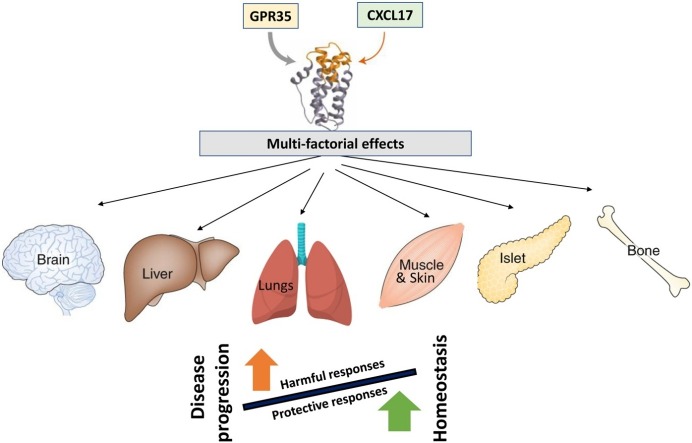
Graphical abstract
Abbreviations: 1ICW, interleukin-8 mutant with Glu 38 replaced by Cys and Cys 50 replaced by Ala; ADP, adenosine diphosphate; AMPK, activated protein kinase; AMPs, antimicrobial peptides; ang-2, angiopoietin2; APCs, antigen-presenting cells; BAL, bronchioalveolar lavage; BEAS-2B, immortalized human bronchial epithelial cells; bFGF, basic fibroblast growth factor; cAMP, cyclic adenosine monophosphate; CCL16, C-C motif chemokine ligand 16; CCL17, C-C motif chemokine ligand 17; CCL20, C-C motif chemokine ligand 20; CCL24, C-C motif chemokine ligand 24; CCL25, C-C motif chemokine ligand 25; CCL26, C-C motif chemokine ligand 26; CCL28, C-C motif chemokine ligand 28; CCR2, C-C motif chemokine receptor 2; CCR5, C-C motif chemokine receptor 5; CD102, cluster of differentiation 102; CD11b, cluster of differentiation 11b; CD138, cluster of differentiation 138; CD68, cluster of differentiation 68; CD8, cluster of differentiation 8; CXCL14, C-X-C motif chemokine ligand 14; CXCL15, C-X-C motif chemokine ligand 15; CXCL16, C-X-C motif chemokine ligand 16; CXCL-17, C-X-C motif chemokine 17; CXCL5, C-X-C motif chemokine ligand 5; CXCL8, C-X-C motif chemokine ligand 8; CXCR2, C-X-C motif chemokine receptor 2; CXCR3, C-X-C motif chemokine receptor 3; CXCR4, C-X-C motif chemokine receptor 4; CXCR6, C-X-C motif chemokine receptor 6; CXCR7, C-X-C motif chemokine receptor 7; Da, Daltons; DCs, dendritic cells; DLD-1, D.L. Dexter colon cancer cell line 1; DMC, dendritic cell and monocyte-like protein; EAE, experimental autoimmune encephalomyelitis; ELR, glutamic acid-leucine-arginine triad; ERK1/2, extracellular signal-regulated kinase 1/2; Foxp3, forkhead box P3; GPCR, G protein–coupled receptor; GPR, G protein-coupled receptor; Gr-1, Ly-6G/Ly-6C; GRO-1, growth-regulated oncogene 1; GTP, guanosine triphosphate; HaCaT, human keratinocyte cell line; HepG2, human hepatocellular carcinoma cell line; HHC, human hepatocellular carcinoma; HMVEC, human microvascular endothelial cells; HSV, herpes simplex virus; HUVEC, human umbilical vascular endothelial cells; ICAM2, intracellular adhesion molecule 2; IFN-γ, interferon gamma; IL-10, interleukin 10; IL-12, interleukin 12; IL-13, interleukin 13; IL-17A, interleukin 17A; IL-22, interleukin 22; IL-23, interleukin 23; IL-8, interleukin 8; ILC 3, group 3 innate lymphoid cells; IPF, interstitial pulmonary fibrosis; JAK, Janus kinase; JNK, c-Jun N-terminal kinase; Ki67, antigen Ki67; Leu, leucine; LPS, lipopolysaccharide; MAPKs, mitogen-activated protein kinases; MDSCs, myeloid-derived stem cells; miR-221-3p, micro RNA 221-3p; mRNA, messenger RNA; NHEKs, normal human epidermal keratinocytes; NIH3T3, normal embryonic mouse fibroblast cell line; NSCLC, non-small cell lung cancer; ONPG, nitrophenyl-b-d-galactopyranoise; Phe, phenylalanine; PI3K, phosphatidylinositol-3-kinase; POSTN, periostin; PTX, Pertussis toxin; SIRT1, sirtuin-1; SPDI, Secreted Protein Discovery Initiative; SPVEC, sephranose vascular endothelial cells; STAT, signal transducer and activator of transcription; SW620, human colon cancer cell line; TB, tuberculosis; THP-1, human leukemia monocytic cell line; TNF-α, tumor necrosis factor alpha; Treg, T regulatory cells; uPA, urokinase-type plasminogen activator; uPAR, urokinase-type plasminogen activator receptor; UTR, untranslated region; VCC-1, VEGF co-regulated chemokine 1; VEGF-A, vascular endothelial growth factor A
Keywords: Chemokines, CXCL-17, Mucosal immunology, Pulmonary diseases, Respiratory infections, Lung cancer
Highlights
-
•
C-X-C motif chemokine 17 (CXCL17), plays a functional role in maintaining homeostasis at mucosal barriers.
-
•
CXCL17 expression is associated with both disease progression and protection in various diseases.
-
•
The multifactorial mechanistic properties of CXCL17 could be exploited as a therapeutic target
Abstract
C-X-C motif chemokine 17 (CXCL-17) is a novel chemokine that plays a functional role maintaining homeostasis at distinct mucosal barriers, including regulation of myeloid-cell recruitment, angiogenesis, and control of microorganisms. Particularly, CXCL17 is produced along the epithelium of the airways both at steady state and under inflammatory conditions. While increased CXCL17 expression is associated with disease progression in pulmonary fibrosis, asthma, and lung/hepatic cancer, it is thought to play a protective role in pancreatic cancer, autoimmune encephalomyelitis and viral infections. Thus, there is emerging evidence pointing to both a harmful and protective role for CXCL17 in human health and disease, with therapeutic potential for translational applications. In this review, we provide an overview of the discovery, characteristics and functions of CXCL17 emphasizing its clinical potential in respiratory disorders.
1. Introduction
The respiratory tract plays a vital role in respiratory physiology by enabling gas exchange at the alveolar/capillary membrane. As such, the airways are in continuous contact with the airborne particulate matter, and the respiratory epithelium is colonized by several species of virus, bacteria, and fungi [1]. Nonetheless, infection and disease progression is prevented by the innate pulmonary defense mechanisms [1]. While the continuous functioning of the immune system is necessary to maintain respiratory barrier integrity against microbes, it is also regulated to prevent excessive tissue damage and inflammation. Several cytokines and chemokines shape the magnitude and quality of immune responses occurring at the lungs [2]. Specifically, chemokines regulate the cellular composition of mucosal tissue by inducing the migration of leukocytes and other non-immune cells expressing their cognate receptors [3]. Twenty three chemokine receptor subsets have been identified in humans and are broadly classified into atypical chemokine receptors (n = 4) or the G protein–coupled chemotactic chemokine receptors (n = 19) [4,5]. Although certain chemokine-receptor pairs are highly specific and unique (such as CXCR6/CXCL16), often several chemokine/receptor pairs can be formed, each one with variable specificity depending on the cellular targets induced to migrate [3]. Depending on the differential receptor expression and usage, as well as the potential agonism or antagonism initiated by the chemokine-receptor binding, the functions observed in vivo for chemokines acting at the same G protein–coupled receptor (GPR) might vary [6]. The binding of chemokines to their receptors triggers a chain of molecular events including the dissociation of GTP-bound Gαi subunits from Gβ/γ heterodimers, which initiates calcium release from the endoplasmic-reticulum reservoirs and further activation of calcium-dependent signaling. These events lead to the downstream initiation of JAK/STAT, mitogen-activated protein kinases (MAPKs), and phosphatidylinositol-3-kinase (PI3K) pathways which eventually govern the functional responses induced by these chemokines [7,8].
Chemokines are relatively small molecules classified in four subfamilies according to the number of amino acids (represented by a X) located between the two conserved cysteines (C) at their amino-terminal domain: CXC (α), CC (β), XC (γ), and CX3C (δ) [3,9]. Members of the CXC family can be subdivided based on the presence or absence of the triad glutamic acid-leucine-arginine (ELR) preceding the CXC sequence as ELR-positive or ELR-negative [10]. Besides this structural classification, chemokines are also grouped as “homeostatic” or “inflammatory” based on their physiological properties. Additionally, a third group of “dual” chemokines are recognized which includes those that have overlapping functions [11]. While most of the chemokines have been functionally designated into one of the above-mentioned categories, some chemokines such as CCL16, CXCL15 and CXCL17 are yet to be assigned a specific functional role.
Beyond their immunological functions, chemokines display other biological properties such as induction of stem cell mobilization, promotion of cellular growth, angiogenesis, and bactericidal activity [10,12]. While chemokines are active in their monomeric form, they also form homo- or heterodimers with one or more chemokine species. The resultant chemokine-receptor interactome formed play pivotal roles in processes like embryogenesis, wound healing, vascularization, and pathogen clearance which are beneficial to the host. However, chemokines can also participate in the pathological mechanisms that drive autoimmunity, chronic inflammation, and cancer [13]. Indeed, there is increasing evidence of their implications in clinically relevant pulmonary disorders [[14], [15], [16], [17]]. Hence, these mediators represent promising new targets for translational research, as they could be manipulated to block chemokine/receptor axes implicated in pathological conditions or harnessed in order to promote beneficial chemokine-mediated mechanisms. Despite remarkable advances, some gaps in the understanding of chemokine/receptor networks have delayed their therapeutic use in humans, especially of those chemokines recently discovered whose functions have not been fully characterized such as CXCL17.
CXCL17, a myeloid cell-attracting chemokine, also known as dendritic cell and monocyte-like protein (DMC) or VEGF co-regulated chemokine 1 (VCC-1), is the newest member of the CXCL family of chemotactic cytokines described so far [18]. CXCL17 is produced along the airways both at steady state and induced under inflammatory conditions [19,20], suggesting a role in local immune responses at the respiratory system. Current attempts to characterize the biology of CXCL17 have revealed its involvement in maintenance of homeostasis and cellular composition at different epithelial surfaces. Moreover, recent studies show that CXCL17 is involved in several human health and disease playing either a protective or pathologic role, respectively. Thus, in this review we provide an overview of the discovery, characteristics and functions of CXCL17, specifically discussing its translational potential as a diagnostic biomarker and therapeutic agent in pulmonary medicine.
2. Molecular biology of CXCL17
CXCL17 gene was first described in 2003 by researchers of the Secreted Protein Discovery Initiative (SPDI) [18]. Amino acid sequence-based comparisons revealed similarities with CCL16 and CCL17 [20]. Structural analysis showed an IL-8-like fold similar to that adopted by 1ICW (a mutant of IL-8 with a CXC chemokine core [21]) and CXCL8. Together these findings suggested that the identified protein was a chemokine of the CXC- ligand chemokine family [19].
The CXCL17 gene, located at 19q13.2, is composed of four exons coding a 119 amino acids pro-peptide with a molecular weight of ∼13,819 Da in humans and ∼13,628 Da in mice. Mouse and human immature versions of CXCL17 share 71 % amino acid sequence identity [19,20]. Moreover, the pattern of CXCL17 expression is similar in mucosal tissues of both human and murine species [[22], [23], [24]]. These precursor proteins have six cysteine residues between Leu24 to Leu119, but only four of them (located among Phe64 to Leu119) participate in the building of the CXC motif. Post-translational cleavage removes a 22 amino acids sequence containing two cysteine residues from the amino-terminal domain, which result in a mature protein of 11,418 Da in humans and 11,164 Da in mice [19,20,23]. This maturation process leads to attainment of the full functional capacity of CXCL17, as the four-cysteine mature peptide has a two-fold increase in chemoattractant activity to recruit human THP-1 monocytes and mouse J774 macrophages in vitro, compared with the six-cysteine pro-peptide [23]. Therefore, the amino-terminal sequence may affect the affinity during the receptor binding process, although other functions of this cleaved fraction remain to be elucidated.
3. CXCL17 receptor
The identity of the CXCL17 receptor is somewhat controversial. This chemokine does not have affinity for CCR2, CCR5, CXCR2, CXCR3, CXCR4, and CXCR7 [25]. So far, it has been described that CXCL17 induces a dose-dependent calcium flux in pro B-cell line Ba/F3 cells transfected with GPR35 [25]. However, silencing or antagonism of GPR35 does not inhibit migration of THP-1 and primary human monocytes in responses to a CXCL17 gradient [26,27]. These findings suggest that GPR35 lacks a selective ligand [28], thereby excluding its sole responsibility for CXCL17 activity and raising the possibility of the presence of another as yet unidentified receptor [26]. Despite this, it is now established that CXCL17-induced cell migration is inhibited by Pertussis toxin (PTX) which reduces the affinity of GPR35 for its agonist via ADP ribosylation of Gαi/o heterotrimeric proteins and resultant uncoupling of the GPCR from the G proteins [22,29,30]. Furthermore, there is evidence showing that intracellular signals triggered by the attachment of CXCL17 to its receptor involves the second messenger cyclic adenosine monophosphate (cAMP), and activates the extracellular signal-regulated kinase 1/2 (ERK1/2) and p38 MAPKs pathways [23]. Therefore, most published studies support the fact that CXCL17 receptor is a GPCR with seven transmembrane domains such as GPR35.
4. Tissue expression of CXCL17 under steady state conditions
CXCL17 is a novel member of the group of mucosal chemokines (CCL25, CCL28, and CXCL14) and is expressed in the respiratory and gastrointestinal tracts. CXCL17 expression in healthy human tissues and cell lines showed its basal production in fetal lung samples, as well as in adult trachea, epithelium of bronchi, bronchioles, and alveolar cells [19,20]. Also, its expression is detected in the stomach, small intestine and colon, specifically within the lining epithelium at the luminal surface of epithelial cells, suggesting an active process of secretion of this chemokine into the airways and intestinal lumen, respectively [19,24]. Interestingly, the distribution of CXCL17 is almost restricted to the epithelial barriers that cover the lumen of several hollow organs and secretory conducts, in contrast with other mucosal chemokines, such as CXCL14 and CCL25, which can also be found within the solid parenchyma of different tissues at steady state [[31], [32], [33]]. Notably, lungs and airways also show significant CXCL17 expression in various species of mammals including humans, cattle, sheep, mice and rats, thus supporting a potential role of this chemokine in the physiology of the respiratory epithelium. The tissue expression profile of CXCL17 in human and murine species has been previously described [19,20,23,24,29,34,35], and is summarized in Table 1 .
Table 1.
Basal expression of CXCL17 in different species of mammals.
| Species | Distribution of CXCL17 expression | References |
|---|---|---|
| Human | Fetal lung, trachea, bronchi, bronchioles, alveoli, stomach, small intestine, colon, tongue, urethra, female reproductive system, skeletal muscle, pancreas. | [19,20,24,29] |
| Mice | Lung, thyroid, submaxillary gland, epididymis, uterus, ovary, prostate, brain. | [20,34,35] |
| Rat | Trachea, salivary gland, duodenum, stomach. | [23] |
5. Functional role of CXCL17 in maintaining homeostasis
5.1. Chemotactic properties
CXCL17 is known to induce the migration of monocytes, dendritic cells (DCs) and macrophages via ERK1/2 and p38 but not JNK signaling [19,23,36]. Although CXCL17 has a chemotactic effect on all APCs, it differs in strength between the APC subsets. For instance, mature and immature DCs mobilization responses are weaker compared with those of monocytes [29]. Also, as mentioned before, the four-cysteine mature version of CXCL17 has higher chemoattractant activity over human monocytes and mouse macrophages compared with the six-cysteine pro-peptide [23].
Thus, due to the steady state expression of CXCL17 in the mucosa and endothelial cells of respiratory and gastrointestinal tracts [29], it likely facilitates the infiltration of APCs into such epithelial barriers, where these cells play important functions sensing the antigen composition of the luminal environment. Indeed, CXCL17−/− mice exhibit a slight decrease in the number of alveolar macrophages but have normal number of lung interstitial macrophages, with no differences in cellular subsets in other tissues [36]. Other cells may amplify CXCL17 signaling from the epithelium, such as endothelial cells which are also producers of CXCL17 [24], suggesting that this chemokine facilitates the exit of APCs from the vasculature. Indeed, pretreatment of monocytes and DCs with CXC17 enhances their ability to attach to the intracellular adhesion molecule 2 (ICAM2, also known as CD102), an integrin binding protein relevant for leukocyte traffic across endothelium [29].
It is of interest to note that this chemoattractant property of CXCL17 is restricted to the APCs and not lymphocytes [19]. Thus, the specificity of CXCL17 to impact innate immune responses and not adaptive immunity might suggests a differential role for this chemokine in infectious and metabolic diseases.
5.2. Angiogenic effect
Angiogenic activity of CXC chemokines is dependent on the presence or absence of the ELR motif [10,37]. Although the ELR motif has not been described in CXCL17, functionally it behaves as a member of the group of angiogenic factors [20,23,38]. In fact, several human endothelial cell lines such as human microvascular endothelial cells (HMVEC), sephranose vascular endothelial cells (SPVEC) and human umbilical vascular endothelial cells (HUVEC) express higher levels of CXCL17 during proliferation or tube formation [20]. HUVEC cells transfected with CXCL17 increase their expression of genes involved in angiogenesis, such as vascular endothelial growth factor (VEGF-A), basic fibroblast growth factor (bFGF), angiopoietin-2 (ang-2), urokinase-type plasminogen activator (uPA), and uPA receptor (uPAR) [20]. Also, treatment of THP-1 monocytes with mature CXCL17 enhances their ability to produce VEGF-A [23]. Additionally, expression of CXCL17 is co-regulated with other proangiogenic molecules as IL-8, GRO-1 and VEGF in samples from lung, breast and esophageal cancers [20]. Finally, CXCL17 is one of the most important genes mutated within specific genetic loci of stroke susceptibility in stroke-prone spontaneously hypertensive rats, a murine model of spontaneous cerebral hemorrhage suggesting a potential participation of this chemokine in the maintenance of vascular structure [38].
5.3. Antimicrobial activity
Similar to other mucosal-associated such as CCL28 and CXCL14 [39,40], CXCL17 also exhibits broad spectrum anti-microbial activity in a dose dependent manner against Escherichia coli, Staphylococcus aureus, Salmonella sp., Pseudomonas aeruginosa and Candida albicans [24]. Interestingly, CXCL17 does not kill the known probiotic Lactobacillus casei, which downregulates the pro-inflammatory responses elicited by pathogenic bacteria like E.coli [41,42], indicating the selective and beneficial nature of this chemokine as a potential shaping factor of the microbiome.
While the killing activity of mucosal chemokines such as CCL28 and CXCL14 is retained within their carboxyl-terminal domain and amino-terminal respectively [39,40], that of CXCL17 is yet to be discovered [24]. A possible mechanism underlying the bactericidal effect of CXCL17 is associated with membrane permeabilization, as shown in assays using E. coli ML35 cells, in which exposure to the chemokine resulted in hydrolysis of extracellular nitrophenyl-b-d-galactopyranoise (ONPG) by cytoplasmic b-galactosidase [24]. This membrane permeabilizing effect of CXCL17 is akin to that of AMPs such as granulysin, which can permeabilize cholesterol free microbial membranes but is largely ineffective against intracellular pathogens [43]. Therefore, targeted studies to define the peptide sequences determining the bactericidal features of CXCL17 would pave the way for the complete characterization of this novel chemokine to enable its optimum assessment as a potential therapeutic target.
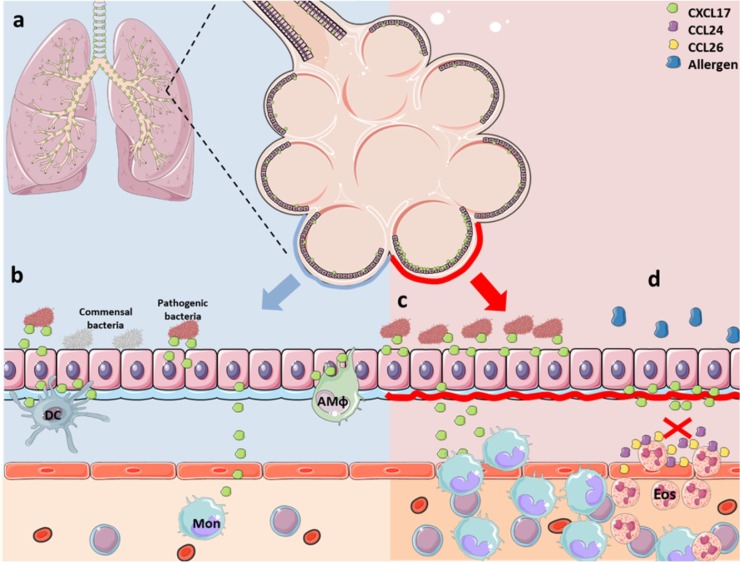
The multifaceted biological activities exhibited by CXCL17 are shown in Fig. 1 .
Fig. 1.
Biological activities of CXCL17.
The functions of CXCL17 are illustrated by exemplifying its possible participation in the maintenance of homeostasis of the respiratory tract. (a) CXCL17 expression is restricted to the lining epithelium of the airways and distant alveoli. (b) CXCL17 has a potent bactericidal activity over pathogenic bacterial strains, but not against commensal bacteria, suggesting a role in shaping the composition of bacterial community residing at different epithelial surfaces. In addition, CXCL17 controls the recruitment of certain subsets of myeloid cells, such as dendritic cells, monocytes and macrophages across the endothelium into the epithelium. (c) During mucosal infections, production of CXCL17 may increase to counteract bacterial replication by its direct antimicrobial activity, or via regulating the infiltration of myeloid cells into the infected epithelium. (d) CXCL17 also plays an anti-inflammatory role, as illustrated in the case of eosinophilic inflammation of the airways elicited by allergens in patients with type 2 asthma. In these settings, CXCL17 inhibits the production of chemokines important for the recruitment of eosinophils, such as CCL24 and CCL26. AMφ, alveolar macrophages; DC, dendritic cells; Eos, eosinophils; Mon, monocytes. The art pieces used in this figure were modified from Servier Medical Art by Servier, licensed under a Creative Commons Attribution 3.0 Unported License (https://smart.servier.com/).
6. Regulation of CXCL17 production under pathological conditions
CXL17 is considered a “dual chemokine”, due to its high levels of basal expression as well as induced expression during disruption of homeostasis. Although exposure to both commensal and pathogenic microorganisms at the different mucosal surfaces triggers CXCL17 production, the levels induced by commensal microorganisms are much lower in comparison to those induced by pathogenic microorganisms [36], such as the herpes simplex virus (HSV) [44]. This phenomenon is mainly observed at the lung and stomach mucosal surface, suggesting a potential importance of this chemokine in the interaction between mucosal defenses and the respiratory/intestinal microbiome, as well as in the responses against infectious aggressions.
The production of CXCL17 is potentiated by pro-inflammatory signals provided by other cytokines. Treatment of HaCaT cells and normal human epidermal keratinocytes (NHEKs) with IFN-γ was shown to increase the production of CXCL17 in a dose-dependent manner [45]. This increase was also observed in primary gastric cells in response to lipopolysaccharide (LPS) and alcohol [23], confirming that pro-inflammatory signals induce CXCL17 production and demonstrating that other cell types may also become reservoirs of this protein under certain inflammatory conditions. The cellular subsets, receptors and signaling agents responsible for exacerbated CXCL17 production at the mucosal surfaces is yet to be fully understood. However, there is some evidence of post-transcriptional regulation of CXCL17 expression with recent data indicating that CXCL17 is a target of miR-221-3p, as the 3′-untranslated region (UTR) of CXCL17 gene contains sequences that match with the sequence of has-miR-221-3p. Indeed, transfection of human BEAS-2B bronchial cells with this miRNA suppressed expression of CXCL17 [46]. These observations shed light about the regulatory mechanisms of CXCL17 production specifically at the lung airways.
7. CXCL17 in human diseases
7.1. CXCL17 in inflammatory and autoimmune disorders
Due to its significant in vivo physiological role both under homeostasis and pathogenesis CXCL17 is considered as a principal player in different diseases and disorders. Interestingly, CXCL17 expression is also increased in the skin under pathological conditions such as psoriasis. In fact, CXCL17 expression is reported to be increased in skin specimens from humans with psoriasis and mice with imiquimod-induced psoriasis-like skin inflammation [45], wherein the epidermal keratinocytes are the main source of CXCL17 production [45]. A recent communication also reported higher levels of CXCL17 in saliva and lacrimal fluid from patients affected by Sjögren syndrome, although this did not correlate with disease severity [47].
Despite these data, the pathogenic or regulatory nature of the CXCL17 production during inflammatory settings is not clear. Currently there is a concise body of evidence suggesting that CXCL17 is an anti-inflammatory mediator in conditions such as experimental psoriasis in mice, autoimmune diseases and respiratory afflictions in humans [35,45,46]. Indeed, in mice with experimental psoriasis, the local administration of CXCL17 has been related to a reduced infiltration of lymphocytes and neutrophils in the skin, reduced T cell responses as well as lower local levels of IL-17A, IL-22, TNF-α, IL-12 and IL-23, but increased expression of IL-10 and Foxp3 [45]. These changes are also associated with recruitment of myeloid-derived stem cells (MDSCs) to the sites of CXCL17 exposure, which subsequently attract T regulatory (Treg) cells in a CCL4- and CCL5-dependent way [45]. Moreover, in vitro assays have shown that the CXCL17 treatment also attenuates the LPS-induced production of inflammatory cytokines and nitric oxide by macrophages [23]. Finally, the genetic knockdown of CXCL17 in mice has been recently associated with increased susceptibility to autoimmunity in a model of experimental autoimmune encephalomyelitis (EAE), suggesting that deficiencies in CXCL17 signaling are important for the development and maintenance of auto-tolerance [35]. Collectively, these data strengthen the notion that CXCL17 has a potent anti-inflammatory role in autoimmune diseases.
7.2. CXCL17 in infectious diseases
Chemokine/receptor axes are known mediate both protection and susceptibility against microorganisms via its antibacterial activity and recruitment of leukocytes or by promoting pathogen dissemination, respectively [[48], [49], [50], [51], [52], [53], [54], [55]]. In this context, the role of CXCL17 in the immunity to infection remains under investigation. Recently, it was observed that expression of CXCL17 was highly increased in the duodenum of humans with acute cholera, but the nature of its contribution to the defense against Vibrio cholerae was undetermined [56]. Likewise, in a mouse model of HSV-1 infection, the inoculation of the virus enhanced CXCL17 production at the vaginal mucosa of mice [44]. Concurrently, mice deficient in CXCL17 were more susceptible to HSV-1, as they could not control viral replication nor virus dissemination to the dorsal ganglia. These disease phenotypes were associated with decreased proportion of GPR35-expressing antigen-specific memory CD8+T cells within the vaginal tissue of these animals [44]. The broad-spectrum bactericidal activity of CXCL17 against bacteria associated with respiratory infections indicates the involvement of this chemokine in lung defense. However, in some bacterial diseases such as tuberculosis (TB), CXCL17 gene expression was upregulated among ILC3 cells isolated from lung tissues of patients with active disease, suggesting that this chemokine may participate in the early recruitment of myeloid cells to the lung parenchyma during mycobacterial infection [57]. Together, these observations further stress the dual role played by this chemokine in infectious diseases.
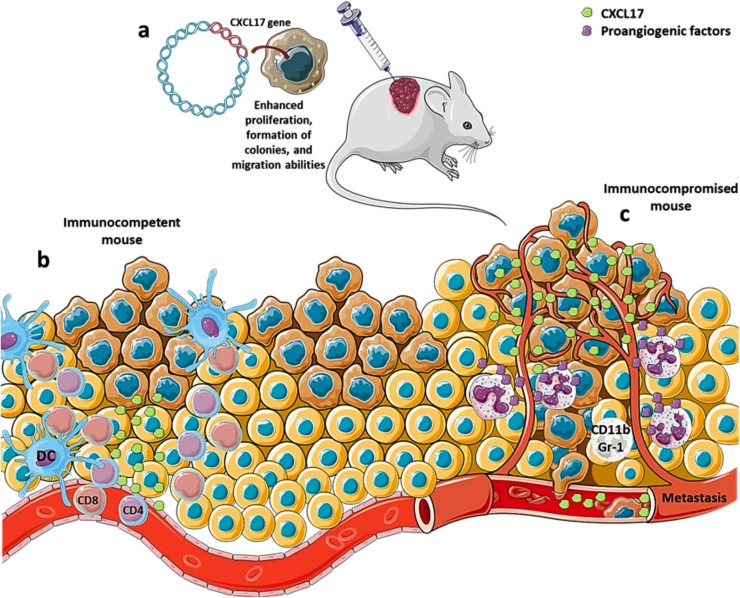
7.3. CXCL17 in cancer
Emerging evidence support a dual role for CXCL17 in cancer (see Fig. 2 ). Several research groups have demonstrated an increased expression of CXCL17 in human tissue samples and cell lines from breast, colon, gastric, pancreatic, bladder, renal, uterine cervical, human hepatocellular carcinoma (HHC) and non-small cell lung cancer (NSCLC) [20,22,29,[58], [59], [60], [61], [62], [63], [64]]. This enhanced expression of CXCL17 is also associated to its abundance in the surrounding peri-tumoral tissue [59,60,64], which has been linked to poor survival and recurrence in patients with HCC and breast cancer [[59], [60], [61],64].
Fig. 2.
CXCL17 in cancer.
(a) Current experimental approaches to uncover the role of CXCL17 in cancer are based on the usage of cancer cell lines transfected with the CXCL17 gene by plasmids or viral vectors. These cells acquire better capacity to form tumors when injected into mice. (b) In immunocompetent animals, tumors made of CXCL17-transfected cells elicit an immune response in which DCs, CD8 and CD4 T cells are recruited into the tumor and inhibit cancer progression. (c) Meanwhile, in immunocompromised mice, CXCL17 promotes the formation of tumors with increased vascularization, and recruits CD11b + Gr-1+ cells which further support angiogenesis. Some tumors made of CXCL17-expressing cells also possess an increased ability to metastasize. Thus, CXCL17 may play a dual role in cancer. DC, dendritic cell; CD4, T helper cell, CD8, cytotoxic T lymphocyte. The art pieces used in this figure were modified from Servier Medical Art by Servier, licensed under a Creative Commons Attribution 3.0 Unported License (https://smart.servier.com/).
The functional mechanism underlying this tumorigenic potential could be due to increased cellular proliferation, as the overexpression of CXCL17 in normal embryonic mouse fibroblast cell line NIH3T3 leads to generation of tumors into immunodeficient mice [20,22]. Also, HHC cell lines such as HepG2 and SMMC7721 cells, as well as breast cancer cell lines transfected with plasmids carrying CXCL17 increase their ability of proliferation in vitro and form larger tumors in vivo [59,61,64,65].
CXCL17 may also protect cancer cells from apoptosis. For instance, HHC cell lines transfected with CXCL17 have a mild degree of resistance to cisplatin-induced apoptosis [59]. In addition, CXCL17 inhibits autophagy by limiting activation of AMP-activated protein kinase (AMPK) pathway [64]. As recent studies have shown that CXCL17 expression in tumor samples does not correlate with presence of markers of cell proliferation such as Ki67, the importance of the apoptotic pathway as a potential driving force for the tumorigenic effects of CXCL17 gains importance [60].
Another feature associated with the tumorigenic potential of CXCL17 maybe its ability to promote metastasis, as described in HHC cell lines and breast cancer cells transfected with CXCL17 [59,61]. As proposed for other chemokines [[66], [67], [68], [69]], the mechanism by which CXCL17 mediates metastasis may be related to the aberrant over expression of both the chemokine and its receptor that leads malignant cells to migrate in the direction of the chemotactic gradient. This hypothesis is partially supported by observations about increased expression of CXCL17 and GPR35 in breast cancer clinical samples [61]. Also, CXCL17 mRNA expression is higher in lymph nodes invaded by metastatic colon cancer and this correlates with poor survival and risk of recurrence after treatment [63].
Another critical tumorigenic feature of CXCL17 is due to its role in angiogenesis. Formation of new blood vessels within tumors is a pivotal event that supports nutrient supply, cancer progression and better access to blood vessels enabling cancer cells to metastasize [70]. CXCL17 is co-regulated with VEGF in clinical samples from individuals with cancer [20]. Secondly, fibroblast cell lines and colon cancer cell lines (DLD-1, SW620) expressing CXCL17 form tumors with increased vasculature and abundant blood supply when injected into immunodeficient mice [22]. Some of these tumors were characterized by the infiltration of CD11b+Gr-1+ cells that migrate in response to CXCL17 gradients and participate in the promotion of tumor formation and vascularization [22]. Therefore, these data suggest that CXCL17 may promote tumor vascularization both directly acting on local vascular niches or indirectly via recruitment of cell populations that support angiogenesis.
Finally, CXCL17 may also modify the immune microenvironment of tumors. For instance, in tissue samples from humans with HCC and colon cancer, a high expression of CXCL17 was associated with the presence of CD68+ cells, the proportion of which correlates with survival [60,62]. Also, CXCL17 is a known recruiter of MDSC and Treg cells [45], and it is already established that MDSC can synergize with Treg cells to prevent tumor immunity and promote tumor progression [71]. In contrast there is currently insufficient evidence to support a role for CXCL17-mediated anti-tumoral immune responses. Interestingly, CXCL17 mediate the infiltration of immature myeloid DCs into pancreatic intraductal papillary mucinous carcinomas and promotes rendering of the tumor susceptible to cytotoxic T cell mediated cytolysis [29]. Also, expression of CXCL17 is lost progressively as pancreatic tumors become more malignant [29], supporting a protective effect during early stages of pancreatic cancer development. However, whether such an anti-tumor role for CXCL17 would extend to other cancer subtypes would be a necessary avenue for future research.
8. Implications of CXCL17 in respiratory medicine
8.1. CXCL17 in IPF
Increased concentrations of CXCL17 have been reported in bronchoalveolar lavage (BAL) samples from patients with interstitial pulmonary fibrosis (IPF) suggesting that this chemokine may actively participate in the pathogenesis of this disease, although the exact mechanism remains unclear. It is likely that the recruitment of inflammatory immune cells and the resultant profibrotic cytokine secretion and vascular remodeling leading to lung fibrosis could be involved [[72], [73], [74], [75], [76], [77], [78]]. Although the specific role of such vascular remodeling in IPF pathophysiology is yet controversial, certain angiogenic CXC chemokines, such as CXCL5 and CXCL8 are increased in IPF patients [[78], [79], [80]]. In fact, certain angiogenic CXC chemokines, such as CXCL5 and CXCL8 are increased in IPF patients [79,80], and together with CXCL17 may be promoting excessive vascularization associated with deposition of fibrotic tissue. However, this hypothesis should be experimentally tested in mouse models and human samples from IPF patients.
Finally, some chemokines with a known role in IPF, such as CXCL12, promote the recruitment of fibroblasts to the lung leading to increased production of extracellular matrix [[81], [82], [83]]. Although, there is currently no evidence for the chemotactic activity of CXCL17 on fibroblasts or their precursors, it is possible that CXCL17 could support the local proliferation of lung fibroblasts. However, this line of reasoning is also questionable as although transfection of the CXCL17 gene into embryonic mouse fibroblast cell lines promotes formation of tumors, it is not mediated by an improvement of the proliferative capacity of the fibroblasts [22]. Nevertheless, investigation of the potential induction of cell proliferation mediated by CXCL17 needs to be performed using human primary lung fibroblasts or human lung fibroblasts cell lines to definitively rule out this mechanism. If subsequent studies confirm a role for CXCL17 in pathogenesis of IPF, then this chemokine would constitute a novel target to focus the development of novel therapeutic approaches against this devastating disease.
8.2. CXCL17 in asthma
Recently, the participation of CXCL17 in the regulation of eosinophilic inflammation responsible of type 2 asthma has been established by assessing the expression of CXCL17 in bronchial brushing samples from asthmatic patients, who showed higher transcripts of this chemokine compared to healthy controls [46]. Such increased expression was restricted to the bronchial epithelium. Furthermore, the mechanism was evaluated in vitro in a bronchial cell line, wherein overexpression of CXCL17 gene inhibited the production of CCL24, CCL26 and epithelial periostin (POSTN; all molecules involved in recruitment of eosinophils) in response to exogenous stimulation with IL-13. Also, an inverse correlation between CXCL17 transcript levels and miR-221 was observed while overregulation of miR-221 increased production of CCL24, CCL26, POSTN, as well as lung eosinophilic inflammation by suppressing CXCL17 expression [46]. This suggests an anti-inflammatory role of CXCL17 in asthma, as CCL26 and CCL24 are key players in eosinophilic recruitment, proliferation and airway remodeling in asthma [84,85], while miR-221 participates in airway epithelial cell injury via sirtuin-1 (SIRT1) [86]. Thus, the enhanced production of CXCL17 at respiratory epithelium in asthmatic individuals might reflect a compensatory effort to counteract inflammation of the airways which makes this chemokine a potential target for immunotherapeutic development. Nonetheless, it is also possible that CXCL17 mediates contrasting roles during different stages of asthma, but this notion should be evaluated in future investigations. Additionally, this feature of increased CXCL17 in asthmatic individuals makes it a potential diagnostic biomarker, but targeted studies validating this are yet to be conducted. Finally, findings described here should prompt clinical researchers to look for a potential role of CXCL17 in other allergic respiratory diseases such as rhinitis, as well as in pulmonary disorders caused by altered infiltration of eosinophils, as is the case of eosinophilic interstitial lung disease.
8.3. CXCL17 in respiratory viral infections
CXCL17 is a key chemotactic factor for lung macrophages [36], which are the sentinel cells partaking in defense against infectious assault in the normal lung and during conditions associated with chronic inflammation. As such, the possibility for a potential role for this chemokine in respiratory infections is warranted. Indeed, CXCL17 along with other chemokines such as CXCL1, 8, 10, 11 and 16 has been found to be highly expressed in human bronchial epithelial, human tracheobronchial epithelial and A549 cells infected with influenza A/H3N2 virus but reduced in these cells infected with A/H5N1 and A/H7N9 strains [87]. Avian influenza A/H5N1 and A/H7N9 strains are more virulent due to acquired genetic properties contributing to a faster replication rate and rate of infection compared to seasonal influenza A/H1N1 and A/H3N2 strains [88,89]. Coincidentally, in an as yet unpublished study conducted in Mexico City during the 2018–2019 Flu season, it was found that the levels of CXCL17 were significantly increased in the sera of patients suffering from severe pneumonia caused by the pandemic influenza A/H1N1 virus (Dr. Joaquin Zuniga, unpublished data). Interestingly, patients with higher levels of CXCL17 exhibited a trend for decreased disease severity and better survival indicating an enhanced host response to thwart progressing infection. However, further studies deconvoluting the role of CXCL17 and influenza would be needed to fully ascertain this link (Dr. Joaquin Zuniga, unpublished data).
While there is a paucity of published studies assessing the expression of CXCL17 in response to the severe acute respiratory syndrome coronavirus (SARS-COV), the Influenza Research Database provides a wealth of curated data from ongoing research on the immune responses induced in response to this deadly virus. One such study assessed the significantly altered genes induced in vitro in Calu-3 (2B-4) human lung epithelial cells infected with the virulent wild-type icSARS-COV or the attenuated mutant strains, icSARSExoNI [mutation in exoribonuclease (ExoN) harbored in nonstructural protein 14 (nsp14) governing the activity of guanine-N7-methyltransferase involved in infection and pathogenesis)] and icSARS dNSP16 (mutations in a 12 conserved 2′O methyltransferase which impacts immune responses and pathogenesis) [90,91]. The data from this study indicates that CXCL17 expression is significantly upregulated in cells infected with the attenuated mutant strain, icSARS dNSP16 in comparison with the virulent WT SARS-COV strain [92] indicating that virulent strains with intact 2′O methyltransferase maybe avoiding induction of strong innate immune responses in host cells.
Collectively, it is of interest to note that in all the studies listed above the ability to induce CXCL17 expression is inversely related to virulence of these viral strains. This indicates a potential protective influence of CXCL17 in response to influenza and SARS-CoV infections. Although there are currently no studies assessing the potential impact of this chemokine in the context of the novel SARS-CoV-2, the causative agent of the ongoing COVID-19 pandemic, it is anticipated that future research would be directed towards deciphering this, thus paving the way towards identification of potential therapeutic targets against these viruses.
8.4. CXCL17- in lung cancer
Lung cancer leads the list of killer neoplasia worldwide [93]. Currently, there is an urgent necessity to identify novel molecules implicated in cancer biology that can fulfill the role as biomarkers and therapeutic targets to stop the burden caused by different histological subtypes of lung cancer. In this regard, the fact that expression of CXCL17 has been observed in human tissue samples from patients with NSCLC arouses the interest of exploring the possible participation of this chemokine in molecular pathogenesis of lung cancer [22]. For this, studies comparing the concentration of CXCL17 between biological samples (BAL, bronchial brushing, sputum, biopsy specimens, plasma) from humans with lung cancer and healthy controls would be needed. Next, investigations looking for correlation between levels of this chemokine and clinical parameters such as risk of mortality, recurrence after treatment and incidence of metastasis, will reveal the pro- or anti-tumorigenic features of CXCL17 activity in the context of lung cancer. Furthermore, animal models using knockout mice, as well as genetic manipulation of CXCL17 expression in lung cancer cell lines will reveal the underlying mechanisms including promotion of cellular proliferation, escape from apoptosis, metastasis, regulation of anti-tumoral immune responses, and support of angiogenesis. This latter mechanism may deserve particular consideration since angiogenic pathways play a remarkable role in the promotion of tumor growth in NSCLC [94]. Currently, treatment with anti-angiogenic factors such as bevacizumab, an inhibitor of VEGF, is the main strategy for the management of advanced NSCLC [95]. However, resistance to bevacizumab may appear in some patients due to the activation of other angiogenic pathways different from VEGF signaling. These compensatory mechanisms include FGF signaling [96], a pro-angiogenic factor that is regulated by CXCL17 [20]. Therefore, targeting CXCL17 could be a good strategy to improve efficacy of anti-VEGF agents in lung cancer.
8.5. CXCL17 as an antimicrobial drug for respiratory bacterial infections
Bacterial pneumonia is one of the main causes of morbidity around the world. Rise in the prevalence of drug resistant bacteria contributes to morbidity and mortality of this infectious lung diseases [97]. Anti-microbial peptides (AMPs) have gained attention as potential therapeutic agents [98], since most of them possess a broad spectrum activity and less risk of resistance development. Administration of mixtures of AMPs and exogenous surfactants is an innovative strategy under investigation to deliver molecules with antimicrobial activity directly into the respiratory tract [99,100]. CXCL17 has a potent bactericidal activity over bacterial strains causative of respiratory infections that tend to develop resistance to antibiotics, such as Staphylococcus aureus and Pseudomonas aeruginosa [24]. Therefore, CXCL17 may represent a novel candidate for this therapeutic approach. Nonetheless, further demonstration of the bactericidal activity of this chemokine in vivo is necessary. Moreover, complete characterization of the structural basis of its antimicrobial properties is required to isolate the peptide sequence responsible of such activity and limit collateral damages resulting from excessive CXCL17 signaling.
9. Conclusions
As the role of CXCL17 in several diseases is continued to be explored, its potential as a target for immunotherapy is envisaged. Although considerable progress has been made in understanding the biology of CXCL17, there are still several knowledge gaps that could be pursued by researchers to gain more knowledge on the role of CXCL17 in health disorders. One area of priority is to identify the GPCR mediating CXCL17 signaling, which will aid in dissipating current controversies regarding the potential implications of CXCL17/CXCL17-receptor axes in the pathogenesis of several human diseases. As a key participant in maintaining the homeostasis at respiratory epithelium, targeting CXCL17 represents an interesting approach for the development of novel therapeutics and diagnostics for respiratory diseases. The literature curated and hypotheses generated in this review provide a theoretical framework helpful for future investigations aimed to explore the multitude of potential clinical applications of CXCL17.
Author contributions
JCP and ST participated in the intellectual conception of the study and drafted the manuscript. JZ and SAK designed the study, contributed to the writing process of the manuscript and revised it for intellectual content. All the authors read and approved the final version of the manuscript.
Funding
JCP was supported by the National Council of Science and Technology of Mexico (CONACyT, CVU 737347) to achieve his Ph.D. degree. This work was supported by Washington University in St. Louis, NIH grant HL105427 to S.A.K., AI123780, AI111914 and RO1 AI134236 to S.A.K.
Declaration of Competing Interest
The current study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Dr. Nicole Howard and Dr. Shibali Das, Department of Molecular Microbiology, Washington University School of Medicine in St Louis, for their scientific critique of the manuscript.
Biographies

José Alberto Choreño-Parra obtained his MD degree at the National Autonomous University of Mexico (UNAM) in 2015. Then he moved to the National Institute of Respiratory Diseases of Mexico (INER) in Mexico City where he was working on characterizing immunophenotype of NK cells from tuberculosis patients and exploring memory NK cell responses in mice. He received his MS degree in 2017 at the National School of Biological Sciences, National Polytechnic Institute of Mexico (ENCB, IPN). Then, he spent a year in Dr.Khader’s lab at the Department of Molecular Microbiology at the Washington University in St. Louis, MO, where he focused his research on the role of specific chemokines (including CXCL17) to the immune responses against tuberculosis. José Alberto Choreño-Parra has moved to the INER in Mexico City, where he is conducting clinical studies in patients with tuberculosis and influenza to obtain his PhD degree.

Shyamala Thirunavukkarasu received her PhD from the University of Sydney focusing on the role of pathogen and host associated lipids in the macrophage immune responses to Mycobacterium avium subsp. paratuberculosis-infection. She completed her postdoctoral training at the University of Tennessee Health Science Center working on the gender specific role of cytochrome P450 1B1 mediated effects on steroid metabolism alterations in cardiovascular and renal diseases. She then completed a senior postdoctoral research fellowship at the Idaho Veterans Research and Education Foundation on the cell cycle/cell death programming in myoblasts in response to non-steroidal anti-inflammatory drug administration during group A streptococcal infections. Her research interests involve identifying the mechanisms that contribute to host immune response to infections and metabolic diseases & disorders. She is currently a Staff Scientist at Dr. Shabaana Khader’s lab at the Department of Molecular Microbiology at the Washington University in St. Louis, MO, where her research involves the identification of common inter-species immune correlates of inflammation and risk of TB and utilizing animal models to determine the function of genes identified as correlates of risk of disease in humans.

Joaquín Zúñiga received his PhD from the National Autonomous University of Mexico, and then moved to Dr. Edmond Yunis’ lab at Harvard Medical School in Boston, MA, where he carried out his Post-doctoral training. Dr. Zúñiga then joined the National Institute of Respiratory Diseases (INER) in Mexico City, where he has conducted clinical research studies in patients with pulmonary tuberculosis and influenza virus infection. Dr. Zúñiga participated in the initial description of the first cases of severe pneumonia caused by the pandemic influenza A/H1N1 virus, which emerged in Mexico in 2009. Since then, Dr. Zúñiga’s research has focused on the study of protective immunity against this virus, as well as on the epigenetic control of immune responses occurring at the lung. Since 2017, Dr. Zúñiga is the head of the Research Department of the INER.

Shabaana Khader received her PhD in Biotechnology from Madurai Kamaraj University, India where she studied host-pathogen interactions during the mycobacterial disease, leprosy. Dr. Khader then carried out her Post-doctoral training at the Trudeau Institute, NY, where she continued studying host immune responses to another globally relevant mycobacterial disease, tuberculosis. During her stay at the Trudeau Institute, Dr. Khader demonstrated a critical role for the cytokine Interleukin-17 in vaccine-induced immunity to tuberculosis, as well as described seminal roles for IL-12 cytokines in tuberculosis. Dr. Khader then joined the University of Pittsburgh in 2007 as Assistant Professor in the Department of Pediatrics where her lab continued to study the role of cytokines in immunity to intracellular pathogens such as Mycobacterium tuberculosis and Francisella tularensis. In 2013, Dr. Khader and her research team moved to the Department of Molecular Microbiology at the Washington University in St. Louis, where she is now a tenured Professor, in the Department of Molecular Microbiology. Her lab is focused on the immunopathogenesis of tuberculosis including aspects of both innate and adaptive immunity as well as vaccine-induced immunity to tuberculosis.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.cytogfr.2020.04.004.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.O’Dwyer D.N., Dickson R.P., Moore B.B. The lung microbiome, immunity, and the pathogenesis of chronic lung disease. J. Immunol. 2016;196(12):4839–4847. doi: 10.4049/jimmunol.1600279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tomankova T., Kriegova E., Liu M. Chemokine receptors and their therapeutic opportunities in diseased lung: far beyond leukocyte trafficking. Am. J. Physiol. Lung Cell Mol. Physiol. 2015;308(7):L603–18. doi: 10.1152/ajplung.00203.2014. [DOI] [PubMed] [Google Scholar]
- 3.Zlotnik A., Yoshie O. The chemokine superfamily revisited. Immunity. 2012;36(5):705–716. doi: 10.1016/j.immuni.2012.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vassilatis D.K., Hohmann J.G., Zeng H., Li F., Ranchalis J.E., Mortrud M.T., Brown A., Rodriguez S.S., Weller J.R., Wright A.C., Bergmann J.E., Gaitanaris G.A. The G protein-coupled receptor repertoires of human and mouse. Proc. Natl. Acad. Sci. U. S. A. 2003;100(8):4903–4908. doi: 10.1073/pnas.0230374100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lodowski D.T., Palczewski K. Chemokine receptors and other G protein-coupled receptors. Curr. Opin. HIV AIDS. 2009;4(2):88–95. doi: 10.1097/COH.0b013e3283223d8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Murphy P.M. Chemokines and the molecular basis of cancer metastasis. N. Engl. J. Med. 2001;345(11):833–835. doi: 10.1056/NEJM200109133451113. [DOI] [PubMed] [Google Scholar]
- 7.Thiele S., Rosenkilde M.M. Interaction of chemokines with their receptors--from initial chemokine binding to receptor activating steps. Curr. Med. Chem. 2014;21(31):3594–3614. doi: 10.2174/0929867321666140716093155. [DOI] [PubMed] [Google Scholar]
- 8.Legler D.F., Thelen M. New insights in chemokine signaling. F1000Res. 2018;7:95. doi: 10.12688/f1000research.13130.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zlotnik A., Yoshie O. Chemokines: a new classification system and their role in immunity. Immunity. 2000;12(2):121–127. doi: 10.1016/s1074-7613(00)80165-x. [DOI] [PubMed] [Google Scholar]
- 10.Kiefer F., Siekmann A.F. The role of chemokines and their receptors in angiogenesis. Cell. Mol. Life Sci. 2011;68(17):2811–2830. doi: 10.1007/s00018-011-0677-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moser B., Wolf M., Walz A., Loetscher P. Chemokines: multiple levels of leukocyte migration control. Trends Immunol. 2004;25(2):75–84. doi: 10.1016/j.it.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Beider K., Abraham M., Peled A. Chemokines and chemokine receptors in stem cell circulation. Front. Biosci. 2008;13:6820–6833. doi: 10.2741/3190. [DOI] [PubMed] [Google Scholar]
- 13.Raman D., Sobolik-Delmaire T., Richmond A. Chemokines in health and disease. Exp. Cell Res. 2011;317(5):575–589. doi: 10.1016/j.yexcr.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Donnelly L.E., Barnes P.J. Chemokine receptors as therapeutic targets in chronic obstructive pulmonary disease. Trends Pharmacol. Sci. 2006;27(10):546–553. doi: 10.1016/j.tips.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 15.Palmqvist C., Wardlaw A.J., Bradding P. Chemokines and their receptors as potential targets for the treatment of asthma. Br. J. Pharmacol. 2007;151(6):725–736. doi: 10.1038/sj.bjp.0707263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keane M.P. Vol. 17. 2008. pp. 151–156. (The Role of Chemokines and Cytokines in Lung Fibrosis). 109. [Google Scholar]
- 17.Rivas-Fuentes S., Salgado-Aguayo A., Pertuz Belloso S., Gorocica Rosete P., Alvarado-Vasquez N., Aquino-Jarquin G. Role of chemokines in non-small cell lung cancer: angiogenesis and inflammation. J. Cancer. 2015;6(10):938–952. doi: 10.7150/jca.12286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clark H.F., Gurney A.L., Abaya E., Baker K., Baldwin D., Brush J., Chen J., Chow B., Chui C., Crowley C., Currell B., Deuel B., Dowd P., Eaton D., Foster J., Grimaldi C., Gu Q., Hass P.E., Heldens S., Huang A., Kim H.S., Klimowski L., Jin Y., Johnson S., Lee J., Lewis L., Liao D., Mark M., Robbie E., Sanchez C., Schoenfeld J., Seshagiri S., Simmons L., Singh J., Smith V., Stinson J., Vagts A., Vandlen R., Watanabe C., Wieand D., Woods K., Xie M.H., Yansura D., Yi S., Yu G., Yuan J., Zhang M., Zhang Z., Goddard A., Wood W.I., Godowski P., Gray A. The secreted protein discovery initiative (SPDI), a large-scale effort to identify novel human secreted and transmembrane proteins: a bioinformatics assessment. Genome Res. 2003;13(10):2265–2270. doi: 10.1101/gr.1293003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pisabarro M.T., Leung B., Kwong M., Corpuz R., Frantz G.D., Chiang N., Vandlen R., Diehl L.J., Skelton N., Kim H.S., Eaton D., Schmidt K.N. Cutting edge: novel human dendritic cell- and monocyte-attracting chemokine-like protein identified by fold recognition methods. J. Immunol. 2006;176(4):2069–2073. doi: 10.4049/jimmunol.176.4.2069. [DOI] [PubMed] [Google Scholar]
- 20.Weinstein E.J., Head R., Griggs D.W., Sun D., Evans R.J., Swearingen M.L., Westlin M.M., Mazzarella R. VCC-1, a novel chemokine, promotes tumor growth. Biochem. Biophys. Res. Commun. 2006;350(1):74–81. doi: 10.1016/j.bbrc.2006.08.194. [DOI] [PubMed] [Google Scholar]
- 21.Eigenbrot C., Lowman H.B., Chee L., Artis D.R. Structural change and receptor binding in a chemokine mutant with a rearranged disulfide: X-ray structure of E38C/C50AIL-8 at 2 A resolution. Proteins. 1997;27(4):556–566. [PubMed] [Google Scholar]
- 22.Matsui A., Yokoo H., Negishi Y., Endo-Takahashi Y., Chun N.A., Kadouchi I., Suzuki R., Maruyama K., Aramaki Y., Semba K., Kobayashi E., Takahashi M., Murakami T. CXCL17 expression by tumor cells recruits CD11b+Gr1 high F4/80- cells and promotes tumor progression. PLoS One. 2012;7(8):e44080. doi: 10.1371/journal.pone.0044080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee W.Y., Wang C.J., Lin T.Y., Hsiao C.L., Luo C.W. CXCL17, an orphan chemokine, acts as a novel angiogenic and anti-inflammatory factor. Am. J. Physiol. Endocrinol. Metab. 2013;304(1):E32–40. doi: 10.1152/ajpendo.00083.2012. [DOI] [PubMed] [Google Scholar]
- 24.Burkhardt A.M., Tai K.P., Flores-Guiterrez J.P., Vilches-Cisneros N., Kamdar K., Barbosa-Quintana O., Valle-Rios R., Hevezi P.A., Zuniga J., Selman M., Ouellette A.J., Zlotnik A. CXCL17 is a mucosal chemokine elevated in idiopathic pulmonary fibrosis that exhibits broad antimicrobial activity. J. Immunol. 2012;188(12):6399–6406. doi: 10.4049/jimmunol.1102903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maravillas-Montero J.L., Burkhardt A.M., Hevezi P.A., Carnevale C.D., Smit M.J., Zlotnik A. Cutting edge: GPR35/CXCR8 is the receptor of the mucosal chemokine CXCL17. J. Immunol. 2015;194(1):29–33. doi: 10.4049/jimmunol.1401704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Binti Mohd Amir N.A.S., Mackenzie A.E., Jenkins L., Boustani K., Hillier M.C., Tsuchiya T., Milligan G., Pease J.E. Evidence for the existence of a CXCL17 receptor distinct from GPR35. J. Immunol. 2018;201(2):714–724. doi: 10.4049/jimmunol.1700884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park S.J., Lee S.J., Nam S.Y., Im D.S. GPR35 mediates lodoxamide-induced migration inhibitory response but not CXCL17-induced migration stimulatory response in THP-1 cells; is GPR35 a receptor for CXCL17? Br. J. Pharmacol. 2018;175(1):154–161. doi: 10.1111/bph.14082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCarthy C.G., Wenceslau C.F. Adopting an orphan: how could GRP35 contribute to angiotensin II-dependent hypertension? Am. J. Hypertens. 2018;31(9):973–975. doi: 10.1093/ajh/hpy090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hiraoka N., Yamazaki-Itoh R., Ino Y., Mizuguchi Y., Yamada T., Hirohashi S., Kanai Y. CXCL17 and ICAM2 are associated with a potential anti-tumor immune response in early intraepithelial stages of human pancreatic carcinogenesis. Gastroenterology. 2011;140(1):310–321. doi: 10.1053/j.gastro.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 30.Mangmool S., Kurose H. G(i/o) protein-dependent and -independent actions of Pertussis Toxin (PTX) Toxins (Basel) 2011;3(7):884–899. doi: 10.3390/toxins3070884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vicari A.P., Figueroa D.J., Hedrick J.A., Foster J.S., Singh K.P., Menon S., Copeland N.G., Gilbert D.J., Jenkins N.A., Bacon K.B., Zlotnik A. TECK: a novel CC chemokine specifically expressed by thymic dendritic cells and potentially involved in T cell development. Immunity. 1997;7(2):291–301. doi: 10.1016/s1074-7613(00)80531-2. [DOI] [PubMed] [Google Scholar]
- 32.Hromas R., Broxmeyer H.E., Kim C., Nakshatri H., Christopherson K., 2nd, Azam M., Hou Y.H. Cloning of BRAK, a novel divergent CXC chemokine preferentially expressed in normal versus malignant cells. Biochem. Biophys. Res. Commun. 1999;255(3):703–706. doi: 10.1006/bbrc.1999.0257. [DOI] [PubMed] [Google Scholar]
- 33.Maerki C., Meuter S., Liebi M., Muhlemann K., Frederick M.J., Yawalkar N., Moser B., Wolf M. Potent and broad-spectrum antimicrobial activity of CXCL14 suggests an immediate role in skin infections. J. Immunol. 2009;182(1):507–514. doi: 10.4049/jimmunol.182.1.507. [DOI] [PubMed] [Google Scholar]
- 34.Fil D., Borysiewicz E., Konat G.W. A broad upregulation of cerebral chemokine genes by peripherally-generated inflammatory mediators. Metab. Brain Dis. 2011;26(1):49–59. doi: 10.1007/s11011-010-9231-9. [DOI] [PubMed] [Google Scholar]
- 35.Hernandez-Ruiz M., Othy S., Herrera C., Nguyen H.T., Arrevillaga-Boni G., Catalan-Dibene J., Cahalan M.D., Zlotnik A. Cxcl17(-/-) mice develop exacerbated disease in a T cell-dependent autoimmune model. J. Leukoc. Biol. 2019;105(5):1027–1039. doi: 10.1002/JLB.3A0918-345RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burkhardt A.M., Maravillas-Montero J.L., Carnevale C.D., Vilches-Cisneros N., Flores J.P., Hevezi P.A., Zlotnik A. CXCL17 is a major chemotactic factor for lung macrophages. J. Immunol. 2014;193(3):1468–1474. doi: 10.4049/jimmunol.1400551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Strieter R.M., Polverini P.J., Kunkel S.L., Arenberg D.A., Burdick M.D., Kasper J., Dzuiba J., Van Damme J., Walz A., Marriott D. The functional role of the ELR motif in CXC chemokine-mediated angiogenesis. J. Biol. Chem. 1995;270(45):27348–27357. doi: 10.1074/jbc.270.45.27348. [DOI] [PubMed] [Google Scholar]
- 38.Niiya K., Ohara H., Isono M., Sheikh A.M., Matsuo H., Fujikawa K., Isomura M., Kato N., Nabika T. Further dissection of QTLs for salt-induced stroke and identification of candidate genes in the stroke-prone spontaneously hypertensive rat. Sci. Rep. 2018;8(1):9403. doi: 10.1038/s41598-018-27539-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hieshima K., Ohtani H., Shibano M., Izawa D., Nakayama T., Kawasaki Y., Shiba F., Shiota M., Katou F., Saito T., Yoshie O. CCL28 has dual roles in mucosal immunity as a chemokine with broad-spectrum antimicrobial activity. J. Immunol. 2003;170(3):1452–1461. doi: 10.4049/jimmunol.170.3.1452. [DOI] [PubMed] [Google Scholar]
- 40.Dai C., Basilico P., Cremona T.P., Collins P., Moser B., Benarafa C., Wolf M. CXCL14 displays antimicrobial activity against respiratory tract bacteria and contributes to clearance of Streptococcus pneumoniae pulmonary infection. J. Immunol. 2015;194(12):5980–5989. doi: 10.4049/jimmunol.1402634. [DOI] [PubMed] [Google Scholar]
- 41.Ahrne S., Nobaek S., Jeppsson B., Adlerberth I., Wold A.E., Molin G. The normal Lactobacillus flora of healthy human rectal and oral mucosa. J. Appl. Microbiol. 1998;85(1):88–94. doi: 10.1046/j.1365-2672.1998.00480.x. [DOI] [PubMed] [Google Scholar]
- 42.Llopis M., Antolin M., Carol M., Borruel N., Casellas F., Martinez C., Espin-Basany E., Guarner F., Malagelada J.R. Lactobacillus casei downregulates commensals’ inflammatory signals in Crohn’s disease mucosa. Inflamm. Bowel Dis. 2009;15(2):275–283. doi: 10.1002/ibd.20736. [DOI] [PubMed] [Google Scholar]
- 43.Dotiwala F., Mulik S., Polidoro R.B., Ansara J.A., Burleigh B.A., Walch M., Gazzinelli R.T., Lieberman J. Killer lymphocytes use granulysin, perforin and granzymes to kill intracellular parasites. Nat. Med. 2016;22(2):210–216. doi: 10.1038/nm.4023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Srivastava R., Hernandez-Ruiz M., Khan A.A., Fouladi M.A., Kim G.J., Ly V.T., Yamada T., Lam C., Sarain S.A.B., Boldbaatar U., Zlotnik A., Bahraoui E., BenMohamed L. CXCL17 chemokine-dependent mobilization of CXCR8(+)CD8(+) effector memory and tissue-resident memory T cells in the vaginal mucosa is associated with protection against genital herpes. J. Immunol. 2018;200(8):2915–2926. doi: 10.4049/jimmunol.1701474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oka T., Sugaya M., Takahashi N., Takahashi T., Shibata S., Miyagaki T., Asano Y., Sato S. CXCL17 attenuates imiquimod-induced psoriasis-like skin inflammation by recruiting myeloid-derived suppressor cells and regulatory T cells. J. Immunol. 2017;198(10):3897–3908. doi: 10.4049/jimmunol.1601607. [DOI] [PubMed] [Google Scholar]
- 46.Zhang K., Liang Y., Feng Y., Wu W., Zhang H., He J., Hu Q., Zhao J., Xu Y., Liu Z., Zhen G. Decreased epithelial and sputum miR-221-3p associates with airway eosinophilic inflammation and CXCL17 expression in asthma. Am. J. Physiol. Lung Cell Mol. Physiol. 2018;315(2):L253–l264. doi: 10.1152/ajplung.00567.2017. [DOI] [PubMed] [Google Scholar]
- 47.Hernandez-Ruiz M., Zlotnik A., Llorente L., Hernandez-Molina G. Markedly high salivary and lacrimal CXCL17 levels in primary Sjogren’s syndrome. Joint Bone Spine. 2018;85(3):379–380. doi: 10.1016/j.jbspin.2017.05.014. [DOI] [PubMed] [Google Scholar]
- 48.Sato N., Ahuja S.K., Quinones M., Kostecki V., Reddick R.L., Melby P.C., Kuziel W.A., Ahuja S.S. CC chemokine receptor (CCR)2 is required for langerhans cell migration and localization of T helper cell type 1 (Th1)-inducing dendritic cells. Absence of CCR2 shifts the Leishmania major-resistant phenotype to a susceptible state dominated by Th2 cytokines, b cell outgrowth, and sustained neutrophilic inflammation. J. Exp. Med. 2000;192(2):205–218. doi: 10.1084/jem.192.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Robben P.M., LaRegina M., Kuziel W.A., Sibley L.D. Recruitment of Gr-1+ monocytes is essential for control of acute toxoplasmosis. J. Exp. Med. 2005;201(11):1761–1769. doi: 10.1084/jem.20050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stein L.H., Redding K.M., Lee J.J., Nolan T.J., Schad G.A., Lok J.B., Abraham D. Eosinophils utilize multiple chemokine receptors for chemotaxis to the parasitic nematode Strongyloides stercoralis. J. Innate Immun. 2009;1(6):618–630. doi: 10.1159/000233235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Noor S., Habashy A.S., Nance J.P., Clark R.T., Nemati K., Carson M.J., Wilson E.H. CCR7-Dependent immunity during acute Toxoplasma gondii. Infection. 2010;78(5):2257–2263. doi: 10.1128/IAI.01314-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sullivan N.L., Eickhoff C.S., Zhang X., Giddings O.K., Lane T.E., Hoft D.F. Importance of the CCR5-CCL5 axis for mucosal Trypanosoma cruzi protection and B cell activation. J. Immunol. 2011;187(3):1358–1368. doi: 10.4049/jimmunol.1100033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dunlap M.D., Howard N., Das S., Scott N., Ahmed M., Prince O., Rangel-Moreno J., Rosa B.A., Martin J., Kaushal D., Kaplan G., Mitreva M., Kim K.W., Randolph G.J., Khader S.A. A novel role for C-C motif chemokine receptor 2 during infection with hypervirulent Mycobacterium tuberculosis. Mucosal Immunol. 2018;11(6):1727–1742. doi: 10.1038/s41385-018-0071-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lambert H., Hitziger N., Dellacasa I., Svensson M., Barragan A. Induction of dendritic cell migration upon Toxoplasma gondii infection potentiates parasite dissemination. Cell. Microbiol. 2006;8(10):1611–1623. doi: 10.1111/j.1462-5822.2006.00735.x. [DOI] [PubMed] [Google Scholar]
- 55.Campanella G.S., Tager A.M., El Khoury J.K., Thomas S.Y., Abrazinski T.A., Manice L.A., Colvin R.A., Luster A.D. Chemokine receptor CXCR3 and its ligands CXCL9 and CXCL10 are required for the development of murine cerebral malaria. Proc. Natl. Acad. Sci. U. S. A. 2008;105(12):4814–4819. doi: 10.1073/pnas.0801544105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Flach C.-F., Qadri F., Bhuiyan T.R., Alam N.H., Jennische E., Lönnroth I., Holmgren J. Broad up-regulation of innate defense factors during acute cholera. Infect. Immun. 2007;75(5):2343–2350. doi: 10.1128/IAI.01900-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ardain A., Domingo-Gonzalez R., Das S., Kazer S.W., Howard N.C., Singh A., Ahmed M., Nhamoyebonde S., Rangel-Moreno J., Ogongo P., Lu L., Ramsuran D., de la Luz Garcia-Hernandez M., K.U. T, Darby M., Park E., Karim F., Melocchi L., Madansein R., Dullabh K.J., Dunlap M., Marin-Agudelo N., Ebihara T., Ndung’u T., Kaushal D., Pym A.S., Kolls J.K., Steyn A., Zuniga J., Horsnell W., Yokoyama W.M., Shalek A.K., Kloverpris H.N., Colonna M., Leslie A., Khader S.A. Group 3 innate lymphoid cells mediate early protective immunity against tuberculosis. Nature. 2019;570(7762):528–532. doi: 10.1038/s41586-019-1276-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saghir F.S., Rose I.M., Dali A.Z., Shamsuddin Z., Jamal A.R., Mokhtar N.M. Gene expression profiling and cancer-related pathways in type I endometrial carcinoma. Int. J. Gynecol. Cancer. 2010;20(5):724–731. doi: 10.1111/igc.0b013e3181e1c14c. [DOI] [PubMed] [Google Scholar]
- 59.Zhou Z., Lu X., Zhu P., Zhu W., Mu X., Qu R., Li M. VCC-1 over-expression inhibits cisplatin-induced apoptosis in HepG2 cells. Biochem. Biophys. Res. Commun. 2012;420(2):336–342. doi: 10.1016/j.bbrc.2012.02.160. [DOI] [PubMed] [Google Scholar]
- 60.Li L., Yan J., Xu J., Liu C.Q., Zhen Z.J., Chen H.W., Ji Y., Wu Z.P., Hu J.Y., Zheng L., Lau W.Y. CXCL17 expression predicts poor prognosis and correlates with adverse immune infiltration in hepatocellular carcinoma. PLoS One. 2014;9(10):e110064. doi: 10.1371/journal.pone.0110064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Guo Y.J., Zhou Y.J., Yang X.L., Shao Z.M., Ou Z.L. The role and clinical significance of the CXCL17-CXCR8 (GPR35) axis in breast cancer. Biochem. Biophys. Res. Commun. 2017;493(3):1159–1167. doi: 10.1016/j.bbrc.2017.09.113. [DOI] [PubMed] [Google Scholar]
- 62.Ohlsson L., Hammarstrom M.L., Lindmark G., Hammarstrom S., Sitohy B. Ectopic expression of the chemokine CXCL17 in colon cancer cells. Br. J. Cancer. 2016;114(6):697–703. doi: 10.1038/bjc.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rashad Y., Olsson L., Israelsson A., Oberg A., Lindmark G., Hammarstrom M.L., Hammarstrom S., Sitohy B. Lymph node CXCL17 messenger RNA: a new prognostic biomarker for colon cancer. Tumour Biol. 2018;40(9) doi: 10.1177/1010428318799251. 1010428318799251. [DOI] [PubMed] [Google Scholar]
- 64.Wang L., Li H., Zhen Z., Ma X., Yu W., Zeng H., Li L. CXCL17 promotes cell metastasis and inhibits autophagy via the LKB1-AMPK pathway in hepatocellular carcinoma. Gene. 2019;690:129–136. doi: 10.1016/j.gene.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 65.Mu X., Chen Y., Wang S., Huang X., Pan H., Li M. Overexpression of VCC-1 gene in human hepatocellular carcinoma cells promotes cell proliferation and invasion. Acta Biochim. Biophys. Sin. (Shanghai) 2009;41(8):631–637. doi: 10.1093/abbs/gmp051. [DOI] [PubMed] [Google Scholar]
- 66.Wiley H.E., Gonzalez E.B., Maki W., Wu M.T., Hwang S.T. Expression of CC chemokine receptor-7 and regional lymph node metastasis of B16 murine melanoma. J. Natl. Cancer Inst. 2001;93(21):1638–1643. doi: 10.1093/jnci/93.21.1638. [DOI] [PubMed] [Google Scholar]
- 67.Mashino K., Sadanaga N., Yamaguchi H., Tanaka F., Ohta M., Shibuta K., Inoue H., Mori M. Expression of chemokine receptor CCR7 is associated with lymph node metastasis of gastric carcinoma. Cancer Res. 2002;62(10):2937–2941. [PubMed] [Google Scholar]
- 68.Gunther K., Leier J., Henning G., Dimmler A., Weissbach R., Hohenberger W., Forster R. Prediction of lymph node metastasis in colorectal carcinoma by expression of chemokine receptor CCR7. Int. J. Cancer. 2005;116(5):726–733. doi: 10.1002/ijc.21123. [DOI] [PubMed] [Google Scholar]
- 69.Cunningham H.D., Shannon L.A., Calloway P.A., Fassold B.C., Dunwiddie I., Vielhauer G., Zhang M., Vines C.M. Expression of the C-C chemokine receptor 7 mediates metastasis of breast cancer to the lymph nodes in mice. Transl. Oncol. 2010;3(6):354–361. doi: 10.1593/tlo.10178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bielenberg D.R., Zetter B.R. The contribution of angiogenesis to the process of metastasis. Cancer J. 2015;21(4):267–273. doi: 10.1097/PPO.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lindau D., Gielen P., Kroesen M., Wesseling P., Adema G.J. The immunosuppressive tumour network: myeloid-derived suppressor cells, regulatory T cells and natural killer T cells. Immunology. 2013;138(2):105–115. doi: 10.1111/imm.12036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moore B.B., Paine R., 3rd, Christensen P.J., Moore T.A., Sitterding S., Ngan R., Wilke C.A., Kuziel W.A., Toews G.B. Protection from pulmonary fibrosis in the absence of CCR2 signaling. J. Immunol. 2001;167(8):4368–4377. doi: 10.4049/jimmunol.167.8.4368. [DOI] [PubMed] [Google Scholar]
- 73.Gharaee-Kermani M., McCullumsmith R.E., Charo I.F., Kunkel S.L., Phan S.H. CC-chemokine receptor 2 required for bleomycin-induced pulmonary fibrosis. Cytokine. 2003;24(6):266–276. doi: 10.1016/j.cyto.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 74.Okuma T., Terasaki Y., Kaikita K., Kobayashi H., Kuziel W.A., Kawasuji M., Takeya M. C-C chemokine receptor 2 (CCR2) deficiency improves bleomycin-induced pulmonary fibrosis by attenuation of both macrophage infiltration and production of macrophage-derived matrix metalloproteinases. J. Pathol. 2004;204(5):594–604. doi: 10.1002/path.1667. [DOI] [PubMed] [Google Scholar]
- 75.Inoshima I., Kuwano K., Hamada N., Hagimoto N., Yoshimi M., Maeyama T., Takeshita A., Kitamoto S., Egashira K., Hara N. Anti-monocyte chemoattractant protein-1 gene therapy attenuates pulmonary fibrosis in mice. Am. J. Physiol. Lung Cell Mol. Physiol. 2004;286(5):L1038–44. doi: 10.1152/ajplung.00167.2003. [DOI] [PubMed] [Google Scholar]
- 76.Belperio J.A., Dy M., Murray L., Burdick M.D., Xue Y.Y., Strieter R.M., Keane M.P. The role of the Th2 CC chemokine ligand CCL17 in pulmonary fibrosis. J. Immunol. 2004;173(7):4692–4698. doi: 10.4049/jimmunol.173.7.4692. [DOI] [PubMed] [Google Scholar]
- 77.Uh S.T., Inoue Y., King T.E., Jr., Chan E.D., Newman L.S., Riches D.W. Morphometric analysis of insulin-like growth factor-I localization in lung tissues of patients with idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 1998;158(5 Pt 1):1626–1635. doi: 10.1164/ajrccm.158.5.9804025. [DOI] [PubMed] [Google Scholar]
- 78.Turner-Warwick M. Precapillary systemic-pulmonary anastomoses. Thorax. 1963;18:225–237. doi: 10.1136/thx.18.3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Keane M.P., Arenberg D.A., Lynch J.P., 3rd, Whyte R.I., Iannettoni M.D., Burdick M.D., Wilke C.A., Morris S.B., Glass M.C., DiGiovine B., Kunkel S.L., Strieter R.M. The CXC chemokines, IL-8 and IP-10, regulate angiogenic activity in idiopathic pulmonary fibrosis. J. Immunol. 1997;159(3):1437–1443. [PubMed] [Google Scholar]
- 80.Keane M.P., Belperio J.A., Burdick M.D., Lynch J.P., Fishbein M.C., Strieter R.M. ENA-78 is an important angiogenic factor in idiopathic pulmonary fibrosis. Am. J. Respir. Crit. Care Med. 2001;164(12):2239–2242. doi: 10.1164/ajrccm.164.12.2104106. [DOI] [PubMed] [Google Scholar]
- 81.Phillips R.J., Burdick M.D., Hong K., Lutz M.A., Murray L.A., Xue Y.Y., Belperio J.A., Keane M.P., Strieter R.M. Circulating fibrocytes traffic to the lungs in response to CXCL12 and mediate fibrosis. J. Clin. Invest. 2004;114(3):438–446. doi: 10.1172/JCI20997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Xu J., Mora A., Shim H., Stecenko A., Brigham K.L., Rojas M. Role of the SDF-1/CXCR4 axis in the pathogenesis of lung injury and fibrosis. Am. J. Respir. Cell Mol. Biol. 2007;37(3):291–299. doi: 10.1165/rcmb.2006-0187OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Makino H., Aono Y., Azuma M., Kishi M., Yokota Y., Kinoshita K., Takezaki A., Kishi J., Kawano H., Ogawa H., Uehara H., Izumi K., Sone S., Nishioka Y. Antifibrotic effects of CXCR4 antagonist in bleomycin-induced pulmonary fibrosis in mice. J. Med. Invest. 2013;60(1–2):127–137. doi: 10.2152/jmi.60.127. [DOI] [PubMed] [Google Scholar]
- 84.Kohan M., Puxeddu I., Reich R., Levi-Schaffer F., Berkman N. Eotaxin-2/CCL24 and eotaxin-3/CCL26 exert differential profibrogenic effects on human lung fibroblasts. Ann. Allergy Asthma Immunol. 2010;104(1):66–72. doi: 10.1016/j.anai.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 85.Larose M.-C., Chakir J., Archambault A.-S., Joubert P., Provost V., Laviolette M., Flamand N. Correlation between CCL26 production by human bronchial epithelial cells and airway eosinophils: involvement in patients with severe eosinophilic asthma. J. Allergy Clin. Immunol. 2015;136(4):904–913. doi: 10.1016/j.jaci.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 86.Zhang H., Sun Y., Rong W., Fan L., Cai Y., Qu Q., Gao Y., Zhao H. miR-221 participates in the airway epithelial cells injury in asthma via targeting SIRT1. Exp. Lung Res. 2018;44(6):272–279. doi: 10.1080/01902148.2018.1533051. [DOI] [PubMed] [Google Scholar]
- 87.Cao Y., Huang Y., Xu K., Liu Y., Li X., Xu Y., Zhong W., Hao P. Differential responses of innate immunity triggered by different subtypes of influenza a viruses in human and avian hosts. BMC Med. Genomics. 2017;10(Suppl. 4):70. doi: 10.1186/s12920-017-0304-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Eagles D., Siregar E.S., Dung D.H., Weaver J., Wong F., Daniels P. H5N1 highly pathogenic avian influenza in Southeast Asia. Rev. Sci. Technol. 2009;28(1):341–348. doi: 10.20506/rst.28.1.1864. [DOI] [PubMed] [Google Scholar]
- 89.Simon P.F., de La Vega M.A., Paradis É., Mendoza E., Coombs K.M., Kobasa D., Beauchemin C.A.A. Avian influenza viruses that cause highly virulent infections in humans exhibit distinct replicative properties in contrast to human H1N1 viruses. Sci. Rep. 2016;6:24154. doi: 10.1038/srep24154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chen Y.R., Zhong S., Fei Z., Hashimoto Y., Xiang J.Z., Zhang S., Blissard G.W. The transcriptome of the baculovirus Autographa californica multiple nucleopolyhedrovirus in Trichoplusia ni cells. J. Virol. 2013;87(11):6391–6405. doi: 10.1128/JVI.00194-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Menachery V.D., Yount B.L., Jr., Josset L., Gralinski L.E., Scobey T., Agnihothram S., Katze M.G., Baric R.S. Attenuation and restoration of severe acute respiratory syndrome coronavirus mutant lacking 2’-o-methyltransferase activity. J. Virol. 2014;88(8):4251–4264. doi: 10.1128/JVI.03571-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Influenza Research Database. Available from: https://www.fludb.org/brc/hostFactorExperimentDetails.spg?method=SubmitForm&fromDetail=true&biosetIds=1320&expSeqId=178&resultMatrixUserDefId=SCL008_R_N_RM&decorator=influenza. (Accessed 8 April 2020).
- 93.Bray F., Ferlay J., Soerjomataram I., Siegel R.L., Torre L.A., Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 94.Cox G., Jones J.L., Walker R.A., Steward W.P., O’Byrne K.J. Angiogenesis and non-small cell lung cancer. Lung Cancer. 2000;27(2):81–100. doi: 10.1016/s0169-5002(99)00096-3. [DOI] [PubMed] [Google Scholar]
- 95.Ellis P.M., Al-Saleh K. Multitargeted anti-angiogenic agents and NSCLC: clinical update and future directions. Crit. Rev. Oncol. Hematol. 2012;84(1):47–58. doi: 10.1016/j.critrevonc.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 96.Lieu C., Heymach J., Overman M., Tran H., Kopetz S. Beyond VEGF: inhibition of the fibroblast growth factor pathway and antiangiogenesis. Clin. Cancer Res. 2011;17(19):6130–6139. doi: 10.1158/1078-0432.CCR-11-0659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gross A.E., Van Schooneveld T.C., Olsen K.M., Rupp M.E., Bui T.H., Forsung E., Kalil A.C. Epidemiology and predictors of multidrug-resistant community-acquired and health care-associated pneumonia. Antimicrob. Agents Chemother. 2014;58(9):5262–5268. doi: 10.1128/AAC.02582-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kang H.K., Kim C., Seo C.H., Park Y. The therapeutic applications of antimicrobial peptides (AMPs): a patent review. J. Microbiol. 2017;55(1):1–12. doi: 10.1007/s12275-017-6452-1. [DOI] [PubMed] [Google Scholar]
- 99.Banaschewski B.J., Veldhuizen E.J., Keating E., Haagsman H.P., Zuo Y.Y., Yamashita C.M., Veldhuizen R.A. Antimicrobial and biophysical properties of surfactant supplemented with an antimicrobial peptide for treatment of bacterial pneumonia. Antimicrob. Agents Chemother. 2015;59(6):3075–3083. doi: 10.1128/AAC.04937-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Banaschewski B.J.H., Baer B., Arsenault C., Jazey T., Veldhuizen E.J.A., Delport J., Gooyers T., Lewis J.F., Haagsman H.P., Veldhuizen R.A.W., Yamashita C. The antibacterial and anti-inflammatory activity of chicken cathelicidin-2 combined with exogenous surfactant for the treatment of cystic fibrosis-associated pathogens. Sci. Rep. 2017;7(1):15545. doi: 10.1038/s41598-017-15558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.