Highlights
-
•
WHO published draft Target Product Profiles (TPPs) for Rift Valley Fever virus (RVFV) vaccines.
-
•
The TPPs contain restrictive requirements aimed at reducing the risk of genetic reassortment.
-
•
We find no evidence for reassortment despite use of live RVFV vaccines.
-
•
If genetic reassortment occurred with wild-type RVFV it would be of no consequence.
The hypothetical risks of reassortment do not outweigh the benefits of vaccination
Keywords: Rift Valley Fever vaccine, Target Product Profile, Genetic reassortment
Abstract
In November 2019, The World Health Organization (WHO) issued a draft set of Target Product Profiles (TPPs) describing optimal and minimally acceptable targets for vaccines against Rift Valley fever (RVF), a Phlebovirus with a three segmented genome, in both humans and ruminants. The TPPs contained rigid requirements to protect against genomic reassortment of live, attenuated vaccines (LAVs) with wild-type RVF virus (RVFV), which place undue constraints on development and regulatory approval of LAVs. We review the current LAVs in use and in development, and conclude that there is no evidence that reassortment between LAVs and wild-type RVFV has occurred during field use, that such a reassortment event if it occurred would have no untoward consequence, and that the TPPs should be revised to provide a more balanced assessment of the benefits versus the theoretical risks of reassortment.
1. Introduction
On 5 November 2019, WHO issued a draft set of Target Product Profiles (TPPs) describing optimal and minimally acceptable targets for vaccines against Rift Valley fever (RVF) in both humans and ruminants (https://www.who.int/news-room/articles-detail/rift-valley-fever-vaccines-target-product-profile). RVF is on WHO’s Blueprint list of priority diseases with epidemic potential for which there are no or insufficient, countermeasures available. As will be described below, currently there are approved and investigational RVF live, attenuated vaccines (LAVs) for veterinary use. Only one investigational RVF LAV has so far been tested in humans, but promising new LAVs are in preclinical development.
Two sets of TPPs, one for human and one for veterinary vaccines, were provided by WHO for public comment. Both the human and veterinary TPPs have many features in common, and both contain rigid requirements to protect against genomic reassortment of LAVs with wild-type RVF virus (RVFV). We believe the draft TPPs place undue constraints on development and regulatory approval of LAVs and need to be revised to provide a more balanced assessment of the benefit:risk equation.
The WHO draft TPPs contain the following statements in the Safety sections of the document:
Veterinary vaccines. “Live attenuated virus vaccines are not to be used for vaccination of potentially viraemic animals during an outbreak of RVFV, given their potential to reassort with wild type virus” (applies to both optimal and minimally acceptable profiles).
Human vaccines. “No live attenuated virus vaccine to be used unless reassorting is excluded (optimal)”, or “Usage of an attenuated live vaccine that may allow reassortment is not indicated in an outbreak setting” (minimal acceptable profile).
In support of these criteria, the WHO Background section states that reassortment of the segmented genome of RVF LAVs is possible on theoretical grounds. As evidence of a safety concern, a single example is cited: “Specifically, reassortment in a man who was co-infected with a wild-type strain and a live-attenuated vaccine strain has been reported [1].” An alternative source indicates the patient was female and had a significant illness from which she fully recovered (R. Swanepoel, pers. comm., 2019). However, the sequence of the isolate (SA184/10) from the patient has been re-evaluated by full genomic sequencing and found not to be a reassortant [2]; the patient likely had a wild-type RVFV infection.
The benefits of a LAV for prevention and control of RVF outbreaks clearly outweigh the theoretical risk of reassortment, which has not been demonstrated to be a safety problem despite marketing of two RVFV LAVs and several others in development. Safety of new vaccines must be determined in suitably powered trials for licensure and thereafter by post-marketing surveillance. Theoretical safety risks, such as that posed by reassortment, can be addressed through vaccine design and experimental studies. However, since the possibility of recombination is a basic attribute of any replicating vaccine virus, and reassortment is a basic attribute of replicating vaccine viruses with segmented genomes, theoretical risks should not be a priori restrictions on use of vaccines otherwise shown to be safe and effective.
The following commentary first deals with the LAV question, and then specifically with the RVF vaccines intended for veterinary and human use.
2. Live, attenuated Rift Valley fever vaccines in use and in development
Table 1 provides a summary of the RVF LAVs that are in use or in development. These are described in more detail below.
Table 1.
Live, attenuated replication competent RVFV vaccines in use or in development.
| Vaccine | Derivation/Basis for attenuation | Marketing/Usage | Target indication | Adverse effects and other potential concerns | Evaluated for human use | Characteristics reducing risk of reassortment |
|---|---|---|---|---|---|---|
| Smithburn Neurotropic Strain (SNS) | Derived by empirical passage/ Not defined | Onderstepoort Biological Products (OBP) and (intermittently) other manufacturers (Egypt, Kenya)/50 years use in parts of Africa | Adult, (non-pregnant) ruminants |
|
No | |
| Clone-13 | Derived by empirical passage/ Internal deletion of 569 nucleotides in NSs | OBP/Africa since 2010 | Ruminants |
|
No | No detectable viremia (ruminants) below threshold for mosquito infection |
| MP-12 | Derived by passage with chemical mutagenesis/ Multiple attenuating mutations in all 3 segments. | Zoetis/Conditionally licensed for use in U.S. | Ruminants, humans |
|
Phase I-II trials with promising results | Low viremia in ruminants and humans, below threshold for mosquito infection |
| MP-12-NSm-del | Derived by reverse genetics/ Deletion of NSm plus MP-12 attenuating mutations. | M.C.I Santé Animale/in development | Ruminants | None reported | No | No detectable viremia in ruminants. Not infectious for mosquitoes. |
| ΔNSs-ΔNSm rRVFV (DDVax™) | Derived by reverse genetics. Deletion of NSs and NSm | In development | Humans, ruminants | None reported | In development | No detectable viremia in ruminants. Not infectious for mosquitoes. |
| RVFV-4s | Derived by reverse genetics/ Split M segment, 4 segments, NSs deletion. | In development | Humans, Ruminants | None reported | In development | No detectable viremia in ruminants. |
2.1. Smithburn Neurotropic vaccine
The first and oldest LAV is the Smithburn Neurotropic Strain (SNS) that has been used for over 50 years in parts of Africa. While the SNS vaccine is still in use in countries where RVF outbreaks have occurred in the past, concerns remain about safety and efficacy, consistency of manufacture, vaccine stability, inadequate timeliness and coverage of vaccination before and during epizootics. This experience, which is informed by the history of attenuating passages and inability to adequately control the balance of attenuation and virulence, supports development and introduction of improved vaccines and improved policies for their use.
SNS has been used exclusively for immunization of ruminants and has not been tested in humans because it is abortigenic in ruminants and retains neurovirulence for nonhuman primates. The SNS vaccine originated by serial passage of a RVFV strain isolated from mosquitoes in Uganda in 1944 in mouse brains [3]. It underwent additional serial passages in mouse brain and in embryonated duck eggs by yolk sac inoculation, with initial commercial lots of ‘avianized’ vaccine produced in the early 1950s [4]. Subsequently, virus at mouse brain passage level 102 followed by 54 passes in duck embryos and a further 16 passages in mouse brains was used to prepare commercial vaccine (10% freeze-dried mouse brain suspension) until 1958 when new lots were prepared in mouse brain tissue directly from mouse passage 102 virus (without duck embryo passage). Since 1971, vaccine has been produced in continuous BHK-21 baby hamster kidney cells infected with mouse brain passage 102 and marketed by Onderstepoort Biological Products (OBP). It is recommended for use in healthy adult animals only and is not safe for pregnant animals. An inactivated vaccine, based on an adjuvanted, formalin-inactivated virulent strain of RVFV, is also marketed by OBP. This vaccine may be applied to animals during all physiological stages, including pregnancy, but repeated vaccinations are required for optimal efficacy. Although both these classical vaccines have proven valuable in controlling RVF in endemic/enzootic areas, a vaccine that combines the efficacy of the live vaccine with the safety of the inactivated vaccine would be extremely valuable.
Because of the safety issues surrounding the SNS LAV in ruminants, newer candidates have been developed, as described below. The goal of new vaccines has been to improve the safety profile, while retaining the advantages of LAVs (single dose, rapid onset of protection, and durability of immunity).
In considering these vaccines, it is important to separate the safety concerns related to abortion, congenital infection, and transmissibility (mosquito infection) from those related to genetic reassortment. Vaccines should be demonstrably safe and effective with no documented adverse events consistent with the severity of natural disease.
Clone-13. Live and inactivated SNS vaccines remained the only registered veterinary countermeasures available in some African countries for decades until the introduction of Clone 13 in 2010 by OBP. This attenuated strain, originally described by Muller et al. contains a spontaneous large internal deletion of 549 nucleotides that removes 69% of the open reading frame of NSs that occurred during serial passage of a virulent isolate of RVFV [5]. NSs is a non-structural protein of RVFV and has been determined to be the major virulence determinant counteracting host innate immune responses [6], [7]. Clone 13 does not induce detectable viremia and has been tested in cattle, sheep and goats in large open field trials in Kenya and the data indicated that it was safe [8]. A large open field study in pregnant sheep and goats was also performed in Senegal, and no evidence of the vaccine causing abortions was found [9]. However, a subsequent experimental study showed that Clone 13 was associated with fetal malformations and less frequently, stillbirths [10]. The virus is capable of infecting mosquitoes experimentally, but transmission efficiency is low [11]. Since Clone 13 does not induce detectable viremia in the target species for vaccination, the chance of transmission from vaccinated animals to mosquitoes is considered negligible. Clone-13 has not been evaluated for human vaccination.
MP-12. MP-12 is another LAV vaccine for the prevention of RVF that was first developed by the US Army Medical Research Institute of Infectious Diseases (USAMRIID) for human use by a process of chemical mutagenesis. The vaccine is under development by the Sabin Vaccine Institute, Washington DC. MP-12 vaccine is conditionally licensed by the US Department of Agriculture (USDA) for veterinary use in the U.S. MP-12 is attenuated based on multiple (23) single nucleotide permutations (SNP) on all three RNA segments, L, M and S. For this reason, the potential for reversion to virulence by reassortment with wild-type RVFV is minimized or precluded since acquisition of one or more wild-type segments by the vaccine virus would be attenuated by mutations in the remaining gene(s). There is no evidence at all that a “novel” strain with increased virulence or tropism would emerge from such an event. MP-12 has been clinically tested in over 90 human volunteers and found to rapidly elicit neutralizing antibody titers that lasted over 5 years with minimal or absent viremia, genetic stability in vivo, and no significant adverse effects [12], [13]. The vaccine is similarly effective in protecting laboratory animals (including nonhuman primates), and livestock against virulent RVFV challenge [14]. Morrill demonstrated that pregnant sheep vaccinated with MP-12 were protected against challenge using virulent RVF virus, and that blood from newborn lambs was free of RVFV neutralizing antibody, indicating that transplacental infection had not occurred. However lambs born to vaccinated ewes gained protective antibody after the first nursing from maternal colostrum [15]. There is a single, unsubstantiated report of abortion in sheep associated with MP-12 [16], but multiple other studies showed no safety signals in pregnant sheep or cows [15], [17], [18], [19]. MP-12 can infect mosquitoes experimentally, but transmission is considered to be excluded based on the absent or minimal viremia observed in ruminants and humans [20].
MP-12-NSm-del. Won et al. used reverse genetics to modify MP-12 by deleting a region of the open reading frame encoding the non-structural protein, NSm and observed that the resulting virus replicated in vitro equally well as the parental MP-12 [21]. Deletion of the NSm virulence factor is combined with attenuating mutations on all three segments of MP-12, and would retain an attenuated phenotype even if reassortment with wild-type virus reconstituted the NSm gene. Morrill et al. showed that vaccination of sheep and calves with MP-12-NSm-del resulted in RVFV neutralizing antibodies levels comparable to MP-12 [22], [23]. The vaccine was then tested in goats, sheep and calves in Tanzania and Morocco and found to induce antibodies that neutralized MP-12 and presumably virulent RVFV as well. The level of response was slightly lower than tests using animals from North America, but still reached what is believed to be protective titers [24], [25]. The deletion of NSm precludes infection of mosquito vectors. The vaccine is in advanced development for veterinary indications by M.C.I Santé Animale, Mohammedia, Morocco.
2.2. Recombinant live, attenuated RVF vaccines containing complete deletion of NSs or both NSs and NSm
Bird et al. used reverse genetics to develop a recombinant RVFV, containing the deletion of the NSs gene alone (ΔNSs rRVFV) or the NSs/NSm genes in combination, ΔNSs-ΔNSm rRVFV (DDVax™), which contains complete gene deletions of the two known virulence factors, the NSs and NSm genes [26], [27]. NSs and NSm are not required in cell culture for efficient virus replication, assembly, or maturation. Both candidates were highly attenuated, immunogenic, and efficacious in a rat model and in sheep with no detectable post-vaccination viremia. The vaccine was not teratogenic in pregnant sheep. Both vaccines were immunogenic and protective in non-human primates [28]. The attenuating deletions in two RNA segments reduces the likelihood of reversion to virulence by reassortment with wild-type virus. The NSm deletion alone renders the vaccine incapable of infecting mosquitoes in experimental studies [29]. The vaccine was originally constructed by the Centers for Disease Control and is now being developed by Colorado State University and the University of California, Davis with the goal of human testing.
2.3. Four segmented RVFV (RVFV-4s)
The most recently developed live-attenuated RVF vaccine was created by splitting the M genome segment into two M-type segments [30]. The resulting vaccine virus depends on the co-packaging of 4, instead of the naturally occurring 3 genome segments and lacks the NSs gene. The split M genome segment and the NSs deletion were shown to independently render the virus non-virulent. The resulting vaccine was shown to be safe for mice, young lambs, pregnant sheep, goats, cattle and marmosets and to provide sterilizing immunity after a single vaccination of mice, sheep, goats and cattle. (manuscript in preparation and [31], [32]). Complete absence of viremia in all evaluated species, even after application of an overdose, underscores that risks of genetic reassortment or transmission of the vaccine via mosquitoes are negligible. The vaccine is being developed by Central Veterinary Institute, Wageningen Bioveterinary Research, The Netherlands, with the goal of human testing.
3. Theoretical reassortment risk assessment
3.1. What is the evidence for reassortment of vaccine viruses, in general?
In 2003 and 2013, the WHO convened informal consultations on characterization and quality aspects of vaccines based on live virus vectors; representatives from all major regulatory authorities participated. One concern that emerged was that recombination of a live virus-vectored vaccine with a circulating or reactivated latent virus could theoretically generate a more pathogenic strain.
To follow up on this report, the Brighton Collaboration (a global, non-profit, scientifically independent, group created for the purpose of providing reliable, high quality international information and guidelines relevant to vaccine safety) charged a working group to explore the relevance of recombination to vaccine safety. The working group findings in 2016 [33] considered examples of, and risks attributed to recombination and reassortment of traditional LAVs and novel, chimeric vectored vaccines. All extant examples of such interactions were cited.
One important conclusion of this search for examples of recombination is that they have rarely occurred, and have had limited consequences, considering the long history of use of LAVs (Table 2). Interestingly, genomic recombination of LAVs and wild-type viruses has actually occurred more frequently with single-stranded RNA viruses than with viruses having segmented genomes. LAVs against segmented viruses have been developed or commercialized for veterinary use (RVFV, bluetongue [34], African horsesickness [35], canine influenza [36], and for human use [influenza [37] (US and Russian commercial vaccines)]. Unlike RVFV which consists of a single virus, some LAVs, such as African horsesickness and bluetongue are formulated with multiple distinct serotype viruses; reassortment between vaccine strains has been associated with either reversion to virulence or no phenotypic change [38], [39], [40], [41]. It is relevant to note that FDA labeling of live influenza vaccine (FluMist®), containing four genetically engineered influenza strains, does not contain precautions for reassortment.
Table 2.
Examples of recombination or reassortment of live attenuated vaccines and wild-type viruses.
| Live, attenuated vaccine | Target species | Genome type | Vaccine and Recombination event | Estimated frequency | Recombination mechanism | Phenotypic change | Clinical relevance | Epidemiological relevance |
|---|---|---|---|---|---|---|---|---|
| Segmented genome viruses | ||||||||
| African horsesickness | Horses | Reoviridae, orbivirus, 9 serotypes, double-strand RNA, 10 segments | Reassortants with individual genome segments derived from multiple different virus types present in the trivalent vaccine | 3 reported outbreaks caused by distinct reassortant viruses | Reassortment | Increased virulence | Hemorrhagic disease, possibly lower case-fatality | Three outbreaks in Cape Province, South Africa |
| Bluetongue | Sheep, cattle | Reoviridae, orbivirus, 26+ serotypes, double-strand RNA, 10 segments | Three pentavalent vaccines in three sequential inocula: (1) serotypes 1, 4, 6, 12, and 14; (2) serotypes 3, 8, 9, 10, and 11; and (3) serotypes 2, 5, 7, 13, and 19. Reversion or reassortment of LAV vaccine strains and between LAV and wild-type virus | Several reports | Reassortment of LAV vaccine strains and between LAV and wild-type virus | Not reported | No clear cut evidence of increased virulence of reassortant strains reported | None recognized |
| Non-segmented genome viruses | ||||||||
| Newcastle disease virus (NDV) | Chickens | Paramyxovirus negative sense nonsegmented single-strand (ss) RNA | Recombination with wild-type NDV | Probably common | Both intra- and intergenic recombination events between LAVs and wild-type viruses | Unknown | Unknown | Vaccine sequences circulate in recombinant strains play a role in evolution |
| Oral polio vaccine (OPV) | Humans | Picornavirus positive sense non-segmented ssRNA | Recombination with wild-type poliovirus | Relatively common | Homologous intertypic recombination with wild-type polio, Coxsackie, and other enteroviruses | Increased virulence for transgenic mice | Vaccine associated paralytic disease in human | Over 30 described epidemics of vaccine-associated paralytic polio caused by circulating recombinant strains |
| Bovine viral diarrhea | Cows | Pestivirus positive sense non-segmented ssRNA | Recombination of LAV with persistently infecting non-cytopathic viruses | 5 cases, but may be frequent | homologous and nonhomologous recombination | Increased cytopathology in cell culture | Converts non-cytopathic persistently infecting virus to virulent strain causing mucosal disease | Sporadic mucosal disease |
| Infectious laryngotracheitis virus | Chickens | Herpesvirus double stranded linear DNA | Recombination of LAV and wild-type | Common | Homologous recombination | Increased virulence for poultry | Virulent recombinant strains | Outbreaks of disease in poultry flocks |
| Porcine reproductive and respiratory syndrome virus (PRRSV) | Swine | Arterivirus positive sense non-segmented ssRNA | Recombination of LAV and wild type | Single report | Intergenic recombination | Not studied | Isolate made during an outbreak of PRRS but pathogenicity of recombinant not known | Unknown |
The Brighton Collaboration report cites the following variables that should be considered in assessing risk of recombination.
-
1.
Intrinsic recombination properties of the parent virus
-
2.
Sequence relatedness of vector and wild virus
-
3.
Host range, pathogenesis and transmission
-
4.
Replication competency in target host
-
5.
Mechanism of attenuation
-
6.
Additional factors potentially affecting virulence
These factors will be considered below in the case of RVFV vaccines.
3.2. What is the evidence for reassortment of RVFV, specifically?
The evidence from phylogenetic studies of RVFV strains indicates that reassortment between RVFV strains (but not other viruses) has played a role in the evolution of the virus, but that low levels of diversity have been observed over 67 years [42]. Reassortment events, while reported in nature, have been rare compared to sequence variations resulting from mutations [43]. Reassortment has occurred between RVFV strains, rather than with heterologous phleboviruses, or more distantly related bunyaviruses. It may be inferred that similar limitations would reduce the potential for successful reassortment of an LAV with heterologous viruses, creating a chimera with unknown pathogenicity. Experimental studies have recently borne out this fact; a recent study evaluated the potential of MP-12 LAV to reassort with other related viruses of the family Phenuiviridae including Arumowot virus, a phlebovirus and no viable reassortant viruses were produced [44].
3.3. What is the evidence for and risk of reassortment of live, attenuated RVF vaccines?
With respect to the points #1 and 2 cited by Condit et al. [33], it is acknowledged that RVFV LAVs have segmented genomes, and that such vaccines have sequence homologies with wild-type RVFV strains, both of which present theoretical risks of reassortment.
Notwithstanding this potential, the evidence for reassortment of LAVs and wild-type strains is extremely limited. As cited above [1], the WHO document background section cites, as evidence of a safety concern, a single example to support a general concern about reassortment, and doubt remains whether the patient’s illness was due to an LAV-wild-type reassortant or wild-type virus. In addition, the isolate from the patient (SA/184/10) was re-evaluated by full genomic sequencing and found not to be a reassortant [2].
Unlike orbiviruses such as bluetongue and African horsesickness LAVs that have more complex 10-segmented genomes and multiple serotypes, requiring that vaccines consist of mixtures of multiple co-infecting viruses that can reassort in vivo, RVF LAV consists of a single virus that cannot reassort unless simultaneous coinfection occurs with an exogenous virus.
Gaudrealt et al. [45]. provide a comprehensive review of reassortment of RVFV, citing examples from experimental and field studies with LAVs. The review supports the conclusion that, while reassortant wild-type viruses have been identified, this was an uncommon phenomenon. The evidence provided for reassortment between wild-type and attenuated LAVs in natural infection was limited to the SA184/10 strain from the patient with a needle stick injury cited earlier, for which full genomic sequencing indicates that it is not a reassortant virus [2]. Where reassortment has been demonstrated in experimental studies (by coinfection in vitro or in mosquitoes) no evidence for strains of increased pathogenicity has been found.
The risk of reassortment of the SNS vaccine with wild-type virus was also reviewed by Grobelaar et al. [1]. The authors point to the methods used in vaccinating livestock, where automatic syringes are used with intermittent needle changes, affording a means of iatrogenic virus transfer that would enhance the chances of coinfection with vaccine (SNS) and wild-type RVFV. Despite this, sequencing studies of multiple strains from ruminants during outbreaks where the vaccine was widely used has not revealed clear evidence for reassortment [1], [45].
In the setting of an RVF epizootic (and potential spill-over to humans), risks associated with LAV have been deemed acceptable. Such risks would be even more acceptable in the case of LAVs with lower pathogenicity (for both livestock and humans) than the SNS and with molecular constraints limiting viremia and vector infection. We see no empirical evidence to support rigid constraints related to reassortment as posited in the WHO TPP. It is noteworthy that the Coalition for Epidemic Preparedness Innovations (CEPI) is currently funding the manufacturing and Phase I/II clinical evaluation of two LAV (DDVax™ and the RVFV-4 s vaccine).
With respect to points #3–6 cited by Condit et al. [33], reassortments between LAVs and wild-type virus would be unlikely to produce novel viruses with pathogenicity, host range, or transmission potential greater than the wild-type virus responsible for co-infection. LAVs in development (described above) all have documented mechanisms of attenuation, and some have redundant deletions, polygenic mutations, or genetic rearrangements that by design mitigate risks accompanying theoretical reassortment events.
Each vaccine candidate has a specific set of risks based on its mechanism of attenuation (Condit et al. [33] point #5). For MP-12 and MP-12-NSm-del, which have attenuating mutations on all three genome segments, attenuation would remain after substitution of a wild-type genome segment; conversely acquisition of an MP-12 or MP-12-NSm-del genome segment by wild-type virus would be attenuating, as shown experimentally [46]. For Clone 13 reassortment with the S segment from a wild-type strain would reconstitute virulence but the single animal in which coinfection occurred would have an outcome no worse than the original wild-type infection. Theoretically the reassorted (now fully wild-type) virus could be transmitted but would have no relevance in an area where wild-type strains were already circulating. Similarly, the DD-Vax and RVFV-4s vaccines have polygenic deletions or genome rearrangements that should reduce any hypothetical risk of reversion to virulence through reassortment with a wild-type virus.
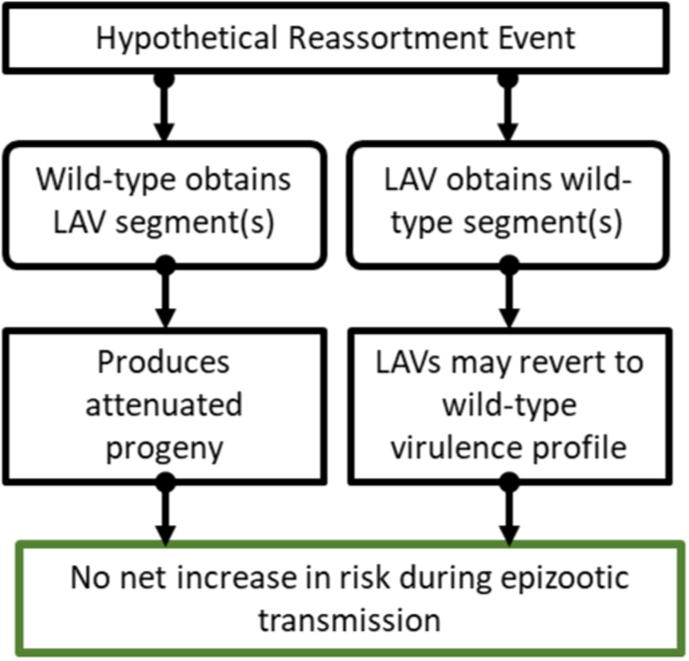
Aside from iatrogenic needle-syringe transmission between ruminants noted above, the settings in which reassortment are limited to: (1) co-infection with a wild-type strain in the vector mosquito, which could acquire blood meals by interrupted feeding on ruminants infected with vaccine and wild-type viruses, or could have been infected with wild-type virus in a previous gonotrophic cycle; (2) co-infection in a vaccinated ruminant or human by a mosquito infected with wild-type virus or by direct contact with infected ruminant blood or tissues; or (3) vaccination of a ruminant or human during acute infection with wild-type virus. If, in these circumstances, reassortment occurred it would be of no consequence (Fig. 1).
Fig. 1.
Genetic reassortment of live attenuated vaccine candidates with wild-type RVFV is unlikely to result in a more virulent or transmissible phenotype. 1. Wild-type virus that obtains an LAV segment(s) would be partially attenuated or retain the original phenotype. 2. LAVs that obtain a wild-type segment(s) would not exceed the original virulence profile of the circulating wild-type parental strain.
Fig. 1 depicts the range of phenotypic outcomes of reassortment between a LAV and wild-type virus. If an LAV genome segment was acquired by a wild-type virus, the phenotype of the resulting virus would be attenuated or unchanged. If a wild-type virus genome segment was acquired by an LAV, its host range, viremia level, pathogenicity, and transmissibility (shedding, arthropod infection) could be increased, but is unlikely to exceed that of the wild-type virus itself. Experimental observations of reassortment between the MP-12 LAV and wild-type RVFV have illustrated these conclusions [30]. Since it is impossible to exclude all biological possibilities through empirical, experimental studies of this sort, a risk-based approach to application of LAVs is required.
From a practical perspective, it would be advisable to limit opportunities for reassortment by changing practices that promote iatrogenic spread of viruses and coinfections (LAVs, wild-type virus, and reassorted viruses). For veterinary vaccines, needles should be changed between animals or alternate devices used to deliver vaccines. For human immunization, it is general practice to exclude patients who are acutely ill until they are recovered, and this would apply to new vaccines, including LAVs and defective vector vaccines. These factors could be considered in the WHO TPP, without stipulations that exclude use of vaccines during epizootics or epidemics.
4. Specific comments on the WHO TPP for animal RVF vaccines.
The WHO is encouraged to provide a more balanced view of reassortment, emphasizing that reassortment between RVFV LAVs and wild-type strains have been rarely documented compared to other vaccines, with no indication that reassortant events would result in novel strains with enhanced pathogenicity or transmission potential. Despite use of RVF LAVs in multiple epizootics, clear-cut evidence for reassortment has not been observed by genomic analysis of multiple strains. Moreover, reassortment between an LAV and a wild-type virus is unlikely to result in a virus with virulence characteristics higher than the wild-type virus causing the coinfection.
LAV developers should consider reassortment in experimental studies of vaccine candidates and to provide a risk-based analysis of vaccine safety. WHO should consider adding language encouraging vaccine developers to consider reassortment in a vaccine-specific risk-based analysis, considering the factors listed in the Brighton Collaboration document [33] and the risks and benefits of vaccine use in both epizootic/epidemic and endemic settings.
4.1. TPP for veterinary use
Safety/Reactogenicity: We disagree that the target profile for veterinary vaccines should be less restrictive with respect to reassortment than for human vaccines. The risk of co-infection and reassortment in ruminants (the viremic host species that amplify circulation of RVFV) is certainly greater than in humans due to their higher exposure to mosquito vectors, high viremia, inapparent infection in adults favoring vaccination of infected animals, and the cross-contaminating needle practices..
We also disagree with the restriction against use of LAVs during an outbreak since the benefit of vaccination outweighs the (theoretical) low risks and consequences of reassortment, while the risk of expanding disease is high. However, it is important to increase awareness of farmers to prevent transmission of wild-type RVFV via repeated needle use. A benefit:risk ratio (e.g. RVF abortions prevented per excess LAV related abortion) could be estimated based on modeling.
We agree with the TPP that the vaccine not be abortigenic or teratogenic. However, vertical transmission to the fetus may be acceptable provided it is not abortigenic or teratogenic. We suggest that the statement that “Live attenuated vaccines in any form must be sufficiently weakened not to cause reversion to virulence or creation of reassortments transmissible via mosquitoes” be changed to read “Live attenuated vaccines should contain safeguards against reversion to virulence and transmissibility through mutation or reassortment”. This statement provides guidance for risk-based regulatory assessments without unduly limiting development.
We agree with the optimal and minimally acceptable target that the vaccine neither cause significant adverse effects to animal health nor compromise the food chain. We suggest adding a requirement that LAVs be cleared rapidly and that the period of viremia, tissue infection, shedding, and biodistribution of LAVs be defined during vaccine development.
Efficacy: We agree with the targets regarding the percent of animals seroconverting. We suggest that the statement of protection through colostrum apply to livestock in general, not only sheep. With respect to Differentiating Infected from Vaccinated Animals (DIVA), WHO recommendations should be compliant with the Office International des Epizooties (OIE) Terrestrial Manual, which states that “Although DIVA is an important property of any future vaccine, a requirement for DIVA should not hinder or block the development or licensing of an effective RVF vaccine” [47].
Stability and Storage: Since some animal vaccines are currently stored and delivered in liquid nitrogen in Africa (and elsewhere), the Minimally Acceptable Target criteria should be changed to allow for a liquid frozen vaccine.
4.2. Human vaccine TPP
Indication for use: We suggest that “other control measures” be defined, with an emphasis on animal vaccination to reduce infection of humans [48].
Safety/reactogenicity. We disagree with the optimal target description “No live-attenuated virus vaccine to be used unless reassorting is excluded”. Reassortment cannot be categorically “excluded” for LAVs but is unlikely to have untoward consequences, as described above. The TPP should stipulate that LAVs should contain safeguards against reversion and reassortment and should have a favorable benefit:risk ratio when used for RVFV prevention and outbreak control.
We disagree with the minimally acceptable target description “Usage of an attenuated live vaccine that may allow reassortment is not indicated in an outbreak setting.” As pointed out above, reassortment cannot be categorically “excluded” for LAVs and is unlikely to have untoward consequences. LAVs in use and under development already contain safeguards against reversion and reassortment. The benefit:risk ratio (cases of RVF illness, retinitis or death prevented per excess illness caused by a theoretical reassortant) will be highly favorable for an LAV used for RVF epidemic control. Moreover, there is no evidence for human-to-human or human-mosquito transmission of wild-type RVFV, and this will likely be true for both LAVs and for a LAV-wild-type reassorted virus as well.
Efficacy: The statement “It is advised to broadly characterize the immune response after vaccination including profiles of the humoral and cellular immune response” could be strengthened to advise that a biomarker of protective immunity be defined (critical to assessments of durability of protection and of efficacy in different populations, e.g. children, elderly). It is likely that neutralizing antibody mediates protection, but a biomarker (antibody titer) has not been defined.
Product stability and storage: The minimally acceptable target “Shelf life of at least 12 months at −20 °C, and demonstration of at least 1 month stability at 2–8 °C” should be expanded to allow for frozen liquid vaccine held at < -60 °C, given recent experience with distribution of Ervebo® (Ebola) vaccine during epidemics in Africa.
5. Future studies on reassortment of LAVs
Once LAVs are approved and widely used to vaccinate ruminants and/or humans, it is important to monitor for reassortment and to better define the frequency of such events. Post-marketing studies could sample animals (humans) during the first few days after vaccination (the timing based on the period of viremia or evidence for replication based on biodistribution studies of the vaccine), particularly when vaccinations are performed during periods of concurrent RVFV circulation. Additional surveillance of mosquito vectors for reassortant virus during such periods would also be useful. Full genomic sequencing of suspect reassortant viruses should be performed for verification. If reassortants are found, phenotypic characterization will be important, and could include experimental studies of virulence and host range [45]. The latter require that the virus is isolated, followed by establishment of a low-passage virus stock, preferably in mosquito cells to avoid phenotypic changes due to laboratory passage. Careful consideration is needed of experimental design for virulence and host range studies, benchmarked against both the parental LAV and wild-type viruses.
6. Conclusion
LAVs have significant advantages over other vaccine designs, including inactivated, subunit and single-cycle vectored vaccines, since they induce rapid onset of immunity after a single dose, and durable protection [49]. These attributes are especially important when vaccines are used to control an ongoing epizootic in ruminants [50] or an epidemic in humans, a critical goal for vaccines against RVFV. An important factor limiting reassortment that distinguishes RVF LAVs from other LAVs is that the wild-type field-virus has relatively low genetic diversity, allowing vaccines to contain only a single virus type, whereas other LAVs, exemplified by bluetongue and African horsesickness, must be polyvalent and contain mixtures of multiple viruses and serotypes to provide adequate protection against a much wider antigenic diversity, a feature that promotes the potential for genetic reassortment. The safety of any new RVFV vaccine must be determined in suitably powered trials for licensure and monitored thereafter by post-marketing surveillance. Theoretical safety risks, such as that posed by reassortment, can be addressed through rational vaccine design, redundant attenuating markers, and thoughtful experimental studies. The possibility of recombination is a basic theoretical attribute of any replicating vaccine, and likewise among those with segmented genomes reassortment is a basic attribute of replicating vaccines; however, these theoretical risks should not be a priori restrictions on use of vaccines otherwise shown to be safe and effective. Rather, new vaccines should be evaluated using benefit:risk criteria in the context of the natural disease and balance the needs for rapid-onset and durable protection against theoretical impacts of reassortment or recombination. The benefits of a LAV for prevention and control of RVF outbreaks clearly outweigh the theoretical risk of reassortment, which has not been demonstrated to be a safety problem despite marketing widespread field-use of two RVFV LAVs, and in preclinical studies of several others in development.
Disclaimers
This work received no external funding. The views expressed in this article do not necessarily reflect the official policy or position of the Centers for Disease Control and Prevention, Department of the Navy, Department of Defense, nor the United States Government.
Copyright statement
Smith, D.R. is a military service member and federal employee of the United States government. This work was prepared as part of her official duties. Title 17 U.S.C. 105 provides that ‘copyright protection under this title is not available for any work of the United States Government.' Title 17 U.S.C. 101 defines a U.S. Government work as work prepared by a military service member or employee of the U.S. Government as part of that person's official duties.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Dr. Monath is a consultant to the Sabin Vaccine Institute, which owns the license to the MP-12 live attenuated RVFV vaccine.
Dr. Bird is developing a live, attenuated Rift Valley fever vaccine, DDVax®, with funding from the Coalition for Epidemic Preparedness Innovations.
Dr. Kortekaas is developing the RVFV-4s live attenuated vaccine against RVFV, with funding from the Coalition for Epidemic Preparedness Innovations.
Drs. Watts is developing a live attenuated MP12-NSm deletion veterinary vaccine against RVFV, with support from USAID, and is collaborating with the vaccine manufacturer, M.C.I Santé Animale, Mohammedia, Morocco.
Drs. Peters, Morrill, Bettinger, and Pittman were formerly engaged in development of the MP-12 live RVFV vaccine, with support from the US Army; however, there are no current financial relationships related to this work.
References
- 1.Grobbelaar A.A., Weyer J., Leman P.A. Molecular Epidemiology of Rift Valley Fever Virus. Emerg Infect Dis. 2011;17:2270–2276. doi: 10.3201/eid1712.111035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grobbelaar A.A., Weyer J., Leman P.A. Correction: Molecular Epidemiology of Rift Valley Fever Virus. Letter to the Editor. Emerg Infect Dis. 2020 doi: 10.3201/eid1712.111035. (Submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smithburn K.C. Rift Valley fever; the neurotropic adaptation of the virus and the experimental use of this modified virus as a vaccine. Br J Exp Pathol. 1949;30:1–16. [PMC free article] [PubMed] [Google Scholar]
- 4.Kaschula V.R. University of Pretoria; 1953. The propagation and modification of strains of Rift Valley fever viruses in embryonated eggs and their use as immunizing agents for domestic ruminants. DVSc thesis. [Google Scholar]
- 5.Muller R., Saluzzo J.F., Lopez N. Characterization of clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, which is altered in the small segment. Am J Trop Med Hyg. 1995;53:405–411. doi: 10.4269/ajtmh.1995.53.405. [DOI] [PubMed] [Google Scholar]
- 6.Billecocq A., Spiegel M., Vialat P. NSs protein of Rift Valley fever virus blocks interferon production by inhibiting host gene transcription. J Virol. 2004;78:9798–9806. doi: 10.1128/JVI.78.18.9798-9806.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ly H.J., Ikegami T. Rift Valley fever virus NSs protein functions and the similarity to other bunyavirus NSs proteins. Virol J. 2016;13:118. doi: 10.1186/s12985-016-0573-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Njenga M.K., Njagi L., Thumbi S.M. Randomized Controlled Field Trial to Assess the Immunogenicity and Safety of Rift Valley Fever Clone 13 Vaccine in Livestock. PLoS Negl Trop Dis. 2015;9(3) doi: 10.1371/journal.pntd.0003550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lo M.M., Mbao V., Sierra P. Safety and immunogenicity of Onderstepoort Biological Products' Rift Valley fever Clone 13 vaccine in sheep and goats under field conditions in Senegal. Onderstepoort J Vet Res. 2015;82(1):857. doi: 10.4102/ojvr.v82i1.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makoschey B., van Kilsdonk E., Hubers W.R. Rift Valley Fever Vaccine Virus Clone 13 Is Able to Cross the Ovine Placental Barrier Associated with Foetal Infections, Malformations, and Stillbirths. PLoS Negl Trop Dis. 2016;10(3) doi: 10.1371/journal.pntd.0004550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moutailler S., Krida G., Madec Y. Replication of Clone 13, a naturally attenuated avirulent isolate of Rift Valley fever virus, in Aedes and Culex mosquitoes. Vector Borne Zoonotic Dis. 2010;10:681–688. doi: 10.1089/vbz.2009.0246. [DOI] [PubMed] [Google Scholar]
- 12.Pittman P.R., McClain D., Quinn X. Safety and immunogenicity of a mutagenized, live attenuated Rift Valley fever vaccine, MP-12, in a Phase 1 dose escalation and route comparison study in humans. Vaccine. 2016;34:424–429. doi: 10.1016/j.vaccine.2015.12.030. [DOI] [PubMed] [Google Scholar]
- 13.Pittman P.R., Norris S.L., Brown E.S. Rift Valley fever MP-12 vaccine Phase 2 clinical trial: Safety, immunogenicity, and genetic characterization of virus isolates. Vaccine. 2016;34:523–530. doi: 10.1016/j.vaccine.2015.11.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller M.M., Bennett K.E., Drolet B.S. Evaluation of the efficacy, potential for vector transmission, and duration of immunity of MP-12, an attenuated Rift Valley fever virus vaccine candidate, in sheep. Clin Vaccine Immunol. 2015;22:930–937. doi: 10.1128/CVI.00114-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morrill J.C., Carpenter L., Taylor D. Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine. 1991;9:35–41. doi: 10.1016/0264-410x(91)90314-v. [DOI] [PubMed] [Google Scholar]
- 16.Hunter P., Erasmus B., Vorster J. Teratogenicity of a mutagenised Rift Valley fever virus (MVP 12) in sheep. Onderstepoort J Vet Res. 2002;69:95–98. [PubMed] [Google Scholar]
- 17.Morrill J., Jennings G., Caplen H., Turell M., Johnson A., Peters C. Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am J Vet Res. 1987;48:1042–1047. [PubMed] [Google Scholar]
- 18.Morrill J., Mebus C., Peters C. Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am J Vet Res. 1997;58:1104–1109. [PubMed] [Google Scholar]
- 19.Baskerville A., Hubbard K.A., Stephenson J.R. Comparison of the pathogenicity for pregnant sheep of Rift Valley fever virus and a live attenuated vaccine. Res Vet Sci. 1992;52:307–311. doi: 10.1016/0034-5288(92)90029-2. [DOI] [PubMed] [Google Scholar]
- 20.Turrell M.J., Rossi C.A. Potential for mosquito transmission of attenuated strains of Rift Valley fever virus. Am J Trop Med Hyg. 1991;44:278–282. doi: 10.4269/ajtmh.1991.44.278. [DOI] [PubMed] [Google Scholar]
- 21.Won S., Ikegami T., Peters C.J., Makino S. NSm Protein of Rift Valley Fever Virus Suppresses Virus-Induced Apoptosis. J Virology. 2007;81:13335–13345. doi: 10.1128/JVI.01238-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morrill J.C., Laughlin R.C., Lokugamage N. Safety and Immunogenicity of recombinant Rift Valley fever MP-12 vaccine candidates in sheep. Vaccine. 2013;31:559–565. doi: 10.1016/j.vaccine.2012.10.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morrill J.C., Laughlin R.C., Lokugamage N. Immunogenicity of a recombinant Rift Valley fever MP-12-NSm deletion vaccine candidate in calves. Vaccine. 2013;31:4988–4994. doi: 10.1016/j.vaccine.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salekwa L.P., Nyundo S.B., Adamson E.K. Evaluation of the Immunogenicity of a Mutagenized Rift Valley Fever MP-12 and a Recombinant Rift Valley Fever arMP12ΔNsm21/384 Vaccine Candidates in Indigenous Species of Cattle, Sheep, and Goats in Tanzania. J Vaccines Vaccinology. 2019;10(2):401. [Google Scholar]
- 25.Boumart Z., Daouam S., Bamouh Z. Safety and immunogenicity of a live attenuated Rift Valley Fever recombinant arMP-12DNSm21/384 vaccine candidate for sheep, goats and calves. Vaccine. 2019;37:1642–1650. doi: 10.1016/j.vaccine.2019.01.067. [DOI] [PubMed] [Google Scholar]
- 26.Bird B.H., Albarino C.G., Hartman A.L. Rift valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J Virol. 2008;82(6):2681–2691. doi: 10.1128/JVI.02501-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bird B.H., Maartens L.H., Campbell S. Rift Valley fever virus vaccine lacking the NSs and NSm genes is safe, nonteratogenic, and confers protection from viremia, pyrexia, and abortion following challenge in adult and pregnant sheep. J Virol. 2011;85(24):12901–12909. doi: 10.1128/JVI.06046-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith D.R., Johnston S.C., Piper A. Attenuation and efficacy of live-attenuated Rift Valley fever virus vaccine candidates in non-human primates. PLoS Negl Trop Dis. 2018;12(5) doi: 10.1371/journal.pntd.0006474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kading R.C., Crabtree M.B., Bird B. Deletion of the NSm Virulence Gene of Rift Valley Fever Virus Inhibits Virus Replication in and Dissemination from the Midgut of Aedes aegypti Mosquitoes. PLoS Negl Trop Dis. 2014;8(2) doi: 10.1371/journal.pntd.0002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wichgers Schreur P.J., Oreshkova N., Moormann R.J.M., Kortekaasa J. Creation of Rift Valley Fever Viruses with Four-Segmented Genomes Reveals Flexibility in Bunyavirus Genome Packaging. J Virol. 2014;88z:10883–10893. doi: 10.1128/JVI.00961-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wichgers Schreur P.J., Kant J., van Keulen L. Four-segmented Rift Valley fever virus induces sterile immunity in sheep after a single vaccination. Vaccine. 2015;33(12):1459–1464. doi: 10.1016/j.vaccine.2015.01.077. [DOI] [PubMed] [Google Scholar]
- 32.Wichgers Schreur P.J., van Keulen L., Kant J., Kortekaas J. Four-segmented Rift Valley fever virus-based vaccines can be applied safely in ewes during pregnancy. Vaccine. 2017;35(23):3123–3128. doi: 10.1016/j.vaccine.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 33.Condit R.C., Williamson A.-L., Sheets R. Unique Safety Issues Associated with Virus Vectored Vaccines: Potential for and Theoretical Consequences of Recombination with Wild Type Virus Strains. Vaccine. 2016;12(34(51)):6610–6616. doi: 10.1016/j.vaccine.2016.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dungu B., Gerdes T., Smit T. The use of vaccination in the control of bluetongue in southern Africa. Vet Ital. 2004;40:616–622. [PubMed] [Google Scholar]
- 35.von Teichman B.F., Dungu B., Smit T.K. In vivo cross-protection to African horse sickness serotypes 5 and 9 after vaccination with serotypes 8 and 6. Vaccine. 2010;28:6505–6517. doi: 10.1016/j.vaccine.2010.06.105. [DOI] [PubMed] [Google Scholar]
- 36.Rodriguez L, Nogales A, Reilly EC, et al. A live-attenuated influenza vaccine for H3N2 canine influenza virus. 2017; 504: 96–106. [DOI] [PubMed]
- 37.Rodriguez L., Blanco-Lobo P., Reilly E.C. Comparative Study of the Temperature Sensitive, Cold Adapted and Attenuated Mutations Present in the Master Donor Viruses of the Two Commercial Human Live Attenuated Influenza Vaccines. Viruses. 2019;11(10):928. doi: 10.3390/v11100928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weyer C.T., Gewar J.D., Burger P. African Horse Sickness Caused by Genome Reassortment and Reversion to Virulence of Live, Attenuated Vaccine Viruses, South Africa, 2004–2014. Emerg Infect Dis. 2016;22:2087–2096. doi: 10.3201/eid2212.160718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van den Bergh C., Coetzee P., Venter E.H. Reassortment of bluetongue virus vaccine serotypes in cattle. J South Afr Vet Assoc. 2018;89 doi: 10.4102/jsava.v89i0.1649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feemstra F., van Rijn P.A. Current and next-generation bluetongue vaccines: Requirements, strategies, and prospects for different field situations. Crit Rev Microbiol. 2017;43:142–155. doi: 10.1080/1040841X.2016.1186005. [DOI] [PubMed] [Google Scholar]
- 41.Batten C.A., Maan S., Shaw A.E. A European field strain of bluetongue virus derived from two parental vaccine strains by genome segment reassortment. Virus Res. 2008;137:56–63. doi: 10.1016/j.virusres.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 42.Bird B.H., Khristova M.L., Rollin P.E. Complete genome analysis of 33 ecologically and biologically diverse Rift Valley fever virus strains reveals widespread virus movement and low genetic diversity due to recent common ancestry. J Virol. 2007;81:2805–2816. doi: 10.1128/JVI.02095-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bird B., Githinji J.W.K., Macharia J.M. Multiple Virus Lineages Sharing Recent Common Ancestry Were Associated with a Large Rift Valley Fever Outbreak among Livestock in Kenya during 2006–2007. J Virol. 2008;82:11152–11166. doi: 10.1128/JVI.01519-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ly H.J., Lokugamage N., Nishiyama S., Ikegami T. Risk analysis of inter-species reassortment through a Rift Valley fever phlebovirus MP-12 vaccine strain. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0185194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gaudreault N.N., Indran S.V., Balaraman V. Molecular aspects of Rift Valley fever virus and the emergence of reassortants. Virus Genes. 2019;55:1–11. doi: 10.1007/s11262-018-1611-y. [DOI] [PubMed] [Google Scholar]
- 46.Ikegami T., Hill T.E., Smith J.K. Rift Valley Fever Virus MP-12 Vaccine Is Fully Attenuated by a Combination of Partial Attenuations in the S, M, and L Segments. J Virol. 2015;89:7262–7276. doi: 10.1128/JVI.00135-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ikegami, T, Hill, TE, Smith, JK, FAO. Rift Valley fever vaccine development, progress and constraints. In: Proceedings of the GF-TADs meeting, January 2011, Rome, Italy. FAO Animal Production and Health Proceedings, No. 12. Rome, Italy, 2011.
- 48.Monath T.P. Vaccines against diseases transmitted from animals to humans: a one health paradigm. Vaccine. 2013;31(46):5321–5338. doi: 10.1016/j.vaccine.2013.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rappuoli R., Dormitzer P., Mandl C., editors. Replicating Vaccines-a New Generation. Burkhäuser Verlag; Basel: 2010. [Google Scholar]
- 50.Dungu B., Lubisi B.A., Ikegami T. Rift Valley fever vaccines: current and future needs. Curr Opin Virol. 2018;29:8–15. doi: 10.1016/j.coviro.2018.02.001. [DOI] [PubMed] [Google Scholar]