Graphical abstract
Infographic summary
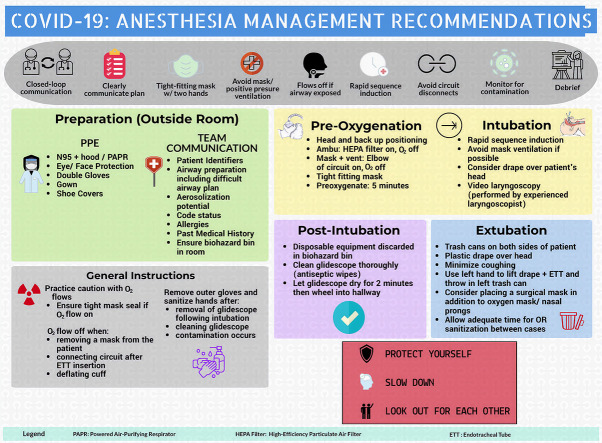
The global pandemic caused by the outbreak of the novel coronavirus, COVID-19, has brought about new concerns for the protection and safety of both patients and the healthcare workers who care for and support them. The protection of healthcare workers is of utmost importance, and the Centers for Disease Control, World Health Organization and the Anesthesia Patient Safety Foundation (APSF) have developed recommendations to minimize transmission of this pathogen from COVID-infected patients to healthcare providers. This infographic summarizes major recommendations for anesthesia management, including the use of personal protective equipment (PPE), team communication, and airway management during intubation and extubation, including precautions to be taken during aerosol generating procedures (AGPs).
AGPs, which include intubation, non-invasive ventilation, tracheotomy, cardio-pulmonary resuscitation, as well as manual ventilation prior to intubation and bronchoscopy, are all associated with increased risk of COVID transmission. Thus, special precautions must be taken when performing these procedures [[1], [2], [3]]. Healthcare providers should wear N95 masks or utilize a Powered Air-Purifying Respirator (PAPR) when performing AGPs, noting that the PAPR provides superior protection and may be warranted for patients with known or suspected COVID infection. Eye protection (goggles or face shield), and a long-sleeved, waterproof gown should also be worn. In addition, the APSF also recommends utilizing the double-glove technique, ensuring the performance of proper hand hygiene for donning and doffing of PPE and at any time contamination may be suspected [2].
In regard to intubation and when responding to an emergency, early intubation should be considered to avoid a crash intubation, leaving the healthcare team with inadequate time to appropriately don PPE. An experienced anesthesia professional should perform intubation, keeping in mind that the number of persons present in the operating room during induction should be minimized and should be specific to the number needed to adequately care for the patient [2]. Always plan for proper disposal of intubation equipment and be sure to clean and disinfect procedure room surfaces promptly [3].
Declaration of competing interest
The authors declare the following conflicts of interest:
Jared A Herman: declares no conflicts of interest
Ivan Urits: declares no conflicts of interest
Richard D. Urman: declares unrelated research funding from Merck, Medtronic. Also consulting fees from Takeda pharma.
Alan D. Kaye: declares no conflicts of interest
Omar Viswanath: declares no conflicts of interest
References
- 1.World Health Organization (WHO) Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Interim guidance. January 2020. https://www.moph.gov.lb/userfiles/files/Prevention/nCoV-%202019/20200110-nCoV-IPC-during-health-care-FINAL%20(1).pdf Available from:
- 2.Kamming D., Gardam M., Chung F. Anaesthesia and SARS. Br J Anaesth. 2003;90:715–718. doi: 10.1093/bja/aeg173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html Available from: