers in the four ISR hospitals were provided by the ASCs, clearly demonstrating the critically important role that the ASCs played and continue to play in the COVID pandemic response. It is important to recognize the leadership role that ASCs play in the 2020 COVID-19 pandemic. SCA is one of many ambulatory surgery center entities in the United States who play a vital role in health care delivery and were vital in rapidly deploying PPE, ventilators, supplies, and staff to the various hospitals. In our particular health system, three of the ambulatory surgery centers remained open for urgent ambulatory surgical care. This further supported the health care resource conundrum, by performing urgent surgical care for less complex ambulatory procedures in the ASCs which allowed the more medically complex COVID-19 patients to have access to the inpatient hospital system. Some guidelines and publications have been established regarding what constitutes an “urgent” procedure within and ASC or outpatient setting [2]. It is generally accepted that an “urgent” procedure is a surgery that would increase the risk of permanent impairment or pain if not performed in a timely manner.
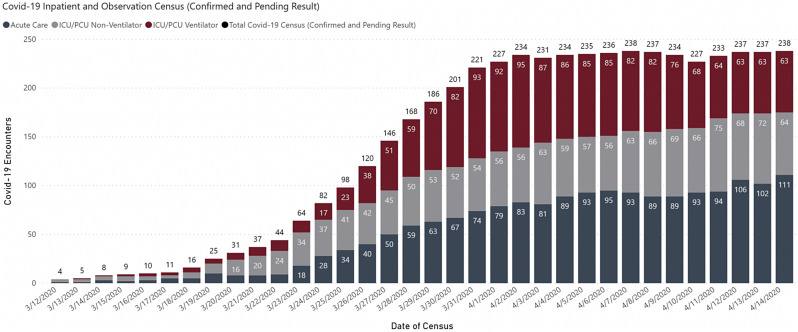
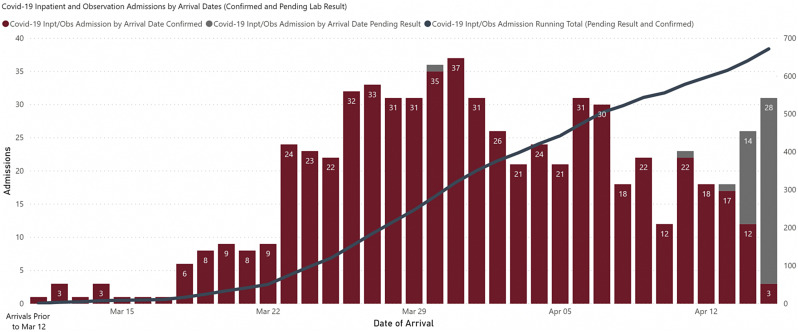
The result of this rapid and effective systemwide planning, utilizing ASC resources in close partnership with our health care system, allowed adequate capacity to handle the COVID-19 surge without any shortages of ventilators or ICU beds. In addition, our health system provided the care for approximately 60% of the COVID-19 patients in the State of Indiana. The social distancing efforts and state-mandated stay-at-home order was effective in “flattening” the curve of clinically relevant viral spread within our state and the subsequent burden placed on our health system (Fig. 1 ). As of April 16, 2020, the State of Indiana reported a flattening of the curve with 45% of ICU beds and 76% of ventilators across the state available. Specifically, the IU Health system data revealed a general flattening of the overall inpatient census with a gradually smaller percentage requiring ICU status and/or ventilator support (Fig. 1). More encouragingly, the daily admissions into the IU Health system declined over the same period after a peak in late March (Fig. 2 ).
Fig. 1.
Inpatient and observation COVID-19 census data for a large academic health system over time demonstrating the flattening curve phenomenon.
Fig. 2.
COVID-19 inpatient and observation admissions by arrival dates at a large academic health system, demonstrating the steady decline of admissions from late May until current.
Post-COVID-19 or “Reverse Surge”
At the time of this publication, there is much speculation about what the future of hip and knee arthroplasty outpatient surgery holds within the United States and abroad. Nonetheless, the statistical models of viral spread are rapidly evolving and becoming more accurate as we continue to understand the details of this novel coronavirus and its clinical sequelae. Our hip and knee arthroplasty program is diligently developing protocols for keeping patients and health care workers safe on the point in time that we resume elective hip and knee arthroplasties. There are multiple factors that will need to be accounted for and the ASCs will likely play an expanded role in access to surgical care for patients with hip and knee arthritis.
First are the protocols that must be developed to safely perform hip and knee arthroplasty in the COVID-19 era. It is probable that every patient regardless of symptoms will need to be tested for COVID-19 before elective surgery within a certain time before surgery. This will need to be embedded in the perioperative medical pathways which are typical for hip and knee arthroplasty programs. It is also likely that all the surgical care teams and providers in the ambulatory surgery centers will need to self-monitor and document they are afebrile and do not have any COVID-19-type symptoms at a minimum before caring for the patients for the day and as rapid testing is further developed and accessible, may need to be performed on a regular basis to the OR personnel because asymptomatic shed of the virus can occur with some frequency. As testing and clinical information become more available and accurate, it is paramount that patient and health care worker safety is the number one priority. Likely the most important component of successfully and safely performing elective total hip and knee surgery is accurate and accessible preoperative COVID-19 testing.
It is important to understand that the specific COVID-19 testing is not a minimal requisite to performing total hip and knee arthroplasty in patients with the expectations for same day discharge. Over the past few years, there has been substantial research that provides guidance on safe patients selection, optimal pathways and protocols, and the essential elements for successfully and safely performing hip and knee arthroplasty in the outpatient and/or ASC environment [[3], [4], [5]], along with recommendations to avoid the most common pitfalls and barriers to discharge such as postoperative urinary retention [6]. It is mandatory that surgeons, institutions, and programs develop and maintain appropriate outpatient arthroplasty protocols, in addition to the additional COVID-19 testing [4].
There is a definite trend in United States over the past few years in performing a greater percentage of total hip and knee arthroplasty patients in the outpatient environment with same day discharge to home. Recent developments include removing total knee arthroplasty off the inpatient-only list in 2018, followed by removing total hip arthroplasty off the inpatient-only list and allowing total knee arthroplasty to be performed in Medicare beneficiaries in a freestanding ASC January 2020. There have been substantial advantages purported for performing hip and knee arthroplasty in the outpatient setting that have included improved patient satisfaction [7], less complications, and minimizing the inpatient hospital burden. It has been further shown that outpatient total knee arthroplasty is feasible in the Medicare population [8]. The latter benefits have the potential to becoming increasingly important in the post-COVID-19 era. From a health care resource perspective, the COVID-19 pandemic has highlighted our national health care infrastructure in some geographies may not have capacity to handle large numbers of medically ill patients without compromising the ability to provide elective surgical care, such as hip and knee arthroplasty. The ASCs can provide a great benefit to the health care system by expanding their capacity to accept hip and knee arthroplasty patients who meet medical and surgical criteria to safely discharge the same day. This conserves bed capacity for the larger inpatient hospitals to safely accept and treat medically ill patients, like those with respiratory illness from COVID-19. This impact will not only be prevalent in the short term, but will also be lasting as it has become known that COVID-19 will continue in our society for the next few years until larger, broad-based immunity is enacted through a vaccine and consistent exposure to the virus by the population. ASC infrastructure will face a challenge in terms of capacity to handle these larger and more complex surgical procedures such as hip and knee arthroplasty. Although COVID-19 has accelerated the push for hip and knee arthroplasty within the outpatient setting, ASCs have been addressing the facility limitations over the past few years because of external forces led by the government and Center for Medicare and Medicaid Services. Now that Medicare beneficiaries are able to undergo knee arthroplasty in freestanding ASCs, these facilities have been attempting to address their subsequent shortcomings that include limited capacity in terms of available square footage, inadequate central sterile processing capacity for larger numbers of trays, and in some cases, lack of qualified staff who are capable of caring for hip and knee arthroplasty patients. Compared with the traditional smaller surgeries performed in ASCs, total hip and knee arthroplasty can be associated with more blood loss, more soft tissue trauma, and unique perioperative issues in the first few hours after surgery that may challenge the ASC staff. However, with proper training, experience, and mentoring from others with experience discharging hip and knee arthroplasty patients the same day of surgery, the ASC staff can become proficient and capable in caring for these patients.
Finally, patient demand will almost certainly fuel an increasing surgical volume of hip and knee arthroplasty into the ASC facilities. Although traditionally only about half of patients were aware that outpatient total joint arthroplasty was an option as reported in one recent study [9], the increased patient demand in the post-COVID-19 era will be primarily driven by the lingering fear by patients and their families that hospitals are the primary societal location of the highly contagious and potentially lethal SARS-CoV-2 virus. This fear has spawned from the data (and media coverage) demonstrating this particular virus is highly contagious and can affect even well-protected health care workers and can be spread in a high percentage of asymptomatic individuals and in some cases, can prove fatal by mechanisms not currently understood.
Conclusion
In summary, the ambulatory and outpatient setting will not be exempt from the significant change and paradigm change occurring as a result of the COVID-19 pandemic. ASCs and hospitals will have a unique set of challenges and also a unique opportunity to be the beneficiary of an accelerated push for the hip and knee arthroplasty to be performed in the outpatient setting. Subsequently, there should be a significant effort and commitment to putting together pathways, protocols, resources, and facilities that can safely care for the hip and knee arthroplasty patient with a plan for same day discharge, to spare and conserve health care resource consumption. From our own personal experience and implementation of rapid redeployment of resources, staff, and supplies with a close partnership and collaboration with our ASCs, IU Health was able to successfully treat all of the COVID-19 patients without overburdening the system and we anticipate also being able to treat these patients safely going forward with a renewed emphasis on early discharge, both from the ambulatory surgery center as well as from within the hospital itself.
Acknowledgment
The author would like to acknowledge Dr. Ripley Worman and Juan Guzman from Indiana Univerisity Health for their partnerhip and collaboration in developing and implimenting the plan described in this article.
Footnotes
This article is published as part of a supplement supported by the American Association of Hip and Knee Surgeons and by an educational grant from Aerobiotix.
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.arth.2020.04.051.
The author has ownership shares in an amulatory surgery center that is jointly owned and operated by Indiana University Health and SCA.
Appendix A. Supplementary Data
References
- 1.Vannabouathong C., Devji T., Ekhtiari S., Chang Y., Phillips S.A., Zhu M. Novel coronavirus COVID-19: current Evidence and evolving strategies. J Bone Joint Surg Am. 2020:e1. doi: 10.2106/JBJS.20.00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DePhillipo N.N., Larson C.M., O’Neill O.R., LaPrade R.F. Guidelines for ambulatory surgery centers for the care of surgically necessary/time-sensitive orthopaedic cases during the COVID-19 pandemic. J Bone Joint Surg Am. 2020:e1. doi: 10.2106/JBJS.20.00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ziemba-Davis M., Caccavallo P., Meneghini R.M. Outpatient joint arthroplasty-patient selection: update on the outpatient Arthroplasty risk assessment score. J Arthroplasty. 2019;34:S40–S43. doi: 10.1016/j.arth.2019.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Meneghini R., Gibson W., Halsey D., Padgett D., Berend K., Della Valle C.J. The American association of hip and knee surgeons, hip society, knee society, and American academy of orthopaedic surgeons position statement on outpatient joint replacement. J Arthroplasty. 2018;33:3599–3601. doi: 10.1016/j.arth.2018.10.029. [DOI] [PubMed] [Google Scholar]
- 5.Kim K.Y., Feng J.E., Anoushiravani A.A., Dranoff E., Davidovitch R.I., Schwarzkopf R. Rapid discharge in total hip arthroplasty: utility of the outpatient Arthroplasty risk assessment tool in predicting same-day and next-day discharge. J Arthroplasty. 2018;33:2412–2416. doi: 10.1016/j.arth.2018.03.025. [DOI] [PubMed] [Google Scholar]
- 6.Ziemba-Davis M., Nielson M., Kraus K., Duncan N., Nayyar N., Meneghini R.M. Identifiable risk factors to minimize postoperative urinary retention in modern outpatient rapid recovery total joint arthroplasty. J Arthroplasty. 2019;34:S343–S347. doi: 10.1016/j.arth.2019.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Kelly M.P., Calkins T.E., Culvern C., Kogan M., Della Valle C.J. Inpatient versus outpatient hip and knee arthroplasty: which has higher patient satisfaction? J Arthroplasty. 2018;33:3402–3406. doi: 10.1016/j.arth.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 8.Courtney P.M., Froimson M.I., Meneghini R.M., Lee G.C., Della Valle C.J. Can total knee arthroplasty be performed safely as an outpatient in the Medicare population? J Arthroplasty. 2018;33:S28–S31. doi: 10.1016/j.arth.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Meneghini R.M., Ziemba-Davis M. Patient perceptions regarding outpatient hip and knee arthroplasties. J Arthroplasty. 2017;32:2701–2705. doi: 10.1016/j.arth.2017.04.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.