In less than two months, an emerging threat entirely and radically changed the life of the population in Latin America.1 From February 25, 2020, when the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the etiological agent of the Coronavirus Disease 2019 (COVID-19), was firstly confirmed in Brazil, proceeding as an imported case from Italy, up to April 23, 2020, more than 124,000 cases have been reported in the Latin America and Caribbean region.2 More than 97,000 of them in South America, and more than 45,000 just in Brazil.3
COVID-19 endanger a broad spectrum of disease, going from asymptomatic cases that may recover with no specific interventions, up to complicated severe, life-threatening and even fatal disease, that may lead to unknown non-acute consequences, still to be better defined.1, 2 In such a complex clinical scenario, the epidemiological situation of Brazil and most countries in Latin America before February 25, 2020, was already intricate, with overlapping epidemics of multiple vector-borne diseases, including especially dengue and yellow fever, but also, still struggling with long-term consequences, and endemicity, of 2014–2016 epidemics of chikungunya and Zika.1, 4
Sadly, also the last years’ vaccine coverages in multiple countries of Latin America, but also some areas of individual nations, have significantly decrease, allowing the imminent menace of imported cases and spreading with local transmission of this once not reported old diseases, such as is especially the case of measles, that in fact, due to forced migration from Venezuela arrived especially to Roraima and Amazonas to lead to thousands of cases in the region.4
If this is not enough, the political scenario is not friendly for evidence-based decisions. The high-rank stakeholders have not broadly followed the recommendations of the World Health Organization (WHO) before or after the arrival of COVID-19 to the new world. Once world-recognized for the efforts in the fight against major infectious threats, such as HIV, tuberculosis, and malaria, Brazil is going facing now a challenge in the control of these infectious diseases but also confronting now one of the major epidemics in the history of the country with the pandemic COVID-19.1
Brazil now has more than 1900 recognized deaths due to COVID-19, reaching even more than 3000 new reported cases per day in April.5 As expected, more than half of the cases have been reported in the South East region, where São Paulo state is located, and where the first case arrived from Milan, Italy, less than two months ago.1 So far, São Paulo state has reported more than 11,000 cases, which is more than the incidence in the whole Ecuador, Chile, or Argentina. Indeed, all the regions and all the states of Brazil have been so far affected. All of them reported COVID-19 associated deaths. The current national incidence rate is 145 cases per 1,000,000 inhabitants, but states are reaching more than 400, and capital cities, such as Fortaleza, with more than 700. In São Paulo city is 634.5
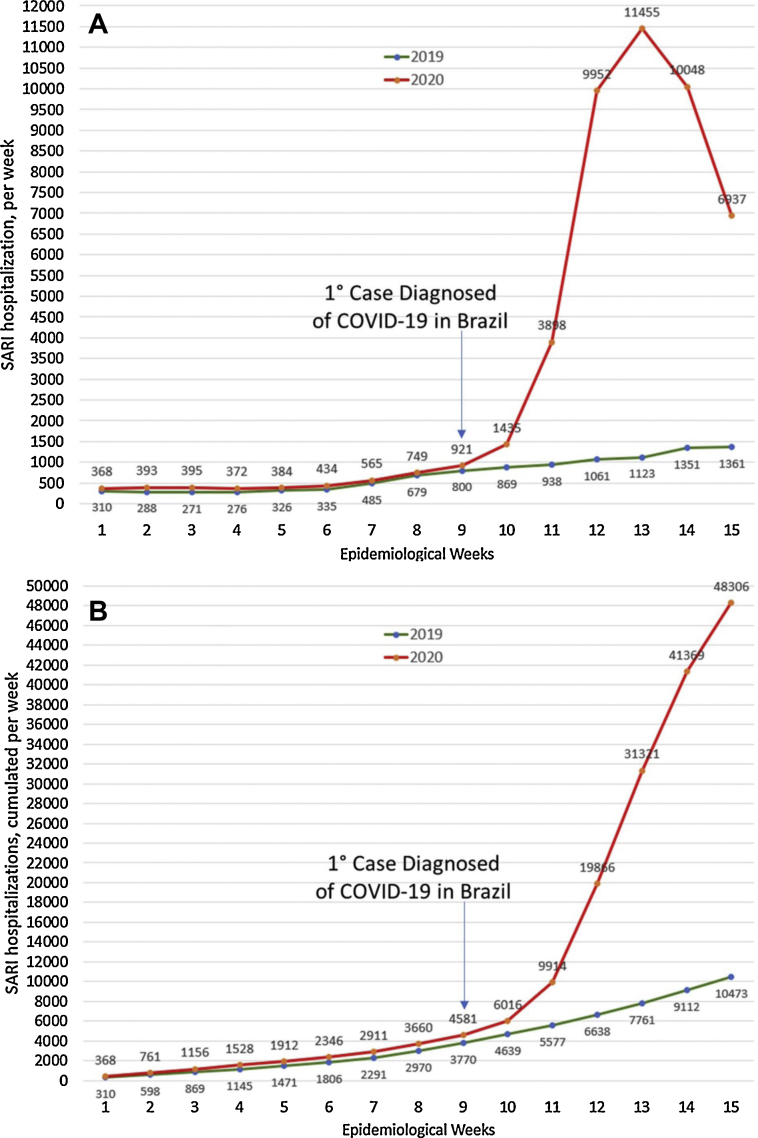
There is concern about those cases not explicitly diagnosed all over the region, as the confirmation of an example of COVID-19 is made with the molecular testing real-time reverse transcriptase-polymerase chain reaction (rRT-PCR). Currently, epidemiological data from Brazil clearly show that there is an unexpected increase in the number of hospitalizations due to severe acute respiratory infections (SARI) (Fig. 1), especially two weeks after the first case diagnosed in São Paulo, coinciding with the disease incubation period. At the 11° epidemiological week of 2020, the cumulative number of SARI hospitalizations was 1.8 times higher than the same week of 2019, but at 12° was already three times. Last week (15°), April 5–11, 2020, there was more than 4.6 times higher number of hospitalizations than in the same week of 2019 (Fig. 1). Much of that would be due to undiagnosed COVID-19 and explained in part due to the profile of infected patients, a significant proportion occurring in older people, with risk factors. In fact, from the total number of deaths confirmed (1924), 61.3% occurred in those ≥60 years old.5
Fig. 1.
Hospitalizations due to Severe Acute Respiratory Infections (SARI), during the first 15 epidemiological weeks of 2019 and 2020. (A) New number per week. (B) Cumulative per week.
Quarantine, isolation, and physical distancing, in this context, are of utmost relevance.6 Work and study activities should be carried out virtually. Still, many commercial activities should be partially restricted.7 Cases with mild respiratory symptoms should stay at home in respiratory isolation and be treated with hydration and paracetamol if needed. Visits to health centers should only be made when justified by the presence of risk factors (underlying severe disease) or warning signs (such as breathing difficulties or cognitive impairment).7 Older patients are especially susceptible to complications, and then, this population should be restricted at home. However, to reduce transmission, people of all ages must be committed to the prevention, education, and health promotion. Thus, in the absence of vaccines (that will take at least a year) or other preventive strategies, reducing the contact rate will be the only strategy to slow the progression of this pandemic.7
These measures and the proper support and advice from scientific societies, such as the Brazilian Society of Infectious Diseases, in addition to the international organizations, such as the Pan-American Health Organization (PAHO) and the WHO, adequately applied, will help to slow the number of new cases expected, will help to decrease them.7 It is difficult to predict how long these preventive measures must be maintained, but epidemiological evolution should be carefully and closely assessed to redefine strategic intervention approaches. As has been indicated before, the earlier and more rigorously they are incorporated, the faster the epidemiological conditions will be reversed, and our regular routines resumed.7
Funding
None.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Rodriguez-Morales A.J., Gallego V., Escalera-Antezana J.P., et al. COVID-19 in Latin America: the implications of the first confirmed case in Brazil. Travel Med Infect Dis. 2020:101613. doi: 10.1016/j.tmaid.2020.101613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Morales A.J., Sánchez-Duque J.A., Hernández-Botero S., et al. Preparación y control de la enfermedad por coronavirus 2019 (COVID-19) en América Latina. Acta Med Peruana. 2020;37:3–7. [Google Scholar]
- 3.PAHO . 2020. COVID-19 situation reports. https://www.paho.org/en/tag/covid-19-situation-reports. [Google Scholar]
- 4.Rodriguez-Morales A.J., Suarez J.A., Risquez A., Delgado-Noguera L., Paniz-Mondolfi A. The current syndemic in Venezuela: measles, malaria and more co-infections coupled with a breakdown of social and healthcare infrastructure. Quo vadis? Travel Med Infect Dis. 2019;27:5–8. doi: 10.1016/j.tmaid.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 5.Secretaria de Vigilância em Saúde - Ministério da Saúde . 2020. Situação Epidemiológica da COVID-19 - Doença pelo Coronavírus 2019. https://portalarquivos.saude.gov.br/images/pdf/2020/April/17/2020-04-16---BE10---Boletim-do-COE-21h.pdf. [Google Scholar]
- 6.Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diaz-Quijano F.A., Rodriguez-Morales A.J., Waldman E.A. Translating transmissibility measures into recommendations for coronavirus prevention. Rev Saude Publica. 2020;54:43. doi: 10.11606/s1518-8787.2020054002471. [DOI] [PMC free article] [PubMed] [Google Scholar]