Abstract
At the beginning of the 21st century, a new deadly infectious disease known as severe acute respiratory syndrome (SARS) was recognized as a global public health threat. Subsequently, ten years after the initial SARS cases occurred in 2002, new cases of another atypical respiratory disease caused worldwide concern. This disease became known as Middle East respiratory syndrome (MERS) and was even more lethal than SARS. Currently, history has repeated itself with the emergence of a new Chinese epidemic at the end of 2019. For this respiratory disease, called COVID-19, a novel coronavirus (SARS-CoV-2) was identified as the etiologic agent. In sum, SARS, MERS and COVID-19 are caused by recently discovered coronaviruses that cause flu-like illnesses, but with a clinical outcome that tends to be more severe. As a result of the current importance of coronaviruses in global public health, we conducted a review to summarize and update, above all, the epidemiological historical aspects of the three major diseases in humans caused by coronaviral infection.
Electronic supplementary material
The online version of this article (10.1007/s00705-020-04628-0) contains supplementary material, which is available to authorized users.
Introduction
Prior to the 21st century, coronaviruses (CoVs) were considered pathogens of great relevance in veterinary medicine but with a reduced impact on human health [1–4]. However, a greater global concern for CoVs in human health began with the epidemic of severe acute respiratory syndrome (SARS) in 2002-2003 and Middle East respiratory syndrome (MERS) in 2012 [5–8]. In addition, at the end of December 2019, another CoV outbreak emerged, again causing global concern in human public health [9–13].
The family Coronaviridae includes enveloped viruses with a positive-sense, single-stranded RNA genome of approximately 30 kb in size. Consequently, they have the largest genomes of RNA viruses. Based on their antigenic and genetic properties, CoVs are organized into four genera: Alphacoronavirus, Betacoronavirus, Gammacoronavirus, and Deltacoronavirus. SARS-CoV and MERS-CoV belong to the genus Betacoronavirus [14, 15]. Recently, full-genome sequencing and phylogenetic analysis of the novel SARS-CoV-2 (previously known as 2019-nCoV) grouped it in the same genus [16, 17].
Four main proteins are encoded by the coronaviral genome: spike (S), envelope (E), membrane (M) and nucleocapsid (N). Each protein plays an individual role in the structure of the viral particle, but they are also involved in other functions of the replication cycle [14, 15]. For more details, see Fig. 1 and the supplementary file.
Fig. 1.
Viral replication cycle in eukaryotic cells. The virus binds to a cell-surface receptor (ACE2 for SARS-CoV and SARS-CoV-2; DPP4 for MERS-CoV), and fusion of the virion and cell membrane occurs on the cell surface or from within endosomes, depending on the virus. The fusion is triggered by low pH, leading to the release of the nucleocapsid into the cytoplasm. The viral genome is translated to produce proteins 1a and 1ab (the latter by recoding ribosomal translation or ribosomal frameshift). These 1a and 1ab proteins are processed by viral proteases to produce a variety of viral proteins, including RNA-dependent RNA polymerase (RdRp), proteins that remodel cell membranes to form structures that are used as viral RNA synthesis sites, enzymes that catalyze several steps in the synthesis of the 5’-terminal cap structure of the mRNA, and an exonuclease involved in proofreading during genome replication. The other viral proteins are encoded by a nested set of mRNAs that share a common leader sequence (5’ UTR) at the 5’ end. Discontinuous RNA synthesis occurs during synthesis of the negative RNA strand. Most of the positive strand is not copied, probably because it loosens when the polymerase completes synthesis up to the 5’ UTR. The resulting negative-strand RNAs, with 3’ UTR sequences at the ends, are then copied to form mRNAs. These mRNAs are translated to form the structural and non-structural proteins. M, S and E proteins attached to the membrane are inserted into the lumen of the endoplasmic reticulum and then move to the site of viral assembly, the intermediate compartment of the endoplasmic reticulum-Golgi (ERGIC). Full-length negative-strand RNAs are produced, and these serve as templates for the synthesis of full-length positive-strand RNAs, which are then encapsulated by protein N. The nucleocapsid buds into the ERGIC, acquiring a membrane that contains the proteins S, E and M. Viral particles are transported to the plasma membrane in smooth-walled vesicles and released from the cell by exocytosis when the carrier vesicle fuses with the plasma membrane [26, 28]
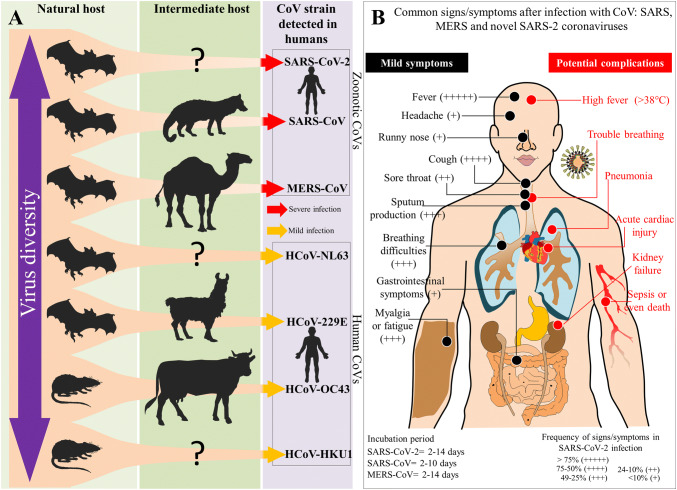
CoVs infect birds (γ- and δ-CoVs) and several species of mammals (mainly α- and β-CoVs), including humans [14, 15, 18]. A review of recent sequences in databases has shown that all human CoVs are of animal origin [19–23]. SARS-CoV-2, SARS-CoV, MERS-CoV, HCoV-229E and HCoV-NL63 probably originated from bats, whereas HCoV-OC43 and HKU1 probably originated from rodents [23, 24]. It is important to highlight that bats, which are considered the primordial hosts, can have different viral populations in the same species, facilitating recombination and the emergence of new variants [22, 25]. These new variants are capable of infecting intermediate hosts, and the combination of deletion and recombination of genes results in drastic changes, such as changes in the tissue tropism of the virus, which tends to cause general changes in the pattern of disease. Examples of this include SARS-CoV and MERS-CoV, which were possibly transmitted directly to humans from market civets and dromedaries, respectively (Fig. 2A) [23, 26].
Fig. 2. A.
Summary of the groups of animals that serve as natural and intermediate hosts for the seven CoVs that can cause disease in humans. The different CoVs can cause moderate or severe infections in humans, and some of the intermediate hosts of these viruses are not yet known. B. Infections by different CoVs cause signs and symptoms that overlap regardless of the type of virus that causes the disease. The signs and symptoms can affect different systems and organs, varying from mild symptoms in most cases (fever, cough, myalgia, headache, and runny nose, among other symptoms), which can progress to complications with a worse prognosis (pneumonia, kidney failure, breathing problems, acute cardiac injury, sepsis and death). The incubation period differs between CoVs, generally ranging from 2 to 14 days [25, 65–69]
SARS-CoV: the first highly pathogenic human CoV outbreak of the 21st century
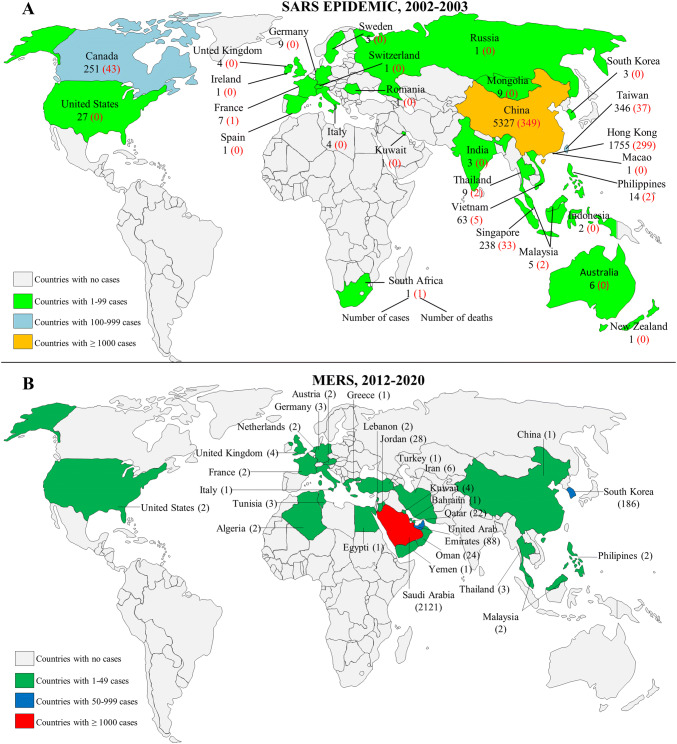
As mentioned above, in 2002, an outbreak of a new disease (SARS) was described for which a novel CoV, known as SARS-CoV, was identified as the etiologic agent [27, 28]. The disease reached pandemic proportions, as it spread to 29 countries on five continents, causing a total of 8096 laboratory-confirmed cases of SARS with 774 deaths by August 2003, when aggressive public health intervention measures managed to contain a potential pandemic (Fig. 3A).
Fig. 3.
Current geographic distribution of SARS (A) and MERS (B). Data are from the World Health Organization (https://www.who.int/csr/sars/country/table2004_04_21/en/). http://www.emro.who.int/health-topics/mers-cov/mers-outbreaks.html) and were collected through March 23, 2020
The first known case of SARS, caused by the novel CoV, was represented by a 45-year-old man in November 2002 in the city of Foshan, Guangdong Province, China [29, 30]. The mysterious respiratory disease, which in the future would be called SARS, had high fever (>38°C), followed by dry cough and rapid progression to respiratory failure as clinical manifestations (Fig. 2B) [31, 32]. Consequently, a clinical picture of atypical pneumonia was noted; however, the detection of the new infectious agent, which was being transmitted from human to human, did not occur until several months later. Thus, it was only in April 2003 that the World Health Organization (WHO) announced that the SARS epidemic was caused by a new pathogen, a member of the CoV family never seen before in humans [33, 34].
Initial SARS cases were restricted to China until February 21, 2003, when an elderly doctor who was treating patients with “atypical pneumonia” in Guangdong traveled to Hong Kong and stayed at a hotel in the Kowloon district. It was at this hotel that some guests were infected and, as a result of the movement of these infected individuals, SARS-CoV spread to a considerable part of the world [27]. The doctor was admitted to a local hospital with symptoms of acute respiratory disease and later died of the disease. It is recognized that from this index case, seven other people who were on the same floor in the hotel were directly affected by SARS. Practically all of these people were foreign visitors, including three visitors from Singapore, one visitor from Vietnam, and two visitors from Canada. Soon after returning to their countries, these infected visitors triggered outbreaks in their places of origin. However, the high speed of the scientific response in understanding this new viral disease was unmatched and contributed to the success of SARS containment.
With the discovery of a novel CoV responsible for the SARS epidemic, new questions need to be clarified as to which animal is the definitive host of this virus. Could any animal have acted as an intermediate host involving the transmission of the virus to humans? To solve this puzzle, it was necessary to return to the initial cases of SARS. However, in the first retrospectively identified case of SARS in the city of Foshan, it was unclear where and how the man had contracted the disease, but it was known that he had not traveled for weeks but had been exposed to different animals and had prepared chicken, domestic cat, and snake for family consumption [29]. Additionally, at the beginning of the SARS epidemic, similar to the first case, the disease afflicted restaurant workers who handled wild mammals as exotic foods [28, 35]. Subsequently, SARS-CoV and/or anti-SARS-CoV antibodies were found in masked palm civets (Paguma larvata) and in animals that were being handled in a market [26, 36]. However, it was only later that studies showed that populations of palm civets on farms were negative for SARS-CoV, while those in markets populations showed positive results (i.e., had a higher SARS-CoV antibody prevalence), suggesting that market animals were probably intermediate hosts and were possibly infected from another source in the markets [26, 37, 38]. Subsequent studies showed that several CoVs were endemic in bats, including a CoV closely related to SARS-CoV. These findings suggest that bats are the natural host of all strains of CoV [19, 22, 39–41].
MERS-CoV: another worrying outbreak of CoV respiratory infection
MERS-CoV is a human CoV that causes SARS-like disease in the Middle East. The first reported case of the virus was in a 60-year-old Saudi man who had a 7-day history of fever, cough, sputum, and shortness of breath and was admitted to a private hospital in Jeddah, Saudi Arabia, on June 13, 2012, and died 11 days after admission to the hospital [42]. A few months later, on September 12 of the same year, a 49-year-old man was transferred from Qatar with acute renal failure and bilateral pneumonia. Molecular tests of patient samples performed in the same month detected a viral genome highly similar to that described in the case of the Saudi Arabian patient [43]. The people who had had close contact with the patient, including health professionals, family and friends, were followed up until ten days after the last contact with the patient in an attempt to better understand the form of dissemination and viral contagion. Thus, 64 people were followed for ten days after their last contact with the hospitalized patient, and there was no confirmed evidence of continuous person-to-person transmission, despite active extensive contact tracking [43, 44].
Health authorities were alerted to the circulation of the novel CoV, classified in November 2012 as a new β-CoV closely related to the CoVs HKU4 and HKU5 present in bats [42]. In December 2012, the European Center for Disease Prevention and Control (ECDC) established a list of countries at risk that included Bahrain, Iran, Iraq, Israel, Jordan, Kuwait, Lebanon, Palestine, Oman, Qatar, Saudi Arabia, Syria, the United Arab Emirates, and Yemen [45]. Subsequently, in May 2013, viral infection was identified in a French patient who had a severe respiratory disease. The male patient had been in the United Arab Emirates and had recently returned to France. A protocol for monitoring contacts close to the patient was adopted, as well as for tracking individuals who had traveled together to the United Arab Emirates, to detect possible other cases and to prevent human-to-human transmission. The contact screening identified a secondary case in a patient admitted to the same hospital room, thereby confirming the person-to-person transmission of the disease [46].
Cases of the disease continued to be identified, and as of June 2013, 55 confirmed cases had been reported, with a mortality rate of 56% due to the 31 deaths caused by the virus. The reported cases occurred in different regions: 45 cases were in countries in the Middle East (Saudi Arabia, Jordan, Qatar, and the United Arab Emirates), eight were in Europe (France, Italy, and the United Kingdom) and two were in Africa (Tunisia) [47]. Viral infection was the topic at the Sixty-Sixth World Health Assembly in Geneva, Switzerland, with the statement that “the novel coronavirus is a threat to the whole world”, mainly because of a lack of information related to the virus [48].
In early 2014, there was an abrupt increase in the number of MERS-CoV infections in the Jeddah region of Saudi Arabia, the location of the first reported case of the disease. A total of 255 cases were identified from January 1 to January 16, with an average age of 45 years among patients, with person-to-person transmission identified mainly in people who had contact with a health unit in the region [49]. Two cases of the infection were identified in the Netherlands after two individuals from the same family returned from a pilgrimage to Medina and Mecca (Saudi Arabia), both aged 70 and over [50]. In April 2014, the first case of infection in Malaysia was identified in a male patient over the age of 50. The patient had traveled to Saudi Arabia days before to make a pilgrimage. There were no positive cases in their close contacts [51]. The first reported case of MERS-CoV infection in the USA was from an individual who had traveled to Saudi Arabia. The case was confirmed on May 2, 2014. A second imported case was also identified, unrelated to the first case [52]. The number of cases of the disease continued to rise. As of May 2014, more than 570 cases had been reported to WHO, with at least 173 deaths [53].
MERS-CoV continued to spread across countries, and the first case of the virus in South Korea was reported on May 20, 2015. The following month, an outbreak in the country brought fear to the population, with more than a hundred confirmed cases [54]. On May 28, a 44-year-old traveler from South Korea was admitted to a hospital in China. MERS-CoV infection was confirmed on May 29, marking the first case confirmed in the laboratory in China. Fear of a new pandemic grew [55].
According to WHO, since April 2012, 2519 laboratory-confirmed cases of MERS-CoV infection had been reported by January 2020. The lethality rate is 34.3%, with 866 confirmed deaths, the majority occurring in Saudi Arabia (2121 cases, including 788 deaths, with a lethality rate of 37.1%) (Fig. 3B) [56].
SARS-CoV-2: again a novel virus and now the CoV pandemic
Surprisingly, at the end of December 2019, an outbreak of mysterious pneumonia occurred in Wuhan City, Hubei Province, China [57, 58]. It was observed that the etiologic agent of the disease was a novel CoV, previously designated 2019-nCoV by WHO and, more recently, SARS-CoV-2 by the International Committee for Taxonomy of Viruses [59, 60]. Consequently, China has been the epicenter of the emergence of the disease called COVID-19 (Coronavirus disease 2019), which WHO characterized the COVID-19 on March 11, 2020 as a pandemic [61, 62].
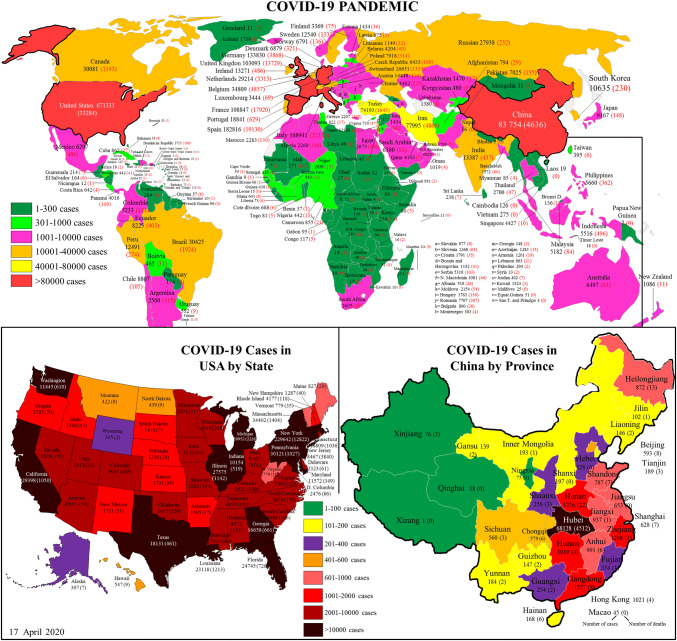
For the initial cases of COVID-19, it was observed that many patients, before falling ill, were exposed to wild animals at a wholesale seafood market in Huanan (Wuhan, China), a place where birds, bats, snakes, and other farm animals were traded [57, 63]. In this scenario, a zoonotic origin of these initial cases was suggested; however, the transmission from person to person was soon recognized due to the various cases of COVID-19 within families and among people who did not go to the Huanan market. Already in January 2020, the disease spread rapidly inside and outside Hubei Province, and even other countries. As of April 17, 2020, a total of 2,114,269 cases of COVID-19 were confirmed worldwide. It is important to note that ~60% (1,265,765/2,114,269) of these cases occurred in Spain, Italy, United States of America, Germany and France. Internationally, cases have been reported in 203 countries, areas or territories on five continents (Fig. 4) [64].
Fig. 4.
Current geographic distribution of COVID-19 cases. Data are from the European CDC (https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases) and were collected through April 17, 2020. At that time, the total number of cases was 2,114,269, with 145,144 deaths
In case series studies, the clinical characteristics of patients diagnosed with COVID-19 were observed (Fig. 2B). Initially, Huang et al. reported that 66% (27/41) of patients admitted to Jinyintan Hospital (Wuhan, China) had a history of exposure to the wholesale seafood market in Huanan [65]. Later, Chen et al. found that 49% (49/99) of the patients admitted to Jinyintan Hospital had a history of exposure to the same market [66]. Subsequently, with the addition of the studies by Wang et al. [67], Yang et al. [68], and Tian et al. [69], the following clinical characteristics of a total of 689 patients were observed: fever (85%, 587/689), cough (58%, 401/689), myalgia or fatigue (29%, 199/689), sputum production (29%, 96/328), dyspnea (17%, 116/689), pharyngitis (13%, 50/386), dizziness (9%, 13/138), headache (7%, 50/689), hemoptysis (5%, 2/41), diarrhea (7%, 28/427), nausea and vomiting (4.4%, 17/386), rhinorrhea (4%, 9/248), and abdominal pain (2%; 3/138) [65–69].
In the clinical characteristics of patients infected with SARS-CoV-2, it is noted that most patients have relatively moderate symptoms and a good prognosis. However, individuals with moderate clinical status can progress to severe cases, including organ dysfunction (shock, SARS, acute cardiac injury, and acute kidney injury), and many deaths have been reported [67]. Recent European Centre for Disease Prevention and Control situation reports show that in total, there were 145,144 deaths, with most deaths confirmed in USA (33,284) Italy (22,172), Spain (19,130), France (17,920) and United Kingdon (13,729). Thus, the current COVID-19 pandemic had already exceeded the number of cases and deaths from SARS and MERS combined [64].
At the time, the pathophysiology of severe cases of SARS-CoV-2 infection, as well as SARS-CoV and MERS-CoV, were not fully understood. However, the first studies have shown that the ‘cytokine storm’ factor was associated with a greater severity of COVID-19, which was also seen in infections by SARS and MERS CoVs. Increased amounts of proinflammatory cytokines (e.g., IL1B, IFNγ, IP10 and MCP1) were observed in the serum. Additionally, the involvement of the cytokine storm factor in the severity of the disease was corroborated by the observation that patients who needed to be admitted to the intensive care unit (ICU) had higher concentrations of cytokines (GCSF, IP10, MCP1, MIP1A and TNFα) than patients who did not require ICU admission. Presently, in addition to increased secretion of T helper-1 cytokines, increases in secretion of T helper-2 cytokines (e.g., IL4 and IL10) were observed [65]. Based on this background, further studies are needed to characterize the response profiles of the immune system in SARS-CoV-2 infection and to better elucidate the mechanism of pathogenesis.
Although the general population is susceptible to SARS-CoV-2, a higher incidence has been observed in elderly males, especially those with chronic diseases, including diabetes, hypertension, and cardiovascular diseases [65–67]. In this context, the most recent case series study involving 138 patients with COVID-19 found an average age of 56 years in this group. The researchers also noted that patients referred to the ICU were older than patients without the need for referral to the ICU (average age, 66 years vs. 51 years) [67]. An additional study by Chen et al. gave similar results, showing that viral infection is more likely to affect elderly men with comorbidities [66].
Approximately 120 days after the beginning of the COVID-19 epidemic in China, in the emerging COVID-19 pandemic in Italy, France, Iran, Spain, Germany, USA, and the United Kingdom, a large number of cases (2,114,269) and a low mortality rate (~6%) compared to SARS (~10%) and MERS (34.3%) were observed [64]. Faced with this scenario, there is a concern that individuals with mild symptoms may spread the virus more easily due to not seeking medical attention [70]. In addition, another factor of concern regarding the high rate of spread of the virus is related to the recent transmission of the virus in asymptomatic individuals in Germany [71]. Additionally, the large number of SARS-CoV-2 cases suggests that this virus may have acquired the ability to undergo efficient human-to-human transmission, including the ability to bind to human cells. It also suggests that the route of transmission of the virus is via saliva, directly or indirectly, even among patients without a cough or other respiratory symptoms, and shows how contagious SARS-CoV-2 is [10, 70, 72].
In sum, with the efforts of scientists, professionals, and health authorities and the urgency to contain the COVID-19 pandemic, impressive results have been achieved in a short time. Among these results, the following stand out: the determination and availability to the public of several full-genome sequences of SARS-CoV-2 isolates from clinical specimens, and the efforts by the CDC of China and other institutions that are conducting drug screening for viral pneumonia and developing a vaccine for SARS-CoV-2 [73–77]. Another factor that has given rise to hope of preventing, or containment, of the COVID-19 epidemic in China and South Korea concerns the rapid isolation of symptomatic individuals and those suspected of having the disease, including self-isolation of those with mild symptoms, in addition to the constant surveillance of people closest to suspected cases. In this context, South Korea has been a model in combating the spread of the dissemination SARS-CoV-2 infection because the country quickly stabilized its COVID-19 outbreak at the beginning of the spread of virus through widespread rigorous quarantine measures and the opening of drive-through up testing centers. The great challenge of containing the spread of SARS-CoV-2 requires the joint effort of people throughout the world and will involve the immediate application of WHO recommendations for basic preventive measures against the novel CoV and rapid and accurate diagnosis for containment and clinical management. In addition, new advances in applied research involving the disease will be necessary to contain the acceleration of the COVID-19 pandemic.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
Vivaldo G da Costa designed study. Vivaldo G da Costa and Marielena V. Saivish performed data review. Vivaldo G da Costa, Marcos L. Moreli and Marielena V. Saivish performed edition review. All authors reviewed and approved the final version of the manuscript.
Funding
VGC was supported by scholarships from Fundação de Apoio à Pesquisa do Distrito Federal (FAPDF) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior-Brasil (CAPES). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Compliance with ethical standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with research involving human participants and/or animals performed by any of the authors.
Informed consent
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Vivaldo Gomes da Costa, Email: vivbiom@gmail.com.
Marcos Lázaro Moreli, Email: marcos_moreli@ufg.br.
References
- 1.Lee C. Porcine epidemic diarrhea virus: An emerging and re-emerging epizootic swine virus. Virol J. 2015;12(1):193. doi: 10.1186/s12985-015-0421-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bande F, Arshad SS, Hair Bejo M, Moeini H, Omar AR. Progress and challenges toward the development of vaccines against avian infectious bronchitis. J Immunol Res. 2015 doi: 10.1155/2015/424860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vabret A, Mourez T, Gouarin S, Petitjean J, Freymuth F. An outbreak of coronavirus OC43 respiratory infection in Normandy, France. Clin Infect Dis. 2003;36(8):985–989. doi: 10.1086/374222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vabret A, Dina J, Gouarin S, Petitjean J, Tripey V, Brouard J, Freymuth F. Human (non-severe acute respiratory syndrome) coronavirus infections in hospitalised children in France. J Paediatr Child Health. 2008;44(4):176–181. doi: 10.1111/j.1440-1754.2007.01246.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Luo G, Gao SJ, Global Health Concern stirred by emerging viral infections. J Med Virol. 2020 doi: 10.1002/jmv.25683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grubaugh ND, Ladner JT, Lemey P, Pybus OG, Rambaut A, Holmes EC, Andersen KG. Tracking virus outbreaks in the 21st century. Nat Microbiol. 2019;4(1):10–19. doi: 10.1038/s41564-018-0296-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK, Al-Omari A, Hajeer AH, Senga M, et al. Middle East respiratory syndrome. N Engl J Med. 2017;376:6. doi: 10.1056/NEJMsr1408795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fouchier RAM, Kuiken T, Schutten M, Amerongen G, Doornum GJJ, Hoogen BGd, Peiris M, Lim W, Stohr K, Osterhaus ADME. Koch’s postulates fulfilled for SARS virus. Nature. 2003;423(6937):240–240. doi: 10.1038/423240a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bassetti M, Vena A, Giacobbe DR. The novel Chinese coronavirus (2019-nCoV) infections: challenges for fighting the storm. Eur J Clin Invest. 2020 doi: 10.1111/eci.13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson R. Pandemic potential of 2019-nCoV. Lancet. 2020 doi: 10.1016/S1473-3099(20)30068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kock RA, Karesh WB, Veas F, Velavan TP, Simons D, Boera LEG, Dar O, Arruda LB. 2019-nCoV in context: lessons learned? Lancet. 2020 doi: 10.1016/S2542-5196(20)30035-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang W, Tang J, Wei F. Updated understanding of the outbreak of 2019 novel coronavirus (2019-nCoV) in Wuhan, China. J Med Virol. 2020 doi: 10.1002/jmv.25689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodríguez-Morales AJ, MacGregor K, Kanagarajah S, Patel D, Patricia S. Going global—travel and the 2019 novel coronavirus. Travel Med Infect Dis. 2020 doi: 10.1016/j.tmaid.2020.101578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. 2019;16(69):1–22. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Regenmortel MHV, Fauquet CM, Bishop DHL, Carstens EB, Estes MK, Lemon SM, et al. Coronaviridae. In: MHV v R, Fauquet CM, DHL B, Carstens EB, Estes MK, Lemon SM, et al., editors. Virus taxonomy: Classification and nomenclature of viruses Seventh report of the International Committee on Taxonomy of Viruses. San Diego: Academic Press; 200: 835–49. ISBN 0123702003
- 16.Chen Y, Liu Q, Guo D. Coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020 doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paraskevis D, Kostaki EG, Magiorkinis G, Panayiotakopoulos G, Sourvinos G, Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect Gen Evol. 2020 doi: 10.1016/j.meegid.2020.104212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saif LJ (2004) Animal coronaviruses: what can they teach us about the severe acute respiratory syndrome? Rev Sci Tech 23:643–660. 10.20506/rst.23.2.1513 [DOI] [PubMed]
- 19.Hu B, Zeng LP, Yang XL, Ge XY, Zhang W, Li B, Xie JZ, Shen XR, Zhang YZ. Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS Pathog. 2017;13(11):e1006698. doi: 10.1371/journal.ppat.1006698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huynh J, Li S, Yount B, Smith A, Sturges L, Olsen JC, Nagel J, Johnson JB, Agnihothram S, Gates JE, et al. Evidence supporting a zoonotic origin of human coronavirus strain NL63. J Virol. 2012;86:12816–12825. doi: 10.1128/JVI.00906-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ithete NL, Stoffberg S, Corman VM, Cottontail VM, Richards LR, Schoeman MC, Drosten C, Drexler JF, Preiser W. Close relative of human Middle East respiratory syndrome coronavirus in bat, South Africa. Emerg Infect Dis. 2013;19:1697–1699. doi: 10.3201/eid1910.130946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu B, Ge X, Wang LF, Shi Z. Bat origin of human coronaviruses. Virol J. 2015;12:221. doi: 10.1186/s12985-015-0422-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev. 2019 doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forni D, Cagliani R, Clerici M, Sironi M. Molecular evolution of human coronavirus genomes. Trends Microbiol. 2017;25:35–48. doi: 10.1016/j.tim.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Corman VM, Muth D, Niemeyer D, Drosten C (2018) Hosts and Sources of Endemic Human Coronaviruses. Adv Virus Res 100:163-179. (Chapter 8). 10.1016/bs.aivir.2018.01.001 [DOI] [PMC free article] [PubMed]
- 26.Wit E, Nv Doremalen, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Christian MD, Poutanen SM, Loutfly MR, Muller MP, Low DE. Severe acute respiratory syndrome. Clin Infect Dis. 2004;38:1420–1427. doi: 10.1086/420743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peiris JSM, Guan Y, Yuen KY. Severe acute respiratory syndrome. Nat Med. 2004;10(12):s88–s97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu RH, He JF, Evans MR, Peng GW, Field HE, Yu DW, Lee CK, Luo HM, et al. Epidemiologic clues to SARS origin in China. Emerg Infect Dis. 2004;10(6):1030–1037. doi: 10.3201/eid1006.030852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cao W, Fang L, Xiao D. What we have learnt from the SARS epdemics in mainland China? Global Heath J. 2019;3(3):55–59. doi: 10.1016/j.glohj.2019.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 31.Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, Ahuja A, Yung MY, Leung CB, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348:1986–1994. doi: 10.1056/NEJMoa030685. [DOI] [PubMed] [Google Scholar]
- 32.Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, Walmsley SL, Mazzulli T, Avendano M, et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- 33.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, Tong S, Urbani C, Comer JA. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 34.Holmes KV. SARS-Associated Coronavirus. N Engl J Med. 2003;2003(348):1948–1951. doi: 10.1056/NEJMp030078. [DOI] [PubMed] [Google Scholar]
- 35.He JF, Peng GW, Min J, Yu DW, Liang WJ, Zhang SY, Xu RH, Zheng HY, Wu XW, et al. Molecular evolution of the SARS coronavirus during the course of the SARS epidemic in China. Science. 2004;303(5664):1666–1669. doi: 10.1126/science.1092002. [DOI] [PubMed] [Google Scholar]
- 36.Guan Y, Zheng BJ, He YQ, Liu XL, Zhuang ZX, Cheung CL, Luo SW, Li PH, Zhang LJ, et al. Isolation and characterization of viruses related to the SARS coronavirus from animals in southern China. Science. 2003;302:276–278. doi: 10.1126/science.1087139. [DOI] [PubMed] [Google Scholar]
- 37.Kan B, Wang M, Jing H, Xu H, Jiang X, Yan M, Liang W, Zheng H, Wan K, et al. Molecular evolution analysis and geographic investigation of severe acute respiratory syndrome coronavirus- like virus in palm civets at an animal market and on farms. J Virol. 2005;79:11892–11900. doi: 10.1128/JVI.79.18.11892-11900.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tu C, Crameri G, Kong X, Chen J, Sun Y, Yu M, Xiang H, Xia X, Liu S, et al. Antibodies to SARS coronavirus in civets. Emerg Infect Dis. 2004;10:2244–2248. doi: 10.3201/eid1012.040520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lau SKP, Woo PCY, Li KSM, Tsoi HW, Wong BHL, Wong SSY, Leung SY, Chan KH, Yuen KY. Severe acute respiratory syndrome coronavirus- like virus in Chinese horseshoe bats. Proc Natl Acad Sci USA. 2005;102:14040–14045. doi: 10.1073/pnas.0506735102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li W, Shi Z, Yu M, Ren W, Smith C, Epstein H, Wang H, Crameri G, Hu Z, Zhang H, et al. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310:676–679. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- 41.Wang LF, Shi Z, Zhang S, Field H, Daszak P, Eaton BT. Review of bats and SARS. Emerg Infect Dis. 2006;12(12):1834–1840. doi: 10.3201/eid1212.060401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zaki AM, Sv Boheemen, Bestebroer TM, Osterhaus ADME, Fouchier RAM. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Eng J Med. 2012;367(19):1814–1820. doi: 10.1056/nejmoa1211721. [DOI] [PubMed] [Google Scholar]
- 43.Pebody RG, Chand MA, Thomas HL, Green HK, Boddington NL, Carvalho C, Brown CS, Anderson SR, Rooney C, et al. The United Kingdom public health response to an imported laboratory confirmed case of a novel coronavirus in September 2012. Euro Surv. 2012;17(40):20292. [PubMed] [Google Scholar]
- 44.Arwady MA, Alraddadi B, Basler C, Azhar EI, Abuelzein E, Sindy AI, Sadiq BMB, Althaqafi AO, Shabouni O, et al. Middle east respiratory syndrome coronavirus transmission in extended family, Saudi Arabia, 2014. Emerg Infect Dis. 2020;22(8):1395–1402. doi: 10.3201/eid2208.152015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.European Centre for Disease Prevention and Control (ECDC). Update: Severe respiratory disease associated with a novel coronavirus. Stockholm: ECDC; 7 Dec 2012. https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-severe-respiratory-disease-associated-novel-coronavirus. Accessed Feb 2020
- 46.Mailles A, Blanckaert K, Chaud P, Werf Svd, Lina B, Caro V, Campese C, Guéry B, Prouvost H et al (2013) First cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infections in France, investigations and implications for the prevention of human-to-human transmission, France, May 2013. Euro Surveill (18)24:20502. 10.2807/ese.18.24.20502-en [PubMed]
- 47.World Health Organization (WHO), Novel Coronavirus Infection – Update (Middle East Respiratory Syndrome-coronavirus). 2013. https://www.who.int/csr/don/2013_06_07/en/. Accessed Feb 2020
- 48.WHO Director-General Praises the World Health Assembly for its Work. https://www.who.int/mediacentre/news/releases/2013/world_health_assembly_20130527/en/. Accessed Feb 2020
- 49.Oboho IK, Tomczyk SM, Al-Asmari AM, Banjar AA, Al-Mugti H, Aloraini MS, Alkhaldi KZ, Almohammadi EL. MERS-CoV outbreak in Jeddah—a link to health care facilities. N Engl J Med. 2014;372(9):846–854. doi: 10.1056/nejmoa1408636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dirkzwager MK, Timen A, Dirksen K, Gelinck L, Leyten E, Groeneveld P, Jansen C, Jonges M, Raj S et al (2014) Middle East respiratory syndrome coronavirus (MERS-CoV) infections in two returning travellers in the Netherlands, May 2014. Euro Surveill 19(21):1–10. 10.2807/1560-7917.es2014.19.21.20817 [DOI] [PubMed]
- 51.Devi JP, Noraini W, Norhayati R, Kheong CC, Badrul AS, Zainah S, Fadzilah K, Hirman I, Hakim L, Hisham AN. Laboratory-confirmed case of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in Malaysia: preparedness and response. Euro Surv. 2014;19(18):1–10. doi: 10.2807/1560-7917.es2014.19.18.20797. [DOI] [PubMed] [Google Scholar]
- 52.Bialek SR, Allen D, Alvarado-Ramy F, Arthur R, Balajee A, Bell D, Best S, Blackmore C, Breakwell L et al (2014) First confirmed cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Infection in the United States, Updated Information on the Epidemiology of MERS-CoV Infection, and Guidance for the Public, Clinicians, and Public Health Authorities-May 2014. MMWR Morb Mortal Wkly Rep 63(19):431–36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5779407/. Accessed Feb 2020 [PMC free article] [PubMed]
- 53.Pavli A, Tsiodras S, Maltezou HC. Middle East respiratory syndrome coronavirus (MERS-CoV): prevention in travelers. Travel Med Infect Dis. 2014;12(6):602–608. doi: 10.1016/j.tmaid.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Park HY, Lee EJ, Ryu YW, Kim Y, Kim H, Lee H, Yi SJ. Epidemiological investigation of MERS-CoV spread in a single hospital in South Korea, May to June 2015. Euro Surv. 2015;20(25):1–6. doi: 10.2807/1560-7917.es2015.20.25.21169. [DOI] [PubMed] [Google Scholar]
- 55.Su S, Wong G, Liu Y, Gao GF, Li S, Bi Y. MERS in South Korea and China: a potential outbreak threat? Lancet. 2015;385(9985):2349–2350. doi: 10.1016/s0140-6736(15)60859-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.WHO. Middle East respiratory syndrome. MERS situation update, December 2019. http://www.emro.who.int/health-topics/mers-cov/mers-outbreaks.html. Accessed Mar 2020
- 57.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Du Z, Wang L, Cauchemez S, Xu X, Wang X, Cowling BJ, Meyers LA. Risk for transportation of 2019 novel coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis. 2020 doi: 10.3201/eid2605.200146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gralinski LE, Menachery VD (2020) Return of the coronavirus: 2019-nCoV. Viruses. 10.3390/v12020135 [DOI] [PMC free article] [PubMed]
- 60.Li X, Zai J, Wang X, Li Y. Potential of large ‘first generation’ human-to-human transmission of 2019-nCoV. J Med Virol. 2020 doi: 10.1002/jmv.25693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Velavan TP, Meyer CG. The covid-19 epidemic. Trop Med Int Health. 2020 doi: 10.3390/v12020135/10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Coronavirus 2019-nCoV, CSSE. Coronavirus 2019-nCoV global cases by johns hopkins CSSE. https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed Feb 2020
- 63.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.European Centre for Disease Prevention and Control. COVID-19. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases. Accessed Apr 2020
- 65.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chen N, Zhau M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yang W, Cao Q, Qin L, Wang X, Cheng Z, Pan A, Dai J, Sun Q, Zhao F, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): A multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80:388–393. doi: 10.1016/j.jinf.2020.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tian S, Hu N, Lou J, Chen K, Kang X, Xiang Z, Chen H, Wang D, Liu D, et al. Characteristics of COVID-19 infection in Beijing. J Infect. 2020;80:401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee PI, Hsueh PR. Emerging threats from zoonotic coronaviruses-from SARS and MERS to 2019-nCoV. J Microbiol Immunol Infect. 2020 doi: 10.1016/j.jmii.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, Zimmer T, Thiel V, Janke C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020 doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.To KKW, Tsang OTY, Yip CCY, Chan KH, Wu TC, Chan JMC, Leung WS, Chik TSH, Choi CYC (2020) Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 10.1093/cid/ciaa149 [DOI] [PMC free article] [PubMed]
- 73.Wu A, Peng Y, Huang B, Ding X, Wang X, Niu P, Meng J, Zhu Z, Zhang Z, et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27:11. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ji W, Wang W, Zhao X, Zai J, Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus 2019-nCoV may boost cross-species transmission from snake to human. J Med Virol. 2020 doi: 10.1002/fut.22099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ceraolo C, Giorgi FM. Genomic variance of the 2019-nCoV coronavirus. J Med Virol. 2020 doi: 10.1002/jmv.25700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ayittey FK, Dzuvor C, Ayittey MK, Chiwero NB, Habib A (2020) Updates on Wuhan 2019 novel coronavirus epidemic. J Med Virol. 10.1002/jmv.25695 [DOI] [PMC free article] [PubMed]
- 77.Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, Fang C, Huang D, Huang LQ, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7:4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.