Dear Editor,
Since the publication of our article, we have received many queries about the slit lamp protective shield [1]. As part of our local experience of stepping up infection control measures in ophthalmology clinics to minimise COVID-19 infection, we installed protective shields on slit lamps (Fig. 1). We believe the close proximity between ophthalmologists and patients during slit lamp examination could put doctors at risk of infection, as droplets from coughs or sneezes could spread the virus to anyone less than 6 ft away [2]. The measured distance between the doctor’s and patient’s face on a standard tower slit lamp is just about 1 ft, while that with a portable slit lamp is about 7–8 in. These distances are indeed closer that that seen on routine physical examinations, for example, respiratory examination on a medical ward. These shields can therefore act as an effective barrier in addition to other personal protective equipment.
Fig. 1.
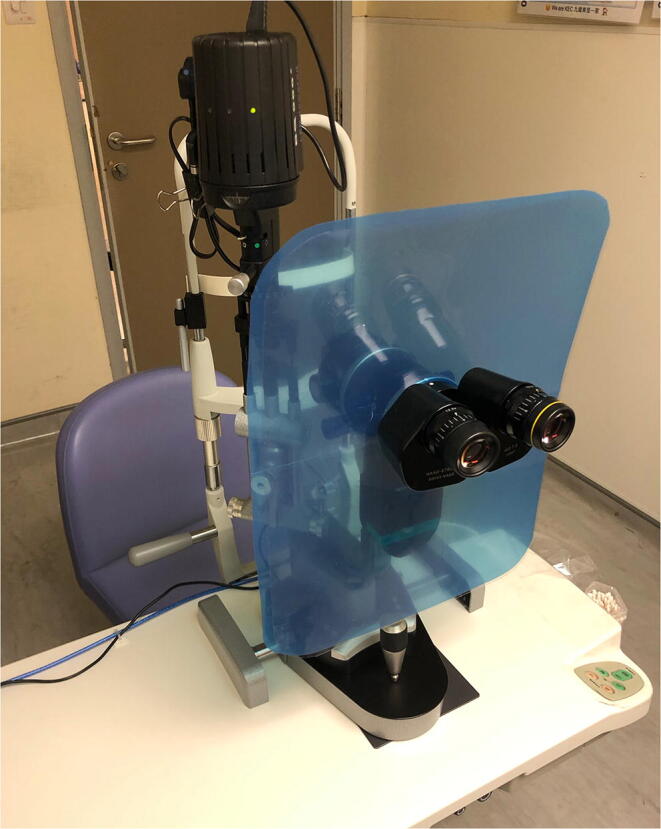
Protective shield with rounded corners on a tower slit lamp
We are aware of the commercially available breath shields for slit lamp but we found them smaller than the ideal size to offer sufficient protection. Also, they may not be readily available due to limited stock, current high demands and shipment time. We are delighted to share our local experience of custom-made, low-cost shields with all readers. We bought durable plastic sheets of A3 size from stationery shops, i.e. approximately 16 by 12 in. (Height × Width). A central cut-out circular area (ranging from 2 to 3 in., size depends on the actual calibre of the slit lamp) is created with scissors (Fig. 2). A3 is the optimal size to still allow the examiner to place his hand comfortably on the patient’s head. The shield can be installed after detaching the biomicroscope from the viewing arm then reattaching it to secure the shield firmly. Installing the film around the eyepieces is also an option for some older slit lamp models.
Fig. 2.
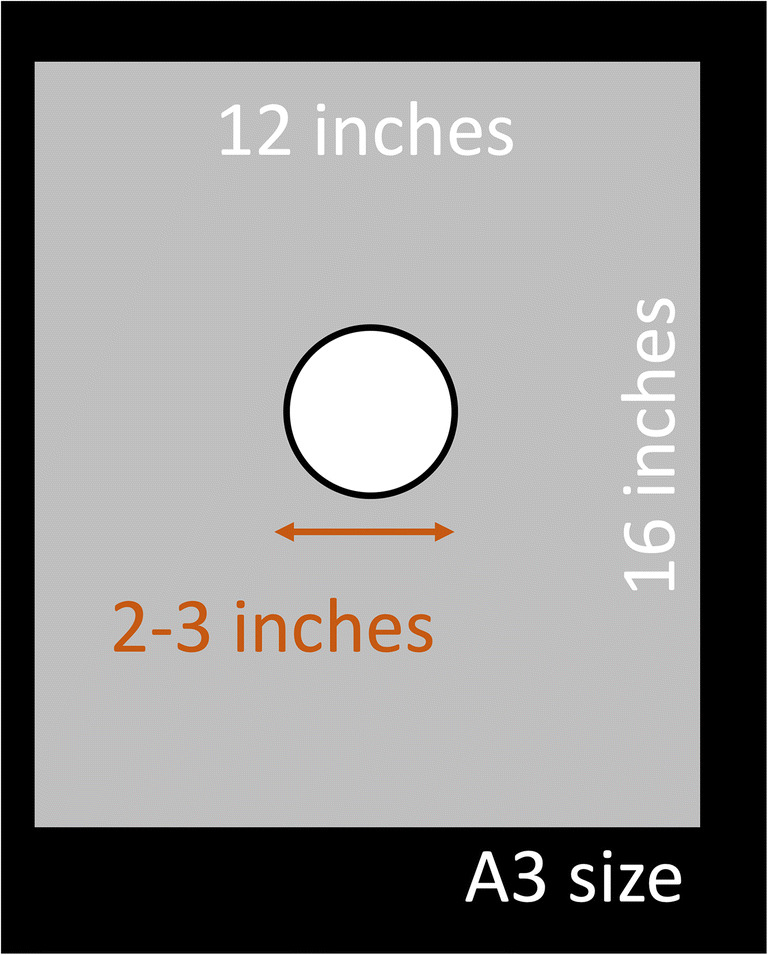
Typical dimensions of a custom made slit lamp shield. A central cut-out circular area (ranging from 2 to 3 in., size depends on the actual calibre of the slit lamp) is created with scissors on a plastic sheet of desired thickness of A3 size, i.e. approximately 16 by 12 in. (Height × Width)
The material chosen can be a consensus among ophthalmologists locally. Our experience is that the film should ideally be transparent to allow the examiner and the patient to see each other, and firm enough. We found that the spectrum of suitable material ranges from those that are firmer and stiffer, e.g. acrylic, to softer and more flexible, e.g. document folders and binding covers made of polyvinyl chloride (PVC) or polypropylene. Firm plastic is ideal as it minimises the chance of the film springing back and forth, the movement which can be easily caused by the examiner’s hand accidentally touching the film during examination. However, one should note that thicker plastic may not be able to fit and it is not possible to cut safely with office tools. Sticking a few pieces of thinner films together by thermal lamination is therefore an option. Chang et al. also suggested using X-ray or MRI photographic film [3]. One may also expose the film to achieve transparency.
We also installed protective shields on other ophthalmic equipment, including portable slit lamps (Fig. 3), optical coherence tomography (OCT) systems (Fig. 4) and fundus cameras. We used clear document folders of A4 size for the portable slit lamps.
Fig. 3.
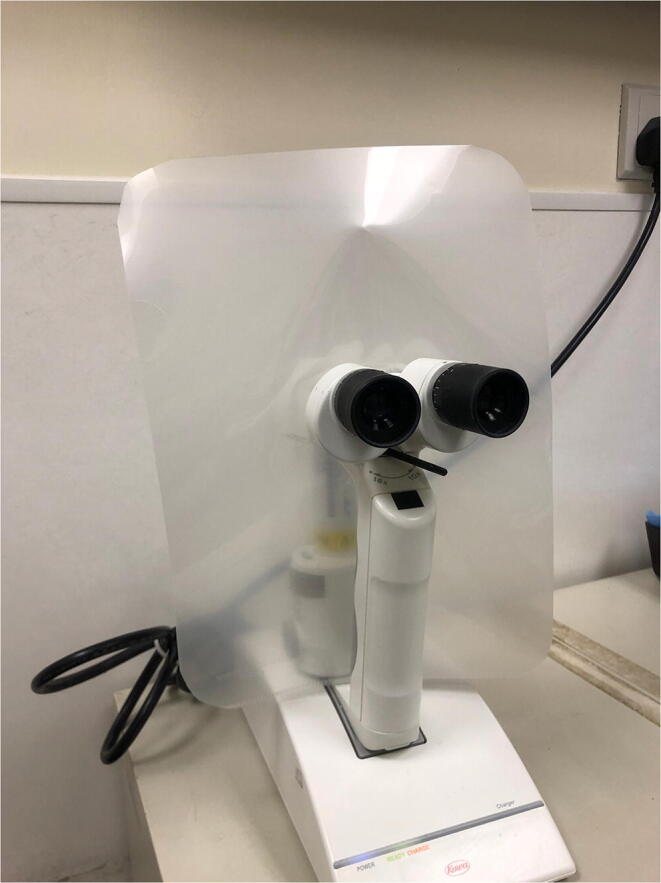
Protective shield on a portable slit lamp. A similar hole is made on a plastic sheet or document folder and secured around the objective lenses and the grip handle with the adhesive tapes. It can be cleaned or replaced regularly
Fig. 4.

Protective shield on an optical coherence tomography system
The Centres for Disease Control and Prevention (CDC) guidelines for disinfecting face shields were observed as slit lamp shields serve a similar role [4]. Along with slit lamps and table surfaces, they were cleaned with wipes containing 70% alcohol and allowed to air dry after each clinic session.
We hope that all readers will be able to benefit from our experience on installation and use of these slit lamp shields. We look forward to ideas of more refined designs of such shields from all around the world, with the hope to offer better protection for patients and ophthalmologists during this pandemic.
Acknowledgements
The authors thank the nursing staff serving our clinic at the United Christian Hospital, Ms Monica ML Lee, Ms KY Chan and Ms Peggy Lam, for their input.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lai TH, Tang WR, Chau SK, Fung KS, Li KK (2020) Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefes Arch Clin Exp Ophthal 258(5):1049–1055 [DOI] [PMC free article] [PubMed]
- 2.How Flu Spreads (2020) Centers for Disease Control and Prevention. https://www.cdc.gov/flu/about/disease/spread.htm. Accessed 23 Mar 2020
- 3.(2020) Coronavirus and ophthalmology: what can ophthalmologists do to protect themselves, staff and patients from COVID-19? Eurotimes. https://www.eurotimes.org/coronavirus-and-ophthalmology/. Accessed 23 March 2020
- 4.Strategies for Optimizing the Supply of Eye Protection (2020) Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/eye-protection.html. Accessed 23 Mar 2020


