Abstract
Purpose
To evaluate the correlation between the position of inferior alveolar nerve canal and the angulation of impacted mandibular third molars using cone beam computed tomography (CBCT) in a hospital-based study in the state of Odisha, India.
Materials and Methodology
Three hundred cases of impacted third molars in 200 patients (154 males; 46 females) were included in the study, for whom an initial periapical or panoramic radiograph had revealed that the mandibular canal and the lower third molars were in close proximity. A CBCT scan of each patient was carried out to assess how the canal position influenced the class and position of impaction, angulation of impaction and bone contact.
Results
Class II position B impactions were found in 78.37% cases where the position of ID canal was approximate to the lingual plate and inferior to third molar (73.75%). The results were statistically significant (p = 0.00). 80% of the ID canals showed bone contact. Of these 73.75% ID canals showed lingual bone contact. Mesioangular impactions were most common in mandible and significantly associated with lingual and inferior positioning of the canal.
Conclusions
The study mostly exhibited patients having mesioangular class II position B third molar impactions of the mandible. The position of the canal has a significant influence on the type of impaction and the bone contact.
Keywords: Inferior alveolar nerve canal, Impactions, Third molars, CBCT
Introduction
One of the most common procedures in the Department of Oral and Maxillofacial Surgery is surgical extractions of unerupted or partially erupted third molars widely known as impacted third molars. A comparatively occasional but alarming complication of impacted mandibular third molar extractions is neurological damage, predominantly the inferior alveolar nerve (IAN). Studies have accounted for this incidence between 0.4 and 6% [1–4]. The likelihood of such accidents is higher when the proximity of the mandibular canal is close to the mandibular third molar [5]. Hence, preoperative radiographic evaluations in the form of periapical (IOPA) or panoramic radiographs (OPG) have been in practice for quite sometime.
Certain signs on the IOPA or OPG suggest the increased risk of IAN damage during the procedure. Although suggestive, the panoramic radiographs have their own limitations in estimating the exactness of the positional relationship of the structures due to being a two-dimensional technology. The overlapping images make it difficult at times proper assessment, especially buccolingually [6–8].
Over the past one or two decades the advancement of cone beam computed tomography (CBCT) has had an important role in clinical and radiological investigations in the field of oral and maxillofacial surgery. The CBCT has the advantage of providing axial, coronal and sagittal sections of the designated area, and additionally, it also depicts the three-dimensional structure of teeth and its surrounding areas [9, 10]. The aim of our study was to evaluate the correlation between the position of inferior alveolar nerve canal and the angulation of impacted mandibular third molars using cone beam computed tomography.
Materials and Methods
The present analytical study was retrospective in nature, which was conducted after obtaining necessary ethical clearance from the Ethical Committee of KIIT University, Bhubaneswar, Odisha, India. The sample consisted of 200 patients (154 males; 46 females) aged between 18 and 38 years, having impacted mandibular third molars and where an initial radiographic assessment demonstrated overlap/close proximity of the mandibular third molar and inferior alveolar nerve canal.
CBCT scans of 200 patients including images in all three planes were analyzed. The data were retrieved from patients reporting to the Department of Oral Medicine and Radiology, Kalinga Institute of Dental Sciences, KIIT University, Bhubaneswar, between January 2016 and September 2017. The images were acquired using Hyperion X9 digital imaging system (MyRay, Italy) with the following parameters: 70–75 kV, 8–10 mA and 11–12.3 s exposure time. The field of view (FOV) size was 11 mm × 8 mm, and the recorded 3D images were formatted to 300-μm image resolution. The recorded CBCT images were evaluated in a 21-inch LCD monitor (HP L1910, Hewlett-Packard Development Co., Palo Alto, CA, USA) with 1280 × 1024 pixels and processed using the NNT Imaging Software (v4.6), Windows edition (MyRay, Italy).
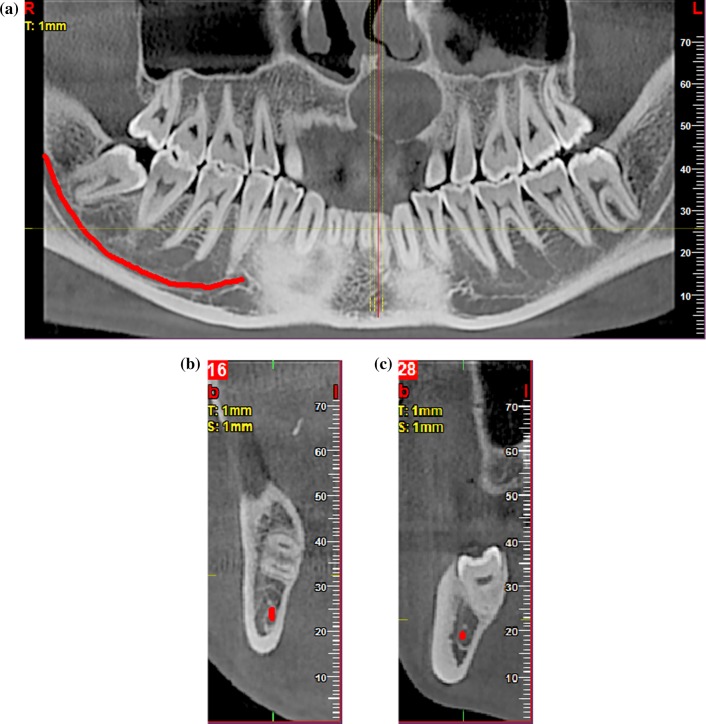
Using the cross-sectional view and adjusting the position in panoramic view the buccolingual position and outline of canal were noted (Fig. 1a, b, c).
Fig. 1.
a Red line indicates the inferior alveolar nerve canal on the panoramic view of CBCT. b Cross-sectional (axial) view shows the canal located lingual and inferior to the impacted tooth. c Cross-sectional view shows the location of canal lingual and inferior to the impacted tooth
All the scans were assessed by a team of one maxillofacial radiologist and one oral and maxillofacial surgeon of Kalinga Institute of Dental Sciences using standard exposure and processing protocols and were interpreted under ideal viewing conditions. The type of impaction of mandibular third molars was identified by the method adapted by Winter, 1926, and subsequently, it was categorized as vertical, horizontal, mesioangular or distoangular impactions. It was also categorized under Pell and Gregory classification in relation to the ramus of mandible (class I, II, III) and the position of third molars in relation to occlusal surface of second molar (A, B, C).
Statistical Analysis
All the recorded data were analyzed by SPSS software (version 20.0.0). Measurements of mandibular canal position, impaction type, angulation and position, and bone contact were sorted out according to their frequency and percentage. Pearson’s Chi-square test was applied to evaluate the correlation between type of impaction, nerve positioning, bone contact and angulation. Results with p value less than 0.05 were considered statistically significant.
Results
The relative position of the mandibular canal in relation to the impacted third molars has been classified under three categories, i.e., buccal and inferior, lingual and inferior, and middle and inferior (apex of roots). In our study, in all the cases, mandibular canal was found to be inferior to the root apex of mandibular third molar.
Table 1 demonstrates that the lingual and inferior position of the canal is associated significantly with class II position B (78.37%), followed by class I position B (77.14%) and class III position C (72.72%), while buccal and inferior relation can be seen maximum in class III position A (50%), and middle and inferior relation of the ID canal is maximum in class I position A (44.44%). The correlation between the mandibular canal and the position of impacted tooth was found statistically significant (p = 0.00).
Table 1.
Relationship of class and position of mandibular third molar impaction and position of mandibular canal
| Class and position of impaction | Position of ID canal | Total | ||
|---|---|---|---|---|
| Buccal + inferior | Lingual + inferior | Middle + inferior | ||
| I A | 3 (6.6%) | 22 (48.88%) | 20 (44.44%) | 45 (100%) |
| I B | 3 (4.28%) | 54 (77.14%) | 13 (18.57%) | 70 (100%) |
| I C | 11 (24.44%) | 29 (64.44%) | 5 (11.11%) | 45 (100%) |
| II A | 4 (13.33%) | 19 (63.33%) | 7 (23.33) | 30 (100%) |
| II B | 5 (6.75%) | 58 (78.37%) | 11 (14.86%) | 74 (100%) |
| II C | 2 (20%) | 5 (50%) | 3 (30%) | 10 (100%) |
| III A | 3 (50%) | 1 (16.66%) | 2 (33.33%) | 6 (100%) |
| III B | 1 (11.11%) | 6 (66.66%) | 2 (22.22%) | 9 (100%) |
| III C | 2 (18.18%) | 8 (72.72%) | 1 (9.09%) | 11 (100%) |
| Total number of cases | 34 (11.33%) | 202 (67.33%) | 64 (21.33%) | 300 (100%) |
Chi2 value = 45.6, p value = 0.00
Table 2 illustrates that the lingual and inferior positioning of the canal was significantly associated with the bone contact (73.75%), whereas 46.66% cases of lingual and inferior position of canal showed no contact which is statistically significant (p = 0.00).
Table 2.
Cortical bone contact and position of mandibular canal
| Bone contact | Position of ID canal | |||
|---|---|---|---|---|
| Buccal + inferior | Lingual + inferior | Middle + inferior | Total | |
| Contact | 22 (9.16%) | 177 (73.75%) | 41 (17.085%) | 240 (100%) |
| No contact | 19 (31.66%) | 28 (46.66%) | 13 (21.66%) | 60 (100%) |
| Total number of cases | 41 (13.66%) | 205 (68.33%) | 54 (18%) | 300 (100%) |
Chi2 value = 23.5, p value = 0.00
Table 3 explains the position of mandibular canal in relation to the angulation of mandibular third molar impaction, according to Winter’s classification. It was seen that mesioangular impaction was highest in number along with lingual and inferior positioning of the nerve (71.15%). Overall, the angulation of impaction can be significantly correlated with the canal position (p value = 0.00).
Table 3.
Relation between angulation of impactions and position of mandibular canal
| Angulation of impaction | Position of ID canal | Total | ||
|---|---|---|---|---|
| Buccal + inferior | Lingual + inferior | Middle + inferior | ||
| Distoangular | 10 (25%) | 16 (40%) | 14 (35%) | 40 (100%) |
| Horizontal | 7 (21.22%) | 15 (45.45%) | 11 (33.33%) | 33 (100%) |
| Mesioangular | 26 (15.75%) | 118 (71.15%) | 21 (12.72%) | 165 (100%) |
| Vertical | 12 (19.35%) | 30 (48.38%) | 20 (33.33%) | 62 (100%) |
| Total number of cases | 55 (18.33%) | 179 (59.66%) | 66 (22%) | 300 (100%) |
Chi2 value = 25.1, p value = 0.00
Superior positioning of the canal was not seen in our sample population.
Discussion
For the removal of impacted third molars, being one of the commonest of oral and maxillofacial procedures, it is of paramount importance to evaluate and understand the vital structures in and around the tooth and to avoid intra- and postoperative complications. The horizontal and vertical positions of the mandibular canal and corresponding third molars are a key anatomic factor of IAN injury [11–13].
Panoramic radiography is one of the widely used modalities in dental office prior to removal of mandibular third molars [8]. It depicts certain radiographic features which indicate higher chances of nerve injury in course of the procedure. However, being a two-dimensional imaging approach it is not accurate in giving the buccolingual relationship of the tooth and the nerve canal [6–8].
Identification and proper knowledge of the positioning of the nerve canals assists the surgeon in quantifying the relative amount and depth of bone removal for extraction of the tooth without damaging the nerve canal [14]. The present study indicates that in our sample, majority of the cases irrespective of the position and depth of the tooth had the mandibular canal placed on the lingual side of the mandibular third molar accounting for 67.33% (Table 1). This result was found to be in accordance with the studies done by Ohman et al., De Melo Albert, Tatanopornkul et al. [15–17].
Shujaat et al. also found in their study of 100 impactions that the majority of cases had the canal positioned on the lingual side [18]. Jhamb et al. in their study showed that the nerve exposure is higher when the canal is placed in the lingual side of the tooth, which was reinforced by Kim et al., who explained that the nerve is more vulnerable to injury when found on the lingual side [19, 20].
In approximately 73.75% of the cases in the present study, the mandibular canal was in close association with the lingual cortical plate [Table 2]. This finding of the study was in conformity with the observations of the studies by Miller et al. and Maegawa et al., giving an indication that it is safe to conduct guttering of buccal bone while extraction of the third molars and to avoid lingual bone removal to avoid neural damage [21, 22].
Quirino de Almeida Barros et al. mentioned in their study that the most prevalent position of the mandibular canal was below the roots of the third molar, followed by the vestibular [23]. This statement was confirmed by studies done by Chen et al. and Maglione et al. [24, 25].
The study revealed that the largest share of the cases in the study were of the mesioangular variant. This observation was also depicted in the study done by Hassan et al. where approximately 33.4% of the Saudi population had mesioangular mandibular impactions. Syed et al. found 50.75% of the Saudi population with mesioangular type, which is also seen in the studies done by Quek et al. [26–28]. On the contrary, Shujaat et al. in their study obtained greater number of horizontal type of mandibular impactions [18].
Several studies have been conducted on the subjects like the influence of CBCT on treatment planning and also the comparison of CBCT versus panoramic radiographs in determining spatial relationships of the tooth and surrounding structures. Although the possibility of nerve damage is widely dependent on the approach and the skill of the operator, three-dimensional characterizations using CBCT have advanced the level of treatment planning considerably over the years [29–32].
Yabroudi et al. in their study of 30 patients showed by doing an analysis on 47 third molars that in most of the cases the nerves were found to be inferior and lingual to the roots of the third molar. The study was also helpful in concluding that using CBCT, the anatomy is better depicted compared to panoramic imaging [33].
Having discussed the advantages of CBCT over conventional 2D radiography in terms of better diagnosis and treatment planning, the financial aspect of the CBCT scans should also be taken into consideration. Due to relatively lower rates of CBCT, compared to regular CTs and MRIs, it is certain and important to inculcate the practice of advising CBCTs for minor and major oral surgical procedures.
Conclusion
The mandibular canal is positioned mostly lingual and inferior to the roots of mandibular third molars. The sample population revealed a majority of mesioangular and class II position B variant of impactions. Irrespective of type, class and position of the teeth, mostly the mandibular canals were found to be placed lingually, inferiorly and in association with the lingual cortical plates.
Due to the limitations in the number of female participants in the sample, sex predilection was not considered. The study was a hospital-based study in a specific state; thus, the findings cannot be generalized. Also the prevalence of nerve injury was not studied. Thus, further extensive studies are required.
Acknowledgement
The study was supported by Department of Oral Medicine and Radiology, Kalinga Institute of Dental Sciences, KIIT University, Bhubaneswar, India.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rajat Mohanty, Email: rajatmohanty007@gmail.com.
Purnendu Rout, Email: purnendu.rout@gmail.com.
Vaibhav Singh, Email: vaibhavsingh24@gmail.com.
References
- 1.Gu L, Zhu C, Chen K, Liu X, Tang Z. Anatomic study of the position of the mandibular canal and corresponding mandibular third molar on cone-beam computed tomography images. Surg Radiol Anat. 2017;40(6):609–614. doi: 10.1007/s00276-017-1928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003;61(12):1379–1389. doi: 10.1016/j.joms.2003.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010;39(4):320–326. doi: 10.1016/j.ijom.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 4.Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(4):377–383. doi: 10.1067/moe.2001.118284. [DOI] [PubMed] [Google Scholar]
- 5.Smith AC, Barry SE, Chiong AY, Hadzakis D, Kha SL, Mok SC, Sable DL. Inferior alveolar nerve damage following removal of mandibular third molar teeth: a prospective study using panoramic radiography. Aust Dent J. 1997;42(3):149–152. doi: 10.1111/j.1834-7819.1997.tb00111.x. [DOI] [PubMed] [Google Scholar]
- 6.Maegawa H, Sano K, Kitagawa Y, Ogasawara T, Miyauchi K, Sekine J, Inokuchi T. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):639–646. doi: 10.1016/S1079-2104(03)00356-1. [DOI] [PubMed] [Google Scholar]
- 7.Monaco G, Montevecchi M, Bonetti GA, Gatto MR, Checchi L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc. 2004;135(3):312–318. doi: 10.14219/jada.archive.2004.0179. [DOI] [PubMed] [Google Scholar]
- 8.Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005;3(1):3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 9.Al-Salehi SK, Horner K. Impact of cone beam computed tomography (CBCT) on diagnostic thinking in endodontics of posterior teeth: a before- after study. J Dent. 2016;53:57–63. doi: 10.1016/j.jdent.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 10.Pohlenz P, Blessmann M, Blake F, Heinrich S, Schmelzle R, Heiland M. Clinical indications and perspectives for intraoperative cone-beam computed tomography in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(3):412–417. doi: 10.1016/j.tripleo.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Hasegawa T, Ri S, Shigeta T, Akashi M, Imai Y, Kakei Y, Shibuya Y, Komori T. Risk factors associated with inferior alveolar nerve injury after extraction of the mandibular third molar—a comparative study of preoperative images by panoramic radiography and computed tomography. Int J Oral Maxillofac Surg. 2013;42:843–851. doi: 10.1016/j.ijom.2013.01.023. [DOI] [PubMed] [Google Scholar]
- 12.Kim JW, Cha IH, Kim SJ, Kim MR. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg. 2012;70:2508–2514. doi: 10.1016/j.joms.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Nakayama K, Nonoyama M, Takaki Y, Kagawa T, Yuasa K, Izumi K, Ozeki S, Ikebe T. Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg. 2009;67:2587–2591. doi: 10.1016/j.joms.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Eyrich G, Seifert B, Matthews F, Matthiessen U, Heusser CK, Kruse AL, Obwegeser JA, Lübbers HT. 3-Dimensional imaging for lower third molars: is there an implication for surgical removal? J Oral Maxillofac Surg. 2011;69(7):1867–1872. doi: 10.1016/j.joms.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 15.De Melo Albert DG, Gomes AC, Do Egito Vasconcelos BC, De Oliveira e Silva ED, Holanda GZ. Comparison of orthopantomographs and conventional tomography image for assessing the relationship between impacted lower third molars and mandibular canal. J Oral Maxillofac Surg. 2006;64:1030–1037. doi: 10.1016/j.joms.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 16.Flygare L, Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig. 2008;12:291–302. doi: 10.1007/s00784-008-0200-1. [DOI] [PubMed] [Google Scholar]
- 17.Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, Kurabayashi T. A comparative study of cone-beam computed tomography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:253–259. doi: 10.1016/j.tripleo.2006.06.060. [DOI] [PubMed] [Google Scholar]
- 18.Shujaat S, Abouelkheir HM, Al-Khalifa KS, Al-Jandan B, Marei HF. Pre-operative assessment of relationship between inferior dental nerve canal and mandibular impacted third molar in Saudi population. Saud Dent J. 2014;26(3):103–107. doi: 10.1016/j.sdentj.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jhamb A, Dolas RS, Pandilwar PK, Mohanty S. Comparative efficacy of spiral computed tomography and orthopantomography in preoperative detection of relation of inferior alveolar neurovascular bundle to the impacted mandibular third molar. J Oral Maxillofac Surg. 2009;67(1):58–66. doi: 10.1016/j.joms.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 20.Kim HG, Lee JH. Analysis and evaluation of relative positions of mandibular third molar and mandibular canal impacts. J Kor Assoc Oral Maxillofac Surg. 2014;40(6):278–284. doi: 10.5125/jkaoms.2014.40.6.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maegawa H, Sano K, Kitgawa Y, Ogasawara T, Miyauchi K, Sekine J, Inokuchi T. Preoperative assessment of the relationship between the mandibular third molar and mandibular canal by axial computed tomography. Oral Surg Oral Med Oral Pathol. 2003;96:639–646. doi: 10.1016/S1079-2104(03)00356-1. [DOI] [PubMed] [Google Scholar]
- 22.Miller CS, Nummikoski PV, Barnett DA, Langlais RP. Cross sectional tomography: a diagnostic technique for determining the buccolingual relationship of the impacted mandibular third molars and the inferior alveolar neurovascular bundle. Oral Surg Oral Med Oral Pathol. 1990;70:791–797. doi: 10.1016/0030-4220(90)90023-L. [DOI] [PubMed] [Google Scholar]
- 23.Quirinode Almeida Barros R, Bezerrade Melo N, de Macedo Bernardino Í, Arêa Leão Lopes Araújo Arruda MJ, Meira Bento P. Association between impacted third molars and position of the mandibular canal: a morphological analysis using cone-beam computed tomography. Br J Oral Maxillofac Surg. 2018;56(10):952–955. doi: 10.1016/j.bjoms.2018.10.280. [DOI] [PubMed] [Google Scholar]
- 24.Chen Y, Liu J, Pei J, et al. The risk factors that can increase possibility of mandibular canal wall damage in adult: a cone-beam computed tomography (CBCT) study in a Chinese population. Med Sci Monit. 2018;24:26–36. doi: 10.12659/MSM.905475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maglione M, Costantinides F, Bazzocchi G. Classification of impacted mandibular third molars on cone-beam CT images. J Clin Exp Dent. 2015;7:e224–e231. doi: 10.4317/jced.51984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hassan AH. Pattern of third molar impaction in Saudi population. Clin Cosmet Investig Dent. 2010;2:109–113. doi: 10.2147/CCIDE.S12394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Syed KB, Kota Z, Ibrahim M, Bagi MA, Assiri MA. Prevalence of impacted molar teeth among Saudi population in Asir region, Saudi Arabia – a retrospective study of 3 years. J Int Oral Health. 2012;5:43–47. [PMC free article] [PubMed] [Google Scholar]
- 28.Quek SL, Tay CK, Tay KH, Toh SL, Lim KC. Pattern of third molar impaction in a Singapore Chinese population: a retrospective radiographic survey. Int J Oral Maxillofac Surg. 2003;32:548–552. doi: 10.1016/S0901-5027(03)90413-9. [DOI] [PubMed] [Google Scholar]
- 29.Ghaeminia H, Gerlach NL, Hoppenreijs TJM, Kicken M, Dings JP, Borstlap WA, de Haan T, Bergé SJ, Meijer GJ, Maal TJ. Clinical relevance of cone beam computed tomography in mandibular third molar removal: a multicentre, randomised, controlled trial. J Craniomaxillofac Surg. 2015;43:2158–2167. doi: 10.1016/j.jcms.2015.10.009. [DOI] [PubMed] [Google Scholar]
- 30.Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Vlijmen OJC, Bergé SJ, Maal TJJ. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral Maxillofac Surg. 2011;40:834–839. doi: 10.1016/j.ijom.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 31.Guerrero ME, Botetano R, Beltran J, Horner K, Jacobs R. Can preoperative imaging help to predict postoperative outcome after wisdom tooth removal? A randomized controlled trial using panoramic radiography versus cone-beam CT. Clin Oral Investig. 2014;18:335–342. doi: 10.1007/s00784-013-0971-x. [DOI] [PubMed] [Google Scholar]
- 32.Guerrero ME, Nackaerts O, Beinsberger J, Horner K, Schoenaers J, Jacobs R. Inferior alveolar nerve sensory disturbance after impacted mandibular third molar evaluation using cone beam computed tomography and panoramic radiography: a pilot study. J Oral Maxillofac Surg. 2012;70:2264–2270. doi: 10.1016/j.joms.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 33.Yabroudi Feras, Sindet-Pedersen Steen. Cone Beam Tomography (CBCT) as a diagnostic tool to assess the relationship between the inferior alveolar nerve and roots of mandibular wisdom teeth. Smile Dent J. 2012;7(3):12–17. [Google Scholar]