ABSTRACT
Background: War captivity is one of the most severe human-made traumatic events which lead to self-amplifying cycle of post-traumatic stress disorder (PTSD) symptoms and attachment insecurities. Solid evidence in the literature pointed out on the intergenerational transmission of PTSD symptoms. However, no research has been conducted on the intergenerational transmission of attachment insecurities and the effect of the self-amplifying cycle among former prisoners of war (ex-POWs) and their offspring attachment insecurities.
Objective: This research aims to explore the intergenerational impact of a self-amplifying cycle of PTSD and attachment insecurities among ex-POWs on their offspring’s attachment orientations.
Method: We sampled dyads of Israeli ex-POWs of the Yom Kippur war and their adult offspring (ex-POW group) (n = 80) as well as dyads of Israeli veterans who fought in the Yom Kippur war, but were never held captive, and their adult offspring (control group) (n = 40). Veterans reported on PTSD severity and attachment orientations (anxiety, avoidance). Offspring reported on attachment orientations. We conducted (a) hierarchical regressions to predict offspring attachment orientations as a function of veterans’ attachment orientations, and (b) moderated mediation analyses examining the role of veterans’ PTSD in the intergenerational transmission of attachment orientations.
Results: Ex-POWs’ attachment anxiety was associated with offspring’s reports of higher attachment anxiety and avoidance, and this intergenerational transmission of attachment was mediated by ex-POWs’ PTSD severity. These effects were not significant in the control group.
Conclusions: Decades after the war end, the intergenerational sequelae of war captivity are evident by the impact of the self-amplifying cycle of PTSD and attachment insecurities among ex-POWs and their offspring’s attachment insecurities. Therefore, it is imperative for clinicians to recognize the intergenerational transmission and to focus not only on the trauma but also on the traumatized person’s attachment injuries and the shattering of core beliefs about the world, self, and others, in the context of attachment-based therapies.
KEYWORDS: Trauma, attachment, intergenerational transmission, captivity, PTSD
Summary
HIGHLIGHTS:
War captivity is a potent pathogen for Posttraumatic Stress Disorder (PTSD) symptoms and attachment injuries apart and simultaneously. Studies revealed the self-amplifying cycle of PTSD symptoms and attachment insecurities decades after the captivity trauma ended. Solid evidence in the literature pointed out on the intergenerational transmission of PTSD symptoms. However, no research has been conducted on the intergenerational transmission of attachment insecurities and the effect of the self-amplifying cycle among former prisoners of war (ex-POWs) and their offspring. Ex-POWs’ attachment anxiety was associated with offspring’s reports of higher attachment anxiety and avoidance, and this intergenerational transmission of attachment was mediated by ex-POWs’ PTSD severity. Therefore, it is imperative for clinicians to recognize the intergenerational transmission and to focus not only on the trauma but also on the traumatized person’s attachment injuries and the shattering of core beliefs about the world, self, and others, in the context of attachment-based therapies.
Antecedentes: El cautiverio en la guerra es uno de los eventos traumáticos provocados por el hombre con mayor severidad, el cual puede llevar a un ciclo auto-amplificador de síntomas de estrés postraumático (TEPT) e inseguridades en el apego. Existe evidencia sólida en la literatura que señala la transmisión intergeneracional de síntomas de TEPT. Sin embargo, no se ha conducido ninguna investigación sobre la transmisión intergeneracional de inseguridades del apego y del efecto del ciclo auto-amplificador entre antiguos prisioneros de guerra (ex-POWs por sus siglas en inglés) y sobre las inseguridades en el apego de sus descendientes.
Objetivo: esta investigación busca explorar el impacto intergeneracional del ciclo auto-amplificador del TEPT e inseguridades en el apego entre ex-POWs en la orientación del apego de su descendencia.
Método: Se obtuvo la muestra de díadas de ex-POWs israelíes de la guerra de Yom Kippur y su descendencia adulta (grupo ex-POWs) (n=80) así como también díadas de veteranos israelíes que combatieron en la guerra de Yom Kippur, pero que nunca estuvieron en cautiverio, y su descendencia adulta (grupo control) (n=40). Los veteranos reportaron sobre la severidad del TEPT y orientación del apego (ansioso, evitativo). La descendencia reportó sobre la orientación del apego. Conducimos (a) una regresión jerárquica para predecir la orientación del apego de la descendencia como función de la orientación del apego de los veteranos y (b) análisis de moderada mediación examinando el rol del TEPT en los veteranos en la transimisión intergeneracional de la orientación del apego.
Resultados: El apego ansioso de los ex-POWs fue asociado con reportes de la descendencia de mayor apego ansioso y evitativo, y esta transmisión intergeneracional fue mediada por la severidad del TEPT de los ex-POWs.
Conclusiones: Décadas después del fin de la guerra, las secuelas intergeneracionales del cautiverio en guerra son evidentes por el impacto del ciclo auto-amplificador del TEPT y las inseguridades en el apego entre ex-POWs y la inseguridad en el apego de su descendencia. Por tanto, es imperativo para los clínicos el poder reconocer la transmisión intergeneracional y focalizarse no sólo en el trauma pero también en el daño en el patrón de apego de la persona, y en el quiebre de creencias nucleares sobre el mundo, el sí mismo y otros, en el contexto de terapias basadas en el apego.
PALABRAS CLAVE: Trauma, Apego, Transmisión intergeneracional, Cautiverio, TEPT
背景: 战争囚禁是最严重的人为创伤事件之一, 会导致创伤后应激障碍 (PTSD) 症状和依恋不安全感的自我增强循环。文献中有确凿证据指出了PTSD症状的代际传递。但是, 尚未开展关于依恋不安全的代际传递以及前战俘 (前POWs) 及其后代依恋不安全之间自我增强循环的影响的研究。
目标: 本研究旨在探究前POWs的PTSD及依恋不安全的自我增强循环对其后代依恋取向的代际影响。
方法: 我们采样了80对赎罪日战争的以色列前POWs及其成年后代 (前POW组), 以及40对在赎罪日战争中战斗但从未被俘虏的以色列退伍军人及其成年后代 (对照组) 。退伍军人报告了PTSD严重程度和依恋取向 (焦虑, 回避), 其后代报告了依恋取向。我们进行了 (a) 分层回归分析, 以退伍军人依恋取向的函数预测后代的依恋取向, 以及 (b) 带有调节的中介分析, 考查退伍军人的PTSD在依恋取向代际传递中的作用。
结果: 前POWs的依恋焦虑与后代报告的更高的依恋焦虑和回避相关, 这种依恋的代际传递被前POWs的PTSD严重程度所中介。
结论: 战争结束几十年后, 前POWs的PTSD及依恋不安全及其后代依恋不安全之间自我增强循环的影响明显体现了战俘的代际后遗症。因此, 在基于依恋的治疗背景中, 临床医生务必要认识到代际传递, 不仅要关注创伤, 还要关注受创伤者的依恋损伤及其对世界, 自我和他人核心信念的瓦解。
关键词: 创伤, 依恋, 代际传递, 俘虏, PTSD
1. Introduction
Recent studies on the long-term consequences of war captivity have revealed a self-amplifying cycle of PTSD symptoms and attachment insecurities (anxiety, avoidance) that contribute to the preservation of the disorder over time (Mikulincer, Ein-Dor, Solomon, & Shaver, 2011). These findings raise an important question about whether this self-amplifying cycle can be transmitted to the offspring of ex-prisoners of war (ex-POWs), thereby preserving the disorder in the second generation of trauma survivors. Studies have provided solid evidence for the intergenerational transmission of PTSD symptoms and the impact of war captivity on the mental health of ex-POWs’ offspring (Zerach & Aloni, 2015; Zerach & Solomon, 2016). However, no research has been conducted on the intergenerational transmission of attachment insecurities among ex-POWs and their offspring. In the current study, we want to fill this gap and to examine whether the self-amplifying cycle of PTSD and attachment insecurities among ex-POWs would contribute to heightened attachment insecurities in their offspring.
War captivity is one of the most severe man-made traumatic events to which an individual can be subjected (Charuvastra & Cloitre, 2008). Prisoners of war endure physical and psychological torture, isolation, systematic humiliation, starvation, and the use of psychological tactics aimed at breaking their psyches (Herman, 1992). As a result, ex-POWs may suffer from long-term mental disorders, the most common of which is PTSD (Solomon, Horesh, Ein-Dor, & Ohry, 2012). Ex-POWs also tend to suffer from other psychiatric co-morbidities, including cognitive dysfunctions, anxiety disorders, and depression (Aloni, Crompton, Levin, & Solomon, 2018; Ginzburg, Ein-Dor, & Solomon, 2010). Moreover, they tend to experience profound personality changes (Van der Kolk, 2002), which may stem from the distorted relationship with the captor that is characterized by total dependence and helplessness (Herman, 1992; Van der Kolk, 2002).
Attachment insecurities along the anxiety and avoidance dimensions constitute one core risk factor for the emergence and consolidation of PTSD among ex-POWs (Mikulincer, Shaver, & Solomon, 2015). A person’s position on the anxiety dimension indicates the degree to which he worries that others will not be available and supportive in times of need and adopts ‘hyperactivating’ attachment strategies – energetic, insistent attempts to obtain support and love from others – as a means of regulating distress (Brennan, Clark, & Shaver, 1998; Mikulincer & Shaver, 2016). A person’s position on the avoidance dimension indicates the extent to which he distrusts others’ goodwill, strives to maintain behavioural independence and emotional distance, and relies on ‘deactivating’ strategies, such as suppression of attachment-related thoughts and emotions (Brennan et al., 1998; Mikulincer & Shaver, 2016).
Attachment insecurities have been found to be associated with heightened negative beliefs about one’s safety and self-worth and others’ benevolence (Arikan, Stopa, Carnelley, & Karl, 2016; Barr, 2014) as well as increased risk for social maladjustment and psychopathology (Mikulincer & Shaver, 2016; Stovall-McClough & Dozier, 2016). On this basis, Mikulincer et al. (Mikulincer et al., 2015) hypothesized that attachment insecurities would increase trauma survivors’ views of the world as a dangerous place, other people as harmful, and themselves as unworthy and vulnerable, all of which, in turn, would heighten PTSD severity in the aftermath of trauma.
Cross-sectional and longitudinal studies have revealed a consistent association between self-reports of attachment insecurities and PTSD severity among trauma survivors (Fraley, Fazzari, Bonanno, & Dekel, 2006; Woodhouse, Ayers, & Field, 2015) and ex-POWs (Dieperink, Leskela, Thuras, & Engdahl, 2001; Mikulincer et al., 2011; Zakin, Solomon, & Neria, 2003). For instance, Mikulincer et al. (Mikulincer et al., 2011) found that attachment insecurities measured 18 years after captivity predicted elevation of PTSD severity 12 and 17 years later. However, across several studies, avoidant attachment has been found to be less predictive of PTSD severity than anxious attachment (Lim, Hodges, & Lilly, 2019).
At the same time, war captivity and PTSD can amplify attachment insecurities, thereby creating a bi-directional association between these two psychological sequelae of trauma. According to Herman (Herman, 1992), war captivity and persistent PTSD can increase negative representations of the self and others, thereby heightening attachment insecurities especially among vulnerable individuals who were already attachment-insecure prior to the trauma. Indeed, Solomon, Dekel, and Mikulincer (Solomon, Dekel, & Mikulincer, 2008) assessed PTSD and attachment orientations 18 and 30 years after captivity, finding that attachment insecurities increased from Time 1 to Time 2 among ex-POWs. Studies also found that attachment insecurities continued to increase 35 years after captivity and that persistent PTSD across the three waves of measurement (18, 30, and 35 years) was associated with greater increases in attachment insecurities over time (Mikulincer et al., 2011). In addition, Murphy, Elklit, Hyland and Shevlin (Murphy, Elklit, Hyland, & Shevlin, 2016) found that chronic PTSD increased attachment insecurities by heightening negative views of the self and others. These findings reflect the action of a self-amplifying cycle by which attachment insecurities prospectively contribute to PTSD severity, and PTSD further heightens attachment insecurities, which, in turn, sustain or even exacerbate the disorder over time (Marshall & Frazier, 2019).
This self-amplifying cycle may be so intense and pervasive over time that it can affect not only the trauma survivor, but also be transmitted to his offspring. Clinical and empirical studies indicate that traumatic events may also affect significant others’ mental health in the form of secondary traumatization: PTSD-like responses similar to those exhibited by the trauma survivor (Dekel & Monson, 2010; Figley, 1995; Galovski & Lyons, 2004). There is evidence that offspring of veterans are at a heightened risk for adjustment difficulties (Jordan et al., 1992), depression and somatization (Maršanić, Margetić, Jukić, Matko, & Grgić, 2014). However, most of these studies have focused on young children and adolescents and have relied on parents’ reports (Ruscio, Weathers, King, & King, 2002). Recently, studies (Zerach & Aloni, 2015; Zerach & Solomon, 2016) found that adult offspring of ex-POWs reported higher rates of depression, anxiety, hostility, PTSD, and attachment insecurities than offspring of veterans who did not experience war captivity. Moreover, ex-POWs’ PTSD severity was associated with the severity of PTSD reported by their adult offspring.
Although these studies provide evidence about the intergenerational transmission of PTSD, they did not examine the extent to which attachment insecurities are also transmitted from the ex-POW to his offspring. In fact, no systematic study has examined the impact of ex-POWs’ self-amplifying cycle of PTSD and attachment insecurities on their offspring’s attachment insecurities.
There is evidence for the intergenerational transmission of attachment in community samples (Mikulincer & Shaver, 2016), when most of these studies have been conducted among mother-child dyads (Van IJzendoorn, 1995). However, over the last two decades studies have examined the intergenerational transmission of attachment from father to offspring (Palm, 2014; Paquette & Bigras, 2010). Findings have consistently indicated that a father’s attachment insecurities contribute to the development of attachment insecurities in his offspring and that this intergenerational link is mediated by paternal insensitivity and father’s engagement in aversive parenting behaviours (Grossmann et al., 2002; Hazen, McFarland, Jacobvitz, & Boyd‐Soisson, 2010; Lucassen et al., 2011). However, none of these studies have examined the intergenerational transmission of attachment among trauma survivors.
In recent years, scholars have devoted growing attention to the involvement of attachment-related processes in the intergenerational transmission of trauma (Belt et al., 2013; Bradfield, 2013; Enlow, Egeland, Carlson, Blood, & Wright, 2014). According to Brothers (Brothers, 2014), ‘the effects of trauma are transmitted within the moment-to-moment relational exchanges, largely nonverbal, that occur between parents and children’ (p.5). Indeed, attachment-related disruptions in both parent and child have been found to explain the effects of a parent’s trauma on a non-traumatized child (Almqvist & Broberg, 2003; De Haene, Dalgaard, Montgomery, Grietens, & Verschueren, 2013). Moreover, findings indicate that attachment security serves as a protective factor in preventing the transmission of PTSD to offspring (Van Ee, Kleber, & Mooren, 2012). However, these studies did not examine whether trauma survivors’ PTSD exacerbates the intergenerational transmission of attachment insecurities.
The main goal of the current study was to shed light on the impact of the self-amplifying cycle of PTSD and attachment insecurities among ex-POWs on their offspring’s attachment insecurities. Based on findings about the self-amplifying cycle of PTSD and attachment insecurities among Israeli ex-POWS (Mikulincer et al., 2011; Solomon et al., 2008), we hypothesized that the intergenerational transmission of attachment insecurities (anxiety, avoidance) would be stronger in the ex-POW group than in the control group and would be exacerbated by the veteran’s PTSD severity. Specifically, we predicted that:
The association between veterans’ attachment anxiety and adult offspring’s attachment anxiety would be stronger among ex-POWs than among control veterans.
The association between veterans’ attachment avoidance and adult offspring’s attachment avoidance would be stronger among ex-POWs than among control veterans.
Veterans’ PTSD severity would heighten the strength of these associations.
2. Method
2.1. Participants and procedure
This study constituted part of a larger longitudinal study assessing the long-term psychosocial impact of war captivity among Israeli veterans of the 1973 Yom Kippur War at three time points (1991, 2003, 2008) (Solomon et al., 2012). The current study relies on veterans’ data collected in the most recent wave of measurement (2008). Data from offspring were collected only once at 2013–2014. The five-year difference in data collection from veterans and their offspring was due to logistic and budget-related reasons.
The current sample consisted of 120 dyads of male veterans of the Israel Defence Forces (IDF) who participated in the 1973 Yom Kippur War and their adult offspring. Upon receiving both the IDF’s and Tel Aviv University’s institutional review board (IRB) approvals, in accordance with the ethical standards laid down in the Declaration of Helsinki. We contacted the veterans and their adult offspring and obtained written informed consent from them.
The sample consisted of two groups: 80 dyads of ex-POWS and their adult offspring (the ex-POW group) and 40 former Israeli combat soldiers who fought in the Yom Kippur war, but were never held captive, and their adult offspring (the control group). No significant differences were found between ex-POWs and controls in socio-demographic variables and military history (see Table 1). In addition, no significant differences were found between the two offspring groups, besides of controls’ offspring reporting more years of education than POWs’ offspring (see Table 1).
Table 1.
Socio-Demographic characteristics of ex-POWs and controls and their adult offspring
| Ex-POW (n = 80) |
Control (n = 40) |
|||
|---|---|---|---|---|
| Fathers’ Variables | ||||
| Age |
M = 57.86 (SD = 6.25) |
M = 56.58 (SD = 4.16) |
t (118) = −1.14 | |
| Education |
M = 14.04 (SD = 4.40) |
M = 14.43 (SD = 3.16) |
t (118) =.49 | |
| Participation in previous wars |
M = .30 (SD = .72) |
M = .62 (SD = 1.02) |
t (118) = 1.81 | |
| Combat exposure |
M = 1.41 (SD = .56) |
M = 1.68 (SD = .71) |
t (118) = 1.65 | |
| Negative life events since war |
M = 7.10 (SD = 5.02) |
M = 6.74 (SD = 5.12) |
t (118) = −.37 | |
| Country of origin | Israel | 50 (62.5%) |
30 (75%) |
χ2 (2) = 4.02 |
| America | 20 (25%) | 7 (17.5%) | ||
| Europe | 10 (12.5%) | 3 (7.5%) | ||
| Religiosity | Secular | 49 (65.3%) | 23 (59%) | χ2 (2) = .80 |
| Traditional | 20 (26.7%) | 11 (28.2%) | ||
| Religious | 6 (8%) | 5 (12.8%) | ||
| Offspring variables | ||||
| Age |
M = 35.12 (SD = 6.49) |
M = 34.84 (SD = 5.44) |
t (118) = −.23 | |
| Education (years) |
M = 14.89 (SD = 2.81) |
M = 16.42 (SD = 2.51) |
t (118) = 3.00** | |
| Negative life events |
M = 2.15 (SD = 1.52) |
M = 2.02 (SD = 1.62) |
t (117) =.42 | |
| Gender | Female | 43 (53.75%) | 20 (50%) | χ2 (1) = 1.05 |
| Male | 37 (46.25%) | 20 (50%) | ||
| Birth order | Firstborn | 42 (52.5%) | 26 (65%) | χ2 (4) = 5.25 |
| Second born | 21 (26.25%) | 11 (27.5%) | ||
| Third born | 9 (11.25%) | 1 (2.5%) | ||
| Fourth born | 6 (7.5%) | 2 (5%) | ||
| Fifth born | 2 (2.5%) | 0 (0%) | ||
| Marital Status | Single | 29 (36.25%) | 14 (35%) | χ2 (3) = 3.76 |
| Married | 42 (52.5%) | 25 (62.5%) | ||
| Divorced | 8 (10%) | 1 (2.5%) | ||
| Other | 1 (1.25%) | 0 (0%) | ||
| Military service | Complete | 62 (79.5%) | 36 (81.8%) | χ2 (3) = 5.40 |
| Partial | 4 (5.1%) | 4 (9.1%) | ||
| National | 2 (2.5%) | 3 (6.8%) | ||
| Other | 10 (12.8%) | 1 (2.3%) | ||
| Religiosity | Secular | 54 (70.1%) | 25 (62.5%) | χ2 (4) = 3.96 |
| Traditional | 13 (16.9%) | 11 (27.5%) | ||
| Religious | 8 (10.4%) | 3 (7.5%) | ||
| Orthodox | 1 (1.3%) | 0 (0%) | ||
| Other | 1 (1.3%) | 1 (2.5%) | ||
| Country of | Israel | 72 (90%) | 37 (92.5%) | χ2 (1) = .18 |
| origin | Other | 8 (10%) | 3 (7.5%) | |
| Income | Well below average | 4 (5.2%) | 6 (15%) | χ2 (4) = 8.77 |
| Below average | 14 (18.7%) | 8 (20%) | ||
| Average | 23 (30.7%) | 6 (15%) | ||
| Above average | 23 (30.7%) | 12 (30%) | ||
| Well above average | 11 (14.7%) | 8 (15%) |
** = p <.01.
2.2. Veteran measures
Veterans’ PTSD intensity was assessed via the PTSD Inventory (Solomon et al., 1993) with regard to the Yom Kippur War. The scale consists of 17 items tapping the 17 PTSD symptoms listed in the DSM-IV-TR (American Psychiatric Association (4th, Text Re), 2000), which was the standard of clinical practice at the time of veterans’ assessment (2008). Participants rated how often they experienced each symptom in the past month on a 4-point scale ranging from 1 (not at all) to 4 (very often). The scale has good psychometric properties, including high convergent validity with clinical interviews based on the SCID (Solomon et al., 1993). In our sample, Cronbach α for the 17 items was.88. For each participant, we then summed up the 17 ratings, with higher scores indicating more severe PTSD (see Ms and SDs in Table 2).
Table 2.
Means, SDs, and F-Tests for Veterans’ and Offspring’s Variables According to Study Group
| Total Sample |
Ex-POWs |
Controls |
F |
|||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | (1,118) | p | |
| Veterans’ variables | ||||||||
| PTSD severity | 6.652 | 5.694 | 9.182 | 5.320 | 1.953 | 2.485 | 69.23 | <.001 |
| Attachment anxiety | 2.743 | 1.044 | 3.020 | 1.056 | 2.229 | .809 | 17.87 | <.001 |
| Attachment avoidance | 3.707 | 1.358 | 4.124 | 1.338 | 2.934 | 1.024 | 25.22 | <.001 |
| Offspring’s variables | ||||||||
| Attachment anxiety | 3.217 | 1.225 | 3.382 | 1.287 | 2.909 | 1.045 | 4.19 | .043 |
| Attachment avoidance | 3.300 | 1.050 | 3.414 | 1.104 | 3.088 | .917 | 2.67 | .105 |
| MANOVA F (5, 114) | 14.56 | <.001 | ||||||
Veterans’ attachment orientations were assessed with a brief 10-item scale (Mikulincer, Florian, & Tolmacz, 1990) tapping attachment anxiety and avoidance (five items per dimension). The anxiety items (e.g. ‘I worry about being abandoned’) correspond to anxiety items on the 36-item Experiences in Close Relationships scale (ECR) (Brennan et al., 1998), the most frequently used scale for assessing attachment orientations (Mikulincer & Shaver, 2016). The avoidance items (e.g. ‘I feel uncomfortable when others get close to me’) correspond to ECR’s avoidance items. We used this brief scale for assessing veterans’ attachment orientations because the ECR scale did not exist (it was constructed at 1998) at the time of the first wave of measurement of veterans’ data (1991) and the 10-item scale was already used in an Israeli sample (Mikulincer et al., 1990). In addition, due to the length of the battery of scales veterans completed at each wave of measurement, we preferred to use a brief scale tapping attachment orientations. Participants were asked to focus on their feelings and thoughts in close relationships in general (and not in a specific kind of relationship, such as romantic relationships or friendships) and to rate the extent to which each item described their feelings and thoughts on a 7-point scale ranging from 1 (not at all) to 7 (very much). There is extensive evidence for the reliability and validity of this measure (Arikan et al., 2016). In the current sample, Cronbach αs were .82 for anxiety and .78 for avoidance subscales. Items on each subscale were then averaged, with a higher score indicating greater anxiety or avoidance (see Ms and SDs in Table 2). A significant correlation was found between these two scores, r(118) = .369, p < .001.
2.3. Offspring measures
Attachment orientations were assessed with the 36-item Experiences in Close Relationships scale (ECR) (Brennan et al., 1998), tapping attachment anxiety and avoidance (18 items per dimension). Since offspring completed only few self-report scales, we decided to use the full 36-item ECR scale to get a more comprehensive assessment of attachment orientations. Participants were asked to focus on their feelings and thoughts in close relationships in general (and not in a specific kind of relationship, such as romantic relationships or friendships) and to rate the extent to which each item described their feelings and thoughts on a 7-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). There is extensive evidence for the ECR’s reliability and validity (Arikan et al., 2016). In the current sample, Cronbach αs were .90 for anxiety and .88 for avoidance subscales. Two scores were then computed for each participant by averaging items from each subscale, with higher scores reflecting greater anxiety and avoidance (see Ms and SDs in Table 2). A significant correlation was found between these two scores, r(118) = .318, p < .001.
2.4. Data analyses
Before examining the study’s predictions, we conducted two preliminary analyses. First, we conducted multivariate and univariate analyses of variance (ANOVAs) examining groups differences in PTSD and attachment scores. Second, we conducted Pearson correlations examining bivariate associations between study variables in the total sample and each study group. In order to test predictions a and b concerning the role of captivity trauma in the intergenerational transmission of attachment orientations, we conducted two-step hierarchical regressions examining the unique and interactive contributions of war captivity (ex-POWs vs. controls) and veterans’ attachment scores (anxiety, avoidance) to offspring’s attachment scores (anxiety, avoidance). Finally, in order to test prediction c concerning the role veterans’ PTSD plays in the intergenerational transmission of attachment orientations following war captivity, we conducted moderated mediation analyses in which we examined the strength and significance of the conditional indirect effects war captivity (ex-POWs vs. controls) and veterans’ attachment scores (anxiety, avoidance) on offspring’s attachment scores (anxiety, avoidance) that were mediated by veterans’ PTSD.
3. Results
3.1. Preliminary analyses
Before testing study’s predictions, we conducted two preliminary analyses. First, we conducted multivariate and univariate analyses of variance (ANOVAs) examining differences between study groups in veterans’ and offspring’s variables. The multivariate group difference was significant (see Table 2). Univariate ANOVAs indicated that ex-POWs reported more severe PTSD symptomatology and higher levels of attachment anxiety and avoidance than did control veterans (see Table 2). In addition, ex-POWs’ offspring reported higher attachment anxiety than offspring of control veterans (see Table 2). No significant group difference was found in offspring’s attachment avoidance.
Second, we conducted Pearson correlations examining bivariate associations between study variables in the total sample and each study group. Veterans’ PTSD severity had significant positive associations with both their own attachment scores and their offspring’s attachment scores in the total sample and among ex-POWs, but not among controls (see Table 3). In addition, veterans’ attachment anxiety had significant positive associations with their offspring’s attachment anxiety and avoidance in the total sample and in the ex-POW group, but not in the control group (see Table 3). Veterans’ attachment avoidance was not significantly associated with offspring’s attachment scores in any of the groups (see Table 3).
Table 3.
Pearson Correlations between Study’s Variables in the Total Sample and Each Study Group
| Total Sample |
Ex-POWs |
Control Veterans |
||||
|---|---|---|---|---|---|---|
| r | p | R | p | r | p | |
| Pearson rs for veteran’s PTSD severity with: | ||||||
| Veteran anxiety | .537 | <.001 | .499 | <.001 | .098 | .535 |
| Veteran avoidance | .518 | <.001 | .420 | <.001 | .108 | .494 |
| Offspring anxiety | .380 | <.001 | .439 | <.001 | −.086 | .589 |
| Offspring avoidance | .341 | <.001 | .424 | <.001 | −.144 | .364 |
| Pearson rs for veteran’s attachment anxiety with: | ||||||
| Offspring anxiety | .320 | <.001 | .431 | <.001 | −.193 | .222 |
| Offspring avoidance | .239 | .009 | .380 | <.001 | −.331 | .032 |
| Pearson rs for veteran’s attachment avoidance with: | ||||||
| Offspring anxiety | .184 | .043 | .193 | .089 | −.101 | .526 |
| Offspring avoidance | .067 | .466 | .083 | .471 | −.224 | .154 |
3.2. Hypothesis testing
The hypothesis that the trauma of captivity would intensify the intergenerational transmission of attachment insecurities was tested with two-step hierarchical regressions. The predicted variables were offspring’s attachment anxiety and avoidance (in separate regressions). In the first step, we examined the main effects for study group (ex-POWs, +1, to control veterans, −1) and veterans’ attachment anxiety and attachment avoidance (mean centred). In the second step, we examined the interactive effects of study group with each veteran’s attachment score (anxiety, avoidance).
The full regression model predicting offspring’s attachment anxiety was significant and explained 18.6% of the variance (see Table 4). In the first step, only the main effect for veterans’ attachment anxiety was significant, with veterans’ attachment anxiety contributing to offspring’s higher attachment anxiety (see Table 4). In the second step, the interaction for study group and veterans’ attachment anxiety was significant (see Table 4). Other effects were not significant (see Table 4). Simple slope effects tests revealed that veterans’ attachment anxiety was significantly and positively associated with offspring’s attachment anxiety only in the ex-POW group, b = .536, t = 4.32, p < .001, 95% Confidence Interval (CI) [.291, .782], but not in the control group, b = −.253, t = −1.15, p = .254, 95% CI [−.692, .185]. That is, a significant intergenerational transmission of attachment anxiety was observed only among ex-POWs.
Table 4.
Regression Analysis for Offspring Attachment Orientations as a Function of Study Group and Veteran’s Attachment Orientations
| b (SE) | t | p | β | 95% CI | |
|---|---|---|---|---|---|
| Offspring’s attachment anxiety | |||||
| Step 1 | |||||
| Study group | .078 (.127) | .61 | .542 | .061 | −.174,.329 |
| Veteran anxiety | .331 (.116) | 2.85 | .005 | .277 | .101,.562 |
| Veteran avoidance | .070 (.122) | 0.57 | .568 | .057 | −.172,.313 |
| R2 Step 1 | .110 | ||||
| Step 2 | |||||
| Group x veteran anxiety | .376 (.139) | 2.69 | .008 | .294 | .099,.652 |
| Group x veteran avoidance | .086 (.147) | .59 | .558 | .065 | −.205,.378 |
| ∆R2 Step 2 | .076 | ||||
| Total R2 | .186 | ||||
| F (5, 114) | 5.19*** | ||||
| Offspring’s attachment avoidance | |||||
| Step 1 | |||||
| Study group | .098 (.112) | .88 | .383 | .089 | −.124,.320 |
| Veteran anxiety | .232 (.102) | 2.27 | .025 | .226 | .029,.434 |
| Veteran avoidance | −.057 (.108) | −0.53 | .600 | −.054 | −.270,.157 |
| R2 Step 1 | .064 | ||||
| Step 2 | |||||
| Group x veteran anxiety | .369 (.122) | 3.03 | .003 | .337 | .128,.610 |
| Group x veteran avoidance | .062 (.128) | .49 | .627 | .054 | −.192,.316 |
| ∆R2 Step 2 | .092 | ||||
| Total R2 | .156 | ||||
| F (5, 114) | 4.23** | ||||
**p <.01; ***p <.001.
A similar pattern of effects was found for offspring’s attachment avoidance. The full regression model was significant and explained 15.6% of the variance (see Table 4). The main effect for veterans’ attachment anxiety was significant, with veterans’ attachment anxiety contributing to offspring’s higher attachment avoidance (see Table 4). The interaction for study group and veterans’ attachment anxiety was also significant. Other effects were not significant (see Table 4). Simple slope effects tests revealed that veterans’ attachment anxiety was significantly and positively associated with offspring’s attachment avoidance in the ex-POW group, b = .406, t = 3.77, p < .001, 95% CI [.192, .619]. In the control group, veterans’ attachment anxiety was significantly and negatively associated with offspring’s attachment avoidance, b = −.383, t = −1.99, p = .049, 95% CI [−.764, −.002]. That is, whereas veterans’ attachment anxiety contributed to offspring’s heightened attachment avoidance in the ex-POW group, it contributed to offspring’s decreased avoidance in the control group.
3.3. The mediating role of veterans’ PTSD
The mediating role of veterans’ PTSD was examined with a moderated mediation analyses using model 8 in PROCESS (Hayes, 2012). The 95% CIs obtained for the indirect effects were estimated from bootstrapping with 10,000 resamples. Predictors were veterans’ attachment anxiety (mean centred) and study group (ex-POWs = +1, control veterans = −1), and the mediator was veterans’ PTSD severity (mean centred). We conducted these analyses separately for each offspring’s attachment score (anxiety, avoidance).
The analysis predicting offspring’s attachment anxiety showed a significant moderated mediation effect, index of moderated mediation = .132, SE = .067, 95% CI [.010, .273] (see Figure 1). Including veterans’ PTSD severity in the model predicting offspring’s attachment anxiety rendered the previously significant interaction of veterans’ attachment anxiety and study group (total effect, t = 3.11, p = .002) no longer significant (direct effect, t = 1.57, p = .143). In addition, there was a significant positive conditional indirect effect of veterans’ attachment anxiety on offspring’s attachment anxiety through veteran’s more severe PTSD among ex-POWs, Meffect = .150, SE = .070, 95% CI [.011, .289]. Among control veterans, this indirect effect was not significant, Meffect = .018, SE = .036, 95% CI [−.036, .108]. Thus, only in the ex-POW group did veterans’ attachment anxiety contribute to more severe PTSD, which subsequently increased offspring’s attachment anxiety.
Figure 1.
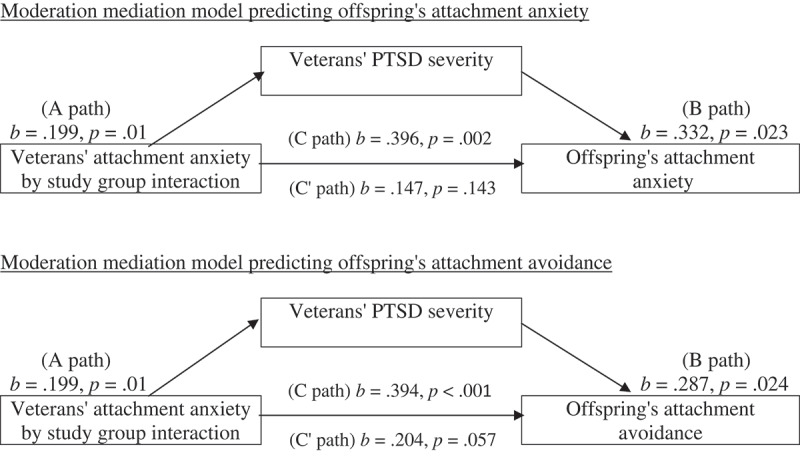
Moderation mediation models of the interactive effect of veterans’ attachment anxiety and study group on offspring’s attachment scores (anxiety, avoidance) via increase in veterans’ PTSD severity (N = 120)
The analysis predicting offspring’s attachment avoidance yielded a similar significant pattern of moderated mediation, index of moderated mediation = .114, SE = .061, 95% CI [.013, .252] (see Figure 1). Including veterans’ PTSD severity in the model predicting offspring’s attachment avoidance rendered the previously significant interaction of veterans’ attachment anxiety and study group (total effect, t = 3.57, p < .001) no longer significant (direct effect, t = 1.92, p = .057). In addition, there was a significant positive conditional indirect effect of veterans’ attachment anxiety on offspring’s attachment avoidance through veteran’s more severe PTSD among ex-POWs, Meffect = .130, SE = .062, 95% CI [.021, .266]. Among control veterans, this indirect effect was not significant, Meffect = .016, SE = .032, 95% CI [−.037, .092]. Thus, only in the ex-POW group did veterans’ attachment anxiety contribute to more severe PTSD, which subsequently increased offspring’s attachment avoidance.
4. Discussion
Our study provides novel evidence about the intergenerational impact of the self-amplifying cycle of PTSD and attachment insecurities following trauma exposure on offspring’s attachment insecurities. Veterans’ attachment anxiety was associated with offspring’s reports of higher attachment insecurities, either anxiety or avoidance. However, this intergenerational effect was found only in the ex-POW group and it was mediated by ex-POWs’ PTSD severity. That is, ex-POWS who reported higher levels of attachment anxiety reported more intense PTSD, which, in turn, contributed to offspring’s higher attachment anxiety or avoidance. Findings also indicated that veterans’ attachment avoidance had no significant impact on offspring’s attachment orientation. Overall, these findings clearly indicate that the trauma of captivity and PTSD heightened the intergenerational associations between fathers’ attachment anxiety and offspring’s attachment insecurities.
The current findings advance attachment research by examining the intergenerational transmission of attachment in light of fathers’ captivity trauma. Fitting our predictions, we found that associations between veterans’ attachment anxiety and adult offspring’s attachment insecurities, either anxiety or avoidance, were stronger among ex-POWs than among control veterans. To the best of our knowledge, no study has examined the intergenerational transmission of attachment orientations among trauma survivors. Our findings are consistent with existing evidence regarding the contribution of a father’s attachment orientations to his offspring’s attachment orientations (Hazen et al., 2010). However, they emphasize that this association is particularly notable among fathers who survived the trauma of war captivity.
Among ex-POWs, attachment anxiety was also associated with offspring’s heightened attachment avoidance. Ex-POWs scoring relatively high on attachment anxiety might worry not only about their worth and lovability, but might also perceive the world as dangerous, people as harmful, and life as unjust and uncontrollable due to their captivity experience (Levin, Mikulincer, & Solomon, 2019). This combination of attachment anxiety and shattered beliefs about the world and others is devastating for ex-POWs’ mental health (Levin et al., 2019) and might interfere with their sensitivity and responsiveness to offspring’s needs, thereby increasing offspring’s attachment insecurities. As a result, the development of offspring’s attachment anxiety might be a direct reflection of father’s worries about worth and lovability, whereas the development of offspring’s attachment avoidance might result from father’s shattered core beliefs about the world and others. Alternatively, the heightening of offspring’s attachment avoidance might reflect a defensive detachment response from the overwhelming helplessness, suffering, and pain experienced by attachment-anxious ex-POWs. In any case, these are post-hoc speculations that should be systematically examined in future studies.
Contrary to our prediction, fathers’ attachment avoidance was not significantly associated with adult offspring’s attachment avoidance among ex-POWs or control veterans. Several studies have documented that people scoring higher on attachment avoidance are less engaged in their parenting role and less sensitive to their offspring’s needs (Bachem, Scherf, Levin, Schröder-Abé, & Solomon, 2019; Berlin, Cassidy, & Appleyard, 2008). As a result, one might expect a heightening of offspring’s attachment insecurities due to lack of sensitive paternal caregiving. However, our findings failed to document this intergenerational process, implying that fathers’ attachment-related anxiety is more detrimental to offspring’s attachment security than fathers’ avoidant, emotionally-detached position within the family. However, one should take into account that self-report scales, like those used in the current study, might have problems in capturing variations on attachment avoidance, because people may reflect on avoidance items as ‘I like doing it myself’ rather than reflecting on the defensive inhibition and denial of their need for attachment. This methodological limitation might explain why findings for attachment avoidance were not as clear as for attachment anxiety. Future studies on the intergenerational transmission of attachment orientations would benefit from including other techniques, such as clinical interviews or projective measures, beyond self-report scales in order to tap more implicit, less conscious manifestations of attachment avoidance.
The tendency of attachment-anxious fathers to overtly express overwhelming distress and pain (Mikulincer & Shaver, 2019) might be so emotionally contagious that it can interfere with offspring’s emotional equanimity and set the basis for the development of attachment insecurities. In contrast, the tendency of attachment-avoidant fathers to remain emotionally detached (Mikulincer & Shaver, 2019) might be less devastating to offspring’s mental state because they can still receive care and love from their mother. That is, whereas mothers can compensate for the attachment-avoidant father’s lack of parental emotional involvement, they might be less able to buffer the extreme distress caused by the tumultuous emotional world of attachment-anxious fathers.
The current findings might also be attributed to potential differences between fathers and mothers in the intergenerational transmission of avoidant attachment. While mothers scoring higher on attachment avoidance are more likely to react with destructive and distress-related responses during conflicts with their children, this tendency was not found among attachment-avoidant fathers (Wilson, Rholes, Simpson, & Tran, 2007). These fathers have been found to report heightened parental burden and work-family conflicts (Kohn et al., 2012). It is therefore possible that attachment-avoidant fathers’ discomfort in the family niche is not enough to heighten offspring’s attachment insecurities; it may, instead, be that these insecurities result from more tumultuous and distress-eliciting interactions with parents.
A third possible explanation concerns the differential involvement of attachment anxiety and avoidance in the self-amplifying PTSD-attachment cycle. Several studies (Elklit, Karstoft, Lahav, & Andersen, 2016; Ogle, Rubin, & Siegler, 2015) and a meta-analysis of 46 studies (Woodhouse et al., 2015) found that attachment anxiety is more strongly related to PTSD symptoms than attachment avoidance. In addition, there are differences between thw two secondary attachment strategies in regulation of emotions (Mikulincer & Shaver, 2016). Whereas attachment anxiety tends to under-regulate (and even exacerbate) the experience and expression of distress and other negative emotions as a means for eliciting others’ sympathy, compassion, and love,, attachment avoidance tends to over-regulate emotions in an attempt to dismiss feelings of vulnerability and neediness and inhibit distress awareness (Van Dijke & Ford, 2015). Therefore, it is reasonable that attachment anxiety, which reflects under-regulation of negative emotions, has been found to be associated with more negative interpretations of distressing events (Collins, 1996), greater emotional intensity (Searle & Meara, 1999), and more negative perceptions of physical and psychological symptoms (Watt, McWilliams, & Campbell, 2005).
All of these can cause attachment-anxious people to respond inconsistently to their children’s needs, being overinvolved or intrusive at times and non-responsive or insensitive at other times (Main & Hesse, 1990). As a result, their offspring might develop hyper-focus on attachment-related thoughts and feelings (Bowlby, 1982; Mikulincer & Shaver, 2003), potentially making it difficult to maintain a stable sense of security. Of course, all these three alternative interpretations are post hoc speculations that should be examined in future studies.
Supporting our third prediction, the link between fathers’ attachment anxiety and offspring’s attachment insecurities among ex-POWs was mediated by fathers’ PTSD severity. Specifically, among ex-POWs, attachment anxiety contributed to more severe PTSD, which, in turn, increased offspring’s attachment anxiety and avoidance). This finding indicates that the self-amplifying PTSD-attachment cycle among ex-POWs not only contributes to the preservation of the disorder over time (Mikulincer et al., 2011), but can also be transmitted to the offspring in the form of heightened attachment insecurities.
The self-amplifying PTSD-attachment cycle seem to interfere with the functioning of the attachment system, reducing the extent to which mental representations of attachment security can soothe and comfort a traumatized person, thereby making it more difficult to mitigate distress and restore emotional equanimity (Mikulincer et al., 2011). This cycle might be transferred to offspring who grow up with a father who is unable to mitigate distress and is overwhelmed by feelings of unlovability, helplessness, and meaningless. This intergenerational transmission may then initiate a similar cascade of mental events in the offspring, including strong feelings of loneliness and rejection, negative core beliefs about the self and others, and reliance on less effective strategies of affect regulation, which prevent resolution of the secondary traumatization. According to Lieberman (Lieberman, 2004), a parent suffering from PTSD carries severe attachment injuries, which might be experienced by the child as terrifying. The internal disorganization of the parent is transmitted to the offspring not only through outbursts of anger and severe punishments, but also from the exposure on a daily basis to situations where children witness parent’s helplessness.
Before finishing this discussion, we want to deal with an unexpected finding concerning group differences in offspring’s educational attainment: Ex-POWs’ offspring had lower educational attainment than controls’ offspring. This difference may play an undetected role in explaining the heightened attachment insecurities and PTSD of ex-POWs’ offspring. It is possible that impoverished education leads ex-POWs’ offspring to be more subject to socioeconomic-related stressors that might amplify their sense of attachment insecurity. Future studies should attempt to provide a more comprehensive assessment of offspring’s educational history and examine whether poor educational attainment may be another important intergenerational outcome of ex-POWs’ attachment anxiety and PTSD.
The current findings should be considered in light of several limitations. First, although our study extends research on the intergenerational transmission of father-child attachment insecurities to adult offspring, we have no information regarding offspring’s attachment orientations during infancy, childhood, or adolescence. Second, all of the findings are based upon self-report measures, entailing a risk of reporting bias. Future studies should include additional methods of data collection, such as observational and clinical assessments of attachment insecurities. In addition, we asked participants to reflect on close relationships in general rather than on a specific kind of relationship (romantic relationships, friendships) or the relationship they held with a specific partner. Future studies can benefit from assessing participants within-relationship attachment orientations. Third, the current study relied only on fathers’ reports and did not provide information about the potential role that mothers’ attachment and stress response could play in the intergenerational transmission of attachment. Further studies should compare ex-POWs to veterans who have comparably high levels of PTSD symptoms in order to better understand the unique contribution of captivity trauma. In addition, future studies should adopt a triadic design and examine the family context in which this intergenerational transmission takes place. Fourth, future studies should attempt to replicate the current findings with other types of trauma and in other societies and cultures.
Nonetheless, the current study has important theoretical and practical implications for the study of trauma, PTSD, and the intergenerational transmission of attachment. The findings suggest that the ex-POWs’ self-amplifying PTSD-attachment cycle seems to have an intergenerational component in that they amplify offspring’s attachment insecurities. These findings may be important for clinicians working with trauma survivors and their offspring. They imply that therapeutic work should focus not only on the trauma but also on the traumatized person’s attachment injuries and the shattering of core beliefs about the world, self, and others. In this context, attachment-based therapies (Bateman & Fonagy, 2010) can be helpful.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Almqvist, K., & Broberg, A. G. (2003). Young children traumatized by organized violence together with their mothers–The critical effects of damaged internal representations. Attachment & Human Development, 5(4), 367–12. [DOI] [PubMed] [Google Scholar]
- Aloni, R., Crompton, L., Levin, Y., & Solomon, Z. (2018). The impact of captivity and posttraumatic stress disorder on cognitive performance among former prisoners of war: A longitudinal study. The Journal of Clinical Psychiatry, 79(3), 17m11577. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (4th, Text Re) . (2000). Diagnostic and statistical manual of mental disorders. Washington: American Psychiatric Association. [Google Scholar]
- Arikan, G., Stopa, L., Carnelley, K. B., & Karl, A. (2016). The associations between adult attachment, posttraumatic symptoms, and posttraumatic growth. Anxiety, Stress, & Coping, 29(1), 1–20. [DOI] [PubMed] [Google Scholar]
- Bachem, R., Scherf, J., Levin, Y., Schröder-Abé, M., & Solomon, Z. (2019). The role of parental negative world assumptions in the intergenerational transmission of war trauma. Social Psychiatry and Psychiatric Epidemiology, 1–11. doi: 10.1007/s00127-019-01801-y [DOI] [PubMed] [Google Scholar]
- Barr, P. (2014). Adult attachment dimensions, worldview schemas, and the psychological health of parents of infants in a neonatal intensive care unit. Journal of Loss and Trauma, 19(6), 537–557. [Google Scholar]
- Bateman, A., & Fonagy, P. (2010). Mentalization based treatment for borderline personality disorder. World Psychiatry, 9(1), 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belt, R. H., Kouvo, A., Flykt, M., Punamäki, R. L., Haltigan, J. D., Biringen, Z., & Tamminen, T. (2013). Intercepting the intergenerational cycle of maternal trauma and loss through mother–infant psychotherapy: A case study using attachment-derived methods. Clinical Child Psychology and Psychiatry, 18(1), 100–120. [DOI] [PubMed] [Google Scholar]
- Berlin, L. J., Cassidy, J., & Appleyard, K. (2008). The influence of early attachments on other relationships. In Cassidy J. & Shaver P. R. (Eds.), Handbook of attachment: Theory, research, and clinical applications (2nd ed., pp. 333–347). New York: The Guilford Press. [Google Scholar]
- Bowlby, J. (1982). Attachment and loss: Retrospect and prospect. American Journal of Orthopsychiatry, 52(4), 664–678. [DOI] [PubMed] [Google Scholar]
- Bradfield, B. C. (2013). The intergenerational transmission of trauma as a disruption of the dialogical self. Journal of Trauma & Dissociation, 14(4), 390–403. [DOI] [PubMed] [Google Scholar]
- Brennan, K. A., Clark, C. L., & Shaver, P. R. (1998). Self-report measurement of adult romantic attachment: An integrative overview. In Simpson J. A. & Rholes W. S. (Eds.), Attachment theory and close relationships (pp. 46–76). New York: Guilford Press. [Google Scholar]
- Brothers, D. (2014). Traumatic attachments: Intergenerational trauma, dissociation, and the analytic relationship. International Journal of Psychoanalytic Self Psychology, 9(1), 3–15. [Google Scholar]
- Charuvastra, A., & Cloitre, M. (2008). Social bonds and posttraumatic stress disorder. Annual Review of Psychology, 59, 301–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, N. L. (1996). Working models of attachment: Implications for explanation, emotion, and behavior. Journal of Personality and Social Psychology, 71(4), 810–832. [DOI] [PubMed] [Google Scholar]
- De Haene, L., Dalgaard, N. T., Montgomery, E., Grietens, H., & Verschueren, K. (2013). Attachment narratives in refugee children: Interrater reliability and qualitative analysis in pilot findings from a two‐Site study. Journal of Traumatic Stress, 26(3), 413–417. [DOI] [PubMed] [Google Scholar]
- Dekel, R., & Monson, C. M. (2010). Military-related post-traumatic stress disorder and family relations: Current knowledge and future directions. Aggression and Violent Behavior, 15(4), 303–309. [Google Scholar]
- Dieperink, M., Leskela, J., Thuras, P., & Engdahl, B. (2001). Attachment style classification and posttraumatic stress disorder in former prisoners of war. American Journal of Orthopsychiatry, 71(3), 374–378. [DOI] [PubMed] [Google Scholar]
- Elklit, A., Karstoft, K. I., Lahav, Y., & Andersen, T. E. (2016). Attachment and posttraumatic stress disorder in multiple trauma samples. Journal of Psychiatry, 19(3), 1–7. [Google Scholar]
- Enlow, M. B., Egeland, B., Carlson, E., Blood, E., & Wright, R. J. (2014). Mother–infant attachment and the intergenerational transmission of posttraumatic stress disorder. Development and Psychopathology, 26(1), 41–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figley, C. (1995). Compassion fatigue: Coping with secondary traumatic stress disorder. New York: Brunner/Mazel. [Google Scholar]
- Fraley, R. C., Fazzari, D. A., Bonanno, G. A., & Dekel, S. (2006). Attachment and psychological adaptation in high exposure survivors of the September 11th attack on the World Trade Center. Personality and Social Psychology Bulletin, 32(4), 538–551. [DOI] [PubMed] [Google Scholar]
- Galovski, T., & Lyons, J. A. (2004). Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran’s family and possible interventions. Aggression and Violent Behavior, 9(5), 477–501. [Google Scholar]
- Ginzburg, K., Ein-Dor, T., & Solomon, Z. (2010). Comorbidity of posttraumatic stress disorder, anxiety and depression: A 20-year longitudinal study of war veterans. Journal of Affective Disorders, 123(1–3), 249–257. [DOI] [PubMed] [Google Scholar]
- Grossmann, K., Grossmann, K. E., Fremmer‐Bombik, E., Kindler, H., Scheuerer‐Englisch, H., & Zimmermann, A. P. (2002). The uniqueness of the child–father attachment relationship: Fathers’ sensitive and challenging play as a pivotal variable in a 16‐year longitudinal study. Social Development, 11(3), 301–337. [Google Scholar]
- Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. Retrieved from www.afhayes.com/public/process2012.pdf
- Hazen, N. L., McFarland, L., Jacobvitz, D., & Boyd‐Soisson, E. (2010). Fathers’ frightening behaviours and sensitivity with infants: Relations with fathers’ attachment representations, father–infant attachment, and children’s later outcomes. Early Child Development and Care, 180(1–2), 51–69. [Google Scholar]
- Herman, J. L. (1992). Trauma and recovery: The aftermath of violence from domestic abuse to political terror. New York: Basic Book. [Google Scholar]
- Jordan, B. K., Marmar, C. R., Fairbank, J. A., Schlenger, W. E., Kulka, R. A., Hough, R. L., & Weiss, D. S. (1992). Problems in families of male Vietnam veterans with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 60(6), 916–926. [DOI] [PubMed] [Google Scholar]
- Kohn, J. L., Rholes, S. W., Simpson, J. A., Martin, A. M., Tran, S., & Wilson, C. L. (2012). Changes in marital satisfaction across the transition to parenthood: The role of adult attachment orientations. Personality and Social Psychology Bulletin, 38(11), 1506–1522. [DOI] [PubMed] [Google Scholar]
- Levin, Y., Mikulincer, M., & Solomon, Z. (2019). Attachment orientations moderate the self-amplifying cycle of posttraumatic stress disorder and negative cognitions—A seven-year longitudinal study. Journal of Social and Clinical Psychology, 38(6), 522–544. [Google Scholar]
- Lieberman, A. F. (2004). Traumatic stress and quality of attachment: Reality and internalization in disorders of infant mental health. Infant Mental Health Journal, 25(4), 336–351. [Google Scholar]
- Lim, B. H., Hodges, M. A., & Lilly, M. M. (2019). The differential effects of insecure attachment on post-traumatic stress: A systematic review of extant findings and explanatory mechanisms. Trauma, Violence, & Abuse, 152483801881513. doi: 10.1177/1524838018815136 [DOI] [PubMed] [Google Scholar]
- Lucassen, N., Tharner, A., Van IJzendoorn, M. H., Bakermans-Kranenburg, M. J., Volling, B. L., FC, V., & Tiemeier, H. (2011). The association between paternal sensitivity and infant–father attachment security: A meta-analysis of three decades of research. Journal of Family Psychology, 25(6), 986–992. [DOI] [PubMed] [Google Scholar]
- Main, M., & Hesse, E. (1990). Parents’ unresolved traumatic experiences are related to infant disorganized attachment status: Is frightened and/or frightening parental behavior the linking mechanism? In Greenberg M. T., Cicchetti D., & Cummings E. M. (Eds.), Attachment in the preschool years: Theory, research, and intervention (pp. 161–182). Chicago: University of Chicago Press. [Google Scholar]
- Maršanić, V. B., Margetić, B. A., Jukić, V., Matko, V., & Grgić, V. (2014). Self-reported emotional and behavioral symptoms, parent-adolescent bonding and family functioning in clinically referred adolescent offspring of Croatian PTSD war veterans. European Child & Adolescent Psychiatry, 23(5), 295–306. [DOI] [PubMed] [Google Scholar]
- Marshall, E. M., & Frazier, P. A. (2019). Understanding posttrauma reactions within an attachment theory framework. Current Opinion in Psychology, 25, 167–171. [DOI] [PubMed] [Google Scholar]
- Mikulincer, M., Ein-Dor, T., Solomon, Z., & Shaver, P. R. (2011). Trajectories of attachment insecurities over a 17-year period: A latent growth curve analysis of the impact of war captivity and posttraumatic stress disorder. Journal of Social and Clinical Psychology, 30(9), 960–984. [Google Scholar]
- Mikulincer, M., Florian, V., & Tolmacz, R. (1990). Attachment styles and fear of personal death: A case study of affect regulation. Journal of Personality and Social Psychology, 58(2), 273. [Google Scholar]
- Mikulincer, M., & Shaver, P. R. (2003). The attachment behavioral system in adulthood: Activation, psychodynamics, and interpersonal processes. Advances in Experimental Social Psychology, 35, 56–152. [Google Scholar]
- Mikulincer, M., & Shaver, P. R. (2016). Attachment patterns in adulthood: Structure, dynamics, and change (2nd ed.). New York: Guilford Press. [Google Scholar]
- Mikulincer, M., & Shaver, P. R. (2019). Attachment orientations and emotion regulation. Current Opinion in Psychology, 25, 6–10. [DOI] [PubMed] [Google Scholar]
- Mikulincer, M., Shaver, P. R., & Solomon, Z. (2015). An attachment perspective on traumatic and posttraumatic reactions. In Safir M., Wallach H., & Rizzo A. (Eds.), Future directions in post-traumatic stress disorder (pp. 79–96). Boston, MA: Springer. [Google Scholar]
- Murphy, S., Elklit, A., Hyland, P., & Shevlin, M. (2016). Insecure attachment orientations and posttraumatic stress in a female treatment-seeking sample of survivors of childhood sexual abuse: A cross-lagged panel study. Traumatology, 22(1), 48–55. [Google Scholar]
- Ogle, C. M., Rubin, D. C., & Siegler, I. C. (2015). The relation between insecure attachment and posttraumatic stress: Early life versus adulthood traumas. Psychological Trauma: Theory, Research, Practice, and Policy, 7(4), 324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palm, G. (2014). Attachment theory and fathers: Moving from “being there” to “being with”. Journal of Family Theory & Review, 6(4), 282–297. [Google Scholar]
- Paquette, D., & Bigras, M. (2010). The risky situation: A procedure for assessing the father–child activation relationship. Early Child Development and Care, 180(1–2), 33–50. [Google Scholar]
- Ruscio, A. M., Weathers, F. W., King, L. A., & King, D. W. (2002). Male war‐zone veterans’ perceived relationships with their children: The importance of emotional numbing. Journal of Traumatic Stress, 15(5), 351–357. [DOI] [PubMed] [Google Scholar]
- Searle, B., & Meara, N. M. (1999). Affective dimensions of attachment styles: Exploring self-reported attachment style, gender, and emotional experience among college students. Journal of Counseling Psychology, 46(2), 147–158. [Google Scholar]
- Solomon, Z., Benbenishty, R., Neria, Y., Abramowitz, M., Ginzburg, K., & Ohry, A. (1993). Assessment of PTSD: Validation of the revised PTSD Inventory. Israel Journal of Psychiatry and Related Sciences, 30, 110–115. [PubMed] [Google Scholar]
- Solomon, Z., Dekel, R., & Mikulincer, M. (2008). Complex trauma of war captivity: A prospective study of attachment and post-traumatic stress disorder. Psychological Medicine, 38(10), 1427–1434. [DOI] [PubMed] [Google Scholar]
- Solomon, Z., Horesh, D., Ein-Dor, T., & Ohry, A. (2012). Predictors of PTSD trajectories following captivity: A 35-year longitudinal study. Psychiatry Research, 199(3), 188–194. [DOI] [PubMed] [Google Scholar]
- Stovall-McClough, K. C., & Dozier, M. (2016). Attachment states of mind and psychopathology in adulthood. In Cassidy J. & Shaver P. R. (Eds.), Handbook of attachment: Theory, research, and clinical applications (3rd ed., pp. 715–738). New York: Guilford Press. [Google Scholar]
- Van der Kolk, B. (2002). The assessment and treatment of complex PTSD. In Yehuda R. (Ed.), Traumatic stress (pp. 127–156). Washington, DC: American Psychiatric Press. [Google Scholar]
- Van Dijke, A., & Ford, J. D. (2015). Adult attachment and emotion dysregulation in borderline personality and somatoform disorders. Borderline Personality Disorder and Emotion Dysregulation, 2(1), 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ee, E., Kleber, R. J., & Mooren, T. T. (2012). War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant Mental Health Journal, 33(5), 459–468. [DOI] [PubMed] [Google Scholar]
- Van IJzendoorn, M. H. (1995). Adult attachment representations, parental responsiveness, and infant attachment: A meta-analysis on the predictive validity of the adult attachment interview. Psychological Bulletin, 117(3), 387–403. [DOI] [PubMed] [Google Scholar]
- Watt, M. C., McWilliams, L. A., & Campbell, A. G. (2005). Relations between anxiety sensitivity and attachment style dimensions. Journal of Psychopathology and Behavioral Assessment, 27(3), 191–200. [Google Scholar]
- Wilson, C. L., Rholes, W. S., Simpson, J. A., & Tran, S. (2007). Labor, delivery, and early parenthood: An attachment theory perspective. Personality and Social Psychology Bulletin, 33(4), 505–518. [DOI] [PubMed] [Google Scholar]
- Woodhouse, S., Ayers, S., & Field, A. P. (2015). The relationship between adult attachment style and post-traumatic stress symptoms: A meta-analysis. Journal of Anxiety Disorders, 35, 103–117. [DOI] [PubMed] [Google Scholar]
- Zakin, G., Solomon, Z., & Neria, Y. (2003). Hardiness, attachment style, and long term psychological distress among Israeli POWs and combat veterans. Personality and Individual Differences, 34(5), 819–829. [Google Scholar]
- Zerach, G., & Aloni, R. (2015). Secondary traumatization among former prisoners of wars’ adult children: The mediating role of parental bonding. Anxiety Stress & Coping, 28(2), 162–178. [DOI] [PubMed] [Google Scholar]
- Zerach, G., & Solomon, Z. (2016). A relational model for the intergenerational transmission of captivity trauma: A 23-year longitudinal study. Psychiatry, 79(3), 297–316. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. Retrieved from www.afhayes.com/public/process2012.pdf


