Abstract
Introduction
The risk of osteonecrosis of the jaw is greater for patients receiving intravenous bisphosphonates for cancer than for patients receiving oral bisphosphonates for osteoporosis or Paget’s disease.
Materials and Methods
This article provides a review of the treatment of Bisphosphonate induced osteonecrosis of jaws.
Conclusion
Bisphonates associated jaw necrosis and its relation to dentisitry and maxillofacial surgery has become common now a days. Proper diagnosis and treatment may help the patients health getting worsen.
Keywords: Bisphosphonate-related osteonecrosis, BIONJ, Bisphosphonates in maxillofacial surgery, Bisphosphonate-induced osteonecrosis
Introduction
Bisphosphonate-induced osteonecrosis of the jaws (BIONJ) refers to a condition characterized by exposure of bone in mandible or maxilla persisting for more than 8 weeks in patient who has taken or is currently taking bisphosphonate and who has no radiation therapy to the jaws. Bisphosphonate-induced osteonecrosis of the jaws (BIONJ) was first described by Marx and Stern in 2002 [1–4].
Bisphosphonates are used in the treatment of metastatic bone diseases, osteoporosis, hypercalcemia of malignancy and Paget’s disease [5]. Various bisphosphonates used for this purpose are alendronate, pamidronate, zoledronate, ibandronate, etc. Although bisphosphonates have been used clinically for more than three decades, there have been no documented long-term complications of their effects on the jaws until recently, where there is now growing evidence of the influence of bisphosphonates on osteonecrosis of the jaws [1, 5].
Terminology Evolution
Bisphosphonate-related osteonecrosis of the jaws (BRONJ) was the term given by American Association of Oral and Maxillofacial Surgeons [6]. Bisphosphonate-associated osteonecrosis of the jaws (BAONJ) was the term coined by American Dental Association [7]. Both terms are inaccurate because they do not explain the underlying mechanism of the condition.
Osteochemonecrosis is also stated in the literature [8]. Avascular necrosis has also been used by few researchers. A more recent term in this list is bisphosphonate-induced osteonecrosis of the jaws (BIONJ) which was widely accepted till 2014 [1].
AAOMS in 2014 finally gave a terminology which is “medication-related osteonecrosis of the jaw” (MRONJ). This condition is also caused by drugs such as RANK ligand inhibitor (denosumab) which is antiresorptive and other antiangiogenic medications [9].
Mechanism of Action
Bisphosphonates are powerful inhibitors of osteoclastic activity. They are analogues of inorganic pyrophosphates with low intestinal absorption, are excreted through the kidneys without metabolic alteration and have a high affinity for hydroxyapatite crystals [10, 11]. Because they are incorporated into the skeleton without being degraded, they are remarkably persistent drugs; the estimated half-life of alendronate is up to 12 years [12].
The non-aminobisphosphonates are metabolized by osteoclasts to inactive non-hydrolyzable adenosine triphosphate analogues that are directly cytotoxic to the cell and induce apoptosis [10, 11]. The newer aminobisphosphonates have two actions [13]: induction of another adenosine triphosphate analogue that induces apoptosis and inhibition of farnesyl diphosphate synthase, which is part of the mevalonate pathway of cholesterol synthesis. Such inhibition results in dysregulation of intracellular transport, cytoskeletal organization and cell proliferation, leading to inhibition of osteoclast function (Fig. 1). In addition, aminobisphosphonates reduce recruitment of osteoclasts and induce osteoblasts to produce an osteoclast-inhibiting factor [14, 15].
Fig. 1.
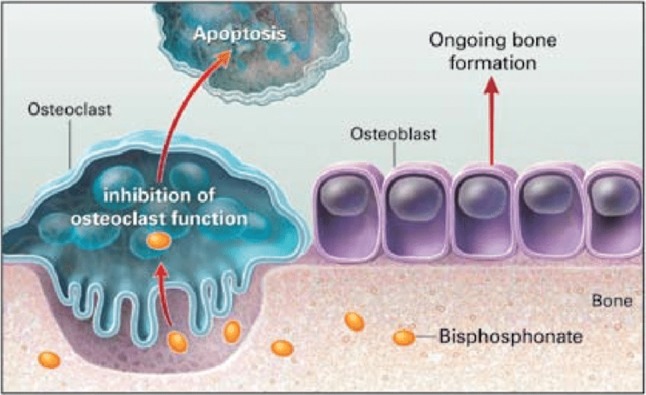
Mechanism of action of bisphosphonates
Why Only in the Jaws?
Dixon et al. studied bone remodeling at various sites and found that alveolar crest remodels at ten times the rate of tibia and five times the rate of mandible at inferior border. Hence, alveolar bone of the jaws has greater uptake of bisphosphonates and drug accumulates in higher concentration. This study also demonstrated that alveolar bone depends more on osteoclastic remodeling and renewal than any other bone in adult skeleton [16].
During normal occlusion, compression forces get concentrated at root apex and crest of furcation, while tension forces are directed on lamina dura throughout the rest of periodontal ligament fibers. So lamina dura remodels in response to these forces. However, if patient has absorbed and accumulated sufficient quantity of bisphosphonates, lamina dura cannot remodel and instead becomes hypermineralized.
If more bisphosphonate accumulates as the demand of remodeling continues or trauma such as tooth extraction occurs, the alveolar bone can no longer respond with new bone from osteoclastic bone resorption followed by new bone formation and it becomes necrotic. The overlying bone is subsequently deprived of its blood supply from underlying bone and breaks down, leading to clinically exposed bone [18] (Fig. 2).
Fig. 2.

Clinical picture of BIONJ.
Image Credits: Mayo Clinic
Revised Staging for BIONJ
Stage 1: One quadrant or less of exposed bone without osteolysis beyond the alveolus or sinus involvement
Stage 2: Two quadrant or more of exposed bone without evidence of osteolysis beyond the alveolus or sinus involvement
Stage 3: Any presentation with osteolysis beyond alveolus or pathologic fracture or cutaneous fistula or sinus involvement [19].
Initiation of BIONJ
Robert Marx studied osteonecrosis on the patient with intravenous bisphosphonates and observed that 25% of BIONJ developed spontaneously and 75% of cases were precipitated by some type of invasive dental procedure performed to resolve dental comorbidity. The most common factor in those cases was surgical dental trauma or inflammatory condition of periodontium [18].
Incidence
BIONJ is most commonly found in mandible with total incidence rate of 68% and less frequent in maxilla, around 28%. Both the jaws are involved 4% of the times [18].
Prevention of BIONJ
As 75% of BIONJ cases are triggered by surgical trauma, uncontrolled occlusal trauma or active dental inflammatory disease, the most effective strategy to prevent BIONJ would be to avoid the need for any invasive dental surgery after bisphosphonate therapy has been initiated [17]. Medical oncologists are well advised to refer all the patients in whom bisphosphonate therapy is indicated to an experienced dentist or Oral and Maxillofacial Surgeon for consultation.
Bisphosphonate therapy should be postponed for 2–3 months if feasible providing adequate time for dental team to remove all concerning initiators of osteonecrosis of jaws and achieve optimum dental health. All the non-restorable and periodontally unsalvageable teeth should be removed first to give maximum time for wound healing. Next, priority should be given to caries control, tooth restoration, root canal treatment and periodontal care including periodontal surgery. Subsequently prosthetic procedures of fixed or removable dentures can be followed. These patients are not candidates of dental implants because it depends on bone remodeling for maintenance of osseointegration. Thus, there are higher chances of osteonecrosis taking place.
Prophylactic antibiotic coverage should be considered for invasive dental procedure because cancer patients carry high risk of infection. Penicillin can be given during the procedure, and penicillin VK 500 mg, four times daily, can be followed for 5 days. For patients allergic to penicillin, azithromycin 500 mg should be given 1–2 h prior to procedure, followed by once daily for 5 days [18, 20–23].
Management of BIONJ
Proper medical history should be elicited which includes: drug name, indication, route, dose, frequency of administration and any concomitant medication. In dental history, it is recommended to check for exposed bone (especially in posterior lingual cortex), mobility of teeth, constant deep pain, intermittent swelling and gingival recession. Any inflammatory of tooth or periodontium has to be noted.
Robert Marx has stressed in his paper that this type of osteonecrosis is a dead bone due to toxic effects of bisphosphonates. So it is likely to be permanent and any attempts of bone debridement short of resection have been counterproductive and produced additional exposed bone, worsening of symptoms and increased risk of pathologic fracture [18]. The exposed bone itself cannot be painful as it is deinnervated, unless secondarily infected. Therefore, prevention and/or control of secondary infection and pain and acceptance of the presence of some exposed bone are the mainstays of therapy.
This approach is reported to be successful related to normal function in a pain-free state in 87% of patients [20].
The article “Management of Medication-Related Osteonecrosis of the Jaw” published in Oral Maxillofacial Surgery Clinics of North America 2015 by Bradford and Felice states various treatment approaches to patients with MRONJ once the diagnosis has been made.
Medical Management [17]
-
Antimicrobials.
Topical antimicrobials.
Oral antimicrobials.
Intravenous antimicrobials.
Pentoxifylline and vitamin E therapy.
Teriparatide.
Hyperbaric oxygen therapy.
Topical Antimicrobials
Chlorhexidine gluconate 0.12% is a topical bactericidal and bacteriostatic agent that has been shown to be effective in the treatment of patients with MRONJ.
There is evidence that the oral flora, and more specifically biofilms, contributes to the disease process which is disrupted by the use of topical antimicrobials.
Chlorhexidine is recommended for management of stage 1 disease as a singular therapy.
For more advanced stages, it can be advised in addition to medical and surgical therapies.
Oral Antimicrobials
Antimicrobials are a mainstay in the management of MRONJ.
Antimicrobial therapy is based on clinical observation and scientific literature, suggesting that pathogenic bacteria may contribute to MRONJ.
Most of the infections are polymicrobial.
Common colonizers of MRONJ lesions are Actinobacteria, Fusobacteria and Bacteroides.
These organisms are susceptible to penicillin; therefore, penicillin remains the first antibiotic choice.
Alternatives to penicillin are clindamycin, fluoroquinolones and/or metronidazole.
Prescribe a 2-week course for patients with persistent stage 1 disease and up to a 4–6-week course for more severe cases.
Intravenous Antimicrobials
Intravenous antimicrobials may be of benefit in patients with pathogenic organisms resistant to oral agents.
IV antimicrobials may provide greater tissue penetration.
However, there have been no satisfactory trials demonstrating greater efficacy of intravenous agents compared with oral medications.
IV should be employed as last chance when all the oral agents have been used.
Long-term (6-week) intravenous antimicrobials should be administered.
Pentoxifylline and Vitamin E
The combination of pentoxifylline and vitamin E has been used successfully in the treatment of jaw osteoradionecrosis and MRONJ.
The specific mechanism of action in MRONJ remains unclear.
Pentoxifylline (Trental), a xanthine derivative with an excellent safety profile, is used primarily for the treatment of vascular diseases.
Vitamin E decreases tissue inflammation and fibrosis and is a scavenger of free radicals capable of cellular injury.
Numerous reports supporting the role of both inflammation and decreased vascularity as contributors to MRONJ make the use of this relatively well-tolerated drug combination a rational choice.
The recommended dose:
Pentoxifylline 400 mg sustained release twice daily
1000 IU vitamin E daily for 36 months.
These medications to be maintained perioperatively in patients who require the surgical treatment of MRONJ.
Teriparatide
Teriparatide (Forteo) is a subcutaneously administered drug used primarily in the treatment of osteoporosis.
This is the only available drug that can stimulate new bone formation.
The drug is composed of 34 amino acids of the N-terminal chain of parathyroid hormone and retains the anabolic effects of endogenous parathyroid hormone, including promotion of bone remodeling.
Teriparatide is thought to stimulate effectively osteoblast function and proliferation, increase osseous cell signaling and activate osteoclasts.
Recommended dosage: 20 mcg SC daily for up to 2 years.
Hyperbaric Oxygen Therapy
HBO therapy has been used for management of osteoradionecrosis of the jaw for many years and more recently has been applied to the treatment of MRONJ.
HBO provides greater oxygen to tissues with impaired vascularization.
Additionally, HBO reverses impaired leukocyte function, thus resulting in improved wound healing and bone turnover.
The clinical utility of HBO for management of MRONJ remains unclear, and for this reason, it is not commonly advised for the patients with MRONJ.
Surgical Management
Patients with stage 0 and stage 1 disease generally do not warrant surgical intervention, but benefit from medical management,
A wide spectrum of disease is often seen with stage 2 MRONJ, ranging from focal minimally symptomatic exposed bone to severely painful widespread bone necrosis.
Maxilla/mandible resection is advised in the cases of stage III MRONJ.
It is thus difficult to recommend a single surgical treatment approach in these patients.
Debridement and marginal and segmental resection are terms commonly seen in the literature describing the surgical treatment of MRONJ.
Debridement and marginal resection both refer to removal of necrotic bone, primarily in the alveolus, with the goal of maintaining an intact inferior border of the mandible.
Segmental resection, on the other hand, refers to en bloc removal of involved bone, including the inferior border of the mandible, with a resulting continuity defect.
Intraoperative fluorescence-guided debridement has been suggested to assist in differentiating necrotic from viable bone.
Tetracycline is incorporated into sites of bone remodeling and thus will only be seen in viable bone.
The technique involves preoperative administration of doxycycline (100 mg twice a day for 10 days before surgery).
A fluorescent light source is applied to the affected region during debridement and areas of necrotic bone are seen to fluoresce as a pale bluish-white color whereas viable bone appears brightly fluorescent.
For the Surgical Management of MRONJ, the Following Principles Should Be Applied:
Appropriate preoperative imaging to assess the extent of disease.
Removal of all necrotic bone and any involved teeth to achieve disease-free bony margins.
Removal of any sharp bony edges and spicules.
Achievement of a layered tension-free primary wound closure whenever possible.
Culture-directed postoperative antibiotic therapy until mucosal healing is seen.
Restraint from wearing any oral prosthetic devices until complete mucosal healing is seen.
Treatment protocol advised by Marx [18, 20] depending on the stage of disease:
- Stage 0 (subclinical):
- Eliminate inflammatory pathologies.
- Withheld therapy for 2–3 months if possible.
- Remove unrestorable tooth.
- Perform procedures for restorations, root canal and periodontal care.
- Undertake procedures of fixed or removable partial dentures.
- Leave impacted tooth undisturbed unless they have oral communication.
- Prophylactic antibiotics for invasive dental procedures.
-
Stages 1 and 2:
Asymptomatic exposed bone can be maintained by 0.12% chlorhexidine rinse three times daily. If accompanied by pain due to infection, antibiotic regimen can be prescribed. There are three types of regimen given:
- Regimen A—penicillin VK 500 mg, four times a day can be ongoing.
- Regimen B—penicillin VK 500 mg, four times a day till pain and infection are controlled.
- Regimen C—levofloxacin 500 mg/azithromycin 500 mg once daily for the patients allergic to penicillin.
-
Stage 3:
Stage 3 osteonecrosis can be palliated with Regimen A, B or C to allow for function. Patients who do not respond to this or have painful pathologic fracture are the candidates for alveolar resection or continuity resection. Titanium plate reconstruction can be followed immediately or delayed depending on the absence or presence of infection. When significant areas of mucosa or skin have been necrosed, a soft tissue flap may also be required [18, 20].
Protocol for Tooth Extraction
Scoletta et al. gave a refined protocol for tooth extractions in intravenous bisphosphonate-treated patients. According to the protocol, antibiotics and 0.12% chlorhexidine were started 1 day prior to the surgical procedure. Local anesthetic was infiltrated at the time of procedure. All the extractions were performed without a vestibular split-thickness flap. Healing was stimulated by filling the extraction site with autologous plasma rich in growth factors (PRGF system). Local and systemic infection control was obtained with dental hygiene and antibiotic therapy. This protocol was successful in 202 extractions performed in 63 patients.
Conclusion
BIONJ can appear spontaneously, but more commonly it is associated with local trauma, predominantly dental extraction [18, 20, 22]. Currently, there is no way of predicting which individuals taking bisphosphonates are at greatest risk of developing BRONJ. Equally, there are no prognostic indicators predictive of outcomes. The only persistent finding is a correlation between duration of therapy and occurrence of BRONJ
Prevention is superior to treatment, and as such, the establishment of meticulous oral hygiene and preemptive surgical treatment prior to commencement of bisphosphonate therapy is recommended. During therapy, strict review and maintenance of oral hygiene practices should occur in order to prevent pathology necessitating surgical management. Patients treated with these drugs need to be aware of complications that can arise in the jaws, especially related to trauma. It should be stressed upon those taking bisphosphonates, especially the intravenous forms, the need to avoid invasive dental management [22].
The most conservative approach to controlling pain and infection is followed. Bone debridement can be tempting, but it is counterproductive and produces additional exposed bone and worsening of symptoms. So it is better avoided [18, 20].
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B, American Association of Oral and Maxillofacial Surgeons American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws—2009 update. J Oral Maxillofac Surg. 2009;67(5 Suppl):2–12. doi: 10.1016/j.joms.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Marx RE, Stern DS. Oral and maxillofacial pathology: a rationale for diagnosis and treatment. Chicago: Quintessence; 2002. [Google Scholar]
- 3.Marx RE. Reconstruction of defects caused by bisphosphonate-induced osteonecrosis of jaws. J Oral Maxillofac Surg. 2009;67:107–119. doi: 10.1016/j.joms.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 4.Marx RE, Sawatari Y, Fortin M, Broumand V. Biphosphonate induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention and treatment. J Oral Maxillofac Surg. 2005;63:1567–1575. doi: 10.1016/j.joms.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg TJ, Ruggiero SL. Osteonecrosis of the jaws associated with the use of bisphosphonates. J Oral Maxillofac Surg. 2003;61(Suppl 1):60. doi: 10.1016/S0278-2391(03)00566-4. [DOI] [PubMed] [Google Scholar]
- 6.Advisory Task Force on Bisphosphonate-Related Osteonecrosis of the Jaws, American Association of Oral and Maxillofacial Surgeons American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2007;65(3):369–376. doi: 10.1016/j.joms.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Edwards BJ, Hellstein JW, Jacobsen PL, Kaltman S, Mariotti A, Migliorati CA, American Dental Association Council on Scientific Affairs Expert Panel on Bisphosphonate-Associated Osteonecrosis of the Jaw Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139(12):1674–1677. doi: 10.14219/jada.archive.2008.0110. [DOI] [PubMed] [Google Scholar]
- 8.Fedele S, Kumar N, Davies R, Fiske J, Greening S, Porter S. Dental management of patients at risk of osteochemonecrosis of the jaws: a critical review. Oral Dis. 2009;15(8):527–537. doi: 10.1111/j.1601-0825.2009.01581.x. [DOI] [PubMed] [Google Scholar]
- 9.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O’Ryan F, American Association of Oral and Maxillofacial Surgeons American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw–2014 update. J Oral Maxillofac Surg. 2014;72(10):1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 10.Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev. 1998;19:80100. doi: 10.1210/edrv.19.1.0325. [DOI] [PubMed] [Google Scholar]
- 11.RussellRG CroucherPI, Rogers MJ. Bisphosphonates:pharmacology, mechanisms of action and clinical uses. Osteoporos Int. 1999;9(Suppl 2):S66–S80. doi: 10.1007/PL00004164. [DOI] [PubMed] [Google Scholar]
- 12.Lin JH, Russell G, Gertz B. Pharmacokinetics of alendronate: an overview. Int J Clin Pract Suppl. 1999;101:18–26. [PubMed] [Google Scholar]
- 13.Green JR. Bisphosphonates: preclinical review. Oncologist. 2004;9(Suppl 4):313. doi: 10.1634/theoncologist.9-90004-3. [DOI] [PubMed] [Google Scholar]
- 14.Hughes DE, MacDonald BR, Russell RG, Gowen M. Inhibition of osteoclast-like cell formation by bisphosphonates in long-term cultures of human bone marrow. J Clin Invest. 1989;83:1930–1935. doi: 10.1172/JCI114100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vitte C, Fleisch H, Guenther HL. Bisphosphonates induce osteoblasts to secrete an inhibitor of osteoclast-mediated resorption. Endocrinology. 1996;137:2324–2333. doi: 10.1210/endo.137.6.8641182. [DOI] [PubMed] [Google Scholar]
- 16.Bradford W, O’Ryan F. Management of medication-related osteonecrosis of the jaw. Oral Maxillofac Surg Clin N Am. 2015;27:517–525. doi: 10.1016/j.coms.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Hellstein JW. Oral and intravenous bisphosphonate-induced osteonecrosis of the jaws: history, etiology, prevention, and treatment. Spec Care Dent. 2012;32(1):33. doi: 10.1111/j.1754-4505.2011.00229.x. [DOI] [Google Scholar]
- 18.(2006) Oral and Intravenous Bisphosphonate-induced osteonecrosis of the jaws. Quintessence, Chicago, pp 64–72
- 19.Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63(11):1567–1575. doi: 10.1016/j.joms.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 20.Marx RE. Bisphosphonate-induced osteonecrosis of the jaws: a challenge, a responsibility, and an opportunity. Int J Periodontics Restor Dent. 2008;28(1):5–6. [PubMed] [Google Scholar]
- 21.Sook-Bin W, Hellstein WJ, Kalmar RJ. Systematic review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med. 2006;144:753–761. doi: 10.7326/0003-4819-144-10-200605160-00009. [DOI] [PubMed] [Google Scholar]
- 22.Marx RE, Cillo JE, Ulloa JJ. Oral bisphosphonate induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention and treatment. J Oral Maxillofac Surg. 2007;65:2397–2410. doi: 10.1016/j.joms.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 23.Scoletta M, Arata V, Arduino PG, Lerda E, Chiecchio A, Gallesio G, Scully C, Mozzati M. Tooth extractions in intravenous bisphosphonate-treated patients: a refined protocol. J Oral Maxillofac Surg. 2013;71(6):994–999. doi: 10.1016/j.joms.2013.01.006. [DOI] [PubMed] [Google Scholar]


