Abstract
The objective of this report is to better understand the initial CT imaging spectrum and the relationship between clinical characteristics and initial CT imaging features of an imported family cluster cases involving 7 laboratory-confirmed COVID-19 patients. We find that initial CT findings of 4 patients were positive within one week after the onset of symptoms and 1 patient was negative before the onset of symptoms. Two asymptomatic patients had typical CT abnormalities. The initial CT imaging manifestations are mainly peripheral or subpleural ground-glass opacities and ground-glass with consolidation. Our report is of potential guiding value for the initial CT screening of imported familial cluster cases since the imported cases have an identified time of infection.
Keywords: SARS-CoV-2, COVID-19, Family cluster, CT imaging
Highlights
-
•
The spectrum of initial CT imaging and the relationship between clinical characteristics and initial CT imaging features of an imported family cluster case involving 7 laboratory-confirmed COVID-19.
-
•
Our report is of potential guiding value for the initial CT screening of imported familial cluster cases since the imported cases have an identified time of infection.
1. Introduction
Pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; previously known as 2019-nCoV) has been starting in Wuhan, Hubei province, China since December 2019, it was later named Corona Virus Disease 2019(COVID-19) and has been declared a global health emergency by the World Health Organization (WHO) [1,2].
Many previous studies have reported the CT imaging features and correlation of chest CT and RT-PCR testing infected with SARS-CoV-2 [[3], [4], [5], [6]]. The main reports of family cluster cases mainly focus on describing the epidemiological characteristics [[7], [8], [9]], while our report describe clinical characteristics, initial CT imaging features and the relationship between these indicators of an imported family cluster cases involving 7 laboratory-confirmed COVID-19 patients.
2. Case report
A Retrospective analysis was made on the epidemic history, symptoms, laboratory examination, CT imaging of a family cluster of 7 confirmed patients in two designated hospitals for the treatment of COVID-19 in city of Pingliang (Gansu province, China), and the correlation of the above indicators was analyzed. The patients were admitted from January 31, 2020 to February 11, 2020 and confirmed by RT-PCR tests successively.
2.1. Clinical characteristics
Asymptomatic carrier 1(confirmed with COVID-19 later) traveled from the epidemic area of Wuhan to Shanxi province (a province in western China), and had contact with asymptomatic carrier 2 (confirmed with COVID-19 later) on January 20, 2020, and asymptomatic carrier 3 (Patient 5 in this report) had contact with asymptomatic carrier 2 on January 24, 2020. Patient 3 is the baby of patient 5,and they are together all the time. Patients 5 and 3 traveled from Shanxi province to Pingliang city of Gansu province and had contacted with patiens1, 2, 4, 7 on January 26, 2020. Patients 1 and 2 contacted with patient 6 on January 30, 2020.
This familial cluster cases caused by close contact between patient 5 or 3 and other family members, since others had no travel history.
In all 7 patients included in the report (2 men, 4 women and 1female infant), the median age was 33 (ranging from 1 to 55). Patients 1–3 admitted to hospital after symptoms onset and were diagnosed with COVID-19 successively. Patient 4–7 admitted to hospital for screening because of close contact with the confirmed patients. Patients 4 and 5 remained asymptomatic during hospitalization, while patients 6 and 7 had symptoms successively. The numbers of patients 1–7 represent the sequence in which the RT-PCR tests are positive.
Patients 1, 2, 3, 6, 7 developed symptoms on the 4th, 6th, 9th, 10th and 13th day after exposure to the source of infection separately. Patient 3 who is a 1 year old female infant presented with diarrhea, which is different from other adults presented with fever and respiratory and/or nervous system symptoms such as cough, fatigue, short of breath and headache. The laboratory results were as follows: The white blood cell counts and Lymphocyte counts were reduced with C-reactive protein level increased in patient 1, while were in normal range for the rest 5 patients except patient 3 has increased white blood cell counts and Lymphocyte counts. Procalcitonin were increased in 5 patients except patient 2 and 3. Clinical characteristics of the patients are shown in Table 1 . Summary of Laboratory examination results are shown in Table 2 .
Table 1.
Clinical characteristics of the patients.
| Patient number | Age | Sex | Time interval of onset after exposure | Time interval of initial CT after exposure/onset | Clinical symptoms |
|---|---|---|---|---|---|
| 1 | 29 | Male | 4 | 11/7 | Fever, cough, headache, limb joint pain |
| 2 | 27 | Female | 6 | 8/2 | Fever, cough, fatigue |
| 3 | 1 | Female | 9 | 15/6 | Diarrhea |
| 4 | 55 | Female | – | 12/– | Asymptomatic |
| 5 | 33 | Female | – | 15/– | Asymptomatic |
| 6 | 54 | Male | 10 | 9/– | Short of breath |
| 7 | 35 | Female | 13 | 15/2 | Cough, pharyngeal itching |
Table 2.
Summary of laboratory examination results of the familial cluster with COVID-19.
| Patient1 | Patient2 | Patient3 | Patient4 | Patient5 | Patient6 | Patient7 | |
|---|---|---|---|---|---|---|---|
| White blood cell count | |||||||
| (× 109 cells per L) (normal range3.5–9.5) |
2.96 | 4.37 | 9.72 | 3.91 | 4.66 | 4.98 | 4.34 |
| Lymphocytes | |||||||
| (× 109 cells per L) (normal range1.1–3.2) |
0.84 | 1.17 | 7.62 | 1.88 | 1.66 | 2.15 | 1.23 |
| C-reactive protein | |||||||
| (mg/L) (normal range0–10) |
18.2 | 2.9 | 3.1 | 4 | 4.5 | 4.3 | 1.6 |
| Serum procalcitonin | |||||||
| (ng/ml) (normal range0–0.5) |
0.7 | 0.5 | 0.3 | 1 | 1.4 | 0.9 | 1.4 |
2.2. Initial manifestations of CT
Patient 6 underwent CT scan 1 day before symptoms onset, and the initial CT image was negative, and his follow-up CT 1 day after symptoms onset showed a single ground-glass opacity in the middle lobe of the right lung (Fig. 1 ). Here, we analyzed the CT images of 6 other patients. Patients 1–5, 7 underwent CT scans 11/7, 8/2, 15/6, 12/−, 15/−, 15/2 days after exposure/onset. The earliest initial CT scan after exposure is the 8th day and the latest is the 15th day. The earliest initial CT scan after symptoms onset was the 2nd day, and the latest was the 7th day. CT findings in the early stage of symptom onset showed single ground-glass opacity or ground-glass with consolidation involving multiple lobes, and about one week after symptoms onset showed multiple ground-glass opacities or ground-glass with consolidation involving multiple lobes. Although ground-glass with consolidation can be seen at the early stage and 1 week after symptoms onset, the extent and degree of consolidation of lesions are different, and the latter is more severe. Weighting in CT imaging findings: pure ground-glass (3/6, 50%), crazy-paving sign (0/6, 0%), ground-glass with consolidation (3/6, 50%), multi-lobe involvement (5/6, 83.30%), pure consolidation/pure nodule (0/6, 0%), pleural effusion (0/6, 0%), lymphadenopathy (0/6, 0%). The initial CT images of patient1–5, 7 are shown in Fig. 2 .
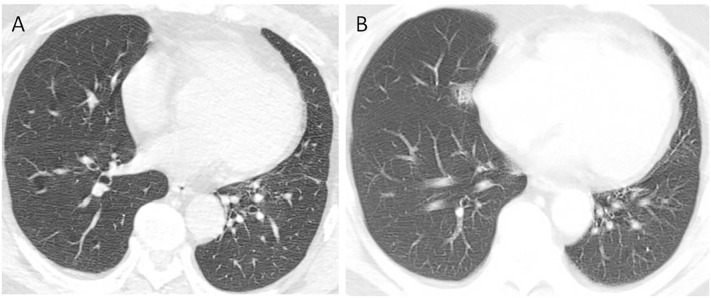
Fig. 1.
A 54-year old male (patient6) with the initial non-contrast chest CT (1 day before the onset of symptoms) shows normal after 9 days exposure to infectious source (A) His follow-up CT (1 day after the onset of symptoms) two days later shows a single ground-glass opacity in the middle lobe of the right lung, it looks like reticular due to noises (B).
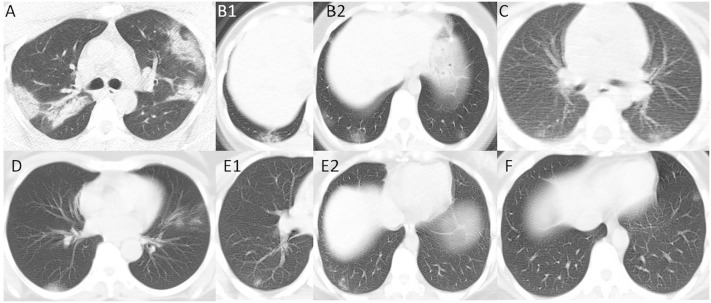
Fig. 2.
29-year old male (patient1), non-contrast chest CT on the 7th day after the onset of symptoms (the 11th day after exposure to the source of infection) shows multiple patchy consolidation shadows in bilateral lungs, which are basically distributed symmetrically along the bilateral upper lobes (A). 27-year old female (patient2), non-contrast chest CT on the 2th day after the onset of symptoms (the 8th day after exposure to the source of infection) shows ground-glass with patchy consolidation shadow in right lower lobe (B1). Multiple ground-glass opacities in bilateral lower lobes (B2). 1-year old baby (patient3), non-contrast chest CT on the 6th day after the onset of symptoms (the 15th day after exposure to the source of infection) shows multiple ground-glass opacities in the dorsal basal segments of the bilateral lower lobes (C). 55-year old female who's asymptomatic (patient4), non-contrast chest CT on the 12th day after exposure to the source of infection shows ground-glass shadows along the vascular bundle in the left upper lobe and lamellar consolidation shadows in the right lower lobe (D). 33-year old female who's asymptomatic (patient5), non-contrast chest CT on the 15th day after exposure to the source of infection shows multiple ground-glass opacities in the right lower lobe (E1, E2). 35-year old female (patient7), non-contrast chest CT on the 2th day after the onset of symptoms (the 15th day after exposure to the source of infection) shows solitary ground-glass opacity in left lower lobe (F).
3. Discussion
The source of infection is transmission from multiple asymptomatic individuals in this report, indicating that the disease is infectious during the incubation period. The novel coronavirus mainly binds to the cellular angiotensin-converting enzyme 2 (ACEI-2) receptor and causes disease. ACEI-2 cells are highly expressed in the respiratory tract, digestive tract and cardiovascular system. ACEI-2 is highly expressed in respiratory alveolar type II epithelium [10]. Among the 7 patients, 5 showed symptoms successively, 2 remained asymptomatic, 4 adults showed common symptoms of fever, cough, fatigue, shortness of breath, and unusual limb joint pain and headache, and 1 infant showed only symptom of diarrhea, which was significantly different from adults.
After exposure, 7 patients underwent the initial CT scan at different times. Patients 1, 2, 3 and 7 underwent initial CT scan at different times after onset,and CT findings were all abnormal. Here, we do not know the CT findings at the onset of symptoms, but there is a literature report that CT is normal at onset of symptoms of a case [6]. The early CT findings after onset were single ground-glass opacity or ground-glass with consolidation involving multiple lobes. About one week after onset, CT findings were multifocal ground-glass opacities or ground-glass with consolidation involving multiple lobes. The CT findings at different times after onset shown ground-glass with consolidation-, but the lesions at about one week after onset were more severe. Patient 6 underwent the initial CT scan on the day before onset, and the result was normal. The second CT scan was performed on the first day after onset, showing a unique ground-glass opacity at the middle lobe of right lung. Two asymptomatic patients underwent the initial CT scan on the 12th and 15th days after exposure, among which the CT results of the older patient was more severe than that of the younger patient. Symptoms first onset in young man, and finally in older man, with the most severe symptoms and CT findings in young man, mild symptoms and CT findings in infant, possibly because of the body's different immune responses to viral infections. CT images were all positive on the 15th day after exposure of this familial cluster. Therefore, we suggested that when performing a CT scan on people with a history of epidemiology, it is possible to perform CT scan one day after onset. If CT result is negative, re-examination should be completed within one week. Asymptomatic patients can undergo CT scan on the 10th to 15th day after exposure. If the image still shows normal, follow-up CT examination should be performed every 3 to 5 days.
A Report of 1014 Cases about correlation of chest CT and RT-PCR Testing in COVID-19 in China published by Tao Ai and Zhenlu Yang showed that with RT-PCR as a reference, the sensitivity of chest CT imaging for COVID-19 was 97%, chest CT may be considered as a primary tool for the current COVID-19 detection in epidemic areas [6]. Our report showed that the positive rate of initial CT examination was 6/7 (85.7%), similar to Tao Ai and Zhenlu Yang's report. In this group of cases we reported, the course of disease of most patients is in the early stage and one case is in the advanced stage. The sensitivity of leukopenia, lymphocytopenia, and C-reactive protein at the initial stage of onset was lower than that of CT. Five patients in this group started with elevated procalcitonin, which is inconsistent with current studies (most are normal) [8]. After infection, the symptom of infant is mild and atypical. The initial CT result after the onset of symptom is mild than that of adults. Laboratory examination is also different from that of adults, which requires our attention.
Family cluster cases have a clear source of infection and time to contact the source of infection, so when there are diagnosed patients in the family, in addition to the close contacts should be isolated, but also according to the time of contact, whether or not have symptoms to establish personalized CT screening in order to manage the disease most efficiently. Our study described the epidemic history, symptoms, laboratory examination, CT imaging of a family cluster, and analyzed the correlation among these indicators, but only one family cluster was involved, and the correlation between different family clusters needs further study. It is hoped that our report will provide help for the initial CT screening of family cluster infected with SARS-Cov-2.
Sources of funding
Lanzhou University's Key Research Base Construction Project of "Special Funds for Basic Research Business of Central Universities" of China (lzujbky-2020-kb27).
References
- 1.Park M., Thwaites R.S. COVID-19: lessons from SARS and MERS. Eur J Immunol. 2020 doi: 10.1002/eji.202070035. [DOI] [Google Scholar]
- 2.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bai Y., Yao L., Wei T. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu P., Zhu J., Zhang Z. A familial cluster of infection associated with the 2019 novel coronavirus indicating potential person-to-person transmission during the incubation period. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan X., Chen D., Xia Y. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi H., Han X., Jiang N. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen Y., Guo Y., Pan Y. Structure analysis of the receptor binding of 2019-nCoV. Biochem Biophys Res Commun. 2020 doi: 10.1016/j.bbrc.2020.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]