Abstract
Background
Patients with chronic kidney disease (CKD) are at increased risk of coronary artery disease (CAD) and adverse cardiac events. Screening for CAD is therefore an important part of preoperative evaluation for kidney transplant candidates. There is significant interest in the role of non‐invasive cardiac investigations and their ability to identify patients at high risk of CAD.
Objectives
We investigated the accuracy of non‐invasive cardiac screening tests compared with coronary angiography to detect CAD in patients who are potential kidney transplant recipients.
Search methods
MEDLINE and EMBASE searches (inception to November 2010) were performed to identify studies that assessed the diagnostic accuracy of non‐invasive screening tests, using coronary angiography as the reference standard. We also conducted citation tracking via Web of Science and handsearched reference lists of identified primary studies and review articles.
Selection criteria
We included in this review all diagnostic cross sectional, cohort and randomised studies of test accuracy that compared the results of any cardiac test with coronary angiography (the reference standard) relating to patients considered as potential candidates for kidney transplantation or kidney‐pancreas transplantation at the time diagnostic tests were performed.
Data collection and analysis
We used a hierarchical modelling strategy to produce summary receiver operating characteristic (SROC) curves, and pooled estimates of sensitivity and specificity. Sensitivity analyses to determine test accuracy were performed if only studies that had full verification or applied a threshold of ≥ 70% stenosis on coronary angiography for the diagnosis of significant CAD were included.
Main results
The following screening investigations included in the meta‐analysis were: dobutamine stress echocardiography (DSE) (13 studies), myocardial perfusion scintigraphy (MPS) (nine studies), echocardiography (three studies), exercise stress electrocardiography (two studies), resting electrocardiography (three studies), and one study each of electron beam computed tomography (EBCT), exercise ventriculography, carotid intimal media thickness (CIMT) and digital subtraction fluorography (DSF). Sufficient studies were present to allow hierarchical summary receiver operating characteristic (HSROC) analysis for DSE and MPS. When including all available studies, both DSE and MPS had moderate sensitivity and specificity in detecting coronary artery stenosis in patients who are kidney transplant candidates [DSE (13 studies) ‐ pooled sensitivity 0.79 (95% CI 0.67 to 0.88), pooled specificity 0.89 (95% CI 0.81 to 0.94); MPS (nine studies) ‐ pooled sensitivity 0.74 (95% CI 0.54 to 0.87), pooled specificity 0.70 (95% CI 0.51 to 0.84)]. When limiting to studies which defined coronary artery stenosis using a reference threshold of ≥ 70% stenosis on coronary angiography, there was little change in these pooled estimates of accuracy [DSE (9 studies) ‐ pooled sensitivity 0.76 (95% CI 0.60 to 0.87), specificity 0.88 (95% CI 0.78 to 0.94); MPS (7 studies) ‐ pooled sensitivity 0.67 (95% CI 0.48 to 0.82), pooled specificity 0.77 (95% CI 0.61 to 0.88)]. There was evidence that DSE had improved accuracy over MPS (P = 0.02) when all studies were included in the analysis, but this was not significant when we excluded studies which did not avoid partial verification or use a reference standard threshold of ≥70% stenosis (P = 0.09).
Authors' conclusions
DSE may perform better than MPS but additional studies directly comparing these cardiac screening tests are needed. Absence of significant CAD may not necessarily correlate with cardiac‐event free survival following transplantation. Further research should focus on assessing the ability of functional tests to predict postoperative outcome.
Keywords: Humans; Kidney Transplantation; Coronary Angiography; Coronary Angiography/standards; Coronary Artery Disease; Coronary Artery Disease/diagnosis; Coronary Artery Disease/etiology; Heart Function Tests; Heart Function Tests/methods; Heart Function Tests/standards; Kidney Failure, Chronic; Kidney Failure, Chronic/complications; Pancreas Transplantation; Reference Standards
Plain language summary
[Summary title]
[Summary text]
Summary of findings
Summary of findings'. 'Summary of results.
| Summary of results: Results of studies on cardiac testing in kidney transplant candidates | ||
|
Review question: Comparison of non‐invasive cardiac screening tests with coronary angiography for the detection of significant CAD in potential kidney transplant recipients Patient population: Kidney transplant candidates undergoing pre‐transplant cardiac evaluation Setting: Investigations performed in hospital or in an outpatient setting Geographical location: Studies were conducted in USA (12 studies), Brazil (4 studies), India, (3 studies) the UK (3 studies), Australia (1 study), Canada (1 study), and Spain (1 study) Index test : Any non‐ or minimally invasive test used to assess risk of CAD. Reference standard: Coronary angiography Included studies: DSE (13 studies; 745 participants), MPS (9 studies; 582 participants), EST (2 studies; 129 participants), EBCT (1 study; 97 participants), DSF (1 study; 86 participants), exercise ventriculography (1 study; 35 participants), CIMT (1 study; 105 participants), resting wall motion abnormality on echocardiography (2 studies; 265 participants), left ventricular dysfunction on echocardiography (1 study; 52 participants), mitral annular calcification on echocardiography (1 study; 125 participants), resting ECG (3 studies; 263 participants). | ||
| Limitations | ||
| Only DSE and MPS were evaluated in detail, although these also had only a limited number of included comparisons with small sample sizes. No studies were found investigating cardiopulmonary exercise testing, CT coronary angiography, magnetic resonance angiography or cardiac magnetic resonance imaging. Fewer than five studies were found for each of EBCT, resting ECG, conventional echocardiography, exercise ventriculography, DSF and CIMT. Sparse directly comparative data also resulted in low power to detect important differences in accuracy between tests. Significant heterogeneity was present among studies investigating the same screening test. Although differences in study population characteristics (e.g. prevalence of chest pain) and test application (diagnostic test threshold, criteria for positive test, choice of stress agent and stress protocol, and operator variability) likely contributed to heterogeneity, we were hindered from estimating their contributions because of relatively sparse data, which resulted in low power. Partial verification, where not all patients who received screening tests also received coronary angiography, occurred in 5/25 comparisons. This may have affected estimates of sensitivity and specificity. Two different reference standard thresholds (≥ 70% stenosis or ≥ 50% stenosis) were used in the included studies, with most studies only using one reference standard threshold or the other. An overall analysis pooling the results of all studies regardless of threshold may introduce additional heterogeneity due to a threshold effect. | ||
| Results | ||
| Test | DSE | MPS |
| Number of studies [all studies] | 13 | 9 |
| Number of participants [all studies] | 745 | 582 |
| Pooled sensitivity (95% CI) [all studies] | 0.79 (0.67 to 0.88) | 0.74 (0.54 to 0.87) |
| Pooled specificity (95% CI) [all studies] | 0.89 (0.81 to 0.94) | 0.70 (0.51 to 0.84) |
| Number of studies [≥ 70% stenosis] | 9 | 7 |
| Number of participants [≥ 70% stenosis] | 668 | 517 |
| Pooled sensitivity (95% CI) [≥ 70% stenosis] | 0.76 (0.60 to 0.87) | 0.67 (0.48 to 0.82) |
| Pooled specificity (95% CI) [≥ 70% stenosis] | 0.88 (0.78 to 0.94) | 0.77 (0.61 to 0.88) |
| Number of false diagnoses of ≤ 70% coronary artery stenosis in a standard population of 100 patients (false negative rate) | 24 (13 to 40) per 100 |
33 (18 to 52) per 100 |
| Number of false diagnoses of ≥ 70% coronary artery stenosis in a standard population of 1000 patients (false positive rate) | 12 (6 to 22) per 100 |
23 (12 to 39) per 100 |
| Positive likelihood ratio [≥ 70% stenosis] (95% CI) | 6.44 (3.03 to 13.70) | 2.89 (1.39 to 5.99) |
| Negative likelihood ratio [≥ 70% stenosis] (95% CI) | 0.26 (0.13 to 0.50) | 0.43 (0.23 to 0.80) |
| Post test probability after positive screening test result for a patient with low risk (10% to 29% pre test probability) disease | 42% to 72% | 24% to 54% |
| Post test probability after positive screening test result for a patient with intermediate risk (30% to 59% pre test probability) disease | 73% to 90% | 55% to 81% |
| Post test probability after positive screening test result for a patient with high risk (60% to 90% pre test probability) disease | 91% to 98% | 81% to 96% |
| Post test probability after negative screening test result for a patient with low risk (10% to 29% pre test probability) disease | 3% to 10% | 5% to 15% |
| Post test probability after negative screening test result for a patient with intermediate risk (30% to 59% pre test probability) disease | 10% to 27% | 16% to 38% |
| Post test probability after negative screening test result for a patient with high risk (60% to 90% pre test probability) disease | 28% to 70% | 39% to 79% |
| Conclusions and comments | ||
| Both tests, especially DSE, have a role as triage tests for intermediate risk transplant candidates, with negative results precluding the need for further evaluation with coronary angiography, thereby avoiding unnecessary risk to patients and potentially reducing healthcare costs. Given the wide heterogeneity in the estimates for both DSE and MPS, there is still considerable uncertainty in the true post‐test probabilities of each test. Current evidence suggests that, where feasible, DSE should be used as the screening investigation of choice over MPS. | ||
| Applicability of tests in clinical practice | ||
| Both DSE and MPS have a role as triage tests for the intermediate risk transplant candidates, with negative results reducing the need for further evaluation with coronary angiography. In high risk patients, a positive non‐invasive DSE or MPS confirms the high risk of severe CAD, but a negative result does not conclusively rule out severe CAD. In these patients, one may consider proceeding immediately to coronary angiography and avoid using functional tests. The relatively low sensitivity and specificity of both DSE and MPS however means that they are not perfect triage tests and a significant number of patients will either have their significant CAD missed (false negatives) or be referred in vain for coronary angiography (false positive). Despite the shortcomings of the non‐invasive tests in their role as triage tests, the very select nature of the population and the unique challenges facing cardiac investigation in this population (particularly, the need to avoid complications arising from an invasive gold standard) and the lack of an alternate better performing test means that we are forced to accept an imperfect triage test. Functional testing may provide additional prognostic information, although an investigation into this was not included under the scope of this review. | ||
| Costs | ||
| None of the studies included a cost‐effectiveness evaluation. MPS is known to be more expensive than DSE, although both are less expensive than the reference standard, coronary angiography. | ||
CAD ‐ coronary artery disease; CI: confidence interval; CIMT: carotid intimal medial thickness; DSE: Dobutamine stress echocardiography; MPS: Myocardial perfusion scintigraphy
Background
Kidney transplantation remains the best treatment for patients with end‐stage kidney disease (ESKD) in terms of prolonging survival and improving quality of life. However, research has shown that transplantation causes significant cardiovascular stress around the time of the operation, and the incidence of myocardial infarction has been estimated to be approximately 5% (Gunnarsson 1984; Lentine 2005). Cardiovascular disease accounts for almost half (40% to 55%) of all deaths following kidney transplantation (Briggs 2001). Screening for coronary artery disease (CAD) is therefore an important part of evaluation for kidney transplantation and a key decision tool to identify which patients need specialised heart imaging tests (coronary angiography) and when. Clinical practice varies considerably in how patients are selected for testing; some centres test only those patients with significant risk factors, others test all kidney transplant candidates; and in which screening test is used (Hofmann 2008). The studies we reviewed used tests such as dobutamine stress echocardiography (DSE), myocardial perfusion scintigraphy (MPS) and stress electrocardiography (EST) versus radiographic tests such as calcium scoring, among others (Hofmann 2008).
Clinical practice guidelines from the American Society of Transplantation (Kasiske 2001), United Kingdom Renal Association (Dudley 2008) and Canadian Society of Transplantation (Knoll 2005) advise cardiac stress testing in potential transplant recipients who have symptoms or significant risk factors, but do not recommend a particular screening test. The guidelines indicate that the test should be determined by local availability and expertise. Although various screening tests for CAD are available, it remains unclear which tests perform best for patients with ESKD.
Target condition being diagnosed
The target condition was significant CAD in potential kidney transplant recipients. We defined significant CAD as the presence of at least 50% stenosis in at least one epicardial coronary artery detected on coronary angiography.
Index test(s)
Any non‐ or minimally invasive test used to assess risk of CAD. These included:
Stress echocardiography (using either exercise or pharmacological stress, such as DSE)
MPS using either exercise or pharmacological stress
EST
Electron beam computed tomography (EBCT)
Resting electrocardiography (ECG)
Conventional echocardiography
Exercise ventriculography
Digital subtraction fluorography (DSF)
Carotid intimal medial thickness (CIMT)
Cardiopulmonary exercise testing
Computed tomography (CT) coronary angiography
Magnetic resonance angiography
Cardiac magnetic resonance imaging.
Rationale
Severe CAD is strongly associated with the risk of myocardial infarction (MI) (Alderman 1993; Manoharan 2009). Non‐invasive cardiac screening tests may enable identification of kidney transplant candidates who are at high risk of significant CAD. Such tests are therefore useful in triaging patients for coronary angiography, a test that provides confirmation of diagnosis and opportunity for timely intervention (endovascular or open surgical intervention, and aggressive risk factor modification, or both). There is significant controversy about which tests should be used in the screening process (Hofmann 2008). Although coronary angiography is the gold standard for detecting coronary artery stenosis, it is invasive, costly, and carries risk of nephrotoxicity, arrhythmia, MI, stroke and femoral artery injury. Although anatomical depiction derived from coronary angiography is a valuable diagnostic asset, the test does not provide perfusion or contractility information when the heart is under physiological stress. Non‐invasive investigations such as DSE and MPS have moderate sensitivity and specificity in detecting significant CAD in the general population (Fleischmann 1998; Schinkel 2003). The applicability of these results in patients with ESKD who are potential kidney transplant recipients is however uncertain. Common comorbidities among patients with chronic kidney disease (CKD) are hypertension, cardiomyopathy, calcific vascular disease and atherosclerosis. Compared with the general population, these comorbidities may influence diagnostic test performance in people with CKD.
Objectives
We investigated the diagnostic accuracy of non‐invasive cardiac screening tests versus coronary angiography in potential kidney transplant recipients. We provided summary estimates of diagnostic accuracy for individual index tests to better understand the utility and limitations of these non‐invasive tests.
Secondary objectives
We compared the diagnostic accuracy among different screening tests through:
Direct comparison: By analysing the results of studies that assessed diagnostic accuracy of two or more tests in the same population head‐to‐head.
Indirect comparison: By comparing the pooled results of studies that assessed accuracy of screening tests in separate populations.
The ability of screening tests to detect severe coronary artery stenosis (≥ 70% stenosis detected on coronary angiography) was also assessed and compared among different screening tests.
Investigation of sources of heterogeneity
We also investigated if diagnostic accuracy varied among studies with different prevalence of symptomatic chest pain and analysed the effect. For this analysis, we included only studies that used a threshold of ≥ 70% stenosis on coronary angiography for the diagnosis of CAD. To avoid partial verification, we considered effects among study participants who underwent both the index test and coronary angiography. This methodology meant that we were able to avoid partial verification.
Methods
Criteria for considering studies for this review
Types of studies
We included all diagnostic cross sectional studies, cohort studies and randomised studies of test accuracy that compared cardiac test accuracy with results obtained from coronary angiography (the reference standard).
Participants
Study participants included all patients who were considered to be potential candidates for kidney transplantation or kidney‐pancreas transplantation at the time the diagnostic tests were performed.
Inclusion criteria
We included studies reporting outcomes relating to patients considered to be potential candidates for kidney transplantation or kidney‐pancreas transplantation at the time diagnostic tests were performed. To ensure that our review was accessible and succinct, we chose to limit the population to patients with CKD who were considered candidates for kidney transplantation, but included all possible tests used to diagnose CAD.
Exclusion criteria
Studies were excluded if they did not explicitly state that all study participants were candidates for kidney transplantation. We also excluded studies that investigated cardiac test accuracy in patients with ESKD who were not transplant candidates (i.e. they were unselected dialysis patients, not undergoing pre‐transplant assessment). Patients with ESKD who are not transplantation candidates differ from patients who are transplant candidates with respect to several key prognostic variables, such as age and fitness for surgery. These differences in the key prognostic variables may result in differences in disease prevalence and test performance. We also excluded studies which investigated patients with features of acute coronary syndrome as our aim was to investigate the performance of cardiac tests in a preoperative screening context. Where it appeared that only some of the study participants were transplantation candidates, we contacted the study authors requesting separate data for only transplantation candidates.
Index tests
Any non‐ or minimally invasive test used to assess risk of CAD. These included:
Stress echocardiography (using either exercise or pharmacological stress, e.g. DSE)
MPS using either exercise or pharmacological stress
EST
EBCT
ECG
Conventional echocardiography
Exercise ventriculography
DSF
CIMT
Cardiopulmonary exercise testing
CT coronary angiography
Magnetic resonance angiography
Cardiac magnetic resonance imaging.
Information regarding the various index tests including the type of result produced, if cut‐off values were present, and how differences in cut‐off points were handled, is provided in Table 2.
1. Description of index tests.
| Test | Description | Advantages | Disadvantages | Type of result | Presence of cut‐off values |
| Screening tests | |||||
|
MPS Stress Exercise dipyridamole dobutamine Radionucleotide thallium‐201 or Tc‐99m sestamibi radionucleotide agents |
This compares perfusion of myocardium at rest and after a ‘stress’ such as exercise or drugs (e.g. dipyridamole).
When coronary arteries are normal, ‘stress’ results in vasodilatation and increased coronary blood flow. However, diseased coronary arteries cannot dilate because they are already maximally dilated and there is no increase in blood flow after a stress. MPS reveals these areas as regions of decreased perfusion. A reversible perfusion defect is a sign of ischaemia. A fixed defect (when there is decreased perfusion before, during and after the stress) is an indicator of infarction. Pharmacological agents overcome limitations of exercise testing in patients with kidney disease |
Non‐invasive Provides information regarding functional status of myocardium under stress conditions |
Neither 100% sensitive nor specific Radiation dose Results subject to interpretation and reader bias False positives due to increase in attenuation artefacts caused by left ventricular hypertrophy False negatives due to balanced ischaemia (e.g. triple vessel disease) More expensive than exercise ECG |
Dichotomous (i.e. stress test positive or stress test negative) | None. However, whether a stress test is interpreted as positive or negative depends largely on observer interpretation |
|
DSE Stress Exercise dobutamine |
Stress echocardiography compares the regional wall motion and thickness of myocardium both at rest and after stress. Regional systolic dysfunction is usually caused by CAD. Pharmacological stress agent overcomes limitations of exercise testing in patients with kidney disease |
Non‐invasive No radiation dose Provides information regarding functional status of myocardium under stress conditions Provides assessment of ventricular size and function |
Neither 100% sensitive nor specific Results subject to interpretation and reader bias Operator dependent Acoustic windows not possible in up to 20% of subjects Hypertensive response to stress agent possible Cardiomyopathies may also show regional variation in function |
Dichotomous (i.e. stress test positive or stress test negative) | None. However, whether a stress test is interpreted as positive or negative depends largely on observer interpretation |
|
Exercise ECG Bruce protocol stress ECG |
Patient exercises on a treadmill while connected to an ECG. The level of exercise is increased in progressive stages. The patient's symptoms and blood pressure response are checked repeatedly. Ischaemic ECG changes or angina symptoms brought on by exercise are highly suggestive of underlying CAD | Non‐invasive Provides information regarding functional status of myocardium under stress conditions |
Neither 100% sensitive nor specific Results subject to interpretation and reader bias Often limited by the inability of CKD patients to achieve an adequate peak exercise workload, development of exercise‐induced hypotension High proportion have abnormal baseline ECG (left ventricular hypertrophy) |
Dichotomous (i.e. stress test positive or stress test negative) | No. However, whether a stress test is interpreted as positive or negative depends largely on observer interpretation |
|
Coronary artery calcium score EBCT Multidetector computed tomography |
Cardiac calcium scoring is a non‐invasive test that uses computed tomography to detect the presence of calcium in plaque on the walls of the arteries of the heart (coronary arteries). A calcium score is then derived, calculated as a summation of all calcified lesions in the coronary arteries. The calcium score is then compared with a reference range appropriate to a patient's age and sex. High calcium scores are associated with higher risks of cardiovascular events | Non‐invasive | Neither 100% sensitive nor specific Radiation dose |
Continuous | There is no uniformly agreed cut‐off value at which patients are considered at high risk of CAD. We planned to analyse results by combining data from studies which share identical cut‐off values |
|
Echocardiography Trans‐thoracic Trans‐oesophageal |
An ultrasound of the heart that enables assessment of structure and function. Impairment in systolic function can result from pre‐existing CAD |
Provides information regarding myocardial function and regional wall abnormalities, which may suggest pre‐existing ischaemia or MI Enables assessment of structure |
Neither highly sensitive nor specific Does not provide any information of reversible ischaemia Results subject to interpretation and reader bias |
Dichotomous (e.g. presence or absence of resting wall motion abnormality) | None |
| CT coronary angiography | Specialised form of CT that enables imaging of the heart and computerised reconstruction of coronary arteries, permitting assessment of the lumen and vessel walls | Non‐invasive Enables diagnosis of precise location and severity of each lesion as opposed to vascular territory affected, as is the case for most functional tests. Assesses not only the lumen of the vessel but also the wall. It can also demonstrate soft atheromatous plaques, which cannot be demonstrated on conventional coronary angiography |
Radiation dose Contrast nephropathy Inability to provide opportunity for immediate intervention (as opposed to coronary angiography) |
Dichotomous (i.e. presence or absence of significant CAD) | Yes (i.e. ≥ 50% stenosis or ≥ 70% stenosis) We planned to manage the issue of different cut points by involving an analysis that included:
|
| Cardiac magnetic resonance imaging | MRI of the heart that enables evaluation of its structure and function | Non‐invasive No radiation dose Enables assessment of structure of myocardium High spatial resolution means low inter‐observer variability |
Neither highly sensitive nor specific |
Dichotomous (e.g. presence or absence of left ventricular systolic dysfunction) | None |
| Resting ECG | Transthoracic interpretation of the electrical activity of the heart over time captured and externally recorded by skin electrodes | Provides information regarding the electrical function of the myocardium, which may suggest pre‐existing ischaemia, left ventricular hypertrophy or arrhythmias | Neither sensitive nor specific Does not provide any information of reversible ischaemia |
Dichotomous (i.e. presence or absence of certain ECG features) | None |
| CIMT | Measurement of the thickness of artery walls, usually by external ultrasound, to detect both the presence and to track the progression of atherosclerotic disease in humans. Used as a surrogate marker for atherosclerosis | Non‐invasive | Neither highly sensitive nor specific Does not provide any information on cardiac function |
Continuous | Yes. This will vary depending on the institution (e.g. 0.75 mm) |
| Cardiopulmonary exercise testing | Evaluates both cardiac and pulmonary function. Cardiac function is evaluated in terms of aerobic capacity and respiratory function. The subject is exercised on a bicycle ergometer or treadmill. The test enables calculation of maximal aerobic capacity and the point during exercise where anaerobic metabolism is used to supplement aerobic metabolism as a source of energy. These can be measured via gas exchange data |
Non‐invasive measurement of ventricular function, respiratory function and cellular function via measurement of gas exchange, as well as detection of myocardial ischaemia Excellent method of evaluating fitness and operative fitness |
Not commonly performed | Dichotomous (e.g. stress ECG positive or stress ECG negative; presence or absence of cardiac failure) and Continuous (e.g. measurement of the maximum aerobic capacity and anaerobic threshold) |
Yes, although these will vary for different variables and for different institutions |
| DSF | Used to detect coronary artery calcification. Digital subtraction improves resolution of conventional fluoroscopic methods | Non‐invasive Non exercise |
Not commonly used Radiation dose |
Dichotomous (i.e. presence or absence of calcification) | None |
| Exercise radionucleotide ventriculography | Technique for a combined assessment of exercise capacity and an evaluation of ventricular size and performance | Not commonly used Radiation dose |
Dichotomous (i.e. stress test positive or stress test negative) | None. However, whether a stress test is interpreted as positive or negative depends largely on observer interpretation | |
| Reference standard | |||||
| Coronary angiography | Coronary catheterisation is an invasive procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It can be performed for both diagnostic and interventional (treatment) purposes. It assesses the diameter of coronary artery lumens, heart chamber size and heart muscle contraction performance | Gold standard for detecting CAD. Enables diagnosis of precise location and severity of each lesion Intervention (PTCA) possible during procedure |
High cost Lack of sensitivity to intramural coronary atherosclerosis Risk of complications Intravenous contrast media may worsen kidney function Little information on function Radiation dose Results subject to interpretation and reader bias, although to a lesser extent than functional tests |
Dichotomous (i.e. presence or absence of significant CAD) | Yes (i.e. ≥ 50% stenosis or ≥ 70% stenosis). We managed the issue of different cut points by involving an analysis which included:
|
CAD: coronary artery disease; CIMT: carotid intimal medial thickness; CT: computed tomography; ECG: electrocardiograph; MPS: myocardial perfusion scintigraphy; MRI: magnetic resonance imaging; PTAC: percutaneous transluminal coronary angioplasty
Comparator tests
Any of the listed index tests where they were compared with each other versus the reference standard of coronary angiography.
Target conditions
Coronary artery stenosis was defined as at least 50% narrowing in at least one epicardial coronary artery on coronary angiography. We defined severe coronary artery stenosis as ≥ 70% stenosis on coronary angiography.
Reference standards
Coronary angiography.
Search methods for identification of studies
Electronic searches
We searched the following resources.
MEDLINE (OvidSP) 1950 ‐ 1 November 2010
EMBASE (OvidSP) 1980 ‐ November 2010, Week 44
A Trials Search Co‐ordinator of the Cochrane Renal Group (RM) formulated specific search strategies for the MEDLINE and EMBASE searches ( Appendix 1).
Citation tracking was performed using Web of Science. No restrictions were imposed in terms of language of publication or publication status. To maximise the sensitivity of our search, we avoided the use of methodology filters when searching for diagnostic accuracy studies because even the most sensitive filters have been found to miss relevant studies (de Vet 2008; Doust 2005).
Searching other resources
We handsearched the reference lists of all primary studies and reviews identified by the initial search.
Data collection and analysis
Selection of studies
Two authors independently reviewed the search results, first by title and abstract, and where necessary by review of full text of the study report, to determine inclusion or exclusion. Resulting sets of citations for inclusion were also compared. A third author was available to arbitrate final decisions to include or exclude.
Data extraction and management
A standardised data extraction form was used to abstract study design features and results data from each publication. For each study data were extracted independently by two authors. We extracted: year of publication, country of study, study design, clinical setting, definition of CAD (stenosis percentage on coronary angiogram), the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) methodological items (Reitsma 2009), prevalence of cardiovascular risk factors in the study population (percentages of participants on haemodialysis; with ESKD, diabetes mellitus (DM), hypertension; who were male; with history of smoking; and symptomatic of heart disease). We also recorded the numbers of true positives, true negatives, false positives and false negatives. These data were then collated in a spreadsheet. A third author was available to adjudicate on disagreements.
Assessment of methodological quality
Methodological quality of included primary studies was assessed by two authors using a modified QUADAS tool (Smidt 2008; Whiting 2003) that included 11 of the 14 mandatory items (representative spectrum, acceptable reference standard, acceptable delay between tests, partial verification avoided, differential verification avoided, incorporation avoided, reference standard results blinded, index test results blinded, relevant clinical information, uninterpretable results explained, withdrawals explained) (Smidt 2008; Whiting 2003). The operational definitions of the QUADAS items are presented in Appendix 2.
Statistical analysis and data synthesis
Extracted data were used to create forest plots of sensitivity and specificity, to depict study‐specific estimates of sensitivity and specificity in receiver operating characteristic (ROC) space for each index test, and to investigate:
the diagnostic performance of each index test
heterogeneity in the diagnostic performance of each index test according to patient characteristics, study design, and study quality factors (identified in Table 3 where sufficient data were available)
the relative diagnostic performance of alternate tests based on all available studies that provided data for at least one test, and when the analysis was restricted to studies that provided data for both tests.
2. Characteristics of included studies.
| Study | Country | Participants | Diabetic patients (%) | Angina (%) | Hypertensive (%) | Male (%) | Reference threshold (% stenosis) | TP | FP | FN | TN |
| Dobutamine stress echocardiography (DSE) | |||||||||||
| Bates 1996 | USA | 17 | 100 | NA | 98 | 64 | 50 | 9 | 1 | 1 | 6 |
| Brennan 1997 | USA | 12 | 56 | 21 | 90 | 45 | 50 | 4 | 1 | 2 | 5 |
| Cai 2010 | USA | 38 | 54 | NA | 86 | 64 | 70 | 15 | 2 | 8 | 13 |
| De Lima 2003 | Brazil | 89 | 30 | 25 | 95 | 77 | 70 | 15 | 7 | 19 | 48 |
| Ferreira 2007 | Brazil | 126 | 27 | 12 | NA | 69 | 70 | 24 | 14 | 10 | 78 |
| Gang 2007 | India | 40 | 100 | 5 | 92 | 90 | 70 | 9 | 1 | 10 | 20 |
| Garcia‐Canton 1998 | Spain | 27 | NA | NA | NA | 67 | 70 | 11 | 2 | 1 | 13 |
| Herzog 1999 | USA | 50 | 82 | 16 | 94 | 60 | 70 | 12 | 8 | 4 | 26 |
| Jassal 2007 | Canada | 18 | 38 | NA | 77 | 44 | 50 | 0 | 0 | 0 | 18 |
| Reis 1995 | USA | 30 | 64 | 30 | 96 | 63 | 50 | 22 | 1 | 1 | 6 |
| Sharma 2005 | UK | 125 | 39 | 42 | 91 | 64 | 70 | 32 | 5 | 4 | 84 |
| Sharma 2009 | UK | 140 | 38 | 27 | 92 | 64 | 70 | 36 | 5 | 4 | 95 |
| West 2000 | USA | 33 | NA | NA | NA | NA | 70 | 12 | 8 | 1 | 12 |
| Myocardial perfusion scintigraphy (MPS) | |||||||||||
| Boudreau 1990 | USA | 80 | 100 | 12.5 | NA | 64 | 70 | 36 | 8 | 6 | 30 |
| De Lima 2003 | Brazil | 65 | 30 | 25 | 95 | 77 | 70 | 8 | 10 | 15 | 32 |
| Garcia‐Canton 1998 | Spain | 27 | NA | NA | NA | 67 | 70 | 11 | 3 | 1 | 12 |
| Garg 2000 | India | 19 | 100 | NA | 100 | 88 | 50 | 9 | 4 | 2 | 4 |
| Gowdak 2010 | Brazil | 219 | 100 | NA | 92 | 69 | 70 | 85 | 31 | 52 | 51 |
| Krawczynska 1988 | USA | 46 | NA | NA | NA | NA | 50 | 20 | 18 | 0 | 8 |
| Marwick 1990 | USA | 45 | 51 | 33 | 81 | 71 | 70 | 4 | 9 | 10 | 22 |
| Vandenberg 1996 | USA | 41 | 100 | 0 | NA | NA | 75 | 10 | 6 | 6 | 19 |
| Worthley 2003 | Australia | 40 | 78 | 18 | 98 | 48 | 70 | 13 | 3 | 2 | 22 |
| Stress electrocardiography (EST) | |||||||||||
| Bennett 1978 | USA | 4 | 100 | NA | 100 | 36 | 70 | 3 | 1 | 0 | 0 |
| Sharma 2005 | UK | 125 | 39 | 42 | 91 | 64 | 70 | 13 | 8 | 23 | 81 |
| Electron beam computed tomography (EBCT) | |||||||||||
| Rosario 2010 | Brazil | 97 | 38 | 29 | 90 | 65 | 70 | 16 | 25 | 9 | 47 |
| Sharples 2004 | UK | 18 | NA | NA | NA | 50 | 75 | * | * | * | * |
| Digital subtraction fluorography (DSF) | |||||||||||
| Marwick 1989 | USA | 86 | 29 | 11 | 36 | 27 | 70 | 28 | 17 | 8 | 33 |
| Exercise ventriculography | |||||||||||
| Vandenberg 1996 | USA | 35 | 100 | 0 | NA | NA | 75 | 7 | 7 | 7 | 14 |
| Carotid intimal media thickness (CIMT) | |||||||||||
| Modi 2006 | India | 105 | 58 | 24 | 100 | NA | 97 | 38 | 14 | 4 | 49 |
| Echocardiography (resting wall motion abnormality) | |||||||||||
| Sharma 2005 | UK | 125 | 39 | 42 | 91 | 64 | 70 | 11 | 4 | 25 | 85 |
| Sharma 2009 | UK | 140 | 38 | 27 | 92 | 64 | 70 | 13 | 5 | 27 | 95 |
| Echocardiography (cardiomegaly or LV dysfunction) | |||||||||||
| Garg 2000 | India | 19 | 100 | NA | 100 | 88 | 50 | 8 | 5 | 19 | 20 |
| Echocardiography (mitral annular calcification) | |||||||||||
| Sharma 2005 | UK | 125 | 39 | 42 | 91 | 64 | 70 | 22 | 25 | 14 | 64 |
| Resting ECG (pathological Q waves, left ventricular hypertrophy, ST depression ≥ 1 mm, ST elevation ≥ 1 mm, T wave inversion or bundle branch block) | |||||||||||
| Gang 2007 | India | 40 | 100 | 5 | 92 | 90 | 70 | 9 | 12 | 10 | 9 |
| Garg 2000 | India | 98 | 100 | NA | 100 | 88 | 50 | 51 | 1 | 22 | 24 |
| Sharma 2005 | UK | 125 | 39 | 42 | 91 | 64 | 70 | 27 | 14 | 9 | 75 |
FN: false negative; FP: false positive; NA: not available; TN: total negative; TP: total positive
* Study unable to contribute data to meta‐analysis as it reported results per coronary vessel, and not per patient
Hierarchical summary receiver operating curve (HSROC) models were fitted using the PROC NLMIXED procedure in SAS9.2®. We applied the HSROC model to derive inferences about diagnostic test accuracy and heterogeneity in test performance where sufficient studies (n ≥ 5) for tests were available. The HSROC model used study specific estimates of sensitivity and specificity to estimate the position and shape of the summary curve (Rutter 2001). The curve was defined by three parameters: threshold (the underlying test positivity rate: a proxy for the cut‐point that defines a positive test); accuracy (the diagnostic log odds ratio); and shape (the dependence of accuracy on threshold). Each study provided an estimate for threshold and accuracy which were assumed to be random effects in the model. When there was no evidence of an association between accuracy and threshold, the summary curve was considered symmetric and its position defined by a constant diagnostic odds ratio (DOR). The model estimates were used to obtain summary estimates for sensitivity, specificity, positive and negative likelihood ratios, DORs and 95% confidence intervals (CI), and the corresponding 95% confidence region for each index test. The corresponding area under the curve (AUC) was computed from the constant DOR as part of the analysis.
HSROC model results were used to create plots of estimated summary curves, summary points and confidence regions, superimposed on study‐specific estimates of sensitivity and specificity.
We provided summary measures of diagnostic accuracy for:
all studies regardless of CAD threshold on coronary angiography
studies that reported ≥ 70% stenosis threshold for diagnosis of significant CAD on coronary angiography.
Pairwise comparisons of test performance among alternative index tests were performed using data from studies where comparisons between tests were made in the same study population (direct comparison) or in different study populations (indirect comparison). A covariate of test type was included in the modelling to assess if the SROC curves for tests differed in shape, or overall accuracy. When comparing the relative performance of two index tests, we initially assumed equal variances for random effects for the tests, but extended the models to accommodate unequal variances for random effects where required.
In studies reporting multiple tests in the same participants, results were expressed separately for each test component.
Investigations of heterogeneity
Factors that could influence diagnostic accuracy other than true test performance included those relating to methodological quality and study design, characteristics of the underlying population, and characteristics of the index and reference test. We detailed and compared patient inclusion criteria for each included study. We also investigated heterogeneity statistically by:
applying separate models to different subgroups
adding covariates to the hierarchical model.
Factors such as differences in study population characteristics (e.g. prevalence of chest pain, hypertension and diabetes) and test application (diagnostic test threshold, criteria for positive test, choice of stress agent and stress protocol, and operator variability) were used to explore any heterogeneity discovered in the analysis for each test separately, and to assess the impact of heterogeneity on the relative accuracy across tests.
For index tests such as ECG and echocardiography, where different definitions of an abnormal test were present, only data that had been measured using the same definitions were combined.
Sensitivity analyses
Where differences were present across studies, we controlled for heterogeneity by conducting sensitivity analyses. In particular, we investigated diagnostic accuracy in studies that:
aimed to provide both index tests and reference tests to their study population (studies that avoided verification bias)
applied a threshold of diagnosis of severe CAD of ≥ 70% stenosis on coronary angiography
consisted entirely of asymptomatic individuals (studies that excluded patients who had either symptoms of cardiac disease or a history of ischaemic heart disease).
Results
Results of the search
The results of electronic database and handsearching are outlined in Figure 1. There were no disagreements between authors about either the number of studies eligible for inclusion, nor data results (κ = 1.0). We identified 26 reports of 25 studies (35 comparisons in total). Seven studies compared more than one test versus coronary angiography, and were interrogated to contribute data to more than one test comparison (De Lima 2003; Gang 2007; Garcia‐Canton 1998; Garg 2000; Sharma 2005; Sharma 2009; Vandenberg 1996). One study was reported twice (Sharma 2005), and one study (Sharples 2004) could not contribute to the meta‐analysis because it reported results per coronary vessel, but not per patient. The diagnostic and treatment pathway is presented at the patient level, but including vessel‐level analysis lead to inappropriate weighting in the combined analysis, and the potential for bias from clustering of patients' results. The details of all studies included in the meta‐analysis are reported in Characteristics of included studies and Table 3.
1.

Flow of studies identified in literature search for systematic review of testing for coronary artery disease in potential kidney transplant recipients
* Some studies investigate more than one test and so contribute to more than one test comparison
CIMT: carotid intimal medial thickness; DSE: dobutamine stress echocardiography; DSF: digital subtraction fluorography; EBCT: electron beam computed tomography; ECG: resting electrocardiography; Echo/LV: echocardiography (left ventricular dysfunction or cardiomegaly); Echo/MAC: echocardiography (mitral annular calcification); Echo/RWMA: echocardiography (resting wall motion abnormality); EST: exercise stress electrocardiography; EV: exercise ventriculography; MPS: myocardial perfusion scintigraphy
We identified a further 11 studies (Caglar 2006; Dahan 1995; Dahan 1998; Dahan 2002; De Vriese 2009; Fujimoto 2006; Fukui 2005; Nishimura 2004; Ohtake 2005; Robinson 2007; Schmidt 2001) that reported diagnostic test accuracy in patients with CKD. However, populations in these studies did not consist entirely of patients who were being considered for kidney transplantation ‐ patients on dialysis or with CKD who were not being considered for transplantation were also represented. These studies were excluded from the review because we were unable to obtain separate data for potential kidney transplant recipients only from the authors of these 11 studies. We excluded a total of 55 studies from our review (see Characteristics of excluded studies).
Methodological quality of included studies
Results of the validity assessment are depicted (Figure 2; Figure 3) for the 25 included studies, including Sharples 2004, which could not contribute data. Only 10 included studies provided sufficient information to enable scoring for the 11 nominated QUADAS methodological items. Seven studies satisfied the QUADAS criteria. All included studies satisfied the QUADAS criteria of including study populations that represented the intended target population (potential kidney transplant recipients) and an acceptable reference standard (coronary angiography). Incorporation bias; which occurs when the index test is incorporated in a composite reference standard, often leading to overestimation of diagnostic test accuracy, was not present in any study. No patients were verified with a second or third reference standard because disease status (CAD) was diagnosed only by coronary angiography. Differential verification was therefore also avoided in all studies. The reference standard was not blinded to investigators in three studies that reported coronary angiography being undertaken although results of non‐invasive index test were known to the investigators (Brennan 1997; De Lima 2003; Gang 2007). It was unclear if index test results were known at the time of coronary angiography in seven studies (Bennett 1978;Cai 2010; Gowdak 2010; Jassal 2007; Krawczynska 1988; Reis 1995; West 2000). In one study (De Lima 2003, author communication), coronary angiography results were known to investigators who interpreted the index test. It was also unclear if coronary angiography results were known at the time of the index test in eight studies (Bennett 1978; Cai 2010; Gang 2007; Gowdak 2010; Jassal 2007; Krawczynska 1988; Rosario 2010; West 2000). Of the 25 included studies, 20 aimed to provide coronary angiography to all patients who underwent index testing. However, only some participants who underwent index testing proceeded to the reference test in five studies (Bates 1996; Brennan 1997; Cai 2010; Krawczynska 1988; Reis 1995).
2.
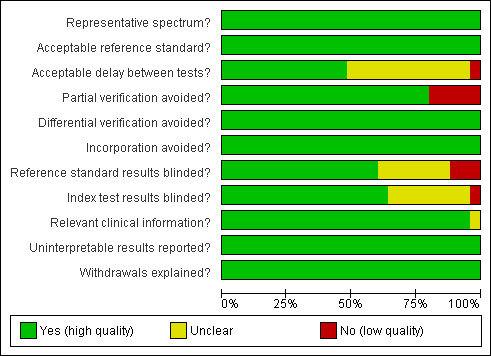
Methodological design and reporting quality of studies included in meta‐analysis according to risk of bias in quality domains assessed using the Quality Assessment of Diagnostic Accuracy Studies tool: review authors' judgements about each methodological quality item presented as percentages across all included studies
3.
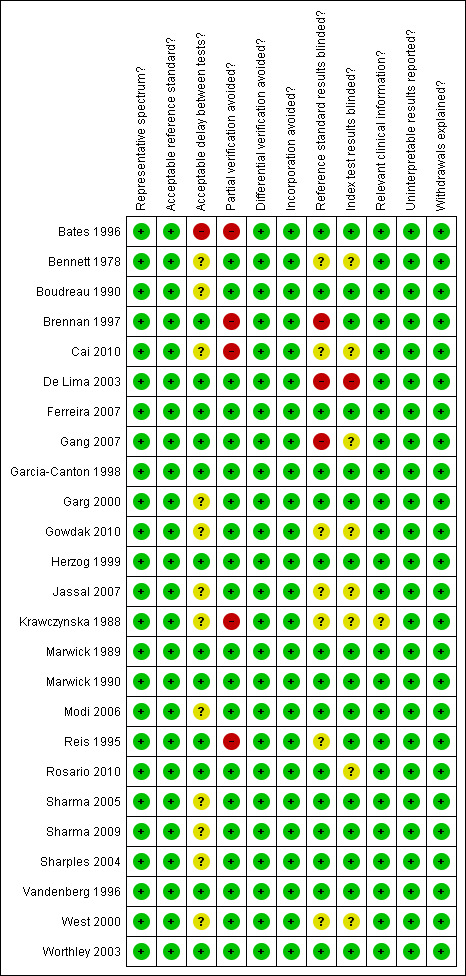
Methodological quality summary of studies: review authors' judgements about each methodological quality item for each included study using the Quality Assessment of Diagnostic Accuracy Studies tool
Findings
We identified 13 studies (745 participants) that evaluated DSE; nine studies (582 participants) of MPS; two exercise EST studies (129 participants), and one study investigated each of EBCT (97 participants), DSF (86 participants), exercise ventriculography (35 participants) and CIMT (105 participants). Two studies (265 participants) investigated the relationship between resting wall motion abnormality on resting transthoracic echocardiography and significant CAD. One study (125 participants) also investigated the relationship between mitral annulus calcification on echocardiography and CAD. Another study (52 participants) investigated the relationship between abnormal echocardiography (left ventricular dysfunction or cardiomegaly) and CAD. Three studies (263 participants) investigated the relationship between abnormal resting ECG and CAD. No studies of diagnostic test accuracy were identified for CT coronary angiography, cardiopulmonary exercise testing, magnetic resonance angiography, or cardiac magnetic resonance imaging.
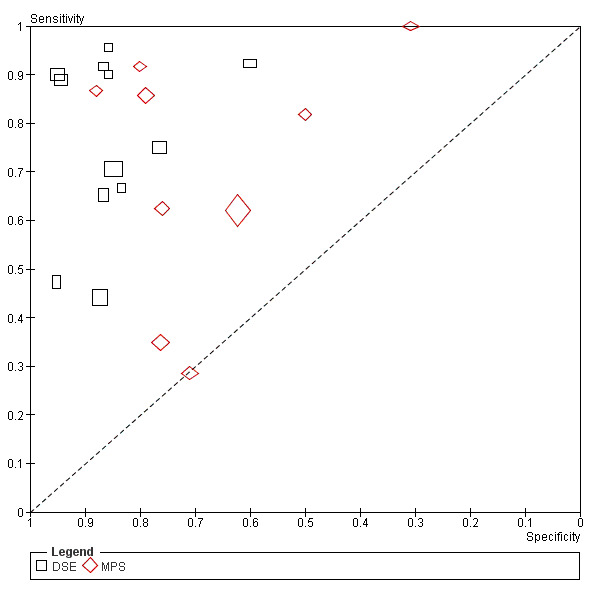
A forest plot of the study estimates of sensitivity and specificity for each test is shown in Figure 4. Figure 5 depicts the SROC plot of sensitivity and specificity, arranged by test comparison, for all studies (with one exception) identified and included in the meta‐analysis. Jassal 2007 was not included because sensitivity could not be calculated due to a lack of patients with CAD.
4.
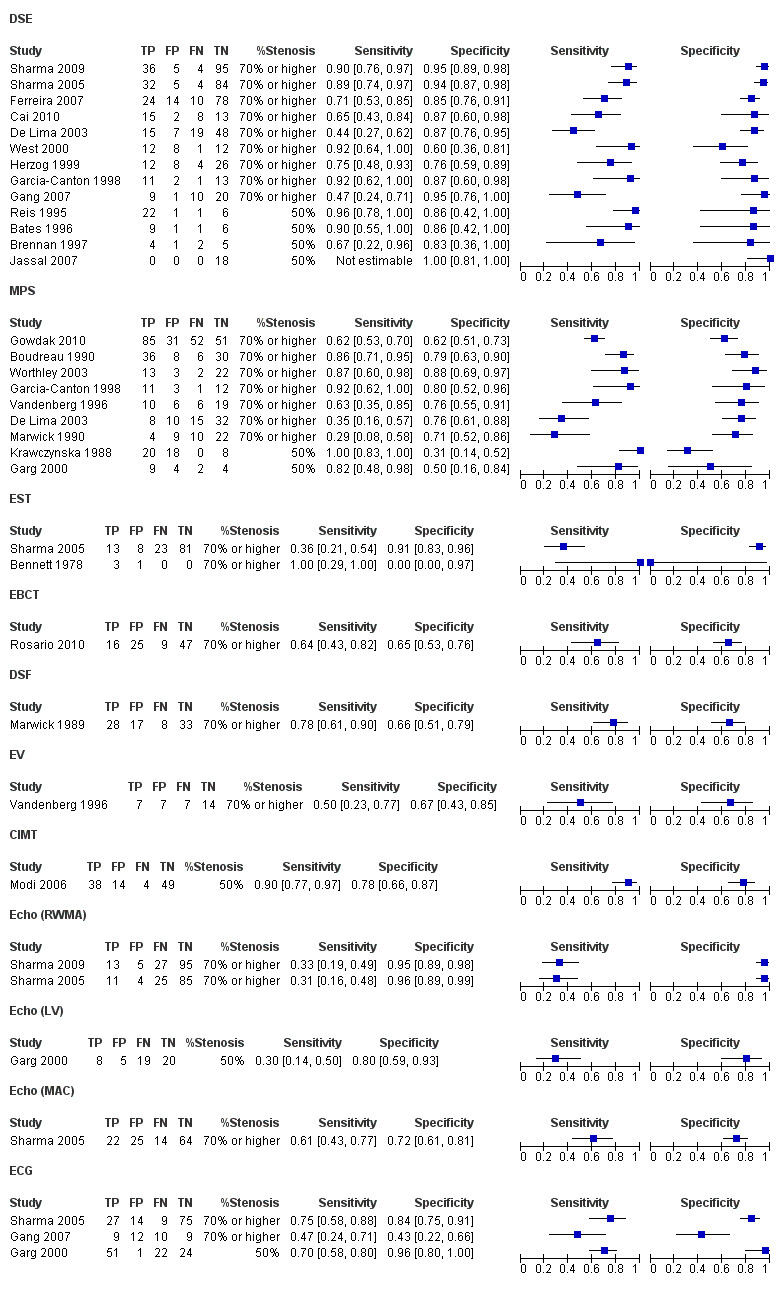
Accuracy of tests for coronary artery disease versus coronary angiography (forest plot); CIMT: carotid intimal medial thickness; DSE: dobutamine stress echocardiography; DSF: digital subtraction fluorography; EBCT: electron beam computed tomography; ECG: resting electrocardiography; Echo (LV): echocardiography (left ventricular dysfunction or cardiomegaly; Echo (MAC): echocardiography (mitral annular calcification); Echo (RWMA): echocardiography (resting wall motion abnormality); EST: exercise stress electrocardiography; EV: exercise ventriculography; FN: false negative; FP: false positive; MPS: myocardial perfusion scintigraphy; NS: not stated; TN: total negative; TP: total positive
5.
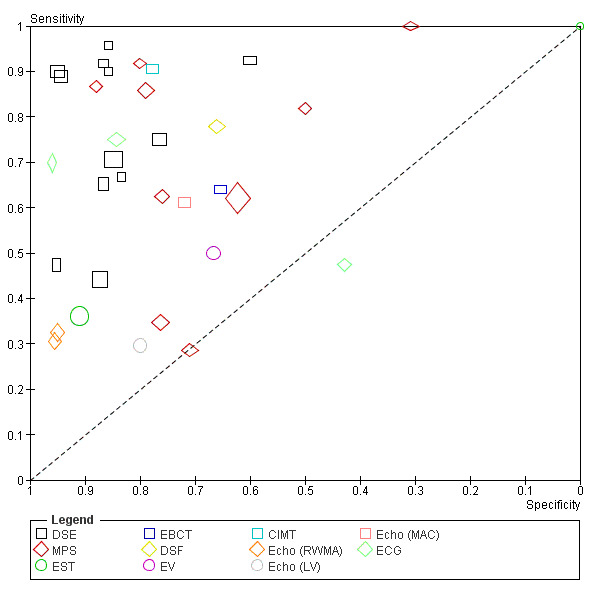
Summary receiver operator curve plot of sensitivity versus specificity for performance of different tests versus coronary angiography. Each symbol represents a study, with the height and width of each symbol being proportional to the inverse standard error of the sensitivity and specificity respectively
CIMT: carotid intimal medial thickness; DSE: dobutamine stress echocardiography; DSF: digital subtraction fluorography; EBCT: electron beam computed tomography; ECG: resting electrocardiography; Echo (LV): echocardiography (left ventricular dysfunction or cardiomegaly); Echo (MAC): echocardiography (mitral annular calcification); Echo (RWMA): echocardiography (resting wall motion abnormality); EST: exercise stress electrocardiography; EV: exercise ventriculography; MPS: myocardial perfusion scintigraphy
Dobutamine stress echocardiography (DSE)
DSE was compared with coronary angiography in 13 studies (745 participants) (Bates 1996; Brennan 1997; Cai 2010; De Lima 2003; Ferreira 2007; Gang 2007; Garcia‐Canton 1998; Herzog 1999; Jassal 2007; Reis 1995; Sharma 2005; Sharma 2009; West 2000). Using induced wall motion abnormalities during dobutamine stress as a positive result indicating CAD, the sensitivity of DSE varied from 44% to 96% and the specificity from 60% to 100%. Overall, DSE had a DOR of 29.98 (95% CI 12.17 to 73.89) and area under the curve (AUC) of 0.91 (95% CI 0.85 to 0.95). The pooled sensitivity was 0.79 (95% CI 0.67 to 0.88), specificity 0.89 (95% CI 0.81 to 0.94). One study also investigated the relationship between peak systolic velocity during DSE for CAD (Sharma 2009). This study reported that ≥ 50% elevation in peak systolic velocity with exercise during DSE was associated with ≥ 70% stenosis on coronary angiography (sensitivity 86%, specificity 88%).
Not all patients who underwent index testing proceeded to have these test results verified by the reference standard. Partial verification was made in three studies (Bates 1996; Brennan 1997; Cai 2010). Furthermore, four studies (Bates 1996; Brennan 1997; Jassal 2007; Reis 1995) used a reference test diagnostic threshold of ≥ 50% stenosis. In the nine studies that used the higher threshold of ≥ 70% stenosis, the pooled sensitivity was 0.76 (95% CI 0.60 to 0.87) and specificity 0.88 (95% CI 0.78 to 0.94) with pooled DOR 23.01 (95% CI 8.08 to 65.51) and AUC 0.90. When only studies that applied a reference standard threshold of ≥ 70% stenosis and avoided partial verification were included, the pooled sensitivity was 0.78 (95% CI 0.59 to 0.89), specificity 0.88 (95% CI 0.76 to 0.94), positive likelihood ratio 6.44 (95% CI 3.03 to 13.70) and negative likelihood ratio 0.26 (95% CI 0.13 to 0.50) with pooled DOR 25.22 (95% CI 7.68 to 82.80) and AUC 0.90.
Overall, there was very strong evidence of heterogeneity among the 13 studies (Figure 6). This remained highly statistically significant even after accounting for differences in reference standard threshold (Figure 7) and partial verification (Figure 8). The remaining studies were similar in the performance of index test and interpretation of test results, but two studies (Sharma 2005; Sharma 2009) were responsible for most of the heterogeneity. There was no statistical evidence of heterogeneity in six studies (De Lima 2003; Ferreira 2007; Gang 2007; Garcia‐Canton 1998; Herzog 1999; West 2000). Sharma 2005 and Sharma 2009 differed from other studies in that they originated from a single research group and had the highest proportion of patients who were symptomatic for chest pain. Despite the hypothesis that prevalence of CAD may have accounted for heterogeneity, we could not investigate any relationship between diagnostic accuracy and prevalence of CAD more formally because of the small number of studies, lack of subgrouped patient data, and five studies (Bates 1996; Cai 2010; Garcia‐Canton 1998; Jassal 2007; West 2000) did not report proportions of symptomatic patients. Two studies (Bates 1996; Gang 2007) enrolled only patients with DM, and sensitivity was found to range from 47% to 90% and specificity from 86% to 95%.
6.
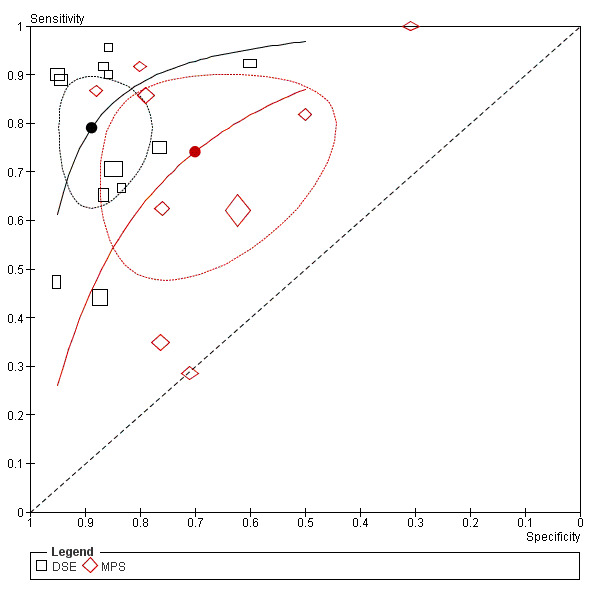
Summary receiver operator curve plot of sensitivity versus specificity for performance of different tests versus coronary angiography: Indirect comparison MPS versus DSE. Each symbol represents a study, with the height and width of each symbol being proportional to the inverse standard error of the sensitivity and specificity respectively. The curves represent the summary receiver operator characteristic curves for MPS and DSE. The circles represent the summary estimate of test performance and the zone outline surrounding it represents the 95% confidence region of this summary estimate
DSE: dobutamine stress echocardiography; MPS: myocardial perfusion scintigraphy
7.
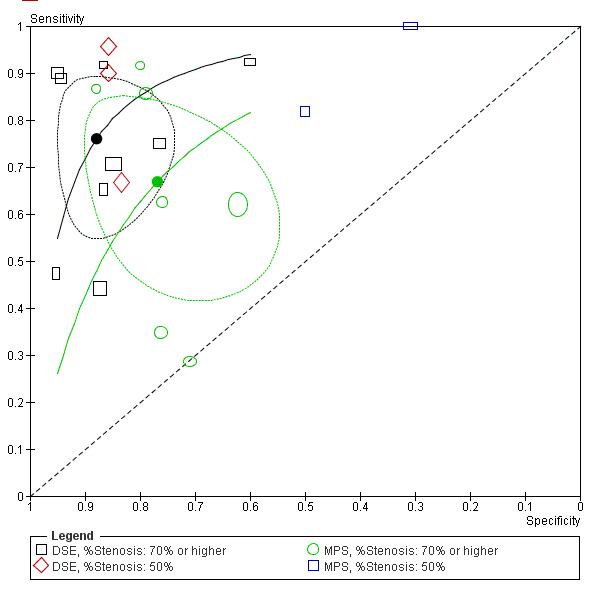
Summary receiver operator curve plot of sensitivity versus specificity for performance of different tests versus coronary angiography: indirect comparison MPS versus DSE, according to reference standard threshold. Each symbol represents a study, with the height and width of each symbol being proportional to the inverse standard error of the sensitivity and specificity respectively. The curves represent the summary receiver operator characteristic curves for MPS and DSE. The circles represent the summary estimate of test performance and the zone outline surrounding it represents the 95% confidence region of this summary estimate
DSE: dobutamine stress echocardiography; MPS: myocardial perfusion scintigraphy
8.
Summary receiver operator curve plot of sensitivity versus specificity for performance of different tests versus coronary angiography: indirect comparison MPS versus DSE, according to presence of partial verification. Each symbol represents a study, with the height and width of each symbol being proportional to the inverse standard error of the sensitivity and specificity respectively. The curves represent the summary receiver operator characteristic curves for MPS and DSE. The circles represent the summary estimate of test performance and the zone outline surrounding it represents the 95% confidence region of this summary estimate
DSE: dobutamine stress echocardiography; MPS: myocardial perfusion scintigraphy.
Myocardial perfusion scintigraphy (MPS)
MPS was compared with coronary angiography in nine studies (582 participants) (Boudreau 1990; De Lima 2003; Garcia‐Canton 1998; Garg 2000; Gowdak 2010; Krawczynska 1988; Marwick 1990; Vandenberg 1996; Worthley 2003). Sensitivity of MPS varied from 29% to 100% and specificity from 31% to 88%. The pooled summary estimates showed that MPS had a DOR 6.69 (95% CI 2.35 to 19.03) and AUC 0.78 (95% CI 0.64 to 0.88). The pooled sensitivity was 0.74 (95% CI 0.54 to 0.87), and specificity 0.70 (95% CI 0.51 to 0.84).
All but one study (Krawczynska 1988) avoided partial verification bias. Two studies (Garg 2000; Krawczynska 1988) used a threshold of ≥ 50% stenosis and not the reference threshold of ≥ 70% stenosis. When these studies were removed from the analysis, DOR remained unchanged at 6.70 (95% CI 1.84 to 24.41) and AUC 0.78. The pooled sensitivity was 0.67 (95% CI 0.48 to 0.82), specificity 0.77 (95% CI 0.61 to 0.88), with positive and negative likelihood ratios of 2.89 (95% CI 1.39 to 5.99) and 0.43 (95% CI 0.23 to 0.80) respectively.
There was very strong evidence of heterogeneity among the nine studies (Figure 6). Heterogeneity remained even after accounting for differences in reference standard threshold (Figure 7) and partial verification (Figure 8). Of the studies that had reference standards of ≥ 70% stenosis and avoided verification bias, four (Boudreau 1990; Garg 2000; Gowdak 2010; Vandenberg 1996) enrolled only patients with DM. Heterogeneity among these four studies of patients with diabetes remained strongly significant, although heterogeneity of the other four studies (De Lima 2003; Garcia‐Canton 1998; Marwick 1990; Worthley 2003) decreased when they were excluded. One study (Worthley 2003) that employed tachycardia pacing in some patients to ensure diagnostic MPS had a much higher sensitivity and specificity compared with the other studies and accounted for much of the remaining heterogeneity.
Meaningful investigation into whether prevalence of angina and/or ischaemic heart disease symptoms on diagnostic test performance was not possible as four studies (Garcia‐Canton 1998; Garg 2000; Gowdak 2010; Krawczynska 1988) did not provide any information regarding prevalence of angina or ischaemic heart disease symptoms in their study populations.
Other tests
Two studies (129 participants) (Bennett 1978; Sharma 2005) compared EST with coronary angiography. In Bennett 1978, only 4/7 participants were able to achieve an adequate heart rate and had a diagnostic exercise stress test; the three remaining participants underwent non‐diagnostic tests due to suboptimal stress capacity. Sensitivity for this study was 1.0 (95% CI 0.29 to 1.0) and specificity 0 (95% CI 0 to 0.97). In Sharma 2005, which enrolled 125 participants, sensitivity was 0.36 (95% CI 0.21 to 0.54) and specificity 0.91 (95% CI 0.83 to 0.96).
One study (97 participants) (Rosario 2010) compared EBCT with coronary angiography. This study reported that when a calcium score threshold of 1330.72 Agatston units was used as a cut‐off point, sensitivity was 0.64 (95% CI 0.43 to 0.82) and specificity 0.65 (95% CI 0.53 to 0.76), using a reference standard threshold of ≥ 70% stenosis to diagnose CAD.
One study (35 participants) (Vandenberg 1996) compared exercise radionuclide ventriculography with coronary angiography showing a sensitivity of 0.50 (95% CI 0.23 to 0.77) and a specificity of 0.67 (95% CI 0.43 to 0.85)
One study (86 participants) (Marwick 1989) compared DSF with coronary angiography, showing a sensitivity of 0.78 (95% CI 0.61 to 0.90) and a specificity of 0.68 (95% CI 0.51 to 0.79).
One study (105 participants) (Modi 2006) compared CIMT with coronary angiography, showing a sensitivity of 0.90 (95% CI 0.77 to 0.97) and a specificity of 0.78 (95% CI 0.66 to 0.87).
Three studies (Garg 2000; Sharma 2005; Sharma 2009) correlated echocardiography findings with CAD. Two studies (Sharma 2005; Sharma 2009) used resting wall motion abnormality to define an abnormal index test. These studies, which were performed by the same authors on similar populations, had very similar sensitivity and specificity (Sharma 2005 reported sensitivity of 0.31 (95% CI 0.16 to 0.48) and specificity of 0.96 (95% CI 0.89 to 0.99); Sharma 2009 found sensitivity of 0.33 (95% CI 0.19 to 0.49) and specificity of 0.95 (95% CI 0.89 to 0.98)). Sharma 2005 also compared mitral annular calcification and CAD and reported that this echocardiographic finding had a sensitivity of 0.61 (95% CI 0.43 to 0.77) and specificity of 0.72 (95% CI 0.61 to 0.81). Garg 2000 used echocardiographic criteria of left ventricular dysfunction or cardiomegaly to define test positivity, and reported sensitivity of 0.30 (95% CI 0.14 to 0.50) and specificity of 0.80 (95% CI 0.59 to 0.93).
Three studies (Gang 2007; Garg 2000; Sharma 2005) investigated resting ECG for CAD diagnosis. In these studies, abnormal resting ECG was defined as the presence of pathological Q waves, left ventricular hypertrophy, ST depression ≥ 1 mm, ST elevation ≥ 1 mm, T wave inversion or bundle branch block. However, results differed. Gang 2007 reported sensitivity of 0.47 (95% CI 0.24 to 0.71) and specificity of 0.43 (95% CI 0.22 to 0.66); Garg 2000 identified sensitivity of 0.70 (95% CI 0.58 to 0.80) and specificity of 0.96 (95% CI 0.80 to 1.00), and Sharma 2005 reported sensitivity of 0.75 (95% CI 0.58 to 0.88) and specificity of 0.84 (95% CI 0.75 to 0.91).
Comparative analysis: DSE versus MPS
Garcia‐Canton 1998 and De Lima 2003 directly compared DSE and MPS (Figure 9). Both studies reported that DSE had a higher specificity and equivalent or better sensitivity compared with MPS. Each applied reference standard thresholds of ≥ 70% stenosis for diagnosing CAD, and avoided partial verification bias.
9.
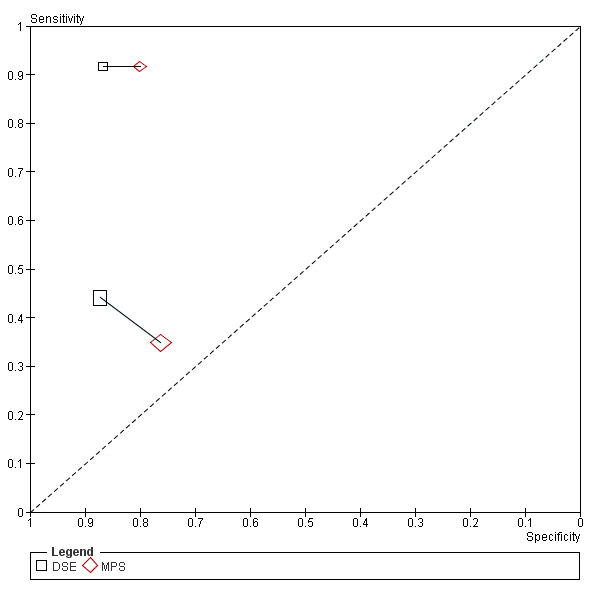
Summary receiver operator curve plot of sensitivity versus specificity for performance of different tests versus coronary angiography: Direct comparison MPS versus DSE. Each symbol represents a study, with the height and width of each symbol being proportional to the inverse standard error of the sensitivity and specificity respectively. The lines connecting paired MPS and DSE studies denote studies which investigated the accuracy of MPS and DSE in the same study population (direct comparison)
DSE: dobutamine stress echocardiography; MPS: myocardial perfusion scintigraphy
Table 4 and Figure 6 summarise indirect comparison results.
3. Comparison of summary estimates of test performance for dobutamine stress echocardiography (DSE) and myocardial perfusion scintigraphy (MPS).
| Test | Studies (N) | Sensitivity (95% CI) | Specificity (95% CI) | Diagnostic odds ratio (95% CI) | AUC | P value for difference in accuracy* |
| Overall results: including all studies | ||||||
| MPS | 9 | 0.74 (0.54 to 0.87) |
0.70 (0.51 to 0.84) |
6.69 (2.35 to 19.03) |
0.78 | 0.02 |
| DSE | 13 | 0.79 (0.67 to 0.88) |
0.89 (0.81 to 0.94) |
29.98 (12.17 to 73.89) |
0.91 | |
| Only including studies where reference standard threshold ≥ 70% coronary artery stenosis on coronary angiography | ||||||
| MPS | 7 | 0.67 (0.48 to 0.82) |
0.77 (0.61 to 0.88) |
6.70 (1.84 to 24.41) |
0.78 | 0.09 |
| DSE | 9 | 0.76 (0.60 to 0.87) |
0.88 (0.78 to 0.94) |
23.01 (8.08 to 65.51) |
0.90 | |
| Only including studies where partial verification was avoided | ||||||
| MPS | 8 | 0.68 (0.51 to 0.81) |
0.75 (0.60 to 0.86) |
6.45 (2.12 to 19.64) |
0.78 | 0.03 |
| DSE | 9 | 0.80 (0.64 to 0.90) |
0.89 (0.79 to 0.95) |
34.28 (11.10 to 105.93) |
0.92 | |
| Only including studies which avoided partial verification and had reference standard threshold ≥ 70% coronary artery stenosis on coronary angiography | ||||||
| MPS | 7 | 0.67 (0.48 to 0.82) |
0.77 (0.61 to 0.88) |
6.70 (1.84 to 24.41) |
0.78 | 0.09 |
| DSE | 8 | 0.78 (0.59 to 0.89) |
0.88 (0.76 to 0.94) |
25.22 (7.68 to 82.80) |
0.90 | |
AUC: area under the curve; CI: confidence interval; DSE: dobutamine stress echocardiography; MPS: myocardial perfusion scintigraphy
* P values for this variable were calculated using the likelihood ratio test in SAS (PROC NLMIXED), and represented the final P value obtained from a backward elimination approach used to eliminate non‐significant terms from the original hierarchical model.
Overall, there was evidence that DSE (13 studies) had better test accuracy than MPS (9 studies) (P = 0.02). Using the results from the earlier analysis, DSE appeared to have a higher pooled sensitivity (DSE: 0.79 (95% CI 0.67 to 0.88) versus MPS: 0.74 (95% CI 0.54 to 0.87) and specificity DSE: 0.89 (95% CI 0.81 to 0.94) versus MPS: 0.70 (95% CI 0.51 to 0.84). The variability in accuracy was smaller for DSE than MPS, demonstrated by the difference in size of the 95% confidence regions in HSROC space. When we included only studies that used definitions of ≥ 70% stenosis on coronary angiography to diagnose severe CAD, DSE (9 studies) had pooled sensitivity and specificity of 0.76 (95% CI 0.60 to 0.87) and 0.88 (95% CI 0.78 to 0.94) respectively. MPS (7 studies) had pooled sensitivity and specificity of 0.67 (95% CI 0.48 to 0.82) and 0.77 (95% CI 0.61 to 0.88) respectively. There was no statistically significant difference between tests (P = 0.09) (Figure 7). When we included only studies where partial verification bias was avoided, DSE (10 studies) had pooled sensitivity and specificity of 0.80 (95% CI 0.64 to 0.90) and 0.89 (95% CI 0.79 to 0.95) respectively. MPS (8 studies) had pooled sensitivity and specificity of 0.68 (95% CI 0.51 to 0.81) and 0.75 (95% CI 0.60 to 0.86) respectively. The difference in accuracy between MPS and DSE tests for these studies was statistically significant (P = 0.03) (Figure 8). When only studies that avoided partial verification and had reference thresholds ≥ 70% stenosis on coronary angiography were included in the analysis, there was no evidence of a statistically significant difference between tests (P = 0.09). DSE (8 studies) appeared to have a higher pooled sensitivity: 0.78 (95% CI 0.59 to 0.89) than MPS 0.67 (95% CI 0.48 to 0.82) and DSE specificity: 0.88 (95% CI 0.76 to 0.94) versus 0.77 (95% CI 0.61 to 0.88)] compared with MPS (7 studies), as well as a higher corresponding AUC.
Subgroup analyses
Sparse data, both in terms of numbers of studies and study participants, meant that we were unable to perform meaningful subgroup analyses on the effect of DM or prevalence of angina and symptomatic ischaemic heart disease (IHD) on diagnostic test performance. Only one study (Vandenberg 1996) included a patient population who had no history of angina or IHD. Therefore, a sensitivity analysis of diagnostic accuracy in studies that enrolled only patients who had no symptoms of cardiac disease or history of IHD could not be conducted.
Discussion
Summary of main results
Preliminary findings of comparisons of DSE and MPS versus coronary angiography have been published by our review team (Wang 2011), but this systematic review represents more index tests and several studies that were since identified. Of the many screening tests available, most studies investigated the accuracy of DSE and MPS. Two systematic reviews were conducted that compared DSE and MPS in the general population. These reviews reported that MPS was more sensitive in detecting CAD, but exercise stress echocardiography had higher specificity (Fleischmann 1998; Schinkel 2003). Findings from our review indicate that DSE and MPS have moderate levels of sensitivity and specificity to detect severe coronary artery stenosis.
Our key findings are presented in Table 1. On direct analysis, DSE had a higher point estimate of sensitivity and specificity compared with MPS. This was statistically significant for both the overall indirect comparison analysis (P = 0.02) and the sensitivity analysis which included only studies that avoided partial verification (P = 0.03). There was no statistical evidence that DSE had higher diagnostic accuracy in the sensitivity analysis which included only studies that avoided partial verification and had reference standard thresholds ≥ 70% stenosis (P = 0.09). However, because results from studies that applied this common threshold were similar to the overall analysis, the lack of statistical significance may have resulted from a reduction of power due to the smaller number of included studies. Although there were few direct comparisons, in two studies that compared DSE and MPS in the same population, DSE had a higher specificity and equivalent or better sensitivity than MPS.
That DSE had a higher specificity than MPS is consistent with the principle that reversible systolic dysfunction (detected by DSE) usually occurs after reversible perfusion abnormalities (detected by MPS). In the general population, MPS should have higher sensitivity but lower specificity than stress echocardiography because systolic dysfunction often occurs only when severe CAD is present. Patients with ESKD often have hypertension, left ventricular hypertrophy and decreased coronary flow reserve, all of which could account for reduced specificity of MPS in kidney transplant candidates (Houghton 1990).
Causes of false negative results in MPS in the general population include balanced triple vessel disease and submaximal heart rate during stress. Although the reason for lower sensitivity in kidney transplant candidates compared with the general population remains unclear, differences in the effect of the stress agent drug among patients with CKD and the general population offers a possible physiological reason for the difference in sensitivity. Dipyridamole, the drug routinely used in MPS, causes vasodilation of coronary blood vessels by promoting accumulation of adenosine, an endogenous vasodilator. Dipyridamole infusion leads to vasodilation of normal coronary arteries, which is interpreted as an appropriate normal increase in cardiac perfusion. The decreased perfusion resulting from reduced vasodilator response of diseased vessels is interpreted as reversible ischaemia. A corresponding rise in heart rate also generally occurs during dipyridamole infusion and is thought to be secondary to vasodilatation, mediated in part by the cardiac nerves. Heart transplant recipients have been shown to have limited vasodilator response to dipyridamole, which has been attributed to increased resting myocardial blood flow in the transplanted heart resulting from increased cardiac workload and cardiac de‐innervation (Rechavia 1992). Similarly, patients with CKD (particularly those who have diabetes) may also experience a degree of functional de‐innervation as part of an autonomic neuropathy, which would potentially reduce the relative efficacy of dipyridamole. CKD is also invariably associated with arterial calcification and reduced coronary artery flow reserve (Niizuma 2008; Sezer 2007). This may also potentially lead to a decrease in responsiveness to the vasodilating properties of dipyridamole. On the other hand, dobutamine which is commonly used in stress echocardiography, has direct inotropic effects on the cardiac myocyte and potentially may be less affected by the mechanism described.
There was also more variability in the spread of the MPS test results in SROC space compared with DSE. This is probably because MPS is a more subjective test. Several studies of MPS demonstrated considerable inter‐ and intra‐patient result variability, which may limit its diagnostic utility (Akesson 2004; Burkhoff 2001). Variability was also observed in the DSE results, which may be due to unevenness in local expertise to interpret test results across different studies.
Significant heterogeneity was present, which could not be explained by differences in reference threshold and partial verification. Clearly, other factors may have contributed to the clinical heterogeneity in the results. These include differences in study population characteristics (such as prevalence of chest pain, prevalence of diabetes) and test application (diagnostic test threshold, criteria for positive test, choice of stress agent and stress protocol, and operator variability). Limited data from the small numbers of studies and participants meant that we were unable to perform subgroup analyses of the effect of DM and prevalence of angina and IHD on diagnostic performance. Other differences across studies may also have played a role. One possible factor was sex of the participants. One study (Gowdak 2010) showed that among patients with diabetes, MPS test performance was influenced by the sex of participants; sensitivity was lower in women (females 56%; males 65%). Accuracy data based on sex was not reported in any of the included studies. Hence, we were unable to determine if the sex of the participant influenced diagnostic accuracy.
Generally, methodological quality was poorly reported. Methodological quality scoring was based on published reports and additional data provided from correspondence with study authors. Unclear reporting of certain methodological issues may not necessarily indicate poor study design; restrictions imposed by journal word limits, or editing, may have precluded reporting all QUADAS items. Several methodological quality items were reported less frequently than others. These included blinding of reference tests (7/25 not reported), blinding of index tests (8/25 not reported), and acceptable delay between tests (12/25 not reported). In addition to the studies where blinding of reference and index tests was uncertain, 3/25 studies reported no blinding of the reference standard; one study reported no blinding of the index test. Therefore, lack of blinding may have affected our results; the overall effect of unblinded reporting of reference and index tests is generally leads to overestimation of diagnostic accuracy (Leeflang 2006).
We did not find any studies that investigated cardiopulmonary exercise testing, CT coronary angiography, magnetic resonance angiography or cardiac magnetic resonance imaging. Fewer than five studies were found for each of EBCT, ECG, conventional echocardiography, exercise ventriculography, DSF and CIMT. This precluded any further meaningful comparisons other than that between DSE and MPS. DSF and exercise ventriculography are seldom used for CAD screening. Nevertheless, results from studies identified for this review (DSF: sensitivity 78%, specificity 66%; exercise ventriculography: sensitivity 50%, specificity 67%) suggest that neither DSF nor exercise ventriculography were likely to be superior to DSE or MPS. EST appeared to have offer high specificity (91%) but poor sensitivity (36%) in the one study that included a sufficient number of participants (Sharma 2005). Resting wall motion abnormality detected on traditional resting transthoracic echocardiography was also found to offer high specificity (95% to 96%) but low sensitivity (31% to 33%). Mitral annular calcification on echocardiography was studied in the same population (Sharma 2005) and this had higher sensitivity (61%) at the expense of lower specificity (72%). The marked variability in sensitivity and specificity of resting ECG confirms that it has no role in triaging patients for CAD. Notwithstanding the limitations posed by few numbers of studies and participants presented, EBCT and calcium scoring methods also appeared to have limited utility in evaluating the cardiac health of potential kidney transplant recipients. This is reflected in the fact that the optimal test performance of EBCT in the only study identified (Rosario 2010) was a calcium score of 1330.72, which is higher than the usual threshold used in the general population. There is also a theoretical disadvantage of calcium scoring methods in potential kidney transplant recipients due to the increased prevalence of arterial calcification in patients with CKD, arising from metabolic bone disease. Although published studies were not identified in this review, other tests that might be expected to have limited application in the pre‐transplant setting for patients with CKD include CT coronary angiography (exposure to nephrotoxic IV contrast that could adversely affect any residual kidney function) and magnetic resonance imaging (MRI) or angiography (risk of gadolinium induced nephrogenic systemic fibrosis).
Strengths and weaknesses of the review
A strength of this review was the sensitive electronic search strategy developed that identified both published and unpublished studies. Our search strategy excluded search filters for diagnostic terms because they have limited utility (Leeflang 2006; Ritchie 2007). Other strengths included our analytic approach of combining results from studies with similar methodological characteristics and applying the HSROC model to conduct our analysis. The hierarchical modelling strategy accounted for sampling variability in estimates of sensitivity and specificity (and their correlations) in each study when estimating the random effects. This resulted in accuracy estimates that provided better assessments of underlying common log odds ratios (Macaskill 2003). To ensure that findings were generalisable, we included only studies that investigated only potential kidney transplant recipients. We excluded studies that enrolled participants with ESKD because it could be reasonably anticipated that inclusion of unselected dialysis patients would modify expected differences in underlying prevalence of CAD, and the presence and severity of other comorbidities, as well as differences in clinical rationales for testing. By concentrating on potential transplant candidates our findings may not be generalisable to dialysis or CKD patients who would not benefit from transplantation. Our vigilance in contacting authors to obtain data missing or not reported in studies was rewarded by a satisfying number of responses.
Significant heterogeneity was present among studies that investigated the same screening test. Given that underlying prevalence of disease in a population has potential to alter diagnostic performance (Leeflang 2009), knowledge of the effect of clinical characteristics such as angina or diabetes on diagnostic performance would enable better informed decisions about screening and interpretation of results. Although differences in study population characteristics, such as prevalence of chest pain, and test application (diagnostic test threshold, criteria for positive test, choice of stress agent and stress protocol, and operator variability) were likely to have contributed to heterogeneity, we were hindered in estimating their contributions because of data paucity, which resulted in low power. Consequently, we were unable to derive summary measures of diagnostic performance for specific patient subgroups. Data that were directly comparative were limited and also resulted in low power to detect important differences in accuracy among tests. Incomplete reporting of baseline characteristics and study design features that are necessary for scoring methodological quality was a further limitation that was resolved by contacting study authors to obtain additional data.
Applicability of findings to the review question
Current guidelines for preoperative cardiac evaluation of transplant candidates are unclear about the optimal method of assessment for potential kidney transplant recipients. Patients are often referred for coronary angiography as a result of a positive non‐invasive screening test or deemed to be at high risk of CAD. Non‐invasive functional tests, such as DSE or MPS, have been used in the general population as a method of triaging patients for coronary angiography. Results from our review provide a base to inform clinical decision making that were derived from studies conducted in relevant populations. Table 5 summarises test performance for transplant candidates relative to the general population.
4. Comparison of systematic reviews studying the test performance of myocardial perfusion scintigraphy and dobutamine stress echocardiography.
| Review | Population | DSE | MPS | ||
| Sensitivity (95% CI) | Specificity (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | ||
| Cochrane review | Kidney transplant candidates only | 0.79 (0.67 to 0.88) | 0.89 (0.81 to 0.94) | 0.74 (0.54 to 0.87) | 0.70 (0.51 to 0.84) |
| Fleischmann 1998 | General population | 0.85 (0.83 to 0.87) | 0.77 (0.74 to 0.80) | 0.87 (0.86 to 0.88) | 0.64 (0.60 to 0.68) |
| Schinkel 2003 | General population | 0.80 (NS) | 0.86 (NS) | 0.84 (NS) | 0.77 (NS) |
DSE: dobutamine stress echocardiography; MPS; myocardial perfusion scintigraphy; NS ‐ not stated
Figure 10 illustrates the applicability of our findings to clinical practice. Patients in the general population who present with stable chest pain for assessment are typically assigned pre‐test probabilities of significant CAD of 10% to 29% (low risk), 30% to 59% (intermediate risk) or 60% to 90% (high risk) determined using risk tables (NICE Clinical Guideline 1995). Given the wide heterogeneity in the estimates for both DSE and MPS, there is considerable uncertainty in the true post‐test probabilities of each test. However, using the summary estimates in this review, both DSE and MPS may prove useful in ruling out CAD in patients considered to be at low risk for the condition. Patients with positive stress test results warrant additional investigation with coronary angiography. However, the true discriminating value of both tests (especially DSE) is in detecting CAD in intermediate risk patients ‐ a category that includes many potential kidney transplant recipients. Both tests help to classify patients at intermediate risk into either high or low risk categories. When DSE was used, patients at intermediate risk of CAD who tested positive had post‐test probability of 73% to 90% (high risk) and those who tested negative were downgraded to low risk (10% to 27%). Both tests, but especially DSE, have roles as triage tests for intermediate risk transplant candidates; negative results can reduce the need for further evaluation with coronary angiography. In high risk patients, a positive non‐invasive DSE or MPS test result confirms the high risk of severe CAD, but a negative result does not conclusively rule out severe CAD. These patients can be managed by being referred for coronary angiography, thus avoiding functional tests. Nevertheless, functional testing may provide additional prognostic information, or help to prioritise patients waiting to be referred for coronary angiography in resource‐limited areas.
10.

†Based on the positive and negative likelihood ratios calculated from the systematic review in studies which avoided partial verification and used a reference standard threshold of ≥70% stenosis. DSE had a positive likelihood ratio of 6.44 (95% CI 3.03 to 13.70) and negative likelihood ratio of 0.26 (95% CI 0.13 to 0.50). MPS had a positive likelihood ratio of 2.89 (95% CI 1.39 to 5.99) and negative likelihood ratio of 0.43 (95% CI 0.23 to 0.80).
DSE and MPS are not perfect triage tests and a significant number of patients will either have their significant CAD missed (false negatives) or be referred unnecessarily for coronary angiography (false positives). Furthermore, the imprecision of the likelihood ratios resulting from significant between‐study heterogeneity produces significant uncertainty in the post‐test probabilities for both positive and negative tests. A negative DSE test would still, in a low risk population, yield a post‐test probability of 10% to 27%. However, both the desire to avoid complications arising from routine referral of such patients to an invasive gold standard investigations, and the lack of a more accurate alternative method of screening may or may not convince clinicians to consider such posterior test probabilities to be sufficiently low to excuse an asymptomatic individual from having further invasive investigation.
Our results need to be considered together with the real world limitations of practising medicine. Despite the apparent superiority of DSE over MPS to detect severe CAD, the interaction of many clinical factors often result in different transplant centres preferring one screening test over another. These factors may be institutional, arising from practicalities such as availability and or expertise of one screening modality, but not both, in a transplant centre; or patient‐related issues such as lack of cardiorespiratory fitness or mobility for exercise stress testing. DSE requires IV infusion and is not available in all cardiology departments. Many cardiology practices offer exercise stress echocardiography, but we were unable to identify any studies of exercise stress echocardiography in potential kidney transplant recipients. The diagnostic accuracy of exercise stress echocardiography is likely to be similar to DSE, although there is a higher chance of submaximal, and therefore uninterpretable, stress test results in patients who undergo this test. The patient factors that affect physician choice of screening test are less likely to be an issue in a population of potential kidney transplant recipients compared with people who are not transplantation candidates, given that transplantation candidates represent a selected healthier subpopulation of those with CKD. MPS requires the presence of a nuclear medicine department. Although these departments are found in tertiary referral hospitals, they may not be present in smaller hospitals or resource‐poor settings.
For this review, we defined coronary artery stenosis as ≥ 50% stenosis, and severe coronary artery stenosis as ≥ 70% stenosis. Although asymptomatic patients with certain high risk coronary lesions (e.g. left main or equivalent disease, and triple vessel CAD, particularly with left ventricular dysfunction) benefit from revascularisation regardless of symptoms (Eagle 2004), the benefit of preoperative revascularisation before transplant surgery remains questionable. Two RCTs (CARP (McFalls 2004) and DECREASE‐V (Poldermans 2007)) did not demonstrate any revascularisation benefit in asymptomatic CAD before major vascular surgery. Nevertheless, the diagnosis of angiographically‐proven significant CAD in kidney transplant candidates imposes further implications on patient management. These include consideration of need for perioperative beta blockade, antiplatelet agents and anticoagulation. A recent registry study (De Lima 2010) confirmed that in patients with CKD and significant CAD, medical therapy results in adequate long‐term event‐free survival. However, in this study, a greater cardiac event rate occurred in patients who fulfilled criteria for revascularisation but declined intervention. Nevertheless, the lack of RCTs specifically addressing this question in kidney transplant settings means that uncertainty remains about if failure to perform coronary intervention when necessary results in an accentuated increased risk of adverse events and death.
Authors' conclusions
Implications for practice.
Of the non‐invasive screening tests available to detect CAD in potential kidney transplant candidates, MPS and DSE have been studied in detail. Both tests, especially DSE, have roles as triage tests for transplant candidates with intermediate of CAD. Negative DSE results preclude need for further evaluation using coronary angiography, avoiding unnecessary risk to patients and potentially reducing healthcare costs. Given the wide heterogeneity in the estimates for both DSE and MPS, considerable uncertainty remains concerning the true post‐test probabilities of each test. Current evidence suggests that where feasible DSE should be used as the screening investigation of choice.
Implications for research.
The ability to identify patients at high risk of CAD may not necessarily enable clinicians to predict cardiac event‐free survival following transplantation. In the postoperative period, other factors such as inflammation, sympathetic nervous system activation, hypercoagulability and hypoxia contribute to increased cardiac morbidity and mortality (Yao 2004). Patients with kidney disease have abnormal coronary microcirculation and reduced coronary flow reserve, which may result in cardiac ischaemic events, even in the absence of macrovascular stenoses (Caliskan 2008; Niizuma 2008; Sezer 2007). Future research examining the ability of functional tests to predict postoperative outcome is urgently needed.
Notes
An earlier version of this review was published in the American Journal of Kidney Diseases (Wang 2011).
Acknowledgements
The authors would especially like to thank Petra Macaskill for her assistance in designing the statistical methodology for this review and providing invaluable statistical support. We also thank Professors Les Irwig and Stephen Chadban for their kind comments and assistance in reviewing an earlier version of this review; Narelle Willis, Managing Editor of the Cochrane Renal Group, and Leslee Edwards, the Administrative Officer of the Cochrane Renal Group, for their assistance in managing the editorial aspects of this review.
We would also like to thank the many study authors who provided additional information regarding their research, especially: Daniel Brennan, Maria Dolores Checa, José Jayme Galvão de Lima, An de Vriese, Cesar Garcia‐Canton, Sishir Gang, Thomas Marwick, Gert Mayer, Gilmar Reis, Sylvia Rosas, Alice Schmidt, Jamshid Shirani, Nakul Sinha and Matthew Worthley.
This research was supported, in part, by the Jacquot Research Establishment Award administered by The Royal Australasian College of Physicians and the Australian and New Zealand Society of Nephrology. Dr Andrew Hayen has also received financial support from the Australian National Health and Medical Research Council Program (Grant Number 402764).
Appendices
Appendix 1. Electronic search strategies
| Database | Search terms |
| MEDLINE |
|
| EMBASE |
|
Appendix 2. QUADAS methodological items and operational definitions
| Methodological variable | Operational definition/information required from each study |
| 1. Representative spectrum (spectrum bias) | When included patients did not represent the intended targeted population, this may have led to an under‐ or overestimation of diagnostic accuracy depending on the difference between the targeted and included populations. The target spectrum in our review was patients with renal failure who were candidates for kidney transplantation. This was scored 'yes' if study participants included only patients with kidney disease who were considered to be candidates for kidney transplantation |
| 2. Acceptable reference standard | An imperfect reference standard may have resulted in misclassification of disease positives and disease negatives. For the purpose of this review, studies had an acceptable reference standard if they used coronary angiography as the reference standard |
| 3. Acceptable delay between tests (disease progression bias) | Disease may have progressed to a more advanced stage (i.e. greater degree of coronary artery stenosis) if a significant time interval between index and reference tests was observed, thereby leading to disease progression bias. This was scored as ‘yes’ if the delay between test was short (i.e. less than three months) |
| 4. Partial verification avoided (verification bias) | Partial verification bias usually leads to an overestimation of sensitivity, although its effect on specificity varies. This item was scored ‘yes’ if all patients who received the index test were also evaluated by the reference standard |
| 5. Differential verification avoided | This was scored ‘yes’ if no patients were verified with a second or third reference standard |
| 6. Incorporation avoided (incorporation bias) | This bias usually leads to an overestimation of diagnostic test accuracy. Incorporation bias was deemed to have existed if the index test was incorporated in a composite reference standard. Studies were scored ‘yes’ if their classification of disease status did not directly involve the results of the index test |
| 7. Reference standard results blinded (information bias) | When the reference standard was interpreted knowing the index test results, this may have led to the overestimation of diagnostic test accuracy. Studies were scored ‘yes’ if blinding of the reference standard was explicitly stated in the article or if this was acknowledged by authors in subsequent personal communication. Otherwise, the studies were marked ‘unclear’, unless blinding was explicitly stated to be absent |
| 8. Index test results blinded (information bias) | When the index test results were interpreted without the knowledge of results of the reference standard, or with more information than in practice, this may have resulted in bias, usually leading to an overestimation of diagnostic accuracy. This item was scored ‘yes’ if blinding of the index test was explicitly stated in the article or if this was acknowledged by authors in subsequent personal communication. Otherwise, the studies were marked ‘unclear’, unless blinding was explicitly stated to be absent |
| 9. Relevant clinical information (information bias) | The availability of clinical data during interpretation of test results may have affected estimates of test performance. This item was scored ‘yes’ if the data available during the study of diagnostic test accuracy was the same as that which would have been available in normal clinical practice |
| 10. Uninterpretable results explained | This item was scored ‘yes’ if uninterpretable results were explained or if there were no uninterpretable results present. This item was scored 'no' if uninterpretable results were found but not explained |
| 11. Withdrawals explained | Excluding patients from the study may have led to an overestimation of diagnostic accuracy. This item was scored ‘yes’ if withdrawals were explained or if there were no withdrawals from the study. This item was scored 'no' if there were withdrawals from the study, but these were unexplained |
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
| Test | No. of studies | No. of participants |
|---|---|---|
| 1 DSE | 13 | 745 |
| 2 MPS | 9 | 582 |
| 3 EST | 2 | 129 |
| 4 EBCT | 1 | 97 |
| 5 DSF | 1 | 86 |
| 6 EV | 1 | 35 |
| 7 CIMT | 1 | 105 |
| 8 Echo (RWMA) | 2 | 265 |
| 9 Echo (LV) | 1 | 52 |
| 10 Echo (MAC) | 1 | 125 |
| 11 ECG | 3 | 263 |
1. Test.

DSE.
2. Test.

MPS.
3. Test.

EST.
4. Test.

EBCT.
5. Test.

DSF.
6. Test.

EV.
7. Test.

CIMT.
8. Test.

Echo (RWMA).
9. Test.

Echo (LV).
10. Test.

Echo (MAC).
11. Test.

ECG.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bates 1996.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Prospective, cohort study | |
| Target condition and reference standard(s) |
CAD on coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | Patients were followed‐up for a mean of 498 ± 425 days (range 2 to 1269) after transplantation. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Adult patients with insulin‐dependent DM being considered for kidney and/or kidney‐pancreas transplantation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | No | 18 patients underwent cardiac catheterisation within 101 ± 263 days (range = 200 days before to 557 days after) of DSE. Interval progression of CAD is possible. |
| Partial verification avoided? All tests | No | 18/53 patients underwent coronary angiography. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | All available catheterisation studies were interpreted by a blinded, experienced angiographer using digital callipers. |
| Index test results blinded? All tests | Yes | All studies were interpreted by an experienced echocardiographer blinded to the clinical and stress electrocardiogram data. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Bennett 1978.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests | EST | |
| Follow‐up | 30‐38 months, unless death occurred earlier. | |
| Notes | Three of the seven patients had a non‐diagnostic stress test due to inadequate rate as a result of fatigue. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with juvenile insulin‐dependent DM and ESKD who presented for kidney transplant cardiac evaluation. |
| Acceptable reference standard? All tests | Yes | Coronary artery stenosis measured by coronary angiography. Absolute degree of stenosis recorded for each patient. |
| Acceptable delay between tests? All tests | Unclear | Unclear, but likely to be only short delay between tests. |
| Partial verification avoided? All tests | Yes | All patients received angiography. |
| Differential verification avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Incorporation avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not reported. |
| Index test results blinded? All tests | Unclear | Not reported. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Boudreau 1990.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Dipyridamole‐Tl‐201 scintigraphy MPS (40 oral, 40 IV dipyridamole)
|
|
| Follow‐up | None. | |
| Notes | Patients were reported as being followed‐up long‐term to assess the risk factors (including the thallium scan) for cardiac events after kidney transplantation, although no published data were available. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with type 1 DM and ESKD who presented for kidney transplant evaluation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be a short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test also received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Coronary angiograms were analysed by a blinded observer (not the person who performed the angiography) who was unaware of the Tl‐201 scan results or the patient’s history. |
| Index test results blinded? All tests | Yes | The scans were interpreted by consensus of three experienced radiologists who were unaware of the angiography results or patient history. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No missing patients. |
Brennan 1997.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | Follow‐up (range 3 to 64 months) data were obtained for all 47 participants. | |
| Notes | Of the 47 patients who underwent DSE, all 5 patients who tested positive received coronary angiography. Seven other patients who had negative DSE received coronary angiography. The decision about providing coronary angiography for those who were index test negative was not made on grounds of clinical or high pre‐test suspicion (author correspondence). | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with ESKD at risk of CAD who presented for kidney transplant cardiac evaluation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Yes | Average time from DSE to coronary angiography < 9 months (author correspondence). |
| Partial verification avoided? All tests | No | Of the 47 patients who underwent DSE, 5 who tested positive underwent coronary angiography, and 7 others who had negative DSE results also underwent coronary angiography. The reason that patients who were index test negative underwent coronary angiography was for other than clinical or high pre‐test suspicion (author correspondence) |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | No | It is probable that the person who performed the coronary angiogram was aware of the DSE result. However, because later coronary angiograms were performed by an outside institution, this was not necessarily the case (author correspondence). |
| Index test results blinded? All tests | Yes | All studies were reviewed independently by two experienced echocardiographers who were blinded to the clinical data. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Cai 2010.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants | Patients at intermediate to high risk of CAD underwent DSE 1 to 12 months (median 5 months) before kidney transplantation
|
|
| Study design | Retrospective cohort study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | Patients were followed up for a mean of 60 months (range 3 to 145 months) after DSE. The time from kidney transplant to follow‐up was 1 to 135 months (median 49 months). | |
| Notes | For the purpose of the analysis, only inducible wall motion abnormalities were counted as positive DSE. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with ESKD and intermediate to high risk of CAD awaiting kidney transplantation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be short delay between tests. |
| Partial verification avoided? All tests | No | 38 patients (23 with and 15 without inducible ischaemia on DSE) underwent coronary angiography after DSE. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not reported. |
| Index test results blinded? All tests | Unclear | Not reported. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
De Lima 2003.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | Five participants were lost to follow‐up. Minimum and mean follow‐up periods were 6 and 26 months, respectively. The outcome measure was cardiac events, predefined as sudden death, MI, life‐threatening arrhythmia, heart failure, pulmonary oedema, unstable angina, and myocardial revascularisation. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Kidney transplantation candidates as part of cardiac evaluation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | Interval between tests was 2 to 6 weeks (author correspondence). |
| Partial verification avoided? All tests | Yes | All participants who underwent an index test also received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | No | No blinding for outcomes assessment. |
| Index test results blinded? All tests | No | No blinding for outcomes assessment. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | The number of tests that were submaximal were reported. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Ferreira 2007.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
Exclusion criteria
|
|
| Study design | Cross sectional study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Dobutamine/atropine stress echocardiography
|
|
| Follow‐up | ||
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with ESKD who were kidney transplant candidates undergoing cardiac evaluation. Examinations performed one day after haemodialysis. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | Not longer than 2 months. |
| Partial verification avoided? All tests | Yes | All participants who underwent an index test also received the reference standard test. |
| Differential verification avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Incorporation avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Reference standard results blinded? All tests | Yes | The measurement bias was controlled through the “blind” interpretation of the test regarding the coronary angiography, which was considered the reference standard. |
| Index test results blinded? All tests | Yes | The recorded images were later interpreted by two members who were blinded to the patients’ clinical data, as independent observers. The discordance was solved by consensus between the two observers. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | Of 148 patients submitted to the test, 135 finished the protocol, which corresponds to a feasibility of 91%. The reasons that led to test interruption were: attaining 85% of maximum CF for age: 121 (81%); limiting side effects: 13 (9%); echocardiographic signs of ischaemia: 10 (7%) and end of the protocol: 4 (3%). |
| Withdrawals explained? All tests | Yes | Thirteen patients presented an early withdrawal of the protocol due to limiting side effects: 12 (8.5%) due to hypertensive response and 1 (0.5%) due to severe angina. |
Gang 2007.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
Resting ECG
|
|
| Follow‐up | None | |
| Notes |
|
|
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with DM and ESKD who presented for kidney transplant cardiac evaluation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | DSE and coronary angiography were performed within the same week (author correspondence). |
| Partial verification avoided? All tests | Yes | All participants who underwent an index test also received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | No | The person who interpreted the coronary angiogram reports was not blinded to DSE results (author correspondence). |
| Index test results blinded? All tests | Unclear | All coronary angiograms were performed after DSE, so index tests were likely to be performed without influence from the reference standard. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals reported. |
Garcia‐Canton 1998.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | None reported. | |
| Notes | Conference presentation. Unpublished as a study. Additional information obtained from correspondence with authors. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients who presented for cardiac evaluation before kidney transplantation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | All coronary angiography was performed from two weeks to three months after the other tests (author correspondence). |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test also had the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Coronary angiography result was reported by a cardiology team member who was unaware of other test results (author correspondence). |
| Index test results blinded? All tests | Yes | MIBI scan and DSE results were interpreted by clinical and technical experts without knowledge of the other. Both were conducted before coronary angiography. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided concerning the performance and analysis of both the index and reference tests (author correspondence). |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable results. |
| Withdrawals explained? All tests | Yes | There were no withdrawals reported. |
Garg 2000.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSTS
Echocardiography
Resting ECG
|
|
| Follow‐up | Survival data are available. | |
| Notes | All patients underwent coronary angiography, echocardiography and resting ECG. 19 patients underwent dipyridamole MPS. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with DM who were candidates for kidney transplant. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent an index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Each angiogram was independently reviewed by two experienced cardiologists who were blinded to the clinical data and uninvolved in patient management. |
| Index test results blinded? All tests | Yes | Studies were interpreted qualitatively and quantitatively. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Gowdak 2010.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
SPECT+ Sestamibi cardiac scintigraphy
|
|
| Follow‐up | Data not available. | |
| Notes | Data obtained from poster presented at the European Society of Cardiology conference in 2010 http://spo.escardio.org/AbstractDetails.aspx?id=91377 | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients with DM who were candidates for kidney transplant. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Not reported. |
| Partial verification avoided? All tests | Yes | All patients underwent coronary angiography. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not reported. |
| Index test results blinded? All tests | Unclear | Not reported. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No uninterpretable results present. |
| Withdrawals explained? All tests | Yes | No withdrawals reported. |
Herzog 1999.
| Clinical features and settings |
Clinical features Patients referred for kidney transplantation evaluation from June 1992 to January 1995
Setting
|
|
| Participants |
Exclusion criteria
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | Patients were followed up for a mean of 22.5 ± 10.1 months. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients referred for kidney transplantation evaluation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | 47 patients had angiography within 2 weeks after DSE (median, 2 days; mean, 12.4 ± 41 days); three patients had angiographic studies at 69, 85, and 280 days after DSE (angiography was delayed wound infection (1 patient) and psychosocial reasons (2 patients). |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | All lesions occurring in the major coronary artery segments or their proximal branches were visually identified, and an initial qualitative assessment made by a skilled reader blinded to all clinical data. |
| Index test results blinded? All tests | Yes | All DSE studies were analysed in digital format independently by three echocardiographers blinded to angiographic data. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No uninterpretable results were present. |
| Withdrawals explained? All tests | Yes | 55 eligible patients participated; 2 were excluded for unstable angina before scheduled testing; 3 underwent DSE and subsequently declined coronary angiography; 50 patients completed the research protocol. 39/50 patients qualified for DSE by the prespecified inclusion criterion of ESKD secondary to diabetic nephropathy (regardless of exercise capacity). The remaining 11 patients were unable to perform treadmill exercise because of peripheral vascular disease (4 patients), musculoskeletal disease (4 patients), lung disease (1 patient), and generalised fatigue (2 patients). |
Jassal 2007.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | None reported | |
| Notes | Only data for the 18 patients referred for pre‐renal transplant workup were considered. Sufficient data in published report to create 2 x 2 table | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Patients who presented for cardiac evaluation before kidney transplantation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test also had the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not reported. |
| Index test results blinded? All tests | Unclear | Not reported. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No uninterpretable results were present. |
| Withdrawals explained? All tests | Yes | No withdrawals were reported. |
Krawczynska 1988.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Thalium‐201 Cardiac SPECT
|
|
| Follow‐up | Postoperative data available for outcomes of death and adverse cardiac events. | |
| Notes | Only available in abstract form (presentation). | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Prerenal transplant cardiac assessment. 305 ESKD patients waiting kidney transplantation. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be short delay between tests. |
| Partial verification avoided? All tests | No | 38 patients received both coronary angiography and stress test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not stated in abstract. |
| Index test results blinded? All tests | Unclear | Not stated in abstract. |
| Relevant clinical information? All tests | Unclear | Insufficient clinical information provided about performance and analysis of the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Marwick 1989.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSF
|
|
| Follow‐up | None reported. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Yes | Tests performed at the same time. |
| Partial verification avoided? All tests | Yes | All participants who underwent an index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Author correspondence. |
| Index test results blinded? All tests | Yes | Author correspondence. |
| Relevant clinical information? All tests | Yes | Relevant clinical information provided regarding performance and analysis of the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals were reported. |
Marwick 1990.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
Exclusion criteria
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Dipyridamole SPECT Thallium Imaging
|
|
| Follow‐up | Follow up over 25 ± 14 months. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | Thallium scanning was performed within a week of coronary angiography. |
| Partial verification avoided? All tests | Yes | All participants who received an index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Author correspondence. |
| Index test results blinded? All tests | Yes | Author correspondence. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding performance and analysis of the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals were reported. |
Modi 2006.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
CIMT measurement
|
|
| Follow‐up | None reported. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Yes, coronary angiography with a reference standard threshold of ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Unclear, but likely to be only short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who received an index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Incorporation avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Reference standard results blinded? All tests | Yes | Reference standard performed before index test. Therefore it was not influenced by results of index test. |
| Index test results blinded? All tests | Yes | An operator, who was blinded with respect to the results of the coronary angiography, measured CIMT in all patients prior to coronary angiography and recorded it on videotape. Two independent observers who were blinded to the result of coronary angiography, measured CIMT offline to validate its predictive accuracy as a noninvasive test in predicting the presence or absence of CAD. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals were present. |
Reis 1995.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | 12 ± 6 months. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 50% stenosis. |
| Acceptable delay between tests? All tests | Yes | Within 4 months. |
| Partial verification avoided? All tests | No | Coronary angiography was performed in 30/97 patients. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not reported. |
| Index test results blinded? All tests | Yes | All DSE studies were reviewed by experienced echocardiographers blinded to angiographic data. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
Rosario 2010.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study. | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Multi‐detector CT exams
|
|
| Follow‐up | Follow‐up ongoing. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | CKD patients already in a haemodialysis program and referred to be submitted to kidney transplant. |
| Acceptable reference standard? All tests | Yes | Yes, coronary angiography with a reference standard threshold of ≥ 50 and 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | Time elapsed between Multi‐detector CT and coronary angiography was on average 99.03 days, SD 87.65 days, and median 79 days. Minimum interval was 2 days, and maximum interval was 380 days. Only 2 cases exceeded 1 year, and 16 cases had an interval over 6 months. |
| Partial verification avoided? All tests | Yes | All participants who received an index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Incorporation avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Reference standard results blinded? All tests | Yes | An observer experienced in QCA technique and who did not participate in the Multi‐detector CT analysis ‐ also blind and independent. |
| Index test results blinded? All tests | Unclear | Not reported. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals were present. |
Sharma 2005.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
Exclusion criteria
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
|
|
| Follow‐up | Patients were followed up for 1.32 ± 0.48 years (range 0.19 ± 2.12 years). | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Angiograms were interpreted by two experienced, blinded observers with consensus for disagreement. |
| Index test results blinded? All tests | Yes | All images were reported offline by two experienced observers blinded to the rest of the study. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals were reported. |
Sharma 2009.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
Exclusion criteria
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
Echocardiography
|
|
| Follow‐up | Mean follow‐up was 2.3 ± 0.7 years (range 0.2 to 3.3 years) | |
| Notes | The authors reported that this study population was different from the study results published in 2005. We were able to create 2 x 2 tables using tabulated results from the study. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Unclear, but likely to be only short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Incorporation avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Reference standard results blinded? All tests | Yes | Angiograms were interpreted blindly by two experienced observers and consensus was obtained in discordant cases from a third experienced operator. |
| Index test results blinded? All tests | Yes | The analysis of conventional and tissue Doppler imaging stress echo data was performed off‐line by two independent, experienced observers blinded to clinical and coronary angiography data. Consensus was obtained in discordant cases from a third experienced operator. |
| Relevant clinical information? All tests | Yes | All patients missing from the final analysis were accounted for. |
| Uninterpretable results reported? All tests | Yes | No results were reported to be uninterpretable. |
| Withdrawals explained? All tests | Yes | No withdrawals were reported. |
Sharples 2004.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cross sectional study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
EBCT
|
|
| Follow‐up | None reported. | |
| Notes | Results reported per vessel, not per patient. Insufficient data to construct meaningful 2 x 2 table. Therefore, study did not contribute data to the meta‐analysis. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients assessed for CAD before kidney transplant. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 75% stenosis. |
| Acceptable delay between tests? All tests | Unclear | Likely to be short delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Analysis of the coronary angiograms was performed using a digital analysis system operated by a cardiologist blinded to the calcification score. |
| Index test results blinded? All tests | Yes | The acquired images were scored with the use of Imatron software by a single radiologist blinded to the clinical or angiographic history of the patient. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable results. |
| Withdrawals explained? All tests | Yes | There were no withdrawals. |
Vandenberg 1996.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Pharmacologic stress thallium scintigraphy
Exercise radionuclide ventriculography
|
|
| Follow‐up | The mean time from thallium scintigraphy to the latest follow‐up visit was 35 ± 19 months. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | Renal failure patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Yes, coronary angiography with a reference standard threshold of ≥75% stenosis. |
| Acceptable delay between tests? All tests | Yes | Angiography was performed 55 ± 42 days after thallium scintigraphy in 42 patients and 50 ± 45 days after exercise radionuclide ventriculography in 40 patients. |
| Partial verification avoided? All tests | Yes | All participants who received an index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Incorporation avoided? All tests | Yes | This was not an issue in this study. Disease status (CAD) is diagnosed only through coronary angiography. |
| Reference standard results blinded? All tests | Yes | Measurements were made by a single observer without knowledge of the results of the imaging tests. |
| Index test results blinded? All tests | Yes | Images were interpreted by the consensus of two experienced radiologists who were unaware of the angiography results. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of both the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | Yes. One MPS was technically suboptimal and was therefore not included in the analysis. Exercise ventriculography was suboptimal in five patients and they were not included in the analysis. |
| Withdrawals explained? All tests | Yes | All patients missing from the final analysis were accounted for. |
West 2000.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
DSE
|
|
| Follow‐up | Patients were followed up for an unspecified time. | |
| Notes | ||
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary artery stenosis measured by coronary angiography. CAD defined as the presence of ≥ 1 coronary arteries with ≥ 70% diameter stenosis, or > 50% in left main coronary artery. |
| Acceptable delay between tests? All tests | Unclear | Likely to be only delay between tests. |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Unclear | Not reported. |
| Index test results blinded? All tests | Unclear | Not reported. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable results. |
| Withdrawals explained? All tests | Yes | Nine patients were excluded because of prior coronary angiography (5), class III ± IV angina (3), and refusal to participate in the study (1). |
Worthley 2003.
| Clinical features and settings |
Clinical features
Setting
|
|
| Participants |
Exclusion criteria
|
|
| Study design | Cohort study | |
| Target condition and reference standard(s) |
Coronary artery stenosis measured by coronary angiography
|
|
| Index and comparator tests |
Tachycardic‐stress perfusion imaging
|
|
| Follow‐up | Mean follow‐up of 28 ± 10 months. | |
| Notes | Informed consent was obtained before study entry. | |
| Table of Methodological Quality | ||
| Item | Authors' judgement | Description |
| Representative spectrum? All tests | Yes | ESKD patients undergoing cardiac evaluation as part of transplant workup. |
| Acceptable reference standard? All tests | Yes | Coronary angiography with a reference standard threshold of ≥ 70% stenosis. |
| Acceptable delay between tests? All tests | Yes | Tests were done at the same time (author correspondence). |
| Partial verification avoided? All tests | Yes | All participants who underwent the index test received the reference standard test. |
| Differential verification avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Incorporation avoided? All tests | Yes | Disease status (CAD) diagnosed by coronary angiography. |
| Reference standard results blinded? All tests | Yes | Angiograms were assessed by 2 cardiologists who were blinded to the perfusion imaging results. |
| Index test results blinded? All tests | Yes | Images were assessed by nuclear cardiologists who were blinded to the cardiac catheterisation results. |
| Relevant clinical information? All tests | Yes | Relevant clinical information was provided regarding the performance and analysis of the index and reference tests. |
| Uninterpretable results reported? All tests | Yes | There were no uninterpretable test results. |
| Withdrawals explained? All tests | Yes | No withdrawals reported. |
bpm: beats per minute; CAD: coronary artery disease; CF: cardiac failure; CHF: congestive heart failure; CIMT: carotid intimal medial thickness; CKD: chronic kidney disease; CVD: cardiovascular disease; DBP: diastolic blood pressure; DM: diabetes mellitus; DSE: dobutamine stress echocardiogram; DSTS: dipyridamole stress thallium scan; EBCT: electron beam computed tomography; ECG: electrocardiogram; ESKD: end‐stage kidney disease; HTN: hypertension; IHD: ischaemic heart disease; IMT: intimal media thickness; IV: intravenous; MI: myocardial infarction; MIBI: methoxyisobutyl isonitrile stress; MPS: myocardial perfusion scintigraphy; QCA: quantitative coronary analysis; RRT: renal replacement therapy; RWM: regional wall motion; SBP: systolic blood pressure; ST: sinus tachycardia; WMA: wall motion abnormality
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ali 2004 | Coronary angiography not routinely performed on patients in study. |
| Arantes 2010 | Prognostic study; not enough data available to allow for diagnostic accuracy comparison with coronary angiography. |
| Braun 1984 | No index tests for comparison. |
| Brown 1989 | Prognostic study; not enough data available to allow for diagnostic accuracy comparison with coronary angiography. |
| Caglar 2006 | Patient population not consisting of patients who are potential transplant recipients; coronary angiography only provided to patients who tested positive to other tests. |
| Camp 1990 | Coronary angiography not used as reference standard. |
| Cortigiani 2005 | Coronary angiography not used as reference standard. |
| Cottier 1990 | Coronary angiography not routinely performed on patients in study. |
| Cross 1996 | Prognostic study; not enough data available to allow for diagnostic accuracy comparison with coronary angiography. |
| Dahan 1995 | Patient population not entirely consisting of patients who are potential transplant recipients. Separate data for potential transplant recipients not available. |
| Dahan 1998 | Patient population not entirely consisting of patients who are potential transplant recipients. Separate data for potential transplant recipients not available. |
| Dahan 2002 | Patient population not entirely consisting of patients who are potential transplant recipients. Separate data for potential transplant recipients not available. |
| De Vriese 2009 | Patient population not entirely consisting of patients who are potential transplant recipients. Roughly 1/3 of the patients that were included in the study were being evaluated for kidney transplantation. The others consented to have the evaluation as a screening test, because the authors explained to them that the majority of patients with CAD on dialysis are asymptomatic (author communication). Separate data for potential transplant recipients not available. |
| Derfler 1991 | Coronary angiography not used as reference standard. |
| Dussol 2004 | Coronary angiography not routinely performed on patients in study, only performed on patients who were index test positive. |
| Eschertzhuber 2005 | Coronary angiography not routinely performed on patients in study. |
| Feola 2002 | Coronary angiography not used as reference standard. |
| Fossati 2004 | Data insufficient to construct appropriate 2 x 2 table. |
| Fujimoto 2006 | This was a study of diagnostic accuracy but the patient population did not consist entirely of patients who are potential transplant recipients. Separate data on patients who were potential transplant recipients not available. |
| Fukui 2005 | This was a study of diagnostic accuracy but the patient population did not consist entirely of patients who are potential transplant recipients. Separate data on patients who were potential transplant recipients not available. |
| Fuster 2000 | Coronary angiography not routinely performed on patients in study, only performed on patients who were index test positive. |
| Holley 1991 | Coronary angiography not routinely performed on patients in study; data insufficient to construct appropriate 2 x 2 table. |
| Iqbal 1991 | Coronary angiography not used as reference standard. |
| Jeloka 2007 | Coronary angiography not used as reference standard. |
| Krotin 2007 | Coronary angiography not used as reference standard. |
| Langford 1997 | Coronary angiography not used as reference standard. |
| Le 1994 | Prognostic study; not enough data available to allow for diagnostic accuracy comparison with coronary angiography. |
| Leonardi 2009 | Single centre case experience; not a study of diagnostic accuracy. |
| Lewis 2002 | Prognostic study; not enough data available to allow for diagnostic accuracy comparison with coronary angiography. |
| Lin 2001 | Coronary angiography not used as reference standard. |
| Ma 2006 | Coronary angiography only used in those with high risk scores. |
| Manske 1997 | Data insufficient to construct appropriate 2 x 2 table. |
| Mao 2010 | Coronary angiography not used as reference standard. |
| Mistry 1998 | Coronary angiography not used as reference standard. |
| Morrow 1983 | Coronary angiography not used as reference standard. |
| Nguyen 2007 | Coronary angiography not used as reference standard. |
| Nishimura 2004 | This was a study of diagnostic accuracy but the patient population did not consist entirely of patients who are potential transplant recipients. Separate data on patients who were potential transplant recipients not available. |
| Ohtake 2005 | This was a study of diagnostic accuracy but the patient population did not consist entirely of patients who are potential transplant recipients. Separate data on patients who were potential transplant recipients not available. |
| Oliveira 2005 | Only coronary angiography studied. No other index tests present. |
| Patel 2003 | Coronary angiography not used as reference standard. |
| Patel 2008 | Coronary angiography not routinely performed on patients in study. |
| Philipson 1986 | Reference standard differentially applied to different treatment groups; unable to construct meaningful 2 x 2 table. |
| Porter 2003 | Coronary angiography not used as reference standard. |
| Rakhit 2006 | Coronary angiography not used as reference standard. |
| Robinson 2007 | This was a study of diagnostic accuracy but the patient population did not consist entirely of patients who are potential transplant recipients. Separate data on patients who were potential transplant recipients not available. |
| Russell 1993 | Prognostic study; not enough data available to enable diagnostic accuracy comparison with coronary angiography. |
| Schmidt 2001 | Patient population not exclusively consisting of patients who are potential transplant recipients; patients were either those who were on long‐term RRT, or who had undergone successful renal transplantation. Separate data on patients who were potential transplant recipients not available. |
| Sharma 2007 | Coronary angiography not used as reference standard. |
| Tita 2008 | Coronary angiography not used as reference standard. |
| Trochu 1991 | Coronary angiography not used as reference standard. |
| Venkataraman 2008 | Coronary angiography not used as reference standard. |
| Weinrauch 1978 | Only coronary angiography studied. No index tests for comparison. |
| Weinrauch 1992 | Coronary angiography not used as reference standard. |
| Witczak 2006 | Only coronary angiography studied. No index tests for comparison. |
| Wong 2008 | Coronary angiography not used as reference standard. |
Differences between protocol and review
Sparsity of data, both in terms of numbers of studies and participants, meant that we were unable to perform meaningful subgroup analyses of the effect of DM or prevalence of angina and symptomatic ischaemic heart disease on diagnostic test performance.
Contributions of authors
Louis W Wang: Designed and co‐ordinated the review, collected data, undertook searches, screened search results, organised study retrieval, screened retrieved studies against inclusion criteria, appraised study quality, extracted data, corresponded with study authors to obtain additional information, data management, entry, analysis and interpretation, review writing.
Angela C Webster: Designed and co‐ordinated the review, corresponded with study authors to obtain additional information, analysed and interpreted data, review writing, provided general advice on the review, performed previous work that was the foundation of the current study, provided methodological and clinical perspectives (transplant physician).
Magid A Fahim: Data collection, undertook searches, screened search results, screened retrieved studies against inclusion criteria, appraised study quality, data extraction.
Ruth Mitchell: Designed search strategies, undertook searches.
Andrew Hayen: Designed the statistical methodology, analysed and interpreted data.
Laura Baines: Performed previous research that formed the foundation of the current review, provided a clinical perspective (nephrology).
Stephen Lord: Performed previous research that formed the foundation of the current review, provided a clinical perspective (cardiology).
Jonathan C Craig: Provided methodological and clinical perspectives, and general advice on the review.
Sources of support
Internal sources
No sources of support supplied
External sources
Jacquot Research Establishment Award, administered by the Royal Australasian College of Physicians and the Australian and New Zealand Society of Nephrology, Australia.
Australian National Health and Medical Research Council Program (Grant Number 402764), Australia.
Declarations of interest
Laura Baines: None known
Jonathan C Craig: None known
Magid A Fahim: None known
Andrew Hayen: None known
Stephen Lord: None Known
Ruth L Mitchell: During the time I have been an author on this review my salary has been supported through a grant from the Cochrane Collaboration for work on the Cochrane register of diagnostic test accuracy studies.
Louis W Wang: None known.
Angela C Webster: None known
New
References
References to studies included in this review
Bates 1996 {published data only}
- Bates JR, Sawada SG, Segar DS, Spaedy AJ, Petrovic O, Fineberg NS, et al. Evaluation using dobutamine stress echocardiography in patients with insulin‐dependent diabetes mellitus before kidney and/or pancreas transplantation. American Journal of Cardiology 1996;77(2):175‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bennett 1978 {published data only}
- Bennett WM, Kloster F, Rosch J, Barry J, Porter GA. Natural history of asymptomatic coronary arteriographic lesions in diabetic patients with end‐stage renal disease. American Journal of Medicine 1978;65(5):779‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Boudreau 1990 {published data only}
- Boudreau RJ, Strony JT, DuCret RP, Kuni CC, Wang Y, Wilson R, F, et al. Perfusion thallium imaging of type I diabetes patients with end stage renal disease: Comparison of oral and intravenous dipyridamole administration. Radiology 1990;175(1):103‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Brennan 1997 {published and unpublished data}
- Brennan DC, Vedala G, Miller SB, Anstey ME, Singer GG, Kovacs, A, et al. Pretransplant dobutamine stress echocardiography is useful and cost‐effective in renal transplant candidates. Transplantation Proceedings 1997;29(1‐2):233‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cai 2010 {published data only (unpublished sought but not used)}
- Cai Q, Serrano R, Kalyanasundaram A, Shirani J. A preoperative echocardiographic predictive model for assessment of cardiovascular outcome after renal transplantation. Journal of the American Society of Echocardiography 2010;23(5):560‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
De Lima 2003 {published and unpublished data}
- Lima JJG, Sabbaga E, Vieira MLC, Paula FJ, Ianhez LE, Krieger EM, et al. Coronary angiography is the best predictor of events in renal transplant candidates compared with noninvasive testing. Hypertension 2003;42(3):263‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ferreira 2007 {published data only}
- Ferreira PAM, Lima VC, Campos FO, Gil MA, Cordovil A, Machado, CV, et al. Feasibility, safety and accuracy of dobutamine/atropine stress echocardiography for the detection of coronary artery disease in renal transplant candidates. Arquivos Brasileiros de Cardiologia 2007;88(1):41‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gang 2007 {published and unpublished data}
- Gang S, Dabhi M, Rajapurkar MM. Ischaemia imaging in type 2 diabetic kidney transplant candidates ‐ is coronary angiography essential?. Nephrology Dialysis Transplantation 2007;22(8):2334‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Garcia‐Canton 1998 {published and unpublished data}
- Garcia‐Canton C, Culebras C, Hernandez‐Briz MJ, Palomar R, Moreno A, Toledo A, et al. Dobutamine stress echocardiography and stress 99M‐Technetium methoxyisobutylisonitrile SPECT in the assessment of coronary artery disease in kidney transplant candidates [abstract]. Journal of the American Society of Nephrology 1998;9(September, Program and Abstracts):708. [Google Scholar]
Garg 2000 {published and unpublished data}
- Garg N, Kapoor A, Umesan CV, Sharma RK, Sinha N. Role of pretransplant arteriography in diabetic end‐stage renal disease. Asian Cardiovascular and Thoracic Annals 2000;8(2):150‐4. [EMBASE: 2000282610] [Google Scholar]
Gowdak 2010 {published data only (unpublished sought but not used)}
- Gowdak LH, Paula FJ, Oliveira AL, Arantes RL, Cesar LA, Ramires JA, et al. Non‐invasive screening for coronary artery disease in renal transplant candidates with diabetes is influenced by gender. European Society of Cardiology Congress; 2010 Aug 28‐Sep 01; Stockholm, Sweden. http://spo.escardio.org/AbstractDetails.aspx?id=91377 (last accessed 04 Oct 2011). 2010.
Herzog 1999 {published data only}
- Herzog CA, Marwick TH, Pheley AM, White CW, Rao VK, Dick CD. Dobutamine stress echocardiography for the detection of significant coronary artery disease in renal transplant candidates. American Journal of Kidney Diseases 1999;33(6):1080‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jassal 2007 {published data only}
- Jassal DS, Neilan TG, Picard MH, Wood MJ. Stress echocardiography: Abnormal response of tissue Doppler‐derived indices to dobutamine in the absence of obstructive coronary artery disease in patients with chronic renal failure. Echocardiography 2007;24(6):580‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Krawczynska 1988 {published data only}
- Krawczynska EG, DePuey EG, Whelchel JD. Tl‐201 cardiac SPECT to evaluate pre‐renal transplant patients [abstract]. Journal of Nuclear Medicine 1988;29(5 Suppl):950. [Google Scholar]
Marwick 1989 {published and unpublished data}
- Marwick T, Hobbs R, Vanderlaan RL, Steinmuller D, Braun W. Use of digital subtraction fluorography in screening for coronary artery disease in patients with chronic renal failure. American Journal of Kidney Diseases 1989;14(2):105‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Marwick 1990 {published and unpublished data}
- Marwick TH, Steinmuller DR, Underwood DA, Hobbs RE, Go RT, Swift C, et al. Ineffectiveness of dipyridamole SPECT thallium imaging as a screening technique for coronary artery disease in patients with end‐stage renal failure. Transplantation 1990;49(1):100‐3. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Modi 2006 {published data only}
- Modi N, Kapoor A, Kumar S, Tewari S, Garg N, Sinha N. Utility of carotid intimal medial thickness as a screening tool for evaluation of coronary artery disease in pre‐transplant end stage renal disease. Journal of Postgraduate Medicine 2006;52(4):266‐70. [MEDLINE: ] [PubMed] [Google Scholar]
Reis 1995 {published and unpublished data}
- Reis G, Marcovitz PA, Leichtman AB, Merion RM, Fay WP, Werns SW, et al. Usefulness of dobutamine stress echocardiography in detecting coronary artery disease in end‐stage renal disease. American Journal of Cardiology 1995;75(10):707‐10. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rosario 2010 {published data only}
- Rosario MA, Lima JJ, Parga JR, Avila LF, Gowdak LH, Lemos PA, et al. Coronary calcium score as predictor of stenosis and events in pretransplant renal chronic failure. Arquivos Brasileiros de Cardiologia 2010;94(2):239‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sharma 2005 {published data only}
- Sharma R, Pellerin D, Gaze DC, Gregson H, Streather CP, Collinson PO, et al. Dobutamine stress echocardiography and the resting but not exercise electrocardiograph predict severe coronary artery disease in renal transplant candidates. Nephrology Dialysis Transplantation 2005;20(10):2207‐14. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Sharma R, Pellerin D, Gaze DC, Shah JS, Streather CP, Collinson PO, et al. Dobutamine stress echocardiography and cardiac troponin T for the detection of significant coronary artery disease and predicting outcome in renal transplant candidates. European Journal of Echocardiography 2005;6(5):327‐35. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sharma 2009 {published data only}
- Sharma R, Mehta RL, Brecker SJD, Gaze DC, Gregson H, Streather CP, et al. The diagnostic and prognostic value of tissue Doppler imaging during dobutamine stress echocardiography in end‐stage renal disease. Coronary Artery Disease 2009;20(3):230‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sharples 2004 {published data only}
- Sharples EJ, Pereira D, Summers S, Cunningham J, Rubens M, Goldsmith D, et al. Coronary artery calcification measured with electron‐beam computerized tomography correlates poorly with coronary artery angiography in dialysis patients. American Journal of Kidney Diseases 2004;43(2):313‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Vandenberg 1996 {published and unpublished data}
- Vandenberg BF, Rossen JD, Grover‐Mckay M, Shammas NW, Burns TL, Rezai K. Evaluation of diabetic patients for renal and pancreas transplantation: Noninvasive screening for coronary artery disease using radionuclide methods. Transplantation 1996;62(9):1230‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
West 2000 {published data only}
- West JC, Napoliello DA, Costello JM, Nassef LA, Butcher RJ, Hartle JE, et al. Preoperative dobutamine stress echocardiography versus cardiac arteriography for risk assessment prior to renal transplantation. Transplant International 2000;13(Suppl 1):S27‐30. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Worthley 2003 {published and unpublished data}
- Worthley MI, Unger SA, Mathew TH, Russ GR, Horowitz JD. Usefulness of tachycardic‐stress perfusion imaging to predict coronary artery disease in high‐risk patients with chronic renal failure. American Journal of Cardiology 2003;92(11):1318‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ali 2004 {published data only}
- Ali M, Giblin L, Farhad K, O'Kelly P, Hickey D, Little D, et al. Pretransplant cardiac investigations in the Irish renal transplant population‐‐the effectiveness of our current screening techniques in predicting cardiac events. Renal Failure 2004;26(4):375‐80. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Arantes 2010 {published data only}
- Arantes RL, Gowdak LH, Paula FJ, Ianhez LE, Ramires JAF, Krieger EM, et al. Myocardial scintigraphy and clinical stratification as predictors of events in renal transplant candidates. Journal of Nephrology 2010;23(3):314‐20. [MEDLINE: ] [PubMed] [Google Scholar]
Braun 1984 {published data only}
- Braun WE, Phillips DF, Vidt DG, Novick AC, Nakamoto S, Popowniak KL, et al. Coronary artery disease in 100 diabetics with end‐stage renal failure. Transplantation Proceedings 1984;16(3):603‐7. [MEDLINE: ] [PubMed] [Google Scholar]
Brown 1989 {published data only}
- Brown KA, Rimmer J, Haisch C. Noninvasive cardiac risk stratification of diabetic and nondiabetic uremic renal allograft candidates using dipyridamole‐thallium‐201 imaging and radionuclide ventriculography. American Journal of Cardiology 1989;64(16):1017‐21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Caglar 2006 {published data only}
- Caglar M, Mahmoudian B, Aytemir K, Kahraman S, Arici M, Kabakci G, et al. Value of 99mTc‐methoxyisobutylisonitrile (99mTc‐MIBI) gated SPECT for the detection of silent myocardial ischemia in hemodialysis patients: clinical variables associated with abnormal test results. Nuclear Medicine Communications 2006;27(1):61‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Camp 1990 {published data only}
- Camp AD, Garvin PJ, Hoff J, Marsh J, Byers SL, Chaitman BR. Prognostic value of intravenous dipyridamole thallium imaging in patients with diabetes mellitus considered for renal transplantation. American Journal of Cardiology 1990;65(22):1459‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cortigiani 2005 {published data only}
- Cortigiani L, Desideri A, Gigli G, Vallebona A, Terlizzi R, Giusti R, et al. Clinical, resting echo and dipyridamole stress echocardiography findings for the screening of renal transplant candidates. International Journal of Cardiology 2005;103(2):168‐74. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cottier 1990 {published data only}
- Cottier C, Pfisterer M, Muller‐Brand J, Thiel G, Burkart F. Cardiac evaluation of candidates for kidney transplantation: value of exercise radionuclide angiocardiography. European Heart Journal 1990;11(9):832‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Cross 1996 {published data only}
- Cross DS, Alagarsamy SH, Adams M, Esquivel‐Avila JG, Carson R, Ahmad M. Dobutamine stress echocardiography for risk stratification in patients for renal transplantation [abstract no: 3967]. Circulation 1996;94. [Google Scholar]
Dahan 1995 {published data only}
- Dahan M, Legallicier B, Himbert D, Faraggi M, Aubry N, Siohan P, et al. [Diagnostic value of myocardial thallium stress scintigraphy in the detection of coronary artery disease in patients undergoing chronic hemodialysis] [Valeur diagnostique de la scintigraphie myocardique au thallium sous stimulation dans la detection de la maladie coronarienne chez l'hemodialyse chronique]. Archives des Maladies du Coeur et des Vaisseaux 1995;88(8):1121‐3. [MEDLINE: ] [PubMed] [Google Scholar]
Dahan 1998 {published data only}
- Dahan M, Viron BM, Faraggi M, Himbert DL, Legallicier BJ, Kolta AM, et al. Diagnostic accuracy and prognostic value of combined dipyridamole‐ exercise thallium imaging in hemodialysis patients. Kidney International 1998;54(1):255‐62. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dahan 2002 {published data only}
- Dahan M, Viron BM, Poiseau E, Kolta AM, Aubry N, Paillole C, et al. Combined dipyridamole‐exercise stress echocardiography for detection of myocardial ischemia in hemodialysis patients: An alternative to stress nuclear imaging. American Journal of Kidney Diseases 2002;40(4):737‐44. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
De Vriese 2009 {published data only (unpublished sought but not used)}
- Vriese AS, Bacquer DA, Verbeke FH, Winter O, Franken PR, Sutter JH, et al. Comparison of the prognostic value of dipyridamole and dobutamine myocardial perfusion scintigraphy in hemodialysis patients. Kidney International 2009;76(4):428‐36. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Derfler 1991 {published data only}
- Derfler K, Kletter K, Balcke P, Heinz G, Dudczak R. Predictive value of thallium‐201‐dipyridamole myocardial stress scintigraphy in chronic hemodialysis patients and transplant recipients. Clinical Nephrology 1991;36(4):192‐202. [MEDLINE: ] [PubMed] [Google Scholar]
Dussol 2004 {published data only}
- Dussol B, Bonnet J‐L, Sampol J, Savin B, Forte C, Mundler O, et al. Prognostic value of inducible myocardial ischemia in predicting cardiovascular events after renal transplantation. Kidney International 2004;66(4):1633‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Eschertzhuber 2005 {published data only}
- Eschertzhuber S, Hohlrieder M, Boesmueller C, Pomaroli A, Steurer W, Junker T, et al. Incidence of coronary heart disease and cardiac events in patients undergoing kidney and pancreatic transplantation. Transplantation Proceedings 2005;37(2):1297‐300. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Feola 2002 {published data only}
- Feola M, Biggi A, Ribichini F, Rovere A, Vado A, Camuzzini G, et al. Predicting cardiac events with TL201 dipyridamole myocardial scintigraphy in renal transplant recipients. Journal of Nephrology 2002;15(1):48‐53. [MEDLINE: ] [PubMed] [Google Scholar]
Fossati 2004 {published data only}
- Fossati N, Meacci L, Amorese G, Bellissima G, Pieri M, Nardi S, et al. Cardiac evaluation for simultaneous pancreas‐kidney transplantation and incidence of cardiac perioperative complications: Preliminary study. Transplantation Proceedings 2004;36(3):582‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fujimoto 2006 {published data only}
- Fujimoto N, Iseki K, Tokuyama K, Tamashiro M, Takishita S. Significance of coronary artery calcification score (CACS) for the detection of coronary artery disease (CAD) in chronic dialysis patients. Clinica Chimica Acta 2006;367(1‐2):98‐102. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fukui 2005 {published data only}
- Fukui M, Mori Y, Takehana K, Masaki H, Motohiro M, Sakamoto N, et al. Assessment of coronary artery disease in hemodialysis patients with delayed systolic blood pressure response after exercise testing. Blood Purification 2005;23(6):466‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fuster 2000 {published data only}
- Fuster D, Magrina J, Ricart MJ, Pascual J, Laterza C, Setoain FJ, et al. Noninvasive assessment of cardiac risk in type I diabetic patients being evaluated for combined pancreas‐kidney transplantation using dipyridamole‐MIBI perfusion tomographic scintigraphy. Transplant International 2000;13(5):327‐32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Holley 1991 {published data only}
- Holley JL, Fenton RA, Arthur RS. Thallium stress testing does not predict cardiovascular risk in diabetic patients with end‐stage renal disease undergoing cadaveric renal transplantation. American Journal of Medicine 1991;90(5):563‐70. [MEDLINE: ] [PubMed] [Google Scholar]
Iqbal 1991 {published data only}
- Iqbal A, Gibbons RJ, McGoon MD, Sterioff S, Frohnert PP, Velosa JA. Noninvasive assessment of cardiac risk in insulin‐dependent diabetic patients being evaluated for pancreatic transplantation using thallium‐201 myocardial perfusion scintigraphy. Clinical Transplantation 1991;5(1):13‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Jeloka 2007 {published data only}
- Jeloka TK, Ross H, Smith R, Huang M, Fenton S, Cattran D, et al. Renal transplant outcome in high‐cardiovascular risk recipients. Clinical Transplantation 2007;21(5):609‐14. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Krotin 2007 {published data only}
- Krotin M, Vukovic D, Stojanovic O, Milovanovic B, Celeketic D, Blagojevic R. Prognostic value of dobutamine stress echocardiography in patients with terminal renal insufficiency undergoing hemodialysis ‐ a 5‐year follow up. Medicinski Pregled 2007;60(7‐8):333‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Langford 1997 {published data only}
- Langford EJ, Belder AJ, Cairns H, Hendry BM, Wainwright RJ. Non‐invasive cardiac investigations in patients awaiting renal transplantation. Journal of the Royal Society of Medicine 1997;90(3):136‐7. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Le 1994 {published data only}
- Le A, Wilson R, Douek K, Pulliam L, Tolzman D, Norman D, et al. Prospective risk stratification in renal transplant candidates for cardiac death. American Journal of Kidney Diseases 1994;24(1):65‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leonardi 2009 {published data only}
- Leonardi G, Tamagnone M, Ferro M, Tognarelli G, Messina M, Giraudi R, et al. Assessment of cardiovascular risk in waiting‐listed renal transplant patients: a single center experience in 558 cases. Clinical Transplantation 2009;23(5):653‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lewis 2002 {published data only}
- Lewis MS, Wilson RA, Walker KW, Wilson DJ, Norman DJ, Barry JM, et al. Validation of an algorithm for predicting cardiac events in renal transplant candidates. American Journal of Cardiology 2002;89(7):847‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lin 2001 {published data only}
- Lin K, Stewart D, Cooper S, Davis CL. Pre‐transplant cardiac testing for kidney‐pancreas transplant candidates and association with cardiac outcomes. Clinical Transplantation 2001;15(4):269‐75. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ma 2006 {published data only}
- Ma IW, Valantine HA, Shibata A, Waskerwitz J, Dafoe DC, Alfrey EJ, et al. Validation of a screening protocol for identifying low‐risk candidates with type 1 diabetes mellitus for kidney with or without pancreas transplantation. Clinical Transplantation 2006;20(2):139‐46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Manske 1997 {published data only}
- Manske CL, Wilson RF, Wang Y, Thomas W. Atherosclerotic vascular complications in diabetic transplant candidates. American Journal of Kidney Diseases 1997;29(4):601‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mao 2010 {published data only}
- Mao J, Karthikeyan V, Poopat C, Song T, Pantelic M, Chattahi J, et al. Coronary computed tomography angiography in dialysis patients undergoing pre‐renal transplantation cardiac risk stratification. Cardiology Journal 2010;17(4):349‐61. [MEDLINE: ] [PubMed] [Google Scholar]
Mistry 1998 {published data only}
- Mistry BM, Bastani B, Solomon H, Hoff J, Aridge DL, Lindsey LM, et al. Prognostic value of dipyridamole thallium‐201 screening to minimize perioperative cardiac complications in diabetics undergoing kidney or kidney‐pancreas transplantation. Clinical Transplantation 1998;12(2):130‐5. [MEDLINE: ] [PubMed] [Google Scholar]
Morrow 1983 {published data only}
- Morrow CE, Schwartz JS, Sutherland DE, Simmons RL, Ferguson RM, Kjellstrand CM, et al. Predictive value of thallium stress testing for coronary and cardiovascular events in uremic diabetic patients before renal transplantation. American Journal of Surgery 1983;146(3):331‐5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nguyen 2007 {published data only}
- Nguyen PT, Coche E, Goffin E, Beguin C, Vlassenbroek A, Devuyst O, et al. Prevalence and determinants of coronary and aortic calcifications assessed by chest CT in renal transplant recipients. American Journal of Nephrology 2007;27(4):329‐35. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nishimura 2004 {published data only}
- Nishimura M, Hashimoto T, Kobayashi H, Fukuda T, Okino K, Yamamoto N, et al. Myocardial scintigraphy using a fatty acid analogue detects coronary artery disease in hemodialysis patients. Kidney International 2004;66(2):811‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ohtake 2005 {published data only}
- Ohtake T, Kobayashi S, Moriya H, Negishi K, Okamoto K, Maesato K, et al. High prevalence of occult coronary artery stenosis in patients with chronic kidney disease at the initiation of renal replacement therapy: an angiographic examination. Journal of the American Society of Nephrology 2005;16(4):1141‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Oliveira 2005 {published data only}
- Oliveira DC, Filho GG, Nakamoto A, Souza FL, Sa JR, Pestana JO, et al. Prevalence of coronary artery disease in type I diabetic candidates for double transplantation (kidney and pancreas). Arquivos Brasileiros de Cardiologia 2005;84(2):108‐110. [MEDLINE: ] [PubMed] [Google Scholar]
Patel 2003 {published data only}
- Patel AD, Abo‐Auda WS, Davis JM, Zoghbi GJ, Deierhoi MH, Heo J, et al. Prognostic value of myocardial perfusion imaging in predicting outcome after renal transplantation. American Journal of Cardiology 2003;92(2):146‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Patel 2008 {published data only}
- Patel RK, Mark PB, Johnston N, McGeoch R, Lindsay M, Kingsmore DB, et al. Prognostic value of cardiovascular screening in potential renal transplant recipients: a single‐center prospective observational study. American Journal of Transplantation 2008;8(8):1673‐83. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Philipson 1986 {published data only}
- Philipson JD, Carpenter BJ, Itzkoff J, Hakala TR, Rosenthal JT, Taylor RJ, et al. Evaluation of cardiovascular risk for renal transplantation in diabetic patients. American Journal of Medicine 1986;81(4):630‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Porter 2003 {published data only}
- Porter GA, Norton TL, Lindsley J, Stevens JS, Phillips DS, Bennett WM. Relationship between elevated serum troponin values in end‐stage renal disease patients and abnormal isotopic cardiac scans following stress. Renal Failure 2003;25(1):55‐65. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rakhit 2006 {published data only}
- Rakhit DJ, Armstrong KA, Beller E, Isbel NM, Marwick TH. Risk stratification of patients with chronic kidney disease: Results of screening strategies incorporating clinical risk scoring and dobutamine stress echocardiography. American Heart Journal 2006;152(2):363‐70. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Robinson 2007 {published data only}
- Robinson J, Tan AU, Wilensky RL, Matthai W, Munoz M, Rosas SE. Electron‐beam computerized tomography correlates with coronary angiogram in chronic kidney disease patients. American Journal of Nephrology 2007;27(3):247‐52. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Russell 1993 {published data only}
- Russell JD, Stanton EB, Lambert K, et al. Risk stratification for cardiovascular disease in renal transplant candidates: The role of dipyridamole thallium scintigraphy [abstract]. Journal of the American Society of Nephrology. 1993; Vol. 4, issue 3:960.
Schmidt 2001 {published data only (unpublished sought but not used)}
- Schmidt A, Stefenelli T, Schuster E, Mayer G. Informational contribution of noninvasive screening tests for coronary artery disease in patients on chronic renal replacement therapy. American Journal of Kidney Diseases 2001;37(1):56‐63. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sharma 2007 {published data only}
- Sharma R, Chemla E, Tome M, Mehta RL, Gregson H, Brecker SJ, et al. Echocardiography‐based score to predict outcome after renal transplantation. Heart 2007;93(4):464‐9. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tita 2008 {published data only}
- Tita C, Karthikeyan V, Stroe A, Jacobsen G, Ananthasubramaniam K. Stress echocardiography for risk stratification in patients with end‐stage renal disease undergoing renal transplantation. Journal of the American Society of Echocardiography 2008;21(4):321‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Trochu 1991 {published data only}
- Trochu JN, Cantarovich D, Renaudeau J, Patra O, du Roscoat P, Helias J. Assessment of coronary artery disease by thallium scan in type‐1 diabetic uremic patients awaiting combined pancreas and renal transplantation. Angiology 1991;42(4):302‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Venkataraman 2008 {published data only}
- Venkataraman R, Hage FG, Dorfman T, Heo J, Aqel RA, Mattos AM, et al. Role of myocardial perfusion imaging in patients with end‐stage renal disease undergoing coronary angiography. American Journal of Cardiology 2008;102(11):1451‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Weinrauch 1978 {published data only}
- Weinrauch L, D'Elia JA, Healy RW, Gleason RE, Christleib AR, Leland OS. Asymptomatic coronary artery disease: angiographic assessment of diabetics evaluated for renal transplantation. Circulation 1978;58(6):1184‐90. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Weinrauch 1992 {published data only}
- Weinrauch LA, D'Elia JA, Monaco AP, Gleason RE, Welty F, Nishan PC, et al. Preoperative evaluation for diabetic renal transplantation: Impact of clinical, laboratory, and echocardiographic parameters on patient and allograft survival. American Journal of Medicine 1992;93(1):19‐28. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Witczak 2006 {published data only}
- Witczak BJ, Hartmann A, Jenssen T, Foss A, Endresen K. Routine coronary angiography in diabetic nephropathy patients before transplantation. American Journal of Transplantation 2006;6(10):2403‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wong 2008 {published data only}
- Wong CF, Little MA, Vinjamuri S, Hammad A, Harper JM. Technetium myocardial perfusion scanning in prerenal transplant evaluation in the United Kingdom. Transplantation Proceedings 2008;40(5):1324‐28. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Additional references
Akesson 2004
- Akesson L, Svensson A, Edenbrandt L. Operator dependent variability in quantitative analysis of myocardial perfusion images. Clinical Physiology and Functional Imaging 2004;24(6):374‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Alderman 1993
- Alderman EL, Corley SD, Fisher LD, Chaitman BR, Faxon DP, Foster ED, et al. Five‐year angiographic follow‐up of factors associated with progression of coronary artery disease in the Coronary Artery Surgery Study (CASS). CASS Participating Investigators and Staff. Journal of the American College of Cardiology 1993;22(4):1141‐54. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Briggs 2001
- Briggs JD. Causes of death after renal transplantation. Nephrology Dialysis Transplantation 2001;16(8):1545‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Burkhoff 2001
- Burkhoff D, Jones JW, Becker LC. Variability of myocardial perfusion defects assessed by thallium‐201 scintigraphy in patients with coronary artery disease not amenable to angioplasty or bypass surgery. Journal of the American College of Cardiology 2001;38(4):1033‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Caliskan 2008
- Caliskan Y, Oflaz H, Demirturk M, Yazici H, Turkmen A, Cimen A, et al. Coronary flow reserve dysfunction in hemodialysis and kidney transplant patients. Clinical Transplantation 2008;22(6):785‐93. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
De Lima 2010
- Lima JJG, Gowdak LHW, Paula FJ, Arantes RL, Oliveira ALV, Ramires JAF, et al. Treatment of coronary artery disease in hemodialysis patients evaluated for transplant‐A registry study. Transplantation 2010;89(7):845‐50. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
de Vet 2008
- Vet HCW, Eisinga A, Riphagen II, Aertgeerts B, Pewsner D. Chapter 7: Searching for Studies. Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy. Version 0.4 [updated September 2008]. The Cochrane Collaboration, 2008. [Google Scholar]
Doust 2005
- Doust JA, Pietrzak E, Sanders S, Glasziou PP. Identifying studies for systematic reviews of diagnostic tests was difficult due to the poor sensitivity and precision of methodologic filters and the lack of information in the abstract. Journal of Clinical Epidemiology 2005;58(5):444‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Dudley 2008
- Dudley C, Harden P. Assessment for renal transplantation, 4th edition. UK Renal Association. http://www.renal.org/guidelines (accessed 17 January 2010) 2008.
Eagle 2004
- Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, et al. ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation 2004;110(9):1168‐1176. [DOI: 10.1161/01.CIR.0000138790.14877.7D] [DOI] [PubMed] [Google Scholar]
Fleischmann 1998
- Fleischmann KE, Hunink MGM, Kuntz KM, Douglas PS. Exercise echocardiography or exercise SPECT imaging? A meta‐analysis of diagnostic test performance. JAMA 1998;280(10):913‐20. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gunnarsson 1984
- Gunnarsson R, Lofmark R, Nondlander R, Nyquist O, Groth CG. Acute myocardial infarction in renal transplant recipients: incidence and prognosis. European Heart Journal 1984;5(3):218‐21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Hofmann 2008
- Hofmann RM. Pretransplant cardiac evaluation: does it really prevent cardiovascular complications?. American Journal of Transplantation 2008;8(8):1575‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Houghton 1990
- Houghton JL, Frank MJ, Carr AA, Dohlen TW, Prisant LM. Relations among impaired coronary flow reserve, left ventricular hypertrophy and thallium perfusion defects in hypertensive patients without obstructive coronary artery disease. Journal of the American College of Cardiology 1990;15(1):43‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kasiske 2001
- Kasiske BL, Cangro CB, Hariharan S, Hricik DE, Kerman RH, Roth D, et al. The evaluation of renal transplantation candidates: clinical practice guidelines. American Journal of Transplantation 2001;1(Suppl 2):3‐95. [MEDLINE: ] [PubMed] [Google Scholar]
Knoll 2005
- Knoll G, Cockfield S, Blydt‐Hansen T, Baran D, Kiberd B, Landsberg D, et al. Canadian Society of Transplantation: consensus guidelines on eligibility for kidney transplantation. CMAJ Canadian Medical Association Journal 2005;173(10):S1‐25. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leeflang 2006
- Leeflang MMG, Scholten RJPM, Rutjes AWS, Reitsma JB, Bossuyt PMM. Use of methodological search filters to identify diagnostic accuracy studies can lead to the omission of relevant studies. Journal of Clinical Epidemiology 2006;59(3):234‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Leeflang 2009
- Leeflang MMG, Bossuyt PMM, Irwig L. Diagnostic test accuracy may vary with prevalence: implications for evidence‐based diagnosis. Journal of Clinical Epidemiology 2009;62(1):5‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lentine 2005
- Lentine KL, Brennan DC, Schnitzler MA. Incidence and predictors of myocardial infarction after kidney transplantation. Journal of the American Society of Nephrology 2005;16(2):496‐506. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Macaskill 2003
- Macaskill P. Empirical bayes estimates generated in a hierarchical summary ROC analysis agreed closely with those of a full Bayesian analysis. Journal of Clinical Epidemiology 2004;57:925‐32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Manoharan 2009
- Manoharan G, Ntalianis A, Muller O, Hamilos M, Sarno G, Melikian N, et al. Severity of coronary arterial stenoses responsible for acute coronary syndromes. American Journal of Cardiology 2009;103(9):1183‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
McFalls 2004
- McFalls EO, Ward HB, Moritz TE, Goldman S, Krupski WC, Littooy F, et al. Coronary‐artery revascularization before elective major vascular surgery. New England Journal of Medicine 2004;351:2795‐804. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
NICE Clinical Guideline 1995
- National Clinical Guideline Centre for Acute and Chronic Conditions. National Clinical Guideline 95. Chest pain of recent onset: Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin. NHS National Institute for Health and Clinical Excellence. http://www.nice.org.uk/guidance/CG95. (accessed June 9 2010) March 2010.
Niizuma 2008
- Niizuma S, Takiuchi S, Okada S, Horio T, Kamide K, Nakata H, et al. Decreased coronary flow reserve in haemodialysis patients. Nephrology Dialysis Transplantation 2008;23(7):2324‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Poldermans 2007
- Poldermans D, Schouten O, Vidakovic R, Bax JJ. Thomson IR. Hoeks SE, et al. A clinical randomized trial to evaluate the safety of a noninvasive approach in high‐risk patients undergoing major vascular surgery: the DECREASE‐V pilot study. Journal of the American College of Cardiology 2007;49(17):1763‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rechavia 1992
- Rechavia E, Araujo LI, Silva R, Kushwaha SS, Lammertsma AA, Jones T, et al. Dipyridamole vasodilator response after human orthotopic heart transplantation: quantification by oxygen‐15‐labeled water and positron emission tomography. Journal of the American College of Cardiology 1992;19(1):100‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Reitsma 2009
- Reitsma JB, Rutjes AWS, Whiting P, Vlassov VV, Leeflang MMG, Deeks JJ. Chapter 9: Assessing methodological quality. In: Deeks JJ, Bossuyt PM, Gatsonis C (editors), Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy Version 1.0.0. The Cochrane Collaboration, 2009. Available from: http://srdta.cochrane.org.
Ritchie 2007
- Ritchie G, Glanville J, Lefebvre C. Do published search filters to identify diagnostic test accuracy studies perform adequately?. Health Information and Libraries Journal 2007;24(3):188‐92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rutter 2001
- Rutter CM, Gatsonis CA. A hierarchical regression approach to meta‐analysis of diagnostic test accuracy evaluations. Statistics in Medicine 2001;20(19):2865‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
SAS9.2® [Computer program]
- Copyright SAS Institute Inc. SAS. Version 9.2. Cary, NC, USA: Copyright SAS Institute Inc.
Schinkel 2003
- Schinkel AFL, Bax JJ, Geleijnse ML, Boersma E, Elhendy A, Roelandt JR, et al. Noninvasive evaluation of ischaemic heart disease: myocardial perfusion imaging or stress echocardiography?. European Heart Journal. 2003;24(9):789‐800. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Sezer 2007
- Sezer M, Ozcan M, Okcular I, Elitok A. Umman S. Umman B, et al. A potential evidence to explain the reason behind the devastating prognosis of coronary artery disease in uraemic patients: Renal insufficiency is associated with poor coronary collateral vessel development. International journal of cardiology 2007;115(3):366‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Smidt 2008
- Smidt N, Deeks J, Moore T (editors). Chapter 4: Guide to the contents of a Cochrane review and protocol. http://srdta.cochrane.org/sites/srdta.cochrane.org/files/uploads/Handbook1CC_Chapter04_101.pdf (accessed 25 May 2010).
Wang 2011
- Wang LW, Fahim MA, Hayen A, Mitchell RL, Baines L, Lord S, et al. Cardiac testing for coronary artery disease in potential kidney transplant recipients: a systematic review of test accuracy studies. American Journal of Kidney Diseases. 2011;57(3):476‐87. [DOI: 10.1053/j.ajkd.2010.11.018; MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Whiting 2003
- Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Medical Research Methodology 2003;3:25. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yao 2004
- Yao Q, Pecoits‐Filho R, Lindholm B, Stenvinkel P. Traditional and non‐traditional risk factors as contributors to atherosclerotic cardiovascular disease in end‐stage renal disease. Scandinavian Journal of Urology and Nephrology 2004;38(5):405‐16. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


