Abstract
Rehospitalization following pediatric heart transplantation is common. However, existing data remain somewhat limited. Using a novel linkage between administrative and clinical databases, pediatric heart transplant (HT) recipients from 29 centers who survived to discharge were retrospectively reviewed to determine the frequency, timing of, and indication for all-cause rehospitalizations in the year following transplant discharge. Of 2870 pediatric HT recipients, 1835 (63.9%) were rehospitalized in the first year post-discharge (5429 total readmissions). Rehospitalization rates varied significantly across centers (46% to 100%) and were inversely correlated to center transplant volume (r2 0.25, p < 0.01). The median number of rehospitalizations per patient was 2 (IQR 1–4) and the median time to first rehospitalization was 29 days (IQR 9–99 days). Independent risk factors for rehospitalization included younger age at HT (HR 0.99, 95% CI 0.97–0.99), congenital heart disease (HR 1.2, 95% CI 1.1–1.4), listing status 1B at transplant (HR 1.3, 95% CI 1.1–1.5), and post-transplant complications including rejection prior to discharge (HR 1.5 95% CI 1.3–1.8) and chylothorax (HR 1.3, 95% CI 1.0–1.6). Cardiac diagnoses were the most common indication for rehospitalization (n = 1600, 29.5%), followed by infection (n = 1367, 25.2%). These findings may serve to guide the development of interventions aimed at reducing post-HT hospitalizations.
Keywords: Rehospitalization, Hospital readmission, Pediatric heart transplant
Introduction
HT recipients are at risk of life-long morbidity from transplant complications and as such, are at a greater risk of repeated hospitalizations. Data from The International Society for Heart and Lung Transplantation (ISHLT) registry support that readmission following pediatric HT is common, with over a third of patients rehospitalized in the first year [1]. Studies examining hospital readmission after adult solid organ transplant have found similar early readmission rates of approximately 30–45%, with wide variation in rehospitalization rates across transplant centers [2–4]. Primary causes for readmission in this population include infection and acute graft rejection [5–8].
In the pediatric HT population, readmission rates have been reported to be as high as 55–84% [9, 10]. However, these data were derived from a small number of centers and therefore may not be generalizable to centers nationwide. To guide future efforts in reducing hospital readmissions after pediatric HT, this study aimed to describe patterns of rehospitalization and assess the indications for rehospitalization in pediatric HT recipients utilizing a large multi-center database linkage.
Methods
The Scientific Registry of Transplant Recipients (SRTR) and Pediatric Health Information System (PHIS) databases were linked at the patient level using indirect identifiers (hospital, date of birth, sex, and date of transplant), the results of which have been previously described [11]. The SRTR data system includes data on all donors, wait-listed candidates, and transplant recipients in the United States, submitted by the members of the Organ Procurement and Transplantation Network (OPTN). The Health Resources and Services Administration, U.S. Department of Health and Human Services provides oversight to the activities of the OPTN and SRTR contractors. The SRTR includes data from every organ transplant and waitlist addition since late 1987. The PHIS database is an administrative and billing database that collects clinical and resource utilization data from hospital encounters (inpatient, observation, emergency department, and ambulatory surgery encounters) from > 50 tertiary children’s hospitals in the United States. In PHIS, children can be tracked across encounters using a unique encrypted medical record number, allowing an in-depth assessment of hospital readmissions following HT.
All patients ≤ 21 years of age who underwent HT between 2002 and 2016 and survived to hospital discharge were identified from the linked database for inclusion in the analysis. Rehospitalizations were assessed for one year following the date of initial discharge from the transplant hospitalization and included hospitalizations categorized as either inpatient or observation encounters in the PHIS database. Standard descriptive statistics were used to compare patients who required rehospitalization within one year post-discharge and those who did not. Variables assessed included age at transplantation, blood type, underlying diagnosis (cardiomyopathy, congenital heart disease, or retransplantation), sex, race, markers of socioeconomic status including median household income and insurance status, listing status at the time of HT, clinical factors including ventricular assist device (VAD), extracorporeal membrane oxygenation (ECMO), inotropic support, and mechanical ventilation at the time of HT, post-HT length of stay, day of week of discharge from the HT admission, and post-HT complications including cardiac or other reoperations, prolonged chest tube requirement, chylothorax, need for dialysis, pacemaker implantation, cardiac rejection, and stroke prior to discharge from the HT admission. The data source utilized for each variable is shown in Supplemental Table 1. The Chi-squared test was used to compare categorical data and the Wilcoxon rank-sum test was used for continuous data, as appropriate. The Kruskal–Wallis test was used to compare the number of rehospitalizations across seasons. Seasons were defined as follows: spring from March to May; summer from June to August; fall from September to November; winter from December to February. The Kaplan Meier method was used to assess overall freedom from rehospitalization, with standard error estimates adjusted for clustering within centers.
Classification of the etiologies for rehospitalization was completed in multiple steps. Admissions were categorized into mutually exclusive groups based on All Patient Refined-Diagnosis Related Group (APR-DRG, 3 M Health Information Systems) codes assigned to the specific hospital encounter (Supplemental Table 2). For admissions that were unable to be grouped based on APR-DRG codes, the primary International Classification of Diseases (ICD) diagnosis codes were used. For each hospital encounter, PHIS records up to 41 distinct ICD diagnosis codes; the first of these codes indicates the primary reason for the hospital admission. The primary ICD diagnosis code for the hospital encounter was categorized using Clinical Classification Software (CCS) freely available from the Healthcare Cost and Utilization Project. CCS utilizes both ICD-9 and ICD-10 codes and represents a standardized coding system that collapses ICD diagnosis and procedure codes into a smaller number of clinically meaningful categories that are more useful for presenting descriptive statistics than are individual ICD codes [12]. CCS categories were subsequently collated into the previously defined mutually exclusive categories. Defined categories included cardiac, fluids/electrolyte/nutrition, gastrointestinal, hematologic, infection, malignancy, neurologic, psychiatric, renal, endocrine, and respiratory (Supplemental Table 2). Any hospitalizations that remained uncategorized following utilization of both APR-DRG and the primary ICD diagnosis code were grouped as “unknown.” For patients categorized as having a cardiac or infectious indication for rehospitalization, the remaining ICD codes were tabulated to fully describe the indications for hospitalization in these groups. Rehospitalizations were also assessed based on the need for intensive care unit (ICU) admission, ECMO support, and the need for mechanical ventilation. In-hospital mortality during rehospitalization was also documented.
Center-specific factors examined in association with hospital readmission included annual transplant volume (determined using publicly available data from the Organ Procurement and Transplantation Network over the past 10 years) and median post-transplant length of stay. The rate of rehospitalization was calculated for each center. The association between annual center transplant volume, median post-transplant hospital length of stay, and the rate of rehospitalization was assessed using Spearman correlations.
Risk factors for rehospitalization were assessed using a Cox proportional hazard model. Variables were chosen for inclusion in the multivariable model if p < 0.1 on univariate analysis. Post-transplant length of stay is a marker of illness following transplant and is related to post-transplant complications. Given this relationship, post-transplant length of stay was excluded from this analysis due to concerns for collinearity with post-transplant complications including need for dialysis, rejection, chylothorax, prolonged chest tube requirement, and non-cardiac surgical intervention.
All statistical analyses were performed in SAS version 9.4 (SAS Institute; Cary, NC) or STATA version 15 (StataCorp LLC; College Station, TX) with two-sided p < 0.05 considered statistically significant. This project was approved by the Vanderbilt University IRB, PHIS, and SRTR.
Results
A total of 2870 HT recipients from 29 different centers were identified for inclusion from the linked database. In this group, 1835 (63.9%) patients required at least one hospitalization within the first year following discharge (1648 patients with inpatient admissions and 187 patients with only observation encounters). Patient demographics are shown in Table 1. Rehospitalized patients were younger, more likely to have an original diagnosis of congenital heart disease, more likely to have private or government insurance, less likely to be listed 1A at the time of transplant, and less likely to be supported with a ventricular assist device. These patients also had evidence of a more complicated post-transplant course including a longer post-transplant length of stay and a higher incidence of non-cardiac surgical intervention, prolonged chest tube requirement, chylothorax, need for dialysis, and rejection prior to hospital discharge. The median time from discharge to the first rehospitalization was 29 days (IQR 9–99 days). For patients requiring rehospitalization, the median number of admissions within one year following discharge was 2 (IQR 1–4) and the median number of total rehospitalized days was 9 (IQR 4–20). Of the 5,429 total rehospitalizations, 69.8% (n = 3792) were inpatient admissions and 30.2% (n = 1637) were observation encounters. By season, 1417 (26.1%) rehospitalizations occurred during the spring, 1424 (26.2%) during the summer, 1247 (23%) during the fall, and 1341 (24.7%) during the summer. No significant difference was detected in the number of rehospitalizations by season (p = 0.133). Overall freedom from rehospitalization is shown in Fig. 1.
Table 1.
Patient and HT admission characteristics
| Total | Not rehospitalized | Rehospitalized | p valuea | |
|---|---|---|---|---|
| n = 2870 | n = 1035 (36.1) | n = 1835 (63.9) | ||
| Age (years) | 4 (0–12) | 6 (0–13) | 3 (0–12) | < 0.001 |
| Blood type | 0.190 | |||
| O | 1294 (45.1) | 479 (46.3) | 815 (44.4) | |
| A | 1086 (37.8) | 399 (38.6) | 687 (37.4) | |
| B | 373 (13.0) | 116 (11.2) | 257 (14.0) | |
| AB | 117 (4.1) | 41 (4.0) | 76 (4.1) | |
| Diagnosis | < 0.001 | |||
| Cardiomyopathy | 1,376 (48.5) | 571 (55.7) | 805 (44.5) | |
| Congenital heart disease | 1,303 (46.0) | 399 (38.9) | 904 (50.0) | |
| Retransplant | 157 (5.5) | 55 (5.4) | 102 (5.6) | |
| Male gender | 1555 (54.2) | 544 (52.6) | 1,011 (55.1) | 0.191 |
| Race | 0.111 | |||
| Caucasian | 1680 (58.5) | 582 (56.2) | 1,098 (59.8) | |
| African American | 536(18.7) | 211 (20.4) | 325 (17.7) | |
| Asian | 92 (3.2) | 40 (3.9) | 52 (2.8) | |
| Hispanic | 488 (17.0) | 171 (16.5) | 317 (17.3) | |
| Other | 74 (2.6) | 31 (3.0) | 43 (2.3) | |
| Median household income (US dollars) | 40,422 (31,883–53,387) | 40,632 (31,674–53,361) | 40,230 (31,968–53,387) | 0.947 |
| Insurance status | 0.009 | |||
| Private | 1072 (38.6) | 391 (38.6) | 681 (38.7) | |
| Government | 1283 (46.2) | 443 (43.7) | 840 (47.7) | |
| Other payor | 436 (15.1) | 180 (17.8) | 240 (13.6) | |
| Listing status | 0.036 | |||
| 1A | 2374 (82.7) | 880 (85.0) | 1,494 (81.4) | |
| 1B | 310(10.8) | 101 (9.8) | 209 (11.4) | |
| 2 | 186 (6.5) | 54 (5.2) | 132 (7.2) | |
| ECMO at HT | 124 (4.3) | 50 (4.8) | 74 (4.0) | 0.313 |
| Inotrope at HT | 1439 (50.1) | 527 (50.9) | 912 (49.7) | 0.531 |
| Mechanical ventilation at HT | 454 (15.8) | 151 (14.6) | 303 (16.5) | 0.175 |
| VAD at HT | 493 (17.2) | 202 (19.5) | 291 (15.9) | 0.013 |
| Post-transplant length of stay (days) | 18 (12–32) | 15 (10–24) | 20 (13–35) | < 0.001 |
| Post-transplant complications | ||||
| Cardiac reoperation | 138 (6.2) | 55 (6.8) | 83 (5.9) | 0.403 |
| Chest tube > 2 weeks | 137 (7.2) | 31 (4.5) | 106 (8.7) | 0.001 |
| Chylothorax | 140 (4.9) | 33 (3.2) | 107 (5.8) | 0.002 |
| Dialysis | 93 (3.3) | 22 (2.1) | 71 (3.9) | 0.011 |
| Other operations | 284 (12.8) | 85 (10.5) | 199 (14.2) | 0.014 |
| Pacemaker | 19 (0.7) | 5 (0.5) | 14 (0.8) | 0.373 |
| Rejection | 340 (13.2) | 79 (8.6) | 261 (15.7) | < 0.001 |
| Stroke | 68 (2.4) | 19 (1.8) | 49 (2.7) | 0.154 |
| Weekend discharge from transplant admission | 261 (9.1) | 91 (8.8) | 170 (9.3) | 0.662 |
HT heart transplant, US United States, ECMO extracorporeal membrane oxygenation, VAD ventricular assist device Data presented as n (%) for categorical and median (IQR) for continuous variables
p values from Chi-squared test for categorical and Wilcoxon rank-sum test for continuous variables
Fig. 1.
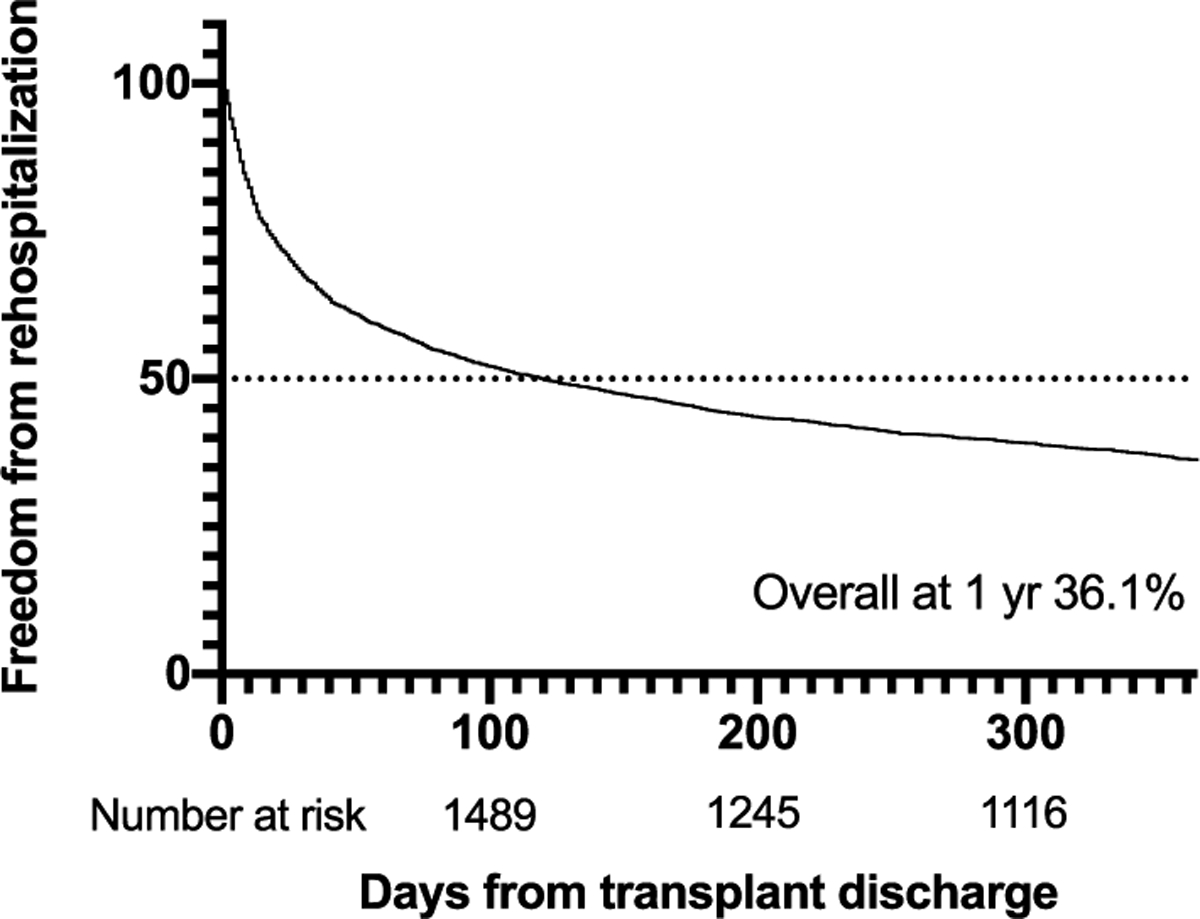
Freedom from rehospitalization in the first year following discharge from the transplant hospitalization (n = 2870)
The indications for hospital readmission grouped by etiology are shown in Fig. 2. Cardiac diagnoses were the most common indication for rehospitalization (n = 1600, 29.5%), with complications of transplant having the highest prevalence (n = 1043, 65.2%). Prior to the implementation of the ICD10 in 2015, a code for rejection did not exist. Of the 313 rehospitalizations with a cardiac etiology that occurred following the transition to ICD10, 32.3% were due to heart transplant rejection (n = 101, 6.3% of all rehospitalizations). The second most common indication for rehospitalization was infection (n = 1367, 25.2%), with the most common being intestinal infections (n = 214, 15.7%), followed by viral infections (n = 188, 13.8%).
Fig. 2.
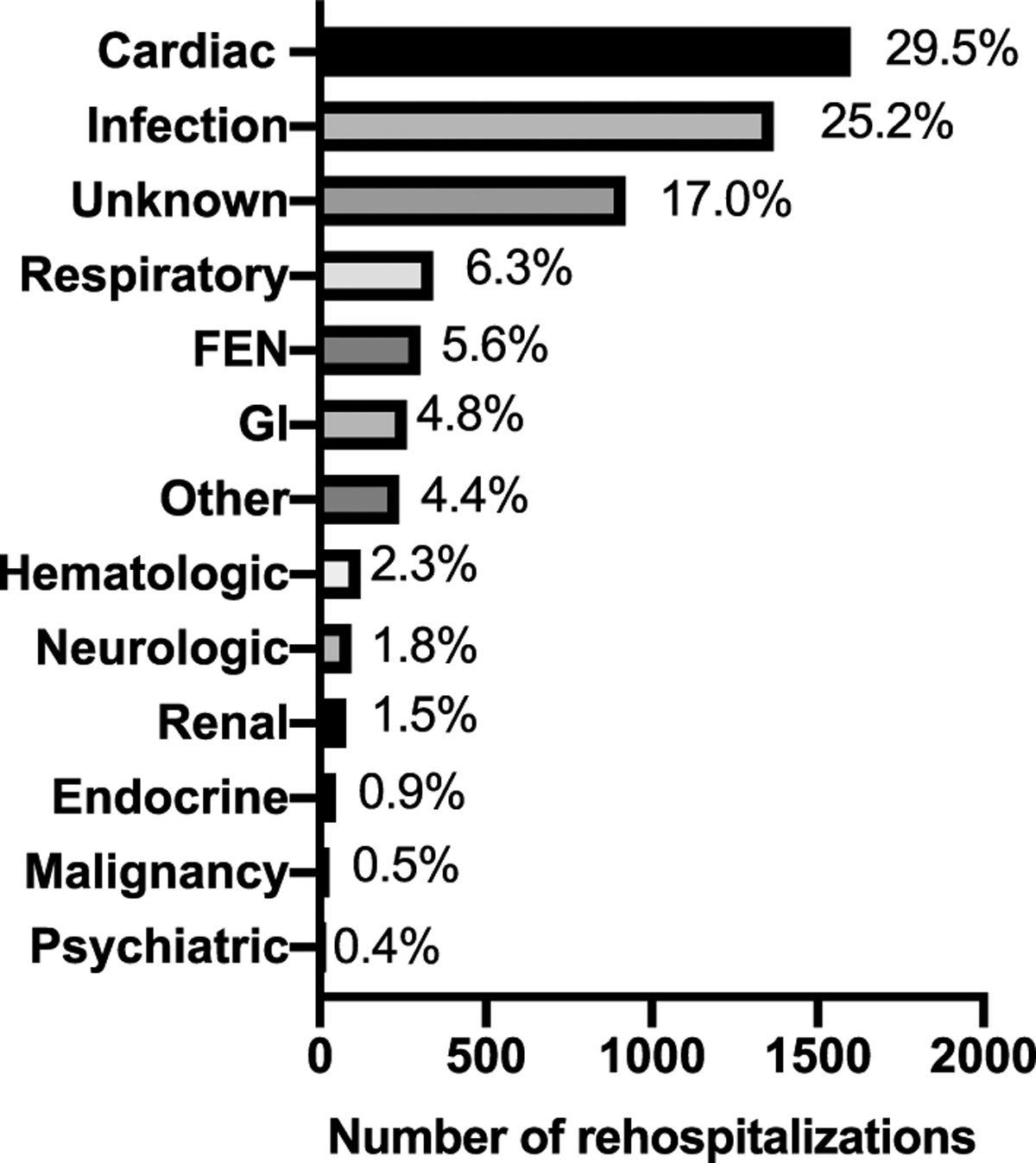
Total number of rehospitalizations in the first year following transplant discharge (n = 5429) categorized by the indication for rehospitalization. FEN fluid, electrolyte, nutrition; GI gastrointestinal
Among the rehospitalized cases, ICU care was required in 1108 (20.4%), ECMO was utilized in 30 (0.6%), and mechanical ventilation was required in 396 (7.3%). A total of 62 (1.1%) patients died during a readmission encounter.
Rates of rehospitalization across the 29 centers included in the analysis varied from 46% (1 center) to 100% (3 centers). Center-specific rehospitalization rates demonstrated an inverse correlation with transplant center volume (r2 = 0.25, p = 0.006) (Fig. 3). No significant relationship was detected between center-specific rehospitalization rates and post-transplant length of stay (r2 = 0.09, p = 0.083) (Supplemental Fig. 1).
Fig. 3.
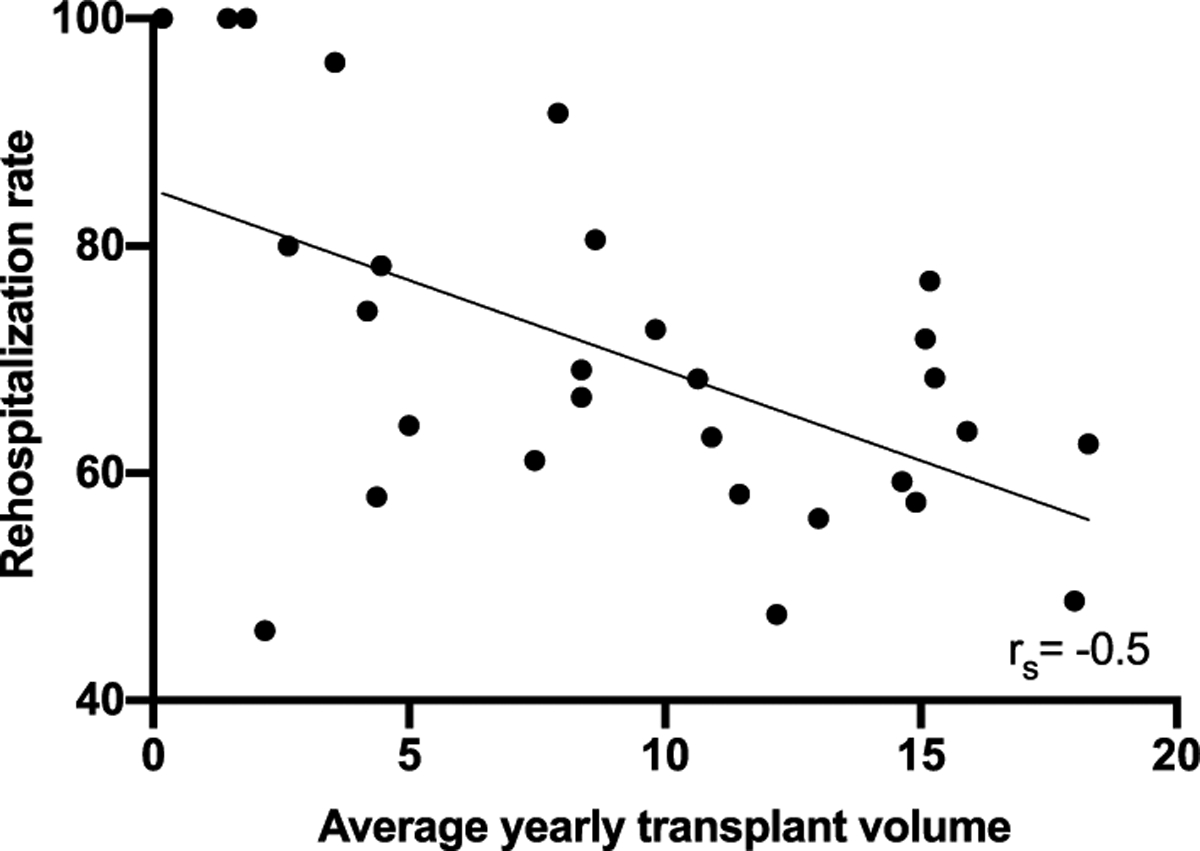
Correlation between center rehospitalization rate and average annual transplant volume across 29 pediatric heart transplant centers
Factors independently associated with rehospitalization in the first year on time-to-event analysis include patient age (HR 0.99, 95% CI 0.97–0.99, p = 0.008), an underlying diagnosis of congenital heart disease (HR 1.23, 95% CI 1.07–1.39, p = 0.003), listing status 1B at the time of transplantation (HR 1.27, 95% CI 1.05–1.54, p = 0.013), rejection prior to initial hospital discharge (HR 1.51, 95% CI 1.31–1.76, p < 0.001), and post-transplant chylothorax (HR 1.27, 95% CI 1.03–1.55, p = 0.024), as shown in Fig. 4.
Fig. 4.
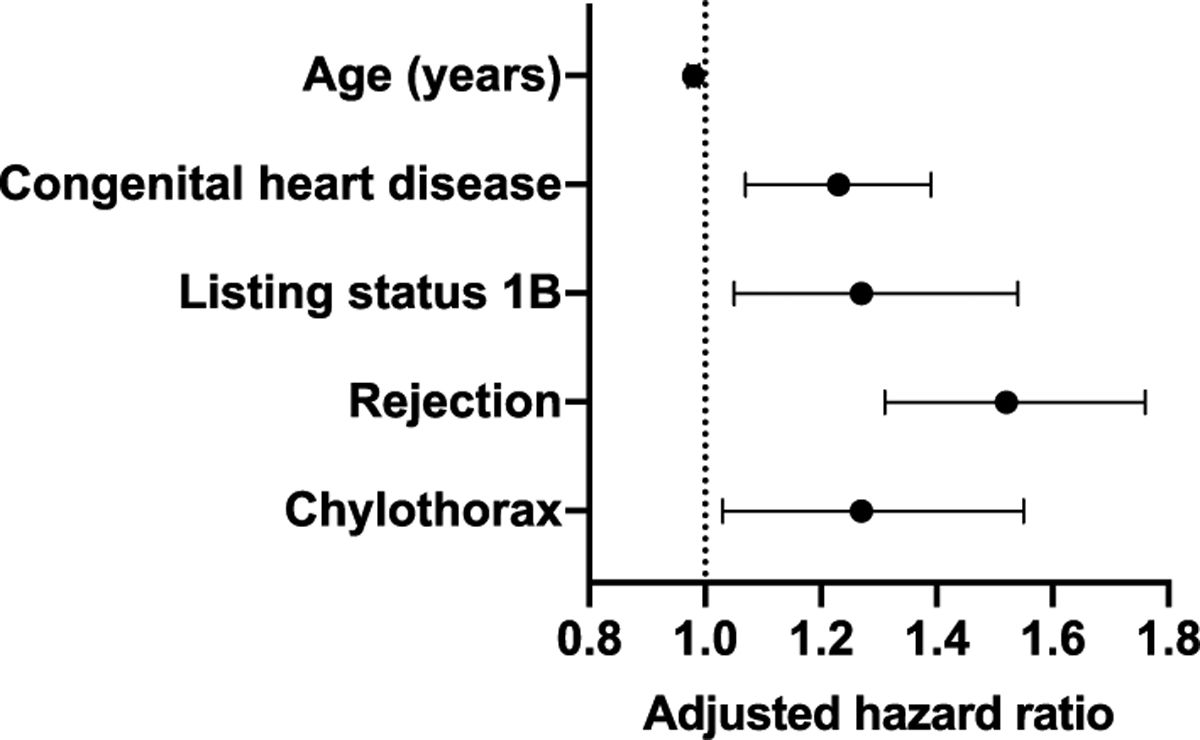
Patient factors independently associated with rehospitalization in the first year following transplant discharge
Discussion
This study represents the largest analysis of rehospitalization following pediatric HT to date. Notably, across the 29 HT centers included in the study, over 60% of patients were rehospitalized in the year following their transplant discharge. This is higher than the previously reported 30–45% readmission rate from single-center studies and ISHLT registry data [1, 9]. This may be partially explained by the inclusion of observation admissions, which accounted for 6.5% of the rehospitalization rate in our analysis. However, recently published data from the Clinical Trials in Organ Transplantation for Children (CTOTC-04) collaborative have reported a similarly high rate of readmission, 56.8%, in the first year following HT [10]. Approximately half of all rehospitalizations in our study occurred early, within 30 days of transplant admission discharge, a finding corroborated by the 29.5% early readmission rate reported by Mahle et al. [10].
A third of all rehospitalizations were indicated as cardiac diagnoses, including rejection. Due to reliance on ICD coding data to determine the cause for hospital readmission, further breakdown of the cardiac diagnoses was not possible as the primary indication for admission was coded as “complications of transplant” for the majority of cases. Rehospitalization for rejection may have been coded as “complications of transplant” prior to 2015, as an ICD code for rejection did not exist prior to the implementation of ICD-10. The second most common indication for rehospitalization was for infection, with intestinal infection being the most common diagnosis. This finding is unsurprising given the immunosuppressed state of heart transplant recipients early after transplant and the subsequent increased risk for infection, as well as the common nature of viral infections in children. The findings of graft rejection and infection as the most common causes of post-transplant hospital readmissions have been demonstrated following pediatric solid organ transplant and in adult HT recipients [4, 9, 10, 13]. Among rehospitalizations, admission to the ICU was less common, with the utilization of ECMO or mechanical ventilation rarer still, findings that were similar to those reported by Hollander et al. [9].
The finding that the rehospitalization rate correlates inversely with transplant center volume may also have implications for nationwide practice. There has been ongoing interest in the impact of center volume on transplant outcomes. Both 30-day and 1-year survival following transplant in adults with congenital heart disease is significantly worse at low-volume centers [14]. Additionally, listing at low-volume centers is independently associated with higher waitlist mortality [15]. The same practices at larger-volume centers that result in better post-transplant outcomes may explain the inverse association between center volume and rehospitalization rate found in this study. The sharing of practice protocols from larger transplant centers may be an effective strategy for reducing post-transplant rehospitalizations nationwide.
This study found several factors associated with rehospitalization including younger age, diagnosis of congenital heart disease, listing status 1B, and the complications of graft rejection and chylothorax prior to initial discharge. Younger age and postoperative complications have been previously documented as risk factors for readmission following pediatric cardiac surgery [16]. Patients with a pretransplant diagnosis of congenital heart disease are known to have increased morbidity and mortality following transplant, for which they may require more frequent hospitalization [1]. The association between a pretransplant listing status of 1B and rehospitalization following transplant is not readily explained; however, listing status other than 1A was also identified for a risk factor for readmission by Mahle et al. [10] It is conceivable that this finding originates from the inferior post-transplant survival in patients listed status 1A, but also may indicate that current allocation system does not adequately quantify patient risk [17]. The risk factors identified in this study, derived from a diverse population of patients across many centers, should be more generalizable to the pediatric transplant population compared to prior studies. While no individual factor stands out as a strong predictor of rehospitalization, together they may be used to target efforts aimed at reducing post-transplant readmissions as well as inform patient expectations of the year following transplant.
There are inherent limitations to our analysis. Although the rehospitalizations analyzed have been classified as either inpatient or observation encounters, we are unable to discriminate hospital admissions related to routine procedures, such as surveillance myocardial biopsies. While many of the largest transplant centers participate in PHIS, not all centers participate. We found rehospitalization rates to correlate inversely with center volume. However, larger transplant programs may admit patients to outside hospitals, not accounted for in our dataset, at a higher frequency compared to smaller programs that may lack these affiliations. Despite these limitations, our analysis represents the largest analysis of hospital readmissions to date and includes a wide spectrum of transplant centers. The inherent limitations of ICD coding make identification of the indication for hospital readmission challenging. The use of CCS software aided in classifying readmissions into clinically meaningful categories, but also has limitations. Errors in coding also may be present, but the incidence of such errors cannot be readily assessed by our analysis. Lastly, the incidence of rehospitalization may be underestimated as our analysis cannot capture readmissions to hospitals other than each patient’s primary transplant center.
Conclusions
Nearly two-thirds of pediatric HT recipients are rehospitalized in the year following transplant, with cardiac complications and infection being the most common reasons for rehospitalization. The rates of rehospitalization are highly variable across centers and associated with center transplant volume. Sharing best practices between centers, especially in high-risk patient groups, may be an effective strategy to reduce post-HT hospitalizations.
Supplementary Material
Funding
This project was supported through internal funding from the Katherine Dodd Faculty Scholar Program at Vanderbilt University (JG). Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health T32HL105334 (NL). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest
No authors have conflict of interest to declare in relation to the material presented.
Disclosures The data reported here have been supplied by the Hennepin Healthcare Research Institute as the contractor for the SRTR. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy of or interpretation by the SRTR or the U.S. Government.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s00246–020-02326-x) contains supplementary material, which is available to authorized users.
References:
- 1.Rossano JW, Cherikh WS, Chambers DC, Goldfarb S, Hayes D Jr, Khush KK, Kucheryavaya AY, Toll AE, Levvey BJ, Meiser B, Stehlik J (2018) The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: twenty-first pediatric heart transplantation report-2018; Focus theme: Multiorgan Transplantation. J Heart Lung Transpl 37:1184–1195 [DOI] [PubMed] [Google Scholar]
- 2.McAdams-Demarco MA, Grams ME, Hall EC, Coresh J, Segev DL (2012) Early hospital readmission after kidney transplantation: patient and center-level associations. Am J Transpl 12:3283–3288 [DOI] [PubMed] [Google Scholar]
- 3.Pereira AA, Bhattacharya R, Carithers R, Reyes J, Perkins J (2012) Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transpl 18:1037–1045 [DOI] [PubMed] [Google Scholar]
- 4.Donovan MP, Drusin RE, Edwards NM, Lietz K (2002) Analysis of trends in hospital readmissions and postoperative complications in heart transplant recipients: single center study. Transpl Proc 34:1853–1854 [DOI] [PubMed] [Google Scholar]
- 5.Boubaker K, Harzallah A, Ounissi M, Becha M, Guergueh T, Hedri H, Kaaroud H, Abderrahim E, Ben Abdellah T, Kheder A (2011) Rehospitalization after kidney transplantation during the first year: length, causes and relationship with long-term patient and graft survival. Transpl Proc 43:1742–1746 [DOI] [PubMed] [Google Scholar]
- 6.Jalowiec A, Grady KL, White-Williams C (2008) Predictors of rehospitalization time during the first year after heart transplant. Heart Lung 37:344–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dharnidharka VR, Stablein DM, Harmon WE (2004) Post-transplant infections now exceed acute rejection as cause for hospitalization: a report of the NAPRTCS1. Am J Transpl 4:384–389 [DOI] [PubMed] [Google Scholar]
- 8.Tsao CI, Chou NK, Chi NH, Yu HY, Chen YS, Wang CH, Ko WJ, Chen SC, Wang SS (2010) Unplanned readmission within 1 year after heart transplantation in Taiwan. Transpl Proc 42:946–947 [DOI] [PubMed] [Google Scholar]
- 9.Hollander SA, McElhinney DB, Almond CS, McDonald N, Chen S, Kaufman BD, Bernstein D, Rosenthal DN (2017) Rehospitalization after pediatric heart transplantation: incidence, indications, and outcomes. Pediatr Transpl 21:e12857. [DOI] [PubMed] [Google Scholar]
- 10.Mahle WT, Mason KL, Dipchand AI, Richmond M, Feingold B, Canter CE, Hsu DT, Singh TP, Shaddy RE, Armstrong BD, Zeevi A, Ikle DN, Diop H, Odim J, Webber SA (2019) Hospital readmission following pediatric heart transplantation. Pediatr Transpl. 10.1111/petr.13561:e13561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Godown J, Thurm C, Dodd DA, Soslow JH, Feingold B, Smith AH, Mettler BA, Thompson B, Hall M (2017) A unique linkage of administrative and clinical registry databases to expand analytic possibilities in pediatric heart transplantation research. Am Heart J 194:9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Healthcare Cost and Utilization Project (H-CUP) Clinical classification software. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed 26 June 2019
- 13.Dharnidharka VR, Stablein DM, Harmon WE (2004) Post-transplant infections now exceed acute rejection as cause for hospitalization: a report of the NAPRTCS. Am J Transpl 4:384–389 [DOI] [PubMed] [Google Scholar]
- 14.Menachem JN, Lindenfeld J, Schlendorf K, Shah AS, Bichell DP, Book W, Brinkley DM, Danter M, Frischhertz B, Keebler M, Kogon B, Mettler B, Rossano J, Sacks SB, Young T, Wigger M, Zalawadiya S (2018) Center volume and post-transplant survival among adults with congenital heart disease. J Heart Lung Transpl 37:1351–1360 [DOI] [PubMed] [Google Scholar]
- 15.Rana A, Fraser CD, Scully BB, Heinle JS, McKenzie ED, Dreyer WJ, Kueht M, Liu H, Brewer ED, Rosengart TK, O’Mahony CA, Goss JA (2017) Inferior outcomes on the waiting list in low-volume pediatric heart transplant centers. Am J Transpl 17:1515–1524 [DOI] [PubMed] [Google Scholar]
- 16.Kogon BE, Oster ME, Wallace A, Chiswell K, Hill KD, Cox ML, Jacobs JP, Pasquali S, Karamlou T, Jacobs ML (2019) Readmission after pediatric cardiothoracic surgery: an analysis of the Society of Thoracic Surgeons Database. Ann Thorac Surg 107:1816–1823 [DOI] [PubMed] [Google Scholar]
- 17.Magnetta DA, Godown J, West S, Zinn M, Rose-Felker K, Miller S, Feingold B (2019) Impact of the 2016 revision of US pediatric heart allocation policy on waitlist characteristics and outcomes. Am J Transpl. 10.1111/ajt.15567 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


