Introduction
Endonasal approach for frontal sinus pathology has become the gold standard for sinus surgery. However, cases recurrent and refractory to functional endoscopic sinus surgery (FESS) need to be dealt with conventional (open) techniques.
Mucoceles of the paranasal sinuses are “benign, chronic, expanding lesions, filled with sterile mucus and epithelial cells” [1]. The term “Mucocele” was coined by Rollet in 1896. Mucoceles of paranasal sinuses were first described by Langenback [2].
Mucoceles are caused by obstruction of the sinus ostium leading to accumulation of the mucous secretion within the sinus [3]. The two most frequent causes of frontal sinus mucoceles are trauma and inflammation [1]. An infected mucocele is termed a mucopyocele. They behave like expansile cystic lesions, eroding the surrounding bone and displacing the adjacent structures, even extending intracranially. Signs and symptoms include frontal pain, swelling, exophthalmos, diplopia and loss of vision [4]. Erosion of posterior table may lead to meningitis, meningoencephalitis, pneumocephalus, brain abscess, seizures or CSF fistulas [5].
The diagnosis of mucocele is based on clinical examination along with computed tomography (with contrast) or MRI [4].
The mainstay of management of mucocoeles is surgery, which ranges from functional endoscopic sinus surgery to craniotomy, and craniofacial exposure, with or without obliteration of the sinus [6]. Endoscopic procedures rely on establishing surgical drainage of the frontal sinus and marsupialization, whereas open techniques when employed are most frequently used for sinus obliteration.
We present two cases of frontal mucopyoceles refractory to endoscopic approach managed by external sinus surgery.
Case Reports
Case 1
A 58-year-old female, presented with right frontotemporal headache for 5 years and nasal obstruction since 6 months. There was no contributory ophthalmological history. The CT scan revealed a collection in the right frontal sinus with thickening of the sinus mucosa completely obstructing the ostium (Fig. 1). Since the patient had undergone endoscopic sinus surgery unsuccessfully multiple times, conventional (open) technique was opted for. A gull wing incision combined with endoscopic transillumination was performed to locate and expose the frontal sinus (Fig. 2). Osteoplastic flap made with beveled osteotomy cuts was raised. The sinus lining was completely enucleated and sinus obliterated using abdominal fat (Fig. 3). Osteoplastic flap was repositioned and secured to the frontal bone using miniplates (Fig. 4). The patient was followed up for over 2 years, and she remained asymptomatic.
Fig. 1.

Coronal section of CT scan showing collection in the right frontal sinus with complete obstruction of the ostium
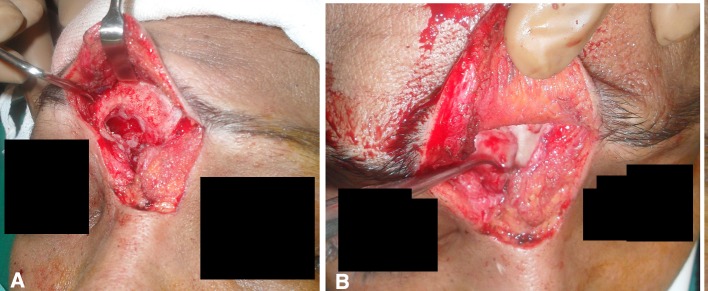
Fig. 2.

Transillumination technique to locate the frontal sinus
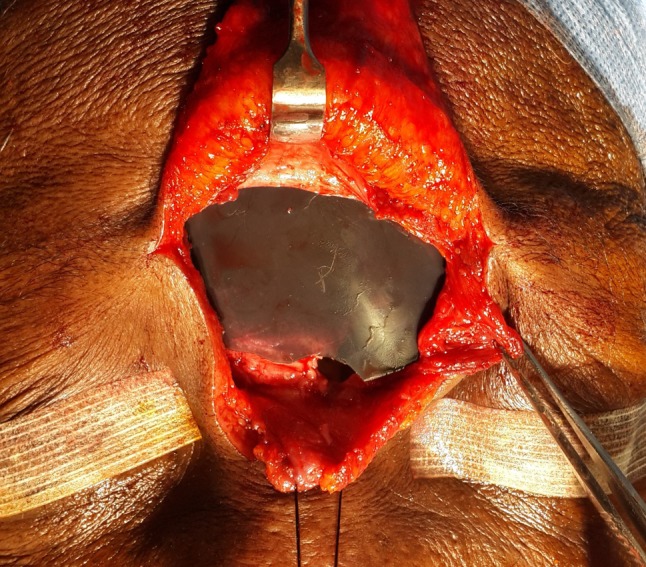
Fig. 3.
a Exposed frontal sinus after raising osteoplastic flap. b Complete enucleation of right frontal sinus
Fig. 4.
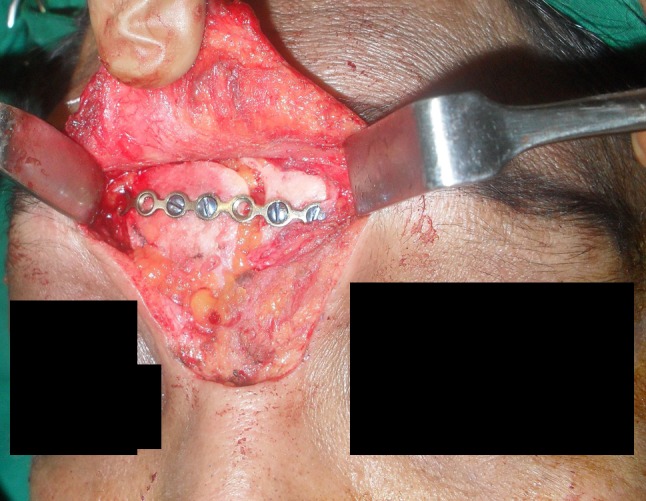
Sinus obliterated using abdominal fat and osteoplastic flap repositioned using miniplate
Case 2
A 55-year-old female presented with recurrent pain and swelling over the left frontal sinus region since 2 years. There was history of fever, nasal obstruction and headache since a week. Patient had undergone balloon sinuplasty for the same a year ago. A soft fluctuant mass over the left frontal sinus region with mild ptosis of left eye was noted. No other ophthalmologic abnormalities were seen. CT scan showed homogenous soft tissue opacity in left frontal sinus, with erosion of posterior table (Fig. 5). Axial sections revealed a very thin layer of bone (< 1 mm) between the sinus pathology and intra cranial contents. A diagnosis of recurrent mucopyocele was made. A gull wing approach was used to expose the fronto-nasal region followed by sinus mapping using a cut-out from radiographic film (Fig. 6). Once identified, further dissection was done to discover a defect of the anterior table through which purulent material was drained (Fig. 7). Mucosal lining of the frontal sinus was enucleated. A small dural tear noted intraoperatively was sealed using fibrin glue. Sinus obliteration was done using abdominal fat graft. Lastly, procerus muscle flap was used to close the anterior aspect of sinus (Fig. 8). Patient was followed up for 6 months and remained asymptomatic.
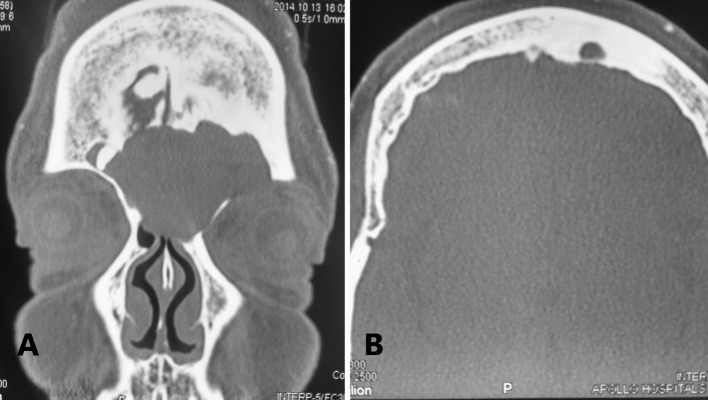
Fig. 5.
a Coronal CT showing homogenous soft tissue opacity in left frontal sinus with expansion. b Axial section showing erosion of posterior table in region of left frontal sinus
Fig. 6.
Sterile X-ray being used to map the sinus
Fig. 7.
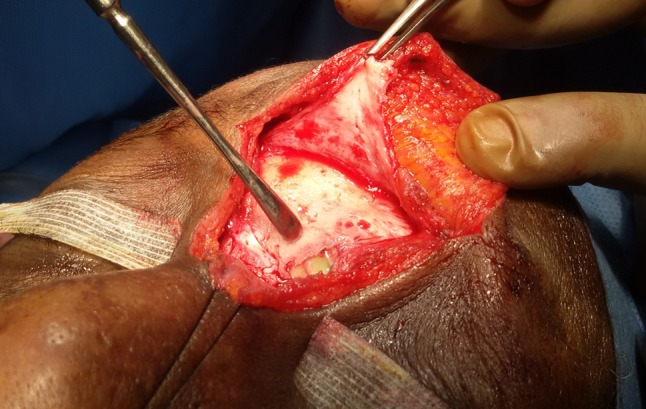
Defect in anterior table of left frontal sinus
Fig. 8.

Procerus muscle flap used to cover the anterior defect
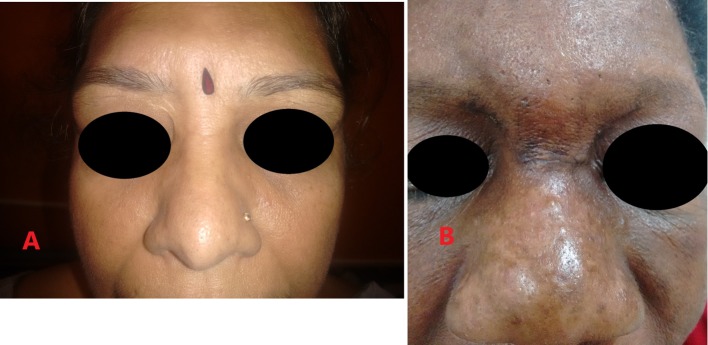
The scar was well hidden in the naso-orbital valley and eyebrow region for both patients (Fig. 9).
Fig. 9.
a Follow-up of Case 1: 2 years after surgery; note the inconspicuous scar. b Follow-up of Case 2: 6 months after surgery; note the blending of scar within natural creases
Discussion
Approximately 60–89% of mucoceles occur in the frontal sinus [7]. Frontal sinus mucoceles can occur at any age in either gender. Most are seen between the fourth and seventh decades of life [8]. The principles of treatment include sanitation of the mucocele with prevention and management of possible intracranial or intraorbital complications, drainage of the mucocele into the nose, either by preservation or extension of the natural nasofrontal duct. Failing this, the aim is to completely remove the mucocele and the mucosa of the frontal sinus and reliable closure of the nasofrontal duct—ideally by obliteration of the sinus. Preservation or reconstruction of the anterior wall of the frontal sinus to maintain the contour of the forehead is of paramount importance [1].
Endoscopic approach is advocated as the treatment of choice for paranasal pathologies, as it aims at preserving the physiology of sinus mucosa and maintaining a patent drainage pathway. It is also associated with lesser morbidity and leaves no facial scar [9]. The most accepted and widely used endoscopic procedures are Draf and nasofrontal approaches and modified hemi-Lothrop, the modified mini-Lothrop and the modified subtotal-Lothrop procedures [10].
One of the significant complications of FESS is stenosis of the widened ostium. It is seen that stenosis of 50–60% occurs in 30–40% of the patients, requiring revision [11]. Re-stenosis is one of the main causes of recurrence. Here, open techniques are a good fallback option.
Advantages of open sinus surgeries are:
Direct visualization and access.
Adequate instrumentation.
Dural exposure can be detected and managed well under direct visualization.
Less chances of scarring and stenosis of drainage tract.
The commonly used open techniques are frontal trephination, external frontoethmoidectomy and the frontal osteoplastic flap. Trephination is used where effective drainage is expected. The external frontoethmoidectomy is almost obsolete due to high rates of obstruction of the nasofrontal outflow tract. The osteoplastic flap with fat obliteration remains the procedure of choice in case of salvage procedures and traumatic deformities [12]. Obliteration of the nasofrontal duct aims to prevent an ascending frontal sinus infection and prevent the growth of the nasal mucosa upward into the frontal sinus [1].
In both of our cases, we obliterated the sinus along with the frontonasal outflow tract using abdominal fat. The scars were faint and well hidden in 6 months.
Conclusion
The first line of treatment for most frontal mucopyoceles is endoscopic marsupialization and establishment of drainage. However, iatrogenic injury to the outflow tract, postoperative healing/fibrosis or the nature of the pathology itself can lead to recurrences which cause much harassment to the patient. It is in these situations, conventional open transfacial techniques play an important role in salvage surgery.
Funding
This research did not receive any specific Grant from funding agencies in the public, commercial or not-for-profit sectors.
Compliance with Ethical Standards
Conflict of interest
The author declares that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Constantinidis J, Steinhart H, Schwerdtfeger K, et al. Therapy of invasive mucoceles of the frontal sinus. Rhinology. 2001;39:33. [PubMed] [Google Scholar]
- 2.Aslan G, Ugur MB, Bassullu M. Giant mucocele originating from the middle concha in a 5-year-old child: a case report. J Med Case Rep. 2013;7:246. doi: 10.1186/1752-1947-7-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fernandes R, Pirgousis P. Longstanding giant frontal sinusmucocele resulting in extraaxial proptosis orbital displacement and loss of vision. J Oral Maxillofac Surg. 2010;68:3051. doi: 10.1016/j.joms.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 4.Park C, Stoffella E, Gile J, et al. Osteoplasty flap technique for repair of latent (30-year) post-traumatic frontal sinus mucocele: case report and review of the literature. J Oral Maxillofac Surg. 2012;70:2092. doi: 10.1016/j.joms.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 5.Mourouzis C, Evans B, Shenouda E. Late presentation of a mucocele of the frontal sinus: 50 years postinjury. J Oral Maxillofac Surg. 2008;66:1510. doi: 10.1016/j.joms.2007.12.031. [DOI] [PubMed] [Google Scholar]
- 6.Galiè M, Mandrioli S, Tieghi R, Clauser L. Giant mucocele of the frontal sinus. J Craniofac Surg. 2005;16:933–935. doi: 10.1097/01.scs.0000168999.20258.ca. [DOI] [PubMed] [Google Scholar]
- 7.Arrue P, Kany MT, Serrano E, Lacroix F, Percodani J, Yardeni E, et al. Mucoceles of the paranasal sinuses: uncommon location. J Laryngol Otol. 1998;112:840–844. doi: 10.1017/S0022215100141854. [DOI] [PubMed] [Google Scholar]
- 8.Lai PC, Liao SL, Jou JR, et al. Transcaruncular approach for the management of frontoethmoid mucoceles. Br J Ophthalmol. 2004;88:725. doi: 10.1136/bjo.87.6.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martel-Martín M, Gras-Cabrerizo JR, Bothe-González C, Montserrat-Gili JR, De JuanDelago M, Massegur-Solench H. Clinical analysis and surgical results of 58 paranasal sinus mucoceles. Acta Otorrinolaringol Esp. 2015;66:92–97. doi: 10.1016/j.otorri.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Eloy JA, Vazquez A, Liu JK, Baredes S. Endoscopic approaches to the frontal sinus modifications of the existing techniques and proposed classification. Otolaryngol Clin N Am. 2016;49:1007–1018. doi: 10.1016/j.otc.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 11.Tran KN, Beule AG, Singal D, Wormald PJ. Frontal ostium restenosis after the endoscopic modified lothrop procedure. Laryngoscope. 2007;117(8):1457–1462. doi: 10.1097/MLG.0b013e31806865be. [DOI] [PubMed] [Google Scholar]
- 12.Lawson W, Ho Y. Open frontal sinus surgery a lost art. Otolaryngol Clin N Am. 2016;49:1067–1089. doi: 10.1016/j.otc.2016.03.027. [DOI] [PubMed] [Google Scholar]