Abstract
Synovial chondromatosis is a rare condition characterized by the presence of loose cartilaginous bodies, due to the abnormal proliferation of synovial membrane. However, its manifestation in the temporomandibular joint is a rare finding, occurring predominantly in females. This case report describes the clinical features, diagnosis and management of a case of synovial chondromatosis.
Keywords: TMJ, Synovial membrane, Calcified nodules
Introduction
Synovial chondromatosis (SC) is a rare condition characterized by the presence of loose cartilaginous bodies, due to the abnormal proliferation of synovial membrane. Synovial chondromatosis is defined by the World Health Organization as a benign nodular cartilaginous proliferation arising from the joint synovium, bursae or tendon sheaths [1]. It mainly affects large joints such as knee, hip, shoulder and elbow, commonly in males. However, its manifestation in the temporomandibular joint (TMJ) is a rare finding, occurring predominantly in females [2]. SC was originally described by Ambroise Pare in 1558, and the involvement of the TMJ was described in 1933 by Auhausen [3]. Two forms of the SC have been recognized: primary and secondary. It may develop as a primary lesion or may arise after a trauma or another disease process such as osteoarthritis. The pathogenesis of the primary form of SC is unknown. It has been proposed that the disease develops as a response to repetitive, low-grade trauma. Inflammation, parafunctional habits or joint overuse, as well as degeneration, has been seen as potential causative factors for the secondary form. SC is observed in 17% of patients treated arthroscopically due to TMJ osteoarthritis [4].
Panoramic radiographs, CBCT and CT facilitate the clinical diagnosis of SC; however, histopathological analysis is mandatory to confirm the disease. We report a case of a SC treated successfully through a surgical approach.
Case Report
A 38-year-old male patient visited the Department of Oral and Maxillofacial Surgery, Vydehi Institute of Dental Sciences and Hospital, in February 2015 with a chief complaint of pain and swelling in the right preauricular region since 8 years. He gave a history of right ear pain and preauricular tenderness while opening and closing his mouth. Physical examination revealed tenderness and swelling in the TMJ region, with a mouth opening of 38 mm. There was slight deviation to the right and a clicking sound in the right joint during mouth opening. There was no history of trauma or any parafunctional habit.
A panoramic radiograph showed multiple calcified loose bodies around the right mandibular condyle. There was an increase in the joint space with mild erosive changes in the condylar head. CBCT showed the presence of faint opacities in the medial, anterior, posterior and superior aspect of condyle which probably represented extra-articular calcifications. Axial and coronal CT images (Figs. 1, 2) show distinct nodules within an expanded upper joint compartment and also revealed widening of the TMJ space and multiple calcifications around it. The images also showed bony erosion with sclerotic changes in the adjacent articular eminence and glenoid fossa. Based on clinical and imaging findings, a presumptive diagnosis of SC of the left TMJ was made.
Fig. 1.
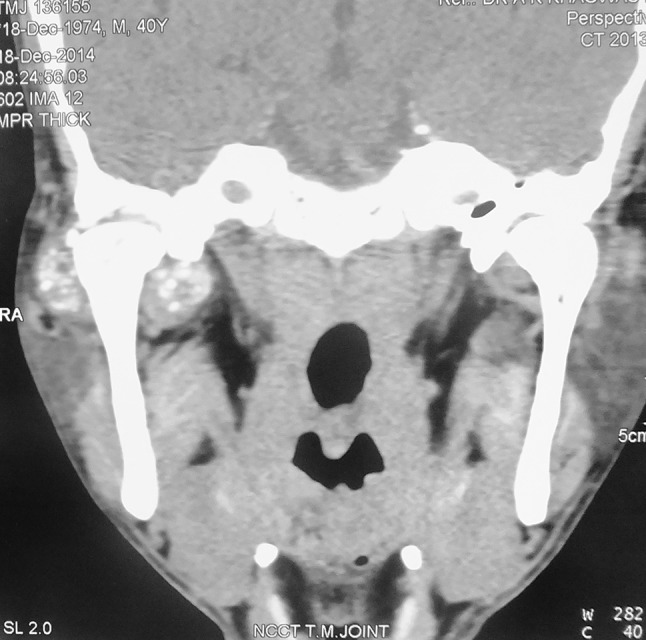
Coronal CT
Fig. 2.

Axial CT
Surgical exploration of the mass via an Alkayat Bramley incision was performed under general anaesthesia. Layered dissection was done to expose the tumour mass situated lateral to the right condylar region which was composed of multiple pebble-like cartilaginous structures (Fig. 3). This lateral part of the tumour was removed. Subsequently, osteotomy of the neck of the condyle was performed. Then the condyle was swung to gain approach to the medial aspect of the condyle, and calcified bodies (Fig. 4) were removed. The articular disc was repositioned and sutured, and condylar shave and glenoid fossa shave were done in the region of the erosion. The condylar neck was fixed with two titanium miniplates and screws (Fig. 5).
Fig. 3.

Exposed pathology
Fig. 4.

Fixation of osteotomized condyle
Fig. 5.
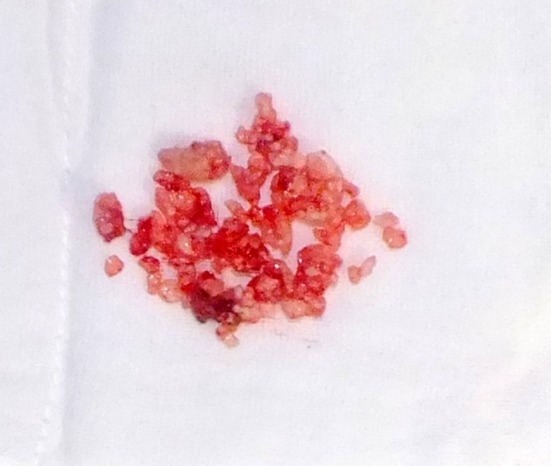
Specimen of the pathology
The diagnosis was confirmed with histopathological investigation. The gross pathologic appearance showed hyperplastic synovium covering white multilobulated nodular projections of hyaline cartilage. Histopathology of the same revealed globular masses of cartilage tissue which exhibited areas of calcification. Chondrocytes showing mild atypia in the lacunae were seen. The synovial connective tissue between the cartilages was delicate and fibrillar. The peripheries of the globular masses were cellular with numerous blood vessels.
Based on the clinical, radiological and histopathological findings, the diagnosis of SC of right TMJ was made. The patient showed good functional recovery after surgery, and no evidence of recurrence or residual disease was detected in the operated joint after 3 years (Fig. 6).
Fig. 6.
OPT after 3 years
Discussion
Synovial chondromatosis (SC) is a non-neoplastic and infrequent joint disease characterized as a proliferative disorder of the synovium associated with the formation of metaplastic cartilaginous nodules originating from the synovial membrane [5]. It is also known as synovial osteochondromatosis and synovial chondrometaplasia and commonly manifests with joint swelling, pain and joint dysfunction [6].
Because of the absence of physical signs and symptoms, SC of the TMJ often receives a delayed diagnosis or is misdiagnosed for other common diseases with similar symptoms such as TMJ disorders or arthritis. The mean latency period is relatively long, and the average time of onset of SC of the TMJ is more than 1 year. While the clinical features are not usually conclusive, diagnosis of SC of the TMJ is usually made using conventional radiography, computed tomography (CT) and magnetic resonance imaging (MRI) which reveal loose bodies in the joint space. Although conventional radiographs as the first-line technique for diagnosis of TMJ disorders can show widening of the joint spaces, those in which the cartilaginous nodules lack calcification or ossification may not be detected. CT and MRI are used to evaluate TMJ diseases and can make a more accurate diagnosis [7].
The histological staging of synovial chondromatosis was published by Milgram in 1977 and is based on disease activity and development. Stage 1 is the early stage and represents intrasynovial metaplasia without loose bodies; peri-focal macrophages may be present. Stage 2 is the transitional stage, in which synovial involvement and detached bodies are present. Stage 3 shows no more active intrasynovial disease (metaplasia), but the joint space is full of multiple detached bodies, and secondary calcification or ossification may be present. The secondary calcification is called Henderson–Jones syndrome. The loose bodies in the joint space may be surrounded by a layer of synovial membrane. Over 80% of patients are at Milgram stage 3 when the diagnosis of synovial chondromatosis is made [8].
There have been rare reports of bilateral involvement [9, 10] and involvement of both compartments [11].
A classic open surgical approach to the TMJ is the treatment of choice because of the impossibility of removing all of the loose bodies by other means. Synovectomy is the most frequent procedure because of the association with loose bodies. The synovial membrane and loose bodies are all removed from the joint space, often accompanied by articular disc resection and less frequently by condylar resection [6].
A combination of open surgery and arthroscopy for the treatment of synovial chondromatosis (SC) of the temporomandibular joint (TMJ) has also been mentioned. This technique has the benefits of the complete elimination of diseased tissues with a minimal osteotomy and a short surgical duration [12].
The recurrence rate of SC appears to be very low. The probable reasons were bony erosions on the condyle or fossa, which were ignored during the initial operation when the lesion inside the marrow was not removed thoroughly. The cause of the recurrence is probably the active metaplastic foci in the tiny bony erosion that was recorded as being in an early stage of Milgram classification. These foci probably continued to grow, proliferate and invade the bone, finally inducing recurrence [13]. The significant literature pertaining to the condition is enumerated in Table 1.
Table 1.
Literature review of significant articles related to synovial chondromatosis
| No. | Authors | Journal | Incidence |
|---|---|---|---|
| 1 | Holmlund AB, Eriksson L, Reinholt FP | Int J Oral Maxillofac Surg 32:143, 2003 | Clinical, surgical and radiological aspects |
| 2 | Leon Ardekian et al. | J Oral Maxillofac Surg 63:941–947, 2005 | Report and analysis of 11 cases |
| 3 | Jong-Ki Huh | Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;101:e83–e88 | Condylar extension |
| 4 | Lieger O, Zix J, Stauffer-Brauch EJ, Iizuka T | J Oral Maxillofac Surg 2007;65:2073–80 | Case report and literature review |
| 5 | Li-wei Peng, De-min Yan, Yong-gong Wang and Ya-dong Li | J Oral Maxillofac Surg 67:893–895, 2009 | Bilateral involvement |
| 6 | J. Sato, K.-I. Notani, J. Goto, M. Shindoh, Y. Kitagawa | Int. J. Oral Maxillofac. Surg. 2010; 39:86–88 | Involvement of both joint spaces |
| 7 | Meng J, Guo C, Yi B, et al. | Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:441, 2010 | Clinical and radiological findings |
| 8 | Raquel Guijarro-Martínez et al. | Journal of Cranio-Maxillo-Facial Surgery 39 (2011) 261–265 | Bilateral involvement |
| 9 | Yui Mori et al. | Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:e35–e39 | 17-year follow-up |
| 10 | Masahiro Wake et al. | British Journal of Oral and Maxillofacial Surgery 51 (2013) 164–169 | Inflammatory mediators in synovial fluid |
| 11 | Aecio Abner Campos Pinto Jr et al. | Head and Neck Pathol (2015) 9:525–529 | Surgical treatment |
| 12 | Xingguang Liu, Zhongyang Huang, Wangyong Zhu, Peisheng Liang and Qian Tao | J Oral Maxillofac Surg 74:2159–2168, 2016 | Analysis of 10 cases and literature review |
| 13 | Z.-X. Han, M.-J. Chen, C. Yang, M.-J. Dong | BJOMS 55 2017. 965–967 | 274 cases in 16 years |
| 14 | J.N. Khanna R. Ramaswami | Int. J. Oral Maxillofac. Surg. 2017; 46:1579–1583 | Cranial extension |
| 15 | G. Bai, C. Yang, Y. Qiu, M. Chen | Int. J. Oral Maxillofac. Surg. 2017; 46:208–213 | Open surgery assisted with arthroscopy |
Compliance with Ethical Standards
Conflict of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Priyangana Nath, Email: priyangana17@gmail.com.
Suresh Menon, Email: psurmenon@gmail.com.
References
- 1.Miller MV, King A, Mertens F. Synovial chondromatosis. In: Fletcher CDM, Unni KK, Mertens F, editors. World Health Organization classification of tumours. Pathology and genetics of tumours of soft tissue and bone. Lyon: IARC Press; 2002. p. 246. [Google Scholar]
- 2.Pinto AAC, Jr, e Costa RF, de Sousa SF, Chagas MRP, do Carmo MAV, de Lacerda JCT. Synovial chondromatosis of the temporomandibular joint successfully treated by surgery. Head Neck Pathol. 2015;9:525–529. doi: 10.1007/s12105-015-0626-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ginaldi S. Computed tomography feature of synovial osteochondromatosis. Skeletal Radiol. 1980;5:219–222. doi: 10.1007/BF00580593. [DOI] [PubMed] [Google Scholar]
- 4.Ivask Oksana, Leibur Edvitar, Voog-Oras Ülle. Synovial chondromatosis in the temporomandibular joint: case report with review of the literature. Stomatol Balt Dent Maxillofac J. 2015;17:97–101. [PubMed] [Google Scholar]
- 5.Holmlund AB, Eriksson L, Reinholt FP. Synovial chondromatosis of the temporomandibular joint: clinical, surgical and histological aspects. Int J Oral Maxillofac Surg. 2003;32:143. doi: 10.1054/ijom.2002.0300. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Huang Z, Zhu W, Liang P, Tao Q. Clinical and imaging findings of temporomandibular joint synovial chondromatosis: an analysis of 10 cases and literature review. J Oral Maxillofac Surg. 2016;74:2159–2168. doi: 10.1016/j.joms.2016.04.029. [DOI] [PubMed] [Google Scholar]
- 7.Meng J, Guo C, Yi B, et al. Clinical and radiologic findings of synovial chondromatosis affecting the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:441. doi: 10.1016/j.tripleo.2009.09.036. [DOI] [PubMed] [Google Scholar]
- 8.Lieger O, Zix J, Stauffer-Brauch EJ, Iizuka T. Synovial chondromatosis of the temporo-mandibular joint with cranial extension: a case report and literature review. J Oral Maxillofac Surg. 2007;65:2073–2080. doi: 10.1016/j.joms.2006.04.039. [DOI] [PubMed] [Google Scholar]
- 9.Guijarro-Martínez R, Torres MP, Mateo MM, García IS, Alba LM, Gimilio MEI, Hermosa GP-H, Gil JVP. Bilateral synovial chondromatosis of the temporomandibular joint. J Craniomaxillofac Surg. 2011;39:261–265. doi: 10.1016/j.jcms.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 10.Peng Li-wei, Yan De-min, Wang Yong-gong, Li Ya-dong. Synovial chondromatosis of the temporomandibular joint: a case report with bilateral occurrence. J Oral Maxillofac Surg. 2009;67:893–895. doi: 10.1016/j.joms.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 11.Sato J, Notani K-I, Goto J, Shindoh M, Kitagawa Y. Synovial chondromatosis of the temporomandibular joint accompanied by loose bodies in both the superior and inferior joint compartments: case report. Int J Oral Maxillofac Surg. 2010;39:86–88. doi: 10.1016/j.ijom.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Bai G, Yang C, Qiu Y, Chen M. Open surgery assisted with arthroscopy to treat synovial chondromatosis of the temporomandibular joint. Int J Oral Maxillofac Surg. 2017;46:208–213. doi: 10.1016/j.ijom.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 13.Han Z-X, Chen M-J, Yang C, Dong M-J. Recurrent synovial chondromatosis of the temporomandibular joint: report of two cases. Br J Oral Maxillofac Surg. 2017;55:965–967. doi: 10.1016/j.bjoms.2017.08.367. [DOI] [PubMed] [Google Scholar]



