Abstract
Olfactory loss is frequent. However, in public not many people complain of that, or they are even not (fully) aware of it. This indicates that it is possible to live a life without a sense of smell, albeit it is more dangerous, less pleasant, and food tastes much less interesting. Most common causes for smell loss are sinunasal disease (chronic rhinosinusitis with and without nasal polyps), acute infections of the upper airways, head trauma, and neurodegenerative disorders. In many people smell loss seems to be due to the aging process. Before treatment olfactory disorders are diagnosed according to cause with the medical history being a big portion of the diagnostic process. Olfactory disorders are in principle reversible, with a relatively high degree of spontaneous improvement in olfactory loss following infections of the upper respiratory tract. Medical treatment is according to cause. It also involves surgical approaches as well as conservative treatments including the use of corticosteroids, antibiotics, or smell training. Because today olfactory dysfunction seems to receive more attention than in previous years it can be expected that tomorrow we will have more specific and effective treatment options available.
Keywords: Olfactory Epithelium, Olfactory Function, Olfactory Dysfunction, Kallmann Syndrome, Olfactory Loss
Epidemiology of Olfactory Loss
Population-based studies of olfactory loss show a prevalence of olfactory impairment of 22 % (25-75 years; [31.1]), 19 % ( years; [31.2]), or 24 % ( years; [31.3]), with the highest prevalence in older men. However, unawareness of olfactory loss is common [31.3, 31.4, 31.5]. It also has to be kept in mind that total loss of the sense of smell is seen much less frequently (3-10 %) [31.6].
With regard to patients presenting themselves to specialized clinical centers, the most common etiologies of smell loss are post viral upper respiratory tract infection (URTI ) (18-45 %) and sinunasal disease (SND ) (7-56 %), followed by head trauma (8-20 %), exposure to toxins/drugs (2-6 %), and congenital anosmia (0-4 %) [31.10, 31.11, 31.12, 31.13, 31.14, 31.15, 31.7, 31.8, 31.9]. A survey in Germany, Austria, and Switzerland shows higher results for SND [31.16].
For qualitative disorders, the prevalence is considerably lower. In the general population, the prevalence of phantosmia is estimated between 0.8 and 2.1 % [31.17] and parosmia to about 4 % [31.18]. Among patients with olfactory disorders, parosmia frequency ranges from 10 to 60 % [31.19, 31.20, 31.7] – possibly indicating that the detection of parosmia is critically dependent on how the investigator asks for parosmia.
Definitions of Olfactory Dysfunction
Quantitative Olfactory Disorders
Normosmia indicates a normal sense of smell; hyposmia indicates a decrease in olfactory function and anosmia indicates the loss of olfactory function. Next to general anosmia, specific anosmias have been described, where only certain odors cannot be perceived whereas most odors are [31.21]. The term functional anosmia was chosen since many subjects with severe olfactory loss appear to be able to still perceive a few single odors. Nevertheless, those rare and weak olfactory impressions are too poor to be of any help to these patients in daily life.
Qualitative Olfactory Disorders
The term qualitative olfactory disorder reflects the qualitatively changed perception of odorous sensation [31.19, 31.20, 31.22, 31.23]. Their diagnosis relies on the patients’ complaints [31.23]. They can be graded in four grades 0–III (frequency of occurrence: daily = 1 point; intensity: very intense = 1 point; social/important other consequences (weight loss, change of daily activities)= 1 point; the degree of parosmia/phantosmia is the sum of points).
Qualitative olfactory disorders are frequently, but not necessarily associated with quantitative olfactory disorders. Parosmia describes the distorted perception of smells in the presence of an odor source; parosmias are triggered by odors. They occur particularly often after infections of the URTI or head trauma [31.24]. The distorted odors are mostly perceived as unpleasant (although some exceptions seem to exist [31.25]). Parosmias are thought to be the result of changes at a peripheral or central-nervous level [31.26, 31.27]; at the moment it is unclear how they are generated. The diagnosis qualitative olfactory disorder can be supported by relatively lower scores in an odor identification test [31.19] or the presence of relatively small olfactory bulbs (OB ) compared to patients without parosmia/phantosmia [31.28].
Clinically important, most parosmic impressions tend to weaken over months and finally disappear after years [31.24]. Currently it is also not entirely clear whether parosmias are a positive sign in terms of the prognosis of post-URTI and post-traumatic olfactory loss [31.29]. Phantosmia describes the distorted perception of smells in the absence of an odor source. Most often phantosmias occur after trauma or URTI [31.24]. Stress-related phantosmias have also been reported [31.30]. Similar to parosmia, the exact explanation of the molecular modifications leading to phantosmia is yet unknown and also the site of its generation remains unclear. Phantosmias also have a tendency to disappear over the course of years.
Otorhinolaryngological Examination
Evaluation of a patient starts with a thorough history [31.31]. This should include demographics, eating, drinking or smoking habits, listing of major illnesses and injuries, medications taken in relation to symptom onset, history of present illness, endocrine information (thyroid gland, diabetes), general nasal health including obstruction, rhinorrhea, and changes of the sense of smell (Fig. 31.1 ). Physical examination should include at least the patient’s head and neck. Sometimes a neurological examination may be needed. Specific nasal examination should include nasal endoscopy. Radiological evaluation is helpful to rule out the presence of tumors or vascular malformations [31.32, 31.33], to judge the volume of the OB [31.34], measure the depth of the olfactory sulcus [31.35, 31.36], and to investigate the paranasal sinuses. Especially the volume of the OB seems to carry also prognostic information – the larger its volume the more likely recovery [31.37].
Fig. 31.1.


History questionnaire
Additional diagnostic tests may include the search for other underlying causes of the olfactory disorders, deficiency of vitamin A or B12, or hypothyroidism. Finally, biopsies of the olfactory epithelium may be helpful in the diagnosis of olfactory disorders [31.27, 31.38, 31.39].
Questionnaires
To detect changes related to olfactory loss, several questionnaires have been developed [31.40]. The sinonasal outcome test-16 specifically addresses nasal dysfunction [31.41] (see also [31.42, 31.43, 31.44, 31.45, 31.46]; it is a 16-item measure that assesses the degree of rhinosinusitis based on the presence of symptoms associated with sinusitis. The relatively elaborate questionnaire of olfactory disorders (QOD ) [31.47, 31.48] was designed to asses daily life problems associated with olfactory loss and has been used in a number of studies [31.49, 31.50]. It consists of 26 items that can be divided into three domains: negative statements indicating patients suffering from olfactory impairment and distorted odorous perceptions (parosmia or phantosmia), positive statements about coping with the disorder, and statements of social desirability, for control. Another questionnaire asks about the importance of olfaction in daily life [31.51]. This questionnaire does not focus on impairments, but asks how often and in which circumstances people use their sense of smell.
In addition, questionnaires are available to measure mood states or quality of life (QoL ) [31.52], with the short form-36 health survey being the standard QoL questionnaire [31.53]. However, there is a choice of questionnaires that allows the selection of the best suited tool [31.54, 31.55]. Depressive symptoms are often assessed with the Beck depression inventory (BDI ) questionnaire [31.56], or its more modern version [31.57]. However, it has to be kept in mind that olfactory loss is often confounded with comorbidity. In fact, in patients with chronic rhinosinusitis the additional effect of olfactory loss on general QoL seems to be not very high [31.58]. In order to be able to track the patients’ ability to cope with the olfactory disorder, Nordin et al. introduced an 11-question instrument [31.59].
Psychophysical Methods of Olfactory Testing
The basic principle of psychophysical testing of olfaction is to expose a patient to an odor and to collect responses to that exposure. These procedures are easy to understand by the patient, but, importantly, they are also easily understood by the investigator. Asking the patient about his/her chemosensory function does not appear to be useful, at least not in all patients [31.60, 31.61, 31.62]; in addition, may patients confuse taste and retronasal olfactory function (flavor).
Numerous tests for olfactory function are available many of which are based on odor identification (for review, see [31.63]). In daily clinical life, these tests serve as quick screening tools for olfactory dysfunction [31.64]. All olfactory tests should be reliable and valid. Tests apart from screening tools should distinguish between anosmic, hyposmic, and normosmic subjects, respectively, which requires availability of normative data acquired and validated on large samples of healthy and diseased subjects, respectively. In addition, it should be known which change of the test score indicates a clinically significant change of function [31.65]. Most of these requirements apply only to a few olfactory tests [31.66, 31.67, 31.68, 31.69, 31.70, 31.71]. The best-validated olfactory tests include the University of Pennsylvania smell identification test (UPSIT ) [31.67], the Connecticut Chemosensory Clinical Research Center test (CCCRC ) [31.72], and the Sniffin’ Sticks [31.68, 31.69] (Fig. 31.2).
Fig. 31.2.

Sniffin’ Sticks and how they are presented to the patient (courtesy of T. Hummel)
Most odor identification tests are presented within a forced choice paradigm. The subjects have to identify odors at supra-threshold concentrations from a list of descriptors [31.73, 31.74]. For example, subjects receive a rose odor, and they are asked whether the odor was banana, fish, rose, or coffee; such tasks are no problem for healthy people, but they are very difficult for people with smell loss. The forced-choice procedure controls the patients’ response bias. The result of the test corresponds to the sum of the correctly identified items. Smell identification tests are most widely used [31.66, 31.67, 31.68, 31.69, 31.70, 31.71, 31.75]. The more odors the test contains the more reliable it is [31.76, 31.77]. Identification tests have to be adjusted to the various cultures [31.78, 31.79], simply because not all odors are known everywhere; for example, many Europeans do not know the smell of wintergreen or root beer, whereas this is well known in the United States.
Two other widely used test designs are threshold tests and tests of odor discrimination. The idea of threshold tests is to expose a subject repeatedly to ascending and descending concentrations of the same odorant and to identify the least detectable concentration for this individual odor [31.80, 31.81, 31.82]. Other designs are based on logistic regression [31.83, 31.84]. Discrimination tasks mainly consist of a three-alternative forced choice technique [31.68, 31.85]. Two of the administered odors are identical, one is different. The subjects’ task is to find out the different one. Tests for odor threshold/odor discrimination can be easily used repetitively, which is more difficult with odor identification tests.
Generally, identification and discrimination tests are believed to reflect central olfactory processing while thresholds are thought to reflect peripheral olfactory function to a stronger degree [31.86, 31.87, 31.88]. For example, in patients with chronic rhinosinusitis a low threshold score and normal identification and discrimination are frequently seen [31.89].
In order to investigate retronasal function, simple and inexpensive flavor identification tests have been investigated for their test–retest reliability and their validity [31.90, 31.91, 31.92]. One test, the taste powders (Schmeckpulver), is also validated on a multinational level [31.93]. Other tests of olfactory function include the investigation of pupillary reflexes [31.94, 31.95], blinking reflexes [31.96], psychogalvanic skin reactions [31.97], or changes in respiratory/sniffing pattern [31.98, 31.99].
Electrophysiological/Imaging Techniques
Electroolfactogram (EOG )
Electroolfactograms (EOG) are electrical potentials of the olfactory epithelium that occur in response to olfactory stimulation. The EOG represents the sum of generator potentials of olfactory receptor neurons (ORN s) [31.100]. Although this technique appears to be attractive [31.101], for example, for the functional characterization of the human olfactory epithelium [31.102], there are only a handful of reports utilizing the human EOG [31.103, 31.104, 31.105, 31.106, 31.107, 31.108]. Notably there are no published investigations in patients.
Chemosensory Event-Related Potentials (CSERP )
Event-related potentials are EEG-derived signals. They are due to the activation of cortical neurons, which generate electromagnetic fields [31.109]. To extract event-related potentials (ERP ) from the background electroencephalogram (EEG ) activity, stimuli are presented repeatedly and the individual recordings are then averaged, which improves the signal-to-noise ratio (random activity would cancel itself out; nonrandom activation would remain). In addition, stimuli are presented with a steep onset () in a monotonous environment such that stimulus onset synchronizes the activity of as many cortical neurons as possible. Olfactory ERP are direct correlates of neuronal activation; they have a high temporal resolution in the range of microseconds, and they can be obtained independently of the subject’s response bias, they are well-suited for medico-legal investigations [31.110].
Based on a system developed by Kobal [31.104, 31.111], odors are applied intranasally (Fig. 31.3). Presentation of odorous stimuli does not produce mechanical or thermal sensations because odor pulses are embedded in a constantly flowing air stream [31.104, 31.112, 31.113]. ERP peaks are either early or late. Earlier peaks like N1 encode exogenous stimulus characteristics to a larger extent (What is the nature of this stimulus?) than later, so-called endogenous components (What is the meaning of this stimulus?) [31.114, 31.115]. Although there is a very clear concept available as to how to record and analyze olfactory ERP [31.116, 31.117] recently there have been a number of attempts to improve the signal-to-noise ratio [31.118, 31.119, 31.120] and to extract additional information from the stimulus-related EEG [31.121, 31.122].
Fig. 31.3.
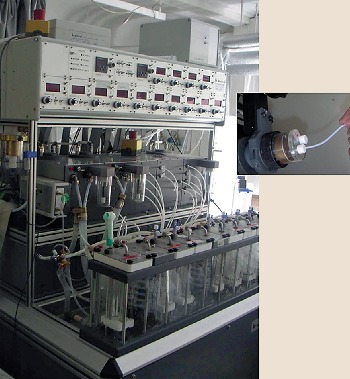
Olfactometer OMb6 (Burghart, Wedel, Germany) and how stimuli are presented intranasally (courtesy of T. Hummel)
Using magneto-encephalographic techniques [31.123] cortical generators of the responses to trigeminal stimulation with CO2 were localized in the secondary somato-sensory cortex [31.124], sources in response to olfactory stimulation were found in the anterior-central parts of the insula, the para-insular cortex, and the superior temporal sulcus [31.125, 31.126, 31.127]. More recent work based on EEG [31.128] suggests that olfactory information in humans is processed first ipsilaterally to the stimulated nostril and then sequentially activates the major relays in olfactory information processing in both hemispheres.
Other EEG-related tests are based on the contingent negative variation (CNV), which occurs in response to an expectation [31.129, 31.130] or more general EEG changes [31.131] (Fig. 31.4).
Fig. 31.4a,b.
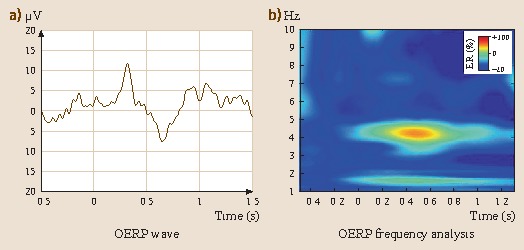
Olfactory event-related activity shown in the time domain (a): negativity upward or the frequency domain (b). Stimulus presentation (phenylethylalcohol: PEA ) started at time 0 for 200 ms
Functional Magnetic Resonance Imaging (fMRI ), Positron Emission Tomography (PET )
Brain imaging allows to study the human olfactory system in detail [31.132, 31.133, 31.134, 31.135, 31.136, 31.137, 31.138, 31.139]. In contrast to electroencephalogram (EEG) and magneto-encephalogram (MEG ), PET and fMRI largely reflect blood-flow related changes. In addition, PET and fMRI have a relatively low temporal resolution whereas they exhibit a better spatial resolution than EEG and MEG. Although there are some data available on fMRI and PET in patients with olfactory loss [31.140, 31.141, 31.142], it seems that the use of these techniques in individual patients with smell or taste disorders is difficult.
Causes and Symptoms of Smell Disorders
Most Common Causes
Olfactory Loss Following Infections of the URTI
The patients’ history typically starts with an episode of a cold during, which they lose their sense of smell [31.143, 31.144, 31.145, 31.146, 31.147, 31.20]. Some authors claim viral (influenza, parainfluenza viruses type III, rhinovirus, coronavirus, and Epstein Barr) rather than bacterial infections to be responsible for olfactory disturbances [31.148, 31.149] and observed a higher incidence of dysosmias after spring and summer URTI [31.144]. Furthermore, women above 45 years of age seem to be affected at a higher percentage than men [31.10, 31.144, 31.7] – which brings up the potential olfactory protective effect of estrogens [31.150]. Nevertheless, the effect of estrogen on olfactory function remains an open debate [31.151, 31.17]. It is important to inform patients with post-URTI olfactory loss about the possibility of parosmia (see above). It tends to occur 1-3 months after the URTI, although it appears sometimes to occur directly after the URTI. The frequency of parosmia is in the range of 25 % [31.152, 31.153].
Posttraumatic Olfactory Disorders
Posttraumatic olfactory disorders are said to occur after occipital trauma. The current explanation is that coup-contre-coup lesions or tearing of the filae olfactoriae leads to anosmia or hyposmia. Although the entity of posttraumatic olfactory loss has already been described at the end of the last century it has received little systematic attention, like most olfactory disorders [31.154]. Olfactory loss seems to correlate with the severity of the trauma [31.155, 31.156, 31.157], although several authors pointed out the fact that there is considerable individual variability in terms of the vulnerability of olfactory structures [31.157, 31.158]. The injured parts of the olfactory system are most often the filae olfactoriae which cross the cribriform plate. However, central structures such as the orbitofrontal cortex and gyrus rectus have also been found to be affected from head trauma [31.147, 31.155]. Similar to post-URTI olfactory impairment, these patients are prone to develop parosmia and phantosmia several months after the trauma. Clinical experience shows that most patients with posttraumatic olfactory disturbance realize the alteration with some latency [31.159].
Sinunasal Disorders
Sinunasal disorders constitute the most frequent causes of olfactory loss [31.16]. This is due to mechanical obstruction of nasal cavity (septal deviation, nasal polyposis, congested mucosa) and/or the inflammatory component of chronic rhinosinusitis [31.160, 31.161, 31.162, 31.163, 31.164, 31.165]. Mild olfactory impairments could also be identified in other groups of patients with SNDs such as allergic and uncomplicated chronic rhinosinusitis [31.147, 31.166, 31.167]. In contrast to posttraumatic and post-URTI olfactory dysfunctions, these patients rarely exhibit parosmia or phantosmia.
Neurodegenerative Causes
Olfactory loss is common in patients with idiopathic Parkinson’s disease (IPD) [31.168, 31.169, 31.170]. While a decreased sniff volume seems to add to the decrease in olfactory function [31.171], electrophysiological recordings in response to passive olfactory stimulation clearly established the presence of olfactory impairment in IPD [31.172, 31.173]. This olfactory deficit is so reliable that it can be used as a marker of IPD [31.170, 31.174]. In other words: If a patient with normal olfactory function presents with IPD symptoms the diagnosis should be re-investigated. Olfactory loss precedes the onset of motor symptoms by 4-6 years [31.175, 31.176, 31.177]. Olfactory loss is also observed regularly in Alzheimer’s disease, and at a much lower frequency/less pronounced in multiple system atrophy, Huntington’s disease, and motor neuron disease [31.178].
Idiopathic Olfactory Loss
Idiopathic olfactory loss seems to reflect the poor understanding of factors interfering with olfaction [31.147]. With further insight and research this percentage should decrease. A considerable number of these idiopathic causes might be due to SND, post-URTI dysosmias following an almost undetected URTI, or neurodegenerative diseases [31.165].
Less Frequent Causes
Diabetes is probably among the best investigated endocrine diseases concerning olfactory disorders [31.179, 31.180, 31.2]. Most studies reveal slight olfactory deficiencies in diabetic patients especially at threshold levels indicating a peripheral patho-mechanism compatible with a possible diabetic micro-angiopathy or peripheral polyneuropathy. However, olfactory impairment in diabetes is relatively mild. Two recent studies conducted with identification tests in large study samples could not find diabetic patients to exhibit a decreased ability to identify odors compared to healthy controls [31.17, 31.2]; there is evidence showing that olfactory loss is most prominent in complicated diabetes II [31.181]. Several other endocrine diseases like hypothyroidism [31.182] or adrenocortical insufficiency (Addison’s disease) [31.183] have been reported to cause olfactory loss.
Affections of the kidney [31.184] and liver [31.17, 31.185, 31.186] have been associated with decreased olfactory function. Olfactory disturbances in those patients are of special importance because they are discussed as a potential cause of malnutrition [31.187]. Olfactory loss may be induced by drugs [31.188]. Among these cardiovascular drugs [31.189], anti-hypertensive drugs [31.190, 31.191], antibiotics [31.192], and chemotherapeutic agents [31.193] are frequently mentioned. However, most information has been accumulated on the basis of case reports [31.194, 31.195]. Typically, the chemosensory side effects disappear when the medication is discontinued.
Isolated congenital anosmia seems to appear at a frequency of approximately 1:8000. Only magnetic resonance (MR) imaging leads to a more definitive diagnosis [31.196, 31.35, 31.36]. In the frontal imaging planes just tangential to the eye bulbs hypoplastic or aplastic olfactory bulbs (OLB) can be visualized (Fig. 31.5). This plane also allows an evaluation of the olfactory sulcus which is flattened in case the OLB is absent or hypoplastic. This is a useful indicator of congenital anosmia, especially because the bulb is not always easy to identify. Congenital/inborn anosmia as part of a syndrome is the Kallmann syndrome [31.197, 31.198] – here decreased olfactory function is associated with hypogonadotropic hypogonadism meaning the missing/slowed development of the gonads because of decreased levels of hormones, so-called gonadotropins [31.199].
Fig. 31.5a,b.
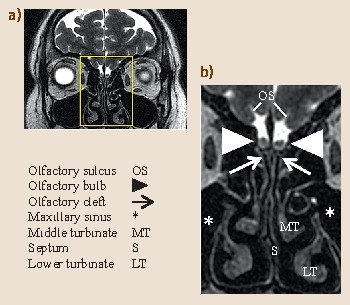
Coronal sections (MR-scans) of the head including olfactory bulbs: (a) section through whole head; (b) magnification of rectangular section indicated in the whole head section
Symptoms/Quality of Life
Patients with olfactory disorders are impaired in areas of food intake, safety, personal hygiene, and in their sexual life [31.200, 31.201]. Most often, difficulties related to eating are reported [31.202], also reduced appetite [31.59, 31.8] and difficulties in preparing food/cooking [31.40]. Many patients have problems detecting spoiled food [31.203]. Interestingly, however, these eating problems do not lead to a general pattern of reduced food intake [31.204]. In a study by Ferris and Duffy, 18 % of the smell patients described an increase in food consumption, 20 % a decrease, and the majority reported no change in food consumption [31.202].
No significant weight difference and no difference in food preferences was found in patients who were born without a sense of smell in comparison to an age-matched control group [31.198]. This is also supported from observations indicating that congenital absence of olfaction does not result in markedly aberrant food preferences [31.205]. As patients with acquired olfactory disorders, congenitally anosmic people report enhanced problems with burning food and detecting spoiled food [31.198].
Another common problem is worry about failure to detect fire, gas, or smoke [31.40]. The failure to detect fire or smoke is a main risk associated with olfactory disorder [31.206, 31.59]. Patients also express problems related to personal hygiene and also social relations are reported to be affected by olfactory disorders [31.59]. Impaired sex life has been reported inconsistently [31.207, 31.208, 31.209, 31.42]. Problems in working life have been reported to various degrees [31.62].
Olfactory dysfunction also affects QoL [31.210]. However, in SND, for example, it is difficult to separate the effects of olfactory disorders from those of decreased nasal patency. A similar situation is present in posttraumatic olfactory loss, where patients not only exhibit olfactory loss, but often more severe trauma-related disorders.
Finally, most patients also suffer from a feeling of not being recognized as being sensory disabled since both healthcare professionals and peers often lack any knowledge about smell disorders. This non recognition of the smell-impaired person is reported to generate a lot of frustration and has been overlooked in the past [31.211, 31.212].
Spontaneous Recovery of Smell Disorders
Age-related anosmia does not seem to exhibit spontaneous recovery. Sinunasal smell disorders have a tendency to become worse over time – typical is a gradual loss of the sense of smell. This leads to a situation that the entire process may not be noticed or that patients only complain of orthonasal loss but not of loss of retronasal olfactory function. Toxic and drug-induced smell disorders may recover once the drug intake is interrupted [31.192, 31.193].
Several authors described recovery rates for post-URTI and posttraumatic disorders to be highest within the first year [31.20, 31.213, 31.214, 31.215]. This is probably due to the ability of olfactory neurons to regenerate [31.216, 31.217]. Post-URTI disorders have a better prognosis compared to posttraumatic disorders, probably (at least in part) owing to the fact that they often cause hyposmia rather than anosmia [31.146]. In approximately 5 % of the cases total recovery can be observed, while up to 60 % of all patients experience partial recovery of some olfactory function over the following years [31.145].
Positive predictors of spontaneous recovery include: short duration of disease, young age, viral cause of olfactory loss better than trauma, presence of parosmia, women better than men, higher olfactory function (also indicated in the presence of olfactory/trigeminal ERP and larger volume of the OLB), and nonsmoking [31.146, 31.218, 31.29, 31.34]. In contrast to quantitative olfactory disorders, qualitative disorders seem to have a better prognosis of spontaneous disappearance. Parosmias tend to decrease to a bearable level after approximately one year [31.152]. However, recent work revealed that more than 50 % of the parosmias still are present after 2 years [31.210]. Over time, parosmia seems to lose its devastating effect on QoL. To summarize, the best current therapeutic attitude toward post-URTI and posttraumatic olfactory disorders is to correctly inform the patient, without taking any hope of recovery nor promising quick and complete recovery. The patients should receive satisfactory olfactory testing. Follow-up investigations give both the physician and the patient the possibility to observe improvements.
Treatment of Olfactory Disorders
Surgical Therapy of SND-Related Olfactory Loss
Most of the patients undergo surgery to remedy decreased nasal patency, a feeling of pressure or recurrent infections of the nasal sinuses. Surgery is rarely performed to specifically treat olfactory dysfunction. However, when asked, postoperative improvement of olfactory function is reported by a majority of the patients [31.219, 31.220, 31.221]. When olfactory function is measured, a different picture emerges with 25 % of patients with preoperative hyposmia and 5 % with preoperative anosmia [31.222] (compare [31.223]). In terms of the sense of smell, nasal surgery produced the highest success rates in patients with eosinophilia and a high degree of polyposis [31.223]; in addition, higher success rates were found in women, and patients with aspirin-intolerance [31.224]. Neither age, presence of asthma, nor the number of preoperative surgical interventions had a major impact on the outcome of surgery [31.223, 31.224]. Findings of endoscopical investigations do not correlate with improvement of the sense of smell [31.225]. While beneficial in many cases, surgery may also pose a certain, albeit low risk to olfactory function [31.223, 31.226].
Conservative Therapy of SND-Related Olfactory Loss
Antibiotics
In the chronic form of putrid sinusitis Staphylococcus aureus and Pseudomonas aeruginosa are of high significance. Whenever possible antibiotic therapy should only be started after the bacteria have been identified and tested for resistances to antibiotics. It is important to note that in chronic putrid sinusitis, antibiotic treatment is not always successful.
Steroids
Among many other effects, corticosteroids act as anti-inflammatory drugs, the effects of which are produced via a number of different pathways including inhibition of phospholipase A2 through induction of lipocortin [31.227]. They reduce submucosal edema and mucosal hypersecretion and thereby increase nasal patency. Systemically administered steroids are of help in many SND patients [31.228, 31.229, 31.230, 31.231, 31.232, 31.9]. In addition to the anti-inflammatory activity it has been postulated that corticosteroids directly improve olfactory function [31.233, 31.234] by modulating the function of ORN through effects on olfactory Na, K-ATPase [31.227]. In fact, systemic steroids are often helpful even in patients without nasal obstruction due to polyps or obvious inflammatory changes [31.165, 31.231, 31.235].
Steroids may be administered systemically or topically. With regard to idiopathic olfactory dysfunction systemic administration is often applied for diagnostic purposes [31.165]. If systemic steroids improve olfactory function treatment is typically continued with locally administered steroids [31.167, 31.228, 31.230, 31.236]; however, the role of topical steroids in the treatment of SND-related olfactory loss has been questioned [31.165, 31.237, 31.238]. One reason why systemic steroids have a higher therapeutic efficacy compared to topical steroids [31.239, 31.9] may relate to the deposition of the spray in the nasal cavity with only few droplets reaching the olfactory cleft [31.238, 31.240]. In fact, it has been shown that only a small amount of nasally applied drugs reaches the olfactory epithelium which is situated in an effectively protected area of the nasal cavity [31.241, 31.242, 31.243]. This situation can be remedied by the use of longer applicators [31.244], which allow to reach further into the nasal cavity so that the spray can reach the olfactory epithelium more effectively.
Other Treatments
Other treatments include the use of antileukotrienes [31.245, 31.246], saline lavages [31.247], dietary changes [31.248], acupuncture [31.249], anti-allergy immunotherapy [31.250], or herbal treatments [31.251].
Conservative Therapy of Post-URTI/Posttraumatic Olfactory Loss
Post-URTI smell dysfunction seems to be due to an impairment of ORN, both in function and in numbers [31.252, 31.253]. While numerous treatments have been tried in post-URTI anosmia no pharmacological therapy has been clearly established so far [31.254, 31.255, 31.256, 31.257].
However, there are numerous candidates for the conservative treatment of olfactory dysfunction. One of them is alpha-lipoic acid (ALA ) which is used in the treatment of diabetic neuropathy [31.258]. The effect of ALA is well described both in experimental animals and in humans (for review see [31.259]). It is known to stimulate the expression of nerve growth factor, substance P, and neuropeptide Y [31.260, 31.261]. It enhances motor nerve conduction velocity as well as microcirculation [31.262]. Further, ALA also has neuroprotective capabilities [31.263]. Preliminary work indicated that it may be useful in post-URTI olfactory loss [31.264]. Other encouraging pilot studies have been performed with the NMDA-antagonist caroverine (NMDA: N-methyl-d-aspartate) [31.265]. Potential mechanisms for the hypothesized effect included both reduced feedback inhibition in the OLB as a consequence of NMDA-antagonistic actions or antagonism of an excitotoxic action of glutamate.
Although frequently mentioned as a therapeutic option, studies on olfactory dysfunction with zinc have produced negative results [31.254, 31.266]. It may, however, be of therapeutic value in patients with severe zinc deficiency, in hemodialysis. In studies in postmenopausal women, estrogens have been reported to provide a certain protection against olfactory disturbances [31.7]. However, as mentioned above, recent studies [31.151] indicate that estrogens are probably ineffective in the treatment of olfactory loss. Finally, although discussed frequently, the potential therapeutic use of orally administered vitamin A [31.255, 31.267] is questionable; at least doses as high as 10000 IU do not seem to be effective [31.268].
A different approach to the treatment of olfactory disorders is the detection and treatment of underlying causes. This approach may also involve the replacement of drugs suspect to affect the sense of smell [31.194, 31.269, 31.270, 31.271]. Among the nonpharmacological treatments acupuncture has been mentioned frequently [31.249, 31.272, 31.273] although its effectivity is a matter of discussion [31.274].
The use of phophodiesterase inhibitors has been described in several studies, none of which was double-blinded, throwing some doubt on the results [31.275, 31.276, 31.277, 31.278, 31.279, 31.280]. In addition, animal studies indicated a decreased amplitude of responses recorded from the olfactory epithelium after topical administration [31.281].
Numerous studies indicate the usefulness of olfactory training , which is typically performed over a period of 12 or more weeks [31.282]. Patients expose themselves twice daily to four intense odors (phenyl ethyl alcohol: rose, eucalyptol: eucalyptus, citronellal: lemon, eugenol: cloves). A number of studies, from different laboratories [31.283, 31.284, 31.285], one of them performed in a blinded way [31.286], indicate that patients training with odors experience a significant improvement in olfactory function over patients who do not perform such a training. One idea about the effectivity of that training relates to the possible stimulation of regenerative capacities of the olfactory epithelium [31.287].
Concluding Remarks and Outlook
Olfactory dysfunction receives more attention than in previous years probably because modern societies not only care about simple survival but much about QoL. It can be expected that soon we will (1) have a better understanding of the processes leading to smell loss and (2) have more specific and effective treatment options available for people with olfactory disorders.
Biographies
Dr Hummel received his medical education in at the Friedrich-Alexander University of Erlangen-Nürnberg, where he also participated in a special program on pharmacology and toxicology. He worked in the Department of Pharmacology at the University of Iowa and was Assistant Professor in the Department of Otorhinolaryngology of the University of Pennsylvania, before joining TU Dresden where he works at an olfactory/gustatory dysfunction clinic.
![]()
Basile Landis went to Medical School in Zurich and Geneva and is an ear, nose, and throat specialist. He is currently Head of the Rhinology-Olfactology Unit, University Hospital of Geneva. In addition to studying in Geneva (Silvain Lacroix), he was trained in Dresden (Thomas Hummel) and Bern (Marco Caversaccio). His activities are patient care, nasal surgery and research, as well as clinical work-ups for chemosensory disorders.
![]()
Philippe Rombaux is Head of the Dept. or Otorhinolaryngolgy at the University of Louvain in Brussels. His principal interest is medical and surgical rhinology with a special focus on the chemosensory perception. He developed with his collaborators a Smell and Taste Center where all the common techniques to measure the chemosensory function in the clinic are performed such as psychophysic, electrophysiology and imagery.
![]()
Contributor Information
Andrea Buettner, Email: andrea.buettner@ivv.fraunhofer.de.
Thomas Hummel, Email: thummel@mail.zih.tu-dresden.de.
Basile N. Landis, Email: basile.landis@hcuge.ch
Philippe Rombaux, Email: philippe.rombaux@uclouvain.be.
References
- [1].Vennemann M.M., Hummel T., Berger K. The association between smoking and smell and taste impairment in the general population. J. Neurol. 2008;255:1121–1126. doi: 10.1007/s00415-008-0807-9. [DOI] [PubMed] [Google Scholar]
- [2].Brämerson A., Johansson L., Ek L., Nordin S., Bende M. Prevalence of olfactory dysfunction: The Skövde population-based study. Laryngoscope. 2004;114:733–737. doi: 10.1097/00005537-200404000-00026. [DOI] [PubMed] [Google Scholar]
- [3].Murphy C., Schubert C.R., Cruickshanks K.J., Klein B.E., Klein R., Nondahl D.M. Prevalence of olfactory impairment in older adults. Jama. 2002;288:2307–2312. doi: 10.1001/jama.288.18.2307. [DOI] [PubMed] [Google Scholar]
- [4].Shu C.H., Hummel T., Lee P.L., Chiu C.H., Lin S.H., Yuan B.C. The proportion of self-rated olfactory dysfunction does not change across the life span. Am. J. Rhinol. Allergy. 2009;23:413–416. doi: 10.2500/ajra.2009.23.3343. [DOI] [PubMed] [Google Scholar]
- [5].Nordin S., Monsch A.U., Murphy C. Unawareness of smell loss in normal aging and Alzheimer’s disease: Discrepancy between self-reported and diagnosed smell sensitivity. J. Gerontol. 1995;50:187–192. doi: 10.1093/geronb/50B.4.P187. [DOI] [PubMed] [Google Scholar]
- [6].Landis B.N., Hummel T. New evidence for high occurrence of olfactory dysfunctions within the population. Am. J. Med. 2006;119:91–92. doi: 10.1016/j.amjmed.2005.07.039. [DOI] [PubMed] [Google Scholar]
- [7].Deems D.A., Doty R.L., Settle R.G., Moore-Gillon V., Shaman P., Mester A.F., Kimmelman C.P., Brightman V.J., Snow J.B.J. Smell and taste disorders: A study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch. Otorhinolaryngol. Head Neck Surg. 1991;117:519–528. doi: 10.1001/archotol.1991.01870170065015. [DOI] [PubMed] [Google Scholar]
- [8].Temmel A.F., Quint C., Schickinger-Fischer B., Klimek L., Stoller E., Hummel T. Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch. Otolaryngol. Head Neck Surg. 2002;128:635–641. doi: 10.1001/archotol.128.6.635. [DOI] [PubMed] [Google Scholar]
- [9].Seiden A.M., Duncan H.J. The diagnosis of a conductive olfactory loss. Laryngoscope. 2001;111:9–14. doi: 10.1097/00005537-200101000-00002. [DOI] [PubMed] [Google Scholar]
- [10].Quint C., Temmel A.F., Schickinger B., Pabinger S., Ramberger P., Hummel T. Patterns of non-conductive olfactory disorders in eastern Austria: A study of 120 patients from the Department of Otorhinolaryngology at the University of Vienna. Wien. Klin. Wochenschr. 2001;113:52–57. [PubMed] [Google Scholar]
- [11].Mullol J., Alobid I., Marino-Sanchez F., Quinto L., de Haro J., Bernal-Sprekelsen M., Valero A., Picado C., Marin C. Furthering the understanding of olfaction, prevalence of loss of smell and risk factors: A population-based survey (OLFACAT study) BMJ Open. 2012;2(6):e001256. doi: 10.1136/bmjopen-2012-001256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Henkin R.I., Levy L.M., Fordyce A. Taste and smell function in chronic disease: A review of clinical and biochemical evaluations of taste and smell dysfunction in over 5000 patients at The Taste and Smell Clinic in Washington DC. Am. J. Otolaryngol. 2013;34:477–489. doi: 10.1016/j.amjoto.2013.04.006. [DOI] [PubMed] [Google Scholar]
- [13].Lee W.H., Wee J.H., Kim D.K., Rhee C., Lee C.H., Ahn S., Lee J.H., Cho Y.S., Lee K.H., Kim K.S., Kim S.W., Lee A., Kim J.W. Prevalence of subjective olfactory dysfunction and its risk factors: Korean national health and nutrition examination survey. PLoS One. 2013;8:e62725. doi: 10.1371/journal.pone.0062725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Schubert C.R., Cruickshanks K.J., Fischer M.E., Huang G.H., Klein B.E., Klein R., Pankow J.S., Nondahl D.M. Olfactory impairment in an adult population: The Beaver Dam Offspring Study. Chem. Senses. 2012;37:325–334. doi: 10.1093/chemse/bjr102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Fonteyn S., Huart C., Deggouj N., Collet S., Eloy P., Rombaux P. Non-sinonasal-related olfactory dysfunction: A cohort of 496 patients. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2014;131:87–91. doi: 10.1016/j.anorl.2013.03.006. [DOI] [PubMed] [Google Scholar]
- [16].Damm M., Temmel A., Welge-Lüssen A., Eckel H.E., Kreft M.P., Klussmann J.P., Gudziol H., Hüttenbrink K.B., Hummel T. Epidemiologie und Therapie von Riechstörungen in Deutschland, Österreich und der Schweiz. HNO. 2004;52:112–120. doi: 10.1007/s00106-003-0877-z. [DOI] [PubMed] [Google Scholar]
- [17].Landis B.N., Konnerth C.G., Hummel T. A study on the frequency of olfactory dysfunction. Laryngoscope. 2004;114:1764–1769. doi: 10.1097/00005537-200410000-00017. [DOI] [PubMed] [Google Scholar]
- [18].Nordin S., Brämerson A., Millqvist E., Bende M. Prevalence of parosmia: The Skövde population-based studies. Rhinology. 2007;45:50–53. [PubMed] [Google Scholar]
- [19].Nordin S., Murphy C., Davidson T.M., Quinonez C., Jalowayski A.A., Ellison D.W. Prevalence and assessment of qualitative olfactory dysfunction in different age groups. Laryngoscope. 1996;106:739–744. doi: 10.1097/00005537-199606000-00014. [DOI] [PubMed] [Google Scholar]
- [20].Faulcon P., Portier F., Biacabe B., Bonfils P. Anosmie secondaire à une rhinite aiguë: sémiologie et évolution à propos d’une série de 118 patients. Ann. Otolaryngol. Chir. Cervicofac. 1999;116:351–357. [PubMed] [Google Scholar]
- [21].Amoore J.E. Specific anosmias. In: Getchell T.V., Doty R.L., Bartoshuk L.M., Snow J.B.J., editors. Smell and Taste in Health and Disease. New York: Raven; 1991. pp. 655–664. [Google Scholar]
- [22].Frasnelli J., Landis B.N., Heilmann S., Hauswald B., Huttenbrink K.B., Lacroix J.S., Leopold D.A., Hummel T. Clinical presentation of qualitative olfactory dysfunction. Eur. Arch. Otorhinolaryngol. 2003;11:11–13. doi: 10.1007/s00405-003-0703-y. [DOI] [PubMed] [Google Scholar]
- [23].Leopold D. Distortion of olfactory perception: Diagnosis and treatment. Chem. Senses. 2002;27:611–615. doi: 10.1093/chemse/27.7.611. [DOI] [PubMed] [Google Scholar]
- [24].Reden J., Maroldt H., Fritz A., Zahnert T., Hummel T. A study on the prognostic significance of qualitative olfactory dysfunction. Eur. Arch. Otorhinolaryngol. 2007;264:139–144. doi: 10.1007/s00405-006-0157-0. [DOI] [PubMed] [Google Scholar]
- [25].Landis B.N., Frasnelli J., Hummel T. Euosmia: A rare form of parosmia. Acta Otolaryngol. 2006;126:101–103. doi: 10.1080/00016480510043954. [DOI] [PubMed] [Google Scholar]
- [26].Rombaux P., Mouraux A., Bertrand B., Nicolas G., Duprez T., Hummel T. Olfactory function and olfactory bulb volume in patients with postinfectious olfactory loss. Laryngoscope. 2006;116:436–439. doi: 10.1097/01.MLG.0000195291.36641.1E. [DOI] [PubMed] [Google Scholar]
- [27].Holbrook E., Leopold D., Schwob J. Abnormalities of axon growth in human olfactory mucosa. Laryngoscope. 2005;115:2144–2154. doi: 10.1097/01.MLG.0000181493.83661.CE. [DOI] [PubMed] [Google Scholar]
- [28].Mueller A., Rodewald A., Reden J., Gerber J., von Kummer R., Hummel T. Reduced olfactory bulb volume in post-traumatic and post-infectious olfactory dysfunction. Neuroreport. 2005;16:475–478. doi: 10.1097/00001756-200504040-00011. [DOI] [PubMed] [Google Scholar]
- [29].Hummel T., Lötsch J. Prognostic factors of olfactory dysfunction. Arch. Otolaryngol. Head Neck Surg. 2010;136:347–351. doi: 10.1001/archoto.2010.27. [DOI] [PubMed] [Google Scholar]
- [30].Kaufman M.D., Lassiter K.R., Shenoy B.V. Paroxysmal unilateral dysosmia: A cured patient. Ann. Neurol. 1988;24:450–451. doi: 10.1002/ana.410240315. [DOI] [PubMed] [Google Scholar]
- [31].Welge-Luessen A., Leopold D.A., Miwa T. Smell and taste disorders – Diagnostic and clinical work-up. In: Welge-Luessen A., Hummel T., editors. Management of Smell and Taste Disorders: A Practical Guide for Clinicians. Thieme: Stuttgart; 2013. pp. 49–57. [Google Scholar]
- [32].Hoekman P.K., Houlton J.J., Seiden A.M. The utility of magnetic resonance imaging in the diagnostic evaluation of idiopathic olfactory loss. Laryngoscope. 2014;124:365–368. doi: 10.1002/lary.24248. [DOI] [PubMed] [Google Scholar]
- [33].Mueller C., Temmel A.F., Toth J., Quint C., Herneth A., Hummel T. Computed tomography scans in the evaluation of patients with olfactory dysfunction. Am. J. Rhinol. 2006;20:109–112. [PubMed] [Google Scholar]
- [34].Rombaux P., Huart C., Deggouj N., Duprez T., Hummel T. Prognostic value of olfactory bulb volume measurement for recovery in postinfectious and posttraumatic olfactory loss. Otolaryngol. Head Neck Surg. 2012;147:1136–1141. doi: 10.1177/0194599812459704. [DOI] [PubMed] [Google Scholar]
- [35].Abolmaali N.D., Hietschold V., Vogl T.J., Huttenbrink K.B., Hummel T. MR evaluation in patients with isolated anosmia since birth or early childhood. AJNR Am. J. Neuroradiol. 2002;23:157–164. [PMC free article] [PubMed] [Google Scholar]
- [36].Huart C., Meusel T., Gerber J., Duprez T., Rombaux P., Hummel T. The depth of the olfactory sulcus is an indicator of congenital anosmia. AJNR Am. J. Neuroradiol. 2011;32:1911–1914. doi: 10.3174/ajnr.A2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Huart C., Rombaux P., Hummel T. Plasticity of the human olfactory system: The olfactory bulb. Mol. 2013;18:11586–11600. doi: 10.3390/molecules180911586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Yee K.K., Pribitkin E.A., Cowart B.J., Vainius A.A., Klock C.T., Rosen D., Feng P., McLean J., Hahn C.G., Rawson N.E. Neuropathology of the olfactory mucosa in chronic rhinosinusitis. Am. J. Rhinol. Allergy. 2010;24:110–120. doi: 10.2500/ajra.2010.24.3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Witt M., Bormann K., Gudziol V., Pehlke K., Barth K., Minovi A., Hahner A., Reichmann H., Hummel T. Biopsies of olfactory epithelium in patients with Parkinson’s disease. Mov Disord. 2009;24:906–914. doi: 10.1002/mds.22464. [DOI] [PubMed] [Google Scholar]
- [40].Miwa T., Furukawa M., Tsukatani T., Costanzo R.M., DiNardo L.J., Reiter E.R. Impact of olfactory impairment on quality of life and disability. Arch. Otolaryngol. Head Neck Surg. 2001;127:497–503. doi: 10.1001/archotol.127.5.497. [DOI] [PubMed] [Google Scholar]
- [41].Anderson E.R., Murphy M.P., Weymuller E.A.J. Clinimetric evaluation of the sinonasal outcome test-16. Otolaryngol. Head Neck Surg. 1999;121:702–707. doi: 10.1053/hn.1999.v121.a100114. [DOI] [PubMed] [Google Scholar]
- [42].Hufnagl B., Lehrner J., Deecke L. Development of a questionnaire for the assessment of self reported olfactory functioning. Chem. Senses. 2003;28:E27. [Google Scholar]
- [43].de Jong N., Mulder I., de Graaf C., van Staveren W.A. Impaired sensory functioning in elders: The relation with its potential determinants and nutritional intake. J. Gerontol. A. Biol. Sci. Med. Sci. 1999;54:B324–331. doi: 10.1093/gerona/54.8.B324. [DOI] [PubMed] [Google Scholar]
- [44].Takebayashi H., Tsuzuki K., Oka H., Fukazawa K., Daimon T., Sakagami M. Clinical availability of a self-administered odor questionnaire for patients with olfactory disorders. Auris Nasus Larynx. 2011;38:65–72. doi: 10.1016/j.anl.2010.05.013. [DOI] [PubMed] [Google Scholar]
- [45].Varga E.K., Breslin P.A., Cowart B.J. The impact of chemosensory dysfunction on quality of life. Chem. Senses. 2000;25:654. [Google Scholar]
- [46].Pusswald G., Moser D., Gleiss A., Janzek-Hawlat S., Auff E., Dal-Bianco P., Lehrner J. Prevalence of mild cognitive impairment subtypes in patients attending a memory outpatient clinic-comparison of two modes of mild cognitive impairment classification: Results of the Vienna Conversion to Dementia Study. Alzheimers Dement. 2013;9:366–376. doi: 10.1016/j.jalz.2011.12.009. [DOI] [PubMed] [Google Scholar]
- [47].Frasnelli J., Hummel T. Olfactory dysfunction and daily life. Eur. Arch. Otorhinolaryngol. 2005;262:231–235. doi: 10.1007/s00405-004-0796-y. [DOI] [PubMed] [Google Scholar]
- [48].Neuland C., Bitter T., Marschner H., Gudziol H., Guntinas-Lichius O. Health-related and specific olfaction-related quality of life in patients with chronic functional anosmia or severe hyposmia. Laryngoscope. 2011;121:867–872. doi: 10.1002/lary.21387. [DOI] [PubMed] [Google Scholar]
- [49].Shu C.H., Lee P.O., Lan M.Y., Lee Y.L. Factors affecting the impact of olfactory loss on the quality of life and emotional coping ability. Rhinology. 2011;49:337–341. doi: 10.4193/Rhino10.130. [DOI] [PubMed] [Google Scholar]
- [50].Katotomichelakis M., Simopoulos E., Zhang N., Tripsianis G., Danielides G., Livaditis M., Bachert C., Danielides V. Olfactory dysfunction and asthma as risk factors for poor quality of life in upper airway diseases. Am. J. Rhinol. Allergy. 2013;27:293–298. doi: 10.2500/ajra.2013.27.3903. [DOI] [PubMed] [Google Scholar]
- [51].Croy I., Buschhuter D., Seo H.S., Negoias S., Hummel T. Individual significance of olfaction: Development of a questionnaire. Eur. Arch. Otorhinolaryngol. 2010;267:67–71. doi: 10.1007/s00405-009-1054-0. [DOI] [PubMed] [Google Scholar]
- [52].Bullinger M. Assessing health related quality of life in medicine: An overview over concepts, methods and applications in international research. Restor. Neurol. Neurosci. 2002;20:93–101. [PubMed] [Google Scholar]
- [53].Ware J.E., Jr. SF-36 health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- [54].Derogatis L.R. SCL-90: Administration, Scoring and Procedures Manual for the Revised Version. Baltimore: Clinical Psychometric Research; 1987. [Google Scholar]
- [55].Zerssen D.V. Die Befindlichkeitsskala. Test, Gottingen: Beltz; 1975. [Google Scholar]
- [56].Beck A.T., Ward C.M., Mendelson M., Mock J.E., Erbaugh J.K. An inventory for measuring depression. Arch. Gen. Psychiat. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- [57].Beck A.T., Steer R.A., Brown G.K. Beck Depression Inventory. 2. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- [58].Litvack J.R., Mace J.C., Smith T.L. Olfactory function and disease severity in chronic rhinosinusitis. Am. J. Rhinol. Allergy. 2009;23:139–144. doi: 10.2500/ajra.2009.23.3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Nordin S., Blomqvist E.H., Olsson P., Stjarne P., Ehnhage A. Effects of smell loss on daily life and adopted coping strategies in patients with nasal polyposis with asthma. Acta. Otolaryngol. 2011;131:826–832. doi: 10.3109/00016489.2010.539625. [DOI] [PubMed] [Google Scholar]
- [60].Landis B.N., Hummel T., Hugentobler M., Giger R., Lacroix J.S. Ratings of overall olfactory function. Chem. Senses. 2003;28:691–694. doi: 10.1093/chemse/bjg061. [DOI] [PubMed] [Google Scholar]
- [61].Soter A., Kim J., Jackman A., Tourbier I., Kaul A., Doty R.L. Accuracy of self-report in detecting taste dysfunction. Laryngoscope. 2008;118:611–617. doi: 10.1097/MLG.0b013e318161e53a. [DOI] [PubMed] [Google Scholar]
- [62].Haxel B.R., Bertz-Duffy S., Fruth K., Letzel S., Mann W.J., Muttray A. Comparison of subjective olfaction ratings in patients with and without olfactory disorders. J. Laryngol. Otol. 2012;126:692–697. doi: 10.1017/S002221511200076X. [DOI] [PubMed] [Google Scholar]
- [63].Doty R.L. Office procedures for quantitative assessment of olfactory function. Am. J. Rhinol. 2007;21:460–473. doi: 10.2500/ajr.2007.21.3043. [DOI] [PubMed] [Google Scholar]
- [64].Hummel T., Konnerth C.G., Rosenheim K., Kobal G. Screening of olfactory function with a four-minute odor identification test: Reliability, normative data, and investigations in patients with olfactory loss. Ann. Otol. Rhinol. Laryngol. 2001;110:976–981. doi: 10.1177/000348940111001015. [DOI] [PubMed] [Google Scholar]
- [65].Gudziol V., Lotsch J., Hahner A., Zahnert T., Hummel T. Clinical significance of results from olfactory testing. Laryngoscope. 2006;116:1858–1863. doi: 10.1097/01.mlg.0000234915.51189.cb. [DOI] [PubMed] [Google Scholar]
- [66].Cain W.S. Testing olfaction in a clinical setting. Ear Nose Throat J. 1989;68:321–328. [PubMed] [Google Scholar]
- [67].Doty R.L., Shaman P., Kimmelman C.P., Dann M.S. University of Pennsylvania Smell Identification Test: A rapid quantitative olfactory function test for the clinic. Laryngoscope. 1984;94:176–178. doi: 10.1288/00005537-198402000-00004. [DOI] [PubMed] [Google Scholar]
- [68].Hummel T., Sekinger B., Wolf S.R., Pauli E., Kobal G. Sniffin sticks: Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem. Senses. 1997;22:39–52. doi: 10.1093/chemse/22.1.39. [DOI] [PubMed] [Google Scholar]
- [69].Kobal G.K.L., Wolfensberger M., Gudziol H., Temmer A., Owen C.M., Seeber H., Pauli E., Hummel T. Multicenter investigation of 1036 subjects using a standardized method for the assessment of olfactory function combining tests of odor identification, odor discrimination, and olfactory thresholds. Eur. Arch. Otorhinolaryngol. 2000;257:205–211. doi: 10.1007/s004050050223. [DOI] [PubMed] [Google Scholar]
- [70].Kondo H., Matsuda T., Hashiba M., Baba S. A study of the relationship between the T and T olfactometer and the University of Pennsylvania smell identification test in a Japanese population. Am. J. Rhinol. 1998;12:353–358. doi: 10.2500/105065898780182390. [DOI] [PubMed] [Google Scholar]
- [71].Cardesin A., Alobid I., Benitez P., Sierra E., de Haro J., Bernal-Sprekelsen M., Picado C., Mullol J. Barcelona Smell Test-24 (BAST-24): Validation and smell characteristics in the healthy Spanish population. Rhinology. 2006;44:83–89. [PubMed] [Google Scholar]
- [72].Cain W.S., Gent J.F., Goodspeed R.B., Leonard G. Evaluation of olfactory dysfunction in the Connecticut Chemosensory Clinical Research Center (CCCRC) Laryngoscope. 1988;98:83–88. doi: 10.1288/00005537-198801000-00017. [DOI] [PubMed] [Google Scholar]
- [73].Gudziol V., Hummel T. The influence of distractors on odor identification. Arch. Otolaryngol. Head Neck Surg. 2009;135:143–145. doi: 10.1001/archotol.135.2.143. [DOI] [PubMed] [Google Scholar]
- [74].Negoias S., Troeger C., Rombaux P., Halewyck S., Hummel T. Number of descriptors in cued odor identification tests. Arch. Otolaryngol Head Neck Surg. 2010;136:296–300. doi: 10.1001/archoto.2009.231. [DOI] [PubMed] [Google Scholar]
- [75].Briner H.R., Simmen D. Smell diskettes as screening test of olfaction. Rhinology. 1999;37:145–148. [PubMed] [Google Scholar]
- [76].Doty R.L., McKeown D.A., Lee W.W., Shaman P. A study of the test-retest reliability of ten olfactory tests. Chem. Senses. 1995;20:645–656. doi: 10.1093/chemse/20.6.645. [DOI] [PubMed] [Google Scholar]
- [77].Haehner A., Mayer A.M., Landis B.N., Pournaras I., Lill K., Gudziol V., Hummel T. High test-retest reliability of the extended version of the Sniffin’ Sticks test. Chem. Senses. 2009;34:705–711. doi: 10.1093/chemse/bjp057. [DOI] [PubMed] [Google Scholar]
- [78].Doty R.L., Marcus A., Lee W.W. Development of the 12-item Cross-Cultural Smell Identification Test (CC-SIT) Laryngoscope. 1996;106:353–356. doi: 10.1097/00005537-199603000-00021. [DOI] [PubMed] [Google Scholar]
- [79].Konstantinidis I., Printza A., Genetzaki S., Mamali K., Kekes G., Constantinidis J. Cultural adaptation of an olfactory identification test: The Greek version of Sniffin’ Sticks. Rhinology. 2008;46:292–296. [PubMed] [Google Scholar]
- [80].Doty R.L., Laing D.G. Psychophysical measurement of human olfactory function, including odorant mixture assessment. In: Doty R.L., editor. Handbook of Olfaction and Gustation. 2. New York: Marcel Dekker; 2003. pp. 203–228. [Google Scholar]
- [81].Ehrenstein W.H., Ehrenstein A. Psychophysical methods. In: Windhorst U., Johansson H., editors. Modern Techniques in Neuroscience Research. Berlin: Springer; 1999. pp. 1211–1241. [Google Scholar]
- [82].Croy I., Lange K., Krone F., Negoias S., Seo H.S., Hummel T. Comparison between odor thresholds for phenyl ethyl alcohol and butanol. Chem. Senses. 2009;34:523–527. doi: 10.1093/chemse/bjp029. [DOI] [PubMed] [Google Scholar]
- [83].Lotsch J., Lange C., Hummel T. A simple and reliable method for clinical assessment of odor thresholds. Chem. Senses. 2004;29:311–317. doi: 10.1093/chemse/bjh034. [DOI] [PubMed] [Google Scholar]
- [84].Linschoten M.R., Harvey L.O., Jr., Eller P.M., Jafek B.W. Fast and accurate measurement of taste and smell thresholds using a maximum-likelihood adaptive staircase procedure. Percept. Psychophys. 2001;63:1330–1347. doi: 10.3758/BF03194546. [DOI] [PubMed] [Google Scholar]
- [85].Weierstall R., Pause B.M. Development of a 15-item odour discrimination test (Dusseldorf Odour Discrimination Test) Perception. 2012;41:193–203. doi: 10.1068/p7113. [DOI] [PubMed] [Google Scholar]
- [86].Doty R.L., Smith R., McKeown D.A., Raj J. Tests of human olfactory function: Principle component analysis suggests that most measure a common source of variance. Percept. Psychophys. 1994;56:701–707. doi: 10.3758/BF03208363. [DOI] [PubMed] [Google Scholar]
- [87].Hedner M., Larsson M., Arnold N., Zucco G.M., Hummel T. Cognitive factors in odor detection, odor discrimination, and odor identification tasks. J. Clin. Exp. Neuropsychol. 2010;30:1–6. doi: 10.1080/13803391003683070. [DOI] [PubMed] [Google Scholar]
- [88].Lotsch J., Reichmann H., Hummel T. Different odor tests contribute differently to the evaluation of olfactory loss. Chem. Senses. 2008;33:17–21. doi: 10.1093/chemse/bjm058. [DOI] [PubMed] [Google Scholar]
- [89].Moll B., Klimek L., Eggers G., Mann W. Comparison of olfactory function in patients with seasonal and perennial allergic rhinitis. Allergy. 1998;53:297–301. doi: 10.1111/j.1398-9995.1998.tb03890.x. [DOI] [PubMed] [Google Scholar]
- [90].Leon E.A., Catalanotto F.A., Werning J.W. Retronasal and orthonasal olfactory ability after laryngectomy. Arch. Otolaryngol. Head Neck Surg. 2007;133:32–36. doi: 10.1001/archotol.133.1.32. [DOI] [PubMed] [Google Scholar]
- [91].Heilmann S., Strehle G., Rosenheim K., Damm M., Hummel T. Clinical assessment of retronasal olfactory function. Arch. Otorhinolaryngol. Head Neck Surg. 2002;128:414–418. doi: 10.1001/archotol.128.4.414. [DOI] [PubMed] [Google Scholar]
- [92].Renner B., Mueller C.A., Dreier J., Faulhaber S., Rascher W., Kobal G. The candy smell test: A new test for retronasal olfactory performance. Laryngoscope. 2009;119:487–495. doi: 10.1002/lary.20123. [DOI] [PubMed] [Google Scholar]
- [93].Rawson N.E. Cell and molecular biology of olfaction. Quintessence Int. Berl. Ger. 1999;30:335–341. [PubMed] [Google Scholar]
- [94].Sneppe R., Gonay P. Evaluation objective, quantitative et qualitative de l’olfaction. Electrodiagn. Ther. 1973;10:5–17. [PubMed] [Google Scholar]
- [95].Schneider C.B., Ziemssen T., Schuster B., Seo H.S., Haehner A., Hummel T. Pupillary responses to intranasal trigeminal and olfactory stimulation. J. Neural Transm. 2009;116:885–889. doi: 10.1007/s00702-009-0244-7. [DOI] [PubMed] [Google Scholar]
- [96].Ichihara M., Komatsu A., Ichihara F., Asaga H., HirayoshiK K. Test of smell based on the wink response. Jibiinkoka. 1967;39:947–953. [PubMed] [Google Scholar]
- [97].Asaka H. The studies on the objective olfactory test by galvanic skin response. J. Otorhinolaryngeal Soc. 1965;68:100–112. doi: 10.3950/jibiinkoka.68.100. [DOI] [PubMed] [Google Scholar]
- [98].Gudziol H., Wächter R. Gibt es olfaktorisch evozierte Atemänderungen? Laryngo-Rhino-Otol. 2004;83:367–373. doi: 10.1055/s-2004-814369. [DOI] [PubMed] [Google Scholar]
- [99].Frank R.A., Dulay M.F., Niergarth K.A., Gesteland R.C. A comparison of the sniff magnitude test and the University of Pennsylvania smell identification test in children and nonnative English speakers. Physiol. Behav. 2004;81:475–480. doi: 10.1016/j.physbeh.2004.02.020. [DOI] [PubMed] [Google Scholar]
- [100].Ottoson D. Analysis of the electrical activity of the olfactory epithelium. Acta Physiol. Scand. 1956;35:1–83. [PubMed] [Google Scholar]
- [101].Lapid H., Hummel T. Recording odor-evoked response potentials at the human olfactory epithelium. Chem. Senses. 2013;38:3–17. doi: 10.1093/chemse/bjs073. [DOI] [PubMed] [Google Scholar]
- [102].Leopold D.A., Hummel T., Schwob J.E., Hong S.C., Knecht M., Kobal G. Anterior distribution of human olfactory epithelium. Laryngoscope. 2000;110:417–421. doi: 10.1097/00005537-200003000-00016. [DOI] [PubMed] [Google Scholar]
- [103].Lapid H., Shushan S., Plotkin A., Voet H., Roth Y., Hummel T., Schneidman E., Sobel N. Neural activity at the human olfactory epithelium reflects olfactory perception. Nat. Neurosci. 2011;14:1455–1461. doi: 10.1038/nn.2926. [DOI] [PubMed] [Google Scholar]
- [104].Kobal G. Elektrophysiologische Untersuchungen Des Menschlichen Geruchssinns. Stuttgart: Thieme; 1981. [Google Scholar]
- [105].Hummel T., Knecht M., Wolf S., Kobal G. Recording of electro-olfactograms in man. Chem. Senses. 1996;21:481. doi: 10.1093/chemse/21.1.75. [DOI] [Google Scholar]
- [106].Hummel T., Mojet J., Kobal G. Electro-olfactograms are present when odorous stimuli have not been perceived. Neurosci. Lett. 2006;397:224–228. doi: 10.1016/j.neulet.2005.12.048. [DOI] [PubMed] [Google Scholar]
- [107].Lapid H., Seo H.S., Schuster B., Schneidman E., Roth Y., Harel D., Sobel N., Hummel T. Odorant concentration dependence in electroolfactograms recorded from the human olfactory epithelium. J. Neurophysiol. 2009;102:2121–2130. doi: 10.1152/jn.91321.2008. [DOI] [PubMed] [Google Scholar]
- [108].Spehr M., Schwane K., Heilmann S., Gisselmann G., Hummel T., Hatt H. Dual capacity of a human olfactory receptor. Curr. Biol. 2004;14:R832–833. doi: 10.1016/j.cub.2004.09.034. [DOI] [PubMed] [Google Scholar]
- [109].Picton T.W., Hillyard S.A. Endogenous event-related potentials. In: Picton T.W., editor. EEG-Handbook. Amsterdam: Elsevier; 1988. [Google Scholar]
- [110].Hummel T., Kobal G. Olfactory event-related potentials. In: Simon S.A., Nicolelis M.A.L., editors. Methods and Frontiers in Chemosensory Research. Boca Raton: CRC; 2001. pp. 429–464. [Google Scholar]
- [111].Kobal G., Plattig K.H. Methodische anmerkungen zur gewinnung olfaktorischer EEG-antworten des wachen menschen (objektive Olfaktometrie) Z EEG-EMG. 1978;9:135–145. [PubMed] [Google Scholar]
- [112].Murphy C., Wetter S., Morgan C.D., Ellison D.W., Geisler M.W. Age effects on central nervous system activity reflected in the olfactory event-related potential, Evidence for decline in middle age. Ann. N. Y. Acad. Sci. 1998;855:598–607. doi: 10.1111/j.1749-6632.1998.tb10630.x. [DOI] [PubMed] [Google Scholar]
- [113].Lorig T.S., Matia D.C., Pezka J.J., Bryant D.N. The effects of active and passive stimulation on chemosensory event-related potentials. Int. J. Psychophysiol. 1996;23:199–205. doi: 10.1016/S0167-8760(96)00061-X. [DOI] [PubMed] [Google Scholar]
- [114].Pause B.M., Sojka B., Krauel K., Ferstl R. The nature of the late positive complex within the olfactory event-related potential. Psychophysiology. 1996;33:168–172. doi: 10.1111/j.1469-8986.1996.tb01062.x. [DOI] [PubMed] [Google Scholar]
- [115].Krauel K., Pause B.M., Sojka B., Schott P., Ferstl R. Attentional modulation of central odor processing. Chem. Senses. 1998;23:423–432. doi: 10.1093/chemse/23.4.423. [DOI] [PubMed] [Google Scholar]
- [116].Welge-Lussen A. Chemosensory evoked potentials: Applications and significance in routine clinical practice. HNO. 1999;47:453–455. doi: 10.1007/s001060050403. [DOI] [PubMed] [Google Scholar]
- [117].Hummel T., Klimek L., Welge-Lussen A., Wolfensberger G., Gudziol H., Renner B., Kobal G. Chemosensorisch evozierte Potentiale zur klinischen Diagnostik von Riechstörungen. HNO. 2000;48:481–485. doi: 10.1007/s001060050602. [DOI] [PubMed] [Google Scholar]
- [118].Lotsch J., Hummel T. The clinical significance of electrophysiological measures of olfactory function. Behav. Brain Res. 2006;170:78–83. doi: 10.1016/j.bbr.2006.02.013. [DOI] [PubMed] [Google Scholar]
- [119].Schaub F., Damm M. A time-saving method for recording chemosensory event-related potentials. Eur. Arch. Otorhinolaryngol. 2012;269:2209–2217. doi: 10.1007/s00405-011-1921-3. [DOI] [PubMed] [Google Scholar]
- [120].Rombaux P., Bertrand B., Keller T., Mouraux A. Clinical significance of olfactory event-related potentials related to orthonasal and retronasal olfactory testing. Laryngoscope. 2007;117:1096–1101. doi: 10.1097/MLG.0b013e31804d1d0d. [DOI] [PubMed] [Google Scholar]
- [121].Huart C., Legrain V., Hummel T., Rombaux P., Mouraux A. Time-frequency analysis of chemosensory event-related potentials to characterize the cortical representation of odors in humans. PLoS One. 2012;7:e33221. doi: 10.1371/journal.pone.0033221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Boesveldt S., Haehner A., Berendse H.W., Hummel T. Signal-to-noise ratio of chemosensory event-related potentials. Clin. Neurophysiol. 2007;118:690–695. doi: 10.1016/j.clinph.2006.11.004. [DOI] [PubMed] [Google Scholar]
- [123].Williamson S.J., Kaufman L. Analysis of neuromagnetic signals. In: Gevins A.S., Rèmond A.A., editors. Handbook of Electroencephalography and Clinical Neurophysiologgy. Amsterdam: Elsevier; 1987. pp. 405–448. [Google Scholar]
-
[124].Huttunen J., Kobal G., Kaukoronta E., Hari R. Cortical responses to painful CO
 -stimulation of nasal mucosa: A magnetencephalographic study in man. Electroenceph. Clin. Neurophysiol. 1986;64:347–349. doi: 10.1016/0013-4694(86)90159-8. [DOI] [PubMed] [Google Scholar]
-stimulation of nasal mucosa: A magnetencephalographic study in man. Electroenceph. Clin. Neurophysiol. 1986;64:347–349. doi: 10.1016/0013-4694(86)90159-8. [DOI] [PubMed] [Google Scholar] - [125].Ayabe-Kanamura S., Endo H., Kobayakawa T., Takeda T., Saito S. Measurement of olfactory evoked magnetic fields by a 64-channel whole-head SQUID system. Chem. Senses. 1997;22:214–215. [Google Scholar]
- [126].Kettenmann B., Hummel C., Stefan H., Kobal G. Magnetoencephalographical recordings: Separation of cortical responses to different chemical stimulation in man. Funct. Neurosci. (EEG Suppl.) 1996;46:287–290. [PubMed] [Google Scholar]
- [127].Kettenmann B., Hummel T., Stefan H., Kobal G. Multiple olfactory activity in the human neocortex identified by magnetic source imaging. Chem. Senses. 1996;22:493–502. doi: 10.1093/chemse/22.5.493. [DOI] [PubMed] [Google Scholar]
- [128].Lascano A.M., Hummel T., Lacroix J.S., Landis B.N., Michel C.M. Spatio-temporal dynamics of olfactory processing in the human brain: An event-related source imaging study. Neurosci. 2010;167:700–708. doi: 10.1016/j.neuroscience.2010.02.013. [DOI] [PubMed] [Google Scholar]
- [129].Lorig T.S., Roberts M. Odor and cognitive alteration of the contingent negative variation. Chem. Senses. 1990;15:537–545. doi: 10.1093/chemse/15.5.537. [DOI] [Google Scholar]
- [130].Mrowinski D., Scholz G. Objective olfactometry by recording simultaneously olfactory evoked potentials and contingent negative variation. Chem. Senses. 1996;21:487. [Google Scholar]
- [131].Perbellini D., Scolari R. L’elettroencefalo-olfattometria. Ann. Lar. Ot. Rin. Far. 1966;65:421–429. [PubMed] [Google Scholar]
- [132].Savic I. Imaging of brain activation by odorants in humans. Curr. Opin. Neurobiol. 2002;12:455–461. doi: 10.1016/S0959-4388(02)00346-X. [DOI] [PubMed] [Google Scholar]
- [133].Zald D.H., Pardo J.V. Functional neuroimaging of the olfactory system in humans. Int. J. Psychophysiol. 2000;36:165–181. doi: 10.1016/S0167-8760(99)00110-5. [DOI] [PubMed] [Google Scholar]
- [134].Sobel N., Prabhakaran V., Desmond J.E., Glover G.H., Sullivan E.V., Gabrieli J.D. A method for functional magnetic resonance imaging of olfaction. J. Neurosci. Methods. 1997;78:115–123. doi: 10.1016/S0165-0270(97)00140-4. [DOI] [PubMed] [Google Scholar]
- [135].Hummel T., Yousem D.M., Alsop D.C., Geckle R.J., Doty R.L. Functional MRI of olfactory and intranasal chemosensory trigeminal nerve activation. Soc. Neursci. Abstr. 1997;23:2076. [Google Scholar]
- [136].Small D.M., Jones-Gotman M., Zatorre R.J., Petrides M., Evans A.C. Flavor processing: More than the sum of its parts. Neuroreport. 1997;8:3913–3917. doi: 10.1097/00001756-199712220-00014. [DOI] [PubMed] [Google Scholar]
- [137].Kareken D.A., Sabri M., Radnovich A.J., Claus E., Foresman B., Hector D., Hutchins G.D. Olfactory system activation from sniffing: Effects in piriform and orbitofrontal cortex. Neuroimage. 2004;22:456–465. doi: 10.1016/j.neuroimage.2004.01.008. [DOI] [PubMed] [Google Scholar]
- [138].Savic I., Berglund H. Passive perception of odors and semantic circuits. Hum. Brain Mapp. 2004;21:271–278. doi: 10.1002/hbm.20009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [139].Anderson A.K., Christoff K., Stappen I., Panitz D., Ghahremani D.G., Glover G., Gabrieli J.D., Sobel N. Dissociated neural representations of intensity and valence in human olfaction. Nat. Neurosci. 2003;6:196–202. doi: 10.1038/nn1001. [DOI] [PubMed] [Google Scholar]
- [140].Henkin R.I., Levy L.M., Lin C.S. Taste and smell phantoms revealed by brain functional MRI (fMRI) J. Comput. Assist. Tomogr. 2000;24:106–123. doi: 10.1097/00004728-200001000-00022. [DOI] [PubMed] [Google Scholar]
- [141].Iannilli E., Gerber J., Frasnelli J., Hummel T. Intranasal trigeminal function in subjects with and without an intact sense of smell. Brain Res. 2007;1139:235–244. doi: 10.1016/j.brainres.2006.12.082. [DOI] [PubMed] [Google Scholar]
- [142].Iannilli E., Bitter T., Gudziol H., Burmeister H.P., Mentzel H.J., Chopra A.P., Hummel T. Differences in anosmic and normosmic group in bimodal odorant perception: A functional-MRI study. Rhinology. 2011;49:458–463. doi: 10.4193/Rhino11.110. [DOI] [PubMed] [Google Scholar]
- [143].Jafek B.W., Hartman D., Eller P.M., Johnson E.W., Strahan R.C., Moran D.T. Postviral olfactory dysfunction. Am. J. Rhinol. 1990;4:91–100. doi: 10.2500/105065890782009497. [DOI] [Google Scholar]
- [144].Sugiura M., Aiba T., Mori J., Nakai Y. An epidemiological study of postviral olfactory disorder. Acta Otolaryngol. Suppl. (Stockh.) 1998;538:191–196. doi: 10.1080/00016489850182918. [DOI] [PubMed] [Google Scholar]
- [145].Duncan H.J., Seiden A.M. Long-term follow-up of olfactory loss secondary to head trauma and upper respiratory tract infection. Arch. Otolaryngol. Head Neck Surg. 1995;121:1183–1187. doi: 10.1001/archotol.1995.01890100087015. [DOI] [PubMed] [Google Scholar]
- [146].Reden J., Mueller A., Mueller C., Konstantinidis I., Frasnelli J., Landis B.N., Hummel T. Recovery of olfactory function following closed head injury or infections of the upper respiratory tract. Arch. Otolaryngol. Head Neck Surg. 2006;132:265–269. doi: 10.1001/archotol.132.3.265. [DOI] [PubMed] [Google Scholar]
- [147].Fark T., Hummel T. Olfactory disorders: Distribution according to age and gender in 3,400 patients. Eur. Arch. Otorhinolaryngol. 2013;270:777–779. doi: 10.1007/s00405-012-2108-2. [DOI] [PubMed] [Google Scholar]
- [148].Konstantinidis I., Haehner A., Frasnelli J., Reden J., Quante G., Damm M., Hummel T. Post-infectious olfactory dysfunction exhibits a seasonal pattern. Rhinology. 2006;44:135–139. [PubMed] [Google Scholar]
- [149].Suzuki M., Saito K., Min W.P., Vladau C., Toida K., Itoh H., Murakami S. Identification of viruses in patients with postviral olfactory dysfunction. Laryngoscope. 2007;117:272–277. doi: 10.1097/01.mlg.0000249922.37381.1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Dhong H.J., Chung S.K., Doty R.L. Estrogen protects against 3-methylindole-induced olfactory loss. Brain Res. 1999;824:312–315. doi: 10.1016/S0006-8993(99)01241-X. [DOI] [PubMed] [Google Scholar]
- [151].Hughes L.F., McAsey M.E., Donathan C.L., Smith T., Coney P., Struble R.G. Effects of hormone replacement therapy on olfactory sensitivity: Cross-sectional and longitudinal studies. Climacteric. 2002;5:140–150. doi: 10.1080/cmt.5.2.140.150. [DOI] [PubMed] [Google Scholar]
- [152].Portier F., Faulcon P., Lamblin B., Bonfils P. Sémiologie, étiologie et évolution des parosmies: À propos de 84 cas. Ann. Otolaryngol. Chir. Cervicofac. 2000;117:12–18. [PubMed] [Google Scholar]
- [153].Frasnelli J., Landis B.N., Heilmann S., Hauswald B., Huttenbrink K.B., Lacroix J.S., Leopold D.A., Hummel T. Clinical presentation of qualitative olfactory dysfunction. Eur. Arch. Otorhinolaryngol. 2004;261:411–415. doi: 10.1007/s00405-003-0703-y. [DOI] [PubMed] [Google Scholar]
- [154].Legg J.W. A case of anosmia following a blow. Lancet. 1873;2:659–660. doi: 10.1016/S0140-6736(02)66313-5. [DOI] [Google Scholar]
- [155].Yousem D.M., Geckle R.J., Bilker W.B., Kroger H., Doty R.L. Posttraumatic smell loss: Relationship of psychophysical tests and volumes of the olfactory bulbs and tracts and the temporal lobes. Acad. Radiol. 1999;6:264–272. doi: 10.1016/S1076-6332(99)80449-8. [DOI] [PubMed] [Google Scholar]
- [156].Zusho H. Posttraumatic anosmia. Arch. Otolaryngol. 1982;108:90–92. doi: 10.1001/archotol.1982.00790500026006. [DOI] [PubMed] [Google Scholar]
- [157].Sumner D. Post-traumatic anosmia. Brain. 1964;87:107–120. doi: 10.1093/brain/87.1.107. [DOI] [PubMed] [Google Scholar]
- [158].Delank K.W., Fechner G. Zur Pathophysiologie der posttraumatischen Riechstörungen. Laryngol. Rhinol. Otol. 1996;75:154–159. doi: 10.1055/s-2007-997554. [DOI] [PubMed] [Google Scholar]
- [159].Gudziol V., Hoenck I., Landis B., Podlesek D., Bayn M., Hummel T. The impact and prospect of traumatic brain injury on olfactory function: A cross-sectional and prospective study. Eur. Arch. Otorhinolaryngol. 2014;271:1533–1540. doi: 10.1007/s00405-013-2687-6. [DOI] [PubMed] [Google Scholar]
- [160].Seiden A.M. Olfactory loss secondary to nasal and sinus pathology. In: Seiden A.M., editor. Taste and Smell Disorders. New York: Thieme; 1997. pp. 52–71. [Google Scholar]
- [161].Fein B.T., Kamin P.B., Fein N.N. The loss of sense of smell in nasal allergy. Ann. Allergy. 1966;24:278–283. [PubMed] [Google Scholar]
- [162].Klimek L., Hummel T., Moll B., Kobal G., Mann W.J. Lateralized and bilateral olfactory function in patients with chronic sinusitis compared with healthy control subjects. Laryngoscope. 1998;108:111–114. doi: 10.1097/00005537-199801000-00021. [DOI] [PubMed] [Google Scholar]
- [163].Doty R.L., Mishra A. Olfaction and its alteration by nasal obstruction, rhinitis, and rhinosinusitis. Laryngoscope. 2001;111:409–423. doi: 10.1097/00005537-200103000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [164].Hotchkiss W.T. Influence of prednisone on nasal polyposis with anosmia. Arch. Otolaryngol. 1956;64(6):478–479. doi: 10.1001/archotol.1956.03830180028006. [DOI] [PubMed] [Google Scholar]
- [165].Heilmann S., Huettenbrink K.B., Hummel T. Local and systemic administration of corticosteroids in the treatment of olfactory loss. Am. J. Rhinol. 2004;18:29–33. [PubMed] [Google Scholar]
- [166].Apter A.J., Mott A.E., Frank M.E., Clive J.M. Allergic rhinitis and olfactory loss. Ann. Allergy Asthma Immunol. 1995;75:311–316. [PubMed] [Google Scholar]
- [167].Stuck B.A., Blum A., Hagner A.E., Hummel T., Klimek L., Hormann K. Mometasone furoate nasal spray improves olfactory performance in seasonal allergic rhinitis. Allergy. 2003;58:1195. doi: 10.1034/j.1398-9995.2003.00162.x. [DOI] [PubMed] [Google Scholar]
- [168].Ansari K.A., Johnson A. Olfactory function in patients with Parkinson’s disease. J. Chron. Dis. 1975;28:493–497. doi: 10.1016/0021-9681(75)90058-2. [DOI] [PubMed] [Google Scholar]
- [169].Doty R.L., Deems D., Steller S. Olfactory dysfunction in Parkinson’s disease: A general deficit unrelated to neurologic signs, disease stage, or disease duration. Neurology. 1988;38:1237–1244. doi: 10.1212/WNL.38.8.1237. [DOI] [PubMed] [Google Scholar]
- [170].Haehner A., Boesveldt S., Berendse H.W., Mackay-Sim A., Fleischmann J., Silburn P.A., Johnston A.N., Mellick G.D., Herting B., Reichmann H., Hummel T. Prevalence of smell loss in Parkinson’s disease a multicenter study. Parkinsonism Relat. Disord. 2009;15:490–494. doi: 10.1016/j.parkreldis.2008.12.005. [DOI] [PubMed] [Google Scholar]
- [171].Sobel N., Thomason M.E., Stappen I., Tanner C.M., Tetrud J.W., Bower J.M., Sullivan E.V., Gabrieli J.D. An impairment in sniffing contributes to the olfactory impairment in Parkinson’s disease. Proc. Natl. Acad. Sci. 2001;98:4154–4159. doi: 10.1073/pnas.071061598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [172].Barz S., Hummel T., Pauli E., Majer M., Lang C.J., Kobal G. Chemosensory event-related potentials in response to trigeminal and olfactory stimulation in idiopathic Parkinson’s disease. Neurology. 1997;49:1424–1431. doi: 10.1212/WNL.49.5.1424. [DOI] [PubMed] [Google Scholar]
- [173].Hawkes C.H., Shephard B.C. Olfactory evoked responses and identification tests in neurological disease. Ann. Acad. Sci. 1998;855:608–615. doi: 10.1111/j.1749-6632.1998.tb10631.x. [DOI] [PubMed] [Google Scholar]
- [174].Mesholam R.I., Moberg P.J., Mahr R.N., Doty R.L. Olfaction in neurodegenerative disease: A meta-analysis of olfactory functioning in Alzheimer’s and Parkinson’s diseases. Arch. Neurol. 1998;55:84–90. doi: 10.1001/archneur.55.1.84. [DOI] [PubMed] [Google Scholar]
- [175].Ponsen M.M., Stoffers D., Booij J., van Eck-Smit B.L., Wolters E.C., Berendse H.W. Idiopathic hyposmia as a preclinical sign of Parkinson’s disease. Ann. Neurol. 2004;56:173–181. doi: 10.1002/ana.20160. [DOI] [PubMed] [Google Scholar]
- [176].Sommer U., Hummel T., Cormann K., Mueller A., Frasnelli J., Kropp J., Reichmann H. Detection of presymptomatic Parkinson’s disease: Combination of olfactory tests, transcranial sonography, and 123 I-FP-CIT-SPECT. Movement Disorders. 2004;19:1196–1202. doi: 10.1002/mds.20141. [DOI] [PubMed] [Google Scholar]
- [177].Ross G.W., Petrovitch H., Abbott R.D., Tanner C.M., Popper J., Masaki K., Launer L., White L.R. Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann. Neurol. 2008;63:167–173. doi: 10.1002/ana.21291. [DOI] [PubMed] [Google Scholar]
- [178].Hawkes C. Olfaction in neurodegenerative disorder. Adv. Otorhinolaryngol. 2006;63:133–151. doi: 10.1159/000093759. [DOI] [PubMed] [Google Scholar]
- [179].Jorgensen M.B., Buch N.H. Studies on the sense of smell and taste in diabetics. Arch. Otolaryngol. 1961;53:539–545. doi: 10.3109/00016486109126521. [DOI] [PubMed] [Google Scholar]
- [180].Weinstock R.S., Wright H.N., Smith D.U. Olfactory dysfunction in diabetes mellitus. Physiol. Behav. 1993;53:17–21. doi: 10.1016/0031-9384(93)90005-Z. [DOI] [PubMed] [Google Scholar]
- [181].Naka A., Riedl M., Luger A., Hummel T., Mueller C.A. Clinical significance of smell and taste disorders in patients with diabetes mellitus. Eur. Arch. Otorhinolaryngol. 2010;267:547–550. doi: 10.1007/s00405-009-1123-4. [DOI] [PubMed] [Google Scholar]
- [182].Doty R.L. Gender and endocrine-related influences on human olfactory perception. In: Meiselman R., editor. Clinical Measurement of Taste and Smell. New York: MacMillan; 1986. pp. 377–413. [Google Scholar]
- [183].Henkin R.I., Bartter F.C. Studies on olfactory thresholds in normal man and in patients with adrenal cortical insufficiency: The role of adrenal cortical steroids and of serum sodium concentration. J. Clin. Invest. 1966;45:1631–1639. doi: 10.1172/JCI105470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [184].Frasnelli J.A., Temmel A.F., Quint C., Oberbauer R., Hummel T. Olfactory function in chronic renal failure. Am. J. Rhinol. 2002;16:275–279. [PubMed] [Google Scholar]
- [185].Henkin R.I., Smith F.R. Hyposmia in acute viral hepatitis. Lancet. 1971;1(7704):823–826. doi: 10.1016/S0140-6736(71)91495-4. [DOI] [PubMed] [Google Scholar]
- [186].Kleinschmidt E.G., Kramp B., Schwager A. Functional study on the sense of smell in patients with chronic liver disease. Z. Gesamte. Inn. Med. 1976;31:853–856. [PubMed] [Google Scholar]
- [187].Reaich D. Odour perception in chronic renal disease. Lancet. 1997;350:1191. doi: 10.1016/S0140-6736(05)63448-4. [DOI] [PubMed] [Google Scholar]
- [188].Lotsch J., Geisslinger G., Hummel T. Sniffing out pharmacology: Interactions of drugs with human olfaction. Trends Pharmacol. Sci. 2012;33:193–199. doi: 10.1016/j.tips.2012.01.004. [DOI] [PubMed] [Google Scholar]
- [189].Doty R.L., Philip S., Reddy K., Kerr K.L. Influences of antihypertensive and antihyperlipidemic drugs on the senses of taste and smell: A review. J. Hypertens. 2003;21:1805–1813. doi: 10.1097/00004872-200310000-00003. [DOI] [PubMed] [Google Scholar]
- [190].Kharoubi S. Anosmie toxi-médicamenteuse à la nifédipine. Presse Med. 2003;32:1269–1272. [PubMed] [Google Scholar]
- [191].Levenson J.L., Kennedy K. Dysosmia, dysgeusia, and nifedipine. Ann. Intern. Med. 1985;102:135–136. doi: 10.7326/0003-4819-102-1-135_2. [DOI] [PubMed] [Google Scholar]
- [192].Welge-Luessen A., Wolfensberger M. Reversible anosmia after amikacin therapy. Arch. Otolaryngol. Head Neck Surg. 2003;129:1331–1333. doi: 10.1001/archotol.129.12.1331. [DOI] [PubMed] [Google Scholar]
- [193].Steinbach S., Hummel T., Bohner C., Berktold S., Hundt W., Kriner M., Heinrich P., Sommer H., Hanusch C., Prechtl A., Schmidt B., Bauerfeind I., Seck K., Jacobs V.R., Schmalfeldt B., Harbeck N. Qualitative and quantitative assessment of taste and smell changes in patients undergoing chemotherapy for breast cancer or gynecologic malignancies. J. Clin. Oncol. 2009;27:1899–1905. doi: 10.1200/JCO.2008.19.2690. [DOI] [PubMed] [Google Scholar]
- [194].Ackerman B.H., Kasbekar N. Disturbances of taste and smell induced by drugs. Pharmacotherapy. 1997;17:482–496. [PubMed] [Google Scholar]
- [195].Hastings L., Miller M.L. Olfactory loss to toxic exposure. In: Seiden A.M., editor. Taste and Smell Disorders. New York: Thieme; 1997. pp. 88–106. [Google Scholar]
- [196].Yousem D.M., Geckle R.J., Bilker W., McKeown D.A., Doty R.L. MR evaluation of patients with congenital hyposmia or anosmia. Am. J. Radiol. 1996;166:439–443. doi: 10.2214/ajr.166.2.8553963. [DOI] [PubMed] [Google Scholar]
- [197].Kallmann F.J., Schoenfeld W.A., Barrera S.E. The genetic aspects of primary eunuchoidism. Am. J. Ment. Defic. 1944;48:203–236. [Google Scholar]
- [198].Croy I., Negoias S., Novakova L., Landis B.N., Hummel T. Learning about the functions of the olfactory system from people without a sense of smell. PLoS One. 2012;7:e33365. doi: 10.1371/journal.pone.0033365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [199].Karstensen H.G., Tommerup N. Isolated and syndromic forms of congenital anosmia. Clin. Genet. 2012;81:210–215. doi: 10.1111/j.1399-0004.2011.01776.x. [DOI] [PubMed] [Google Scholar]
- [200].Tennen H., Affleck G., Mendola R. Coping with smell and taste disorder. In: Getchell T.V., Doty R.L., Bartoshuk L.M., Snow J.B., editors. Smell and Taste in Health and Disease. New York: Raven; 1991. pp. 787–802. [Google Scholar]
- [201].Van Toller S. Assessing the impact of anosmia: Review of a questionnaire’s findings. Chem. Senses. 1999;24:705–712. doi: 10.1093/chemse/24.6.705. [DOI] [PubMed] [Google Scholar]
- [202].Ferris A.M., Duffy V.B. Effect of olfactory deficits on nutritional status. Ann. N. Y. Acad. Sci. 1989;561:113–123. doi: 10.1111/j.1749-6632.1989.tb20975.x. [DOI] [PubMed] [Google Scholar]
- [203].Santos D.V., Reiter E.R., DiNardo L.J., Costanzo R.M. Hazardous events associated with impaired olfactory function. Arch. Otolaryngol. Head Neck Surg. 2004;130:317–319. doi: 10.1001/archotol.130.3.317. [DOI] [PubMed] [Google Scholar]
- [204].Aschenbrenner K., Hummel C., Teszmer K., Krone F., Ishimaru T., Seo H.S., Hummel T. The influence of olfactory loss on dietary behaviors. Laryngoscope. 2008;118:135–144. doi: 10.1097/MLG.0b013e318155a4b9. [DOI] [PubMed] [Google Scholar]
- [205].Doty R.L. Food preference ratings of congenitally-anosmic humans. In: Kare M.R., Maller O., editors. Chemical Senses and Nutrition II. New York: Academic; 1977. pp. 315–325. [Google Scholar]
- [206].Blomqvist E.H., Bramerson A., Stjarne P., Nordin S. Consequences of olfactory loss and adopted coping strategies. Rhinology. 2004;42:189–194. [PubMed] [Google Scholar]
- [207].Brämerson A., Nordin S., Bende M. Clinical experience with patients with olfactory complaints and their quality of life. Acta Otolaryngol. 2007;127:167–174. doi: 10.1080/00016480600801357. [DOI] [PubMed] [Google Scholar]
- [208].Gudziol V., Wolff-Stephan S., Aschenbrenner K., Joraschky P., Hummel T. Depression resulting from olfactory dysfunction is associated with reduced sexual appetite – A cross-sectional cohort study. J. Sex Med. 2009;6:1924–1929. doi: 10.1111/j.1743-6109.2009.01266.x. [DOI] [PubMed] [Google Scholar]
- [209].Croy I., Bojanowski V., Hummel T. Men without a sense of smell exhibit a strongly reduced number of sexual relationships, women exhibit reduced partnership security – A reanalysis of previously published data. Biol. Psychol. 2013;92:292–294. doi: 10.1016/j.biopsycho.2012.11.008. [DOI] [PubMed] [Google Scholar]
- [210].Croy I., Nordin S., Hummel T. Olfactory disorders and quality of life – An updated review. Chem. Senses. 2014;39:185–194. doi: 10.1093/chemse/bjt072. [DOI] [PubMed] [Google Scholar]
- [211].Landis B.N., Stow N.W., Lacroix J.S., Hugentobler M., Hummel T. Olfactory disorders: The patients’ view. Rhinology. 2009;47:454–459. doi: 10.4193/Rhin08.174. [DOI] [PubMed] [Google Scholar]
- [212].Keller A., Malaspina D. Hidden consequences of olfactory dysfunction: A patient report series. BMC Ear Nose Throat Disord. 2013;13:8. doi: 10.1186/1472-6815-13-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [213].Bonfils P., Corre F.L., Biacabe B. Semiologie et etiologie des anosmies: A propos de 306 patients. Ann. Otolaryngol. Chir. Cervicofac. 1999;116:198–206. [PubMed] [Google Scholar]
- [214].Costanzo R.M., Zasler N.D. Head trauma. In: Getchell T.V., Doty R.L., Bartoshuk L.M., Snow J.B.J., editors. Smell and Taste in Health and Disease. New York: Raven; 1991. pp. 711–730. [Google Scholar]
- [215].Murphy C., Doty R.L., Duncan H.J. Clinical disorders of olfaction. In: Doty R.L., editor. Handbook of Olfaction and Gustation. New York: Marcel Dekker; 2003. pp. 461–478. [Google Scholar]
- [216].Beidler L.M., Smallman R.L. Renewal of cells within taste buds. J. Cell Bio. 1965;27:263–272. doi: 10.1083/jcb.27.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [217].Gradziadei P.P.C., Monti-Graziadei G.A. Continuous nerve cell renewal in the olfactory system. In: Jacobson M., editor. Handbook of Sensory Physiology. New York: Springer; 1978. p. 55. [Google Scholar]
- [218].Rombaux P., Huart C., Collet S., Eloy P., Negoias S., Hummel T. Presence of olfactory event-related potentials predicts recovery in patients with olfactory loss following upper respiratory tract infection. Laryngoscope. 2010;120:2115–2118. doi: 10.1002/lary.21109. [DOI] [PubMed] [Google Scholar]
- [219].Min Y.G., Yun Y.S., Song B.H., Cho Y.S., Lee K.S. Recovery of nasal physiology after functional endoscopic sinus surgery: Olfaction and mucociliary transport. ORL J. Otorhinolaryngol. Relat. Spec. 1995;57:264–268. doi: 10.1159/000276755. [DOI] [PubMed] [Google Scholar]
- [220].Lund V.J., Scadding G.K. Objective assessmant of endoscopic sinus surgery in the management of chronic rhinosinusitis: An update. J. Laryngol. Otol. 1994;108:749–753. doi: 10.1017/S0022215100128014. [DOI] [PubMed] [Google Scholar]
- [221].Ophir D., Gross-Isseroff R., Lancet D., Marshak G. Changes in olfactory acuity induced by total inferior turbinectomy. Arch. Otolaryngol. Head Neck Surg. 1986;112:195–197. doi: 10.1001/archotol.1986.03780020075017. [DOI] [PubMed] [Google Scholar]
- [222].Delank K.W., Stoll W. Olfactory function after functional endoscopic sinus surgery for chronic sinusitis. Rhinology. 1998;36:15–19. [PubMed] [Google Scholar]
- [223].Pade J., Hummel T. Olfactory function following nasal surgery. Laryngoscope. 2008;118:1260–1264. doi: 10.1097/MLG.0b013e318170b5cb. [DOI] [PubMed] [Google Scholar]
- [224].Minovi A., Hummel T., Ural A., Draf W., Bockmuhl U. Predictors of the outcome of nasal surgery in terms of olfactory function. Eur. Arch. Otorhinolaryngol. 2008;265:57–61. doi: 10.1007/s00405-007-0409-7. [DOI] [PubMed] [Google Scholar]
- [225].Hosemann W., Görtzen W., Wohlleben R., Wolf S.R., Wigand M.E. Olfaction after endoscopic endonasal ethmoidectomy. Am. J. Rhinol. 1993;7:11–15. doi: 10.2500/105065893781976564. [DOI] [Google Scholar]
- [226].Kimmelman C.P. The risk to olfaction from nasal surgery. Laryngoscope. 1994;104:981–988. doi: 10.1288/00005537-199408000-00012. [DOI] [PubMed] [Google Scholar]
- [227].Fong K.J., Kern R.C., Foster J.D., Zhao J.C., Pitovski D.Z. Olfactory secretion and sodium, potassium-adenosine triphosphatase: Regulation by corticosteroids. Laryngoscope. 1999;109:383–388. doi: 10.1097/00005537-199903000-00008. [DOI] [PubMed] [Google Scholar]
- [228].Golding-Wood D.G., Holmstrom M., Darby Y., Scadding G.K., Lund V.J. The treatment of hyposmia with intranasal steroids. J. Laryngol. Otol. 1996;110:132–135. doi: 10.1017/S0022215100132967. [DOI] [PubMed] [Google Scholar]
- [229].Tos M., Svendstrup F., Arndal H., Orntoft S., Jakobsen J., Borum P., Schrewelius C., Larsen P.L., Clement F., Barfoed C., Rømeling F., Tvermosegaard T. Efficacy of an aqueous and a powder formulation of nasal budesonide compared in patients with nasal polyps. Am. J. Rhinol. 1998;12:183–189. doi: 10.2500/105065898781390217. [DOI] [PubMed] [Google Scholar]
- [230].Mott A.E., Cain W.S., Lafreniere D., Leonard G., Gent J.F., Frank M.E. Topical corticosteroid treatment of anosmia associated with nasal and sinus disease. Arch. Otolaryngol. Head Neck Surg. 1997;123:367–372. doi: 10.1001/archotol.1997.01900040009001. [DOI] [PubMed] [Google Scholar]
- [231].Jafek B.W., Moran D.T., Eller P.M., Rowley J.C., III, Jafek T.B. Steroid-dependent anosmia. Arch. Otolaryngol. Head Neck Surg. 1987;113:547–549. doi: 10.1001/archotol.1987.01860050093023. [DOI] [PubMed] [Google Scholar]
- [232].Schriever V.A., Merkonidis C., Gupta N., Hummel C., Hummel T. Treatment of smell loss with systemic methylprednisolone. Rhinology. 2012;50:284–289. doi: 10.4193/Rhino.11.207. [DOI] [PubMed] [Google Scholar]
- [233].Mott A.E., Leopold D.A. Disorders in taste and smell. Med. Clin. North Am. 1991;75:1321–1353. doi: 10.1016/S0025-7125(16)30391-1. [DOI] [PubMed] [Google Scholar]
- [234].Klimek L., Eggers G. Olfactory dysfunction in allergic rhinitis is related to nasal eosinophilc inflammation. J. Allergy Clin. Immunol. 1997;100:159–164. doi: 10.1016/S0091-6749(97)70218-5. [DOI] [PubMed] [Google Scholar]
- [235].Stevens M.H. Steroid-dependent anosmia. Laryngoscope. 2001;111:200–203. doi: 10.1097/00005537-200102000-00002. [DOI] [PubMed] [Google Scholar]
- [236].Meltzer E.O., Jalowayski A.A., Orgel A., Harris A.G. Subjecive and objective assessments in patients with seasonal allergic rhinitis: Effects of therapy with mometasone furoate nasal spray. J. Allergy Clin. Immunol. 1998;102:39–49. doi: 10.1016/S0091-6749(98)70053-3. [DOI] [PubMed] [Google Scholar]
- [237].Blomqvist E.H., Lundblad L., Bergstedt H., Stjarne P. Placebo-controlled, randomized, double-blind study evaluating the efficacy of fluticasone propionate nasal spray for the treatment of patients with hyposmia/anosmia. Acta Otolaryngol. 2003;123:862–868. doi: 10.1080/00016480310002140. [DOI] [PubMed] [Google Scholar]
- [238].Benninger M.S., Hadley J.A., Osguthorpe J.D., Marple B.F., Leopold D.A., Derebery M.J., Hannley M. Techniques of intranasal steroid use. Otolaryngol. Head Neck Surg. 2004;130:5–24. doi: 10.1016/j.otohns.2003.10.007. [DOI] [PubMed] [Google Scholar]
- [239].Ikeda K., Sakurada T., Suzaki Y., Takasaka T. Efficacy of systemic corticosteroid treatment for anosmia with nasal and paranasal sinus disease. Rhinology. 1995;33:162–165. [PubMed] [Google Scholar]
- [240].Scheibe M., Bethge C., Witt M., Hummel T. Intranasal administration of drugs. Arch. Otorhinolaryngol. Head Neck Surg. 2008;134:643–646. doi: 10.1001/archotol.134.6.643. [DOI] [PubMed] [Google Scholar]
- [241].Hardy J.G., Lee S.W., Wilson C.G. Intranasal drug delivery by spray and drops. J. Pharmacy Pharmacol. 1985;37:294–297. doi: 10.1111/j.2042-7158.1985.tb05069.x. [DOI] [PubMed] [Google Scholar]
- [242].Newman S.P., Moren F., Clarke S.W. Deposition pattern from a nasal pump spray. Rhinology. 1987;25:77–82. [PubMed] [Google Scholar]
- [243].McGarry G.W., Swan I.R. Endoscopic photographic comparison of drug delivery by ear-drops and by aerosol spray. Clin. Otolaryngol. 1992;17:359–360. doi: 10.1111/j.1365-2273.1992.tb01013.x. [DOI] [PubMed] [Google Scholar]
- [244].Shu C.H., Lee P.L., Shiao A.S., Chen K.T., Lan M.Y. Topical corticosteroids applied with a squirt system are more effective than a nasal spray for steroid-dependent olfactory impairment. Laryngoscope. 2012;122:747–750. doi: 10.1002/lary.23212. [DOI] [PubMed] [Google Scholar]
- [245].Parnes S.M., Chuma A.V. Acute effects of antileukotrienes on sinonasal polyposis and sinusitis. Ear Nose Throat J. 2000;79:18–20. [PubMed] [Google Scholar]
- [246].Parnes S.M., Chuma A.V. Acute effects of antileukotrienes on sinonasal polyposis and sinusitis. Ear Nose Throat J. 2000;79:24–25. [PubMed] [Google Scholar]
- [247].Bachmann G., Hommel G., Michel O. Effect of irrigation of the nose with isotonic salt solution on adult patients with chronic paranasal sinus disease. Eur. Arch. Otorhinolaryngol. 2000;257:537–541. doi: 10.1007/s004050000271. [DOI] [PubMed] [Google Scholar]
- [248].Rundles W. Prognosis in the neurologic manigfestations of pernicious anemia. Am. Soc. Hematol. 1946;1:209–219. [PubMed] [Google Scholar]
- [249].Tanaka O., Mukaino Y. The effect of auricular acupuncture on olfactory acuity. Am. J. Chin. Med. 1999;27:19–24. doi: 10.1142/S0192415X99000045. [DOI] [PubMed] [Google Scholar]
- [250].Stevenson D.D., Hankammer M.A., Mathison D.A., Christiansen S.C., Simon R.A. Aspirin desensitization treatment of aspirin-sensitive patients with rhinosinusitis-asthma: Long-term outcomes. J. Allergy Clin. Immunol. 1996;98:751–758. doi: 10.1016/S0091-6749(96)70123-9. [DOI] [PubMed] [Google Scholar]
- [251].Reden J., El-Hifnawi D.J., Zahnert T., Hummel T. The effect of a herbal combination of primrose, gentian root, vervain, elder flowers, and sorrel on olfactory function in patients with a sinonasal olfactory dysfunction. Rhinology. 2011;49:342–346. doi: 10.4193/Rhino10.151. [DOI] [PubMed] [Google Scholar]
- [252].Moran D.T., Jafek B.W., Eller P.M., Rowley J.C. Ultrastructural histopathology of human olfactory dysfunction. Microsc. Res. Tech. 1992;23:103–110. doi: 10.1002/jemt.1070230202. [DOI] [PubMed] [Google Scholar]
- [253].Yamagishi M., Fujiwara M., Nakamura H. Olfactory mucosal findings and clinical course in patients with olfactory disorders following upper respiratory viral infection. Rhinology. 1994;32:113–118. [PubMed] [Google Scholar]
- [254].Henkin R.I., Schecter P.J., Friedewald W.T., Demets D.L., Raff M. A double-blind study of the effects of zinc sulfate on taste and smell dysfunction. Am. J. Med. Sci. 1976;272:285–299. doi: 10.1097/00000441-197611000-00006. [DOI] [PubMed] [Google Scholar]
- [255].Yee K.K., Rawson N.E. Retinoic acid enhances the rate of olfactory recovery after olfactory nerve transection. Brain Res. Dev. Brain Res. 2000;124:129–132. doi: 10.1016/S0165-3806(00)00108-5. [DOI] [PubMed] [Google Scholar]
- [256].Hendriks A.P.J. Olfactory dysfunction. Rhinology. 1988;26:229–251. [PubMed] [Google Scholar]
- [257].Reden J., Herting B., Lill K., Kern R. T, Hummel: Treatment of postinfectious olfactory disorders with minocycline: A double-blind, placebo-controlled study. Laryngoscope. 2011;121:679–682. doi: 10.1002/lary.21401. [DOI] [PubMed] [Google Scholar]
- [258].Reljanovic M., Reichel G., Rett K., Lobisch M., Schuette K., Moller W., Tritschler H.J., Mehnert H. Treatment of diabetic polyneuropathy with the antioxidant thioctic acid (alpha-lipoic acid): A two year multicenter randomized double-blind placebo-controlled trial (ALADIN II). Alpha Lipoic Acid in Diabetic Neuropathy. Free Radic. Res. 1999;31:171–179. doi: 10.1080/10715769900300721. [DOI] [PubMed] [Google Scholar]
- [259].Packer L., Kraemer K., Rimbach G. Molecular aspects of lipoic acid in the prevention of diabetes complications. Nutr. 2001;17:888–895. doi: 10.1016/S0899-9007(01)00658-X. [DOI] [PubMed] [Google Scholar]
- [260].Hounsom L., Horrobin D.F., Tritschler H., Corder R., Tomlinson D.R. A lipoic acid-gamma linolenic acid conjugate is effective against multiple indices of experimental diabetic neuropathy. Diabetologia. 1998;41:839–843. doi: 10.1007/s001250050996. [DOI] [PubMed] [Google Scholar]
- [261].Garrett N.E., Malcangio M., Dewhurst M., Tomlinson D.R. Alpha-lipoic acid corrects neuropeptide deficits in diabetic rats via induction of trophic support. Neurosci. Lett. 1997;222:191–194. doi: 10.1016/S0304-3940(97)13383-3. [DOI] [PubMed] [Google Scholar]
- [262].Coppey L.J., Gellett J.S., Davidson E.P., Dunlap J.A., Lund D.D., Yorek M.A. Effect of antioxidant treatment of streptozotocin-induced diabetic rats on endoneurial blood flow, motor nerve conduction velocity, and vascular reactivity of epineurial arterioles of the sciatic nerve. Diabetes. 2001;50:1927–1937. doi: 10.2337/diabetes.50.8.1927. [DOI] [PubMed] [Google Scholar]
- [263].Lynch M.A. Lipoic acid confers protection against oxidative injury in non-neuronal and neuronal tissue. Nutr. Neurosci. 2001;4:419–438. doi: 10.1080/1028415X.2001.11747378. [DOI] [PubMed] [Google Scholar]
- [264].Hummel T., Heilmann S., Hüttenbrink K.B. Lipoic acid in the treatment of smell dysfunction following viral infection of the upper respiratory tract. Laryngoscope. 2002;112:2076–2080. doi: 10.1097/00005537-200211000-00031. [DOI] [PubMed] [Google Scholar]
- [265].Quint C., Temmel A.F.P., Hummel T., Ehrenberger K. The quinoxaline derivative caroverine in the treatment of sensorineural smell disorders: A proof of concept study. Acta Otolaryngol. 2002;122:877–881. doi: 10.1080/003655402_000028054. [DOI] [PubMed] [Google Scholar]
- [266].Quint C., Temmel A.F., Hummel T., Ehrenberger K. The quinoxaline derivative caroverine in the treatment of sensorineural smell disorders: A proof-of-concept study. Acta Otolaryngol. 2002;122:877–881. doi: 10.1080/003655402_000028054. [DOI] [PubMed] [Google Scholar]
- [267].Laster M.G., Russell R.M., Jacques P.F. Impairment of taste and olfaction in patients with cirrhosis, the role of vitamin A. Hum. Nutr. Clin. Nutr. 1984;38:203–214. [PubMed] [Google Scholar]
- [268].Reden J., Lill K., Zahnert T., Haehner A., Hummel T. Olfactory function in patients with postinfectious and posttraumatic smell disorders before and after treatment with vitamin A: A double-blind, placebo-controlled, randomized clinical trial. Laryngoscope. 2012;122:1906–1909. doi: 10.1002/lary.23405. [DOI] [PubMed] [Google Scholar]
- [269].Schiffman S. Drugs influencing taste and smell perception. In: Getchell T.V., Doty R.L., Bartoshuk L.M., Snow J.B., editors. Smell and Taste in Health and Disease. New York: Raven; 1991. pp. 845–850. [Google Scholar]
- [270].Henkin R.I. Drug-induced taste and smell disorders. Incidence, mechanisms and management related primarily to treatment of sensory receptor dysfunction. Drug Saf. 1994;11:318–377. doi: 10.2165/00002018-199411050-00004. [DOI] [PubMed] [Google Scholar]
- [271].Doty R.L., Bromley S.M. Effects of drugs on olfaction and taste. Otolaryngol. Clin. North Am. 2004;37:1229–1254. doi: 10.1016/j.otc.2004.05.002. [DOI] [PubMed] [Google Scholar]
- [272].Michael W. Anosmia treated with acupuncture. Acupunct. Med. 2003;21:153–154. doi: 10.1136/aim.21.4.153. [DOI] [PubMed] [Google Scholar]
- [273].Vent J., Wang D.W., Damm M. Effects of traditional Chinese acupuncture in post-viral olfactory dysfunction. Otolaryngol. Head Neck Surg. 2010;142:505–509. doi: 10.1016/j.otohns.2010.01.012. [DOI] [PubMed] [Google Scholar]
- [274].Silas J., Doty R.L. No evidence for specific benefit of acupuncture over vitamin B complex in treating persons with olfactory dysfunction. Otolaryngol. Head Neck Surg. 2010;143:603. doi: 10.1016/j.otohns.2010.07.008. [DOI] [PubMed] [Google Scholar]
- [275].Henkin R.I., Velicu I., Schmidt L. An open-label controlled trial of theophylline for treatment of patients with hyposmia. Am. J. Med. Sci. 2009;337:396–406. doi: 10.1097/MAJ.0b013e3181914a97. [DOI] [PubMed] [Google Scholar]
- [276].Henkin R.I., Velicu I., Schmidt L. Relative resistance to oral theophylline treatment in patients with hyposmia manifested by decreased secretion of nasal mucus cyclic nucleotides. Am. J. Med. Sci. 2011;341:17–22. doi: 10.1097/MAJ.0b013e3181f1fdc8. [DOI] [PubMed] [Google Scholar]
- [277].Henkin R.I. Comparative monitoring of oral theophylline treatment in blood serum, saliva, and nasal mucus. Ther. Drug Monit. 2012;34:217–221. doi: 10.1097/FTD.0b013e3182492a20. [DOI] [PubMed] [Google Scholar]
- [278].Levy L.M., Henkin R.I., Lin C.S., Hutter A., Schellinger D. Increased brain activation in response to odors in patients with hyposmia after theophylline treatment demonstrated by fMRI. J. Comput. Assist. Tomogr. 1998;22:760–770. doi: 10.1097/00004728-199809000-00019. [DOI] [PubMed] [Google Scholar]
- [279].Levy L.M., Henkin R.I., Lin C.S., Hutter A., Schellinger D. Odor memory induces brain activation as measured by functional MRI. J. Comput. Assist. Tomogr. 1999;23:487–498. doi: 10.1097/00004728-199907000-00001. [DOI] [PubMed] [Google Scholar]
- [280].Gudziol V., Hummel T. Effects of pentoxifylline on olfactory sensitivity: A postmarketing surveillance study. Arch. Otolaryngol. Head Neck Surg. 2009;135:291–295. doi: 10.1001/archoto.2008.524. [DOI] [PubMed] [Google Scholar]
- [281].Gudziol V., Pietsch J., Witt M., Hummel T. Theophylline induces changes in the electro-olfactogram of the mouse. Eur. Arch. Otorhinolaryngol. 2010;267:239–243. doi: 10.1007/s00405-009-1076-7. [DOI] [PubMed] [Google Scholar]
- [282].Hummel T., Rissom K., Hähner A., Reden J., Weidenbecher M., Hüttenbrink K.B. Effects of olfactory training in patients with olfactory loss. Laryngoscope. 2009;119:496–499. doi: 10.1002/lary.20101. [DOI] [PubMed] [Google Scholar]
- [283].Konstantinidis I., Tsakiropoulou E., Bekiaridou P., Kazantzidou C., Constantinidis J. Use of olfactory training in post-traumatic and postinfectious olfactory dysfunction. Laryngoscope. 2013;123:85–90. doi: 10.1002/lary.24390. [DOI] [PubMed] [Google Scholar]
- [284].Fleiner F., Lau L., Goktas O. Active olfactory training for the treatment of smelling disorders. Ear Nose Throat J. 2012;91:198–203. doi: 10.1177/014556131209100508. [DOI] [PubMed] [Google Scholar]
- [285].Geissler K., Reimann H., Gudziol H., Bitter T., Guntinas-Lichius O. Olfactory training for patients with olfactory loss after upper respiratory tract infections. Eur. Arch. Otorhinolaryngol. 2014;271:1557–1562. doi: 10.1007/s00405-013-2747-y. [DOI] [PubMed] [Google Scholar]
- [286].Damm M., Pikart L.K., Reimann H., Burkert S., Goktas O., Haxel B., Frey S., Charalampakis I., Beule A., Renner B., Hummel T., Hüttenbrink K.B. Olfactory training is helpful in postinfectious olfactory loss – A randomized controlled multicenter study. Laryngoscope. 2014;124:826–831. doi: 10.1002/lary.24340. [DOI] [PubMed] [Google Scholar]
- [287].Youngentob S.L., Kent P.F. Enhancement of odorant-induced mucosal activity patterns in rats trained on an odorant. Brain Res. 1995;670:82–88. doi: 10.1016/0006-8993(94)01275-M. [DOI] [PubMed] [Google Scholar]








