Abstract
Mothers with a history of gestational diabetes mellitus (GDM) have an increased risk of developing diabetes in the future and a lifelong cardiovascular risk. Postpartal expression profile of cardiovascular/cerebrovascular disease associated microRNAs was assessed 3–11 years after the delivery in whole peripheral blood of young and middle-aged mothers with a prior exposure to GDM with the aim to identify a high-risk group of mothers at risk of later development of diabetes mellitus and cardiovascular/cerebrovascular diseases who would benefit from implementation of early primary prevention strategies and long-term follow-up. The hypothesis of the assessment of cardiovascular risk in women was based on the knowledge that a series of microRNAs play a role in the pathogenesis of diabetes mellitus and cardiovascular/cerebrovascular diseases. Abnormal expression profile of multiple microRNAs was found in women with a prior exposure to GDM (miR-1-3p, miR-16-5p, miR-17-5p, miR-20a-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-29a-3p, miR-100-5p, miR-103a-3p, miR-125b-5p, miR-126-3p, miR-130b-3p, miR-133a-3p, miR-143-3p, miR-145-5p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, miR-342-3p, miR-499a-5p, and-miR-574-3p). Postpartal combined screening of miR-1-3p, miR-16-5p, miR-17-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-26a-5p, miR-29a-3p, miR-103a-3p, miR-133a-3p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p showed the highest accuracy for the identification of mothers with a prior exposure to GDM at a higher risk of later development of cardiovascular/cerebrovascular diseases (AUC 0.900, p < 0.001, sensitivity 77.48%, specificity 93.26%, cut off >0.611270413). It was able to identify 77.48% mothers with an increased cardiovascular risk at 10.0% FPR. Any of changes in epigenome (upregulation of miR-16-5p, miR-17-5p, miR-29a-3p, and miR-195-5p) that were induced by GDM-complicated pregnancy are long-acting and may predispose mothers affected with GDM to later development of diabetes mellitus and cardiovascular/cerebrovascular diseases. In addition, novel epigenetic changes (upregulation of serious of microRNAs) appeared in a proportion of women that were exposed to GDM throughout the postpartal life. Likewise, a previous occurrence of either GH, PE, and/or FGR, as well as a previous occurrence of GDM, is associated with the upregulation of miR-1-3p, miR-17-5p, miR-20a-5p, miR-20b-5p, miR-29a-3p, miR-100-5p, miR-125b-5p, miR-126-3p, miR-130b-3p, miR-133a-3p, miR-143-3p, miR-145-5p, miR-146a-5p, miR-181a-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p. On the other hand, upregulation of miR-16-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-103a-3p, miR-195-5p, miR-342-3p, and miR-574-3p represents a unique feature of aberrant expression profile of women with a prior exposure to GDM. Screening of particular microRNAs may stratify a high-risk group of mothers with a history of GDM who might benefit from implementation of early primary prevention strategies.
Keywords: cardiovascular/cerebrovascular diseases, cardiovascular risk, gestational diabetes mellitus, microRNA expression, mothers, pregnancy complications, primary prevention, screening
1. Introduction
Recently, we demonstrated that history of pregnancy-related complications, such as gestational hypertension (GH), preeclampsia (PE), and/or fetal growth restriction (FGR), was associated with postpartum epigenetic changes characteristic for cardiovascular and cerebrovascular diseases [1,2,3].
We showed that previous occurrence of either GH, PE, and/or FGR might predispose a proportion of women to later development of cardiovascular and cerebrovascular diseases due to the presence of alterations in the expression of cardiovascular and cerebrovascular disease-associated microRNAs in their whole peripheral blood [1,2,3].
Gestational diabetes mellitus (GDM) is defined as carbohydrate intolerance that develops during pregnancy, usually during second or third trimester of gestation [4]. Women with GDM have an increased risk of developing diabetes (predominantly type 2 diabetes) later in life. It is estimated that up to 70% of women with GDM will develop diabetes within 22–28 years after pregnancy [4,5,6,7].
The incidence of GDM increases with the same risk factors seen for type 2 diabetes such as obesity, sedentary lifestyle, and increasing reproductive age of women [4,5,6,7].
The initial criteria for diagnosis of GDM were established more than 40 years ago to identify women at a high risk for development of diabetes after pregnancy [8,9,10]. The two-step screening approach to testing for GDM is currently recommended by The American College of Obstetricians and Gynecologists [4] and The International Association of Diabetes and Pregnancy Study Groups (IADPSG) [10]. Overall, using the proposed IADPSG criteria, 18% of pregnant women in the United States are identified as having GDM [10].
The goal of the current study was to evaluate the risk of later development of diabetes mellitus, and cardiovascular and cerebrovascular diseases based on an epigenetic profile of cardiovascular/cerebrovascular disease associated microRNAs in whole peripheral blood of young and middle-aged mothers with a history of gestational diabetes mellitus (GDM) 3–11 years after the delivery. The hypothesis of the assessment of cardiovascular risk in women was based on the knowledge that a series of microRNAs play a role in the pathogenesis of diabetes mellitus and cardiovascular/cerebrovascular diseases (Table 1) [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170].
Table 1.
The role of differentially expressed microRNAs in mothers with a history of GDM in the pathogenesis of diabetes mellitus, cardiovascular/cerebrovascular diseases.
| miRBase ID | Gene Location on Chromosome |
Role in the Pathogenesis of Cardiovascular/Cerebrovascular Diseases |
|---|---|---|
| hsa-miR-1-3p | 20q13.3 18q11.2 [11] |
Acute myocardial infarction, heart ischemia, post-myocardial infarction complications [12], diabetes mellitus [13,14], vascular endothelial dysfunction [15] |
| hsa-miR-16-5p | 13q14.2 | Myocardial infarction [16,17], heart failure [18], acute coronary syndrome, cerebral ischaemic events [19], gestational diabetes mellitus [20,21], diabetes mellitus [22,23,24] |
| hsa-miR-17-5p | 13q31.3 [25,26] | Cardiac development [27], ischemia/reperfusion-induced cardiac injury [28], kidney ischemia-reperfusion injury [29], diffuse myocardial fibrosis in hypertrophic cardiomyopathy [30], acute ischemic stroke [31], coronary artery disease [32], adipogenic differentiation [33], gestational diabetes mellitus [20,21], diabetes mellitus [24,34] |
| hsa-miR-20a-5p | 13q31.3 [35] | Pulmonary hypertension [36], gestational diabetes mellitus [20,21,37], diabetic retinopathy [38], diabetes with abdominal aortic aneurysm [39] |
| hsa-miR-20b-5p | Xq26.2 [35] | Hypertension-induced heart failure [40], insulin resistance [41], T2DM [42,43], diabetic retinopathy [44] |
| hsa-miR-21-5p | 17q23.2 [45] | Homeostasis of the cardiovascular system [46], cardiac fibrosis and heart failure [47,48], ascending aortic aneurysm [49], regulation of hypertension-related genes [50], myocardial infarction [51], insulin resistance [41], T2DM [52], T2DM with major cardiovascular events [53], T1DM [54,55,56], diabetic nephropathy [57] |
| hsa-miR-23a-3p | 19p13.12 | Heart failure [58], coronary artery disease [59], cerebral ischemia-reperfusion [60], vascular endothelial dysfunction [15], small and large abdominal aortic aneurysm [61], obesity and insulin resistance [62] |
| hsa-miR-24-3p | 19p13.12 | Asymptomatic carotid stenosis [63], familial hypercholesterolemia and coronary artery disease [64], angina pectoris [65], ischemic dilated cardiomyopathy [66], small and large abdominal aortic aneurysm [61], myocardial ischemia/reperfusion [67,68], diabetes mellitus [14,24,52,54] |
| hsa-miR-26a-5p | 3p22.2 12q14.1 [69] |
Heart failure, cardiac hypertrophy [70], myocardial infarction [51,71,72], ischemia/reperfusion injury [73], pulmonary arterial hypertension [74], T1DM [75], diabetic nephropathy [57] |
| hsa-miR-29a-3p | 7q32.3 | Ischemia/reperfusion-induced cardiac injury [76], cardiac cachexia, heart failure [77], atrial fibrillation [78], diffuse myocardial fibrosis in hypertrophic cardiomyopathy [30], coronary artery disease [79], pulmonary arterial hypertension [74], gestational diabetes mellitus [80], diabetes mellitus [13,23,81,82] |
| hsa-miR-100-5p | 11q24.1 | Failing human heart, idiopathic dilated cardiomyopathy, ischemic cardiomyopathy [66], regulation of hypertension-related genes [50], T1DM [54] |
| hsa-miR-103a-3p | 5q34 20p13 [83] |
Hypertension [84], hypoxia-induced pulmonary hypertension [85], myocardial ischemia/reperfusion injury, acute myocardial infarction [84], ischemic dilated cardiomyopathy [66], obesity, regulation of insulin sensitivity [86], T1DM [87] |
| hsa-miR-125b-5p | 11q24.1 21q21.1 [88] |
Acute ischemic stroke [89], acute myocardial infarction [90,91], ischemic dilated cardiomyopathy [66], ascending aortic aneurysm [49], gestational diabetes mellitus [92], T1DM [93,94], T2DM [95] |
| hsa-miR-126-3p | 9q34.3 [96] | Acute myocardial infarction [72], T2DM [53,97], T2DM with major cardiovascular events [53], gestational diabetes mellitus [98] |
| hsa-miR-130b-3p | 22q11.21 | Hypertriglyceridemia [99,100], intracranial aneurysms [101], hyperacute cerebral infarction [102], T2DM [52,103,104], gestational diabetes mellitus [98] |
| hsa-miR-133a-3p | 18q11.2 20q13.33 [105] |
Heart failure [106], myocardial fibrosis in hypertrophic cardiomyopathy [30,107], arrhythmogenesis in the hypertrophic and failing hearts [108,109], coronary artery calcification [110], ascending aortic aneurysm [49], diabetes mellitus [13,14] |
| hsa-miR-143-3p | 5q33 | Intracranial aneurysms [111], coronary heart disease [112], myocardial infarction [113], myocardial hypertrophy [114], dilated cardiomyopathy [115], pulmonary arterial hypertension [116], acute ischemic stroke [89], ascending aortic aneurysm [49] |
| hsa-miR-145-5p | 5q33 | Hypertension [117,118], dilated cardiomyopathy [119], myocardial infarction [120,121], stroke [121], acute cerebral ischemic/reperfusion [122], T2DM [24,123], T1DM [52], diabetic retinopathy [124], gestational diabetes mellitus [125] |
| hsa-miR-146a-5p | 5q33.3 [126,127] | Angiogenesis [128], hypoxia, ischemia/reperfusion-induced cardiac injury [129], myocardial infarction [17], coronary atherosclerosis, coronary heart disease in patients with subclinical hypothyroidism [130], acute ischemic stroke, acute cerebral ischemia [131], T2DM [24,52], T1DM [75], diabetic nephropathy [57] |
| hsa-miR-181a-5p | 1q32.1 9q33.3 [132] |
Regulation of hypertension-related genes [50], atherosclerosis [132], metabolic syndrome, coronary artery disease [133], non-alcoholic fatty liver disease [134], ischaemic stroke, transient ischaemic attack, acute myocardial infarction [135,136], obesity and insulin resistance [62,132,133], T1DM [52,137], T2DM [132,136] |
| hsa-miR-195-5p | 17p13.1 [138] | Cardiac hypertrophy, heart failure [139,140], abdominal aortic aneurysms [141], aortic stenosis [142], T2DM [123], gestational diabetes mellitus [143] |
| hsa-miR-199a-5p | 1q24.3 19p13.2 |
Hypertension [144], congenital heart disease [145], pulmonary artery hypertension [146], unstable angina [147], diabetic retinopathy [148], T1DM, T2DM, gestational diabetes mellitus [149] |
| hsa-miR-221-3p | Xp11.3 | Asymptomatic carotid stenosis [63], cardiac amyloidosis [150], heart failure [151], atherosclerosis [152,153], aortic stenosis [154], acute myocardial infarction [155], acute ischemic stroke [156], focal cerebral ischemia [157], pulmonary artery hypertension [158], obesity [159] |
| hsa-miR-342-3p | 14q32.2 | Cardiac amyloidosis [150], obesity [160], T1DM [52,149,161], T2DM [149,162,163], GDM [149], endothelial dysfunction [164] |
| hsa-miR-499a-5p | 20q11.22 | Myocardial infarction [17,165], hypoxia [166], cardiac regeneration [167], vascular endothelial dysfunction [15] |
| hsa-miR-574-3p | 4p14 | Myocardial infarction [168], coronary artery disease [100], cardiac amyloidosis [150], stroke [169], T2DM [104,170] |
Postpartal epigenetic profiling of microRNAs (miR-1-3p, miR-16-5p, miR-17-5p, miR-20a-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-29a-3p, miR-92a-3p, miR-100-5p, miR-103a-3p, miR-125b-5p, miR-126-3p, miR-130b-3p, miR-133a-3p, miR-143-3p, miR-145-5p, miR-146a-5p, miR-155-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-210-3p, miR-221-3p, miR-342-3p, miR-499a-5p, and miR-574-3p) known to be involved in the onset of insulin resistance and diabetes, dyslipidemia, hypertension, vascular inflammation, atherosclerosis, angiogenesis, coronary artery disease, myocardial infarction and heart failure, stroke, intracranial aneurysm, pulmonary arterial hypertension, and peripartum cardiomyopathy was the subject of our interest.
MicroRNAs, small noncoding RNAs, are known to regulate gene expression at the posttranscriptional level by blocking translation or degrading of target messenger RNA [171].
To the best of our present knowledge, no study on expression profiling of microRNAs associated with diabetes mellitus, and cardiovascular and cerebrovascular diseases in whole peripheral blood of mothers after pregnancies affected by gestational diabetes mellitus has been carried out.
2. Results
MicroRNA gene expression was compared between mothers after normal and GDM-complicated pregnancies in maternal whole peripheral blood 3 to 11 years postpartum. Just the results, when the complicated cases reached a statistical significance, are presented below.
2.1. Expression Profile of MicroRNAs Associated with Diabetes Mellitus and Cardiovascular/Cerebrovascular Diseases in Mothers after GDM Pregnancies
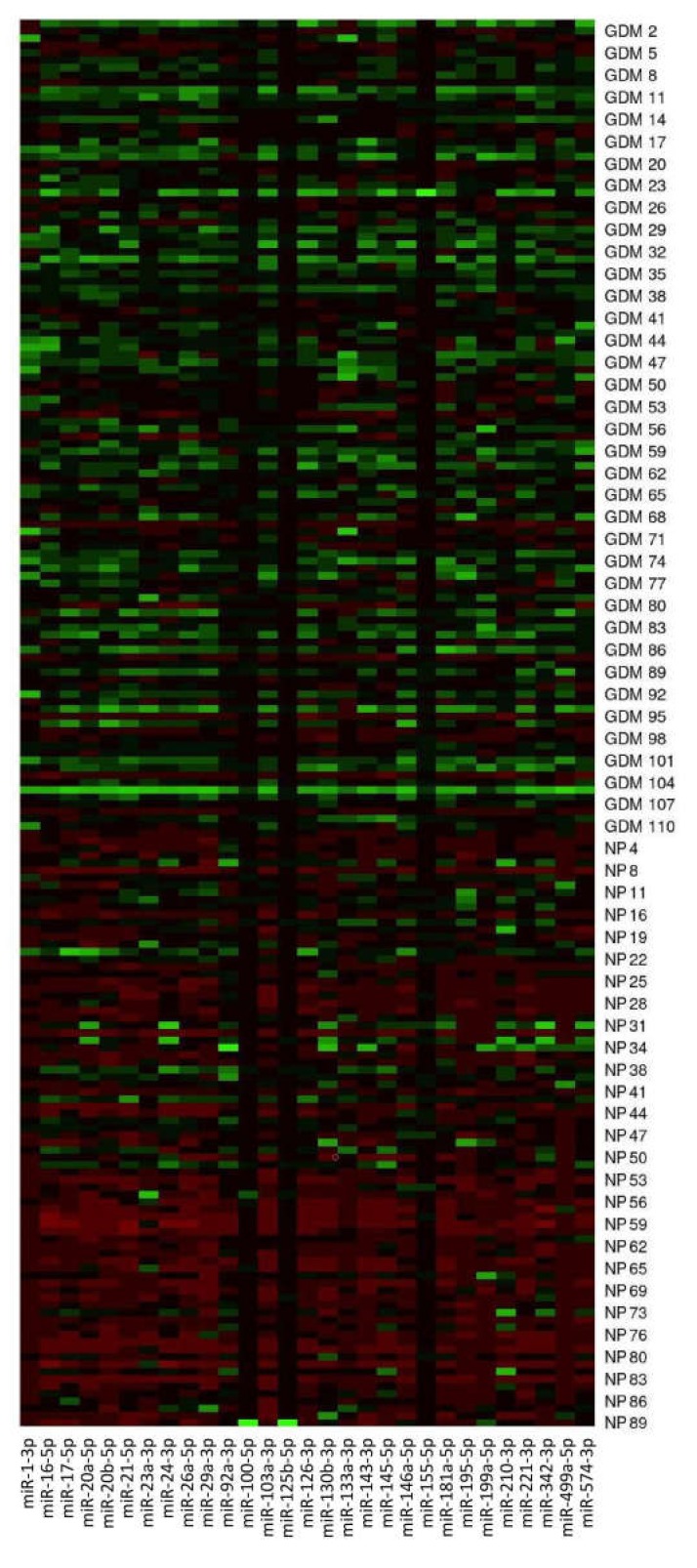
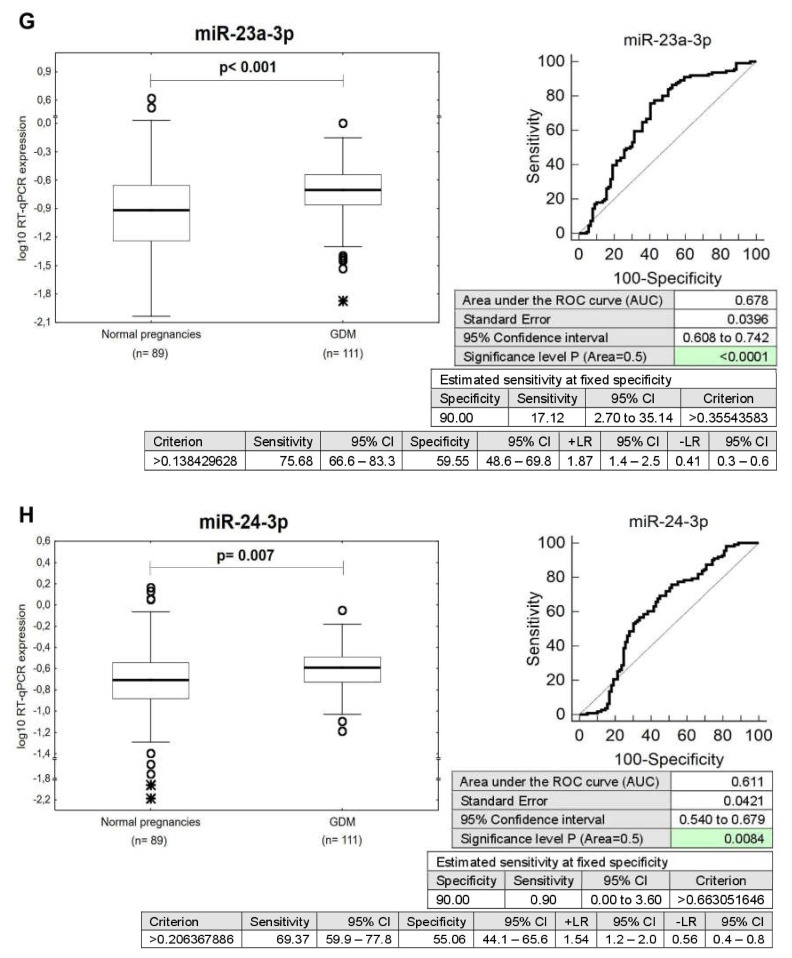
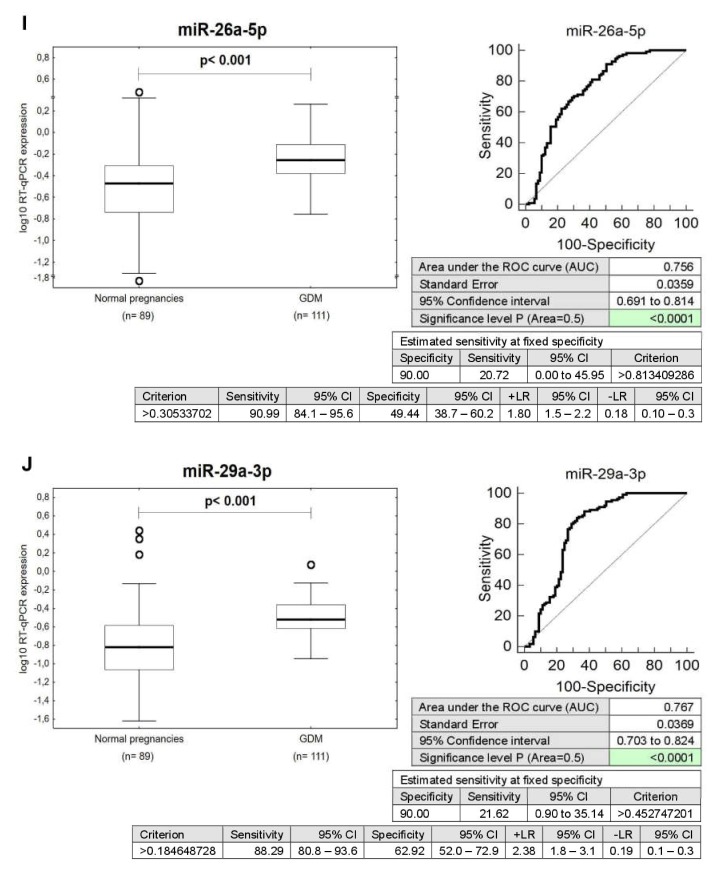
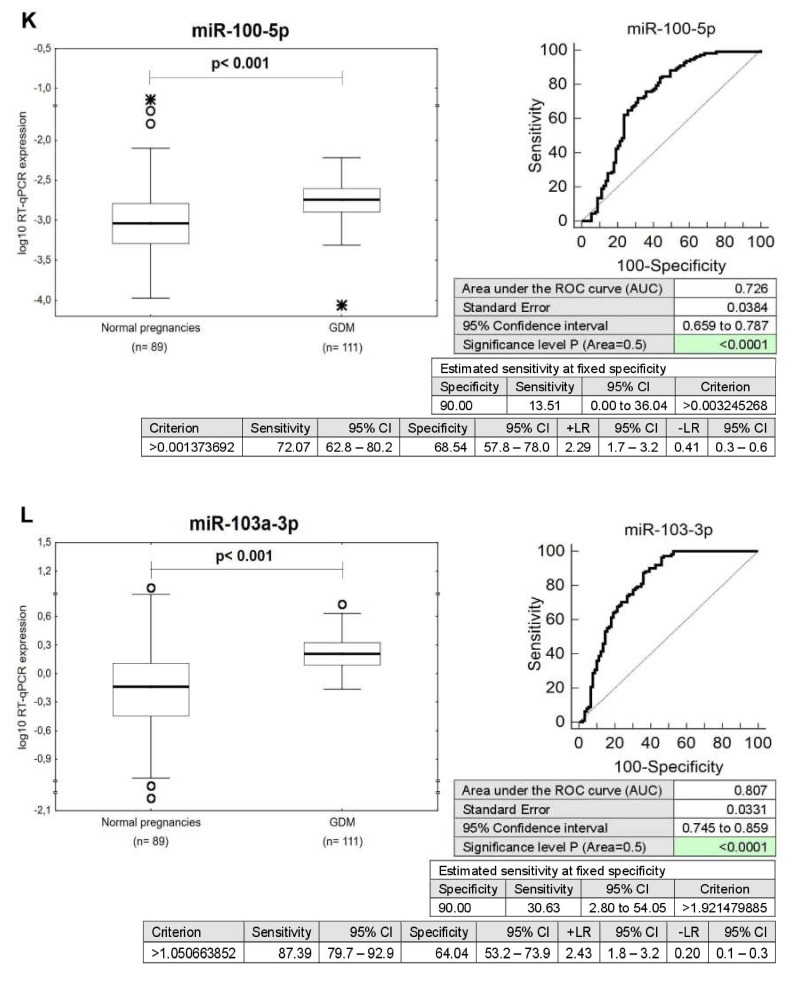
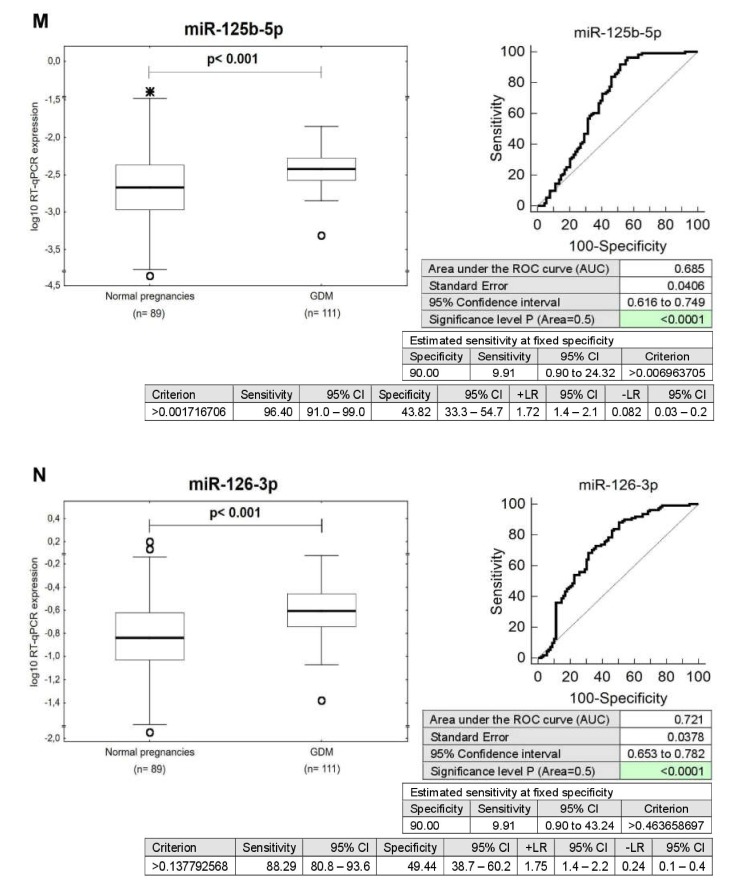
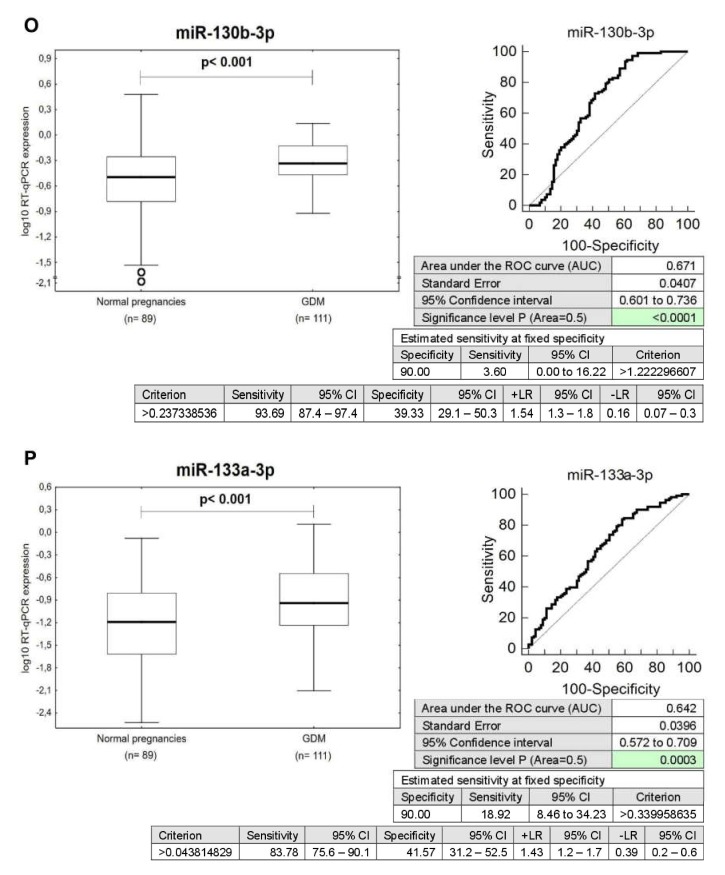
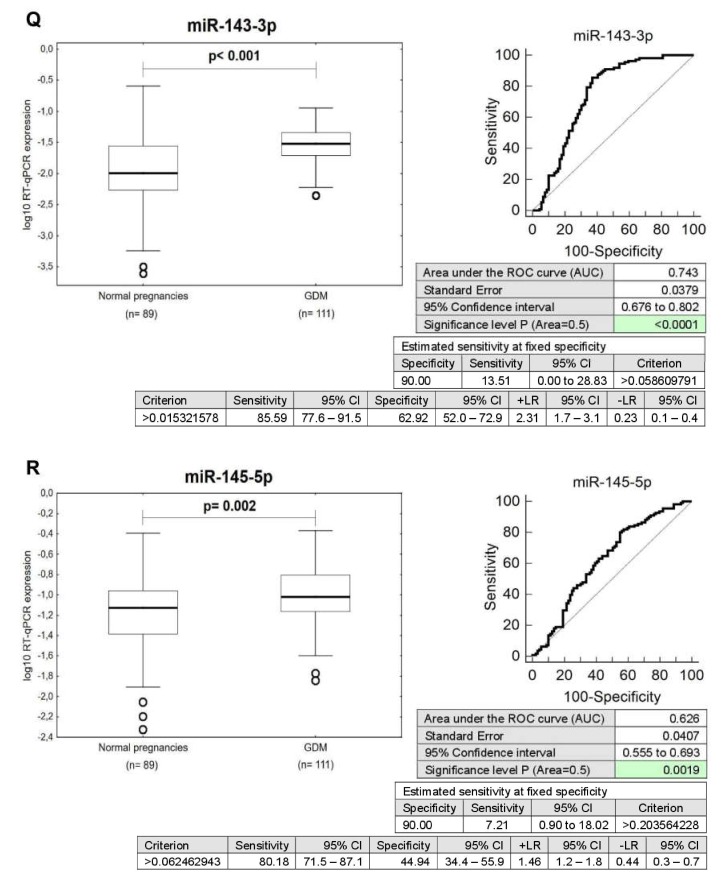
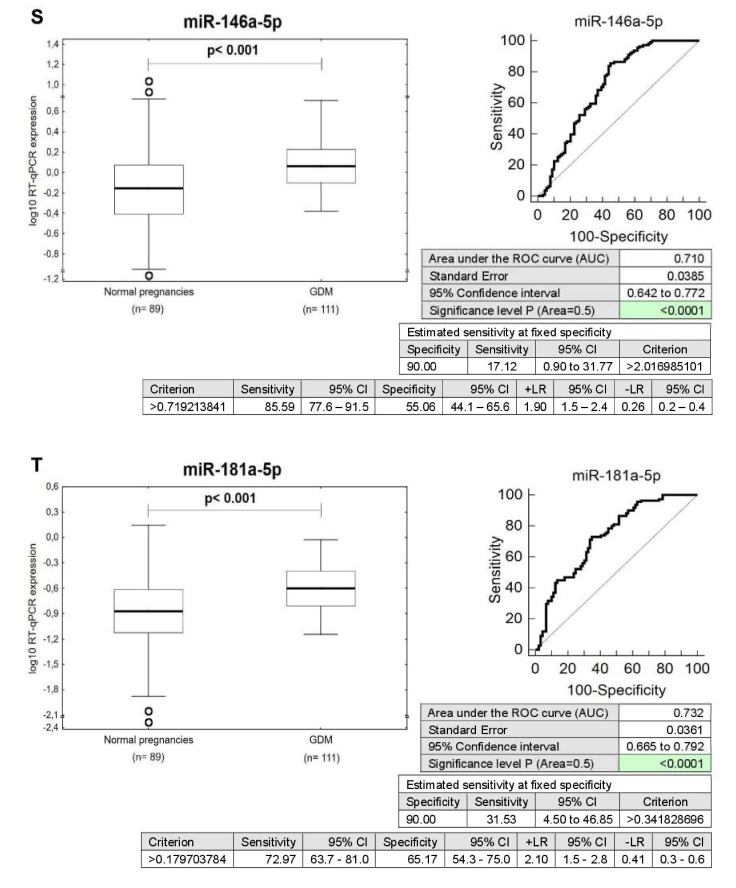
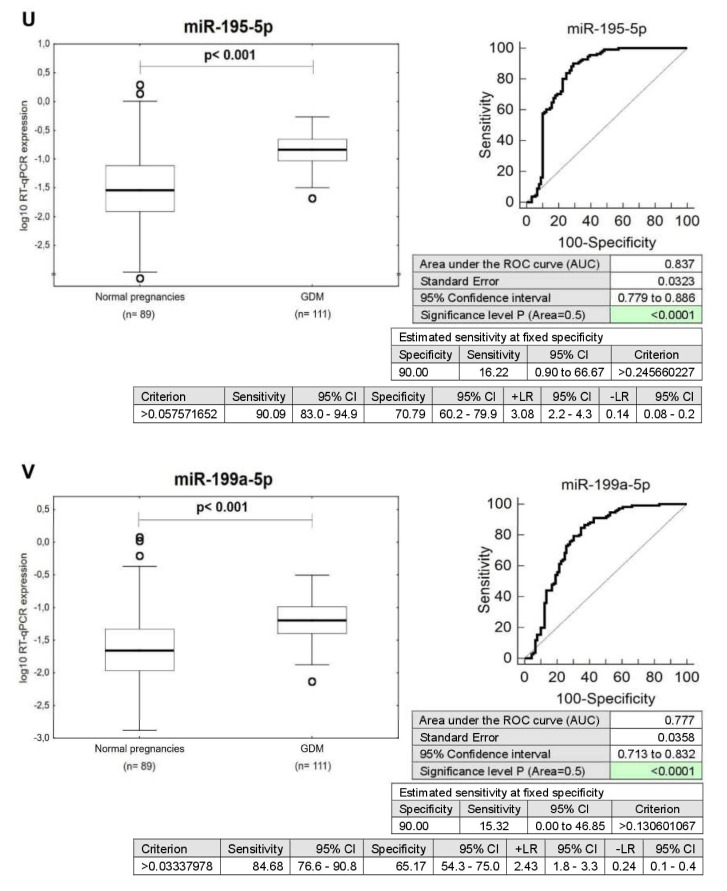
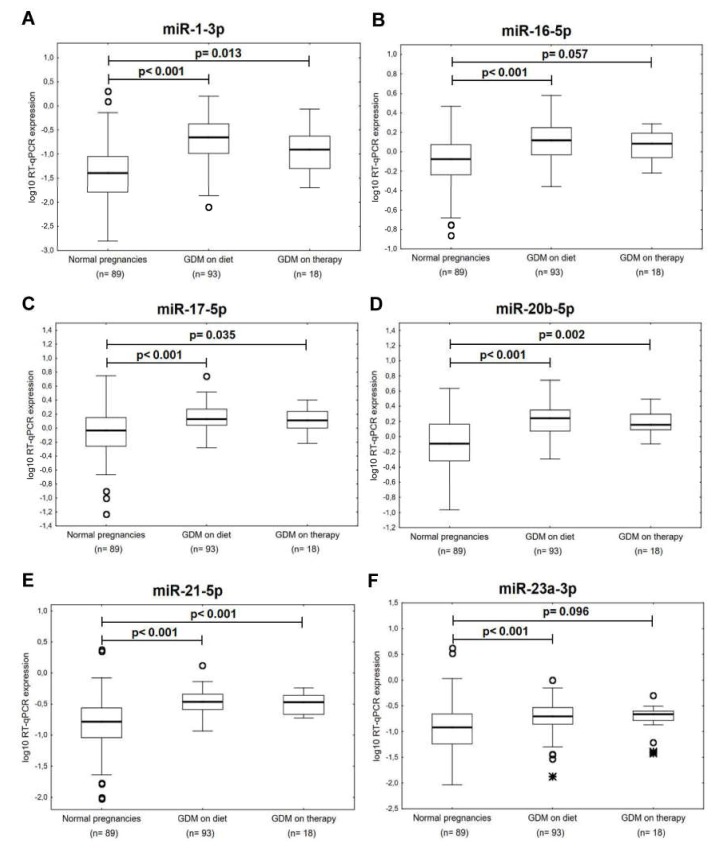
The expression of miR-1-3p (p < 0.001), miR-16-5p (p < 0.001), miR-17-5p (p < 0.001), miR-20a-5p (p < 0.001), miR-20b-5p (p < 0.001), miR-21-5p (p < 0.001), miR-23a-3p (p < 0.001), miR-24-3p (p = 0.007), miR-26a-5p (p < 0.001), miR-29a-3p (p < 0.001), miR-100-5p (p < 0.001), miR-103a-3p (p < 0.001), miR-125b-5p (p < 0.001), miR-126-3p (p < 0.001), miR-130b-3p (p < 0.001), miR-133a-3p (p < 0.001), miR-143-3p (p < 0.001), miR-145-5p (p = 0.002), miR-146a-5p (p < 0.001), miR-181a-5p (p < 0.001), miR-195-5p (p < 0.001), miR-199a-5p (p < 0.001), miR-221-3p (p < 0.001), miR-342-3p (p = 0.003), miR-499a-5p (p < 0.001), and miR-574-3p (p < 0.001) differed significantly between the control group and women previously affected with GDM. These microRNAs were upregulated in GDM-affected patients (Figure 1 and Figure 2).
Figure 1.
Postpartal microRNA expression profile in mothers with a history of GDM pregnancies. MicroRNA gene expression data (2−ΔΔCt) are visualized using the heat map. In this setting, each row represents a sample (GDM1–GDM111, NP1–NP89) and each column represents a microRNA gene. The color and intensity of the boxes are used to represent changes of gene expression (2−ΔΔCt). Green color indicates upregulation, and red color indicates downregulation. NP, normal pregnancies.
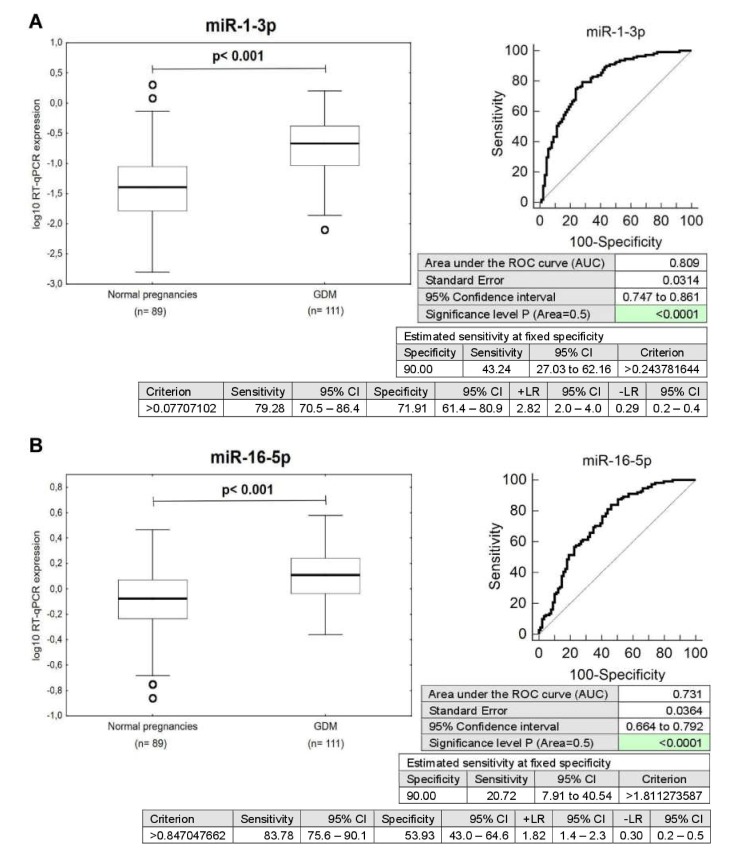
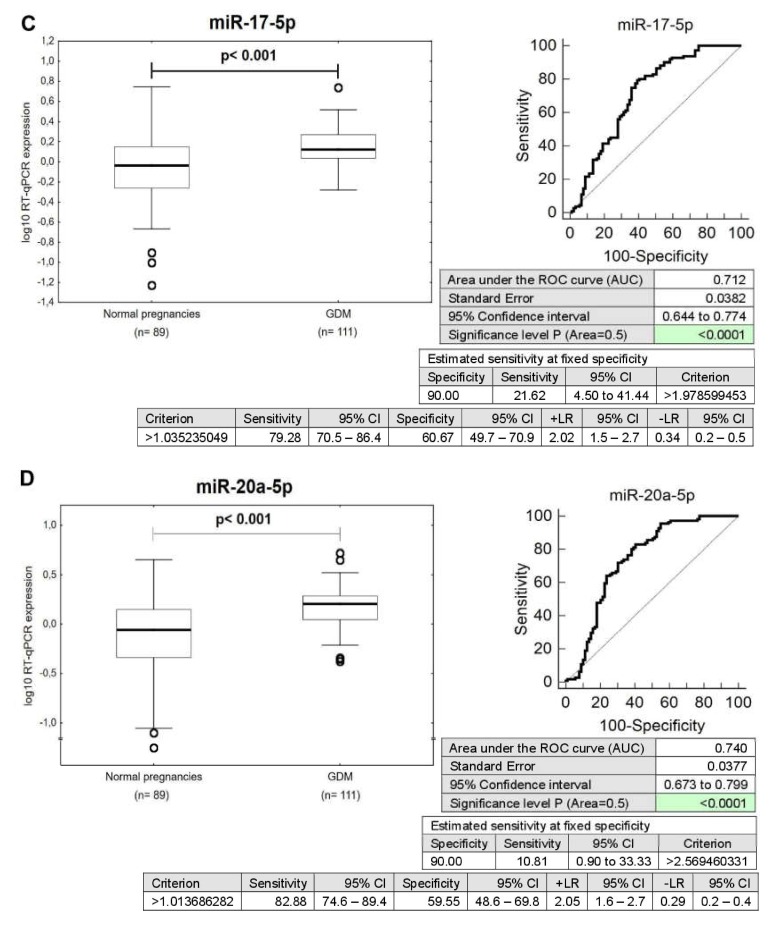
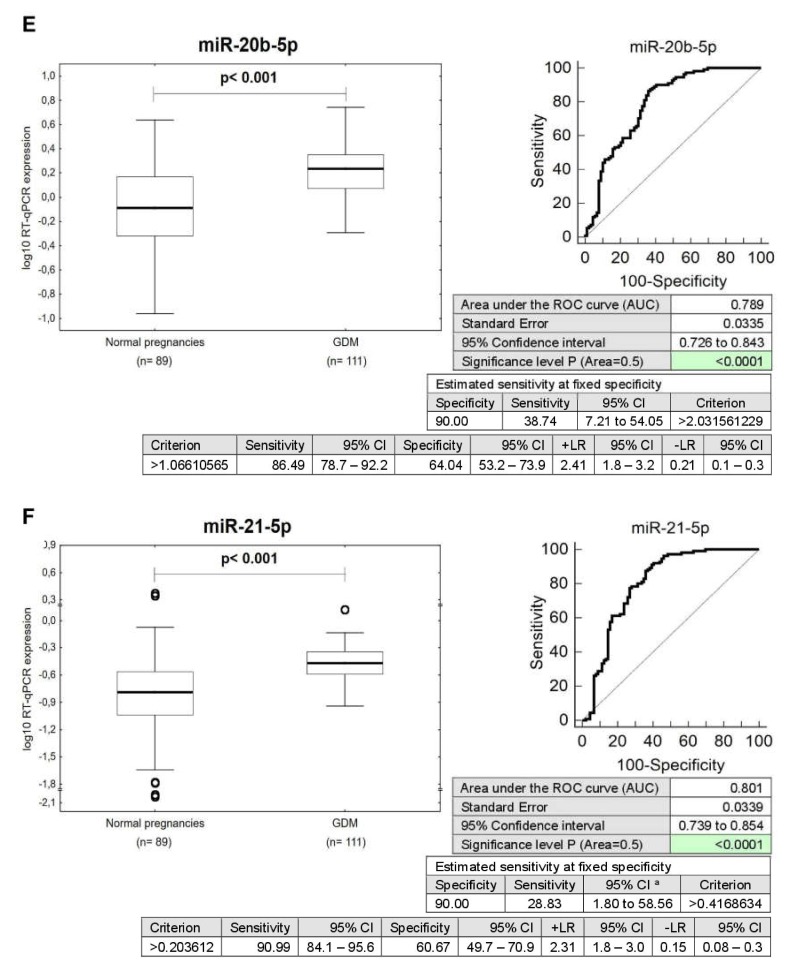
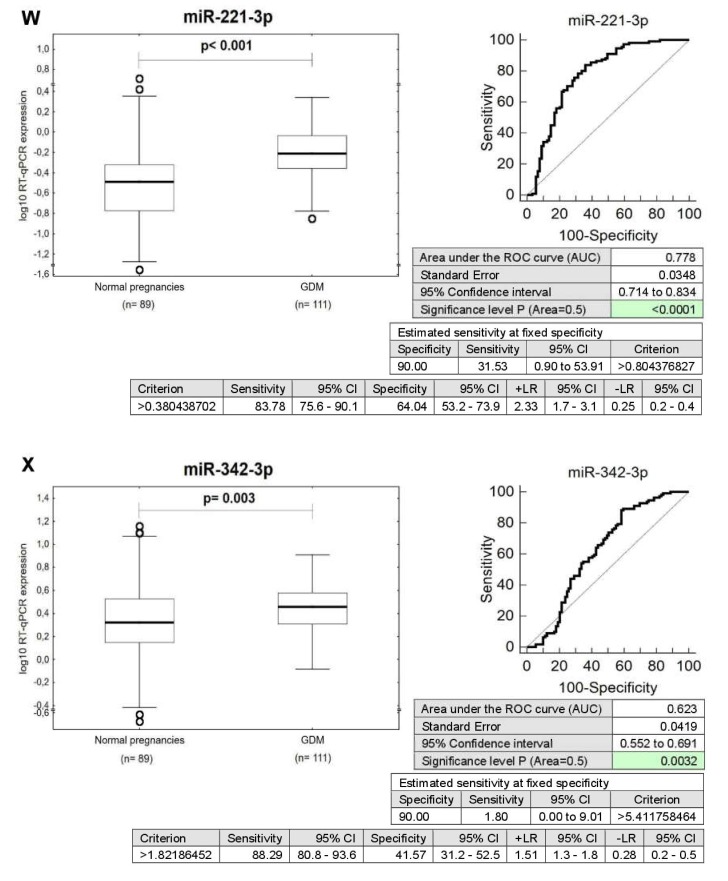
Figure 2.
Postpartal microRNA expression profile in mothers with a history of GDM pregnancies. (A–Z) Upregulation of miR-1-3p, miR-16-5p, miR-17-5p, miR-20a-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-29a-3p, miR-100-5p, miR-103a-3p, miR-125b-5p, miR-126-3p, miR-130b-3p, miR-133a-3p, miR-143-3p, miR-145-5p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, miR-342-3p, miR-499a-5p, and miR-574-3p was observed in mothers after GDM pregnancies when the comparison to the controls was performed using Mann–Whitney test. Receivers operating characteristic (ROC) curves were constructed to calculate the area under the curve (AUC), the best cut-off point (criterion), the sensitivity, specificity, likelihood ratio positive (LR+), and likelihood ratio negative (LR−) for particular microRNA. In addition, respective sensitivity at 90.0% specificity was reported for miR-1-3p (43.24%), miR-16-5p (20.72%), miR-17-5p (21.62%), miR-20a-5p (10.81%), miR-20b-5p (38.74%), miR-21-5p (28.83%), miR-23a-3p (17.12%), miR-24-3p (0.90%), miR-26a-5p (20.72%), miR-29a-3p (21.62%), miR-100-5p (13.51%), miR-103a-3p (30.63%), miR-125b-5p (9.91%), miR-126-3p (9.91%), miR-130b-3p (3.60%), miR-133a-3p (18.92%), miR-143-3p (13.51%), miR-145-5p (7.21%), miR-146a-5p (17.12%), miR-181a-5p (31.53%), miR-195-5p (16.22%), miR-199a-5p (15.32%), miR-221-3p (31.53%), miR-342-3p (1.8%), miR-499a-5p (28.83%), and miR-574-3p (10.81%).
The ROC curve analysis confirmed a significant upregulation of these particular microRNAs for mothers with a history of GDM when the comparison to the controls was performed (Figure 1).
The very good sensitivity at 10.0% FPR for miR-1-3p (43.24%), miR-16-5p (20.72%), miR-17-5p (21.62%), miR-20b-5p (38.74%), miR-21-5p (28.83%), miR-23a-3p (17.12%), miR-26a-5p (20.72%), miR-29a-3p (21.62%), miR-103a-3p (30.63%), miR-133a-3p (18.92%), miR-146a-5p (17.12%), miR-181a-5p (31.53%), miR-195-5p (16.22%), miR-199a-5p (15.32%), miR-221-3p (31.53%), and miR-499a-5p (28.83%) is found (Figure 2).
However, despite the upregulation of microRNAs, the poor sensitivity at 10.0% FPR for miR-20a-5p (10.81%), miR-24-3p (0.90%), miR-100-5p (13.51%), miR-125b-5p (9.91%), miR-126-3p (9.91%), miR-130b-3p (3.60%), miR-143-3p (13.51%), miR-145-5p (7.21%), miR-342-3p (1.8%), and miR-574-3p (10.81%) was detected, therefore, these particular microRNAs were not further used for diabetes mellitus and cardiovascular risk assessment in mothers previously affected with GDM (Figure 2).
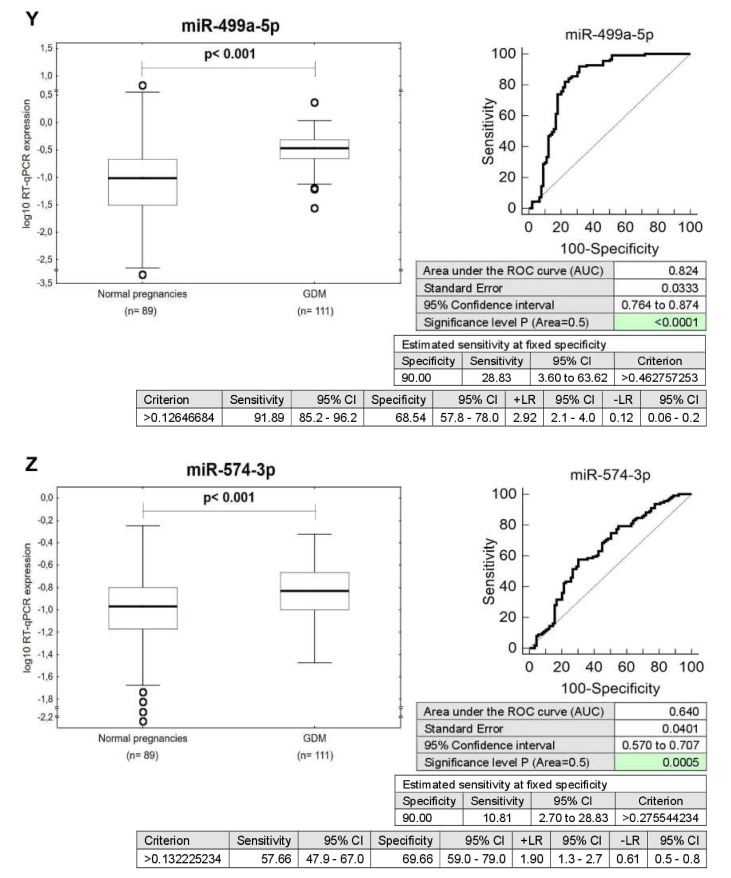
Combined screening of miR-1-3p, miR-16-5p, miR-17-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-26a-5p, miR-29a-3p, miR-103a-3p, miR-133a-3p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p showed the highest accuracy for mothers with a prior exposure to GDM (AUC 0.900, p < 0.001, sensitivity 77.48%, specificity 93.26%, cut off > 0.611270413). It was able to identify 77.48% of mothers with an increased cardiovascular risk at 10.0% FPR (Figure 3).
Figure 3.
Combined postpartal screening of microRNAs in the identification of mothers with a history of GDM at an increased cardiovascular risk. Postpartal combined screening of miR-1-3p, miR-16-5p, miR-17-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-26a-5p, miR-29a-3p, miR-103a-3p, miR-133a-3p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p showed the highest accuracy for the identification of mothers with a prior exposure to GDM at a higher risk of later development of diabetes mellitus, and cardiovascular/cerebrovascular diseases.
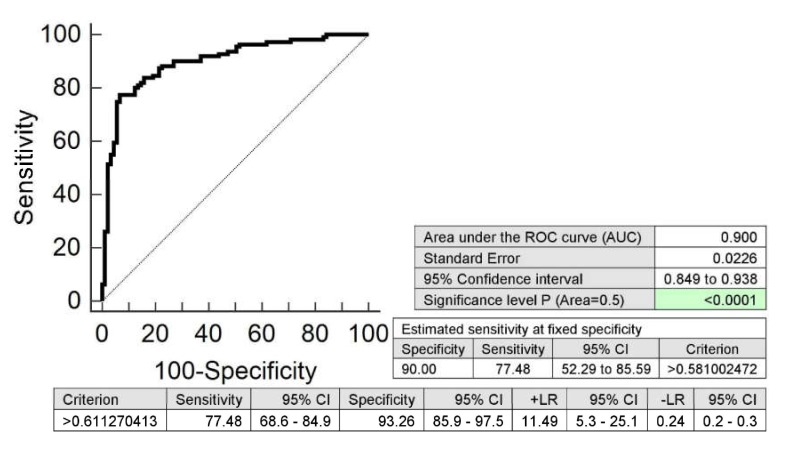
2.2. Expression Profile of MicroRNAs Associated with Diabetes Mellitus and Cardiovascular/Cerebrovascular Diseases in Mothers after GDM Pregnancies with Regard to the Treatment Strategies (Diet Only and/or Diet and Therapy)
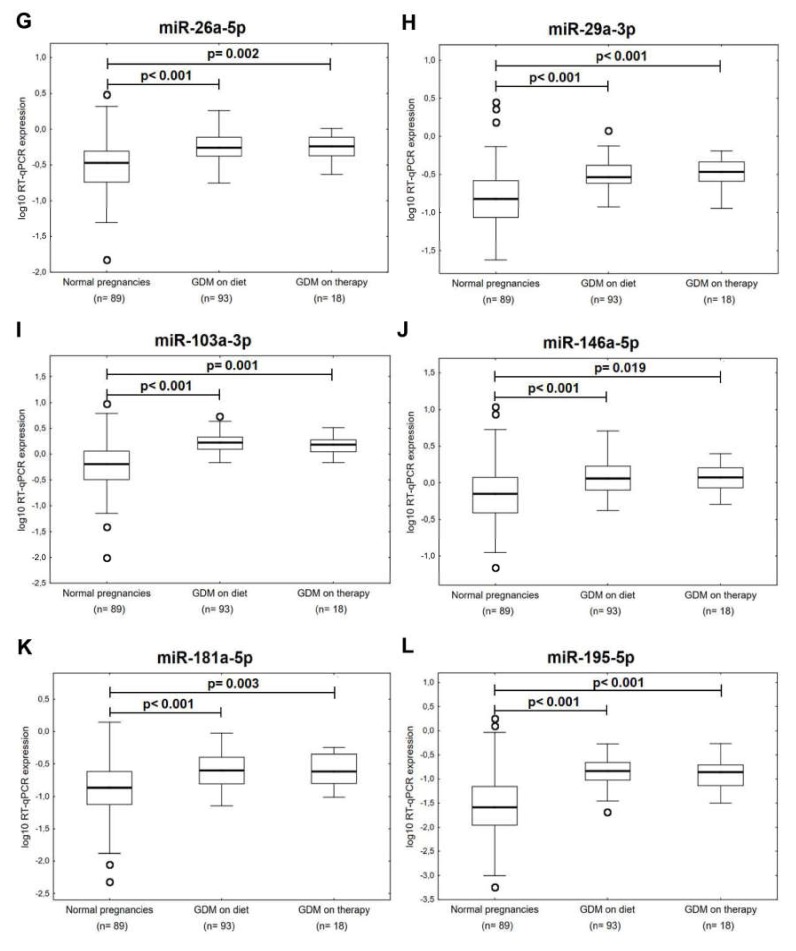
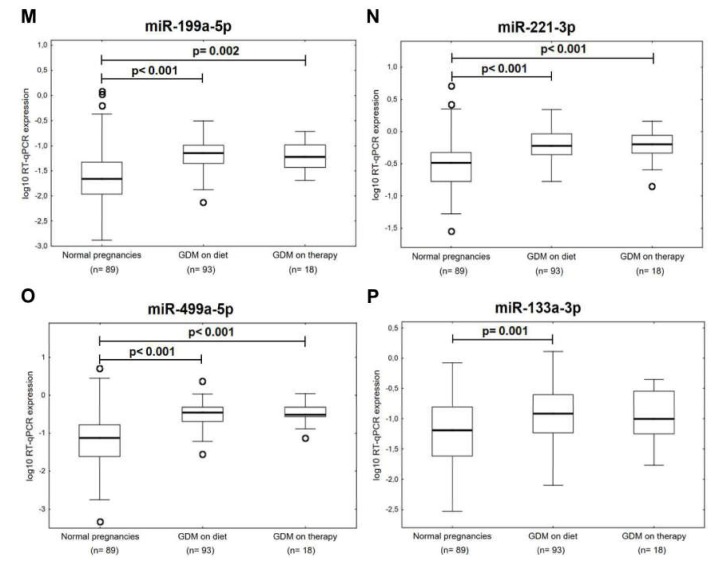
Concurrently, it was observed that the expression of miR-1-3p (p < 0.001, p = 0.013), miR-16-5p (p < 0.001, p = 0.057), miR-17-5p (p < 0.001, p = 0.035), miR-20b-5p (p < 0.001, p = 0.002), miR-21-5p (p < 0.001, p < 0.001), miR-23a-3p (p < 0.001, p = 0.096), miR-26a-5p (p < 0.001, p = 0.002), miR-29a-3p (p < 0.001, p < 0.001), miR-103a-3p (p < 0.001, p = 0.001), miR-146a-5p (p < 0.001, p = 0.019), miR-181a-5p (p < 0.001, p = 0.003), miR-195-5p (p < 0.001, p < 0.001), miR-199a-5p (p < 0.001, p = 0.002), miR-221-3p (p < 0.001, p < 0.001), and miR-499a-5p (p < 0.001, p < 0.001) differed significantly or showed a trend toward statistical significance between the groups of mothers affected with GDM regardless of the treatment strategies (diet only and/or the combination of diet and therapy) and the controls (Figure 4). Nevertheless, miR-133a-3p was upregulated just in the group of patients previously affected with GDM on diet only (p = 0.001) (Figure 4).
Figure 4.
Postpartal microRNA expression profile in mothers with a history of GDM pregnancies with regard to the treatment strategies. (A–O) Upregulation or trend towards upregulation of miR-1-3p, miR-16-5p, miR-17-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-26a-5p, miR-29a-3p, miR-103a-3p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p was observed in mothers after GDM pregnancies regardless of the treatment strategies (diet only and/or the combination of diet and therapy). (P) Upregulation of miR-133a-3p was observed in mothers after GDM pregnancies on diet only.
Due to a low number of women on the diet and therapy (n = 18) in our studied group of patients previously affected with GDM, we decided not to perform ROC curve analysis for particular groups of patients regarding the GDM treatment strategies (diet only and/or combination of diet and therapy).
No difference in microRNA expression profiles was observed between the groups of mothers with a history of GDM on diet only and on the combination of diet and therapy (p = 1.0 for nearly all examined microRNAs).
2.3. Information on MicroRNA-Gene-Biological Pathway Interactions
The extensive file of predicted targets of all microRNAs aberrantly expressed in whole peripheral blood of mothers with a history of GDM indicates that a large group of genes is involved in biological pathways related to insulin signaling, type 1 diabetes mellitus, and type 2 diabetes mellitus (Table 2, Table 3 and Table 4).
Table 2.
A list of predicted targets of appropriate microRNAs dysregulated in whole peripheral blood of patients with a history of GDM in relation to insulin signaling pathway using miRWalk2.0 database.
| microRNA | Predicted Targets |
|---|---|
| miR-1 | CALM2, CBL, IKBKB, KRAS, PHKG2, PIK3R5, PTPN1, PTPRF, TRIP10 |
| miR-16-5p | IKBKB, PHKA1, PRKAR1A, MAP2K1, RAF1, IRS4, MKNK1, EXOC7, FASN |
| miR-17-5p | PHKA2, CRK, GRB2, PDE3A, PHKG1, PIK3R2, PRKAA2, PRKAR2A, MAPK9, PRKX, PPP1R3B, HK1, PCK1, SREBF1 |
| miR-20a-5p | BRAF, MKNK2, CRK, SLC2A4, TRIP10, KRAS, PCK1 |
| miR-20b-5p | CRK, GRB2, PDE3A, PHKA2, PHKG1, PIK3R2, PRKAA2, PRKAR2A, MAPK9, PRKX, PPP1R3B, HK1, PCK1, SREBF1 |
| miR-21-5p | PPP1R3A, PPP1R3D |
| miR-23a-3p | G6PC, IRS2, IKBKB, PIK3CB, FASN, PRKAG3 |
| miR-24-3p | IKBKB, PIK3CB, PTPRF, SHC2, INPP5K, PHKG1, PRKAG3 |
| miR-26a-5p | G6PC, MKNK2, GYS2, PPP1R3D, RHOQ, KRAS, PRKAG1, PYGL |
| miR-29a-3p | NRAS, EIF4E2, CALM3 |
| miR-100-5p | MTOR |
| miR-103a-3p | FAS, RAPGEF1, PDE3B, ACACB, PHKAR1A, PRKCI, IRS2, LIPE, PRKC2, MAPK3, TRIP10, CBLC, CALML5 |
| miR-125b-5p | PHKA1, RAF1, ACACB, FLOT2, HK2, EIF4E2, PHKG1 |
| miR-126-3p | TSC1 |
| miR-130b-3p | RPS6KB1, MAP2K1, SOS2, FLOT2, EXOC7, PHKG2, PIK3CA, PRKC2, TSC2, PRKAG3 |
| miR-133a-3p | PRKAB1 |
| miR-143-3p | FOXO1, KRAS, HK2, PHKG2, MAPK3, MAPK9, SREBF1 |
| miR-145-5p | IRS1, IRS2, PIK3R5, PRKAG3 |
| miR-181a-5p | NRAS, AKT3, SOCS4, HK2, PDE3B, PPP1R3C, PRKAR2A, MAPK1, PPP1R3D, PRKAA1 |
| miR-195-5p | IKBKB, PHKA1, PRKAR1A, MAP2K1, RAF1, IRS4, MKNK1, EXOC7, FASN |
| miR-199a-5p | PRKX, PCK1, IRS1, SLC2A4, MAPK9, RHEB, PRKAR1A |
| miR-221-3p | AKT3, PIK3CD, MAPK10 |
| miR-342-3p | PDPK1, INSR, PHKG2, EIF4E2, PIK3CD, RPS6KB2 |
| miR-499a-5p | AKT2, CRK, KRAS, PIK3CD, PRKAR1A, SOS2 |
| miR-574-3p | PRKCZ, HK1 |
Table 3.
A list of predicted targets of appropriate microRNAs dysregulated in whole peripheral blood of patients with a history of GDM in relation to type 1 diabetes mellitus pathway using miRWalk2.0 database.
| microRNA | Predicted Targets |
|---|---|
| miR-1 | CD28, LTA |
| miR-16-5p | HLA-DQA1 |
| miR-17-5p | FASLG, CD28, HLA-DQA, GAD2, HLA-DPA1 |
| miR-20a-5p | IL12A |
| miR-20b-5p | HLA-DOA, FASLG, CD28, HLA-DPA1, GAD2 |
| miR-21-5p | HLA-DPB1, FASLG, IL12A |
| miR-23a-3p | IFNG |
| miR-24-3p | CD28, CD86, IFNG, FASLG, IL1B, HLA-DOA |
| miR-26a-5p | HLA-DPB1, HLA-DPA1, HLA-A, IFNG |
| miR-29a-3p | HLA-DQA2 |
| miR-103a-3p | HLA-DPB1, CD80 |
| miR-125b-5p | PRF-1 |
| miR-130b-3p | HLA-DOA, HLA-DQB1, HLA-A, HLA-B, HLA-C, HLA-G |
| miR-133a-3p | HLA-DOA, CD28, GAD2, LTA |
| miR-143-3p | HLA-DOA, HLA-DPB1, HLA-DPA1, IFNG, CD28 |
| miR-146a-5p | CD80, CD86, PRF1, ICA1, HLA-C, GAD2 |
| miR-181a-5p | IL2, HLA-E, IL1A |
| miR-195-5p | HLA-DQA1 |
| miR-199a-5p | G2MB, ICA1,TNF |
| miR-221-3p | HLA-DQA1, PTPRN |
| miR-342-3p | PTPRN2, HLA-A, HLA-F |
Table 4.
A list of predicted targets of appropriate microRNAs dysregulated in whole peripheral blood of patients with a history of GDM in relation to type 2 diabetes mellitus pathway using miRWalk2.0 database.
| microRNA | Predicted Targets |
|---|---|
| miR-16-5p | CACNA1E, IKBKB, IRS4 |
| miR-17-5p | PIK3R2, MAPK9, HK1 |
| miR-20a-5p | SLC2A4 |
| miR-20b-5p | MAPK9, HK1 |
| miR-23a-3p | IRS2, IKBKB, PIK3CB |
| miR-24-3p | IKBKB, PIK3CB, KCNJ11 |
| miR-26a-5p | PRKCD |
| miR-29a-3p | CACNA1A, CACNA1B |
| miR-100-5p | MTOR |
| miR-103a-3p | CACNA1E, IRS2, PRKCZ, MAPK3 |
| miR-125b-5p | HK2 |
| miR-130b-3p | PIK3CA, PRKCZ |
| miR-143-3p | CACNA1A, HK2, PRKCE, MAPK3, MAPK9 |
| miR-145-5p | IRS2, IRS1, PIK3R5 |
| miR-146a-5p | PRKCE |
| miR-181a-5p | SOCS4, HK2, MAPK1 |
| miR-195-5p | CACNA1E, IKBKB, IRS4 |
| miR-199a-5p | IRS1, SLC2A4, MAPK9, PKM, TNF, CACNA1G |
| miR-221-3p | PIK3CD, MAPK10 |
| miR-342-3p | CACNA1C, INSR, PIK3CD |
| miR-499a-5p | PRKCE, PIK3CD |
| miR-574-3p | PRKCZ, HK1 |
The miRWalk database and the predicted target module were used to provide information on predicted interactions between appropriate microRNAs and specific genes involved in human biological pathways such as insulin signaling, type 1 diabetes mellitus, and type 2 diabetes mellitus.
3. Discussion
Postpartal expression profile of cardiovascular/cerebrovascular disease associated microRNAs was assessed 3–11 years after the delivery in whole peripheral blood of young and middle-aged mothers with a prior exposure to GDM with the aim to identify a high-risk group of mothers at risk of later development of diabetes mellitus and cardiovascular and cerebrovascular diseases who would benefit from implementation of early primary prevention strategies and long-term follow-up. The hypothesis of the assessment of cardiovascular risk in women was based on the knowledge that a serious of microRNAs play a role in the pathogenesis of diabetes mellitus and cardiovascular/cerebrovascular diseases (Table 1) [11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170].
As expected, the expression profile of microRNAs differed between mothers affected with GDM and controls. Abnormal expression profile of multiple microRNAs was found in mothers with a history of GDM (26/29 studied microRNAs: miR-1-3p, miR-16-5p, miR-17-5p, miR-20a-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-29a-3p, miR-100-5p, miR-103a-3p, miR-125b-5p, miR-126-3p, miR-130b-3p, miR-133a-3p, miR-143-3p, miR-145-5p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, miR-342-3p, miR-499a-5p, and miR-574-3p).
Nevertheless, when the ROC curve analysis was performed, only 16/26 microRNAs (miR-1-3p, miR-16-5p, miR-17-5p, miR-20b-5p, miR-21-5p, miR-23a-3p, miR-26a-5p, miR-29a-3p, miR-103a-3p, miR-133a-3p, miR-146a-5p, miR-181a-5p, miR-195-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p) with aberrant postpartal expression profile in whole peripheral blood of mothers with a prior exposure to GDM showed a higher sensitivity, ranging from 15.32% to 43.24%, at 10.0% FPR.
Screening based on the combination of these particular microRNAs was superior over using individual microRNAs, since it showed the highest accuracy for mothers with a history of GDM (AUC 0.900, p < 0.001, sensitivity 77.48%, specificity 93.26%, cut off > 0.611270413). It was able to identify 77.48% mothers with an increased cardiovascular risk at 10.0% FPR.
Subsequently, epigenetic profile was compared between groups with regard to the treatment strategy (GDM on diet only, GDM on the combination of diet and therapy). The upregulation or trend towards upregulation of almost all studied microRNAs (with the exception of miR-133a-3p) was present in both groups of mothers affected with GDM regardless of the treatment strategies.
Previously, we demonstrated that pregnancy-related complications, such as gestational hypertension, preeclampsia, and/or fetal growth restriction, were associated with postpartum alterations in gene expression of cardiovascular/cerebrovascular disease-associated microRNAs [1,2,3].
Likewise, a previous occurrence of GH, as well as a previous occurrence of GDM, was associated with the upregulation of miR-20a-5p, miR-143-3p, miR-146a-5p, miR-181a-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p [1,2,3].
Moreover, the compilation of data resulting from our previous and current studies showed that the upregulation of miR-17-5p, miR-20b-5p, miR-29a-3p, and miR-126-3p was a mutual phenomenon observed in women with a prior exposure to GH, severe PE, and/or GDM [1,2,3].
In addition, a history of GH, early PE, and/or GDM was associated with postpartal upregulation of miR-1-3p and miR-17-5p. Parallel, women affected with GH and/or late PE showed similar postpartal expression profile (upregulation of miR-17-5p, miR-20b-5p, and miR-29a-3p) as women with a history of GDM [1,2,3].
Alike, as in women affected with severe PE and/or early PE, upregulation of miR-133a-3p was also present in women affected with GDM. Moreover, a history of severe PE and/or GDM was associated with upregulation of miR-130b-3p [1,2,3].
Furthermore, women with a history of GDM demonstrated upregulation of miR-100-5p, miR-125b-5p, miR-133a-3p, and miR-145-5p as women with prior exposure to PE and/or FGR with abnormal Doppler parameters [1,2,3].
On the other hand, our study revealed that upregulation of miR-16-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-103a-3p, miR-195-5p, miR-342-3p, and miR-574-3p represented a unique feature of aberrant expression profile of women with a prior exposure to GDM.
Interestingly, interaction network analysis via Cytoscale V.3.6.1 revealed that miR-145-5p together with miR-875-5p are upregulated microRNAs that target the most genes in gestational diabetes mellitus [125].
In addition, increased expression of miR-126-3p and miR-130b-3p was observed in human umbilical vein endothelial cells (HUVECs) derived from GDM patients [98].
Moreover, a set of circulating microRNAs associated with cardiovascular/cerebrovascular diseases (miR-16-5p, miR-17-5p, miR-20a-5p, miR-29a-3p, miR-125b-5p, and miR-195-5p) was reported by several independent studies [20,21,80,92,143,172,173] to be upregulated during various gestational ages in serum or plasma of mothers with already-diagnosed GDM or mothers who were destined to develop GDM later during pregnancy. The data resulting from these prenatally ongoing studies and interaction network analysis [20,21,80,92,98,125,143,172,173] may support our current finding referring to upregulated expression profile of these particular microRNAs in whole peripheral blood of women with a prior exposure to GDM.
In addition, from the portfolio of microRNAs we tested, just miR-16-5p, miR-17-5p, miR-20a-5p, and miR-29a were identified by other investigators as the most promising biomarkers of GDM or the best predictors of GDM, respectively [21,173], which is consistent with our current finding, since during the course of postpartum screening, miR-16-5p (20.72%), miR-17-5p (21.62%), and miR-29a-3p (21.62%) upregulation persisted in a larger proportion of women with a prior exposure to GDM.
In compliance with our study, which showed a low sensitivity of miR-20a-5p (10.81%) to select women with a higher cardiovascular risk after GDM gestation based on its upregulated profile, miR-20a-5p also added little value as the predictor of GDM due to its low predictive value based on its upregulated profile (ROC, AUC just 0.740) [21,173].
This study demonstrated that the dysregulation of at least four microRNAs (miR-16-5p, miR-17-5p, miR-29a-3p, and miR-195-5p) induced by GDM-complicated pregnancy in maternal circulation (plasma or serum) is present as well in circulation (whole peripheral blood) of a larger proportion of mothers (20.72%, 21.62%, 21.62%, 16.22%) with hindsight (3 to 11 years after the delivery) after the exposure to GDM.
It is obvious that changes in epigenome induced by GDM, which are persistently present in maternal circulation, may cause later development of diabetes mellitus and cardiovascular and cerebrovascular diseases in women with a prior exposure to GDM.
However, most of microRNAs, which were the subjects of our interest, have not yet been observed by other investigators to be dysregulated in maternal circulation (peripheral blood, plasma, or serum samples) of women with clinically established GDM or before the onset of GDM [20,21,37,80,92,143,149,172,173,174,175,176]. So, it is feasible that epigenetic profiles of a series of microRNAs have also been changing with time by force of various circumstances as a result of the interaction between genetic and environmental factors [177].
4. Materials and Methods
4.1. Participants
The study included a prospectively collected cohort of Caucasian mothers with a history of GDM (n = 111) and age-matched mothers after normal course of gestation (n = 89). In-person visit was conducted 3–11 years after the pregnancy ended. Of the 111 GDM pregnancies, 93 were on diet only and 18 were on the combination of diet and therapy (17 patients required insulin administration and in 1 patient metformin, an oral hypoglycemic agent, was prescribed).
The clinical characteristics of mothers after GDM-complicated pregnancies are presented in Table 5, Table 6 and Table 7.
Table 5.
Characteristics of cases and controls, pre-existing cardiovascular risk factors before gestation.
| Normotensive Term Pregnancies (n = 89) |
GDM on Diet Only (n = 93) |
GDM on Diet and Therapy (n = 18) |
|
|---|---|---|---|
| Rheumatoid arthritis | 0 (0%) | 1 (1.08%) | 0 (0%) |
| SLE | 0 (0%) | 0 (0%) | 0 (0%) |
| On blood pressure treatment | 0 (0%) | 0 (0%) | 0 (0%) |
| Hypercholesterolemia | 0 (0%) | 1 (1.08%) | 0 (0%) |
| Dispensarisation at Dpt. of Cardiology (valve problems and heart defects) |
0 (0%) | 4 (4.30%) Mitral valve prolapse Heart arrhythmia Hypertrophic cardiomyopathy AV nodal reentrant tachycardia |
1 (5.55%) Mitral valve regurgitation |
| Chronic venous insufficiency | 0 (0%) | 0 (0%) | 0 (0%) |
| Thrombosis | 0 (0%) | 2 (2.15%) | 0 (0%) |
| Presence of risk factors for chronic kidney disease | 0 (%) | 6 (6.45%) Pyelonephritis Glomerulonephritis Ureteral stent Nephrolithiasis Hydronephrosis |
0 (0%) |
| Chronic kidney disease | 0 (%) | 1 (0.98%) Chronic renal insufficiency |
0 (0%) |
Table 6.
Characteristics of cases and controls, data gained at follow-up.
| Normotensive Term Pregnancies (n = 89) |
GDM on Diet Only (n = 93) |
GDM on Diet and Therapy (n = 18) |
p-value1 | p-value2 | |
|---|---|---|---|---|---|
| Age (years) | 38.33 ± 0.38 | 38.70 ± 0.37 | 38.61 ± 0.80 | 0.465 | 0.564 |
| Time elapsed since delivery (years) | 5.75 ± 0.20 | 5.49 ± 0.12 | 5.33 ± 0.20 | 0.965 | 0.045 |
| BMI | 23.15 ± 0.38 | 23.85 ± 0.37 | 27.21 ± 0.83 | 1.000 | 1.000 |
| Normal (< 25) | 67 (75.28%) | 70 (75.27%) | 5 (27.78%) | 0.633 | < 0.001 |
| Overweight (≥ 25 <30) | 18 (20.22%) | 16 (17.20%) | 9 (50.00%) | ||
| Obese (≥ 30) | 4 (4.49%) | 7 (7.53%) | 4 (22.22%) | ||
| Smoking | - | - | |||
| Non-Smoker | 54 (60.67%) | 78 (83.87%) | 16 (88.88%) | ||
| Ex-smoker | 21 (23.60%) | 6 (6.45%) | 2 (11.11%) | ||
| Smoker | 14 (15.73%) | 9 (9.68%) | 0 (0%) | ||
| Angina or heart attack in a first degree relative before the age of 60 years | 2 (2.22%) | 6 (6.45%) | 2 (11.11%) | - | - |
| Atrial fibrillation | 0 (0%) | 0 (0%) | 0 (0%) | - | - |
| DM type I | 0 (0%) | 0 (0%) | 0 (0%) | - | - |
| DM type II | 0 (0%) | 0 (0%) | 0 (0%) | - | - |
| Fasting serum glucose levels | - | - | |||
| Normal (3.33–5.59 mmol/L) | 89 (100.0%) | 90 (96.77%) | 18 (100.0%) | ||
| High (> 5.59 mmol/L) | 0 (0%) | 3 (3.23%) | 0 (0%) | ||
| Fasting serum total cholesterol levels | - | - | |||
| Normal (2.9–5.0 mmol/L) | 43 (48.31%) | 51 (54.84%) | 10 (55.55%) | ||
| High (> 5.0–7.9 mmol/L) | 46 (51.69%) | 41(44.09%) | 8 (44.44%) | ||
| Critical (≥ 8.0 mmol/L) | 0 (0%) | 1 (1.08%) | 0 (0%) | ||
| Fating serum LDL cholesterol levels | 0.987 | 0.281 | |||
| Normal (1.2–3.0 mmol/L) | 42 (47.19%) | 44 (47.31%) | 6 (33.33%) | ||
| High (> 3.0 mmol/L) | 47 (52.81%) | 49 (52.69%) | 12 (66.67%) | ||
| SBP | - | - | |||
| Normal (< 140 mmHg) | 89 (100.0%) | 92 (98.92%) | 18 (100.0%) | ||
| High (≥ 140–179 mmHg) | 0 (0%) | 1 (1.08%) | 0 (0%) | ||
| Critical (≥ 180 mmHg) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| DBP | - | - | |||
| Normal (< 90 mmHg) | 88 (98.88%) | 90 (96.77%) | 17 (94.44%) | ||
| High (≥ 90–109 mmHg) | 1 (1.12%) | 3 (3.23%) | 1 (5.56%) | ||
| Critical (≥ 110 mmHg) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| On blood pressure treatment | 0 (0%) | 0 (0%) | 0 (0%) | - | - |
| Chronic kidney disease | 0 (%) | 1 (0.98%) Chronic renal insufficiency |
0 (0%) | - | - |
| Chronic venous insufficiency | 0 (0%) | 0 (0%) | 0 (0%) | - | - |
| Thrombosis | 0 (0%) | 2 (2.15%) | 0 (0%) | - | - |
| Relative QRISK®3-2018 risk score | 0.926 ± 0.05 | 0.889 ± 0.04 | 1.022 ± 0.08 | 1.0 | 1.0 |
| Hormonal contraceptive use | 0.040 | 0.474 | |||
| No | 12 (13.48%) | 5 (5.38%) | 2 (11.11%) | ||
| In the past | 63 (70.79%) | 80 (86.02%) | 15 (83.33%) | ||
| Yes | 14 (15.73%) | 8 (8.60%) | 1 (5.56%) | ||
| Total number of pregnancies per patient | 0.924 | 0.440 | |||
| 1 | 9 (10.11%) | 8 (8.60%) | 2 (11.11%) | ||
| 2 | 44 (49.44%) | 48 (51.61%) | 6 (33.33%) | ||
| 3+ | 36 (40.45%) | 37 (39.78%) | 10 (55.55%) | ||
| Total parity per patient | 0.991 | 0.217 | |||
| 1 | 13 (14.61%) | 13 (13.98%) | 2 (11.11%) | ||
| 2 | 62 (69.66%) | 65 (69.89%) | 10 (55.55%) | ||
| 3+ | 14 (15.73%) | 15 (16.13%) | 6 (33.33%) | ||
Data are presented as mean ± SE for continuous variables and as number (percent) for categorical variables. Statistically significant results are marked in bold. Continuous variables were compared using Mann–Whitney test. p-value1, the comparison among normal pregnancies and GDM on diet; p-value2, the comparison among normal pregnancies and GDM on diet and therapy, respectively. Categorical variables were compared using a chi-square test. GA, gestational age; SBP, systolic blood pressure; DBP, diastolic blood pressure; CS, caesarean section.
Table 7.
Characteristics of cases and controls, data gained during gestation.
| Normotensive Term Pregnancies (n = 89) |
GDM on Diet Only (n = 93) |
GDM on Diet and Therapy (n = 18) |
p-value1 | p-value2 | |
|---|---|---|---|---|---|
| Maternal age at delivery (years) |
32.62 ± 0.36 | 33.20 ± 0.35 | 33.28 ± 0.83 | 0.111 | 1.000 |
| GA at delivery (weeks) | 39.90 ± 0.10 | 39.59 ± 0.09 | 39.20 ± 0.23 | 0.961 | 1.000 |
| Fetal birth weight (g) | 3397.53 ± 40.42 | 3436.56 ± 35.96 | 3526.11 ± 63.35 | 1.000 | 1.000 |
| Mode of delivery | < 0.001 | 0.015 | |||
| Vaginal | 82 (92.13%) | 57 (61.29%) | 13 (72.22%) | ||
| CS | 7 (7.87%) | 36 (38.71%) | 5 (27.78%) | ||
| Fetal sex | 0.476 | 0.281 | |||
| Boy | 47 (52.81%) | 54 (58.06%) | 12 (66.67%) | ||
| Girl | 42 (47.19%) | 39 (41.94%) | 6 (33.33%) | ||
| Infertility treatment | 0.006 | 0.846 | |||
| Yes | 4 (4.49%) | 16 (17.20%) | 1 (5.56%) | ||
| No | 85 (95.51%) | 77 (82.80%) | 17 (94.44%) | ||
Data are presented as mean ± SE for continuous variables and as number (percent) for categorical variables. Statistically significant results are marked in bold. Continuous variables were compared using Mann–Whitney test. p-value1, the comparison among normal pregnancies and GDM on diet; p-value2, the comparison among normal pregnancies and GDM on diet and therapy, respectively. Categorical variables were compared using a chi-square test. GA, gestational age; SBP, systolic blood pressure; DBP, diastolic blood pressure; CS, caesarean section.
Gestational diabetes mellitus is defined as any degree of glucose intolerance with onset or first recognition during pregnancy [10,178,179]. The International Association of Diabetes and Pregnancy Study Groups’ (IADPSG) recommendations on the diagnosis and classification of hyperglycemia in pregnancy were followed [10]. The first screening phase detects, during the first trimester of gestation, women with overt diabetes (fasting plasma glucose level is ≥7.0 mmol/L) and women with GDM (fasting plasma glucose level ≥ 5.1 mmol/L < 7.0 mmol/L). The second screening phase, 2-h 75-g OGTT, at 24–28 weeks of gestation is done in all women not previously found to have overt diabetes or GDM, and identifies GDM if fasting plasma glucose level is ≥5.1 mmol/L or 1-h plasma glucose is ≥10.0 mmol/L or 2-h plasma glucose is ≥8.5 mmol/L [10].
Patients demonstrating other pregnancy-related complications, such as gestational hypertension, preeclampsia, fetal growth restriction, premature rupture of membranes, in utero infections, fetal anomalies or chromosomal abnormalities, and fetal demise in utero or stillbirth, were not involved in the study.
Written informed consent was provided for all participants included in the study. The study was approved by the Ethics Committee of the Institute for the Care of the Mother and Child, Prague, Czech Republic (grant no. AZV 16-27761A, long-term monitoring of complex cardiovascular profile in the mother, fetus, and offspring descending from pregnancy-related complications, date of approval: 28 May 2015) and by the Ethics Committee of the Third Faculty of Medicine, Prague, Czech Republic (grant no. AZV 16-27761A, long-term monitoring of complex cardiovascular profile in the mother, fetus, and offspring descending from pregnancy-related complications, date of approval: 27 March 2014).
4.2. Processing of Samples
Homogenized cell lysates were prepared immediately after collection of whole peripheral blood samples (EDTA tubes, 200 µL) using QIAamp RNA Blood Mini Kit (Qiagen, Hilden, Germany, no: 52304).
Total RNA was extracted from homogenized cell lysates stored at −80 °C using a mirVana microRNA Isolation kit (Ambion, Austin, USA, no: AM1560) and followed by an enrichment procedure for small RNAs. To minimize DNA contamination, the eluted RNA was treated for 30 min at 37 °C with 5 µL of DNase I (Thermo Fisher Scientific, CA, USA, no: EN0521). A RNA fraction highly enriched in short RNAs (< 200 nt) was obtained. The concentration and quality of RNA was assessed using a NanoDrop ND-1000 spectrophotometer (NanoDrop Technologies, USA). If the A(260/280) absorbance ratio of isolated RNA was 1.8–2.0 and the A(260/230) absorbance ratio was greater than 1.6, the RNA fraction was pure and used for the consecutive analysis.
4.3. Reverse Transcriptase Reaction
Individual microRNAs were reverse transcribed into complementary DNA (cDNA) in a total reaction volume of 10 µL using microRNA-specific stem-loop RT primers, components of TaqMan MicroRNA Assays (Table 8), and TaqMan MicroRNA Reverse Transcription Kit (Applied Biosystems, Branchburg, USA, no: 4366597). Reverse transcriptase reactions were performed with the following thermal cycling parameters: 30 min at 16 °C, 30 min at 42 °C, 5 min at 85 °C, and then held at 4 °C using a 7500 Real-Time PCR system (Applied Biosystems, Branchburg, USA).
Table 8.
Characteristics of microRNAs involved in the study.
| Assay Name | miRBase ID | NCBI Location Chromosome | microRNA Sequence |
|---|---|---|---|
| hsa-miR-1 | hsa-miR-1-3p | Chr20: 61151513-61151583 [+] | 5´-UGGAAUGUAAAGAAGUAUGUAU-3´ |
| hsa-miR-16 | hsa-miR-16-5p | Chr13: 50623109-50623197 [−] | 5´-UAGCAGCACGUAAAUAUUGGCG- 3´ |
| hsa-miR-17 | hsa-miR-17-5p | Chr13: 92002859-92002942 [+] | 5´-CAAAGUGCUUACAGUGCAGGUAG-3´ |
| hsa-miR-20a | hsa-miR-20a-5p | Chr13: 92003319-92003389 [+] | 5´-UAAAGUGCUUAUAGUGCAGGUAG-3´ |
| hsa-miR-20b | hsa-miR-20b-5p | ChrX: 133303839-133303907 [−] | 5´-CAAAGUGCUCAUAGUGCAGGUAG-3´ |
| hsa-miR-21 | hsa-miR-21-5p | Chr17: 57918627-57918698 [+] | 5´-UAGCUUAUCAGACUGAUGUUGA-3´ |
| hsa-miR-23a | hsa-miR-23a-3p | Chr19: 13947401-13947473 [−] | 5´-AUCACAUUGCCAGGGAUUUCC-3´ |
| hsa-miR-24 | hsa-miR-24-3p | Chr19: 13947101-13947173 [−] | 5´-UGGCUCAGUUCAGCAGGAACAG-3´ |
| hsa-miR-26a | hsa-miR-26a-5p | Chr3: 38010895-38010971 [+] | 5´-UUCAAGUAAUCCAGGAUAGGCU-3´ |
| hsa-miR-29a | hsa-miR-29a-3p | Chr7: 130561506-130561569 [−] | 5´-UAGCACCAUCUGAAAUCGGUUA-3´ |
| hsa-miR-92a | hsa-miR-92a-3p | Chr13: 92003568-92003645 [+] | 5´-UAUUGCACUUGUCCCGGCCUGU-3´ |
| hsa-miR-100 | hsa-miR-100-5p | Chr11: 122022937-122023016 [−] | 5´-AACCCGUAGAUCCGAACUUGUG-3´ |
| hsa-miR-103 | hsa-miR-103a-3p | Chr20: 3898141-3898218 [+] | 5´-AGCAGCAUUGUACAGGGCUAUGA-3´ |
| hsa-miR-125b | hsa-miR-125b-5p | Chr21: 17962557-17962645 [+] | 5´-UCCCUGAGACCCUAACUUGUGA-3´ |
| hsa-miR-126 | hsa-miR-126-3p | Chr9: 139565054-139565138 [+] | 5´-UCGUACCGUGAGUAAUAAUGCG-3´ |
| hsa-miR-130b | hsa-miR-130b-3p | Chr22: 22007593-22007674 [+] | 5´-CAGUGCAAUGAUGAAAGGGCAU-3´ |
| hsa-miR-133a | hsa-miR-133a-3p | Chr20: 61162119-61162220 [+] | 5´-UUUGGUCCCCUUCAACCAGCUG-3´ |
| hsa-miR-143 | hsa-miR-143-3p | Chr5: 148808481-148808586 [+] | 5´-UGAGAUGAAGCACUGUAGCUC-3´ |
| hsa-miR-145 | hsa-miR-145-5p | Chr5: 148810209-148810296 [+] | 5´-GUCCAGUUUUCCCAGGAAUCCCU-3´ |
| hsa-miR-146a | hsa-miR-146a-5p | Chr5: 159912359-159912457 [+] | 5´-UGAGAACUGAAUUCCAUGGGUU-3´ |
| hsa-miR-155 | hsa-miR-155-5p | Chr21: 26946292-26946356 [+] | 5´-UUAAUGCUAAUCGUGAUAGGGGU-3´ |
| hsa-miR-181a | hsa-miR-181a-5p | Chr9: 127454721-127454830 [+] | 5´-AACAUUCAACGCUGUCGGUGAGU-3´ |
| hsa-miR-195 | hsa-miR-195-5p | Chr17: 6920934-6921020 [−] | 5´-UAGCAGCACAGAAAUAUUGGC-3´ |
| hsa-miR-199a | hsa-miR-199a-5p | Chr19: 10928102-10928172 [−] | 5´-CCCAGUGUUCAGACUACCUGUUC-3´ |
| hsa-miR-210 | hsa-miR-210-3p | Chr11: 568089-568198 [−] | 5´-CUGUGCGUGUGACAGCGGCUGA-3´ |
| hsa-miR-221 | hsa-miR-221-3p | ChrX: 45605585-45605694 [−] | 5´-AGCUACAUUGUCUGCUGGGUUUC-3´ |
| hsa-miR-342-3p | hsa-miR-342-3p | Chr14: 100575992-100576090 [+] | 5´-UCUCACACAGAAAUCGCACCCGU-3´ |
| mmu-miR-499 | hsa-miR-499a-5p | Chr20: 33578179-33578300 [+] | 5´-UUAAGACUUGCAGUGAUGUUU-3´ |
| hsa-miR-574-3p | hsa-miR-574-3p | Chr4: 38869653-38869748 [+] | 5´-CACGCUCAUGCACACACCCACA-3´ |
4.4. Relative Quantification of MicroRNAs by Real-Time PCR
The cDNA (3 µL) was mixed with specific TaqMan MGB probes and primers (TaqMan MicroRNA Assay, Applied Biosystems, Branchburg, USA), and the components of the TaqMan Universal PCR Master Mix (Applied Biosystems, Branchburg, USA, no: 4318157). A total reaction volume was 15 µL. TaqMan PCR conditions were set up as described in the TaqMan guidelines for a 7500 Real-Time PCR system. All PCRs were performed in duplicates with the involvement of multiple negative controls such as NTC (water instead of cDNA sample), NAC (nontranscribed RNA samples), and genomic DNA (isolated from equal biological samples), which did not generate any signal during PCR reactions. The samples were considered positive if the amplification signal occurred at Ct < 40 (before the 40th threshold cycle).
The expression of particular microRNA was determined using the comparative Ct method [180] relative to normalization factor (geometric mean of two selected endogenous controls) [181]. Two noncoding small nucleolar RNAs (RNU58A and RNU38B) were optimal for qPCR data normalization in this setting. They demonstrated equal expression between children descending from normal and complicated pregnancies. RNU58A and RNU38B also served as positive controls for successful extraction of RNA from all samples and were used as internal controls for variations during the preparation of RNA, cDNA synthesis, and real-time PCR.
A reference sample, RNA fraction highly enriched for small RNAs isolated from the fetal part of one randomly selected placenta derived from gestation with normal course, was used throughout the study for relative quantification.
4.5. Statistical Analysis
Data normality was assessed using the Shapiro–Wilk test [182]. Since our experimental data did not follow a normal distribution, microRNA levels were compared between groups using the Kruskal–Wallis one-way analysis of variance with post hoc test for the comparison among multiple groups. The significance level was established at a p-value of p < 0.05.
Receivers operating characteristic (ROC) curves were constructed to calculate the area under the curve (AUC) and the best cut-off point for particular microRNA was used in order to calculate the respective sensitivity at 90.0% specificity (MedCalc Software bvba, Ostend, Belgium). For every possible threshold or cut-off value, the MedCalc program reports the sensitivity, specificity, likelihood ratio positive (LR+), likelihood ratio negative (LR−).
To select the optimal combinations of microRNA biomarkers, logistic regression was used (MedCalc Software bvba, Ostend, Belgium). The logistic regression procedure allowed us to analyses the relationship between one dichotomous dependent variable and one or more independent variables. Another method to evaluate the logistic regression model makes use of ROC curve analysis. In this analysis, the power of the model’s predicted values to discriminate between positive and negative cases is quantified by the area under the ROC curve (AUC). To perform a full ROC curve analysis, the predicted probabilities are first saved and next used as a new variable in ROC curve analysis. The dependent variable used in logistic regression then acts as the classification variable in the ROC curve analysis dialog box.
Box plots encompassing the median (dark horizontal line) of log-normalized gene expression values for particular microRNAs were generated using Statistica software (version 9.0; StatSoft, Inc., USA). The upper and lower limits of the boxes represent the 75th and 25th percentiles, respectively. The upper and lower whiskers indicate the maximum and minimum values that are no more than 1.5 times the span of the interquartile range (range of the values between the 25th and the 75th percentiles). Outliers are marked by circles and extremes by asterisks.
4.6. Information on MicroRNA-Gene-Biological Pathway Interactions
MiRWalk database (available: http://www.umm.uni-heidelberg.de/apps/zmf/mirwalk/) and the Predicted Target module were used to provide information on predicted targets of those microRNAs that have been found to be dysregulated in whole peripheral blood of patients with a history of GDM. Only those predicted targets involved in particular human biological pathways (insulin signaling pathway, type 1 diabetes mellitus pathway, and type 2 diabetes mellitus pathway) are reported [183].
MiRWalk is a comprehensive database that provides information on microRNAs from human, mouse, and rat on their predicted and/or validated target genes. MiRWalk2.0 not only documents miRNA binding sites within the complete sequence of a gene, but also combines this information with a comparison of binding sites resulting from 12 existing miRNA-target prediction programs (DIANA-microTv4.0, DIANA-microT-CDS, miRanda, mirBridge, miRDB4.0, miRmap, miRNAMap, DoRiNA, PicTar2, PITA, RNA22v2, RNAhybrid2.1, and Targetscan6.2) to build novel comparative platforms of binding sites for the promoter (4 prediction datasets), cds (5 prediction datasets), 5’- (5 prediction datasets), and 3’-UTR (13 prediction datasets) regions. Information on miRNA-target interactions on 2035 disease ontologies (DO), 6727 human phenotype ontologies (HPO) and 4980 OMIM disorders is available. It provides possible interactions between microRNAs and genes associated with 597 KEGG, 456 Panther, and 522 Wiki pathways.
5. Conclusions
In conclusion, epigenetic changes characteristic for diabetes mellitus and cardiovascular/cerebrovascular diseases are also present in whole peripheral blood of a proportion of mothers with a history of GDM. Likewise, a previous occurrence of either GH, PE, and/or FGR, as well as a previous occurrence of GDM, is associated with the upregulation of miR-1-3p, miR-17-5p, miR-20a-5p, miR-20b-5p, miR-29a-3p, miR-100-5p, miR-125b-5p, miR-126-3p, miR-130b-3p, miR-133a-3p, miR-143-3p, miR-145-5p, miR-146a-5p, miR-181a-5p, miR-199a-5p, miR-221-3p, and miR-499a-5p.
On the other hand, upregulation of miR-16-5p, miR-21-5p, miR-23a-3p, miR-24-3p, miR-26a-5p, miR-103a-3p, miR-195-5p, miR-342-3p, and miR-574-3p represents a unique feature of aberrant expression profile of women with a prior exposure to GDM.
Any changes in epigenome (upregulation of miR-16-5p, miR-17-5p, miR-29a-3p, and miR-195-5p) that were induced by GDM-complicated pregnancy are long-acting and may predispose mothers affected with GDM to later development of diabetes mellitus and cardiovascular/cerebrovascular diseases. In addition, novel epigenetic changes (upregulation of a series of microRNAs) appeared in a proportion of women that were exposed to GDM throughout the postpartal life.
Overall, previous occurrence of GDM, therefore, predisposes a proportion of affected individuals to later development of diabetes mellitus and cardiovascular/cerebrovascular diseases. Screening of particular microRNAs may stratify a high-risk group of mothers with a history of GDM that might benefit from implementation of early primary prevention strategies.
Consecutive large-scale studies, including the groups of mothers on diet only and on the combination of diet and therapy, are needed to verify the findings resulting from this particular pilot study.
6. Patents
National patent granted—Industrial Property Office, Czech Republic (Patent no. 308178).
International patent filed—Industrial Property Office, Czech Republic (PCT/CZ2019/050051).
Acknowledgments
All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. We thank the staff of the Institute for the Care of Mother and Child (Katerina Hamplova, Katerina Mackova, Radek Cabela, and Adam Krasny) for assistance with collection of patients´ anamnesis. We also thank Jana Kumprichtova, Sarka Stranska, Veronika Marvanova, and Andrea Semencova for assistance with biological sample collection and processing.
Abbreviations
| GDM | Gestational diabetes mellitus |
| PE | Preeclampsia |
| FGR | Fetal growth restriction |
| GH | Gestational hypertension |
| AUC | Area under the receive operating characteristic curve |
| FPR | False positive rate |
| CI | Confidence interval |
| LR+ | Positive likelihood ratio |
| LR- | Negative likelihood ratio |
| T1DM | Diabetes mellitus type I |
| T2DM | Diabetes mellitus type II |
| OGTT | Oral glucose tolerance test |
| SLE | Systemic lupus erythematosus |
| BMI | Body mass index |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| LDL | Low-density lipoprotein |
| GA | Gestational age |
| CS | Caesarean section |
| EDTA | Ethylenediaminetetraacetic acid |
| SE | Standard error |
| NTC | No template control |
| NAC | No amplification control |
Author Contributions
Conceptualization, I.H. and L.K.; methodology, I.H., K.K., and L.D.; software, I.H. and K.K.; validation, I.H. and L.K.; formal analysis, I.H. and K.K.; investigation, K.K. and L.D.; resources, L.D.; data curation, I.H., K.K., and L.D.; writing—original draft preparation, I.H. and K.K.; writing—review and editing, I.H. and K.K.; visualization, K.K.; supervision, I.H. and L.K.; project administration, I.H. and L.K.; funding acquisition, I.H. and L.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Agency of Medical Research, Ministry of Health, Prague, Czech Republic, grant number AZV 16-27761A and by the Charles University, Prague, Czech Republic, grant number 260529/SVV/2020 and PROGRES Q34. All rights reserved.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Hromadnikova I., Kotlabova K., Dvorakova L., Krofta L. Postpartum profiling of microRNAs involved in pathogenesis of cardiovascular/cerebrovascular diseases in women exposed to pregnancy-related complications. Int. J. Cardiol. 2019;291:158–167. doi: 10.1016/j.ijcard.2019.05.036. [DOI] [PubMed] [Google Scholar]
- 2.Hromadnikova I. Postpartální Epigenetický Profil Kardiovaskulárních mikrorna u Matek Po komplikované Graviditě—Nové Biomarkery Kardiovaskulárního Rizika. Industrial Property Office, Czech Republic. NO. 308178. CZ Patent. 2018 Oct 31;
- 3.Hromadnikova I. Postpartum epigenetic profile of cardiovascular microRNAs in women exposed to pregnancy-related complications. Industrial Property Office, Czech Republic. PCT/CZ2019/050051. PCT International Application. 2019 Oct 30;
- 4.Committee on Practice Bulletins—Obstetrics ACOG Practice Bulletin No. 190: Gestational Diabetes Mellitus. Obstet. Gynecol. 2018;131:e49–e64. doi: 10.1097/AOG.0000000000002501. [DOI] [PubMed] [Google Scholar]
- 5.England L.J., Dietz P.M., Njoroge T., Callaghan W.M., Bruce C., Buus R.M., Williamson D.F. Preventing type 2 diabetes: Public health implications for women with a history of gestational diabetes mellitus. Am. J. Obstet. Gynecol. 2009;200:365.e1–365.e8. doi: 10.1016/j.ajog.2008.06.031. [DOI] [PubMed] [Google Scholar]
- 6.O’Sullivan J.B. Body weight and subsequent diabetes mellitus. JAMA. 1982;248:949–952. doi: 10.1001/jama.1982.03330080031024. [DOI] [PubMed] [Google Scholar]
- 7.Kim C., Newton K.M., Knopp R.H. Gestational diabetes and the incidence of type 2 diabetes: A systematic review. Diabetes Care. 2002;25:1862–1868. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 8.O’Sullivan J.B., Mahan C.M. Criteria for the oral glucose tolerance test in pregnancy. Diabetes. 1964;13:278–285. [PubMed] [Google Scholar]
- 9.Metzger B.E., Buchanan T.A., Coustan D.R., de Leiva A., Dunger D.B., Hadden D.R., Hod M., Kitzmiller J.L., Kjos S.L., Oats J.N., et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care. 2007;30:S251–S260. doi: 10.2337/dc07-s225. [DOI] [PubMed] [Google Scholar]
- 10.International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Metzger B.E., Gabbe S.G., Persson B., Buchanan T.A., Catalano P.A., Damm P., Dyer A.R., Leiva A.D., Hod M., et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–682. doi: 10.2337/dc10-0719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li J., Dong X., Wang Z., Wu J. MicroRNA-1 in Cardiac Diseases and Cancers. Korean J. Physiol. Pharmacol. 2014;18:359–363. doi: 10.4196/kjpp.2014.18.5.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Y.Q., Zhang M.F., Wen H.Y., Hu C.L., Liu R., Wei H.Y., Ai C.M., Wang G., Liao X.X., Li X. Comparing the diagnostic values of circulating microRNAs and cardiac troponin T in patients with acute myocardial infarction. Clinics. 2013;68:75–80. doi: 10.6061/clinics/2013(01)OA12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerlinger-Romero F., Yonamine C.Y., Junior D.C., Esteves J.V., Machado U.F. Dysregulation between TRIM63/FBXO32 expression and soleus muscle wasting in diabetic rats: Potential role of miR-1-3p, -29a/b-3p, and -133a/b-3p. Mol. Cell. Biochem. 2017;427:187–199. doi: 10.1007/s11010-016-2910-z. [DOI] [PubMed] [Google Scholar]
- 14.Kokkinopoulou I., Maratou E., Mitrou P., Boutati E., Sideris D.C., Fragoulis E.G., Christodoulou M.I. Decreased expression of microRNAs targeting type-2 diabetes susceptibility genes in peripheral blood of patients and predisposed individuals. Endocrine. 2019;66:226–239. doi: 10.1007/s12020-019-02062-0. [DOI] [PubMed] [Google Scholar]
- 15.Hromadnikova I., Kotlabova K., Dvorakova L., Krofta L. Evaluation of Vascular Endothelial Function in Young and Middle-Aged Women with Respect to a History of Pregnancy, Pregnancy-Related Complications, Classical Cardiovascular Risk Factors, and Epigenetics. Int. J. Mol. Sci. 2020;21:E430. doi: 10.3390/ijms21020430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang X., Shang Y., Dai S., Wu W., Yi F., Cheng L. MicroRNA-16-5p aggravates myocardial infarction injury by targeting expression of insulin receptor substrates 1 and mediating myocardial apoptosis and angiogenesis. Curr. Neurovasc. Res. :2019. doi: 10.2174/1567202617666191223142743. [DOI] [PubMed] [Google Scholar]
- 17.O´Sullivan J.F., Neylon A., McGorrian C., Blake G.J. miRNA-93-5p and other miRNAs as predictors of coronary artery disease and STEMI. Int. J. Cardiol. 2016;224:310–316. doi: 10.1016/j.ijcard.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 18.Vegter E.L., Schmitter D., Hagemeijer Y., Ovchinnikova E.S., van der Harst P., Teerlink J.R., O’Connor C.M., Metra M., Davison B.A., Bloomfield D., et al. Use of biomarkers to establish potential role and function of circulating microRNAs in acute heart failure. Int. J. Cardiol. 2016;224:231–239. doi: 10.1016/j.ijcard.2016.09.010. [DOI] [PubMed] [Google Scholar]
- 19.Gacoń J., Badacz R., Stępień E., Karch I., Enguita F.J., Żmudka K., Przewłocki T., Kabłak-Ziembicka A. Diagnostic and prognostic micro-RNAs in ischaemic stroke due to carotid artery stenosis and in acute coronary syndrome: A four-year prospective study. Kardiol. Pol. 2018;76:362–369. doi: 10.5603/KP.a2017.0243. [DOI] [PubMed] [Google Scholar]
- 20.Zhu Y., Tian F., Li H., Zhou Y., Lu J., Ge Q. Profiling maternal plasma microRNA expression in early pregnancy to predict gestational diabetes mellitus. Int. J. Gynaecol. Obstet. 2015;130:49–53. doi: 10.1016/j.ijgo.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Cao Y.L., Jia Y.J., Xing B.H., Shi D.D., Dong X.J. Plasma microRNA-16-5p, -17-5p and -20a-5p: Novel diagnostic biomarkers for gestational diabetes mellitus. J. Obstet. Gynaecol. Res. 2017;43:974–981. doi: 10.1111/jog.13317. [DOI] [PubMed] [Google Scholar]
- 22.Duan Y.R., Chen B.P., Chen F., Yang S.X., Zhu C.Y., Ma Y.L., Li Y., Shi J. Exosomal microRNA-16-5p from human urine-derived stem cells ameliorates diabetic nephropathy through protection of podocyte. J. Cell. Mol. Med. 2019 doi: 10.1111/jcmm.14558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Assmann T.S., Recamonde-Mendoza M., Costa A.R., Puñales M., Tschiedel B., Canani L.H., Bauer A.C., Crispim D. Circulating miRNAs in diabetic kidney disease: Case-control study and in silico analyses. Acta Diabetol. 2019;56:55–65. doi: 10.1007/s00592-018-1216-x. [DOI] [PubMed] [Google Scholar]
- 24.Alicka M., Major P., Wysocki M., Marycz K. Adipose-Derived Mesenchymal Stem Cells Isolated from Patients with Type 2 Diabetes Show Reduced "Stemness" through an Altered Secretome Profile, Impaired Anti-Oxidative Protection, and Mitochondrial Dynamics Deterioration. J. Clin. Med. 2019;8:E765. doi: 10.3390/jcm8060765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mogilyansky E., Rigoutsos I. The miR-17/92 cluster: A comprehensive update on its genomics, genetics, functions and increasingly important and numerous roles in health and disease. Cell Death Differ. 2013;20:1603–1614. doi: 10.1038/cdd.2013.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou L., Qi R.Q., Liu M., Xu Y.P., Li G., Weiland M., Kaplan D.H., Mi Q.S. microRNA miR-17-92 cluster is highly expressed in epidermal Langerhans cells but not required for its development. Genes Immun. 2014;15:57–61. doi: 10.1038/gene.2013.61. [DOI] [PubMed] [Google Scholar]
- 27.Danielson L.S., Park D.S., Rotllan N., Chamorro-Jorganes A., Guijarro M.V., Fernandez-Hernando C., Fishman G.I., Phoon C.K., Hernando E. Cardiovascular dysregulation of miR-17-92 causes a lethal hypertrophic cardiomyopathy and arrhythmogenesis. FASEB J. 2013;27:1460–1467. doi: 10.1096/fj.12-221994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Du W., Pan Z., Chen X., Wang L., Zhang Y., Li S., Liang H., Xu C., Zhang Y., Wu Y., et al. By targeting Stat3 microRNA-17-5p promotes cardiomyocyte apoptosis in response to ischemia followed by reperfusion. Cell. Physiol. Biochem. 2014;34:955–965. doi: 10.1159/000366312. [DOI] [PubMed] [Google Scholar]
- 29.Kaucsár T., Révész C., Godó M., Krenács T., Albert M., Szalay C.I., Rosivall L., Benyó Z., Bátkai S., Thum T., et al. Activation of the miR-17 family and miR-21 during murine kidney ischemia-reperfusion injury. Nucleic Acid Ther. 2013;23:344–354. doi: 10.1089/nat.2013.0438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang L., Ellims A.H., Moore X.L., White D.A., Taylor A.J., Chin-Dusting J., Dart A.M. Circulating microRNAs as biomarkers for diffuse myocardial fibrosis in patients with hypertrophic cardiomyopathy. J. Transl. Med. 2015;13:314. doi: 10.1186/s12967-015-0672-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu J., Du K., Lu X. Elevated expressions of serum miR-15a, miR-16, and miR-17-5p are associated with acute ischemic stroke. Int. J. Clin. Exp. Med. 2015;8:21071–21079. [PMC free article] [PubMed] [Google Scholar]
- 32.Chen J., Xu L., Hu Q., Yang S., Zhang B., Jiang H. MiR-17-5p as circulating biomarkers for the severity of coronary atherosclerosis in coronary artery disease. Int. J. Cardiol. 2015;197:123–124. doi: 10.1016/j.ijcard.2015.06.037. [DOI] [PubMed] [Google Scholar]
- 33.Tian L., Song Z., Shao W., Du W.W., Zhao L.R., Zeng K., Yang B.B., Jin T. Curcumin represses mouse 3T3-L1 cell adipogenic differentiation via inhibiting miR-17-5p and stimulating the Wnt signalling pathway effector Tcf7l2. Cell Death Dis. 2017;8:e2559. doi: 10.1038/cddis.2016.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen T.C., Sung M.L., Kuo H.C., Chien S.J., Yen C.K., Chen C.N. Differential regulation of human aortic smooth muscle cell proliferation by monocyte-derived macrophages from diabetic patients. PLoS ONE. 2014;9:e113752. doi: 10.1371/journal.pone.0113752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mendell J.T. miRiad roles for the miR-17-92 cluster in development and disease. Cell. 2008;133:217–222. doi: 10.1016/j.cell.2008.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brock M., Samillan V.J., Trenkmann M., Schwarzwald C., Ulrich S., Gay R.E., Gassmann M., Ostergaard L., Gay S., Speich R., et al. AntagomiR directed against miR-20a restores functional BMPR2 signalling and prevents vascular remodelling in hypoxia-induced pulmonary hypertension. Eur. Heart J. 2014;35:3203–3211. doi: 10.1093/eurheartj/ehs060. [DOI] [PubMed] [Google Scholar]
- 37.Pheiffer C., Dias S., Rheeder P., Adam S. Decreased Expression of Circulating miR-20a-5p in South African Women with Gestational Diabetes Mellitus. Mol. Diagn. Ther. 2018;22:345–352. doi: 10.1007/s40291-018-0325-0. [DOI] [PubMed] [Google Scholar]
- 38.Platania C.B.M., Maisto R., Trotta M.C., D’Amico M., Rossi S., Gesualdo C., D’Amico G., Balta C., Herman H., Hermenean A., et al. Retinal and circulating miRNA expression patterns in diabetic retinopathy: An in silico and in vivo approach. Br. J. Pharmacol. 2019;176:2179–2194. doi: 10.1111/bph.14665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lareyre F., Clément M., Moratal C., Loyer X., Jean-Baptiste E., Hassen-Khodja R., Chinetti G., Mallat Z., Raffort J. Differential micro-RNA expression in diabetic patients with abdominal aortic aneurysm. Biochimie. 2019;162:1–7. doi: 10.1016/j.biochi.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 40.Dickinson B.A., Semus H.M., Montgomery R.L., Stack C., Latimer P.A., Lewton S.M., Lynch J.M., Hullinger T.G., Seto A.G., van Rooij E. Plasma microRNAs serve as biomarkers of therapeutic efficacy and disease progression in hypertension-induced heart failure. Eur. J. Heart Fail. 2013;15:650–659. doi: 10.1093/eurjhf/hft018. [DOI] [PubMed] [Google Scholar]
- 41.Flowers E., Aouizerat B.E., Abbasi F., Lamendola C., Grove K.M., Fukuoka Y., Reaven G.M. Circulating microRNA-320a and microRNA-486 predict thiazolidinedione response: Moving towards precision health for diabetes prevention. Metabolism. 2015;64:1051–1059. doi: 10.1016/j.metabol.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Katayama M., Wiklander O.P.B., Fritz T., Caidahl K., El-Andaloussi S., Zierath J.R., Krook A. Circulating Exosomal miR-20b-5p Is Elevated in Type 2 Diabetes and Could Impair Insulin Action in Human Skeletal Muscle. Diabetes. 2019;68:515–526. doi: 10.2337/db18-0470. [DOI] [PubMed] [Google Scholar]
- 43.Xiong Y., Chen L., Yan C., Zhou W., Endo Y., Liu J., Hu L., Hu Y., Mi B., Liu G. Circulating Exosomal miR-20b-5p Inhibition Restores Wnt9b Signaling and Reverses Diabetes-Associated Impaired Wound Healing. Small. 2020;16:e1904044. doi: 10.1002/smll.201904044. [DOI] [PubMed] [Google Scholar]
- 44.Zhu K., Hu X., Chen H., Li F., Yin N., Liu A.L., Shan K., Qin Y.W., Huang X., Chang Q., et al. Downregulation of circRNA DMNT3B contributes to diabetic retinal vascular dysfunction through targeting miR-20b-5p and BAMBI. EBioMedicine. 2019;49:341–353. doi: 10.1016/j.ebiom.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sekar D., Venugopal B., Sekar P., Ramalingam K. Role of microRNA 21 in diabetes and associated/related diseases. Gene. 2016;582:14–18. doi: 10.1016/j.gene.2016.01.039. [DOI] [PubMed] [Google Scholar]
- 46.Suárez Y., Fernández-Hernando C., Pober J.S., Sessa W.C. Dicer dependent microRNAs regulate gene expression and functions in human endothelial cells. Circ. Res. 2007;100:1164–1173. doi: 10.1161/01.RES.0000265065.26744.17. [DOI] [PubMed] [Google Scholar]
- 47.Dong S., Ma W., Hao B., Hu F., Yan L., Yan X., Wang Y., Chen Z., Wang Z. microRNA-21 promotes cardiac fibrosis and development of heart failure with preserved left ventricular ejection fraction by up-regulating Bcl-2. Int. J. Clin. Exp. Pathol. 2014;7:565–574. [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang J., Xing Q., Zhou X., Li J., Li Y., Zhang L., Zhou Q., Tang B. Circulating miRNA-21 is a promising biomarker for heart failure. Mol. Med. Rep. 2017;16:7766–7774. doi: 10.3892/mmr.2017.7575. [DOI] [PubMed] [Google Scholar]
- 49.Licholai S., Blaż M., Kapelak B., Sanak M. Unbiased Profile of MicroRNA Expression in Ascending Aortic Aneurysm Tissue Appoints Molecular Pathways Contributing to the Pathology. Ann. Thorac. Surg. 2016;102:1245–1252. doi: 10.1016/j.athoracsur.2016.03.061. [DOI] [PubMed] [Google Scholar]
- 50.Kriegel A.J., Baker M.A., Liu Y., Liu P., Cowley A.W., Jr., Liang M. Endogenous microRNAs in human microvascular endothelial cells regulate mRNAs encoded by hypertension-related genes. Hypertension. 2015;66:793–799. doi: 10.1161/HYPERTENSIONAHA.115.05645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Velle-Forbord T., Eidlaug M., Debik J., Sæther J.C., Follestad T., Nauman J., Gigante B., Røsjø H., Omland T., Langaas M., et al. Circulating microRNAs as predictive biomarkers of myocardial infarction: Evidence from the HUNT study. Atherosclerosis. 2019;289:1–7. doi: 10.1016/j.atherosclerosis.2019.07.024. [DOI] [PubMed] [Google Scholar]
- 52.Demirsoy İ.H., Ertural D.Y., Balci Ş., Çınkır Ü., Sezer K., Tamer L., Aras N. Profiles of Circulating MiRNAs Following Metformin Treatment in Patients with Type 2 Diabetes. J. Med. Biochem. 2018;37:499–506. doi: 10.2478/jomb-2018-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Olivieri F., Spazzafumo L., Bonafè M., Recchioni R., Prattichizzo F., Marcheselli F., Micolucci L., Mensà E., Giuliani A., Santini G., et al. MiR-21-5p and miR-126a-3p levels in plasma and circulating angiogenic cells: Relationship with type 2 diabetes complications. Oncotarget. 2015;6:35372–35382. doi: 10.18632/oncotarget.6164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Assmann T.S., Recamonde-Mendoza M., De Souza B.M., Crispim D. MicroRNA expression profiles and type 1 diabetes mellitus: Systematic review and bioinformatic analysis. Endocr. Connect. 2017;6:773–790. doi: 10.1530/EC-17-0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lakhter A.J., Pratt R.E., Moore R.E., Doucette K.K., Maier B.F., DiMeglio L.A., Sims E.K. Beta cell extracellular vesicle miR-21-5p cargo is increased in response to inflammatory cytokines and serves as a biomarker of type 1 diabetes. Diabetologia. 2018;61:1124–1134. doi: 10.1007/s00125-018-4559-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grieco G.E., Cataldo D., Ceccarelli E., Nigi L., Catalano G., Brusco N., Mancarella F., Ventriglia G., Fondelli C., Guarino E., et al. Serum Levels of miR-148a and miR-21-5p Are Increased in Type 1 Diabetic Patients and Correlated with Markers of Bone Strength and Metabolism. Noncoding RNA. 2018;4:E37. doi: 10.3390/ncrna4040037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gholaminejad A., Abdul Tehrani H., Gholami Fesharaki M. Identification of candidate microRNA biomarkers in diabetic nephropathy: A meta-analysis of profiling studies. J. Nephrol. 2018;31:813–831. doi: 10.1007/s40620-018-0511-5. [DOI] [PubMed] [Google Scholar]
- 58.Long B., Gan T.Y., Zhang R.C., Zhang Y.H. miR-23a Regulates Cardiomyocyte Apoptosis by Targeting Manganese Superoxide Dismutase. Mol. Cells. 2017;40:542–549. doi: 10.14348/molcells.2017.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wang S., He W., Wang C. MiR-23a Regulates the Vasculogenesis of Coronary Artery Disease by Targeting Epidermal Growth Factor Receptor. Cardiovasc. Ther. 2016;34:199–208. doi: 10.1111/1755-5922.12187. [DOI] [PubMed] [Google Scholar]
- 60.Cong X., Li Y., Lu N., Dai Y., Zhang H., Zhao X., Liu Y. Resveratrol attenuates the inflammatory reaction induced by ischemia/reperfusion in the rat heart. Mol. Med. Rep. 2014;9:2528–2532. doi: 10.3892/mmr.2014.2090. [DOI] [PubMed] [Google Scholar]
- 61.Černá V., Ostašov P., Pitule P., Moláček J., Třeška V., Pešta M. The Expression Profile of MicroRNAs in Small and Large Abdominal Aortic Aneurysms. Cardiol. Res. Pract. 2019;2019:8645840. doi: 10.1155/2019/8645840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lozano-Bartolomé J., Llauradó G., Portero-Otin M., Altuna-Coy A., Rojo-Martínez G., Vendrell J., Jorba R., Rodríguez-Gallego E., Chacón M.R. Altered Expression of miR-181a-5p and miR-23a-3p Is Associated With Obesity and TNFα-Induced Insulin Resistance. J. Clin. Endocrinol. Metab. 2018;103:1447–1458. doi: 10.1210/jc.2017-01909. [DOI] [PubMed] [Google Scholar]
- 63.Dolz S., Górriz D., Tembl J.I., Sánchez D., Fortea G., Parkhutik V., Lago A. Circulating MicroRNAs as Novel Biomarkers of Stenosis Progression in Asymptomatic Carotid Stenosis. Stroke. 2017;48:10–16. doi: 10.1161/STROKEAHA.116.013650. [DOI] [PubMed] [Google Scholar]
- 64.De Gonzalo-Calvo D., Cenarro A., Garlaschelli K., Pellegatta F., Vilades D., Nasarre L., Camino-Lopez S., Crespo J., Carreras F., Leta R., et al. Translating the microRNA signature of microvesicles derived from human coronary artery smooth muscle cells in patients with familial hypercholesterolemia and coronary artery disease. J. Mol. Cell. Cardiol. 2017;106:55–67. doi: 10.1016/j.yjmcc.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 65.Gecys D., Tatarunas V., Veikutiene A., Lesauskaite V. New potential modulators of CYP4F2 enzyme activity in angina pectoris: Hsa-miR-24-3p and hsa-miR-34a-5p. Biomarkers. 2020;25:40–47. doi: 10.1080/1354750X.2019.1690580. [DOI] [PubMed] [Google Scholar]
- 66.Onrat S.T., Onrat E., Ercan Onay E., Yalım Z., Avşar A. The Genetic Determination of the Differentiation between Ischemic Dilated Cardiomyopathy and Idiopathic Dilated Cardiomyopathy. Genet. Test. Mol. Biomarkers. 2018;22:644–651. doi: 10.1089/gtmb.2018.0188. [DOI] [PubMed] [Google Scholar]
- 67.Tan H., Qi J., Fan B.Y., Zhang J., Su F.F., Wang H.T. MicroRNA-24-3p Attenuates Myocardial Ischemia/Reperfusion Injury by Suppressing RIPK1 Expression in Mice. Cell. Physiol. Biochem. 2018;51:46–62. doi: 10.1159/000495161. [DOI] [PubMed] [Google Scholar]
- 68.Xiao X., Lu Z., Lin V., May A., Shaw D.H., Wang Z., Che B., Tran K., Du H., Shaw P.X. MicroRNA miR-24-3p Reduces Apoptosis and Regulates Keap1-Nrf2 Pathway in Mouse Cardiomyocytes Responding to Ischemia/Reperfusion Injury. Oxid. Med. Cell. Longev. 2018;2018:7042105. doi: 10.1155/2018/7042105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gao J., Liu Q.G. The role of miR-26 in tumors and normal tissues. Oncol. Lett. 2011;2:1019–1023. doi: 10.3892/ol.2011.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zheng L., Lin S., Lv C. MiR-26a-5p regulates cardiac fibroblasts collagen expression by targeting ULK1. Sci. Rep. 2018;8:2104. doi: 10.1038/s41598-018-20561-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bye A., Røsjø H., Nauman J., Silva G.J., Follestad T., Omland T., Wisløff U. Circulating microRNAs predict future fatal myocardial infarction in healthy individuals - The HUNT study. J. Mol. Cell. Cardiol. 2016;97:162–168. doi: 10.1016/j.yjmcc.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 72.Hsu A., Chen S.J., Chang Y.S., Chen H.C., Chu P.H. Systemic approach to identify serum microRNAs as potential biomarkers for acute myocardial infarction. Biomed Res. Int. 2014 doi: 10.1155/2014/418628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xing X., Guo S., Zhang G., Liu Y., Bi S., Wang X., Lu Q. miR-26a-5p protects against myocardial ischemia/reperfusion injury by regulating the PTEN/PI3K/AKT signaling pathway. Braz. J. Med. Biol. Res. 2020;53:e9106. doi: 10.1590/1414-431x20199106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chouvarine P., Geldner J., Giagnorio R., Legchenko E., Bertram H., Hansmann G. Trans-Right-Ventricle and Transpulmonary MicroRNA Gradients in Human Pulmonary Arterial Hypertension. Pediatr. Crit. Care Med. 2019 doi: 10.1097/PCC.0000000000002207. [DOI] [PubMed] [Google Scholar]
- 75.Garavelli S., Bruzzaniti S., Tagliabue E., Prattichizzo F., Di Silvestre D., Perna F., La Sala L., Ceriello A., Mozzillo E., Fattorusso V., et al. Blood Co-Circulating Extracellular microRNAs and Immune Cell Subsets Associate with Type 1 Diabetes Severity. Int. J. Mol. Sci. 2020;21:E477. doi: 10.3390/ijms21020477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ye Y., Hu Z., Lin Y., Zhang C., Perez-Polo J.R. Downregulation of microRNA-29 by antisense inhibitors and a PPAR-gamma agonist protects against myocardial ischaemia-reperfusion injury. Cardiovasc. Res. 2010;87:535–544. doi: 10.1093/cvr/cvq053. [DOI] [PubMed] [Google Scholar]
- 77.Moraes L.N., Fernandez G.J., Vechetti-Júnior I.J., Freire P.P., Souza R.W.A., Villacis R.A.R., Rogatto S.R., Reis P.P., Dal-Pai-Silva M., Carvalho R.F. Integration of miRNA and mRNA expression profiles reveals microRNA-regulated networks during muscle wasting in cardiac cachexia. Sci. Rep. 2017;7:6998. doi: 10.1038/s41598-017-07236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhao Y., Yuan Y., Qiu C. Underexpression of CACNA1C Caused by Overexpression of microRNA-29a Underlies the Pathogenesis of Atrial Fibrillation. Med. Sci. Monit. 2016;22:2175–2181. doi: 10.12659/MSM.896191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang L., Zhang Y., Xue S., Ding H., Wang Y., Qi H., Wang Y., Zhu W., Li P. Clinical significance of circulating microRNAs as diagnostic biomarkers for coronary artery disease. J. Cell. Mol. Med. 2020;24:1146–1150. doi: 10.1111/jcmm.14802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wander P.L., Boyko E.J., Hevner K., Parikh V.J., Tadesse M.G., Sorensen T.K., Williams M.A., Enquobahrie D.A. Circulating early- and mid-pregnancy microRNAs and risk of gestational diabetes. Diabetes Res. Clin. Pract. 2017;132:1–9. doi: 10.1016/j.diabres.2017.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kong L., Zhu J., Han W., Jiang X., Xu M., Zhao Y., Dong Q., Pang Z., Guan Q., Gao L., et al. Significance of serum microRNAs in pre-diabetes and newly diagnosed type 2 diabetes: A clinical study. Acta Diabetol. 2011;48:61–69. doi: 10.1007/s00592-010-0226-0. [DOI] [PubMed] [Google Scholar]
- 82.Widlansky M.E., Jensen D.M., Wang J., Liu Y., Geurts A.M., Kriegel A.J., Liu P., Ying R., Zhang G., Casati M., et al. miR-29 contributes to normal endothelial function and can restore it in cardiometabolic disorders. EMBO Mol. Med. 2018;10:E8046. doi: 10.15252/emmm.201708046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Moncini S., Salvi A., Zuccotti P., Viero G., Quattrone A., Barlati S., De Petro G., Venturin M., Riva P. The role of miR-103 and miR-107 in regulation of CDK5R1 expression and in cellular migration. PLoS ONE. 2011;6:e20038. doi: 10.1371/journal.pone.0020038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Huang L., Li L., Chen X., Zhang H., Shi Z. MiR-103a targeting Piezo1 is involved in acute myocardial infarction through regulating endothelium function. Cardiol. J. 2016;23:556–562. doi: 10.5603/CJ.a2016.0056. [DOI] [PubMed] [Google Scholar]
- 85.Deng B., Du J., Hu R., Wang A.P., Wu W.H., Hu C.P., Li Y.J., Li X.H. MicroRNA-103/107 is involved in hypoxia-induced proliferation of pulmonary arterial smooth muscle cells by targeting HIF-1β. Life Sci. 2016;147:117–124. doi: 10.1016/j.lfs.2016.01.043. [DOI] [PubMed] [Google Scholar]
- 86.Trajkovski M., Hausser J., Soutschek J., Bhat B., Akin A., Zavolan M., Heim M.H., Stoffel M. MicroRNAs 103 and 107 regulate insulin sensitivity. Nature. 2011;474:649–653. doi: 10.1038/nature10112. [DOI] [PubMed] [Google Scholar]
- 87.Assmann T.S., Recamonde-Mendoza M., Puñales M., Tschiedel B., Canani L.H., Crispim D. MicroRNA expression profile in plasma from type 1 diabetic patients: Case-control study and bioinformatic analysis. Diabetes Res. Clin. Pract. 2018;141:35–46. doi: 10.1016/j.diabres.2018.03.044. [DOI] [PubMed] [Google Scholar]
- 88.Shaham L., Binder V., Gefen N., Borkhardt A., Izraeli S. MiR-125 in normal and malignant hematopoiesis. Leukemia. 2012;26:2011–2018. doi: 10.1038/leu.2012.90. [DOI] [PubMed] [Google Scholar]
- 89.Tiedt S., Prestel M., Malik R., Schieferdecker N., Duering M., Kautzky V., Stoycheva I., Böck J., Northoff B.H., Klein M., et al. RNA-Seq Identifies Circulating miR-125a-5p, miR-125b-5p, and miR-143-3p as Potential Biomarkers for Acute Ischemic Stroke. Circ. Res. 2017;121:970–980. doi: 10.1161/CIRCRESAHA.117.311572. [DOI] [PubMed] [Google Scholar]
- 90.Jia K., Shi P., Han X., Chen T., Tang H., Wang J. Diagnostic value of miR-30d-5p and miR-125b-5p in acute myocardial infarction. Mol. Med. Rep. 2016;14:184–194. doi: 10.3892/mmr.2016.5246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bayoumi A.S., Park K.M., Wang Y., Teoh J.P., Aonuma T., Tang Y., Su H., Weintraub N.L., Kim I.M. A carvedilol-responsive microRNA, miR-125b-5p protects the heart from acute myocardial infarction by repressing pro-apoptotic bak1 and klf13 in cardiomyocytes. J. Mol. Cell. Cardiol. 2018;114:72–82. doi: 10.1016/j.yjmcc.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lamadrid-Romero M., Solís K.H., Cruz-Reséndiz M.S., Pérez J.E., Díaz N.F., Flores-Herrera H., García-López G., Perichart O., Reyes-Muñoz E., Arenas-Huertero F., et al. Central nervous system development-related microRNAs levels increase in the serum of gestational diabetic women during the first trimester of pregnancy. Neurosci. Res. 2018;130:8–22. doi: 10.1016/j.neures.2017.08.003. [DOI] [PubMed] [Google Scholar]
- 93.Satake E., Pezzolesi M.G., Md Dom Z.I., Smiles A.M., Niewczas M.A., Krolewski A.S. Circulating miRNA Profiles Associated With Hyperglycemia in Patients With Type 1 Diabetes. Diabetes. 2018;67:1013–1023. doi: 10.2337/db17-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Samandari N., Mirza A.H., Kaur S., Hougaard P., Nielsen L.B., Fredheim S., Mortensen H.B., Pociot F. Influence of Disease Duration on Circulating Levels of miRNAs in Children and Adolescents with New Onset Type 1 Diabetes. Noncoding RNA. 2018;4:E35. doi: 10.3390/ncrna4040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yu C.Y., Yang C.Y., Rui Z.L. MicroRNA-125b-5p improves pancreatic β-cell function through inhibiting JNK signaling pathway by targeting DACT1 in mice with type 2 diabetes mellitus. Life Sci. 2019;224:67–75. doi: 10.1016/j.lfs.2019.01.031. [DOI] [PubMed] [Google Scholar]
- 96.Wu X.J., Zhao Z.F., Kang X.J., Wang H.J., Zhao J., Pu X.M. MicroRNA-126-3p suppresses cell proliferation by targeting PIK3R2 in Kaposi’s sarcoma cells. Oncotarget. 2016;7:36614–36621. doi: 10.18632/oncotarget.9311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Matsha T.E., Kengne A.P., Hector S., Mbu D.L., Yako Y.Y., Erasmus R.T. MicroRNA profiling and their pathways in South African individuals with prediabetes and newly diagnosed type 2 diabetes mellitus. Oncotarget. 2018;9:30485–30498. doi: 10.18632/oncotarget.25271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tryggestad J.B., Vishwanath A., Jiang S., Mallappa A., Teague A.M., Takahashi Y., Thompson D.M., Chernausek S.D. Influence of gestational diabetes mellitus on human umbilical vein endothelial cell miRNA. Clin. Sci. 2016;130:1955–1967. doi: 10.1042/CS20160305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lan X., Wu L., Wu N., Chen Q., Li Y., Du X., Wei C., Feng L., Li Y., Osoro E.K., et al. Long Noncoding RNA lnc-HC Regulates PPARγ-Mediated Hepatic Lipid Metabolism through miR-130b-3p. Mol. Ther. Nucleic Acids. 2019;18:954–965. doi: 10.1016/j.omtn.2019.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang J., Jazii F.R., Haghighi M.M., Alvares D., Liu L., Khosraviani N., Adeli K. miR-130b is a potent stimulator of hepatic very-low-density lipoprotein assembly and secretion via marked induction of microsomal triglyceride transfer protein. Am. J. Physiol. Endocrinol. Metab. 2020;318:E262–E275. doi: 10.1152/ajpendo.00276.2019. [DOI] [PubMed] [Google Scholar]
- 101.Li P., Zhang Q., Wu X., Yang X., Zhang Y., Li Y., Jiang F. Circulating microRNAs serve as novel biological markers for intracranial aneurysms. J. Am. Heart Assoc. 2014;3:e000972. doi: 10.1161/JAHA.114.000972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tian C., Li Z., Yang Z., Huang Q., Liu J., Hong B. Plasma MicroRNA-16 Is a Biomarker for Diagnosis, Stratification, and Prognosis of Hyperacute Cerebral Infarction. PLoS ONE. 2016;11:e0166688. doi: 10.1371/journal.pone.0166688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Prabu P., Rome S., Sathishkumar C., Aravind S., Mahalingam B., Shanthirani C.S., Gastebois C., Villard A., Mohan V., Balasubramanyam M. Circulating MiRNAs of ’Asian Indian Phenotype’ Identified in Subjects with Impaired Glucose Tolerance and Patients with Type 2 Diabetes. PLoS ONE. 2015;10:e0128372. doi: 10.1371/journal.pone.0128372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Feng T., Li K., Zheng P., Wang Y., Lv Y., Shen L., Chen Y., Xue Z., Li B., Jin L., et al. Weighted Gene Coexpression Network Analysis Identified MicroRNA Coexpression Modules and Related Pathways in Type 2 Diabetes Mellitus. Oxid. Med. Cell. Longev. 2019 doi: 10.1155/2019/9567641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Liang H.W., Yang X., Wen D.Y., Gao L., Zhang X.Y., Ye Z.H., Luo J., Li Z.Y., He Y., Pang Y.Y., et al. Utility of miR-133a-3p as a diagnostic indicator for hepatocellular carcinoma: An investigation combined with GEO, TCGA, meta-analysis and bioinformatics. Mol. Med. Rep. 2018;17:1469–1484. doi: 10.3892/mmr.2017.8040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Van Rooij E., Olson E.N. MicroRNAs: Powerful new regulators of heart disease and provocative therapeutic targets. J. Clin. Investig. 2007;117:2369–2376. doi: 10.1172/JCI33099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wang J., Xu R., Lin F., Zhang S., Zhang G., Hu S., Zheng Z. MicroRNA: Novel regulators involved in the remodeling and reverse remodeling of the heart. Cardiology. 2009;113:81–88. doi: 10.1159/000172616. [DOI] [PubMed] [Google Scholar]
- 108.Kukreja R.C., Yin C., Salloum F.N. MicroRNAs: New players in cardiac injury and protection. Mol. Pharmacol. 2011;80:558–564. doi: 10.1124/mol.111.073528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Duisters R.F., Tijsen A.J., Schroen B., Leenders J.J., Lentink V., van der Made I., Herias V., van Leeuwen R.E., Schellings M.W., Barenbrug P., et al. miR-133 and miR-30 regulate connective tissue growth factor: Implications for a role of microRNAs in myocardial matrix remodeling. Circ. Res. 2009;104:170–178. doi: 10.1161/CIRCRESAHA.108.182535. [DOI] [PubMed] [Google Scholar]
- 110.Liu W., Ling S., Sun W., Liu T., Li Y., Zhong G., Zhao D., Zhang P., Song J., Jin X., et al. Circulating microRNAs correlated with the level of coronary artery calcification in symptomatic patients. Sci. Rep. 2015;5:16099. doi: 10.1038/srep16099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jiang Y., Zhang M., He H., Chen J., Zeng H., Li J., Duan R. MicroRNA/mRNA profiling and regulatory network of intracranial aneurysm. BMC Med. Genomics. 2013;6:36. doi: 10.1186/1755-8794-6-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Liu H., Xiong W., Liu F., Lin F., He J., Liu C., Lin Y., Dong S. Significant role and mechanism of microRNA-143-3p/KLLN axis in the development of coronary heart disease. Am. J. Transl. Res. 2019;11:3610–3619. [PMC free article] [PubMed] [Google Scholar]
- 113.Li C., Li J., Xue K., Zhang J., Wang C., Zhang Q., Chen X., Gao C., Yu X., Sun L. MicroRNA-143-3p promotes human cardiac fibrosis via targeting sprouty3 after myocardial infarction. J. Mol. Cell. Cardiol. 2019;129:281–292. doi: 10.1016/j.yjmcc.2019.03.005. [DOI] [PubMed] [Google Scholar]
- 114.Yu B., Zhao Y., Zhang H., Xie D., Nie W., Shi K. Inhibition of microRNA-143-3p attenuates myocardial hypertrophy by inhibiting inflammatory response. Cell Biol. Int. 2018;42:1584–1593. doi: 10.1002/cbin.11053. [DOI] [PubMed] [Google Scholar]
- 115.Jiao M., You H.Z., Yang X.Y., Yuan H., Li Y.L., Liu W.X., Jin M., Du J. Circulating microRNA signature for the diagnosis of childhood dilated cardiomyopathy. Sci. Rep. 2018;8:724. doi: 10.1038/s41598-017-19138-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Deng L., Blanco F.J., Stevens H., Lu R., Caudrillier A., McBride M., McClure J.D., Grant J., Thomas M., Frid M., et al. MicroRNA-143 Activation Regulates Smooth Muscle and Endothelial Cell Crosstalk in Pulmonary Arterial Hypertension. Circ. Res. 2015;117:870–883. doi: 10.1161/CIRCRESAHA.115.306806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Shi L., Tian C., Sun L., Cao F., Meng Z. The lncRNA TUG1/miR-145-5p/FGF10 regulates proliferation and migration in VSMCs of hypertension. Biochem. Biophys. Res. Commun. 2018;501:688–695. doi: 10.1016/j.bbrc.2018.05.049. [DOI] [PubMed] [Google Scholar]
- 118.Yang X., Niu X., Xiao Y., Lin K., Chen X. MiRNA expression profiles in healthy OSAHS and OSAHS with arterial hypertension: Potential diagnostic and early warning markers. Respir. Res. 2018;19:194. doi: 10.1186/s12931-018-0894-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Toro R., Blasco-Turrión S., Morales-Ponce F.J., Gonzalez P., Martínez-Camblor P., López-Granados A., Brugada R., Campuzano O., Pérez-Serra A., Rosa Longobardo F., et al. Plasma microRNAs as biomarkers for Lamin A/C-related dilated cardiomyopathy. J. Mol. Med. 2018;96:845–856. doi: 10.1007/s00109-018-1666-1. [DOI] [PubMed] [Google Scholar]
- 120.Yuan M., Zhang L., You F., Zhou J., Ma Y., Yang F., Tao L. MiR-145-5p regulates hypoxia-induced inflammatory response and apoptosis in cardiomyocytes by targeting CD40. Mol. Cell. Biochem. 2017;431:123–131. doi: 10.1007/s11010-017-2982-4. [DOI] [PubMed] [Google Scholar]
- 121.Wu G., Tan J., Li J., Sun X., Du L., Tao S. miRNA-145-5p induces apoptosis after ischemia-reperfusion by targeting dual specificity phosphatase 6. J. Cell. Physiol. 2019;234:16281–16289. doi: 10.1002/jcp.28291. [DOI] [PubMed] [Google Scholar]
- 122.Xie X., Peng L., Zhu J., Zhou Y., Li L., Chen Y., Yu S., Zhao Y. miR-145-5p/Nurr1/TNF-α Signaling-Induced Microglia Activation Regulates Neuron Injury of Acute Cerebral Ischemic/Reperfusion in Rats. Front. Mol. Neurosci. 2017;10:383. doi: 10.3389/fnmol.2017.00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nunez Lopez Y.O., Retnakaran R., Zinman B., Pratley R.E., Seyhan A.A. Predicting and understanding the response to short-term intensive insulin therapy in people with early type 2 diabetes. Mol. Metab. 2019;20:63–78. doi: 10.1016/j.molmet.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhang J., Cui C., Xu H. Downregulation of miR-145-5p elevates retinal ganglion cell survival to delay diabetic retinopathy progress by targeting FGF5. Biosci. Biotechnol. Biochem. 2019;83:1655–1662. doi: 10.1080/09168451.2019.1630251. [DOI] [PubMed] [Google Scholar]
- 125.Zamanian Azodi M., Rezaei-Tavirani M., Rezaei-Tavirani M., Robati R.M. Gestational Diabetes Mellitus Regulatory Network Identifies hsa-miR-145-5p and hsa-miR-875-5p as Potential Biomarkers. Int. J. Endocrinol. Metab. 2019;17:e86640. doi: 10.5812/ijem.86640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Taganov K.D., Boldin M.P., Chang K.J., Baltimore D. NF-kappaB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc. Natl. Acad. Sci. USA. 2006;103:12481–12486. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Paterson M.R., Kriegel A.J. MiR-146a/b: A family with shared seeds and different roots. Physiol. Genomics. 2017;49:243–252. doi: 10.1152/physiolgenomics.00133.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zhang X., Ye Z.H., Liang H.W., Ren F.H., Li P., Dang Y.W., Chen G. Down-regulation of miR-146a-5p and its potential targets in hepatocellular carcinoma validated by a TCGA- and GEO-based study. FEBS Open Bio. 2017;7:504–521. doi: 10.1002/2211-5463.12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Wang X., Ha T., Liu L., Zou J., Zhang X., Kalbfleisch J., Gao X., Williams D., Li C. Increased expression of microRNA-146a decreases myocardial ischaemia/reperfusion injury. Cardiovasc. Res. 2013;97:432–442. doi: 10.1093/cvr/cvs356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Quan X., Ji Y., Zhang C., Guo X., Zhang Y., Jia S., Ma W., Fan Y., Wang C. Circulating MiR-146a May be a Potential Biomarker of Coronary Heart Disease in Patients with Subclinical Hypothyroidism. Cell. Physiol. Biochem. 2018;45:226–236. doi: 10.1159/000486769. [DOI] [PubMed] [Google Scholar]
- 131.Li S.H., Chen L., Pang X.M., Su S.Y., Zhou X., Chen C.Y., Huang L.G., Li J.P., Liu J.L. Decreased miR-146a expression in acute ischemic stroke directly targets the Fbxl10 mRNA and is involved in modulating apoptosis. Neurochem. Int. 2017;107:156–167. doi: 10.1016/j.neuint.2017.01.011. [DOI] [PubMed] [Google Scholar]
- 132.Sun X., Sit A., Feinberg M.W. Role of miR-181 family in regulating vascular inflammation and immunity. Trends Cardiovasc. Med. 2014;24:105–112. doi: 10.1016/j.tcm.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hulsmans M., Sinnaeve P., Van der Schueren B., Mathieu C., Janssens S., Holvoet P. Decreased miR-181a expression in monocytes of obese patients is associated with the occurrence of metabolic syndrome and coronary artery disease. J. Clin. Endocrinol. Metab. 2012;97:E1213–E1218. doi: 10.1210/jc.2012-1008. [DOI] [PubMed] [Google Scholar]
- 134.Du X., Yang Y., Xu C., Peng Z., Zhang M., Lei L., Gao W., Dong Y., Shi Z., Sun X., et al. Upregulation of miR-181a impairs hepatic glucose and lipid homeostasis. Oncotarget. 2017;8:91362–91378. doi: 10.18632/oncotarget.20523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wu J., Fan C.L., Ma L.J., Liu T., Wang C., Song J.X., Lv Q.S., Pan H., Zhang C.N., Wang J.J. Distinctive expression signatures of serum microRNAs in ischaemic stroke and transient ischaemic attack patients. Thromb. Haemost. 2017;117:992–1001. doi: 10.1160/TH16-08-0606. [DOI] [PubMed] [Google Scholar]
- 136.Zhu J., Yao K., Wang Q., Guo J., Shi H., Ma L., Liu H., Gao W., Zou Y., Ge J. Circulating miR-181a as a Potential Novel Biomarker for Diagnosis of Acute Myocardial Infarction. Cell. Physiol. Biochem. 2016;40:1591–1602. doi: 10.1159/000453209. [DOI] [PubMed] [Google Scholar]
- 137.Nabih E.S., Andrawes N.G. The Association Between Circulating Levels of miRNA-181a and Pancreatic Beta Cells Dysfunction via SMAD7 in Type 1 Diabetic Children and Adolescents. J. Clin. Lab. Anal. 2016;30:727–731. doi: 10.1002/jcla.21928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.He J.F., Luo Y.M., Wan X.H., Jiang D. Biogenesis of MiRNA-195 and its role in biogenesis, the cell cycle, and apoptosis. J. Biochem. Mol. Toxicol. 2011;25:404–408. doi: 10.1002/jbt.20396. [DOI] [PubMed] [Google Scholar]
- 139.Van Rooij E., Sutherland L.B., Liu N., Williams A.H., McAnally J., Gerard R.D., Richardson J.A., Olson E.N. A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc. Natl. Acad. Sci. USA. 2006;103:18255–18260. doi: 10.1073/pnas.0608791103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.You X.Y., Huang J.H., Liu B., Liu S.J., Zhong Y., Liu S.M. HMGA1 is a new target of miR-195 involving isoprenaline-induced cardiomyocyte hypertrophy. Biochemistry. 2014;79:538–544. doi: 10.1134/S0006297914060078. [DOI] [PubMed] [Google Scholar]
- 141.Zampetaki A., Attia R., Mayr U., Gomes R.S., Phinikaridou A., Yin X., Langley S.R., Willeit P., Lu R., Fanshawe B., et al. Role of miR-195 in aortic aneurysmal disease. Circ. Res. 2014;115:857–866. doi: 10.1161/CIRCRESAHA.115.304361. [DOI] [PubMed] [Google Scholar]
- 142.Du J., Zheng R., Xiao F., Zhang S., He K., Zhang J., Shao Y. Downregulated MicroRNA-195 in the Bicuspid Aortic Valve Promotes Calcification of Valve Interstitial Cells via Targeting SMAD7. Cell. Physiol. Biochem. 2017;44:884–896. doi: 10.1159/000485356. [DOI] [PubMed] [Google Scholar]
- 143.Tagoma A., Alnek K., Kirss A., Uibo R., Haller-Kikkatalo K. MicroRNA profiling of second trimester maternal plasma shows upregulation of miR-195-5p in patients with gestational diabetes. Gene. 2018;672:137–142. doi: 10.1016/j.gene.2018.06.004. [DOI] [PubMed] [Google Scholar]
- 144.Lynch S.M., Ward M., McNulty H., Angel C.Z., Horigan G., Strain J.J., Purvis J., Tackett M., McKenna D.J. Serum levels of miR-199a-5p correlates with blood pressure in premature cardiovascular disease patients homozygous for the MTHFR 677C > T polymorphism. Genomics. 2020;112:669–676. doi: 10.1016/j.ygeno.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 145.Zhou Y., Pang B., Xiao Y., Zhou S., He B., Zhang F., Liu W., Peng H., Li P. The protective microRNA-199a-5p-mediated unfolded protein response in hypoxic cardiomyocytes is regulated by STAT3 pathway. J. Physiol. Biochem. 2019;75:73–81. doi: 10.1007/s13105-018-0657-6. [DOI] [PubMed] [Google Scholar]
- 146.Liu Y., Liu G., Zhang H., Wang J. MiRNA-199a-5p influences pulmonary artery hypertension via downregulating Smad3. Biochem. Biophys. Res. Commun. 2016;473:859–866. doi: 10.1016/j.bbrc.2016.03.140. [DOI] [PubMed] [Google Scholar]
- 147.Wang J., Yu G. A Systems Biology Approach to Characterize Biomarkers for Blood Stasis Syndrome of Unstable Angina Patients by Integrating MicroRNA and Messenger RNA Expression Profiling. Evid.-Based Complement. Alternat. Med. 2013 doi: 10.1155/2013/510208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Massaro J.D., Polli C.D., Costa ESilva M., Alves C.C., Passos G.A., Sakamoto-Hojo E.T., Rodrigues de Holanda Miranda W., Bispo Cezar N.J., Rassi D.M., Crispim F., et al. Post-transcriptional markers associated with clinical complications in Type 1 and Type 2 diabetes mellitus. Mol. Cell. Endocrinol. 2019;490:1–14. doi: 10.1016/j.mce.2019.03.008. [DOI] [PubMed] [Google Scholar]
- 149.Collares C.V., Evangelista A.F., Xavier D.J., Rassi D.M., Arns T., Foss-Freitas M.C., Foss M.C., Puthier D., Sakamoto-Hojo E.T., Passos G.A., et al. Identifying common and specific microRNAs expressed in peripheral blood mononuclear cell of type 1, type 2, and gestational diabetes mellitus patients. BMC Res. Notes. 2013;6:491. doi: 10.1186/1756-0500-6-491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Derda A.A., Pfanne A., Bär C., Schimmel K., Kennel P.J., Xiao K., Schulze P.C., Bauersachs J., Thum T. Blood-based microRNA profiling in patients with cardiac amyloidosis. PLoS ONE. 2018;13:e0204235. doi: 10.1371/journal.pone.0204235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Verjans R., Peters T., Beaumont F.J., van Leeuwen R., van Herwaarden T., Verhesen W., Munts C., Bijnen M., Henkens M., Diez J., et al. MicroRNA-221/222 Family Counteracts Myocardial Fibrosis in Pressure Overload-Induced Heart Failure. Hypertension. 2018;71:280–288. doi: 10.1161/HYPERTENSIONAHA.117.10094. [DOI] [PubMed] [Google Scholar]
- 152.Zhuang X., Li R., Maimaitijiang A., Liu R., Yan F., Hu H., Gao X., Shi H. miR-221-3p inhibits oxidized low-density lipoprotein induced oxidative stress and apoptosis via targeting a disintegrin and metalloprotease-22. J. Cell Biochem. 2019;120:6304–6314. doi: 10.1002/jcb.27917. [DOI] [PubMed] [Google Scholar]
- 153.Pereira-da-Silva T., Coutinho Cruz M., Carrusca C., Cruz Ferreira R., Napoleão P., Mota Carmo M. Circulating microRNA profiles in different arterial territories of stable atherosclerotic disease: A systematic review. Am. J. Cardiovasc. Dis. 2018;8:1–13. [PMC free article] [PubMed] [Google Scholar]
- 154.Coffey S., Williams M.J., Phillips L.V., Galvin I.F., Bunton R.W., Jones G.T. Integrated microRNA and messenger RNA analysis in aortic stenosis. Sci. Rep. 2016;6:36904. doi: 10.1038/srep36904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Coskunpinar E., Cakmak H.A., Kalkan A.K., Tiryakioglu N.O., Erturk M., Ongen Z. Circulating miR-221-3p as a novel marker for early prediction of acute myocardial infarction. Gene. 2016;591:90–96. doi: 10.1016/j.gene.2016.06.059. [DOI] [PubMed] [Google Scholar]
- 156.Sørensen S.S., Nygaard A.B., Nielsen M.Y., Jensen K., Christensen T. miRNA expression profiles in cerebrospinal fluid and blood of patients with acute ischemic stroke. Transl. Stroke Res. 2014;5:711–718. doi: 10.1007/s12975-014-0364-8. [DOI] [PubMed] [Google Scholar]
- 157.Gusar V.A., Timofeeva A.V., Zhanin I.S., Shram S.I., Pinelis V.G. Estimation of Time-Dependent microRNA Expression Patterns in Brain Tissue, Leukocytes, and Blood Plasma of Rats under Photochemically Induced Focal Cerebral Ischemia. Mol. Biol. 2017;51:683–695. doi: 10.1134/S0026893317040100. [DOI] [PubMed] [Google Scholar]
- 158.Nie X., Chen Y., Tan J., Dai Y., Mao W., Qin G., Ye S., Sun J., Yang Z., Chen J. MicroRNA-221-3p promotes pulmonary artery smooth muscle cells proliferation by targeting AXIN2 during pulmonary arterial hypertension. Vascul. Pharmacol. 2019;116:24–35. doi: 10.1016/j.vph.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 159.Villard A., Marchand L., Thivolet C., Rome S. Diagnostic Value of Cell-free Circulating MicroRNAs for Obesity and Type 2 Diabetes: A Meta-analysis. J. Mol. Biomark. Diagn. 2015;6:251. doi: 10.4172/2155-9929.1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wang L., Xu L., Xu M., Liu G., Xing J., Sun C., Ding H. Obesity-Associated MiR-342-3p Promotes Adipogenesis of Mesenchymal Stem Cells by Suppressing CtBP2 and Releasing C/EBPα from CtBP2 Binding. Cell. Physiol. Biochem. 2015;35:2285–2298. doi: 10.1159/000374032. [DOI] [PubMed] [Google Scholar]
- 161.Hezova R., Slaby O., Faltejskova P., Mikulkova Z., Buresova I., Raja K.R., Hodek J., Ovesna J., Michalek J. microRNA-342, microRNA-191 and microRNA-510 are differentially expressed in T regulatory cells of type 1 diabetic patients. Cell. Immunol. 2010;260:70–74. doi: 10.1016/j.cellimm.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 162.Eissa S., Matboli M., Bekhet M.M. Clinical verification of a novel urinary microRNA panal: 133b, -342 and -30 as biomarkers for diabetic nephropathy identified by bioinformatics analysis. Biomed. Pharmacother. 2016;83:92–99. doi: 10.1016/j.biopha.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 163.Cheng S., Cui Y., Fan L., Mu X., Hua Y. T2DM inhibition of endothelial miR-342-3p facilitates angiogenic dysfunction via repression of FGF11 signaling. Biochem. Biophys. Res. Commun. 2018;503:71–78. doi: 10.1016/j.bbrc.2018.05.179. [DOI] [PubMed] [Google Scholar]
- 164.Khalyfa A., Kheirandish-Gozal L., Bhattacharjee R., Khalyfa A.A., Gozal D. Circulating microRNAs as Potential Biomarkers of Endothelial Dysfunction in Obese Children. Chest. 2016;149:786–800. doi: 10.1378/chest.15-0799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hoekstra M. MicroRNA-499-5p: A therapeutic target in the context of cardiovascular disease. Ann. Transl. Med. 2016;4:539. doi: 10.21037/atm.2016.11.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Zhao L., Wang B., Zhang W., Sun L. Effect of miR-499a-5p on damage of cardiomyocyte induced by hypoxia-reoxygenation via downregulating CD38 protein. J. Cell. Biochem. 2020;121:996–1004. doi: 10.1002/jcb.29334. [DOI] [PubMed] [Google Scholar]
- 167.Neshati V., Mollazadeh S., Fazly Bazzaz B.S., de Vries A.A.F., Mojarrad M., Naderi-Meshkin H., Neshati Z., Mirahmadi M., Kerachian M.A. MicroRNA-499a-5p Promotes Differentiation of Human Bone Marrow-Derived Mesenchymal Stem Cells to Cardiomyocytes. Appl. Biochem. Biotechnol. 2018;186:245–255. doi: 10.1007/s12010-018-2734-2. [DOI] [PubMed] [Google Scholar]
- 168.Boštjančič E., Zidar N., Glavač D. MicroRNAs and cardiac sarcoplasmic reticulum calcium ATPase-2 in human myocardial infarction: Expression and bioinformatic analysis. BMC Genomics. 2012;13:552. doi: 10.1186/1471-2164-13-552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Salinas J., Lin H., Aparico H.J., Huan T., Liu C., Rong J., Beiser A., Himali J.J., Freedman J.E., Larson M.G., et al. Whole blood microRNA expression associated with stroke: Results from the Framingham Heart Study. PLoS ONE. 2019;14:e0219261. doi: 10.1371/journal.pone.0219261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Baldeón Rojas L., Weigelt K., de Wit H., Ozcan B., van Oudenaren A., Sempértegui F., Sijbrands E., Grosse L., van Zonneveld A.J., Drexhage H.A., et al. Study on inflammation-related genes and microRNAs, with special emphasis on the vascular repair factor HGF and miR-574-3p, in monocytes and serum of patients with T2D. Diabetol. Metab. Syndr. 2016;8:6. doi: 10.1186/s13098-015-0113-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lai E.C. Micro RNAs are complementary to 3’ UTR sequence motifs that mediate negative post-transcriptional regulation. Nat. Genet. 2002;30:363–364. doi: 10.1038/ng865. [DOI] [PubMed] [Google Scholar]
- 172.Guarino E., Delli Poggi C., Grieco G.E., Cenci V., Ceccarelli E., Crisci I., Sebastiani G., Dotta F. Circulating MicroRNAs as Biomarkers of Gestational Diabetes Mellitus: Updates and Perspectives. Int. J. Endocrinol. 2018 doi: 10.1155/2018/6380463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ibarra A., Vega-Guedes B., Brito-Casillas Y., Wägner A.M. Diabetes in Pregnancy and MicroRNAs: Promises and Limitations in Their Clinical Application. Noncoding RNA. 2018;4:E32. doi: 10.3390/ncrna4040032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhao C., Dong J., Jiang T., Shi Z., Yu B., Zhu Y., Chen D., Xu J., Huo R., Dai J., et al. Early second-trimester serum miRNA profiling predicts gestational diabetes mellitus. PLoS ONE. 2011;6:e23925. doi: 10.1371/journal.pone.0023925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Xu K., Bian D., Hao L., Huang F., Xu M., Qin J., Liu Y. microRNA-503 contribute to pancreatic beta cell dysfunction by targeting the mTOR pathway in gestational diabetes mellitus. EXCLI J. 2017;16:1177–1187. doi: 10.17179/excli2017-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sebastiani G., Guarino E., Grieco G.E., Formichi C., Delli Poggi C., Ceccarelli E., Dotta F. Circulating microRNA (miRNA) Expression Profiling in Plasma of Patients with Gestational Diabetes Mellitus Reveals Upregulation of miRNA miR-330-3p. Front. Endocrinol. 2017;8:345. doi: 10.3389/fendo.2017.00345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hromadnikova I., Kotlabova K., Dvorakova L., Krofta L., Sirc J. Postnatal Expression Profile of microRNAs Associated with Cardiovascular and Cerebrovascular Diseases in Children at the Age of 3 to 11 Years in Relation to Previous Occurrence of Pregnancy-Related Complications. Int. J. Mol. Sci. 2019;20:E654. doi: 10.3390/ijms20030654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.American Diabetes Association Diagnosis and classification of diabetes mellitus (Position Statement) Diabetes Care. 2009;32:S62–S67. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Metzger B.E., Coustan D.R. Summary and recommendations of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. The Organizing Committee. Diabetes Care. 1998;21:B161–B167. [PubMed] [Google Scholar]
- 180.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 181.Vandesompele J., de Preter K., Pattyn F., Poppe B., Van Roy N., de Paepe A., Speleman F. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol. 2002;3 doi: 10.1186/gb-2002-3-7-research0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Shapiro S.S., Wilk M.B. An Analysis of Variance Test for Normality (Complete Samples) Biometrika. 1965;3/4:591–611. doi: 10.1093/biomet/52.3-4.591. [DOI] [Google Scholar]
- 183.Dweep H., Sticht C., Pandey P., Gretz N. miRWalk—Database: Prediction of possible miRNA binding sites by "walking" the genes of three genomes. J. Biomed. Inform. 2011;44:839–847. doi: 10.1016/j.jbi.2011.05.002. [DOI] [PubMed] [Google Scholar]