Abstract
Objectives
To provide a critical reflection of COVID-19 in the context of oncology nursing and provide recommendations for caring for people affected by cancer during this pandemic.
Data sources
Electronic databases, including CINAHL, MEDLINE, PsychINFO, Scopus, professional web sites, and grey literature were searched using Google Scholar.
Conclusion
Nurses are key stakeholders in developing and implementing policies regarding standards of care during the COVID-19 pandemic. This pandemic poses several challenges for oncology services. Oncology nurses are providing a pivotal role in the care and management of the novel COVID-19 in the year landmarked as the International Year of the Nurse.
Implications for Nursing Practice
It is too early to tell what shape this pandemic will take and its impact on oncology care. However, several important clinical considerations have been discussed to inform oncology nursing care and practice.
Key Words: Oncology nursing, COVID-19, coronavirus, workforce, supportive care, pandemic
Introduction
Since late December 2019, a novel coronavirus (COVID-19) has resulted in an ongoing pandemic of viral pneumonia, which started in Wuhan, China.1 , 2 As of 13th April 2020, COVID-19 has affected 213 countries worldwide.3 In general, COVID-19 is an acute illness but it can be deadly, with an average case fatality of 2%.4 COVID-19 causes severe respiratory illness associated with an Intensive Care Unit (ICU) admission, mechanical ventilation, and high mortality.5 The presenting symptoms of COVID-19 include: fever, chills, cough, fatigue, and shortness of breath.1 , 4 , 5 There is recent anecdotal evidence that anosmia with resultant dysgeusia are frequently reported symptoms with COVID-19.
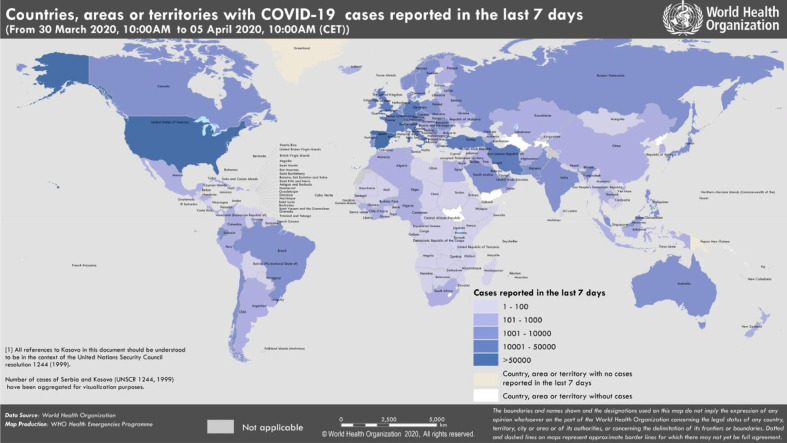
In this global critical care crisis and unparalleled health emergency, nurses are the largest health care professional group providing frontline care. Nurses’ pivotal role in the care and management of the novel COVID-19 comes in the year landmarked as the International Year of the Nurse.6 This global crisis is uncharted territory and the first of its kind for most nurses’ living memory, bringing along new challenges already recognized by international nursing boards.7, 8, 9, 10 At the time of writing this critical reflection, global incidence passes 1,699,595, with more than 106,138 fatalities (see Fig. 1 ).
Fig. 1.
World Health Organization COVID-19 global distribution.5
COVID-19 and Cancer
Early COVID-19 outcome data has suggested a fatality rate of 5.6% among those affected by cancer.11 A further study identified that people affected by cancer had a 3.5 times higher risk of severe COVID-19 disease than other patient groups.12 Around the world, vulnerable groups at risk of COVID-19 are people with specific cancers including those: undergoing active chemotherapy and radical radiotherapy for lung cancer; blood or bone marrow cancers, such as leukemia or multiple myeloma (at any stage of disease); those receiving immunotherapy; antibody treatments for cancer; targeted cancer treatments that can affect the immune system, such as protein kinase inhibitors; individuals who have received a bone marrow or stem cell transplant in the last 6 months; or those taking immunosuppression drugs.13 People affected by cancer could be at elevated risk of severe COVID-19 disease and may experience disrupted and delayed delivery of cancer therapies because of social distancing measures, quarantines, and general disruption in routine cancer service during this pandemic.
Therefore, this article aims to provide a critical reflection of COVID-19 in the context of caring for people affected by cancer. Given that new, emerging evidence will rapidly develop over time in this clinical context, the authors would recommend nurses and clinicians access official web sites for regular updates as they emerge over the course of this pandemic, such as those provided in Table 1 .
Table 1.
Web sites and resources during the COVID-19 pandemic
|
Historical Nursing Perspectives on Global Pandemics
In the Preface to their book, Nurses on the Front Line: When Disaster Strikes, Wall and Keeling note: “What nurses did in the past can inform disaster preparations for today … providing historical evidence to inform disaster policies for the future.”14 , p xi As co-editors and contributors, Wall and Keeling asked authors to analyze nurses’ roles as components of community responses to disasters that occurred in regions in the United States, Canada, Turkey, and Haiti – communicable diseases, earthquakes, hurricanes, accidents, and intentional and unintentional human errors. “Nurses”, they contend, are in positions “to participate in all aspects of the disaster response, including evacuation, triage, physical and psychological care at the scene and afterward, case finding, screening measures, vaccinations, and disease surveillance.”14 , p xii
The 1918 influenza pandemic in the United States
When viewed over the past century, similarities exist between the 1918 Influenza pandemic and the 2019–2020 pandemic attributed to another Coronavindae - SARS-CoV-2 - one of seven such microbes known to affect humans, causing the clinical entity referred to as COVID-19.15 The similarities justify exploring challenges encountered by nurses “on the front lines” and challenges arising during the 1918 influenza pandemic. Both entities are rapidly transmitted through person-to-person and close contact; both are marked by rapid expansion and spread; both are characterized by rapid increases of cluster cases. Clinical signs and symptoms of COVID-19 are often confused with influenza: fever, cough, sore throat, muscle soreness, and dyspnea. And finally, both disease entities have high mortality rates.
The origins of the 1918 influenza pandemic are said to be “inextricably associated with the soldiers who fought during the First World War.”16 , p 190 Between 1918 and 1919, the last 2 years of this war, one third of the global population is estimated to have been infected with influenza.17 Over 675,000 influenza-related deaths in the United States during this time frame are attributed to this virus. Still-evolving estimates indicate that the influenza type A virus responsible for the 1918 influenza pandemic (also sometimes referred to as the “Spanish Influenza” or the “Spanish Lady”) killed between 21.5 and 50 million people between 1918 and 1920. Even then, the real death toll may still be understated by as much as 100%.17 , 18 According to Taubenberger and Morens, “… all influenza A pandemics since that time, and indeed almost all cases of Influenza A worldwide have been caused by descendants of the 1918 virus,”17 , p 15 leading them to refer to the 1918 Influenza as “The Mother of All Pandemics.”17 , p 16
Keen-Payne,19 Deming,20 and Keeling21 provide vivid narrative descriptions of nurses’ efforts and contributions during the 1918 influenza pandemic. Keen-Payne19 suggests that effects of this pandemic are hidden by actions and states of organized medicine and nursing at the time, the status of health, science, health care, and public health in the United States, the context of World War I, and its immediate global aftermath.
Keen-Payne's historical study reveals contagion control in various urban areas, though not standardized, was addressed in several ways.19 In Chicago, Illinois, persons who sneezed or spit openly were threatened with arrests and fines; churches – ventilated by open windows during services - were not closed but ill parishioners were asked to stay home. Theatres, banquets, lectures, restaurants, and movie theaters were closed. Newark, New Jersey officials allowed liquor stores to stay open for sales only – a move protested by local church leaders. Newark hospitals are described as “overwhelmed with civilians and soldiers from nearby military bases.”19 , p 150 In San Diego, California all public facilities were closed. Many cities required face masks – fashioned with layers of square gauze tied at the top of the head and the back of the neck - to be worn in public; compliance varied. Social systems were disrupted, including telephone service, public transportation (train and taxi operators became ill), and nurses, firefighters, teachers, and priests were sick and absent from work. Lillian Wald, founder of public health nursing in New York, wrote to a friend explaining that 40,000 nurses were needed to provide necessary services to the city's poor.19 , p 150
As a student nurse, Dorothy Deming's reflection of her 1918 Influenza pandemic experience noted how swiftly the “attack” occurred: “No one anticipated the suddenness of the attack. … Almost overnight the hospital was inundated by flu victims.”20 , p 1308 Her hospital (with capacity of 250 beds) admitted 850 patients with flu or flu-like pneumonia during 6 weeks. She notes a shortage of nurses during this time – with more than 50 nurses in military service overseas. Deming specifically observed the emotional impact of this work.
“[My classmate and I] were fairly well prepared for this ordeal: prepared, that is, for all but the emotional impact of the situation…. Until the epidemic, death had seemed kindly, coming to the very old, the incurably suffering, or striking suddenly with the knowledge of its victim. Now we saw death clutch cruelly and ruthlessly at vigorous, well-muscled young women in the prime of life.”20, p 1309
Seeing the difficulty of having so little to offer patients and families, Deming says:
“In 1918, we had no miracle drugs, no antibiotics, no oxygen or suction equipment at every bedside. We knew of efforts to develop a vaccine … but never saw its results in our wards. … Over and over again we heard the doctors say, after writing a long list of orders which we came to know almost by heart, ‘Now everything depends on good nursing.’ We tried our best.”20, p 1309
Nevertheless, Deming concludes: “Those were dedicated weeks, as truly under fire as though we were with our brothers in the Argonne. Life was just one long emergency. … For me, nursing came alive during that test.”20 , p 1309 D'Antonio and Whelan convey nurses’ critical roles in preventing greater spread of influenza and reducing the severity of the pandemic they view as “the most devastating epidemic in history.”22 , p 70 Nurses taught “individuals, families and communities about respiratory hygiene, handwashing, disinfection of household utensils, and the critical importance of wearing gauze masks”22 , p 70 … while also providing care for people already stricken with the disease. Special acknowledgement is offered to student nurses, who “provided almost all of the nursing care delivered in U.S. hospitals remaining at patients' bedsides throughout the pandemic; hundreds of them died.”22 , p 70
In a review of disaster nursing literature, Wall and Keeling14 identify seven shared themes regardless of time, place, and circumstance:
-
1)
Improvised activities at local and national scenes;
-
2)
Cooperation and collaboration among previously established professional and social networks;
-
3)
Leadership and courage;
-
4)
Spontaneous community support;
-
5)
Restoration of order out of chaos;
-
6)
Creation of healing narratives; and
-
7)
The crossing of cultural, geographic, and professional boundaries in response to the crisis.14 , p xii
Public Health Approach to the Epidemiology of Infectious and Contagious Diseases
In 2019, the Johns Hopkins Center for Health Safety released its report, Preparedness for a High-Impact Respiratory Pathogen Pandemic” 23 after examining the state of global preparedness for pandemics caused by pathogens with potential for widespread transmission and high mortality. The assessments undertaken identified significant national and international readiness gaps around detection and containment, challenges relating to tools, personnel, surveillance systems, and global governance and response.23
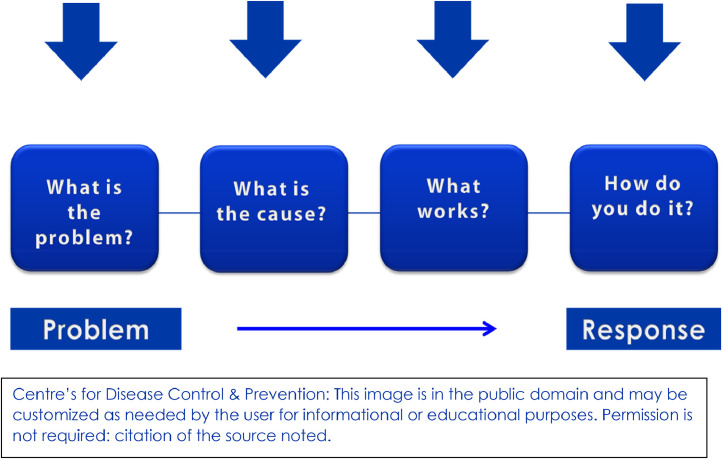
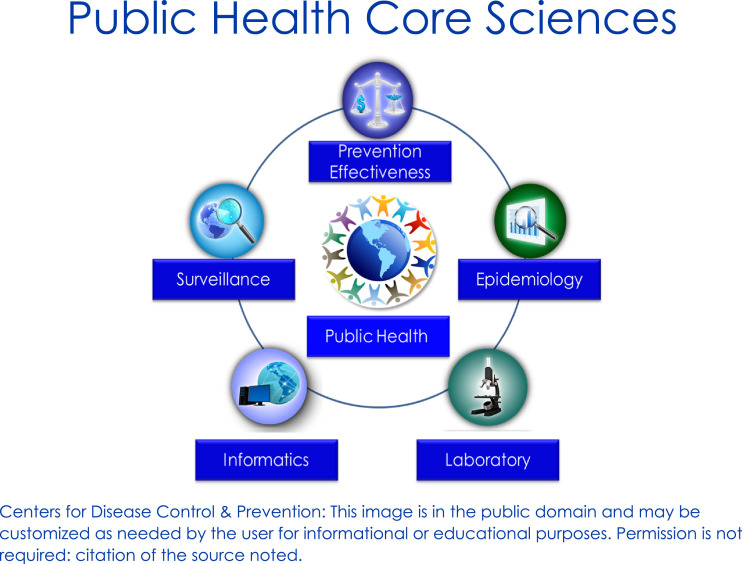
The Public Health approach used now is not much different than that used 1918 (See Fig. 2 ). Application of epidemiologic sciences are useful in identifying distribution and determinants of health problems and suggestion of potential mitigation strategies (See Fig. 3 ).24 Efforts to solve health problems generally follow a four-step scientific approach involving data collection, assessment, hypothesis testing, and action. In the public health approach, data are collected and an initial assessment (or hypothesis) is conducted. The hypothesis is tested, and resulting information is used to devise interventions. As in all sciences, epidemiology applies key terms (noted in Table 2 ).24
Fig. 2.
A public health approach to epidemiology.
Fig. 3.
Public health core sciences.
Table 2.
Key epidemiology terms (US Centers for Disease Control, 2014)
| Epidemic or outbreak: disease occurrence among a population that is in excess of what is expected in a given time and place. |
| Cluster: group of cases in a specific time and place that might be more than expected. |
| Endemic: disease or condition present among a population at all times. |
| Pandemic: a disease or condition that spreads across regions. |
| Rate: number of cases occurring during a specific period; always dependent on the size of the population during that period. |
Of COVID-19, initially identified as a “novel coronavirus,” medical historian Howard Markel, known for his studies of the 1918 flu epidemic, says: “The key word about this coronavirus is ‘novel’ – we don't have any experience with COVID-19…[and] we won't know it's over until long after it's over.”25 , p 3 Gaps remain in our understanding of its molecular structure, the infectious nature of this particular coronavirus, identifying characteristics of COVID-19 diagnoses, modes, and rapidity of transmission, definition of contacts, and the public health management based on observations of similar coronaviruses.
New and important data describing the biology, epidemiology, and clinical spectrum of COVID-19 appears almost daily. Del Rio and Malani26note more than 400 articles listed in PubMed since the outbreak was first reported in late 2019 – challenging even the most attentive readers to stay abreast of the recent findings and clinical guidance. Critical pieces of information remain missing for traditional epidemiologic sciences and practices to be fully applied to effective screening and testing.27
Soon after the Wuhan outbreak was reported, field investigations for suspected and confirmed cases and collection of case respiratory specimens were conducted, initially arriving at the working case definition of “Novel Coronavirus-Infected Pneumonia” (NCIP) based on previous coronavirus case definitions. Suspected case epidemiologic criteria were devised. Accurate and adequate testing capabilities, essential to confronting the outbreak and identification of people with infection, despite minimal symptoms, remain an unmet need.26 Widespread testing is not implemented in many, if not most countries, severely limiting our understanding of the basic biology of this newly discovered virus, and development of effective countermeasures.27
Contact identification and tracing
Until an anti-COVID-19 vaccine is developed and deployed, the most effective means of interrupting transmission, preventing new cases and complications is the public health process of contact tracing.28 Individuals who have been in close contact – within 6 feet of an infected person for a prolonged period of time - are at risk of becoming infected themselves, and further infecting others. Close monitoring of contacts exposed to an infected person facilitates early diagnosis and treatment, preventing further viral transmission. This three-step monitoring process is referred to as “contact tracing” (World Health Organisation29):
-
1)
Contact identification – after a person has a confirmed infection, identification of contacts involves interviews to identify the person's activities, and roles of people around them since the onset of illness. Contacts include anyone who has been in contact with the infected person – family members, work colleagues, friends, and health care providers.
-
2)
Contact listing – Any persons known to have contact with the infected person are listed as “contacts,” and efforts are made to identify each contact, inform them of their at-risk status, actions to follow, information about accessing early care, and disease prevention and mitigation strategies (quarantine or isolation is required for high-risk contacts).
-
3)
Contact follow-up – This is a painstaking, resource-intensive, and expensive process, though technologic advances can diminish the intensity of such tasks. Regular follow-up of close contacts generally consists of daily telephone calls, text messaging, and/or in-person inquiries about fever and other symptoms for 14 days after the last known exposure to a person with confirmed COVID-19. If and when close contacts develop new or worsening symptoms, they are referred for diagnostic testing and appropriate treatment.
Contact tracing is dependent on preconditions, including eliminating barriers to testing. When testing is not fully implemented, public health strategies cannot follow lines of transmission. Another precondition reflects the penetration of the disease in a given community: the disease burden must be low enough to make it practical to investigate potentially infected persons, symptomatic or not. Contact tracing is most useful in containing flare-ups and preventing exponential growth of new cases.28
COVID-19 is a new disease and there is limited information regarding risk factors for severe disease. Based on currently available information and clinical expertise, older adults and people of any age who have serious underlying medical conditions30 might be at higher risk for severe illness from COVID-19. Emerging evidence supports necessary acknowledgement of populations at higher risk for COVID-19, including adults over age 65, individuals with underlying conditions, including obesity, diabetes, hypertension, and those who are immunocompromised by diseases – including cancer – and treatments that impair the immune system.31 Although studies exploring the effects of COVID-19 on cancer care are so far very limited, it is surmised that people with cancer and cancer survivors may well be at higher risk for developing complications relating to COVID-19, including the need for intensive care, mechanical ventilation, and death. A Lancet Oncology editorial32 notes pressures put upon health-care systems struggling to near breaking points as resources are diverted to respond to the COVID-19 crisis. Less considered as the COVID-19 crisis continues throughout the world, may be the cancellation of conferences, jeopardy and prioritizing of research trials and projects, absence of practical laboratory work and field studies, and other consequences for research, education, and collaboration. The world's largest annual oncology nursing conference, that of the Oncology Nursing Society, scheduled for April 30–May 3, 2020, was cancelled.
Clinical Presentation of COVID-19
Published reports have identified that the clinical presentation of COVID-19 is most frequently associated with fever (90%–98%), non-productive cough and sore throat (59%–76%), and lethargy (38%–70%).33, 34, 35 Less frequent reported symptoms include abdominal pain, dizziness, headache, diarrhea, nausea, and vomiting.34 Shortness of breath is another presenting feature, with a median time of development reported at 8 to 8 days (range, 3 to 9 days) from initial onset.34 Patients have also been found to have radiologic evidence of pneumonia.5 In severe COVID-19 cases, patients will experience organ dysfunction: shock, acute respiratory distress syndrome (ARDS), acute cardiac arrest, acute kidney failure, and death can occur in severe cases.5 Moreover, emergent evidence has identified that a subgroup of patients with severe COVID-19 experience cytokine storm syndrome.36 It is recommended that all patients with severe COVID-19 should be screened for hyperinflammation (ferritin, platelet count, and erythrocyte sedimentation rate) because immunosuppression with corticosteroids can decrease mortality for a subgroup of patients.36 Case reports have identified human-to-human transmission.37 , 38 At present, there are no effective vaccines or therapies to treat COVID-19. Diagnosis can be made from specific reverse transcription polymerase chain reaction (RT-qPCR) of nasopharyngeal or oropharyngeal swabs, and lower respiratory tract samples.34
Oncology Nursing Considerations to COVID-19
Globally, health care systems and policy responses to COVID-19 are evolving rapidly. Of the estimated 43.5 million health care workers (HCWs) in the world, it is estimated that 20.7 million of those are nurses.39 Therefore, nurses are at the forefront of this pandemic and are taking a proactive approach with multidisciplinary teams to participate in the pandemic planning within their health organizations. It is critical that nurses regularly review and follow institutional, specialist college, state level, and government recommendations. Measures should be subject to an ongoing review that will reflect organizational, local, state-wide, and national policies (including, criteria for COVID-19 testing, self-isolation, social distancing, quarantine, and personal protective equipment [PPE]).
Service delivery impact
Day by day there is a new release of information and new wave of regulations that impact the oncology service globally. The rapid spread of COVID-19 has the potential to overwhelm primary and acute services, as was experienced in China11 and Italy.21 The challenge to deliver oncology services is further compounded by COVID-19 infection spread to nursing and medical personnel and school closures, all of which impact staffing levels. Moreover, to create new local COVID-19 services means that there is an ongoing re-shuffling and re-allocating of resource (human and budget), which puts additional strain on existing services that were already at full capacity. Figures from China's National Health Commission demonstrated that more than 3,300 HCWs were infected, and 22 had died related to COVID-19.40 As the pandemic accelerates, providing PPE to deliver safe oncology services is a key concern worldwide.12 If acute care services are at maximum capacity, institutions may provide alternative provisions for the care of people affected by cancer. Therefore, oncology nurses will need to be flexible to facilitate the safe delivery of alternative models of care. Alternative and adaptive models of care could increase the use of community care or private facilities.
Following an analysis of nationwide data in China, a number of major strategies were put forward in the clinical management of cancer during this COVID-19 crisis.12 First, that of intentional postponing of adjuvant chemotherapy or elective surgery for people with low risk cancers. Second, should surgery suites be unavailable, and personnel be seconded to other clinical roles, neoadjuvant chemotherapy could be considered for timely delivery of oncologic maneuvers for some malignancies. Hypofractionated radiotherapy protocols should be prescribed whenever possible,41 including single fraction treatments for uncomplicated bone metastases.42 Third, protective approaches such as PPE and personal space modifications should be considered (see Table 3 ). During chemotherapy administration, treatment beds or chairs should be placed with adequate space (1.5 meters) to prevent close contact as much as possible. Limiting or eliminating family attendance, while stressful, may be necessary in limited chemotherapy suite spaces. In such cases, portable technology such as smart phones or iPads could be loaned during the treatment session for patient and family support, and subsequent disinfection between patient use. Finally, more intensive surveillance during and in the recovery period should be considered when patients with cancer are infected with COVID-19, especially older patients and those with multiple co-morbidities.12
Table 3.
Oncology Nursing Society (ONS) interim recommendations for use of PPE during care delivery and administration of hazardous cancer drugs10
| PPE | ONS Recommendation | COVID-19 Interim recommendation |
|---|---|---|
| Gowns | Disposable poly-coated | Regular disposable gown (water resistant) Cloth gown (facility laundered)* |
| Masks | Mask with face and eye protection required only if splashing is likely and for cleaning of spills | N95 masks should be reserved for symptomatic or COVID-19–+ patients, hazardous spills and clean-up Powdered air purifying respirators (PAPRs) |
| Eye protection | Mask with eye protection or goggles if splashing is likely and for cleaning of spills | Full face piece air purifying respirators or PAPRs |
| Gloves | Double chemotherapy-tested gloves | Single chemotherapy-tested gloves, double standard exam gloves, or single standard exam glove |
| Shoe covers | Use in compounding areas only | Work-only washable shoes |
| Safe handling of NIOSH drugs | Poly-coated gown and double chemotherapy tested gloves (single use to hang or take down chemotherapy) | Use one gown per patient – hang gown inside-out near patient and away from surfaces between uses One nurse performs all takedowns of chemotherapy Use gloves only (no gown) for lower hazardous risk drugs |
For infection control and non-hazardous drugs.
People affected by cancer with family members or those in close contact who are infected or suspected with COVID-19 should isolate from these contacts. Patients in such circumstances should be advised to inform their cancer care center of any quarantine requirements. It is important that current health department recommendations regarding isolation and quarantine are followed. All cancer centers should display the symptoms of COVID-19 disease, criteria for when medical advice should be sought, and state the appropriate mode of presentation. For example, services may use a telephone triage, or dedicated COVID-19 community assessment clinics,43 while some countries have built new COVID-19 hospitals within a very short timeframe with isolation and testing facilities.
Impact of COVID-19 on the Nursing Workforce
When facing a large-scale public health event such as COVID-19, the physical and psychological strain on health care professionals cannot be underestimated.44 It has been documented that the main concerns from health care staff during the COVID-19 outbreak in China included being afraid of bringing the virus to their home and families.45 Staff articulated a lack of support in how to manage patients who were unwilling to be quarantined at the hospital, or those patients who did not cooperate with medical measures because of panic.45 Finally, staff articulated concerns about the shortage of PPE and feelings of incapability when faced with critically ill patients45 and difficult decision-making in the allocation of continuous positive airway pressure (CPAP) and ventilators.
Experiences of health professionals during the severe acute respiratory syndrome (SARS) outbreak indicate a sequel of depression, anxiety, fear, frustration,46 and post-traumatic stress.44 Research is currently underway looking into the mental impact of working on the frontline with people infected by COVID-19. Initial data from a large sample (n=1,257) in China suggest similar patterns, with half of the sample of frontline staff experiencing depression and anxiety.47 In fact, being a female nurse indicated a higher risk for depression, anxiety, and psychological distress.47 Caring for deteriorating patients across all ages increases emotional strain and physical exhaustion.48 This experience can be exacerbated when caring for people with cancer; additional burden is placed on overworked nursing staff as the focus shifts to life-preservation, leaving no space for reflection. Re-allocation of the workforce to manage the pandemic can also increase feelings of anxiety because of the potential lack of familiarity in the new role.30 These factors can result in suppressing the natural process of grief and loss and, in the long term, may lead to faster professional burnout.48
Anxiety and depression are two of the most commonly experienced effects of cancer and its treatment49; these can be heightened in the face of an additional life-threatening condition such as COVID-19. Frontline staff are also concerned with how best to identify and manage mental health problems of patients infected by COVID-19, but also how to keep supporting those with pre-existing mental health issues. In existing mental health inpatients, emotional detachment has been observed as a coping strategy.50 At this stage, affected Access to mental health services for managing depression, anxiety, and psychological distress has been reported as a contributing factor for increasing staff stress levels.48 The World Health Organisation51 has released a set of recommendations focusing on ways to cope during the pandemic of COVID-19.
Pandemic nursing workforce planning strategies
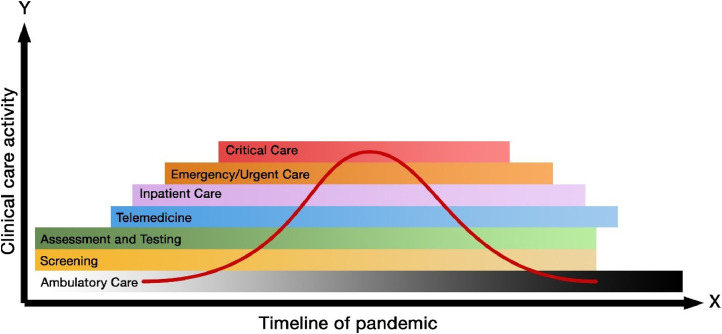
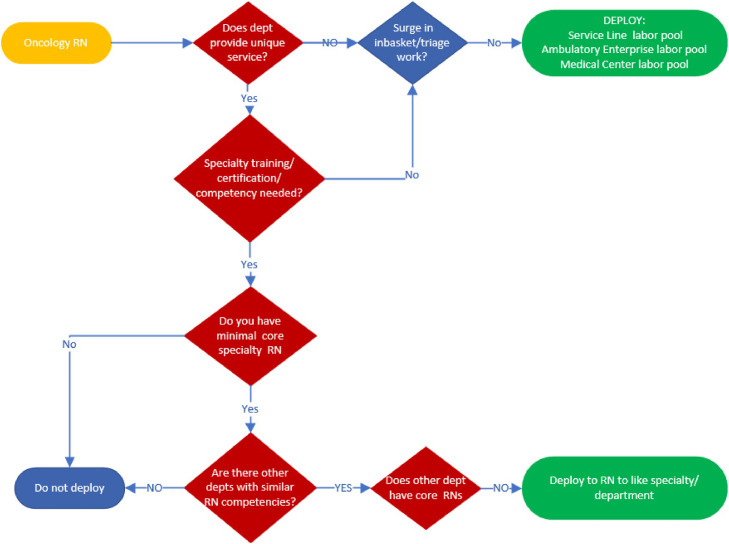
As the number of COVID-19 cases continues to increase, the urgency to flatten the curve52 has enforced stringent measures to reduce exposure of patients and HCWs. Globally, health care organizations have shifted in their approach to care provision. The conversion of clinic visits to telehealth, postponement of routine surveillance appointments, and cancelling of elective procedures are some strategies used to mobilize the nursing workforce reallocation to respond to other duties needed during this crisis. Figure 4 illustrates the nursing workforce during the pandemic phase. Table 4 provides an overview of nursing considerations when developing alternative care delivery models.
Fig. 4.
Illustration of the nursing workforce during a pandemic.
Table 4.
Alternate care delivery model development: nursing considerations
| Nurse scope of practice | Accountability Delegation Supervision |
| Practice considerations | Skills Tasks Setting Required competency |
| Workflow | Geographic clustering Clustering of care |
| Staffing projections | Intensive care unit Inpatient care Ambulatory care (including infusion and radiation oncology) Telehealth |
| Physical resources | Bed availability Equipment PPE |
Health care systems are faced with the increasing pressures of meeting the demands of the pandemic while continuing to meet the needs of the oncology patient population. Emergency preparedness plans provide guidelines for maintaining operations during surge capacity. Department leaders are responsible for identifying core staffing levels for business continuity. Staff unassigned to specific duties within clinical areas may be deployed to a central labor pool to assume various work assignments. Figure 5 is a sample algorithm providing guidance to ensure core staff availability for specialty areas prior to deployment of staff to a labor pool. A comprehensive assessment of previous health care experience, competencies, technical skills, and capabilities of HCWs is a prerequisite to identify educational and training needs during a pandemic.
Fig. 5.
Algorithm for staff deployment to labor pools while ensuring core staff in specialty areas such as cancer care.
Health care organizations are expected to experience staff shortages, and strategies to maintain business operations may include:
-
1.
Staff alternate work agreements - In roles where permitted, telecommuting preserves the health of the cancer workforce by reducing the risk of exposure to COVID-19. With adequate technology, nursing triage, care coordination or navigation, and patient education can be reallocated to those nurses with work restrictions/health concerns. To reduce the frequency of oncology outpatient appointments, nurses can provide telehealth wellness appointments.
-
2.
Consolidation of services and alternate plan for low staffing - Department leaders should identify a discipline-specific staffing threshold that will require a change in standard work. The plan will identify duties or tasks that can be suspended, shifted to other another team member, or shifted to another department. A consolidation plan should be considered to co-locate like services. Expansion of staff work hours may be necessary.
-
3.
Emergency privileges - Temporary or emergency privileges of licensed independent practitioners can be granted to facilitate delivery of critical patient care.
-
4.
Hiring temporary staff– Providing access for external clinical and non-clinical workers to apply for temporary positions during the pandemic should be considered. A survey assessing current role, availability, experience in a health care setting, any specialty clinical experience, and a brief skills inventory will inform appropriate placement. A dedicated team reviewing applications, conducting interviews 7 days a week with flexible hours, and making prompt offers to qualified individuals is crucial.
-
5.
Staff cross-training. Abbreviated orientation to deploy staff to other clinical areas will be important to rapidly activate the nursing labor pool.
Supportive care
Supportive care is defined as a person-centered approach to the provision of tailored services for those living with or affected by cancer to meet their physical, psychological, social, spiritual, or informational needs during diagnosis, treatment, or follow-up phases, including survivorship, palliation, and bereavement.53 People affected by cancer during this pandemic may have different areas of unmet supportive care needs than those already identified in existing systematic reviews.53, 54, 55, 56, 57, 58, 59 There is a greater need for patients in the community setting to develop their confidence and capability in self-management and selfefficacy60 to manage their physical and psychological well-being unsupervised. Nurses play a vital role in supporting self-management and education while providing alternative models of care during the pandemic.
Many people affected by cancer and their loved ones will be distressed and concerned about the real-life impact of COVID-19. It is likely that patients will have a range of unmet informational needs because COVID-19 disease recommendations are likely to change frequently. Oncology nurses should direct patients to evidence-based information and up-to-date resources in their respective countries.
Social isolation/loneliness
As countries are affected by COVID-19 many are implementing social distancing measures, quarantine, self-isolation, and hospital visitor limitations, which undoubtedly will limit opportunities for family support and advocacy. For patient with cancer at high risk of COVID-19, they are being advised to stay at home for a very long time. Moreover, patients in this high-risk group are being advised to stay away from others, including close family members who do not stay in the same household. For example, in the United Kingdom, patients with cancer care are being told to self-isolate up to 6 months.61 To shield the high-risk groups worldwide and reduce the burden on acute care and ICU beds, countries are enforcing lockdowns, curfews, and social isolation to mitigate the spread of this disease. Evidence has already underscored that people affected by cancer can experience loneliness62 , 63 prior to the COVID-19 pandemic. Inevitability, behavioral changes in society for people affected by cancer will impact the experience of boredom,64 sense of connection, social support (including access to emotional, informational, practical, and financial),65 loneliness, and anger.64 Moreover, a recent study has shown that people affected by cancer during this pandemic are at increased risk of depression.66 We strongly advocate for services to recognize these impacts and seek to provide support and intervention using safe non-physical support and contact, such as video or digital technologies67 , 68 or nurse-led telephone services.69
Palliative care
Palliative care services are also affected, facing one of the greatest challenges from the impact of the pandemic. Learning from previous experience on epidemics, the authors have identified issues relating to space and workforce, psycho-social challenges, and issues related to the new profile of the patients that will require palliative care services.70 To date, there is limited evidence on the role of palliative care on managing the COVID-19 pandemic when it should be one of the key components of the strategies. The limited capacity of services to deal with the volume of affected people and families and protective isolation measures that aim to contain transmission can both result in limited or no visits from family members, impacting the preparatory grief processes and the notion of having a good death. Charitable organizations currently offer a range of support services to the public affected by COVID-19.70 , 71
COVID-19 clinical trials/participation in research
Clinical trials in oncology are the most vital approach to improving the management and potential cures for multiple malignancies. Participation in Phase 2 and 3 pharmaceutical trials allow thousands of patients to potentially access and benefit from novel therapeutics. Furthermore, the findings from basic cancer research have informed the development of interventional research in multiple other devastating chronic and acute diseases.
Individual researchers must be aware of issues and guidance specific to their jurisdiction and research methodology. Drug, device, and biological product trials may be immediately impacted. Facility closures, quarantines, and travel restrictions are only a few of the potential restrictions to timely clinical trial conduct.32 Clinical trials personnel and/or trial participants may become infected with COVID-19.
Specific to clinical trial conduct, protocol modifications will be required.72 , 73 Unavoidable protocol deviations and violations will occur as a result of treatment administration or follow-up timing, availability of supportive medications, or multiple other issues specific to a study. Ultimately, safety of the participants and study personnel, maintaining compliance with good clinical practice,74 and minimizing risks to trial integrity remain the critical considerations of principal investigators. Alternative approaches to participation, for example, alternative methods for assessments and follow-up such as phone or video contact, offer not only trial compliance but decreased exposures. Amendments or exceptions to trial activities may be required should alternative approaches be unsatisfactory.
Recognizing the many approaches in oncology research, investigators may benefit from considering alternative methodologies. Surveys, quality-of-life questionnaires, and interviews (individual or online groups) may provide opportunities to explore the cancer experience and avoid viral exposures.
Oncology nursing leadership during crisis management
As a global profession facing a pandemic, leadership lessons can be learned from prior natural disasters, human-created crises, and pandemics to best support the care of patients and HCWs. HCWs and first responders are often the first ones to arrive and care for those in need. Transformational leadership is critical during this time, as well as a structured approach to best support the smallest to largest clinical operation. Transformational leaders are critical during this time of rapid change, when policies and protocols are rapidly evolving, and ambiguity is a constant. Leaders may shift their style in response to the criticality of an event and what is deemed important versus urgent because of the respective timelines of acquiring, negotiating, and planning for critical items to care for patients as well as HCWs.
HCWs suffer during and after crises and psychological first aid is paramount during and after such events.75, 76, 77 Addressing Maslow's hierarchy of needs and ensuring HCW's safety (emotional, physical, and mental) is paramount while a new normal is evolving.78 The oncology nurse leaders’ abilities are critical because they often manage the largest segment of the workforce and need to remain calm, collaborative, and think critically as the situation unfolds. Crisis management and communication plans are critical to organizations. Edmondson and colleagues79 outline the need for nurse leaders to understand the tenets of crisis communication, key behaviors and skills needed during a crisis, priorities within a crisis readiness plan, and the unique role they play.
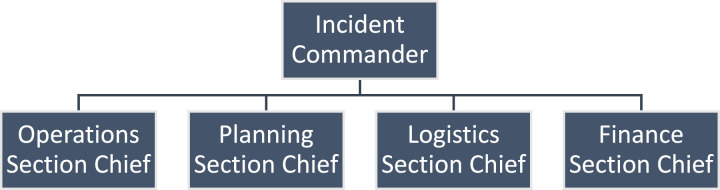
The Hospital Emergency Incident Command System, more commonly referred to as Hospital Incident Command System (HICS) today, was established in the 1980s and 1990s by the Emergency Medical Services Authority.80 This structure provides leaders with an approach that can be applied to a variety of emergencies as well as settings. The model may vary depending upon the type of incident, setting, and resources (see Fig. 6 ). The structure may evolve over time (days to months) depending upon the length of the crisis.
Fig. 6.
Exemplar oncology incident command structure.
The Incident Commander organizes and directs the command center and sets the overall direction. In regard to COVID-19, there may also be other subject matter experts that provide input to the Incident Commander, including infection prevention, infectious disease, laboratory, and risk management. The operations branch is often the largest branch because this involves sub-directors for medical care, infrastructure, hazmat, business continuity, and security. There may also be a staging manager that assists with employee redeployment and equipment and medication staging. The planning branch focuses on resources (human and material), situational, documentation, and demobilization. Planning is essential because traditional hospital units may become COVID-19 units and staffing models may need to be adjusted because of patient surge. The logistics branch focuses on supplies and support of the HCWs and oncology patients. Logistics plays a critical role with oncology HCWs related to PPE and what is required to care for a COVID-19 patient versus routine administration of chemotherapy, when shortages of many products (goggles, masks, gloves, gowns) exists. This branch may also support processes related to N95 mask collection for reuse and sterilization. Finally, the finance branch focuses on time, procurement, compensation/claims, and cost/expenses (see Table 5 for oncology HICS examples). Accurate record-keeping and decision tracking is critical as the situation unfolds. The Incident Commander may establish standing meetings so all section chiefs are aware of key milestones and work plans; this is critical to ongoing success and understanding.
Table 5.
COVID-19 branch work examples
| Operations | Planning | Logistics | Finance |
|---|---|---|---|
| Building of tents for drive up testing Employee screening Lock down of doors Swabbing team Unit staging for COVID-19 rule out and positive Visitor management Visitor screening |
Develops oncology staff redeployment plan. Develops consolidation of sites as volumes decrease Integration of iPads into patient care Telehealth visits for survivorship care |
Inventory of PPE Medical care for health care team Purchasing of PPE |
Tracking and coding of time devoted to response Assists with accounts receivable and payable for expense tracking |
Conclusion
Globally, it is too early to tell what shape COVID-19 will take and its impact on oncology care.
The significance of nurses’ role and contribution is more relevant than ever before; they are the cornerstone of health services, either in the frontline offering compassionate care or in leadership and education by developing and implementing new policies on standards of care.81 COVID-19 poses many challenges for oncology services and people affected by cancer. However, several important clinical considerations have been discussed to inform a way forward in oncology nursing care. The information presented is accurate as of the time of submission.
References
- 1.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 2020;382:1199–1207. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paules C.I., Marston H.D., Fauci A.S. Coronavirus infections-more than just the common cold. JAMA. 2020 doi: 10.1001/jama.2020.0757. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.World Health Organisation. Coronavirus disease (COVID-19) pandemic. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 26 April 2020.
- 4.Xu Z., Shi L., Wang Y. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organisation. Year of the Nurse and the Midwife2020. Available at: https://www.who.int/news-room/campaigns/year-of-the-nurse-andthe-midwife-2020. Accessed 26 April 2020.
- 7.Nursing and Midwifery Board. COVID-19 guidance for nurses and midwives. Available at: https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/COVID19-guidance.aspx. Accessed 25 April 2020.
- 8.Oncology Nursing Society. ONS interim guidelines during the COVID-19 pandemic. Available at: https://www.ons.org/covid-19-interim-guidelines. Accessed 25 April 2020.
- 9.Royal College of Nursing. COVID-19 (coronavirus). Available at: https://www.rcn.org.uk/covid-19. Accessed 23 April 2020.
- 10.Nursing and Midwifery Council. NMC Covid-19 emergency register goes live with more than 7,000 former nurses and midwives ready to support health and social care services across the UK. Available at: https://www.nmc.org.uk/news/press-releases/nmc-covid-19-emergency-register-goes-live/. Accessed 23 April 2020.
- 11.Wu Z., McGoogan J.M.. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 12.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: a nation-wide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organisation. Coronavirus disease (COVID-19) situation report. Available at: https://www.who.int/emergencies/diseases/novelcoronavirus-2019/situation-reports. Accessed 29 April 2020.
- 14.Wall B.M., Keeling A.W.. Springer; New York: 2010. Nurses on the front line: when disaster strikes; pp. 1878–2010. [Google Scholar]
- 15.Sun J., He W.T., Wang L. COVID-19: epidemiology, evolution, and cross-disciplinary perspectives. Trends Molec Med. 2020;25(5):83–495. doi: 10.1016/j.molmed.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Erkoreka A.. Origins of the Spanish Influenza pandemic (1918-1920) and its relation to the First World War. J Mol Genet Med. 2009;3:190–194. doi: 10.4172/1747-0862.1000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taubenberger J.K., Morens D.M.. 1918 Influenza: the mother of all pandemics. Emerg Infect Dis. 2006;12:15–22. doi: 10.3201/eid1201.050979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson N.P., Mueller J.. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull Hist Med. 2002;76:105–115. doi: 10.1353/bhm.2002.0022. [DOI] [PubMed] [Google Scholar]
- 19.Keen-Payne R. We must have nurses: Spanish influenza in America 1918-1919. Nurs Hist Rev. 2000;8:143–156. [PubMed] [Google Scholar]
- 20.Deming D.. Influenza - 1918: Reliving the great epidemic. Am J Nurs. 1957;57:1308–1309. [PubMed] [Google Scholar]
- 21.Keeling A.W.. The Boston Instructive District Nurses Association and the 1918 influenza epidemic: “intelligent cooperation. In: Mann Wall B., Keeling A., editors. Nurses on the front line: when disaster strikes 1878-2010. Springer; New York: 2011. [Google Scholar]
- 22.D'Antonio P., Whelan J.C. Moments when time stood still: Nursing in disaster. Am J Nurs. 2004;104:66–72. doi: 10.1097/00000446-200411000-00032. [DOI] [PubMed] [Google Scholar]
- 23.Nuzzo J, Mullen L, Snyder M, Cicero A, Inglesby TV. Preparedness for a high-impact respiratory pathogen pandemic. Available at: http://www.centerforhealthsecurity.org/our-work/publications/preparedness-for-a-high-impact-respiratory-pathogen-pandemic. Accessed 25 April 2020.
- 24.Centers for Disease Control and Prevention. Introduction to public health. In: Public Health Series. Available at: https://www.cdc.gov/publichealth101/epidemiology.html. Accessed 20 April 2020.
- 25.Chotiner I.. A medical historian on why we must stay the course in fighting the coronavirus: an interview with Howard Markel; The New Yorker; April 1, 2020. [Google Scholar]
- 26.Del Rio C., Malani P.N. COVID-19—new insights on a rapidly changing epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3072. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Fauci A.S., Lane H.C., Redfield R.R. Covid-19—navigating the uncharted. N Engl J Med. 2020;382:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ellen J. Tracking infection. City Journal. Available at: https://www.city-journal.org/covid-19-contact-tracing. Accessed 25 April 2020.
- 29.World Health Organisation. Contact tracing: Online Q & A. Available at: https://www.who.int/features/qa/contact-tracing/en/. Accessed 25 April 2020.
- 30.Centers for Disease Control and Prevention. Coronavirus (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/index.html. Accessed 24 April 2020.
- 31.Ueda M., Martins R., Hendrie P.C. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Canc Netw. 2020 doi: 10.6004/jnccn.2020.7560. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 32.The Lancet Oncology COVID-19: Global Consequences for Oncology. Lancet Oncol. 2020;21:467. doi: 10.1016/S1470-2045(20)30175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guan W.J., Zhong N.S.. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020:382. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus - infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mehta P., McAuley D.F., Brown M. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chan J.F.-W., Yuan S., Kok K.-H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating personto-person transmission: a study of a family cluster. The Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Phan L.T., Nguyen T.V., Luong Q.C. Importation and human-to-human transmission of a novel coronavirus in Vietnam. N Engl J Med. 2020;382:872–874. doi: 10.1056/NEJMc2001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organisation. Health workforce nursing and midwifery. Available at: https://www.who.int/hrh/nursing_midwifery/en/. Accessed 23 April 2020.
- 40.The Lancet Oncology COVID-19: Protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Rashdan A., Roumelioutis M., Quirk S. Adapting radiotherapy treatments for breast cancer patients during the COVID-19 pandemic: hypofractionation and accelerated partial breast irradiation to address World Health Organization recommendations. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.011. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fairchild A., Barnes E., Ghosh S. International patterns of practice in palliative radiotherapy for painful bone metastases: evidence-based practice? Int J Radiat Oncol Biol Phys. 2009;75:1501–1510. doi: 10.1016/j.ijrobp.2008.12.084. [DOI] [PubMed] [Google Scholar]
- 43.Haines A., de Barros E.F., Berlin A., Heymann D.L., Harris M.J. National UK programme of community health workers for COVID-19 response. Lancet. 2020;395:1173–1175. doi: 10.1016/S0140-6736(20)30735-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wu P., Fang Y., Guan Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen Q., Liang M., Li Y. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu T., Chen X., Miao G. Recommendations on diagnostic criteria and prevention of SARS-related mental disorders. J Clin Psychol Med. 2003;13:188–191. [Google Scholar]
- 47.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ayanian JZ. Mental health needs of health care workers providing frontline COVID 19 care. NAMA Network. Available at: https://jamanetwork.com/channels/healthforum/fullarticle/2764228. Accessed 25 April 2020. [DOI] [PubMed]
- 49.Pitman A., Suleman S., Hyde N., Hodgkiss A. Depression and anxiety in patients with cancer. BMJ. 2018;361:k1415. doi: 10.1136/bmj.k1415. [DOI] [PubMed] [Google Scholar]
- 50.National Association of Psychiatric Intensive Care & Low Secure Units. Managing acute disturbance in the context of COVID-19. Available at: https://napicu.org.uk/wp-content/uploads/2020/03/COVID-19_guidance_appendix.pdf. Accessed 23 April 2020.
- 51.World Health Organisation. Mental health and psychosocial considerations during the COVID-19 outbreak. Available at: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf. Accessed 23 April 2020.
- 52.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395:931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Paterson C., Robertson A., Smith A., Nabi G. Identifying the unmet supportive care needs of men living with and beyond prostate cancer: a systematic review. Eur J Oncol Nurs. 2015;19:405–418. doi: 10.1016/j.ejon.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 54.Hyun Y.G., Alhashemi A., Fazelzad R., Goldberg A.S., Goldstein D.P., Sawka A.M. A systematic review of unmet information and psychosocial support needs of adults diagnosed with thyroid cancer. Thyroid. 2016;26:1239–1250. doi: 10.1089/thy.2016.0039. [DOI] [PubMed] [Google Scholar]
- 55.Kotronoulas G., Papadopoulou C., Burns-Cunningham K., Simpson M., Maguire R. A systematic review of the supportive care needs of people living with and beyond cancer of the colon and/or rectum. Eur J Oncol Nurs. 2017;29:60–70. doi: 10.1016/j.ejon.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 56.Maguire R., Kotronoulas G., Simpson M., Paterson C. A systematic review of the supportive care needs of women living with and beyond cervical cancer. Gynecol Oncol. 2015;136:478–490. doi: 10.1016/j.ygyno.2014.10.030. [DOI] [PubMed] [Google Scholar]
- 57.Maguire R., Papadopoulou C., Kotronoulas G., Simpson M.F., McPhelim J., Irvine L. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs. 2013;17:449–464. doi: 10.1016/j.ejon.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 58.Paterson C., Jensen B.T., Jensen J.B., Nabi G. Unmet informational and supportive care needs of patients with muscle invasive bladder cancer: a systematic review of the evidence. Eur J Oncol Nurs. 2018;35:92–101. doi: 10.1016/j.ejon.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 59.Puts M.T., Papoutsis A., Springall E., Tourangeau A.E. A systematic review of unmet needs of newly diagnosed older cancer patients undergoing active cancer treatment. Support Care Cancer. 2012;20:1377–1394. doi: 10.1007/s00520-012-1450-7. [DOI] [PubMed] [Google Scholar]
- 60.Paterson C.. An ecological momentary assessment of self-management in prostate cancer survivors. J Cancer Surviv. 2019;13:364–373. doi: 10.1007/s11764-019-00758-w. [DOI] [PubMed] [Google Scholar]
- 61.United Kingdom Government. Coronavirus what you need to do. Available at: https://www.gov.uk/coronavirus. Accessed 27 April 2020.
- 62.Deckx L., van den Akker M., Buntinx F. Risk factors for loneliness in patients with 778 cancer: a systematic literature review and meta-analysis. Eur J Oncol Nurs. 2014;18:466–477. doi: 10.1016/j.ejon.2014.05.002. 779. [DOI] [PubMed] [Google Scholar]
- 63.Gray T.F., Azizoddin D.R., Nersesian P.V. Loneliness among cancer caregivers: a narrative review. Palliat Support Care. 2019;4:1–9. doi: 10.1017/S1478951519000804. [DOI] [PubMed] [Google Scholar]
- 64.Xiang Y.T., Yang Y., Li W., Zhang L., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cohen S.E., Syme S. Academic Press; Orlando, FL: 1985. Social support and health. [Google Scholar]
- 66.Zheng X., Tao G., Huang P. Self-reported depression of cancer patients under 2019 novel coronavirus pandemic. Lancet. 2020 doi: 10.2139/ssrn.3555252. [Epub ahead of print] [DOI] [Google Scholar]
- 67.Larson J.L., Rosen A.B., Wilson F.A. The effect of telehealth interventions on quality of life of cancer survivors: a systematic review and meta-analysis. Health Informatics J. 2019 doi: 10.1177/1460458219863604. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 68.Zhou X., Snoswell C.L., Hardling L.E. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemedicine and e-Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 69.Wu Q., Kue J., Zhu X. Effects of nurse-led support via WeChat, a smartphone application, for breast cancer patients after surgery: a quasi-experimental study. Telemedicine J E Health. 2019;26:226–234. doi: 10.1089/tmj.2018.0293. [DOI] [PubMed] [Google Scholar]
- 70.Macmillan Cancer Support. End of life care and coronavirus. Available at: https://www.macmillan.org.uk/coronavirus/end-of-life-care-and-coronavirus. Accessed 26 April 2020.
- 71.Cruse Bereavement Care. Coronavirus: dealing with bereavement and grief. Available at: https://www.cruse.org.uk/get-help/coronavirus-dealingbereavement-and-grief. Accessed 26 April 2020.
- 72.National Institutes of Health. Guidance for NIH-funded clinical trials and human subjects’ studies affected by COVID-19. Available at: https://grants.nih.gov/grants/guide/notice-files/NOT-OD-20-087.html. Accessed 25 April 2020.
- 73.US Food and Drug Administration. FDA guidance on conduct of clinical trials of medical products during COVID-19 pandemic guidance for industry, investigators, and institutional review boards. Available at: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/fda-guidanceconduct-clinical-trials-medical-products-during-covid-19-pandemic. Accessed 25 April 2020.
- 74.World Medical Association. WMA Declaration of Helsinki - ethical principles for medical research involving human subjects. Available at: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/. Accessed 26 April 2020.
- 75.Kerfoot K.. Leading through the blur: leadership in difficult times. Nursing Economics. 2001;19:291–293. [PubMed] [Google Scholar]
- 76.Everly G.S., Barnett D.J., Sperry N.L., Links J.M. The use of psychological first aid (PFA) training among nurses to enhance population resiliency. Int J Emerg Ment Health. 2010;12(1):21–31. [PubMed] [Google Scholar]
- 77.Wester M., Giesecke J. Ebola and healthcare worker stigma. Scand J Public Health. 2019;47:99–104. doi: 10.1177/1403494817753450. [DOI] [PubMed] [Google Scholar]
- 78.Petro-Yura H., Walsh M.B.. Appleton-Century-Crofts; New York: 1983. Human needs and the nursing process. [Google Scholar]
- 79.Edmonson C., Sumagaysay D., Cueman M., Chappell S. The nurse leader role in crisis management. J Nurs Adm. 2016;46:417–419. doi: 10.1097/NNA.0000000000000367. [DOI] [PubMed] [Google Scholar]
- 80.California Emergency Medical Services Authority. HICS history and background. Available at: https://emsa.ca.gov/hics-history-and-background/. Accessed 27 April 2020.
- 81.World Health Organisation. State of the world's nursing report - 2020. Available at: https://www.who.int/publications-detail/nursing-report-2020. Accessed 27 April 2020.