Abstract
Blood is classified as a drug and transfusion is one of the most commonly performed procedures in the USA. General knowledge of blood manufacturing, shelf life and storage media, common component modifications, blood types, and product compatibility allows the clinician to better communicate their needs and to understand what options may be available when ordering blood products. All transfusions offer benefits, and the clinician must comprehend the possible adverse events, especially those related to TRALI, which continues to be the most common cause of transfusion-related death reported to FDA, with TACO as the second most-commonly reported event. Transfusing in the setting of hemorrhagic blood loss adds additional challenges regarding volume overload, coagulopathy, and optimum transfusion ratios of red cells, plasma, platelets, and cryoprecipitate. The information imparted in this chapter will help equip the clinician with the knowledge needed to make the best decisions for patients requiring blood products, especially injured patients.
Keywords: Transfusion, Trauma, TRALI, Hemorrhage, Additive solution, Storage, Red cell
Red Blood Cell: Manufacture, Storage, and Transfusion
Blood Collection and Manufacturing
Blood is classified as a drug and the collection and manufacturing processes of this industry are regulated by the US Food and Drug Administration (FDA) [1]. Throughout this chapter, references are made to the Circular of Information (COI), a joint publication of the AABB (formerly the American Association of Blood Banks), the American Red Cross, America’s Blood Centers, and the Armed Services Blood Program, which is also recognized by the FDA as an extension of the blood label. This important document is a useful guide to the clinician and is available online [2]. The most recent National Blood Collection Utilization and Survey (NBCUS) reports that 13,775,000 million allogeneic units of whole blood and red cells (RBCs) were transfused in 2011, which is 8.2 % fewer units than in 2008 [3]. Over 20 million blood components were transfused in 2011 (there is a lag time between the receipt and publication of such data in this and similar reports). Blood centers collected 93.4 % of all components and the remaining amount was collected by hospitals [3]. The USA continues to transfuse red cells at a greater rate than many other countries, with 44 transfusions per 1000 population; this however, is a >10 % decrease from 48.8 transfusions per 1000 population in 2008 [3].
Blood transfusion is a common medical treatment and was listed in the most recent Healthcare Costs and Utilization (HCUP, a quality database supported by Health and Human Services) report as being in the top five procedures for patients aged 1–44 and was the most common procedure for patients aged 45–85 and beyond [4]. Moreover, allogeneic blood donation is a voluntary, unremunerated process. All donations are tested for blood type, specific antibodies and infectious diseases; platelets are also tested for bacterial contamination before they are released [3]. Units with positive or reactive results are destroyed, with appropriate deferral of the donor, per FDA. About 9 million people in the USA donate blood per year, although it is estimated that a much larger percentage could qualify for donation [3, 5].
Whole blood is the unmanipulated product collected from a donor. Autologous blood donations are usually whole blood, though specific components may be drawn using automated collection devices. Allogeneic whole blood collections are separated into individual components soon after collection by centrifugation and manufactured into red blood cells (RBCs), plasma, or platelets destined to become pooled platelet products. Apheresis blood collection uses automated technology that allows for the targeted collection of red cells, single-donor platelets, plasma, and leukocytes (usually stem cells or granulocytes). Products may be collected singly or in multiples depending on donor qualification, the device, and FDA regulations. Plasma may be further manufactured into factor derivatives, albumin, and other medical products. Frozen plasma can be further manufactured into cryoprecipitate and cryoprecipitate-poor plasma. Blood products are a limited commodity with variable shelf-lives and the balance between supply and demand is dynamic, requiring cooperation between donors, blood centers and hospitals. Licensed blood products may be shipped across the USA to other areas in need.
Blood is collected into sterile, disposable, plastic bag sets which are manufactured to meet FDA specifications. Whole blood is collected through a large gauge needle (usually 16 or 17 gauge) by gravity flow from the donor’s arm and into the primary bag, which contains a citrated solution to prevent immediate clotting. Additive solutions extend the RBC storage time. Apheresis collections use specialized bag sets and automated instruments that are designed to continuously draw and centrifuge small volumes of blood, remove the desired component(s) and return the remainder, with minimal impact to the donor’s fluid balance.
ABO/Rh and Compatibility
The ABO blood group system was identified in 1900 by Landsteiner and colleagues and this is undoubtedly one of the most important medical discoveries, as prior to this time, there were myriad deaths due to transfusion incompatibility [6–8]. Variations or subtypes of the common blood types are occasionally seen and present patient blood typing challenges to the laboratory such that even routine blood orders require extra time to fulfill.
Codominant Mendelian inheritance of an A or B allele on chromosome 9q34 predicts blood type [9]. The A and the B allele each encodes for a glycosyltransferase which adds a sugar to the H antigen (FUT 1 gene, chromosome 19 q13.3) [10]. The H antigen resides on an oligosaccharide chain which extends beyond the RBC surface. Adding a specific sugar results in the formation of an A or B antigen [10]. Type O blood results from the homozygous inheritance of a nonfunctional allele (amorph) most commonly caused by a frameshift mutation, resulting in no glycosyltransferase being produced, and leaving the H antigen on the red cell unaltered [10]. The phenotypes of the ABO blood group system are based on expression of the A, B, and H antigens. A and B alleles are codominant. The O phenotype is recessive. In other words, if the genotype is AO the phenotype is A, and if the genotype is AB the phenotype is AB.
H carbohydrate is present on RBCs of almost every ethnic group worldwide and is the substrate upon which A or B antigens are formed [7]. Rarely, RBCs completely lack precursor H substance due to inheritance of two silent alleles of the H antigen, which is the hh genotype, also known as the “Bombay” phenotype [7]. Originally identified in Bombay, India in 1952 by Dr. Bhende, the complete lack of H antigen is seen in approximately 1 in 10,000 Asian Indians and 1 in 150,000 Japanese and is occasionally found in Caucasian populations at an incidence of approximately 1 in 1,000,000 [7].
A clinical example of this rare blood type is typified by a recent elderly patient who was hospitalized following a fall. She claimed that she had the Bombay phenotype, however, the staff did not deem the information to be important and the blood bank was not notified. After several unsuccessful attempts to crossmatch blood for the patient, the sample was referred to the immunohematology reference laboratory (RL) for identification. After extensive workup the Bombay phenotype was identified, and these findings were confirmed with the patient. Fortunately she did not require transfusion, as the only compatible blood for a person with the Bombay phenotype is from a donor with this precise phenotype. The point is that if a patient communicates that they have a rare blood type, the blood bank should be informed, in order to investigate it, and to allow adequate time to locate compatible blood. Such patients may participate in autologous donation and their red cells may be frozen for future use. Patients with unusual blood needs may wear an emergency alert bracelet stating their condition or may verbally relay the information to the clinical staff.
Type A RBCs express A surface antigen, and naturally occurring anti-B antibody is found in the plasma [11]. Type B RBCs express B antigen and anti-A antibody is present in the plasma. Type O RBCs lack A or B antigen and have anti-A and anti-B antibody in the plasma. Finally, type AB blood expresses both A and B antigens on the red cell surface and lack naturally occurring plasma antibodies [11]. Naturally occurring blood group antibodies, also called isohemagglutinins, are not present in the newborn (apart from antibodies present due to passive maternal transmission) but develop around 4–6 months of age by a thymus-independent mechanism following exposure to carbohydrate epitopes on gut bacteria and food [11]. A and B antigens are found on cardiac, gut, and renal endothelium (and other organs) and additionally exist in a soluble form in secretions; for this reason they are also known as “ histo-blood group antigens” and as such, are an important consideration in solid organ transplant [10] (Table 19.1).
Table 19.1.
| Blood and D (Rh) type by ethnicity and approximate percentages | Red cell antigen | Plasma antibody | ||||
|---|---|---|---|---|---|---|
| Caucasian | African-American | Hispanic | Asian | |||
| O | 44 | 49 | 55 | 43 | None | Anti-A and anti-B |
| A | 43 | 27 | 28 | 27 | A | Anti-B |
| B | 9 | 20 | 13 | 25 | B | Anti-A |
| AB | 4 | 4 | 4 | 5 | A and B | None |
| D (Rh) Pos. | 83 | 93 | 93 | 98 | ||
| D (Rh) Neg. | 17 | 7 | 7 | 2 | ||
ABO type compatibility is fundamental to avoiding a hemolytic transfusion reaction, which may occur within minutes of beginning the transfusion and with possibly fatal results. ABO antibodies are primarily of the IgM type, which fix complement well, and are capable of causing acute, intravascular hemolysis. ABO antibodies of the IgG subtype may cause a delayed, extravascular hemolysis. IgG subtypes may also cross the placenta from the maternal circulation to cause hemolytic disease of the fetus and newborn (HDFN) [12]. Antibodies from some blood group systems are more potent than those in other blood group systems in their ability to cause hemolysis [12]. Only one fatality resulting from ABO-mismatched RBCs was reported to FDA in 2013, accounting for 3 % of the total fatalities reported in that year [13]. Undoubtedly, many more ABO-mismatching events transpire without resulting in fatality. In 2011, a total of 42 such events were reported to the NBCUS, which amounted to 1 occurrence per 495,207 transfusions in the USA [3]. It is worth noting that not all hospitals participate in a program of voluntary transfusion reaction reporting, however fatalities due to transfusion must be reported to FDA [3].
Transfusion
Blood Type, Screen and Crossmatch
Persons with type O blood are often called the “universal donor” since their blood is compatible with all recipients. Type O blood is also the first choice of blood in emergency transfusion or trauma situations. Persons with A blood may receive type A or type O blood; persons with type B blood may receive type B or type O blood. Persons with type AB blood may be given any blood type and are sometimes referred to as being the “universal recipient” (Table 19.2).
Table 19.2.
Red cell type and compatibility
| Patient blood type | Compatible red cells for transfusion |
|---|---|
| O | O only |
| A | A or O |
| B | B or O |
| AB | O or A or B or AB |
The Rh blood group system is large and the D antigen is one of more than 50 Rh antigens found to date, but the presence or absence of the D antigen on RBCs is still commonly referred to as Rh-positive or Rh-positive, respectively. D antigen expression varies among ethnic groups (Table 19.1). With respect to transfusion, the D antigen is second in importance to the ABO blood group system. For routine transfusion every effort is made to match the ABO/Rh of the unit to the patient; for example, a patient with B-negative blood should ideally receive blood from a donor who is B-negative (type B, Rh-negative), but O-negative blood would be compatible. Anti-A and anti-B antibodies are naturally occurring and are present depending on blood type (Table 19.1). Non-ABO red cell antibodies are sometimes found in patient serum and are called “unexpected” alloantibodies. About 5 % of patients have unexpected alloantibodies. These antibodies have formed following exposure (usually from transfusion or pregnancy but possibly from other blood exposure) to red cells possessing antigens foreign to the recipient. Determination of RBC phenotype may be performed by serology and molecular testing and may help to predict what antibodies a sensitized person could make. Antibodies differ in their clinical significance, or in their ability to cause hemolysis and/or hemolytic disease of the fetus and newborn (HDFN) . Extra time may be needed by the blood bank to locate blood for patients with rare or multiple alloantibodies.
If a “type and screen” is requested, the “type” is the determination of the patient’s ABO and Rh type and the “screen” detects unexpected alloantibodies in the patient serum, such as anti-K (of the Kell blood group system), anti-Fy (of the Duffy blood group system) and so on. Multiple blood group systems are represented on screening and extended blood panels to improve the chances of detecting clinically significant alloantibodies. Once a person has formed an alloantibody, red cells negative for the offending antigen should be provided if possible, whether or not the alloantibody is detectable. If a “crossmatch” is requested, this is the pairing of patient serum against donor red cells and is the last check of compatibility prior to issue. If there is agglutination or hemolysis the unit is incompatible with the patient. Crossmatched units may be held in reserve for a time, depending on the institution’s policies. Emergency-release blood is usually O-negative or O-positive and is uncrossmatched and requires a physician’s signature to approve the product, either prior to, or in a specified time-frame following its release. Uncrossmatched blood is not necessarily incompatible.
RBC Transfusion
Patients require RBC transfusion in situations including hemorrhagic shock, other blood loss, and symptomatic anemia for myriad medical reasons including surgery, cancer treatment, and red cell exchange transfusion for sickle cell anemia. RBC and oxygen deficit in the patient is manifested by symptoms including fatigue, tachycardia, tachypnea, and hypotension. Informed consent must be provided and signed prior to transfusion of any blood product, by the patient receiving the transfusion or by a parent, guardian or person with power of attorney to make medical decisions. A “time-out” should be performed by staff administering the transfusion, prior to the infusion of each unit, to make sure the right patient is being transfused the correct blood product; every hospital should have a clear policy for such a protocol that is easily accessible by all staff. Certain religious faiths will decline blood product transfusion and their refusal should be respectfully honored and carefully documented according to hospital policy and applicable laws.
Standard blood infusion filter sets must be used when administering blood products, including granulocytes. These filter sets have pore sizes ranging from 150 to 260 μm, which trap tiny clots and particulate aggregates, but still allow blood cells to pass through [2].
Routine transfusions should be administered slowly, especially in the first 15 min, in order to watch for the possibility of a transfusion reaction. Vital signs (temperature, blood pressure, heart rate, and respiratory rate) should be taken prior to the infusion and periodically during and then after the transfusion is complete. Oxygen saturation is useful if available. The remainder of the unit may be transfused at a slightly faster rate, with the goal of infusing a RBC unit over 2–4 h. Rapid infusion, unless medically necessary, should be avoided to mitigate the risk for transfusion-associated circulatory overload (TACO). Although many blood products will not require 4 h to infuse, the COI states that blood products must be infused within 4 h of entry into the bag [2]. If the amount of ordered product cannot be infused within 4 h, request that the blood bank prepare aliquots, or smaller amounts, to avoid product wastage. Pediatric blood products are often aliquoted into regular-size transfer bags, smaller bags designed for pediatric use, or into syringes.
All suspected transfusion reactions should be clinically managed and reported to the blood bank. The most common symptom of a transfusion reaction is fever; however, if a transfusion reaction is suspected for any reason, stop the transfusion and keep the line open with saline and manage the patient clinically.
The Rationale of Switching from O-Negative to O-Positive Blood
The first choice of blood product in a patient of unknown blood type is O, since blood type O possesses no A or B red cell surface antigens and is therefore more likely to survive in the plasma of any recipient. Once the blood type of the patient is determined, and this is usually determined soon after arrival, type-specific blood is given. Upon receiving an alert of an incoming trauma or for emergency blood needs, most hospitals automatically issue 2 or more O-negative RBC units at once, unless the patient’s blood type is already known. As the supply of O-negative blood is limited by the small percentage of donors possessing this blood type (usually around 6 %), good stewardship is necessary. Hospitals often choose to add an O-negative switching protocol to aid clinicians in this endeavor.
In most protocols of this type, women of childbearing potential (or age) receive O-negative blood until their blood type is known. What constitutes childbearing age is determined by each institution but is generally accepted to be females under the age of 45 or 50. If a woman of childbearing age is indeed O-negative, this is the blood type she should continue to receive, to decrease her risk of forming a potentially deadly anti-D antibody that is capable of crossing the placenta and targeting the fetus’ RBCs. Another group that may automatically receive O-negative blood is all patients under 18 years of age, male or female. For women beyond childbearing age and all males greater than 18 years, O-positive blood may be dispensed right away. This approach has been adopted in many large, urban institutions as the need for emergency or trauma blood could never be sustained if only O-negative units were used. Once the patient’s blood type is known, type-specific or compatible blood should be given. An example of a switching protocol is illustrated in Fig. 19.1.
Fig. 19.1.
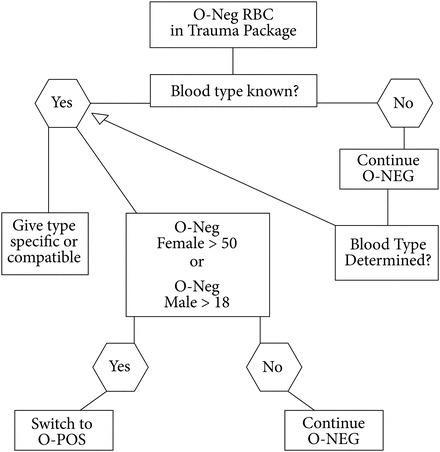
Example of O-Negative Switching Protocol O-negative RBCs are released for trauma and emergency use in most hospitals. If the patient’s blood type is known, type specific or compatible blood should be issued. If the blood type is not known, O-negative blood should be transfused until a blood sample has been sent to the blood bank for ABO/Rh determination and once blood type is known, type specific or compatible blood should be given. If the patient is a woman beyond childbearing years (usually accepted as being older than 45 or 50 years of age), or a male beyond the age of 18 years; some centers switch these patients to O-positive RBCs upon arrival. All women of childbearing capacity and all patients below 18 years of age (pediatric patients) should receive O-negative blood until their blood type is known, and then they should receive type-specific or compatible blood
In transfusion situations that are more serious than what can be managed by an MTP, some hospitals have instituted a catastrophic transfusion protocol (CTP) option which doubles or triples the amount of product that is offered in an MTP package. In these situations, in which very heavy bleeding occurs, it is permissible to temporarily switch a patient from O-negative to O-positive and then switch back to O-negative when the bleeding has stabilized. This approach also allows for better inventory management of a limited resource. Rh immune globulin should not be given to O-negative patients after the infusion of O-positive red cells, but may be considered if an O-negative person has received Rh-positive platelets; consultation with the blood bank or pharmacy may be helpful in such cases.
Intraoperative Blood Salvage
An autotransfusion service (ATS) may be available at medical institutions with robust surgical or trauma services. Program oversight is usually provided by the transfusion medicine, anesthesia or surgery department and procedures are ideally performed by a perfusionist or other specially trained personnel. The service may or may not be accredited by the AABB.
Specialized instruments, or “cell savers,” may be used during planned or emergency surgery in which blood loss is excessive (equal to or greater than 20 % total blood volume loss), for patients with religious objections to receiving allogeneic blood and for patients with known multiple alloantibodies or rare blood types. ATS teams on-call allow for a rapid response and instruments may be partially set-up ahead of time.
Various instruments on the market function in essentially the same manner: intraoperatively shed blood is gently suctioned to preserve red cell morphology and function, washed with an isotonic solution, filtered, and reinfused either intraoperatively or postoperatively. Sponges used intraoperatively may also be washed and rinsed and that fluid can be added into the circuit. Abdominal, thoracotomy, and drain blood from other surgical sites may be processed. Extracorporeal anticoagulation is achieved with heparin (up to 30,000 units per liter of normal saline) or citrate solutions (often ACD-A, which is anticoagulant citrate dextrose, solution A) or a combination of the two. The filters have fairly large pore sizes (40–120 μm) to remove debris such as bony spicules or cement and large cellular aggregates. Due to the washing phase, very little plasma or its solutes (free hemoglobin, interleukins, hemostatic factors, and so on) remains in the final product.
Depending on the processing, the final product may be kept at room temperature for up to 4 or 6 h, or at 1–6 ° C for up to 24 h in a monitored refrigerator [14, 15]. Since the whole-blood product is freshly obtained from the patient and washed, some transfusion reaction risks are reduced, but reactions may still occur, such as from fluid overload or bacterial contamination [16]. The final red cell product is of high quality, with a hematocrit between 40 % and 80 % depending on the device and method used, and is suspended in a small amount of isotonic solution with very little remaining anticoagulant. It has been shown that the red cell survival of cell saver units obtained during bypass surgery are comparable to circulating venous blood after 24 h time [17].
Literature is not abundant regarding the consistent use of the cell saver in the setting of trauma, specifically regarding the quality of chest blood as most current cell saver data are obtained from planned cardiothoracic surgeries. Direct reinfusion of unwashed shed blood does not appear to be well-supported in the setting of trauma, though more studies are needed in this area to clarify the risks and benefits. A recent prospective study of unwashed thorax (pleural) blood from 22 patients at a large trauma hospital was conducted to characterize the solutes present in shed chest blood [18].
An ATS may help the hospital significantly reduce allogeneic red cell costs and meet the aims of its blood management program. Receipt of fewer allogeneic units reduces donor exposure, possible alloimmunization, and some transfusion risks, but beware of the possible coagulopathy which may accompany its use in some patients. Collaboration between the service providing the blood and/or overseeing the cell-saver program and the end-user services, in accordance with AABB guidelines, is essential in order to establish evidence-based guidelines, and to cover topics such as what surgical situations might constitute an absolute (open bowel) or relative contraindication (malignancy) for use of the cell saver [15].
Composition, Shelf Life, and Storage
RBCs, whether separated from whole blood or obtained directly from apheresis collections, are manufactured in such a way that the residual plasma volume is minimal (5–10 mL) [19]. The volume of allogeneic whole blood collections ranges from 400 to 550 mL and the hematocrit of a whole blood unit is approximately that of the donor’s [2]. Donors may not have a pre-donation hematocrit less than 38 % in accordance with FDA collection guidelines [2]. RBCs are collected into anticoagulant/nutritive solutions containing the following solute combinations: citrate–phosphate–dextrose (CPD), citrate–phosphate–dextrose–dextrose (CP2D), and citrate–phosphate–dextrose–adenine (CPDA-1) [2, 20]. Citrate chelates ionized calcium in the donor’s blood to suspend the coagulation cascade and inhibit clotting. Phosphate and dextrose directly provide nutrients to the RBCs. Adenine is a nucleic building block that is added to some RBC solutions (CPDA-1) and additive solutions, allowing shelf life to exceed 3 weeks [2, 20]. RBCs collected in CPD and CP2D have a shelf life of 21 days, and those collected in CDPA-1 have a shelf life of 35 days. The volumes of RBC units vary between 225 to 350 mL with a hematocrit ranging from 65 % to 80 % (average 75 %) [2, 20].
Additive solutions currently available in the USA are: AS-1 (Adsol, Fenwal), AS-3 (Nutricel, Haemonetics), AS-5 (Optisol, TerumoBCT), and AS-7 (SOLX, Haemonetics) [2, 20]. These solutions add an additional 100 or 110 mL of fluid, post-collection, to the RBCs which are originally collected into the anticoagulant/nutrient solution [2, 20]. Additive solutions contain combinations of phosphate, adenine, mannitol, dextrose (glucose), and additional citrate. The solutes provide nutrients and help stabilize the RBC membranes, allowing for increased storage times [2, 20]. These units have a hematocrit of 55–60 %, a unit volume around 300–400 mL, and a shelf life of 42 days [2, 20].
One unit of RBCs is expected to raise the hemoglobin by 1 g/dL and the hematocrit by 3 % in an “average-sized adult”; however, this is a broad statement which cannot apply to every clinical setting. Pediatric patients should be transfused according to weight, usually at a dose of 10–15 mL/kg [21]. One milliliter (mL) of RBCs contains 1.08 mg (mg) of iron [22]. Thus if 200 mL RBCs are donated, approximately 200 mg of iron is lost by the donor and that same amount is ultimately transfused into the recipient [22]. Hemoglobin levels are not an accurate predictor of iron stores and this is currently an area of great interest regarding US blood donors [22]. The 2012 REDS-II donor iron status evaluation (RISE) study results reported absent iron stores (ferritin < 12 ng/mL) in as many as 27 % of frequent female donors and 16 % of frequent male donors [22]. Conversely, the issue of iron overload may exist in blood recipients. Clinically significant iron accumulation may be seen following the transfusion of 50 or more RBC units and possibly sooner in pediatric patients [23]. The total amount of iron transfused may be calculated using the following equation, where Kin is the total amount of iron infused:
Iron is stored in the body as soluble ferritin or as insoluble hemosiderin [23, 24]. Frequently transfused patients have increased morbidity associated with tissue iron deposits in the heart, endocrine organs, and liver [23, 24]. Patients with hemoglobinopathies, hematological malignancies, inherited or acquired anemias, and myelodysplasias are most vulnerable. Depending on the clinical situation, chelation therapy and red cell exchange or erythrocytapheresis, rather than simple transfusion, may benefit some patients [23, 24].
Component Modification
Clinical indications for modified components vary and it may be advantageous to consult with the reference laboratory, blood bank, or a transfusion medicine pathologist prior to ordering these products. Not all products are readily available and considerable time may be required to manufacture or obtain some blood products.
Leukocyte Reduction (and Provision of CMV-Negative Blood)
Leukocyte reduction, or leukoreduction (LR), of RBCs or platelets is a widely performed component modification. Pre-storage LR is done during automated apheresis collections or after whole blood collection. Bedside LR, or post-storage LR, remains an alternate but infrequently chosen option. To qualify as a “Leukocyte Reduced” product, the residual white cell count must be less than 5 × 106 per unit per FDA criteria, which may be easily met by use of any of the current third and fourth generation LR filters [25]. LR of RBCs decreases the incidence of febrile non-hemolytic transfusion reactions, HLA and platelet alloimmunization, and the amount of biologic response modifiers (BRMs), which accumulate during product storage [26–28].
The equivalency of LR to CMV-negative products continues to be debated. Some physicians consider LR blood to be adequate and essentially equivalent to LR blood that is from CMV-seronegative donors. The rationale is that CMV resides within white cells, and with the efficiency of modern LR filters, any risk of CMV would be exceptionally low [29–31]. For CMV-seronegative patients, especially those who are peri- or post-transplant, or low birthweight infants, many clinicians request CMV-negative products and accept LR-only products if CMV-negative and LR products are unavailable [29–31]. In addition, CMV-seronegative donors who test “negative for CMV” on their most recent donation carry a small but real risk of transmitting CMV to a recipient, if the donor happens to be newly infected and is in the window period (the time between infection and the time at which the infection can be detected by testing) [29–31]. The test performed on donor blood detects anti-CMV antibodies [29–31]. Nucleic acid testing (NAT) testing for CMV DNA is available but is not used for donor testing [29–31]. Frequent donors (such as platelet donors) have a theoretically higher risk of transmitting CMV since they are able donate several times during the 6–8 week window period, whereas a single red cell donor can only donate a single unit in the same period of time [29–31]. Indications for CMV-negative blood include the following populations: CMV-seronegative patients who are immunocompromised, fetuses, pregnant females, very-low and low-birthweight infants, transplant recipients of either hematopoietic stem cells or solid organs, and any severely immunocompromised patients including those with HIV.
Again, it must be stated that LR components may suffice in certain clinical situations and when CMV-negative blood is unavailable and the patient requires transfusion [2, 32]. LR should not be confused with the use of standard blood infusion filter sets used when administering blood products. These filters have pore sizes ranging from 150 to 260 μm, to trap large cell and particulate aggregates, but still allow blood cells to freely pass (for reference, RBCs are about 5 μm in diameter) [2, 33].
Washing
Washed RBCs (or platelets) are indicated in cases of very severe or progressively worsening allergic or anaphylactic transfusion reactions to cellular blood products and patients known to be IgA- deficient [34, 35]. Washed cellular products may also be requested for pediatric patients with renal impairment, elevated potassium and related issues, to remove excess potassium in the blood product [34, 35]. However, for the vast majority of patients, the amount of potassium in the plasma should not have any untoward effects on the recipient even if the RBCs are irradiated and near the outdate, if infusions are given slowly, over 2–4 h [34, 35].
Frozen RBCs )must also be washed prior to infusion, to remove the glycerol in which they are stored [20]. RBCs (and platelets) are washed by specialized, automated instruments that progressively wash a single unit in normal saline, and sometimes dextrose, to create a final product that is essentially devoid of plasma and which contains a minimal amount of saline [20]. The final product is usually left in the wash bag, which resembles a flat doughnut. A small percentage of product is normally lost during the washing process [20]. The hematocrit of the RBC product is usually around 75 % with a volume of 180 mL [20].
Up to two additional hours of time may be required to produce a single, washed product. It is important to communicate to the reference lab or blood bank, the time frame in which the product will be needed [2]. Washing changes the expiration date of RBCs to 24 h, stored at 1–6 °C (washed platelets expire in 4 h and are stored at 20–24 °C), or the original expiration date and time, whichever comes first [2]. Requests for washed plasma are not possible to fulfill for obvious reasons. Plasma for IgA- deficient patients should come from donors who are IgA-deficient. Such products are rare and may require nation-wide coordination with such entities as the American Rare Donor Program (ARDP) to identify possible donors and request that they come in for donation [36]. Altogether, several days’ time may be needed to procure the donation, receive the donor’s infectious disease testing results and to transport the product to the patient’s location.
Irradiation
Cellular products (RBC, platelets) may be irradiated to preclude the development of transfusion-associated graft-versus-host disease (TA-GVHD), which is a donor T-cell mediated destruction against the recipient’s immune system. Plasma and cryoprecipitate are by definition, acellular and should not require irradiation. TA-GVHD is most-commonly caused by the infusion of competent donor T-lymphocytes into an immunocompromised recipient, though there have been cases involving immunocompetent recipients [37]. LR is inadequate in comparison to irradiation for preventing TA-GVHD, since even with the most recent LR filters residual leukocytes remain and there is no known minimal threshold of T-cells needed to trigger the reaction [38]. TA-GVHD is similar to post-transplant GVHD, affecting HLA-antigen-dense tissues such as the skin, gastrointestinal tract and liver [38]. There are, however, two findings seen with TA-GVHD: bone marrow aplasia and an earlier onset, usually between day 2 and day 50 following transfusion, which distinguishes it from post-transplant GVHD [38].
Irradiation of cellular blood products is accomplished by X-ray irradiators or gamma-ray irradiators specifically manufactured for blood establishments, or by linear accelerators used in the field of radiation oncology [39]. Linear accelerators are also used for blood irradiation in developing countries and other areas where dedicated blood bank irradiators unavailable [39]. Irradiation causes the damage to the red cell membrane and escape of intracellular potassium, which increases with the age of the red cell and over storage, but is not usually harmful to the recipient [34, 35, 40]. Hyperkalemia has been reported in pediatric patients when large volumes are given or blood is quickly infused, however washing irradiated red cells prior to infusion can remove the supernatant potassium if the clinician is concerned [34, 35, 40]. The use of X-ray compared to gamma rays have not been shown to be significantly different in their effects on red cell membranes [41].
The isotope decay of cobalt-60 or cesium-137 produces gamma-rays, providing the energy source for nuclear irradiators. These radioactive sources are sealed within the body of the instrument and require increased security controls [42]. X-ray irradiators and linear accelerators both emit X-rays and this form of energy is known as ionizing radiation [42]. Whatever energy source is used, irradiation renders residual allogeneic T-lymphocytes incapable of replication by rendering inactive the DNA of leukocytes to a level greater than 5 logs [42]. Mature red cells and platelets lack nuclei and are not affected in the same manner as white cells. Red cells outdate at 28 days from the date of irradiation, or keep the original expiration date, whichever comes first. Platelets retain their usual date of expiration, post-irradiation.
Per FDA criteria the dose to the center of the irradiation chamber must be 25 Gray (Gy) and the dose at any point in the periphery must be 15 Gy, never exceeding 50 Gy at any point in the chamber [43]. Irradiated cellular products may be routinely provided for the following patient needs: intrauterine transfusion, premature, very-low or low birth weight infants, infants needing exchange transfusion, any child suspected of or persons with known congenital immunodeficiency, pediatric extracorporeal membrane oxygenation (ECMO), patients with lymphomas and leukemias, any profoundly immunosuppressed patients with solid tumors, patients on nucleoside (purine) analogs or T-cell function altering drugs (examples: clofarabine, alemtuzumab, fludarabine) .
Components that must be irradiated include donations from family members who are blood-related to the recipient, any human-leukocyte-antigen (HLA)-matched products, and granulocytes [33, 38, 44, 45]. It is not standard practice to irradiate blood for most patients undergoing whole organ transplantation or patients with HIV/AIDS as the sole diagnosis [33, 38, 44, 45].
Component irradiation is performed to prevent interactions from possible human leukocyte antigen (HLA) similarities between donor and recipient [43]. Shared HLA haplotypes are more commonly seen among blood-related family members (consanguinity) or in communities lacking HLA diversity [43]. If the recipient is transfused with T-cells that share an HLA haplotype with a donor who is homozygous for that haplotype, the recipient will not view the donor’s cells as foreign and will allow them to enter the body without opposition. [43]. However, in time the donor’s cells may come to view the recipient as foreign and mount a response to destroy the recipient; this is known as TA-GVHD) [43].
Adverse Events Related to Transfusion
Transfusion complications, or transfusion reactions, may be broadly divided into infectious and noninfectious causes. Donor screening begins prior to the actual donation, with the reading of educational materials, a brief physical exam and completion of a donor history questionnaire; at each step the donor may self-defer or may be deferred. If all criteria are met, a donation may take place. Every time a donor is drawn for allogeneic transfusable products, blood samples from that donation undergo testing for blood ABO and Rh type, unexpected red cell antibodies and infectious disease testing. Tests for the following infectious diseases are also performed in accordance with FDA guidelines: human immunodeficiency virus (HIV) types 1 and 2, hepatitis B and C virus, human T-cell lymphotropic virus (HTLV) types I and II, Treponema pallidum (the organism that causes syphilis), and West Nile Virus (WNV). Donors must be negative for antibodies to the parasite Trypanosoma cruzi, which causes Chagas disease, once in their donation lifetime. In regards to other infectious diseases, the donor questionnaire is written in a way such that donors with the possible risk of transmitting diseases such as malaria or hepatitis A are deferred from donation that day. Testing for cytomegalovirus (CMV) and HLA antibodies may be additionally performed. Donors may be temporarily, indefinitely, or permanently deferred based on the criteria set by FDA or AABB [46]. Criteria for autologous donation are not as strict.
Much of the infectious disease testing is antibody-based and detects the donor’s immune response to the offending agent. Adequate time, days to weeks, must pass until antibodies form; this also known as the window period [47–49]. Nucleic acid testing (NAT) detects viral nucleic acid particles and has greatly reduced the window period to just days [47–49]. NAT is used for detection of HIV-1 RNA, hepatitis B virus DNA, hepatitis C virus RNA, and WNV RNA [47–49]. For example, prior to NAT testing for HIV-1, the window period for detection of antibody formation, even with third generation tests was 21–24 days after infection; in contrast, NAT testing reduces the window period to less than 10 days [47–49] (Table 19.3).
Table 19.3.
| Blood donor test | Risk of infection per number of transfused units |
|---|---|
| HBV | 1:800,000 to 1:1,200,000 |
| HCV | 1:1,100,000 |
| HIV | 1:1,500,000 |
| WNV | Very rare; two cases reported 2008–2014 |
| HTVL | 1:641,000 |
| Chagas | Very low, no cases since screening has been implemented (FDA, 2010) |
| Syphilis | Very low, no cases in last 40 years |
| Bacterial contamination of platelets | 1:3000 |
Blood donation is not a right and the FDA’s primary responsibility is to ensure that the blood supply is safe for recipients. Despite thorough donor health screening and skin site prep, it has been estimated that approximately 1 in 2000 blood products are positive for bacterial contamination, though most are presumed to be normal skin flora which do not survive well at colder temperatures (RBC and plasma storage) [50, 51]. For this reason, the majority of implicated contaminated blood products are platelets, as they are stored at 20–24°C, which is fairly close to room temperature.
Following donation, a representative sample is taken from every platelet and is tested for bacterial growth prior to release. Since platelets are stored at room temperature, there are more reports of sepsis related to platelet products than any other blood product. RBCs are not prospectively tested for bacterial contamination, and are uncommonly implicated in septic reactions, but when they are, it usually involves an organism that thrives at colder temperatures, such as Serratia spp., since red cells are stored at 1–6 °C.
With the numerous current screening and testing measures set into place and the relatively low risk transfusion-transmitted infection, focus has shifted to the noninfectious complications of transfusion. Transfusion-related acute lung injury (TRALI); transfusion-associated circulatory overload (TACO); hemolytic reactions, both acute and delayed; transfusion-associated graft-versus-host disease (TA-GVHD); febrile non-hemolytic transfusion reaction (FNHTR); allergic/anaphylactic; and post-transfusion purpura (PTP) encompass the major noninfectious complications of transfusion (Table 19.4). Of these, only TRALI and TACO are discussed in detail.
Table 19.4.
| Entity | Etiology | Incidence |
|---|---|---|
| Immediate reactions | ||
| Urticarial (allergic) | Patient response to donor Ag | 1:100 to 1:300 |
| Febrile non-hemolytic transfusion reaction (FNHTR) | Patient antibodies to donor WBC or cytokines in component | 1:100 to 1:1000 |
| Transfusion-related acute lung injury (TRALI) | Donor anti-WBC antibodies, pro-inflammatory molecules/biologic response modifiers | 1:500 to 1:63,000 |
| Anaphylactic/anaphylactoid | IgA-deficient pts with anti-IgA antibodies; antibodies to cytokines, haptoglobin or C4 | 1:20,000 to 1:50,000 |
| Hemolytic transfusion reaction (HTR) | ABO-mismatch | 1:76,000 |
| Immunologic, delayed | ||
| Hemolytic (non-ABO) | Patient anamnestic response to RBC antigens | 1:2500 or rarer |
| Transfusion-associated graft-versus-host disease (TA-GVHD) | Donor destruction of patient immunity | Rare |
| Post-transfusion purpura (PTP) | Patient anti-HPA 1a Antibodies destroy donor platelets | Rare |
| Non-immunologic, immediate | ||
| Sepsis | Bacterial contamination | Depends on component |
| Transfusion-associated circulatory overload (TACO) | Volume overload | Less than 1:100 |
|
Other Possible Events Air embolus, non-immune hemolysis, hypothermia, hypotension with ACE-inhibitors, citrate toxicity, and hypocalcemia | ||
Transfusion-Related Acute Lung Injury (TRALI)
TRALI continues to be a significant and under-reported cause of transfusion-related morbidity and mortality in the USA. TRALI has previously been reported in medical literature as occurring as frequently as 1 in 3000 to 1 in 5000 transfusions but the true incidence of TRALI in the USA is unknown as all transfusion reaction reporting is currently voluntary [52]. Critically ill patients (ICU) have up to an 8 % incidence of TRALI; and has been reported in up to 15 % in patients with gastrointestinal bleeding and 30 % in patients with end-stage liver disease [53, 54]. The vast majority of patients with TRALI recover within 96 h, with aggressive, supportive treatment [52, 55]. Recent data from Medicare billing files have concluded that TRALI is much more prevalent than expected in the elderly, which makes sense because the incidence of ALI increases with age [56–58]. With respect to TRALI in pediatric patients, a recent large review performed by the Canadian Blood Services showed that the incidence of reported TRALI was not much different in children (5.58 per 100,000 transfusions) compared to adults (3.75 per 100,000 transfusions) [59].
The outcomes of these studies also reiterate that the incidence of TRALI is much greater in comparison to the data published by NBCUS, which is a voluntary data reporting program. There were 327 reports of TRALI submitted to the NBCUS in 2011 for an incidence of 1:63,940 transfused components [3]. The reporting of any death suspected to be related to transfusion, however, is mandatory per FDA [13]. During fiscal years 2009–2013, 38 % of all transfusion-related deaths reported to FDA were confirmed to be TRALI-related [13]. In fiscal year 2013, FDA reported that 37 % of all transfusion-related deaths were attributable to TRALI. Regarding the 14 TRALI-related deaths in 2013, 51 donors were implicated [13]. Gender data were available for 49 of the donors; 22 were male and 27 were female [13]. Thirty-eight of the donors were tested for the presence of HLA and HNA antibodies and ten of the 14 implicated donors reportedly had antibodies against cognate antigens in the recipient [13]. The majority of the deaths were among patients who received RBC transfusions alone or in patients who received multiple blood products [13].
Post-transfusion reactions consistent with what would now be described as TRALI were first reported in the medical literature in the 1950s; however, the coining of the term “TRALI” is attributed to Popovsky and Moore in the mid-1980s as the constellation of findings and symptoms temporally related to transfusion were unified under one diagnosis [60–62]. The diagnosis of TRALI begins with the recognition of acute lung injury (ALI) in the patient, defined by the American-European Consensus Conference as SpO2 < 90 % or PaO2/FiO2 > 300 mmHg on room air or other demonstration of hypoxemia and bilateral pulmonary edema seen as lung infiltrates by frontal chest radiograph [63]. A combined definition of TRALI, as defined by the National Heart, Lung and Blood Institute Working Group and the Canadian Consensus Conference is an acute, non-cardiogenic lung injury occurring within 6 h of beginning a transfusion (though symptoms are often seen in the first 1–2 h) with respiratory symptoms of tachypnea, dyspnea, pulmonary edema which may be mild to severe and sometimes seen as acomplete “white-out” on frontal chest X-ray [64]. Frothy secretions are sometimes seen coming from the patient’s mouth or endotracheal tube. If measured, the pulmonary artery wedge pressure should be less than 18 mmHg and there must not be any new, abnormal cardiac function [64]. Per this definition, TRALI may also be diagnosed in a patient with worsening preexisting pulmonary insufficiency (unique to the NHLBI definition), such as COPD or pulmonary fibrosis [64]. A diagnosis of possible TRALI may apply to patients with preexisting clinical risk factors for ALI, such as recent surgery, burn injury, coagulopathy, chronic alcoholism, sepsis, and carcinoma [64]. There may be hypotension (hypertension followed by hypotension may be seen), fever, chills, non-productive cough, and transient decreases in white cell counts, especially neutrophils [64–66].
TRALI is diagnosis of exclusion and septic transfusion reaction, volume overload, severe anaphylaxis or a newly manifesting medical problem are often in the differential. If TRALI is suspected during the infusion of multiple consecutive products, all products given to that point within a 6-h time frame are implicated.
All routinely transfused blood products (whole blood, RBCs, platelets, plasma, and cryoprecipitate) have been implicated in the diagnosis of TRALI [52]. Granulocyte and hematopoietic progenitor cell (HPC) products have also been associated with TRALI. Case reports have linked TRALI with the administration of immunoglobulin, first documented in 2001 [67–69].
The pathophysiology of TRALI is attributed to factors present in both the recipient and the transfused blood product. Up to 85 % of TRALI cases may be explained by the infusion of donor antibodies as demonstrated in an ex vivo animal model using isolated perfused rabbit lungs [70]. In these studies, antibodies against human leukocyte antigens (HLA) or human neutrophil antigens (HNA) had the ability to bind to neutrophils which expressed the cognate antigen and induce pulmonary edema [70]. However, the antibody, the cognate antigen on the leukocyte surface, and source of complement (plasma) had to be present in order for ALI to occur and if any of the components was omitted, lung damage was obviated [70]. This model has been refined using rats and demonstrated that a minimum number of antigen sites needed to be present on the neutrophils such that antibody binding must reach a threshold before ALI would occur [71]. This work was also relevant in showing that priming with fMLF (N-formyl-methionine-leucine-phenylalanine,a component of bacterial cell walls) allowed anti-HNA antibodies to directly activate neutrophils in the absence of complement [71].
In vivo TRALI models have demonstrated that a specific monoclonal antibody could cause ALI at a concentration seemingly similar to relatively well patients who come in for a transfusion and develop TRALI [72]. However, in an animal model, when the mice were housed in a pathogen-free environment no TRALI was demonstrated indicating a likely two-event model [72, 73]. Such an in vivo two-event pathogenesis was confirmed in a rat model which also demonstrated that lipids and other biologic response modifiers (BRM) could cause TRALI in older, stored RBCs irrespective of leukoreduction [74]. Both antibodies to MHC class I ligands and the lipids from stored RBCs were capable of priming quiescent neutrophils (PMNs), activating primed PMNs (defined as superoxide anion production and release of granule constituents), and inducing ALI [74]. Specifically, rats that were infused with endotoxin (lipopolysaccharide, or LPS) alone did not develop ALI, however those rats who received LPS and then received a lipid extraction from 42-day-old RBCs did develop ALI [74]. Importantly extractions from fresh (day 1) RBCs or plasma did not result in ALI [74]. In addition, antibodies to common MHC class I or even class II antibodies caused ALI as the second event in this animal model of TRALI, indicating that TRALI, whether caused by antibodies to specific leukocyte antigens or due to BRMs that directly prime PMNs, appears to be the results of two distinct events [74]. The first event is the clinical condition of the patient, which predisposes him to TRALI and the second event is the infusion of the specific antibody or BRM into the patient which activates the sequestered PMNs inducing damage to the vascular endothelium, resulting in capillary leak and ALI [52, 74].
Antibodies implicated in TRALI include those against class I or II HLA and antibodies against HNA [52, 55, 75]. Antibodies to HLA class II antigens have a two-event pathophysiology that differs due to their recognition of these surface antigens on antigen - presenting cells and the in vivo modeling supports the threshold or two-event model [76]. Antibodies to HNA loci, especially HNA-3a, also are postulated to cause TRALI by a two-event pathogenesis as well as inducing TRALI by activating the pulmonary endothelium alone through the CTL-2 receptor [77, 78]. Such direct activation may occur without PMNs and could cause TRALI in neutropenic patients [77]. Other BRMs include soluble CD40 ligand (sCD40L) which has been shown to prime PMNs and are linked with clinical TRALI [79]. Whether due to antibodies or other BRMs, the majority of TRALI cases are the results of PMN activation inducing pulmonary endothelial damage [52]. Histologically, TRALI is indistinguishable from etiologies of diffuse alveolar damage, which include acute interstitial pneumonia, early acute respiratory distress syndrome (ARDS), and others [80, 81]. The two pathways by which TRALI may occur are not mutually exclusive and many patients have cognate antigens to transfused antibodies, yet do not develop TRALI, lending credence to a “threshold” or two- event model [52, 73, 75, 82].
Mitigation
TRALI mitigation strategies are vital to reducing morbidity and mortality related to this transfusion complication. During the 1990s the UK National Blood Service created a voluntary hemovigilance program, launching the Serious Hazards of Transfusion (SHOT) and were the first to collect plasma from male donors, after noting that TRALI or probable TRALI was seen almost seven times more frequently with plasma transfusion and about eight times more frequently with platelet infusion, (in comparison to TRALI occurrence in red cells) when these products were collected from female donors [83]. Their efforts were rewarded following the adoption of this collection strategy for platelets and plasma, and reports of TRALI from plasma transfusion fell from 15.5 cases per million units transfused (1999–2004) to 3 per million (2005–2006) for plasma and from 14 cases per million to just under six cases per million for platelet products [83]. Densmore and colleagues also showed that HLA antibody formation increased with pregnancy, with about 8 % of never-pregnant females showing sensitization, increasing to 15 % of women after one pregnancy, and to about 26 % after three pregnancies [84]. Never-transfused men and never-pregnant women have a 1.7 % prevalence of HLA antibodies [85]. The American Red Cross (ARC) examined their own hemovigilance data and subsequently adopted a similar strategy of collecting plasma from predominantly male donors (95 %) and saw a significant (80 %) decrease in TRALI cases related to plasma infusion [86]. This similar and dramatic decrease in TRALI when female donors were avoided was also shown by Toy and colleagues, who designed a prospective study involving two major academic centers [87].
Effective April 1, 2014, the 29th edition of the AABB Standards outlined one facet of TRALI mitigation [33]. Standard 5.4.1.2 states that for the collection of plasma and whole blood for allogeneic donation, donations must be from males, never-pregnant females, or females with a history of pregnancy only if they have been tested for HLA antibodies since their last pregnancy and are found to be negative [33]. Many institutions have proactively extended this AABB Standard to the collection of platelets, switching their HLA-positive female donors to red cell collections or plasma collections bound for fractionation and some smaller donor centers, especially hospital-based, have applied the standard to all blood product collections.
Additional mitigation strategies include the use of licensed, pooled, solvent-detergent treated plasma products (Octaplas™ Pooled Plasma (Human) Solvent/Detergent Treated; OctaPharma, Lachen, Switzerland). Related to the use of these solvent-detergent plasma products in European hemovigilance systems have not yielded any TRALI cases after using these products for 10–20 years’ time. This may be explained because the pooling of numerous units dilute out the concentration of antibody and by the presence of soluble HLA antigen which is able to bind free antibody. Octaplas may be used interchangeably for frozen plasma including in plasma exchange for patients with thrombotic thrombocytopenic purpura (TTP) but has its limitations, and besides being more expensive than frozen or thawed plasma products, it may not be used in patients with IgA deficiency or severe deficiency of Protein S.
Factor concentrates including Kcentra™ Prothrombin Complex Concentrate (Human) (CSL Behring, King of Prussia, PA) have also never been associated with TRALI, likely due to the same dilution theories.
Additional mitigation strategies include the avoidance of directed donations from blood-related donors, especially from mother to child as the mother has likely been sensitized to any paternally inherited antigens the child has inherited and therefore maternal transfusions have the potential to contain anti-HLA antibodies; this has been reported multiple times in the literature [88]. In addition, irradiation must be performed on donations from blood relatives, to mitigate TA-GVHD, but does not prevent possible TRALI from occurring.
In summary TRALI remains an important and underreported cause of transfusion-related morbidity and mortality. It is a clinical diagnosis for which there is no single, pathognomonic test and until the USA adopts a national, nonvoluntary reporting system or at least one entity able to receive data from multiple reporting systems, it is likely to continue to be underrecognized.
Transfusion-Associated Circulatory Overload (TACO)
TACO is an acute, hydrostatic pulmonary edema which occurs in the setting of transfusion. Especially vulnerable populations include the very young, older patients (over 70 years of age), and those with compromised vascular systems or renal failure. TACO closely followed TRALI in the number of FDA-reported transfusion-related deaths, with 13 confirmed cases in fiscal year 2013, comprising 34 % of transfusion-related deaths, up from eight deaths the previous year [13]. TACO was reported by the 2011 NBCUS (which is the most recent as of 2014) to be voluntarily reported a total of 1512 times, amounting to 1 in 13,843 transfusions [3].
There are several distinguishing factors between TRALI and TACO (Table 19.5). Pulmonary wedge pressure is an invasive measurement to determine the back pressure from the heart, or filling (“wedge”) pressure of the left atrium, by a catheter in the pulmonary artery, and unless the patient already has a Swan-Ganz catheter in place it is not likely to be performed. BNP is a 32 amino acid polypeptide secreted in response to stretched cardiac ventricles, to counteract the renin–angiotensin–aldosterone system. Baseline BNP is not likely to be measured unless the patient is already being monitored for heart failure and may not be useful unless the differences are marked. In general, two of the most helpful distinguishing features are that TACO responds quickly to diuresis, whereas this approach should be avoided in TRALI unless the patient is also fluid overloaded, and, though fever may or may not be seen with TRALI, it is never a feature of TACO. It may be helpful to sit the patient upright; oxygen should be given as needed. It is possible that TRALI and TACO may occur together .
Table 19.5.
| TRALI | TACO | |
|---|---|---|
| Pulmonary edema, bilateral | Yes | Yes |
| Fever | Possibly | No |
| Tachypnea, dyspnea | Yes | Yes |
| Leukopenia | Possibly | No |
| PWP (pulmonary wedge pressure) | Normal | Increased |
| BNP (B-type natriuretic peptide) | <200 pg/mL | Greatly elevated |
| BP | Usually hypotension | Usually hypertension |
| Increased vascular congestion/heart size | No | Yes |
| Diuresis | Hypoperfusion | Resolution of symptoms |
Red Cell Storage
In adults, bone-marrow-derived hematopoietic stem cells may differentiate into myeloid or lymphoid lineages, and it is through the myeloid lineage with subsequent maturation through erythroid progenitors from which mature red cells arise. The kidneys are key regulators in red cell production and when the renal vasculature senses decreased oxygen delivery, renal cortical interstitial cells produce the hormone erythropoietin, which acts on cells in the bone marrow to stimulate red cell production. Oxygen-sensing bodies are also present in the lung and the carotid bodies (near the bifurcation point of the carotid arteries in the neck).
The primary function of red cells is to transport oxygen from the lung to the body’s tissues. RBCs are biconcave disks approximately 5 μm at their widest diameter with a volume of approximately 90 fl [89]. The relatively thinner centers allow the cells great flexibility as they traverse the large capillary bed in the body, participating in gas exchange [89]. Prostaglandins and nitric oxide are two key regulators of the small vessels. Mature red cells lack a nucleus and mitochondria, contain only key organelles and rely on glycolysis for energy production [89]. Approximately 250 billion RBCs are in an average adult and the daily turnover is about 1 % of the circulating volume [89].
The life of a red cell is approximately 120 days and as the cell ages it undergoes changes in its shape, sheds lipids, proteins, and other particles, enduring metabolic and oxidative injury. The RBC storage lesion is a broad term describing these and other changes that occur to the red cell for the duration of its life outside of the body. The consequences of aging are reflected by what is accumulated in the storage plasma, preservative and additive solutions in which the RBCs are stored, and ultimately transfused into the patient.
When a blood donation is made RBCs of every age are collected and pH of the donor’s blood likely ranges from 7.32 to 7.42 (venous blood). Blood banks primarily use a first in, first out (FIFO) model for RBC distribution to hospitals and transfusion services, though clinicians may request fresher blood for certain patient populations, such as transplant, neonatal, or extracorporeal membrane oxygenation (ECMO). This rotation model reduces waste and helps manage inventory.
During routine RBC storage, the shape of the smooth, biconcave disk (discocyte) is changed to an echinocyte, which retains the discoid shape but has small, rounded surface protrusions, then to a spheroechinocyte which resembles a round bumpy ball, and finally to a spheroctye [91, 92]. The longer the RBCs remain in storage, the more the shape reversibility diminishes [91, 92]. These less flexible shapes are unable to easily traverse the smallest vessels and shed lipids and other products and may occasionally occlude vessels [91, 92].
In the body heavily damaged cells are phagocytized or scavenged by the spleen, whereas in a storage bag, dead and dying cells and their by-products accumulate. The individual quality of each donation is donor-dependent. Glucose is metabolized (glycolysis) via the Embden–Meyerhof pathway yielding adenosine triphosphate (ATP) which is a high-energy compound needed for red cell function. By-products are lactate or pyruvate. The two important branch pathways from the primary glycolytic pathway are the 2,3-DPG shunt (Rapoport–Luebering shunt) which uses some of the ATP made in the primary pathway to produce 2,3-DPG and the pentose shunt (hexose monophosphate shunt) which is an important metabolic pathway to produce NADPH.
Hemoglobin is a tetramer of four subunits. Each subunit consists of a large protein chain with an oxygen-binding heme group. In the center of each heme group (or molecule) is an iron atom which binds oxygen in the “relaxed” or high-oxygen affinity state and releases it in the “tensed” or low-oxygen affinity state. The ratio of 2,3-DPG (DPG) to hemoglobin is approximately equal in the red cell. The presence of DPG is important as DPG binds to the subunit and favors the unloading of the oxygen into the tissues. As RBCs age, the ability to produce DPG falls and the oxygen-releasing capacity is reduced. Aucar and colleages concluded that aging red cells had the capacity to significantly and adversely affect the global coagulation status of trauma patients when the activated clotting time (ACT) (and controlled for all other factors) was compared at different RBC storage ages, but was especially prolonged between weeks 3 and 5 of RBC storage [93, 94].
With the application of mass spectroscopy to cells both the proteome and the metabolome of RBCs and stored RBC units have been studied [90, 95–98]. During routine storage RBC metabolomics demonstrates that vital functions begin to change at about 14 days D'Alessandro A, et al. Routine storage of red blood cell (RBC) units in additive solution-3: a comprehensive investigation of the RBC metabolome. Transfusion. 2015 Jun; 55(6):1155-68. PMID:25556331.). At this time intracellular proteins are released with loss of cellular integrity including peroxiredoxin-2 peroxiredoxin-6, glycolytic enzymes, e.g., α-enolase [99]. Some of these enzymes may have the ability to affect extracellular processes and may be masquerading mediators for they may be fully active [99]. Proteomic analysis has determined that AS-3 is the best additive solution because compared to AS-1, AS-5, and SGAM the intracellular proteins are retained longer [97]. Further work is required to determine better RBC storage as sell as the effects of released enzymes, proteins, and lipids on the transfused patient.
Transfusion and, in particular, stored RBCs have been shown to be independent predictors of post-injury multiple organ failure (MOF) in injured patients with moderate ISS (15 < ISS < 30) who received >6 units of RBCs in the first 12 h following injury [100, 101]. In further analysis of these patients, the transfusion of stored RBCs (age ≥ 21 days) was an independent predictor of those patients who developed MOF [102]. Importantly, these studies were controlled for the amount of blood transfused; all patients with intermediate ISS received 6 units of PRBCs in the first 12 h and similar amounts of other blood products. In addition the mechanism of injury was not different. With new, stricter transfusion parameters using a hemoglobin of 7 g/dl as the trigger, only about 5 % of injured patients developed MOF [103]. There is still a significant amount of post-injury ALI and ARDS that appears to be transfusion related; however <5 % of these patients succumb to this complication.
Summary
There is currently a great emphasis on appropriate blood use in all clinical settings. Creation of blood utilization guidelines should be based on the clinical service’s requirements and the usage tools, including transfusion triggers and algorithms, should be developed by each clinical service, supported by medical literature and rooted in patient needs, with involvement from the transfusion medicine pathologist and blood bank. Longer red cell storage times undoubtedly results in cellular alterations, diminished viability and accumulation of undesirable byproducts in the plasma in which cellular blood products are stored. This raises the question: despite the fact that blood may be stored for up to 42 days in additive solution, should it really be transfused up to its date of expiration?
Metabolomics is a burgeoning field and recent study in this area has helped to further distinguish the additive solutions and have promoted the development of new additive solutions such as SOLX, or, AS-7.
Previous retrospective studies, such as the 2008 Cleveland Clinic study led by Dr. Koch, showed that older blood resulted in increased postoperative complications and increased mortality. The concept that fresher red cells are better is supported by other clinical studies. Conclusions from prospective clinical studies including RECESS, ABCPICU, and other trials are anxiously awaited.
Acknowledgement
The authors would like to acknowledge Sara E. West for creation of Fig. 19.1: example of O-negative switching protocol.
Contributor Information
Ernest E. Moore, Email: ernest.moore@dhha.org
Christopher C. Silliman, Email: christopher.silliman@ucdenver.edu
References
- 1.Vaccines for children: a guide for parents and caregivers US Food and Drug Administration. Silver Spring, MD: US Food and Drug Administration; 2014.
- 2.Guidance for Industry: circular of Information for the use of human blood and blood components. FDA. Silver Spring, MD: US Food and Drug Administration; 2014.
- 3.Whitaker B, Hinkins S. The 2011 national blood collection and utilization survey report, Bethesda, MD; 2011.
- 4.Pfuntner A, Wier LM, Stocks C. Most frequent procedures performed in U.S. Hospitals, 2011. Rockville, MD: Agency for Healthcare Research and Quality; 2013. [PubMed] [Google Scholar]
- 5.Schreiber GB, Schlumpf KS, Glynn SA, Wright DJ, Tu Y, King MR, Higgins MJ, Kessler D, Gilcher R, Nass CC, et al. Convenience, the bane of our existence, and other barriers to donating. Transfusion. 2006;46(4):545–53. doi: 10.1111/j.1537-2995.2006.00757.x. [DOI] [PubMed] [Google Scholar]
- 6.Harmening DM. In: Modern blood banking and transfusion practices. 6. Harmening DM, editor. Philadelphia: F.A. Davis Company; 2012. pp. 121–3. [Google Scholar]
- 7.Reid ME, Lomas-Francis C, Olsson ML. The blood group antigens facts book. 3. New York: Elsevier Academic Press; 2012. [Google Scholar]
- 8.Schwarz HP, Dorner F. Karl Landsteiner and his major contributions to haematology. Br J Haematol. 2003;121(4):556–65. doi: 10.1046/j.1365-2141.2003.04295.x. [DOI] [PubMed] [Google Scholar]
- 9.ABO blood group (transferase A, alpha 1-3-N-acetylgalactosaminyltransferase; transferase B, alpha 1-3-galactosyltransferase) [Homo sapiens (human)] NCBI; 2014.
- 10.Yamamoto F, Clausen H, White T, Marken J, Hakomori S. Molecular genetic basis of the histo-blood group ABO system. Nature. 1990;345(6272):229–33. doi: 10.1038/345229a0. [DOI] [PubMed] [Google Scholar]
- 11.Fong SW, Qaqundah BY, Taylor WF. Developmental patterns of ABO isoagglutinins in normal children correlated with the effects of age, sex, and maternal isoagglutinins. Transfusion. 1974;14(6):551–9. doi: 10.1111/j.1537-2995.1974.tb04576.x. [DOI] [PubMed] [Google Scholar]
- 12.Issitt P, Anstee D. Applied blood group serology. 4. Durham, NC: Montgomery Scientific Publications; 1998. [Google Scholar]
- 13.Fatalities reported to the FDA following blood collection and transfusion. FDA; 2013.
- 14.AABB Program Committee . AABB standards for perioperative autologous blood collection and administration. 5. Bethesda: AABB Press; 2013. [Google Scholar]
- 15.Waters J, Dyga RM, Yazer RM. Guidelines for blood recovery and reinfusion in surgery and trauma. Bethesda: AABB Press; 2010. [Google Scholar]
- 16.Ashworth A, Klein AA. Cell salvage as part of a blood conservation strategy in anaesthesia. Br J Anaesth. 2010;105(4):401–16. doi: 10.1093/bja/aeq244. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt H, Lund JO, Nielsen SL. Autotransfused shed mediastinal blood has normal erythrocyte survival. Ann Thorac Surg. 1996;62(1):105–8. doi: 10.1016/0003-4975(96)00219-6. [DOI] [PubMed] [Google Scholar]
- 18.Salhanick M, Corneille M, Higgins R, Olson J, Michalek J, Harrison C, Stewart R, Dent D. Autotransfusion of hemothorax blood in trauma patients: is it the same as fresh whole blood? Am J Surg. 2011;202(6):817–21. doi: 10.1016/j.amjsurg.2011.06.043. [DOI] [PubMed] [Google Scholar]
- 19.Silliman CC, Kelher M, Ambruso DR. Bioactive lipids from stored cellular blood components: in vitro method is crucial for proper interpretation. Transfusion. 2012;52(5):1155–7. doi: 10.1111/j.1537-2995.2012.03564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.AABB . Blood transfusion therapy: a physician's handbook. 10. Bethesda, MD: AABB Press; 2011. [Google Scholar]
- 21.Josephson CD, Meyer E, et al. Neonatal and pediatric transfusion practice. In: Fung M, Grossman B, Hillyer C, et al., editors. Technical manual. 18. Bethesda, MD: AABB Press; 2014. pp. 571–98. [Google Scholar]
- 22.Cable RG, Glynn SA, Kiss JE, Mast AE, Steele WR, Murphy EL, Wright DJ, Sacher RA, Gottschall JL, Tobler LH, et al. Iron deficiency in blood donors: the REDS-II Donor Iron Status Evaluation (RISE) study. Transfusion. 2012;52(4):702–11. doi: 10.1111/j.1537-2995.2011.03401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Josephson CD, et al. Iron overload. In: Hillyer CD, Shaz B, Zimring J, et al., editors. Transfusion medicine and hemostasis: clinical and laboratory aspects. 1. Burlington, MA: Elsevier; 2009. pp. 359–60. [Google Scholar]
- 24.Sheth S, et al. Transfusional iron overload. In: Simon T, Snyder E, Solheim B, et al., editors. Rossi’s principles of transfusion medicine. 4. Bethesda, MD: AABB Press; 2009. pp. 858–62. [Google Scholar]
- 25.Guidance for industry: pre-storage leukocyte reduction of whole blood and blood components intended for transfusion. FDA; 2012.
- 26.The Trial to Reduce Alloimmunization to Platelets Study Group Leukocyte reduction and ultraviolet B irradiation of platelets to prevent alloimmunization and refractoriness to platelet transfusions. N Engl J Med. 1997;337(26):1861–9. doi: 10.1056/NEJM199712253372601. [DOI] [PubMed] [Google Scholar]
- 27.Paglino JC, Pomper GJ, Fisch GS, Champion MH, Snyder EL. Reduction of febrile but not allergic reactions to RBCs and platelets after conversion to universal prestorage leukoreduction. Transfusion. 2004;44(1):16–24. doi: 10.1046/j.0041-1132.2004.00608.x. [DOI] [PubMed] [Google Scholar]
- 28.Sweeney JD. Universal leukoreduction of cellular blood components in 2001? Yes. Am J Clin Pathol. 2001;115(5):666–73. doi: 10.1309/XG61-NB7Q-JM59-PK98. [DOI] [PubMed] [Google Scholar]
- 29.Nichols WG, Price TH, Gooley T, Corey L, Boeckh M. Transfusion-transmitted cytomegalovirus infection after receipt of leukoreduced blood products. Blood. 2003;101(10):4195–200. doi: 10.1182/blood-2002-10-3143. [DOI] [PubMed] [Google Scholar]
- 30.Ziemann M, Heuft HG, Frank K, Kraas S, Gorg S, Hennig H. Window period donations during primary cytomegalovirus infection and risk of transfusion-transmitted infections. Transfusion. 2013;53(5):1088–94. doi: 10.1111/trf.12074. [DOI] [PubMed] [Google Scholar]
- 31.Ziemann M, Hennig H. Prevention of transfusion-transmitted cytomegalovirus infections: which is the optimal strategy? Transfus Med Hemother. 2014;41(1):40–4. doi: 10.1159/000357102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Josephson CD, Castillejo MI, Caliendo AM, Waller EK, Zimring J, Easley KA, Kutner M, Hillyer CD, Roback JD. Prevention of transfusion-transmitted cytomegalovirus in low-birth weight infants (</=1500 g) using cytomegalovirus-seronegative and leukoreduced transfusions. Transfus Med Rev. 2011;25(2):125–32. doi: 10.1016/j.tmrv.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.AABB . Standards for blood banks and transfusion services. 29. Bethesda, MD: AABB Press; 2014. [Google Scholar]
- 34.Strauss RG. Routinely washing irradiated red cells before transfusion seems unwarranted. Transfusion. 1990;30(8):675–7. doi: 10.1046/j.1537-2995.1990.30891020322.x. [DOI] [PubMed] [Google Scholar]
- 35.Strauss RG. RBC storage and avoiding hyperkalemia from transfusions to neonates & infants. Transfusion. 2010;50(9):1862–5. doi: 10.1111/j.1537-2995.2010.02789.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Rare Donor Program American Red Cross; 1998.
- 37.Ohto H, Anderson KC. Survey of transfusion-associated graft-versus-host disease in immunocompetent recipients. Transfus Med Rev. 1996;10(1):31–43. doi: 10.1016/S0887-7963(96)80121-0. [DOI] [PubMed] [Google Scholar]
- 38.Dwyre DM, Holland PV. Transfusion-associated graft-versus-host disease. Vox Sang. 2008;95(2):85–93. doi: 10.1111/j.1423-0410.2008.01073.x. [DOI] [PubMed] [Google Scholar]
- 39.Shastry S, Ramya B, Ninan J, Srinidhi GC, Bhat SS, Fernandes DJ. Linear accelerator: a reproducible, efficacious and cost effective alternative for blood irradiation. Transfus Apher Sci. 2013;49(3):528–32. doi: 10.1016/j.transci.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Maia GA, Reno CO, Medina JM, Silveira AB, Mignaco JA, Atella GC, Cortes VF, Barbosa LA, Santos HL. The effect of gamma radiation on the lipid profile of irradiated red blood cells. Ann Hematol. 2014;93(5):753–60. doi: 10.1007/s00277-013-1944-5. [DOI] [PubMed] [Google Scholar]
- 41.Janatpour K, Denning L, Nelson K, Betlach B, Mackenzie M, Holland P. Comparison of X-ray vs. gamma irradiation of CPDA-1 red cells. Vox Sang. 2005;89(4):215–9. doi: 10.1111/j.1423-0410.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- 42.Petz LD, Calhoun L, Yam P, Cecka M, Schiller G, Faitlowicz AR, Herron R, Sayah D, Wallace RB, Belldegrun A. Transfusion-associated graft-versus-host disease in immunocompetent patients: report of a fatal case associated with transfusion of blood from a second-degree relative, and a survey of predisposing factors. Transfusion. 1993;33(9):742–50. doi: 10.1046/j.1537-2995.1993.33994025025.x. [DOI] [PubMed] [Google Scholar]
- 43.Guidance for Industry: Gamma irradiation of blood and blood components: a pilot program for licensing. FDA; 2000.
- 44.Gulbahce HE, Brown CA, Wick M, Segall M, Jessurun J. Graft-vs-host disease after solid organ transplant. Am J Clin Pathol. 2003;119(4):568–73. doi: 10.1309/395BX683QFN6CJBC. [DOI] [PubMed] [Google Scholar]
- 45.Luban NL, Strauss RG, Hume HA. Commentary on the safety of red cells preserved in extended-storage media for neonatal transfusions. Transfusion. 1991;31(3):229–35. doi: 10.1046/j.1537-2995.1991.31391165172.x. [DOI] [PubMed] [Google Scholar]
- 46.Blood Donor History Questionnaires. AABB Donor History Task Force; 2014.
- 47.Busch MP, Glynn SA, Stramer SL, Strong DM, Caglioti S, Wright DJ, Pappalardo B, Kleinman SH. A new strategy for estimating risks of transfusion-transmitted viral infections based on rates of detection of recently infected donors. Transfusion. 2005;45(2):254–64. doi: 10.1111/j.1537-2995.2004.04215.x. [DOI] [PubMed] [Google Scholar]
- 48.HIV Clinical Resource: diagnostic, monitoring, and resistance laboratory tests for HIV Office of the Medical Director NYSDoHAIiCwtJHUDoID; 2014.
- 49.Zou S, Dorsey KA, Notari EP, Foster GA, Krysztof DE, Musavi F, Dodd RY, Stramer SL. Prevalence, incidence, and residual risk of human immunodeficiency virus and hepatitis C virus infections among United States blood donors since the introduction of nucleic acid testing. Transfusion. 2010;50(7):1495–504. doi: 10.1111/j.1537-2995.2010.02622.x. [DOI] [PubMed] [Google Scholar]
- 50.Hess JR. Red cell storage. J Proteomics. 2010;73(3):368–73. doi: 10.1016/j.jprot.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 51.Hillyer C. D. Bacterial Contamination of Blood Components: Risks, Strategies, and Regulation: Joint ASH and AABB Educational Session in Transfusion Medicine. Hematology. 2003;2003(1):575–589. doi: 10.1182/asheducation-2003.1.575. [DOI] [PubMed] [Google Scholar]
- 52.West FB, Silliman CC. Transfusion-related acute lung injury: advances in understanding the role of proinflammatory mediators in its genesis. Expert Rev Hematol. 2013;6(3):265–76. doi: 10.1586/ehm.13.31. [DOI] [PubMed] [Google Scholar]
- 53.Benson AB, Austin GL, Berg M, McFann KK, Thomas S, Ramirez G, Rosen H, Silliman CC, Moss M. Transfusion-related acute lung injury in ICU patients admitted with gastrointestinal bleeding. Intensive Care Med. 2010;36(10):1710–7. doi: 10.1007/s00134-010-1954-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Gajic O, Rana R, Winters JL, Yilmaz M, Mendez JL, Rickman OB, O'byrne MM, Evenson LK, Malinchoc M, Degoey SR, et al. Transfusion-related acute lung injury in the critically ill: prospective nested case-control study. Am J Respir Crit Care Med. 2007;176(9):886–91. doi: 10.1164/rccm.200702-271OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kopko PM, Holland PV. Transfusion-related acute lung injury. Br J Haematol. 1999;105(2):322–9. doi: 10.1111/j.1365-2141.1999.01357.x. [DOI] [PubMed] [Google Scholar]
- 56.Menis M, Forshee RA, Anderson SA, McKean S, Gondalia R, Warnock R, Johnson C, Mintz PD, Worrall CM, Kelman JA, et al. Posttransfusion purpura occurrence and potential risk factors among the inpatient US elderly, as recorded in large Medicare databases during 2011 through 2012. Transfusion. 2014;55:284–95. doi: 10.1111/trf.12782. [DOI] [PubMed] [Google Scholar]
- 57.Suchyta MR, Clemmer TP, Elliott CG, Orme JF, Jr, Weaver LK. The adult respiratory distress syndrome. A report of survival and modifying factors. Chest. 1992;101(4):1074–9. doi: 10.1378/chest.101.4.1074. [DOI] [PubMed] [Google Scholar]
- 58.Zilberberg MD, Epstein SK. Acute lung injury in the medical ICU: comorbid conditions, age, etiology, and hospital outcome. Am J Respir Crit Care Med. 1998;157(4 Pt 1):1159–64. doi: 10.1164/ajrccm.157.4.9704088. [DOI] [PubMed] [Google Scholar]
- 59.Lieberman L, Petraszko T, Yi QL, Hannach B, Skeate R. Transfusion-related lung injury in children: a case series and review of the literature. Transfusion. 2014;54(1):57–64. doi: 10.1111/trf.12249. [DOI] [PubMed] [Google Scholar]
- 60.Barnard RD. Indiscriminate transfusion: a critique of case reports illustrating hypersensitivity reactions. N Y State J Med. 1951;51(20):2399–402. [PubMed] [Google Scholar]
- 61.Lanman JT, Bierman HR, Byron RL., Jr Transfusion of leukemic leukocytes in man; hematologic and physiologic changes. Blood. 1950;5(12):1099–113. [PubMed] [Google Scholar]
- 62.Popovsky MA, Moore SB. Diagnostic and pathogenetic considerations in transfusion-related acute lung injury. Transfusion. 1985;25(6):573–7. doi: 10.1046/j.1537-2995.1985.25686071434.x. [DOI] [PubMed] [Google Scholar]
- 63.Bernard G, Artigas A, Dellinger P, Esmon C, Faist E, Faust SN, Fischer CJ, Fumagalli R, Grinnell BW, Sprung C. Clinical expert round table discussion (session 3) at the Margaux Conference on critical Illness: the role of activated protein C in severe sepsis. Crit Care Med. 2001;29(7 Suppl):S75–7. doi: 10.1097/00003246-200107001-00025. [DOI] [PubMed] [Google Scholar]
- 64.Toy P, Popovsky MA, Abraham E, Ambruso DR, Holness LG, Kopko PM, McFarland JG, Nathens AB, Silliman CC, Stroncek D. Transfusion-related acute lung injury: definition and review. Crit Care Med. 2005;33(4):721–6. doi: 10.1097/01.CCM.0000159849.94750.51. [DOI] [PubMed] [Google Scholar]
- 65.Nakagawa M, Toy P. Acute and transient decrease in neutrophil count in transfusion-related acute lung injury: cases at one hospital. Transfusion. 2004;44(12):1689–94. doi: 10.1111/j.0041-1132.2004.04194.x. [DOI] [PubMed] [Google Scholar]
- 66.Schmidt AE, Adamski J. Pathology consultation on transfusion-related acute lung injury (TRALI) Am J Clin Pathol. 2012;138(4):498–503. doi: 10.1309/AJCPFF6JKXM7BYOI. [DOI] [PubMed] [Google Scholar]
- 67.Rich AS, Cushing MM, et al. Adverse events associated with hematopoietic progenitor cell product infusion. In: Shaz BH, Hillyer CD, Roshal M, et al., editors. Transfusion medicine and hemostasis clinical and laboratory aspects. Burlington: Elsevier; 2013. pp. 571–2. [Google Scholar]
- 68.Rizk A, Gorson KC, Kenney L, Weinstein R. Transfusion-related acute lung injury after the infusion of IVIG. Transfusion. 2001;41(2):264–8. doi: 10.1046/j.1537-2995.2001.41020264.x. [DOI] [PubMed] [Google Scholar]
- 69.Stoclin A, Delbos F, Dauriat G, Brugiere O, Boeri N, Metivier AC, Thabut G, Camus P, Mal H. Transfusion-related acute lung injury after intravenous immunoglobulin treatment in a lung transplant recipient. Vox Sang. 2013;104(2):175–8. doi: 10.1111/j.1423-0410.2012.01645.x. [DOI] [PubMed] [Google Scholar]
- 70.Seeger W, Schneider U, Kreusler B, von WE, Walmrath D, Grimminger F, Neppert J. Reproduction of transfusion-related acute lung injury in an ex vivo lung model. Blood. 1990;76(7):1438–44. [PubMed] [Google Scholar]
- 71.Bux J, Hardt O, Kohstall M, Sibelius U, Weissmann N. Reproduction of granulocyte antibody-mediated TRALI in an ex-vivo rat lung model. Blood. 2003;102(Suppl):94a. [Google Scholar]
- 72.Looney MR, Su X, Van Ziffle JA, Lowell CA, Matthay MA. Neutrophils and their Fc gamma receptors are essential in a mouse model of transfusion-related acute lung injury. J Clin Invest. 2006;116(6):1615–23. doi: 10.1172/JCI27238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Looney MR, Nguyen JX, Hu Y, Van Ziffle JA, Lowell CA, Matthay MA. Platelet depletion and aspirin treatment protect mice in a two-event model of transfusion-related acute lung injury. J Clin Invest. 2009;119(11):3450–61. doi: 10.1172/JCI38432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kelher MR, Masuno T, Moore EE, Damle S, Meng X, Song Y, Liang X, Niedzinski J, Geier SS, Khan SY, et al. Plasma from stored packed red blood cells and MHC class I antibodies causes acute lung injury in a 2-event in vivo rat model. Blood. 2009;113(9):2079–87. doi: 10.1182/blood-2008-09-177857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sachs UJ. A threshold model for the susceptibility to transfusion-related acute lung injury. Transfus Clin Biol. 2012;19(3):109–16. doi: 10.1016/j.tracli.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 76.Sachs UJ, Wasel W, Bayat B, Bohle RM, Hattar K, Berghofer H, Reil A, Bux J, Bein G, Santoso S, et al. Mechanism of transfusion-related acute lung injury induced by HLA class II antibodies. Blood. 2011;117(2):669–77. doi: 10.1182/blood-2010-05-286146. [DOI] [PubMed] [Google Scholar]
- 77.Bayat B, Tjahjono Y, Sydykov A, Werth S, Hippenstiel S, Weissmann N, Sachs UJ, Santoso S. Anti-human neutrophil antigen-3a induced transfusion-related acute lung injury in mice by direct disturbance of lung endothelial cells. Arterioscler Thromb Vasc Biol. 2013;33(11):2538–48. doi: 10.1161/ATVBAHA.113.301206. [DOI] [PubMed] [Google Scholar]
- 78.Silliman CC, Curtis BR, Kopko PM, Khan SY, Kelher MR, Schuller RM, Sannoh B, Ambruso DR. Donor antibodies to HNA-3a implicated in TRALI reactions prime neutrophils and cause PMN-mediated damage to human pulmonary microvascular endothelial cells in a two-event in vitro model. Blood. 2007;109(4):1752–5. doi: 10.1182/blood-2006-05-025106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Khan SY, Kelher MR, Heal JM, Blumberg N, Boshkov LK, Phipps R, Gettings KF, McLaughlin NJ, Silliman CC. Soluble CD40 ligand accumulates in stored blood components, primes neutrophils through CD40, and is a potential cofactor in the development of transfusion-related acute lung injury. Blood. 2006;108(7):2455–62. doi: 10.1182/blood-2006-04-017251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Patchefsky AS, et al. Nonneoplastic pulmonary diseases. In: Mills SE, Carter D, Greenson JK, et al., editors. Sternberg’s diagnostic surgical pathology. 4. Philadelphia: Lippincott, Williams & Wilkins; 2004. pp. 1119–22. [Google Scholar]
- 81.Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1334–49. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- 82.Silliman CC, Boshkov LK, Mehdizadehkashi Z, Elzi DJ, Dickey WO, Podlosky L, Clarke G, Ambruso DR. Transfusion-related acute lung injury: epidemiology and a prospective analysis of etiologic factors. Blood. 2003;101(2):454–62. doi: 10.1182/blood-2002-03-0958. [DOI] [PubMed] [Google Scholar]
- 83.Chapman CE, Stainsby D, Jones H, Love E, Massey E, Win N, Navarrete C, Lucas G, Soni N, Morgan C, et al. Ten years of hemovigilance reports of transfusion-related acute lung injury in the United Kingdom and the impact of preferential use of male donor plasma. Transfusion. 2009;49(3):440–52. doi: 10.1111/j.1537-2995.2008.01948.x. [DOI] [PubMed] [Google Scholar]
- 84.Densmore TL, Goodnough LT, Ali S, Dynis M, Chaplin H. Prevalence of HLA sensitization in female apheresis donors. Transfusion. 1999;39(1):103–6. doi: 10.1046/j.1537-2995.1999.39199116901.x. [DOI] [PubMed] [Google Scholar]
- 85.Triulzi DJ, Kleinman S, Kakaiya RM, Busch MP, Norris PJ, Steele WR, Glynn SA, Hillyer CD, Carey P, Gottschall JL, et al. The effect of previous pregnancy and transfusion on HLA alloimmunization in blood donors: implications for a transfusion-related acute lung injury risk reduction strategy. Transfusion. 2009;49(9):1825–35. doi: 10.1111/j.1537-2995.2009.02206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Eder AF, Herron RM, Jr, Strupp A, Dy B, White J, Notari EP, Dodd RY, Benjamin RJ. Effective reduction of transfusion-related acute lung injury risk with male-predominant plasma strategy in the American Red Cross (2006–2008) Transfusion. 2010;50(8):1732–42. doi: 10.1111/j.1537-2995.2010.02652.x. [DOI] [PubMed] [Google Scholar]
- 87.Toy P, Gajic O, Bacchetti P, Looney MR, Gropper MA, Hubmayr R, Lowell CA, Norris PJ, Murphy EL, Weiskopf RB, et al. Transfusion-related acute lung injury: incidence and risk factors. Blood. 2012;119(7):1757–67. doi: 10.1182/blood-2011-08-370932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Church GD, Price C, Sanchez R, Looney MR. Transfusion-related acute lung injury in the paediatric patient: two case reports and a review of the literature. Transfus Med. 2006;16(5):343–8. doi: 10.1111/j.1365-3148.2006.00683.x. [DOI] [PubMed] [Google Scholar]
- 89.Koury MJ. Red cell production. In: Simon TL, Snyder EL, Solheim B, editors. Rossi’s principles of transfusion medicine. 4. Bethesda: AABB Press; 2009. pp. 17–28. [Google Scholar]
- 90.D'Alessandro A, Liumbruno G, Grazzini G, Zolla L. Red blood cell storage: the story so far. Blood Transfus. 2010;8(2):82–8. doi: 10.2450/2009.0122-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Berezina TL, Zaets SB, Morgan C, Spillert CR, Kamiyama M, Spolarics Z, Deitch EA, Machiedo GW. Influence of storage on red blood cell rheological properties. J Surg Res. 2002;102(1):6–12. doi: 10.1006/jsre.2001.6306. [DOI] [PubMed] [Google Scholar]
- 92.Usry RT, Moore GL, Manalo FW. Morphology of stored, rejuvenated human erythrocytes. Vox Sang. 1975;28(3):176–83. doi: 10.1111/j.1423-0410.1975.tb02756.x. [DOI] [PubMed] [Google Scholar]
- 93.Aucar JA, Isaak E, Anthony D. The effect of red blood cell age on coagulation. Am J Surg. 2009;198(6):900–4. doi: 10.1016/j.amjsurg.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 94.Aucar JA, Sheth M. The storage lesion of packed red blood cells affects coagulation. Surgery. 2012;152(4):697–702. doi: 10.1016/j.surg.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 95.Anniss AM, Glenister KM, Killian JJ, Sparrow RL. Proteomic analysis of supernatants of stored red blood cell products. Transfusion. 2005;45(9):1426–33. doi: 10.1111/j.1537-2995.2005.00547.x. [DOI] [PubMed] [Google Scholar]
- 96.D'Alessandro A, Gevi F, Zolla L. Red blood cell metabolism under prolonged anaerobic storage. Mol Biosyst. 2013;9(6):1196–209. doi: 10.1039/c3mb25575a. [DOI] [PubMed] [Google Scholar]
- 97.D'Amici GM, Mirasole C, D'Alessandro A, Yoshida T, Dumont LJ, Zolla L. Red blood cell storage in SAGM and AS3: a comparison through the membrane two-dimensional electrophoresis proteome. Blood Transfus. 2012;10(Suppl 2):s46–54. doi: 10.2450/2012.008S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sparrow RL. Red blood cell storage and transfusion-related immunomodulation. Blood Transfus. 2010;8(Suppl 3):s26–30. doi: 10.2450/2010.005S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dzieciatkowska M, Silliman CC, Moore EE, Kelher MR, Banerjee A, Land KJ, Ellison M, West FB, Ambruso DR, Hansen KC. Proteomic analysis of the supernatant of red blood cell units: the effects of storage and leucoreduction. Vox Sang. 2013;105(3):210–8. doi: 10.1111/vox.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sauaia A, Moore FA, Moore EE, Haenel JB, Read RA, Lezotte DC. Early predictors of postinjury multiple organ failure. Arch Surg. 1994;129(1):39–45. doi: 10.1001/archsurg.1994.01420250051006. [DOI] [PubMed] [Google Scholar]
- 101.Sauaia A, Moore FA, Moore EE, Norris JM, Lezotte DC, Hamman RF. Multiple organ failure can be predicted as early as 12 hours after injury. J Trauma. 1998;45(2):291–301. doi: 10.1097/00005373-199808000-00014. [DOI] [PubMed] [Google Scholar]
- 102.Zallen G, Offner PJ, Moore EE, Blackwell J, Ciesla DJ, Gabriel J, Denny C, Silliman CC. Age of transfused blood is an independent risk factor for postinjury multiple organ failure. Am J Surg. 1999;178(6):570–2. doi: 10.1016/S0002-9610(99)00239-1. [DOI] [PubMed] [Google Scholar]
- 103.Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. A 12-year prospective study of postinjury multiple organ failure: has anything changed? Arch Surg. 2005;140(5):432–8. doi: 10.1001/archsurg.140.5.432. [DOI] [PubMed] [Google Scholar]
- 104.Garratty G, Glynn SA, McEntire R. ABO and Rh(D) phenotype frequencies of different racial/ethnic groups in the United States. Transfusion. 2004;44(5):703–6. doi: 10.1111/j.1537-2995.2004.03338.x. [DOI] [PubMed] [Google Scholar]
- 105.CDC West Nile virus transmission via organ transplantation and blood transfusion—Louisiana, 2008. MMWR Morb Mortal Wkly Rep. 2009;58(45):1263–7. [PubMed] [Google Scholar]
- 106.CDC Fatal West Nile virus infection after probable transfusion-associated transmission—Colorado, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(31):622–4. [PMC free article] [PubMed] [Google Scholar]
- 107.Galel SA, et al. Infectious disease screening. In: Fung MK, Grossman B, Hillyer CD, et al., editors. Technical manual. 18. Bethesda: AABB Press; 2014. pp. 193–206. [Google Scholar]
- 108.Schreiber GB, Busch MP, Kleinman SH, Korelitz JJ. The risk of transfusion-transmitted viral infections. The Retrovirus Epidemiology Donor Study. N Engl J Med. 1996;334(26):1685–90. doi: 10.1056/NEJM199606273342601. [DOI] [PubMed] [Google Scholar]


