Abstract
Background
Treatment modalities for cysts have evoked the greatest debates and controversies because of the size, localization, pathological formation and recurrence potential of cysts. Enucleation has been most effective and reliable method to treat cysts. It completely removes the cystic capsule, thus reducing the possibility of recurrence. Certain modifications to the method of enucleation have been proposed for ease of removal and to assure complete enucleation.
Aim and objective
A new modification aimed at increasing the probability of a good and complete enucleation has been proposed at the Department of Oral and Maxillofacial surgery in DAV Dental College, Yamunanagar.
Method
A window is created in the cystic roof with complete aspiration and evacuation of cystic contents following which the complete cystic lumen is packed with a ribbon gauze. The ribbon gauze is then wetted with normal saline or povidone iodine. Once enucleation is started at the correct plane, it gives a stable base from inside the cystic lumen due to which perforation of cyst is reduced markedly.
Conclusion
The newly proposed technique reduced the chances of cystic lining perforation and ensures the in toto enucleation of cysts in majority of the operated cases.
Keywords: Cyst, Enucleation, In toto enucleation
Introduction
A cyst is a pathological cavity in the bone or soft tissue, with an outer wall of connective tissue and an inner wall composed of epithelium. The interior of the cystic cavity is filled with a cystic content, which may be watery, colloidal or semisolid [1]. Several methods of treatment exist depending on the size and localization. Drainage of the cyst ensures that fluid no longer accumulates, and its stimulus on the cystic capsule disappears, which is considered one of the potential causal agents of its progressive growth. Consequently, its autonomic growth is arrested and accordingly further development [1].
Cysts are most frequently treated surgically. The treatment modalities have evoked the greatest debates and controversies because of the size, localization, pathological formation and recurrence potential of the cysts. Management of cysts should focus on selecting the best modality that carries the lowest possible risk of recurrence and minimum morbidity. Management options can broadly be divided into conservative treatment and radical management. Conservative treatment aims at preserving the bony architecture as much as possible while removing the pathology as in marsupialization or decompression. More aggressive forms of management are enucleation with/without curettage along with adjunctive uses of chemical/cryocauterization or resection. In 1965, Fickling [2] enumerated the methods used in treatment of cysts as follows:
Enucleation and closed by suture: Enucleate the cyst lining completely and close the intra-oral incision. This is the ideal, but closure should only be carried out when the operator is clinically certain that enucleation has been complete. This is also called Partsch I [3].
Enucleation and packed open: Enucleate the cyst and open widely to the mouth. This is indicated when enucleation has proved so difficult that it might be incomplete or when the cyst is so large that, even with antibiotics or space-filling materials, breakdown might occur if the wound is closed. The resulting cavity fills quite rapidly.
Lining left, cavity saucerized (Marsupialization): Uncover the cyst by removing the oral bony wall over a wide area and leave the lining. This is the operation described by Dowsett [4] who added the suture of the buccal wall to the remaining lining. Although less popular now, this method goes some way to avoiding damage to the maxillary sinus, nasal floor or mandibular nerve and teeth and causes very little constitutional disturbance in elderly patients or in those with intercurrent disease which might lead to poor healing. This is also called Partsch II [5].
Lining left, small opening maintained by cyst plug: Make a relatively small opening, leave the lining and employ a cyst plug to maintain the opening until regression has occurred. This is especially suitable for large cysts in sites which cannot be saucerized or opened widely, such as those at the tuberosity and ramus. It is a valuable procedure, especially when combined with delayed enucleation as a two-stage operation.
Opened into antrum or nose, mouth closed: Open a maxillary cyst widely into the antrum and nose, perform a nasal antrostomy and close the oral incision. This is especially valuable for cysts which can be demonstrated to be leaking into the nose and for antral cysts. The resulting cavity tends to be dependent but should regress in size; not all remains free from some antral symptoms.
Enucleated by extra-oral approach, wound sutured: Make an extra-oral approach by a submandibular incision, which implies enucleation and closure.
Cyst left alone: Leave the cyst alone, a technique of nonintervention indicated, rarely, in the very aged or infirm, which should be remembered by every surgeon.
Two-stage operation [6]: In the two-stage operation, a carefully shaped cyst plug should be worn for at least 1 year. After that time, enucleation is much simplified and the cavity can either be closed if suitable flaps can be prepared or packed and allowed to granulate.
Apicoectomy in addition to one of the above methods: The preservation of involved teeth by apicoectomy in addition to one of the above methods is applied for treatment of cyst.
Enucleation, so far, has been most effective and reliable method to treat the cysts. It completely removes the cystic capsule, therefore reducing the possibility of recurrence [7], which according to Pindborg [8] amounts to 33%, and according to Toller [9] 44%, and also the possibility of spreading carcinoma from the epithelium of the cystic capsule [10]. Certain modifications in the method of enucleation have been proposed for ease of removal and to assure complete enucleation. Some of these modifications are worth mentioning involving assistance of advanced technologies or modification in the technique of enucleation.
Endoscope-assisted cyst enucleation [11]: In smaller-sized cysts, enucleation can be accomplished without many problems. However, in some instances, the cyst can be very big making complete removal difficult unless a generous incision is made. This approach is overly aggressive for a benign lesion. In this situation, the assistance from a rigid endoscope (4.0-mm, O-degree Hopkins endoscope) is helpful in guiding the enucleation of the cyst safely without affecting the surrounding tissues. A suction elevator can be used to separate the cyst from the surrounding bone. This technique not only reduces the size of the incision required, but it also offers a superior visualization of the difficult corners and angles around different aspects of the lesion. Furthermore, it provides good illumination and a clear and magnified visualization of the operating field, and thus it results in a more conservative surgery with precise enucleation.
Microscope-assisted cyst enucleation [12]: The use of microscope during enucleation of small cysts, e.g., periapical odontogenic cysts helps to get a better view of the extent of defect. Thus, the cyst can be removed in toto and the apices would be observed clearly. The use of microscope gave better visibility and cleaner field, but caused increase in the operation time along with operator and patient fatigue. Incorporation of operating microscope in procedure also needs a well-trained assistant with a good knowledge of the procedure.
Enucleation using injection of hydrocolloid dental impression material [13]: Shira [14] advocated the treatment of mucoceles and ranulas by aspiration of fluid contents of the lesion, followed by injection of alginate. The use of alginate to assist the removal of the lesion allows delimiting the margins of the lesion and maintaining its integrity. Therefore, the surgical excision can be performed quickly without involvement of adjacent structures [15]. When used in big sized ranulas, this technique is practical, safe and easy, avoiding relapse episodes. A possible complication of this technique is the development of a foreign body reaction secondary to inadvertent permanence of a small amount of the alginate within the surgical site. Therefore, all injected material and the lesion should be removed carefully. It should also be addressed that one of the inherent properties of the alginate is the presence of antimicrobial action [16], which enhances the safety of this technique.
The complete review of the literature, however, illustrates one common thing that a good enucleation is the primary factor of importance following any modification. Enucleation has been a procedure which has been carried out since ages. The method of enucleation is used for small cysts, although it should be used whenever possible as it has certain advantages over marsupialization: a method used for surgical treatment of large cysts [17]. The commonest problem encountered with this procedure leading to recurrence and spillage of intracystic contents is often incomplete enucleation. The solution for this problem is ensuring a technique which allows in toto enucleation of the cyst.
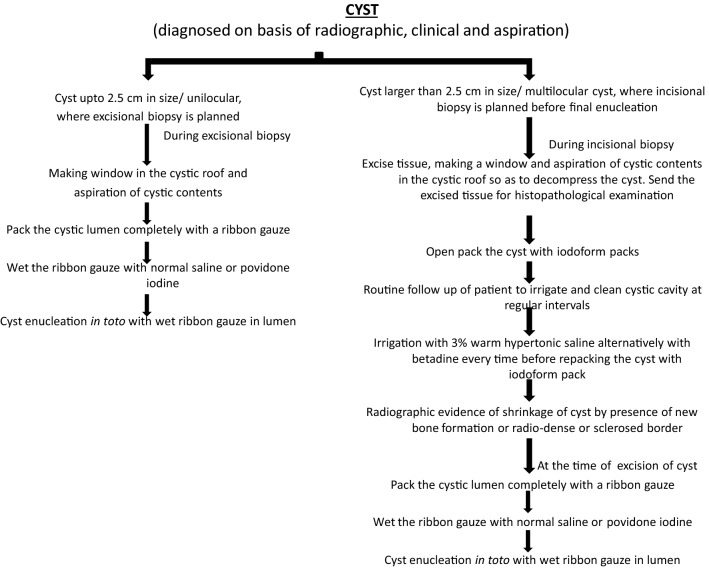
In our institution, we have come up with a new technical modification (Fig. 1). The aim of this modification is very clear, i.e., to increase the probability of a good complete enucleation following which any of the procedural modification as mentioned above can be applied.
Fig. 1.
Modified technique for cyst enucleation in toto
In the proposed modification; depending on the size, location, radiographic presentation if the cyst is smaller than 2.5 cm such that enucleation would be the procedure of choice, we advise to prepare the patient in the usual way. As an excisional biopsy would be the required procedure, we have modified this step slightly. We advise making a window in the cystic roof and complete aspiration and evacuation of cystic contents following which we pack the complete cystic lumen with ribbon gauze so that the lumen is over packed. Now, once the lumen is packed, we wet the ribbon gauze with normal saline or povidone-iodine. The normal saline or povidone-iodine solution acts as wetting agent. Due to capillary action resulting from the pores of gauze piece, the wetting agent sticks to the gauze. Adhesion due to wetting agent in between gauze and the cystic epithelium gives a form to the cyst in turn. Once enucleation is started at the correct plane, it gives a stable base from inside the cystic lumen due to which perforation of cyst is reduced markedly. In the normal case where there is nothing packed in the lumen, there is no stable base over which a plane of dissection could be developed. After the cyst enucleation, the ribbon gauze can be removed from the cyst by not pulling it from the window but by cutting the cyst open and removal of gauze slowly. This maneuver is done before submitting the excised tissue for final histopatholgical examination. Pulling the ribbon gauze might lead to damage of cystic epithelium and thus leading to difficulty in histopatholgical examination.
If the cyst is larger than 2.5 cm and incisional biopsy is the procedure of choice, we advise that during incisional biopsy a window should be excised from the roof of the cyst and aspiration of the cystic contents should be carried out so as to decompress the cyst. Send this excised tissue for histopathological examination. Open packing of the cystic lumen with iodoform packs should be carried out. We advise irrigating the cyst lumen with 3% warm hypertonic saline alternatively with povidone-iodine every time before repacking the cyst with iodoform packs. Controlled secondary bacterial contamination would lead to slight fibroses of the cystic connective tissue, and warm hypertonic 3% solution would also work in a similar fashion inducing fibrosis in the cyst wall. This fibrosis in the cyst connective tissue would help in thickening of the cyst wall thus reducing the chances of cyst wall fragmentation during cyst enucleation (Figs. 2, 3, 4, 5, 6).
Fig. 2.
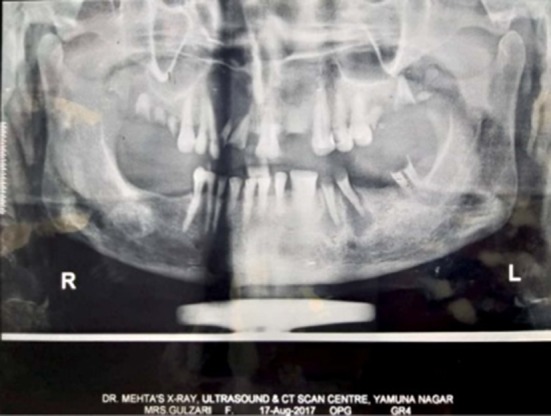
Preoperative OPG showing radiolucent defect on the right maxillary region
Fig. 3.

Flap elevation and exposure of the Cyst
Fig. 4.

Packing of the Cystic Lumen with a ribbon guage after making window in the Cystic roof and aspiration of Cystic contents
Fig. 5.

Cyst enucleation in toto
Fig. 6.

Enucleated cyst with packed ribbon gauge
When the radiographic evidence of cyst cicatrization is evident in the form of formation of new bone, shrinkage of cystic lumen and radio dense and sclerosis of cystic margins after a period of 5 to 6 months such as 60–70% of the cyst dimension has shrunken a second and final procedure of cyst enucleation should be carried out. This procedure would remain the same as discussed above with the wet ribbon gauze in lumen and excising the complete cyst in toto.
Conclusion
In quest of a technique ensuring in toto enucleation of the cysts, a new proposed modification has been employed in more than 80 cases in last 3 years of time at our institution. Intra-operative results and postoperative follow-ups confirm the in toto enucleation of the cysts in majority of these operated cases.
Compliance with Ethical Standards
Conflict of interest
All the authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Naveen Chhabra, Email: naveenprisha@yahoo.co.in.
Shruti Chhabra, Email: drshruti75@gmail.com.
Abhishek Kumar, Email: dr.deshwal.abhishek@gmail.com.
References
- 1.Mice I. OralnaKirurgija. Zagreb: JUMENA; 1983. [Google Scholar]
- 2.Fickling BW (1965) Cysts of the jaw: a long-term survey of types and treatment. In: Proceedings of the royal society of medicine, p. 58 [DOI] [PMC free article] [PubMed]
- 3.Partsch C, Kiefercysten U, Zahnheilkunde MF, Zahnheilkunde MF. 10,271, Quoted from Pogrel MA, Treatment of keratocysts: the case for decompression and marsupialization. J Oral Maxillofac Surg. 2005;63:1667–1673. doi: 10.1016/j.joms.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 4.Dowsett EB. Operative procedures for cysts of the jaws. Proc R Soc Med. 1932;25:47. doi: 10.1177/003591573102500132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wassmund M (1935) Lerhbuch der praktischen Chirurgie des Mundes, Leipzig, pp 67, 82
- 6.Sprawson E. C Proc R Soc Med. 1927;20:67. doi: 10.1177/003591572702001129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laskin DM. Oral and maxillofacial surgery. St. Louis: Mosby; 1985. [Google Scholar]
- 8.Pindborg JJ, Kramer IRH. Studies on odontogenic cyst epithelium. Acta Pathol Microbiol Scan. 1963;58:283. doi: 10.1111/j.1699-0463.1963.tb01572.x. [DOI] [PubMed] [Google Scholar]
- 9.Toller PA. New concepts of odontogenic cysts of the jaws. Oral Surg. 1972;1:3. doi: 10.1016/s0300-9785(72)80031-0. [DOI] [PubMed] [Google Scholar]
- 10.Kobler P. Razvoj karcinoma u radikularnoj cisti mandibule. Acta Stomatol Croat. 1979;13:68–72. [Google Scholar]
- 11.Kahairi A, Khan SA, Amirozi A. Endoscopic-assisted enucleation of radicular cysts: a case report. Malays J Med Sci. 2010;17(1):56–59. [PMC free article] [PubMed] [Google Scholar]
- 12.Kandhari A, Shenoi P. Surgical enucleation of radicular cyst using operating microscope: a case report & overview on use of microscope. Secr Message. 2009;4:64. [Google Scholar]
- 13.Santos TS, Karam FK. Excision of ranula using injection of hydrocolloid dental impression material. J Craniofac Surg. 2013 doi: 10.1097/scs.0b013e3182997cbb. [DOI] [PubMed] [Google Scholar]
- 14.Shira RB. Simplified technique for the management of mucoceles and ranulas. J Oral Surg Anesth Hosp Dent Serv. 1962;20:374Y379. [PubMed] [Google Scholar]
- 15.Ellis E, 3rd, Scott R, Upton LG. An unusual complication after excision of a recurrent mucocele of the anterior lingual gland. Oral Surg Oral Med Oral Pathol. 1983;56:467Y471. doi: 10.1016/0030-4220(83)90089-0. [DOI] [PubMed] [Google Scholar]
- 16.Santos TS, Martins Filho PRS, Menezes FS, et al. Surgical treatment of mucocele using Shira’s technique: case report. UFES Rev Odontol. 2008;10:53Y58. [Google Scholar]
- 17.Partsch K (1910) Zahncysten U: Scheff J. ur. Handbuch der Zahnheilkunde Holder, Wien und Leipzig