Abstract
Introduction
The diagnosis of zygomatic complex fractures is important in planning the treatment since the complex gives form to the projection, width and height of the midface.
Aim
This study was carried out to assess the diagnostic sensitivity and utility of high-resolution ultrasonography in comparison with conventional radiography in the diagnosis of the zygomatic complex fractures.
Materials and Method
Twenty-five cases of clinically diagnosed zygomatic complex fractures were subjected to conventional radiographs and USG study.
Results
The accuracy in terms of specificity and sensitivity of USG was comparable to conventional radiographs in the detection of the fractures of the zygomatic complex.
Conclusion
This study points to the suitability of USG as an alternative to the use of plain radiographs in the diagnosis of zygomatic complex fractures. USG is safe, inexpensive and an accurate adjunct to conventional radiography in diagnosis of zygomatic complex fractures.
Keywords: Zygomatic complex, USG, PNS, Submentovertex radiograph
Introduction
The zygomatic bone is a thick strong bone which forms the key to the structure of the anterolateral surface of the face [1]. The zygomatic complex plays an important role in the function and appearance of the facial skeleton. The prominent convex shape of the zygoma gives the contour of the cheek and makes it vulnerable to traumatic injury [2].
Owing to the articulation of the zygoma to surrounding bony structures, zygomatic complex fracture maybe associated with trauma to the orbital complex leading to either orbital blowout or blow-in fractures with associated complications. Depressed fractures of the zygomatic arch, in isolation or as a part of the fractured zygomatic complex, may impinge upon the coronoid process of the mandible, especially during mouth opening leading to restricted opening of the mouth [3]. The frequency of zygomatic complex fractures is about 45% and is second only to nasal fractures, amongst midface fractures [4].
The gold standard for preoperative imaging of patients with suspected midfacial fractures is three-dimensional imaging using computed tomography (CT), digital volume tomography or cone-beam computed tomography (CBCT). Currently, if there is the clinical suspicion of a midfacial fracture, conventional radiographs of the midface are indicated in order to confirm the diagnosis before three-dimensional imaging. Sonographic diagnosis may offer an alternative to radiology as a first-line imaging modality [5]. It can be considered as the imaging of choice when there is a contraindication to CT or plain films (for example, in pregnant women and patients with cervical spine injuries) or when there is an inaccessibility of CT scan in a primary healthcare set-up. When a trauma occurs, USG can be used to investigate potential fracture lines of the injured bone through a real-time examination [6].
Aim and Objective
The aim of the study was to estimate the diagnostic sensitivity and utility of high-resolution ultrasonography (HRUS) in comparison with conventional radiography in the diagnosis of the zygomatic complex fractures.
The main objective of this study was to evaluate the efficacy of ultrasonography in comparison with conventional radiography in the diagnosis of zygomatic complex fractures by a double blinded study and to explore the possibility of making USG examination a mainstay in the primary diagnosis of such fractures.
Materials and Method
This study was designed to specifically evaluate the efficacy of USG as a reliable imaging and diagnostic modality in diagnosing fractures of the zygomatic complex sustained due to a variety of aetiology.
This study was conducted in the Department of Oral and Maxillofacial Surgery, Vydehi Institute of Dental Sciences and Research Centre, Bangalore, India, with the approval of the ethical committee of the institution. Informed consent was obtained from all patients who participated in this study. The duration of the study was 2 years. Patients who were suspected to have sustained zygomatic complex fractures were included in this study.
A total of twenty-five patients were selected, irrespective of gender and age. The patients were subjected to ultrasonography (USG) examination of the zygomatic complex. Routine conventional radiographs, paranasal sinus radiograph (PNS) and submentovertex views (SMV), were taken. The USG findings were then compared with the findings in PNS and SMV.
Inclusion Criteria
Clinical diagnosis was of an isolated fracture of the zygomatic complex sustained due to trauma.
Both sexes of any age group were included in this study.
Exclusion Criteria
Patients with panfacial trauma/residual deformities/malunited fractures of the zygomatic complex.
Individuals of unsound mind/not capable of taking decisions themselves.
The protocol of this study included recommended imaging in the form of plain radiographs (PNS and SMV) (Figs. 1, 2). All cases were subjected to USG examination of the affected region using HD 15 Philips Healthcare. The equipment used a 7.5 MHz transducer (Fig. 3).
Fig. 1.

PNS view
Fig. 2.

Submentovertex view
Fig. 3.

USG machine
The sonography was subjected in frontozygomatic suture (FZ), infraorbital (IO) region, zygomatic arch (ZA) region and the zygomaticomaxillary buttress (ZB) region. Plain radiographs (paranasal sinus view/submentovertex views) obtained were interpreted by the radiologist and reviewed by the clinician. The sonologist was not shown the plain radiographs to eliminate bias.
Results
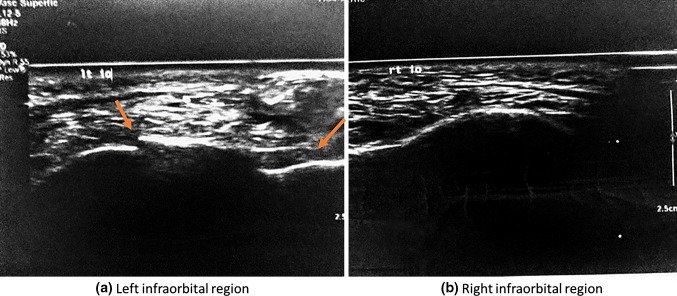
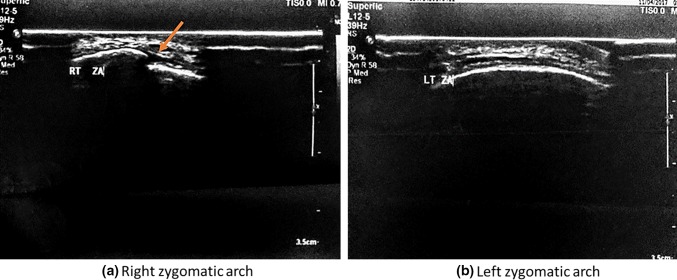
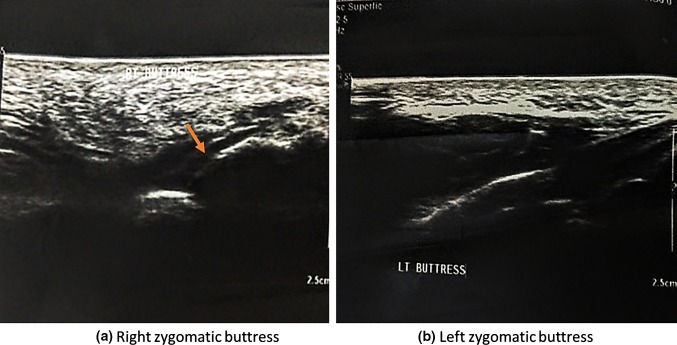
The sonography results in frontozygomatic suture (FZ) (Fig. 4a), infraorbital (IO) region (Fig. 5a), zygomatic arch (ZA) region (Fig. 6a) and the zygomaticomaxillary buttress (ZB) region (Fig. 7a) were compared using the unaffected side as the control (Figs. 4b, 5b, 6b, 7b) with conventional radiographs (PNS, SMV).
Fig. 4.
Discontinuity in the right FZ region, depicting a fracture
Fig. 5.
Discontinuity in the left IO region, depicting a fracture
Fig. 6.
Discontinuity in the right ZA region, depicting a fracture
Fig. 7.
Discontinuity in the right zygomatic buttress region, depicting a fracture
A total number of 25 patients with 26 zygomatic complex fractures were included in the study, and all patients were males (100%).
The age group involved in our study was 17–56 years. Three (12%) patients were less than 20 years of age, 13 (52%) patients were in the age group of 21–30 years, 5 (20%) patients were between the age group of 31–40 years, 2 (8%) were between the age group of 41–50 years and 2 (8%) patients were above the age of 50 years.
The data obtained were then subjected to McNemar’s statistical analysis.
Sensitivity and specificity analysis for estimating the accuracy of ultrasound scanning in detecting the different zygomatic complex fractures as compared to conventional radiographs is as shown in Table 1. The level of significance (p value) was set at p < 0.05.
Table 1.
Comparison of detection of zygomatic complex fractures by USG and conventional radiographs using McNemar’s test
| Location | Fracture | USG | CR | p value | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| FZ | No | 8 | 30.8 | 6 | 23.1 | 0.50 |
| Yes | 18 | 69.2 | 20 | 76.9 | ||
| IO | No | 4 | 15.4 | 3 | 11.5 | 1.00 |
| Yes | 22 | 84.6 | 23 | 88.5 | ||
| ZA | No | 5 | 19.2 | 4 | 15.4 | 1.00 |
| Yes | 21 | 80.8 | 22 | 84.6 | ||
| ZB | No | 9 | 34.6 | 10 | 38.5 | 1.00 |
| Yes | 17 | 65.4 | 16 | 61.5 | ||
In the comparison of detection of zygomatic complex fractures by USG and conventional radiographs, although there was a difference in the values, the significance was not statistically significant in the FZ group (p value 0.50) or in the IO, ZA and ZB groups (p value 1.00).
Discussion
Conventional radiographs are still the most frequently used modality in diagnosis. The advantages of X-rays are that they are widely available, can be specific for some diseases and can help in setting up and guiding a differential diagnosis and can also indicate the method for ascertaining an advanced imaging modality. However, such modalities come with their own limitations, such as being non-specific in many cases, superimposition of adjacent anatomic structures and radiopaque implants in the vicinity of the area of interest, which may produce artefacts in the resultant image. The film-based modality also provides only a two-dimensional representation of the fractures. In addition, radiation exposure to the patient is an important factor that needs to be considered [7].
Ultrasonography is a technique based on sound waves that acquires images in real time and without the use of ionizing radiation. The phenomenon perceived as sound is the result of periodic changes in the pressure of air against the eardrum. The periodicity of these changes lies anywhere between 1500 and 20,000 Hz. Ultrasound has a periodicity greater than the audible range. Diagnostic ultrasonography (sonography), the clinical application of ultrasound, uses vibratory frequencies in the range of 1–20 MHz [8]. Diagnostic USG has various modes, namely A-mode, B-mode, M-mode and D-mode. B-mode or brightness mode is important in diagnostic USG. It produces different scales of grey on the basis of different echogenicities of reflected waves. M-mode or motion mode is extremely valuable for accurate valuation of rapid movements. It has excellent temporal resolution. D-mode or Doppler mode is based on the Doppler effect, i.e. change in frequency (Doppler shift) caused by reciprocal movement of sound generator and observer [8].
In case of fracture, regular 4–12 MHz linear transducers are used in B-mode. The sound waves travel into the body and hit a boundary between soft tissue and bone. The high impedance difference between bone and soft tissue causes an almost complete reflection of the acoustic waves at the bone’s surface. The reflected waves are picked up by the probe and relayed to the machine, forming a two-dimensional image, thereby detecting a fracture.
Ultrasonography (USG) was first applied in the medical field in 1942 by Karl Theodore Dussik to visualize intracranial structures and was the first published work on medical ultrasonic. Ultrasound represented a major advance in diagnostic imaging because it allowed the creation of cross-sectional images without the use of ionizing radiation [9].
Ultrasound has traditionally been used to image irregularities of soft tissue and is used extensively for the examination of the abdomen and pelvis, and the soft tissues of the neck. Its role in maxillofacial surgery is less widely recognized [10]. The studies carried out towards the turn of the century were aided with better technology and software improvements and had started to reveal that USG imaging was in fact superior to conventional X-rays and even comparable to CT images in the diagnosis and intraoperative evaluation of maxillofacial in general and zygomatic complex fractures specifically with sensitivities ranging from 95 to 100% and specificity between 92 and 95% [11–13].
The use of high-resolution ultrasonography as a diagnostic tool for the detection of bone fractures has been established in various studies [2, 10–15]. The twenty-first century saw a dramatic increase in interest towards an enhanced role of USG in maxillofacial trauma with the intention of verifying and establishing the same as a first-line diagnostic modality as compared to conventional radiology and even CT. The numerous studies carried out soundly established the superiority of USG with curved array transducers and higher-resolution machines over the two routine modes with little or no side effects to the patient and the added advantages of providing real-time imaging and evaluation and ease of access [14].
Although there are limitations to the use of USG such as inability to delineate complex multiple facial fractures and malunited fractures, poor visualization of fracture lines in cases of facial oedema and empyema, and difficulty in placement of probe in areas of soft tissue injury which may cause pain and discomfort to the patient, along with the need for operator skill and expertise, USG being an inexpensive, quick and non-invasive imaging modality can provide several advantages especially when there is a contraindication to CT or plain films (for example, in pregnant women and patients with cervical spine injuries) or in a primary healthcare set-up when there is an inaccessibility of CT machine. It can be used to investigate potential fracture lines of the injured bone through a real-time examination.
Zygomatic complex fractures have changed in patterns of occurrence, severity and, more importantly, in the mode of injury. Protection of the globe and maintaining the width of the face are the more important roles of the complex. Diagnosis and treatment planning of such fractures become imperative in the sequencing of repair whether and where indicated, especially in the case of isolated zygomatic complex fractures [14].
In 2010, Nezafati et al. conducted a study in a series of 17 patients to evaluate the efficacy of USG in fracture detection of the zygomatic arch. They found that ultrasound was accurate in assessing the fractured arches with sensitivity of 88.2% (15 of the 17 patients, with two false negatives) and specificity of 100% (no false positives), concluding that ultrasound is accurate in the visualization of zygomatic arch fractures, and they postulated that USG can be used as an adjunct to plain films to reduce the overall radiation exposure. Thus, USG is a reliable diagnostic tool for the evaluation of zygomatic arch fractures [15].
In our series, it was noted that the sensitivity of USG in detecting FZ fracture was 90% and specificity of 100% as compared to that of conventional radiographs which was contradictory to the study carried out by Ogunmuyiwa et al. [2] which reported a sensitivity of only 25%.
The infraorbital region evaluation revealed statistical significance in favour of USG with a p value < .001 and a sensitivity of 95.6%. These findings were also corroborated by earlier studies carried out by McCann et al. [10], Ogunmuyiwa et al. [2] and Menon et al. [14].
In our study, the sensitivity of USG in detecting zygomatic arch fractures was 95.5% with a p value of < .001. These results were similar to the results of the studies carried out by Blessman et al. [5] who shared a similar experience but experienced better and more specific results with displaced fractures as compared to undisplaced fractures. The results were closely similar to those achieved by Ogunmuyiwa et al. [2] and Nezafati et al. [15].
The sensitivity of USG in detecting fractures of the zygomaticomaxillary buttress was 100% and specificity was 90% with a p value of < 0.001 which again shows that USG is far more sensitive and specific in this area of the facial bony architecture than conventional radiographs.
Conclusion
If ultrasound is performed as the first imaging modality in cases of suspected zygomatic complex fractures by an experienced investigator, the visualization of fracture lines can avoid conventional imaging.
This study points to the suitability of USG as an alternative to the use of plain radiographs in the diagnosis of zygomatic complex fractures especially when there is an unobtainability of CT scan in a primary healthcare set-up or places where CT is not accessible.
In a nutshell, ultrasound is safe, inexpensive and an accurate adjunct to conventional radiography in diagnosis of zygomatic complex fractures.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
Ethical clearance was obtained from the ethical committee of Vydehi Institute of Dental Sciences and Research Centre, Bangalore. All investigations performed in the study were in accordance with the ethical standards of the institution.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Priyangana Nath, Email: priyangana17@gmail.com.
Suresh Menon, Email: psurmenon@gmail.com.
A. Suresh, Email: majorasuresh@gmail.com
S. Archana, Email: archana.dr.s@gmail.com
References
- 1.Williams JL, Rowe NL (1994) Rowe and Williams’: maxillofacial injuries. volume I: 25–26, 157–284
- 2.Ogunmuyiwa SA, Fatusi OA, Ugboko VI, Ayoola OO, Maaji SM. The validity of ultrasonography in the diagnosis of zygomaticomaxillary complex fractures. Int J Oral Maxillofac Surg. 2012;41:500–505. doi: 10.1016/j.ijom.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Thiagarajan B, Narashiman S, Arjunan K. Fracture zygoma and its management our experience. Otolaryngol J. 2013;3(1.5):1–17. [Google Scholar]
- 4.Chattopadhyay PK, Chander M. Management of zygomatic complex fracture in armed forces. Med J Armed Forces India. 2009;65(2):128–130. doi: 10.1016/S0377-1237(09)80124-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blessmann M, Pohlenza P, Blake FAS, Lenard M, Schmelzle R, Heiland M. Validation of a new tool for ultrasound as a diagnostic modality in suspected midfacial fractures. Int J Oral Maxillofac Surg. 2007;36:501–506. doi: 10.1016/j.ijom.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Evirgen S, Kamburoğlu K. Review on the applications of ultrasonography in dentomaxillofacial region. World J Radiol. 2016;8(1):50–58. doi: 10.4329/wjr.v8.i1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reddy VK, Shaik M, Sasthrulu G. Ultrasonography in zygomatic arch fractures. Int J Recent Sci Res. 2016;7(6):12102–12105. [Google Scholar]
- 8.Singh GP, Dogra S, Kumari E. Ultrasonography: maxillofacial applications. Ann Dent Spec. 2014;2(3):104–107. [Google Scholar]
- 9.Mohan KR, Rao NK, Krishna GL, Kumar VS, Ranganath N, Lakshmi UV. Role of ultrasonography in oral and maxillofacial surgery: a review of literature. J Maxillofac Oral Surg. 2015;14(2):162–170. doi: 10.1007/s12663-014-0616-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCann PJ, Brocklebank LM, Ayoub AF. Assessment of zygomatico-orbital complex fractures using ultrasonography. Br J Oral Maxillofac Surg. 2000;38(5):525–529. doi: 10.1054/bjom.2000.0501. [DOI] [PubMed] [Google Scholar]
- 11.Piette E, Lenoir JL, Reychler H. The diagnostic limitations of ultrasonography in maxillofacial surgery. J Cranio Max Fac Surg. 1987;15:297–305. doi: 10.1016/S1010-5182(87)80075-6. [DOI] [PubMed] [Google Scholar]
- 12.Akizuki H, Yoshida H, Michi K. Ultrasonographic evaluation during reduction of zygomatic arch fractures. J Cranio Maxillofacial Surg. 1990;18(6):263–266. doi: 10.1016/S1010-5182(05)80428-7. [DOI] [PubMed] [Google Scholar]
- 13.Hirai T, Manders EK, Nagamoto K, Saggers GC. Ultrasonic observation of facial bone fractures. JOMS. 1996;54:779–780. doi: 10.1016/s0278-2391(96)90703-x. [DOI] [PubMed] [Google Scholar]
- 14.Menon RP, Chowdhury SK, Semi RS, Gupta V, Rahman S, Balasundaram T. Comparison of ultrasonography with conventional radiography in the diagnosis of zygomatic complex fractures. J Craniomaxillofac Surg. 2016;44:353–356. doi: 10.1016/j.jcms.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 15.Nezafati S, Javadrashid R, Rad S, Akrami S. Comparison of ultrasonography with submentovertex films and computed tomography scan in the diagnosis of zygomatic arch fractures. Dentomaxillofacial Radiol. 2010;39:11–16. doi: 10.1259/dmfr/97056817. [DOI] [PMC free article] [PubMed] [Google Scholar]