Abstract
BACKGROUND
The first case of pneumonia subsequently attributed to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) occurred in Wuhan, Hubei Province on December 8, 2019. The symptoms included fever, coughing, and breathing difficulties. A few patients with this infection may only have atypical symptoms, which could lead to a misdiagnosis and subsequently further facilitate the spread of the virus.
CASE SUMMARY
A 74-year-old female patient complained of severe diarrhea. She did not have fever, coughing, or breathing difficulties. A physical examination revealed no obvious positive signs. The patient had been hypertensive for more than 10 years. Her blood pressure was well controlled. On January 9, 2020, the patient’s son visited a colleague who was later confirmed positive for SARS-CoV-2 and his first close contact with our patient was on January 17. The patient was first diagnosed with gastrointestinal dysfunction. However, considering her indirect contact with a SARS-CoV-2-infected individual, we suggested that an atypical pneumonia virus infection should be ruled out. A computed tomography scan was performed on January 26, and showed ground-glass nodules scattered along the two lungs, suggestive of viral pneumonia. Given the clinical characteristics, epidemiological history, and examination, the patient was diagnosed with coronavirus disease-2019 (COVID-19).
CONCLUSION
Our patient had atypical symptoms of COVID-19. Careful acquisition of an epidemiological history is necessary to make a correct diagnosis and strategize a treatment plan.
Keywords: SARS-CoV-2, COVID-19, Pneumonia, Ground-glass opacity, Atypical symptoms, Diarrhea
Core tip: Coronavirus disease-2019 (COVID-19) symptoms include fever, coughing, and breathing difficulties. However some patients may only have atypical symptoms, which can lead to a misdiagnosis and further facilitate the spread of the virus. We here report a case of a 74-year-old patient with atypical symptoms, who was later diagnosed with COVID-19.
INTRODUCTION
The first case of coronavirus disease 2019 (COVID-19) was reported in Wuhan, Hubei Province on December 8, 2019. The symptoms included fever, coughing, and breathing difficulties[1-3]. Subsequently, more cases emerged, clustering from the Huanan Seafood Market in Wuhan[4]. On January 2, 2020, the first 41 cases of COVID-19 were confirmed. The Wuhan Institute of Virology collected severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) samples, and on January 2, 2020, its genome was successfully sequenced. The virus strain was then successfully isolated on January 5, 2020. However, the origin of coronaviruses remains unclear, although many reports in the literature suggest that they are likely to be from Rhinolophus sinicus[5]. Coronaviruses are a family of RNA viruses that have been previously identified as having six subtypes, with SARS-CoV-2 now thought to be the seventh. Four of the six subtypes are less pathogenic and usually result in mild catarrhal presentation after infection. Two previously identified viral subtypes, known as the viruses causing Severe Acute Respiratory Syndrome (SARS) and Middle East Respiratory Syndrome (MERS)[6-8]. On January 12, the World Health Organization named the virus discovered in Wuhan “Novel Coronavirus 2019 (2019-nCoV),” which is able to cause an acute respiratory disease[9-11]. Subsequently the virus was named SARS-CoV-2 and the disease COVID-19. On January 21, China’s National Health Commission (NHC) issued a notice that the novel coronavirus pneumonia virus was included in the Class B infectious diseases, but the prevention and control measures were adopted for Class A infectious diseases. Understanding the diagnostic criteria for SARS-CoV-2 is particularly important, as it can lead to an appropriate clinical diagnosis and treatment. The fourth version of the COVID-19 diagnostic criteria issued by the NHC are as follows: (1) Two weeks prior to the onset of the disease, the patient had travelled to Wuhan City, has a history of residence in Wuhan, has been exposed to patients with respiratory symptoms in Wuhan, or has been near a disease cluster; and (2) Clinical manifestations: (a) Fever; (b) Having imaging features of pneumonia; and (c) The total number of white blood cells in the early stages of the disease is normal or decreasing, or the number of lymphocytes has decreased. The disease can be considered ascertained if the patient has one of the epidemiological features and shows two clinical manifestations. Here, we report a patient diagnosed with SARS-CoV-2 infection who had atypical symptoms of diarrhea and did not have any respiratory symptoms.
CASE PRESENTATION
Chief complaints
A 74-year-old woman presented with severe diarrhea for 3 d.
History of present illness
The patient was visiting Shanghai from Wuhan. She presented to the Outpatient Department of Shanghai East Hospital on January 26, 2020 and complained of three days of severe diarrhea, with watery stools passed five to six times per day and sometimes blood-stained. The cause of these symptoms was unknown. The diarrhea was accompanied by anorexia and fatigue. The patient had taken eight pills of Huo Xiang Zheng Qi Wan, a natural herbal supplement that helps restore energy, three times a day, but without any symptomatic improvement. She denied having had any unhygienic food, seafood, or visiting the seafood market in Wuhan. The patient had no fever or cough, no sore throat, no chest tightness, and no shortness of breath.
Epidemiological history
On January 9, the patient’s son visited a colleague who lived in downtown Wuhan and who was reported to have not visited the Huanan Seafood Market within at least 2 wk. The son’s colleague was diagnosed with severe pneumonia, which was later confirmed to be COVID-19 and was put on a ventilator. The patient’s son had not taken any preventative measures on January 9 while meeting with his colleague. The patient travelled with her son, daughter, and granddaughter from Wuhan to Shanghai by train on January 23 after hearing about a possible Wuhan lockdown. Her son showed symptoms of anorexia and fatigue on January 21, and diarrhea with bloody stools on January 23, which lasted for several consecutive days and improved after taking oral moxifloxacin for four days. The patient’s husband developed fever on January 27 and was diagnosed with SARS-CoV-2 infection on January 30 (Table 1). The patient’s daughter and granddaughter remained asymptomatic.
Table 1.
Timeline of symptoms
|
1 |
2 |
3 |
4 |
5 |
6 |
|
| The colleague of the patient’s son | The patient’s son | The patient’s | The patient’s husband | Daughter | Granddaughter | |
| January 9, 2020 | Fever | Contact | ||||
| January 17, 2020 | Contact | Contact | ||||
| January 21, 2020 | Anorexia | |||||
| January 22, 2020 | Nacho | |||||
| January 23, 2020 | Diarrhea | Contact | Contact | |||
| January 24, 2020 | Moxifloxacin | Diarrhea | ||||
| January 25, 2020 | Moxifloxacin | |||||
| January 26, 2020 | Moxifloxacin | |||||
| January 27, 2020 | Died | Moxifloxacin | Confirmed diagnosis | Fever | ||
| January 28, 2020 | Improved | |||||
| January 30, 2020 | Improved | Confirmed diagnosis | ||||
| January 31, 2020 | No | No |
History of past illness
The patient had been hypertensive for more than 10 years. Her blood pressure was well controlled at 120-130/80-90 mmHg (15.99-17.33/10.66-11.99 kPa) with oral amlodipine 5 mg/d. The patient had no history of chronic digestive diseases, or other systemic diseases.
Personal and family history
The medical history of the patient was unremarkable.
Physical examination upon admission
Blood pressure was 153/94 mmHg, respiratory rate 24/min, heart rate 93/min, temperature 36.7 °C, and oxygen saturation was 99%. The patient was conscious and had a clear mind. She was low in spirit but had smooth breathing, no features of anemia, regular heart rhythm without any obvious murmur, no obvious moist crackles or wheezing sounds during auscultation of both lungs, and a soft abdomen. The patient felt pain when pressure was applied on the upper and middle abdomen although no rebound tenderness and no obvious lumps were detected.
Laboratory examinations
Routine blood test results were as follows: White blood cells, 3.50 × 109/L; neutrophils: 58.5%; lymphocytes, 33.9%; total number of lymphocytes, 1.19 × 109/L; fast C-reactive protein, 34.18 mg/L; serum amyloid proteins, 45.96 mg/L; potassium, 3.6 mmol/L; sodium, 136 mmol/L; chlorine, 97.0 mmol/L; creatinine, 43 µmol/L; urea, 3.1 m/L; total protein, 77 g/L; albumin, 44 g/L; alanine aminotransferase, 48 U/L (reference value 9-52 U/L); aspartate aminotransferase, 44 U/L↑(reference value 14-36 U/L). Blood tests for rapid detection of influenza A, influenza B, respiratory syncytial virus, mycoplasma pneumonia and adenovirus were all negative.
Clinical diagnosis
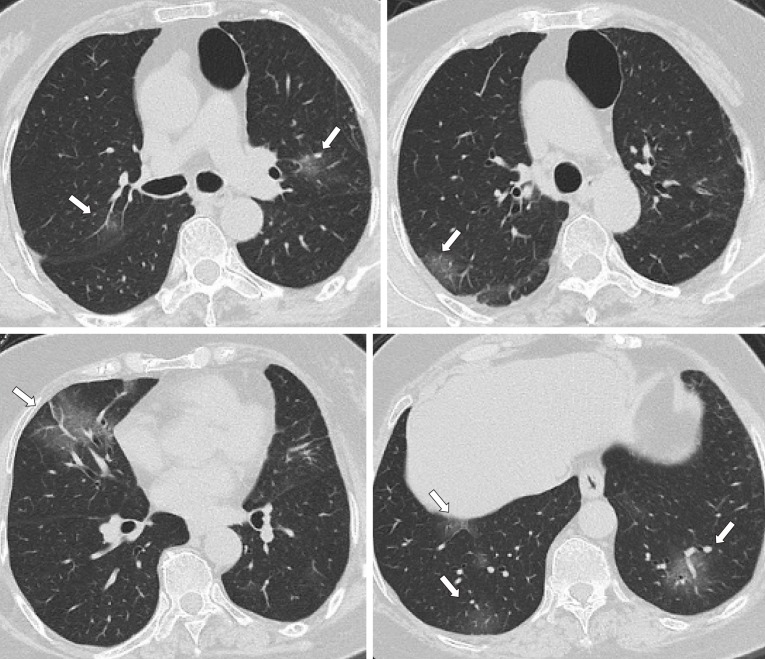
The patient was first diagnosed with gastrointestinal dysfunction, which is commonly seen in the Emergency Department and may be due to a cold, long-distance travels, an irregular diet, change in eating habits. However, considering her close proximity to the epidemic area, atypical pneumonia virus infection had to be ruled out. A computed tomography (CT) scan was performed on January 26, and showed small ground-glass nodules scattered along the two lungs, suggesting viral pneumonia (Figures 1 and 2). Given the clinical characteristics, epidemiological history, and examination, the patient was hospitalized with the diagnosis of suspected SARS-CoV-2 infection.
Figure 1.
Ground-glass nodules are randomly distributed in the upper and lower lobes of the two lungs and the pleural membrane. There is a clear boundary between the nodules, which are scattered with balanced density. The overlapping blood vessels and the path and morphology of bronchi did not show significant changes.
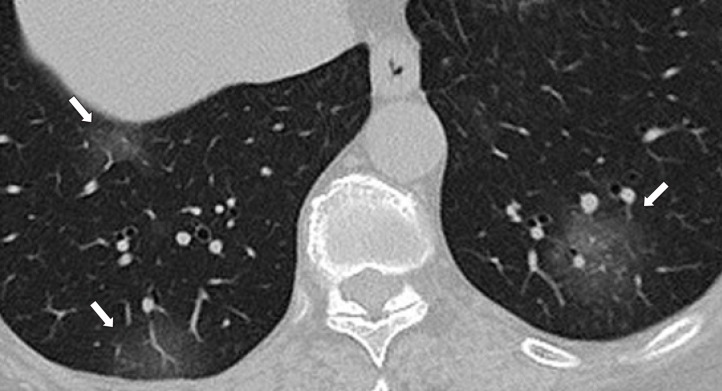
Figure 2.
Magnified image of typical ground-glass computed tomography characteristics. Ground-glass nodules are randomly distributed in the upper and lower lobes of the two lungs and the pleural membrane. There is a clear boundary between the nodules, which are scattered with balanced density. Overlapping blood vessels and the path and morphology of bronchi did not show significant changes. No swollen lymph nodes were observed in the mediastinal septum and no fluid was found in the chest.
FINAL DIAGNOSIS
On January 27, nucleic acid testing by the Centers for Disease Control and Prevention (CDC) gave positive results. Thus, the diagnosis of SARS-CoV-2 infection was confirmed. Then, in accordance with the CDC’s advice, the patient was transferred to the Shanghai Public Health Center for further comprehensive treatment.
TREATMENT
The patient was given 0.4 g QD moxifloxacin i.v. and 0.2 g TID oral Arbidol during in-hospital treatment. She was also treated with lopinavir/ritonavir (200/50 mg) (Kaletra) according to the fourth version of the NHC treatment plan.
OUTCOME AND FOLLOW-UP
After eight days of treatment, the patient's symptoms improved significantly, and she recovered with negative nucleic acid test. By the time of this paper submission, she was waiting to be discharged from hospital.
DISCUSSION
SARS-CoV-2-infected patients rarely show intestinal symptoms, such as diarrhea, while lacking respiratory signs/symptoms, whereas about 20%-25% of patients infected with MERS-CoV or SARS-CoV have diarrhea. According to current reports, COVID-19 has different clinical manifestations, such as fever, cough, fatigue, and breathing difficulties. A small proportion of patients have sore muscles, headache and a sore throat. In rare cases, patients have no typical symptoms and can only be confirmed by nucleic acid testing and/or a CT scan. Therefore, clinicians should be aware of the atypical characteristics of SARS-CoV-2 infection, especially in patients with epidemic contact history. By February 7, the number of confirmed cases had surged to more than 33000 with a further 27657 awaiting confirmation. The rate of both newly confirmed and suspected cases has been declining. No drug has been definitively shown to be effective for the treatment of this virus and thus only a small number of patients have been cured and discharged. The local and central government of China have implemented strict measures in order to curb the outbreak. However, it is an enormous challenge to trace all the people who might have been in contact with the virus after hundreds of thousands of cases have been confirmed or remained to be confirmed. It may be that the virus can spread not only via respiratory droplets, but also through fecal-oral transmission, contact transmission, and aerosol transmission. Asymptomatic patients seem to be able to also spread the virus via the above-mentioned routes. Patients presenting with atypical symptoms can be misdiagnosed, causing further spread of the virus. Current medical care includes inhaling nebulized interferon (five million BID) and Lopinavir/Ritonavir (200/50 mg) (Kaletra), even though there is no proof of their effectiveness. However, there is a report of a 35-year-old man that returned to the United States after visiting his family in Wuhan and was treated with Remdesivir (Gilead), a nucleotide analogue that inhibits the RNA-dependent RNA polymerase (RdRp). After the treatment, the patient showed significant improvement[12,13]. This drug was previously used to treat Ebola, which also has an RdRp activity. Therefore, this drug may also inhibit SARS-CoV-2[13,14]. However, the drug is still under a clinical trial, and its true effects need to be verified. Doctors have also verified the presence of SARS-CoV-2 (positive RT-PCR results) in stool samples of patients with diarrhea, which confirms the possibility of fecal-oral transmission.
CONCLUSION
COVID-19 symptoms include fever, cough, dyspnea, and atypical manifestations such as diarrhea. Therefore, detailed medical history taking, careful physical examination, and critical clinical evaluation will enable a correct diagnosis.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report and accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Peer-review started: February 17, 2020
First decision: March 5, 2020
Article in press: March 27, 2020
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aydin M, Kenzaka T, Tzamaloukas AHH, Vento S S-Editor: Zhang L L-Editor: Med-E Ma JY E-Editor: Wu YXJ
Contributor Information
Rui-Lin Li, Department of Cardiology, Shanghai East Hospital (East Hospital affiliated to Tongji University), Tongji University, Shanghai 200123, China.
Shu-Guang Chu, Department of Medical Imaging, Shanghai East Hospital (East Hospital affiliated to Tongji University), Tongji University, Shanghai 200123, China.
Yu Luo, Department of Cardiology, Shanghai East Hospital (East Hospital affiliated to Tongji University), Tongji University, Shanghai 200123, China.
Zhen-Hao Huang, Department of Cardiology, Shanghai East Hospital (East Hospital affiliated to Tongji University), Tongji University, Shanghai 200123, China.
Ying Hao, Department of Cardiology, Shanghai East Hospital (East Hospital affiliated to Tongji University), Tongji University, Shanghai 200123, China.
Cheng-Hui Fan, Department of Cardiology, Shanghai East Hospital (East Hospital affiliated to Tongji University), Tongji University, Shanghai 200123, China. fchman@163.com.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wuhan Municipal Health Commission. Report of novel coronavirus-infected pneumonia in Wuhan City, January 20, 2020. Available from: http://wjw.wuhan.gov.cn/front/web/showDetail/ 2020012009077.
- 3.Tan WJ, Zhao X, Ma XJ, Wang WL, Niu PH, Xu WB, Gao GF, Wu GZ. Notes from the Field: A Novel Coronavirus Genome Identified in a Cluster of Pneumonia Cases − Wuhan, China 2019−2020. China CDC Weekly. 2020;2:61–62. [PMC free article] [PubMed] [Google Scholar]
- 4.Perlman S. Another Decade, Another Coronavirus. N Engl J Med. 2020;382:760–762. doi: 10.1056/NEJMe2001126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhong NS, Zheng BJ, Li YM, Poon, Xie ZH, Chan KH, Li PH, Tan SY, Chang Q, Xie JP, Liu XQ, Xu J, Li DX, Yuen KY, Peiris, Guan Y. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People's Republic of China, in February, 2003. Lancet. 2003;362:1353–1358. doi: 10.1016/S0140-6736(03)14630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong G, Liu W, Liu Y, Zhou B, Bi Y, Gao GF. MERS, SARS, and Ebola: The Role of Super-Spreaders in Infectious Disease. Cell Host Microbe. 2015;18:398–401. doi: 10.1016/j.chom.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drosten C, Günther S, Preiser W, van der Werf S, Brodt HR, Becker S, Rabenau H, Panning M, Kolesnikova L, Fouchier RA, Berger A, Burguière AM, Cinatl J, Eickmann M, Escriou N, Grywna K, Kramme S, Manuguerra JC, Müller S, Rickerts V, Stürmer M, Vieth S, Klenk HD, Osterhaus AD, Schmitz H, Doerr HW. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348:1967–1976. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 9.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, Xing F, Liu J, Yip CC, Poon RW, Tsoi HW, Lo SK, Chan KH, Poon VK, Chan WM, Ip JD, Cai JP, Cheng VC, Chen H, Hui CK, Yuen KY. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A Novel Coronavirus Emerging in China - Key Questions for Impact Assessment. N Engl J Med. 2020;382:692–694. doi: 10.1056/NEJMp2000929. [DOI] [PubMed] [Google Scholar]
- 11.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, Spitters C, Ericson K, Wilkerson S, Tural A, Diaz G, Cohn A, Fox L, Patel A, Gerber SI, Kim L, Tong S, Lu X, Lindstrom S, Pallansch MA, Weldon WC, Biggs HM, Uyeki TM, Pillai SK Washington State 2019-nCoV Case Investigation Team. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Cui X, Xiao J, Meng T, Zhou W, Liu J, Xiu H. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. bioRxiv. 2020 [Google Scholar]