Abstract
Background:
Tertiary hyperparathyroidism (THPT) is characterized by hypercalcemia and hyperparathyroidism after renal allograft. Limited data exist regarding the use of intraoperative parathyroid hormone (IOPTH) for THPT. We examined our series of parathyroidectomies performed for THPT to determine clinical outcomes with respect to IOPTH.
Materials and methods:
Patients who underwent parathyroidectomy for THPT (1999-2017) were identified for inclusion. Retrospective chart review was performed. Cure was defined as eucalcemia ≥6 mo after surgery. Statistical analysis was performed.
Results:
Of 41 patients included in the study, 41% (n = 17) were female. The median duration of dialysis before renal allograft was 34 mo (interquartile interval [IQI]:6-60). Preoperatively, the median calcium level was 10.4 mg/dL (IQI:10.0-11.2), median parathyroid hormone was 172 pg/mL (IQI:104-293), and renal function was minimally abnormal with median glomerular filtration rate 58 mL/min/1.73 m2 (IQI:49-71). At surgery, the median final IOPTH was 40 pg/mL (IQI:29-73), and median decrease in IOPTH was 78% (IQI:72-87), with 88% (n = 36) of patients demonstrating >50% decrease. Median calcium level ≥6 mo after surgery was 9.4 mg/dL (IQI:8.8-9.7), and only one patient had recurrent hypercalcemia. Failure to achieve >50% decrease in IOPTH was not significantly associated with recurrent hypercalcemia (P = 1.000). With a median follow-up time of 41 mo (IQI:25-70), only three patients had graft failure. The positive predictive value of IOPTH for cure was 89% (95% confidence interval: 0.752-0.971), with 0% negative predictive value and 87% accuracy (95% confidence interval: 0.726-0.957).
Conclusions:
Subtotal parathyroidectomy is a successful operation with durable cure of THPT. IOPTH fails to predict long-term cure in THPT despite minimally abnormal renal function.
Keywords: Tertiary hyperparathyroidism, Intraoperative parathyroid hormone monitoring, IOPTH, PTH, Parathyroid, Parathyroidectomy
Introduction
Tertiary hyperparathyroidism (THPT) is a rare disorder characterized by the autonomous hypersecretion of parathyroid hormone (PTH).1 Unlike primary hyperparathyroidism (PHPT), in which PTH secretion is driven by intrinsic dysfunction of the parathyroid gland, THPT typically occurs in the context of other physiologic derangements, such as secondary hyperparathyroidism.
Secondary hyperparathyroidism in the surgical population is virtually always a result of chronic renal insufficiency. Elevated serum phosphate levels stimulate PTH secretion, which combined with impaired calcitriol synthesis leads to hypocalcemia.2,3 Persistent hypocalcemia induces hyperparathyroidism by multiple mechanisms: desensitization of the calcium-sensing receptor; development of multigland nodular hypertrophy; and mutations in the proliferating parathyroid cells leading to adenomatous transformation.4-6
In patients with secondary hyperparathyroidism, restoration of normal kidney function by renal allograft can lead to development of THPT in approximately 20%.7-9 While both secondary and THPT are characterized by markedly increased PTH levels, secondary hyperparathyroidism is associated with eucalcemia or hypocalcemia, while THPT patients are hypercalcemic.1 Uncontrolled THPT is associated with increased mortality and impaired renal graft survival.10 Similar to PHPT, parathyroidectomy is the only curative therapy for THPT. Operative treatment options include total parathyroidectomy with autotransplantation or subtotal parathyroidectomy with or without routine thymectomy. At our institution, we routinely perform subtotal parathyroidectomy without thymectomy for THPT.
The extent of parathyroid resection is determined by the operating surgeon. Experienced surgical judgment is required to strike the balance between over-resection–inducing iatrogenic hypoparathyroidism and under-resection leading to recurrence. Visual estimates of the parathyroid remnant lack standardization. Assessment of functional status via intraoperative parathyroid hormone (IOPTH) monitoring is intuitively appealing. The value of IOPTH monitoring is well-established in patients with PHPT.11,12 However, in THPT, the literature is conflicting regarding the utility of IOPTH monitoring.1,13 Several IOPTH thresholds have been proposed to predict curative resection, but no consensus exists.14,15 Therefore, the goal of this study was to examine our institutional experience with parathyroidectomy performed for THPT to determine clinical outcomes with respect to IOPTH monitoring.
Materials and methods
Study population
This study was approved by the Institutional Review Board of the University of Pennsylvania. We identified all patients (n = 43) with THPT who underwent parathyroidectomy at our institution between 1999 and 2017. A diagnosis of THPT was made clinically based on hyperparathyroidism with hypercalcemia or signs of end-organ dysfunction. Two patients were excluded because of incomplete IOPTH data; the final study population consisted of 41 subjects. A retrospective cohort study was performed. Patient data were collected prospectively from the electronic medical record and stored in quality assurance databases. Demographic and clinical variables included age, gender, self-reported race, cause of renal failure, biochemical and imaging data, and surgical pathology. Preoperative serum PTH and calcium levels were reported as the levels obtained at the time of surgical evaluation, regardless of cinacalcet status. Glomerular filtration rate was calculated using the Modification of Diet in Renal Disease Study equation.
Definitions and outcomes
Duration of dialysis was defined as the cumulative time undergoing dialysis prior to renal transplant. Renal graft failure was defined as resumption of dialysis. A decrease of >50% in final IOPTH was defined as operative success. The primary outcome was cure, defined as eucalcemia ≥6 mo after parathyroidectomy. Calcium levels <6 mo after surgery and ≥6 mo after parathyroidectomy were included for analysis. Secondary outcome measures included renal graft failure.
Operative technique
Bilateral exploration and subtotal parathyroidectomy was performed for all patients. A subtotal parathyroidectomy was defined as resection of all parathyroid tissue with preservation of a vascularized remnant of the smallest parathyroid gland. The remnant size was visually estimated to approximate the volume of 2-3 normal parathyroid glands. A portion of excised parathyroid tissue was immediately cryopreserved in the Pathology Department of the Hospital of the University of Pennsylvania, for potential future autotransplant. If IOPTH levels failed to decrease by >50% with subtotal parathyroidectomy, further exploration for ectopic and supernumerary glands was performed, including transcervical thymectomy.
Intraoperative parathyroid hormone monitoring
Intraoperative PTH levels were assessed in serum. Samples were obtained by venipuncture prior to incision and 15 min after subtotal parathyroidectomy. Testing was performed in the clinical laboratories of the Hospital of the University of Pennsylvania on an Immulite 2000 Immunoassay System (Siemens Healthcare, Erlangen, Germany) with chemiluminescent immunoassay detection of intact PTH.
Statistics
Descriptive statistics were performed; group comparisons were performed using the Fisher’s exact test. Continuous variables were reported as mean with standard deviation or median with interquartile interval (IQI; 25th percentile-75th percentile) for normally distributed and nonnormally distributed variables, as appropriate. Statistical analysis was performed using STATA 15.1 (Stata Corporation, College Station, TX). Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated to assess the relationship between IOPTH and cure.
Results
Clinical characteristics
Of 41 patients in the final study population (Table 1), the median age was 55 y old (IQI:49-66); 41% of patients were female (n = 17). The majority of patients were white (66%, n = 27) by self-reported race. Before renal allograft, the median duration of dialysis was 34 mo (IQI:6-60). Four patients had prior renal grafts and underwent a subsequent second transplant. One patient had undergone prior subtotal parathyroidectomy for secondary hyperparathyroidism, with a recurrence in an intrathoracic thymic gland treated with transcervical thymectomy and forearm autograft. He subsequently underwent renal transplant and developed THPT localizing to a cervical gland.
Table 1 –
Characteristics of 41 patients with tertiary hyperparathyroidism.
| Characteristic | n, median |
|---|---|
| Median age, y (IQI) | 55 (49, 66) |
| Female gender (%) | 17 (41) |
| Race | |
| White | 27 (66%) |
| Black | 13 (32%) |
| Asian | 1 (2%) |
| Median duration of dialysis, mo (IQI) | 34 (6, 60) |
| Multiple renal grafts | 5 (12%) |
| Prior parathyroidectomy | 1 (2%) |
| Sequelae of hypercalcemia | |
| Nephrolithiasis | 2 (5%) |
| Bone density loss | 18 (44%) |
| Systemic symptoms | 23 (56%) |
| Median preoperative calcium, mg/dL (IQI) | 10.4 (10, 11.2) |
| Median preoperative PTH, pg/mL (IQI) | 172 (104, 293.3) |
| Median preoperative creatinine, mg/dL (IQI) | 1.2 (0.9, 1.5) |
| Median GFR*, mL/min/1.73 m2 (IQI) | 58 (49, 71) |
GFR = glomerular filtration rate; MDRD = Modification of Diet in Renal Disease.
Calculated by MDRD.
Preoperative median serum calcium levels were elevated at 10.4 mg/dL (IQI:10-11.2). Sequelae of hypercalcemia included nephrolithiasis in 5% (n = 2), bone mineral density loss in 44% (n = 18), and systemic and neurocognitive symptoms in 56% (n = 23). Preoperative median PTH was elevated at 172 pg/mL (IQI:104-293.3). Renal function was minimally impaired with a median glomerular filtration rate of 58 mL/min/173 m2 (IQI:49-71) and median serum creatinine level of 1.2 mg/dL (IQI:0.9-1.5). The median time from transplant to parathyroidectomy was 45 mo (IQI:23-92). The indication for surgery in each of the 41 patients is listed in Table 2.
Table 2 –
Indications for parathyroidectomy and time from transplant for study subjects.
| Subject no. | Time from transplant, mo | Indication for parathyroidectomy |
|---|---|---|
| 1 | 38 | Persistent hypercalcemia |
| 2 | 172 | Nephrolithiasis |
| 3 | 275 | Osteoporosis |
| 4 | 90 | Persistent hypercalcemia |
| 5 | 23 | Persistent hypercalcemia |
| 6 | 69 | Osteoporosis |
| 7 | 431 | Persistent hypercalcemia, osteoporosis |
| 8 | 97 | Persistent hypercalcemia |
| 9 | 27 | Persistent hypercalcemia, osteoporosis |
| 10 | 39 | Persistent hypercalcemia |
| 11 | 165 | Persistent hypercalcemia, fragility fractures |
| 12 | 14 | Persistent hypercalcemia |
| 13 | 6 | Persistent hypercalcemia, renal graft impairment |
| 14 | 92 | Persistent hypercalcemia |
| 15 | 41 | Persistent hypercalcemia |
| 16 | 110 | Persistent hypercalcemia |
| 17 | 97 | Osteoporosis, fragility fractures |
| 18 | 56 | Osteoporosis |
| 19 | 3 | Persistent severe hypercalcemia |
| 20 | 57 | Persistent hypercalcemia |
| 21 | 22 | Persistent hypercalcemia |
| 22 | 138 | Persistent hypercalcemia |
| 23 | 19 | Nephrolithiasis |
| 24 | 1230 | Persistent hypercalcemia, nephrolithiasis |
| 25 | 73 | Persistent hypercalcemia |
| 26 | 29 | Osteoporosis |
| 27 | 19 | Persistent hypercalcemia |
| 28 | 3 | Persistent severe hypercalcemia |
| 29 | 36 | Persistent hypercalcemia |
| 30 | 61 | Persistent hypercalcemia |
| 31 | 68 | Persistent hypercalcemia, concomitant thyroid cancer |
| 32 | 72 | Persistent hypercalcemia, renal graft impairment |
| 33 | 44 | Persistent hypercalcemia |
| 34 | 6 | Persistent hypercalcemia, osteoporosis |
| 35 | 12 | Persistent hypercalcemia |
| 36 | 89 | Persistent hypercalcemia, osteoporosis |
| 37 | 123 | Persistent hypercalcemia |
| 38 | 44 | Persistent hypercalcemia, brown tumor of bone |
| 39 | 10 | Persistent hypercalcemia |
| 40 | 45 | Persistent severe hypercalcemia |
| 41 | 32 | Persistent hypercalcemia, osteoporosis |
Operative findings
Subtotal parathyroidectomy was performed for all patients. At the time of surgery, 12% of patients (n = 5) were found to have ectopic glands (Table 3). Thymectomy was performed for two patients. The median percent decrease in IOPTH was 78% (IQI:72-87). Eighty-eight percent (n = 36) of patients demonstrated a >50% drop in PTH after subtotal parathyroidectomy. Median final IOPTH was 40 pg/mL (IQI:29-73), within normal range. On final surgical pathology, the median size of the dominant gland was enlarged at 18 mm (IQI:12-24) with a median mass of 496 mg (IQI:148-970).
Table 3 –
Operative findings in patients undergoing parathyroidectomy for tertiary hyperparathyroidism.
| Characteristic | n, median |
|---|---|
| Dominant gland | |
| Median size, mm (IQI) | 18 (12,24) |
| Median mass, mg (IQI) | 496 (148, 970) |
| Ectopic gland | 5 (12%) |
| IOPTH | |
| Median final IOPTH, pg/mL (IQI) | 40 (29, 73) |
| Median percent decrease in IOPTH (IQI) | 78 (72, 87) |
| IOPTH decrease ≥50% | 36 (88%) |
Clinical outcomes
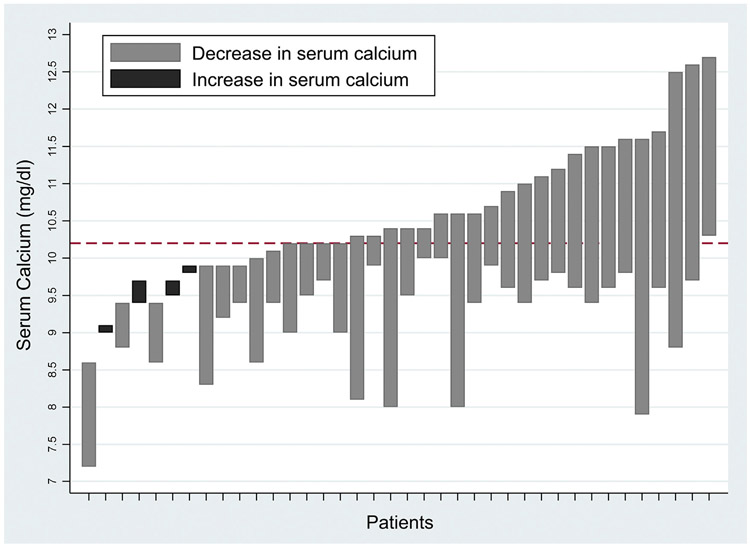
On short-term postoperative follow-up, median serum calcium levels were normal at 9.5 mg/dL (IQI:8.7-9.8), with PTH minimally elevated at 70.5 pg/mL (IQI:47-98.7) (Table 4). At ≥6 mo after parathyroidectomy, the median serum calcium level remained normal at 9.4 mg/dL (IQI:8.8-9.7), while PTH levels slightly increased to 78.3 pg/mL (IQI:50-118), respectively. Preoperative and postoperative calcium levels are shown in Figure. The median duration of follow-up was 40.5 mo (IQI:25-70). At the time of last follow-up, the median renal graft survival was 104 mo (IQI:73-182). Graft failure was observed in three patients; these patients did not have recurrence of hyperparathyroidism. One patient was hypercalcemic at last follow-up, consistent with recurrence. Ninety-eight percent of patients remained eucalcemic at last follow-up. Failure to achieve >50% decrease in IOPTH was not significantly associated with recurrent hypercalcemia (P = 1.000).
Table 4 –
Clinical outcomes after parathyroidectomy for tertiary hyperparathyroidism.
| Characteristic | n, median |
|---|---|
| Median calcium levels, mg/dL | |
| <6 mo postoperatively (IQI) | 9.5 (8.7, 9.8) |
| ≥6 mo postoperatively (IQI) | 9.4 (8.8, 9.7) |
| Median PTH levels, pg/mL | |
| <6 mo postoperatively (IQI) | 70.5 (47, 98.7) |
| ≥6 mo postoperatively (IQI) | 78.3 (50, 118) |
| Median duration of follow-up, mo (IQI) | 40.5 (25, 70) |
| Hypercalcemia at last follow-up | 1 (2%) |
| Median graft survival, mo (IQI) | 104 (73, 182) |
| Graft failure | 3 (7.3%) |
Fig –
Serum calcium levels preparathyroidectomy and postparathyroidectomy for primary hyperparathyroidism. Bar denotes change in serum calcium level, dotted horizontal line denotes upper limit of normal serum calcium range (10.2 mg/dL). For subjects indicated in light gray, the top of the bar indicates the preoperative calcium level and the bottom of the bar indicates the postoperative calcium level. In four subjects (indicated in dark gray) treated with cinacalcet before surgery, the preoperative calcium was lower than the postoperative; the top of the bar indicates the postoperative calcium level and the bottom of the bar indicates the preoperative serum calcium level.
Six subjects did not have all four parathyroid glands identified at the time of surgery. In five subjects, the IOPTH decreased more than 50% after resection of fewer than 3.5 glands. All of these subjects were eucalcemic more than 6 mo after surgery. In one subject, the fourth gland was never found despite extensive exploration, jugular venous sampling, and intraoperative ultrasound. Although IOPTH decreased by 56% after resection of three glands and postoperatively she was eucalcemic (latest calcium 10.0 mg/dL), PTH remained consistently elevated.
To evaluate the relationship between operative success and cure, we assessed the performance characteristics of four published IOPTH criterion for secondary and THPT (Table 5). The standard Miami criteria of a >50% decrease in IOPTH demonstrated an 89% sensitivity for predicting eucalcemia long-term, with 0% specificity, 97% PPV, 0% NPV, and 87% accuracy. To determine whether other criterion performed differently, we compared three other IOPTH thresholds. A >50% decrease in IOPTH and into the normal range was 66% sensitive and 0% specific, with 96% PPV, 0% NPV, and 64% accuracy. A final IOPTH of <200 pg/mL was the most sensitive, with 92% sensitivity, 0% specificity, 97% PPV, 0% NPV, and 90% accuracy. The more stringent criteria of a final IOPTH <60 pg/mL was 68% sensitive and 0% specific, with 96% PPV, 0% NPV and 67% accuracy. All four criteria were nonspecific and failed to accurately predict cure after parathyroidectomy for THPT.
Table 5 –
Comparison of performance of published IOPTH criteria for secondary and tertiary hyperparathyroidism in prediction for eucalcemia ≥6 mo postoperatively.
| IOPTH criteria | Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | Accuracy (95% CI) |
|---|---|---|---|---|---|
| >50% decrease | 89% (0.752-0.971) | 0% (0-0.975) | 97% (0.968-0.974) | 0% | 87% (0.726-0.957) |
| >50% decrease and into normal range | 66% (0.520-0.830) | 0% (0-0.975) | 96% (0.952-0.969) | 0% | 64% (0.472-0.788) |
| <200 pg/mL | 92% (0.786-0.983) | 0% (0-0.975) | 97% (0.970-0.975) | 0% | 90% (0.758-0.971) |
| <60 pg/mL | 68% (0.514-0.825) | 0% (0-0.975) | 96% (0.954-0.970) | 0% | 67% (0.498-0.809) |
To assess the relationship between final intraoperative PTH level and PTH levels after surgery, we evaluated the performance of PTH guidelines for PHPT (PTH greater than the normal range) and secondary hyperparathyroidism (PTH <300 pg/mL). In our cohort, 21 subjects had PTH above the normal range at long-term follow-up. Of these, only one subject was hypercalcemic (calcium 10.3 mg/dL). Two of the 21 subjects failed to achieve 50% or greater drop in PTH; both of these were normocalcemic. When testing the predictive value of an IOPTH decrease of less than 50% for persistently elevated PTH level at long-term follow-up, the sensitivity was 9.5% (95% confidence interval [CI]:1.2%-30.4%) with specificity 92.3% (95% CI:64.0%-99.8%), PPV 66.7% (95% CI:16.7%-95.2%), and NPV 41.2% (95% CI:24.7%-59.3%).
In our cohort, two subjects had PTH greater than 300 pg/mL; both of these were normocalcemic. One of these subjects failed to achieve a 50% or greater drop in PTH. When testing the predictive value of an IOPTH decrease of less than 50% for PTH level greater than 300 pg/mL at long-term follow-up, the sensitivity was 50.0% (95% CI:1.3%-98.7%) with specificity 93.6% (95% CI: 78.6%-99.2%), PPV 33.3% (95% CI:6.8%-77.5%), and NPV 96.7% (95% CI:87.9%-99.2%).
Elevated final IOPTH was not an accurate predictor of PTH above the normal range at follow-up; however, it was a reasonable predictor of PTH greater than 300 pg/mL. None of the subjects who had IOPTH decreases of less than 50% were both hyperparathyroid (either above the normal range or above 300 pg/mL) and hypercalcemic, and therefore none would have clear indications for additional surgery.
Discussion
In this study, we examined our institutional experience with parathyroidectomy for THPT. We found that parathyroidectomy achieved durable eucalcemia in 98% of patients. This high success rate is similar to other published surgical series of THPT, in which rates of normocalcemia range from 94% to 100% after parathyroidectomy.16 Although published techniques of parathyroidectomy vary, results appear to be independent of operative strategy. Our institutional practice is to perform subtotal parathyroidectomy; cryopreservation at the time of surgery allows us to perform maximal tissue resection without concern for inducing permanent hypoparathyroidism. As incomplete parathyroidectomy is associated with recurrence of THPT,17 our practice has been to leave a minimal remnant, as well as having a high index of suspicion for ectopic and supernumerary glands.
In our analysis, an IOPTH decrease of 50% failed to accurately predict cure despite minimally abnormal renal function. Although final IOPTH levels did not meet our criteria in 12% of patients, hypercalcemia was effectively treated by parathyroidectomy, suggesting that hormonal kinetics may differ from those in PHPT. Several other studies have similarly noted delayed PTH clearance in the THPT population.18 The etiology of this is unclear but may be a result of higher initial PTH levels or delayed renal clearance of PTH despite a functioning renal allograft. Given the high incidence of supernumerary glands in the secondary and presumably tertiary hyperparathyroid population, persistently elevated IOPTH may also indicate the presence of additional abnormal parathyroid tissue.19,20 However, all four published IOPTH criteria for secondary and THPT evaluated in this study performed similarly, with very low specificity for recurrent hypercalcemia. Interpretation of IOPTH levels in THPT therefore must be incorporated with surgical judgment given the low accuracy for eucalcemia.
In our patient population, recurrent hyperparathyroidism was not associated with graft failure. However, owing to the small size of this study, we were substantially underpowered to detect a difference in graft survival, and therefore this observation is difficult to interpret. The relationship between renal allograft failure and PTH is incompletely delineated. In secondary hyperparathyroidism, it is well-established that elevated pretransplant PTH levels increase the risk of graft loss in subsequent transplant.21 Therefore maintenance of PTH <300 pg/mL is recommended by the National Kidney Disease Outcomes Quality Initiative guidelines for patients with chronic renal disease.22 In THPT, however, published literature is conflicting. Some studies suggest that posttransplant hypercalcemia may be associated with impaired graft survival and all-cause mortality.10,23 However, no mechanism mediating either allograft loss or mortality has been demonstrated, and these studies were associative rather than causal. Other studies have shown no correlation between either parathyroidectomy and graft survival24,25 or hyperparathyroidism and graft survival26 in the posttransplant population, suggesting that this relationship is still incompletely understood.
Given the dearth of data in this area, many opportunities for future research exist. Establishment of the operative benefits of parathyroidectomy in the tertiary hyperparathyroid population would be of immediate clinical utility to patients and clinicians struggling with decision-making in medically complex settings. Such data would inform indications for parathyroidectomy and could be used as a foundation for management guidelines in THPT. Study of PTH kinetics in this patient population could contribute to the development of IOPTH criterion which better predict clinical outcomes; in this small study, we were unable to identify IOPTH criteria which performed well. Additional research in these promising areas is needed.
Conclusion
Subtotal parathyroidectomy is a successful operation with durable cure of THPT. In our tertiary hyperparathyroid population, IOPTH failed to predict long-term eucalcemia despite minimally abnormal renal function. Although IOPTH is a useful tool to guide the extent of resection in parathyroidectomy, expert surgical judgment is required for optimal operative outcomes.
Acknowledgment
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Meeting Presentation: Academic Surgical Congress, Houston, TX, February 2019.
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
REFERENCES
- 1.Shindo M, Lee JA, Lubitz CC, et al. The changing landscape of primary, secondary, and tertiary hyperparathyroidism: highlights from the American College of surgeons panel, “What’s new for the surgeon caring for patients with hyperparathyroidism”. J Am Coll Surg. 2016;222:1240–1250. [DOI] [PubMed] [Google Scholar]
- 2.Hruska KA, Mathew S, Lund R, Qiu P, Pratt R. Hyperphosphatemia of chronic kidney disease. Kidney Int. 2008;74:148–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tominaga Y, Johansson H, Johansson H, Takagi H. Secondary hyperparathyroidism: pathophysiology, Histopathology, and medical and surgical management. Surg Today. 1997;27:787–792. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham J, Locatelli F, Rodriguez M. Secondary hyperparathyroidism: pathogenesis, disease progression, and therapeutic options. Clin J Am Soc Nephrol. 2011;6:913–921. [DOI] [PubMed] [Google Scholar]
- 5.Fukuda N, Tanaka H, Tominaga Y, Fukagawa M, Kurokawa K, Seino Y. Decreased 1,25-dihydroxyvitamin D3 receptor density is associated with a more severe form of parathyroid hyperplasia in chronic uremic patients. J Clin Invest. 1993;92:1436–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hedinger MKaC pathologic study of parathyroid glands in tertiary hyperparathyroidism. Hum Pathol. 1985;16:772–784. [DOI] [PubMed] [Google Scholar]
- 7.Baliski C, Nosyk B, Melck A, Bugis S, Rosenberg F, H Anis A, et al. The cost-effectiveness of three strategies for the surgical treatment of symptomatic primary hyperparathyroidism. Ann Surg Oncol. 2008;15:2653–2660. [DOI] [PubMed] [Google Scholar]
- 8.Park JH, Kang SW, Jeong JJ, Nam K-H, Chang HS, Chung WY, Park CS. Surgical treatment of tertiary hyperparathyroidism after renal transplantation: a 31-year experience in a single institution. Endocr J. 2011;58:827–833. [DOI] [PubMed] [Google Scholar]
- 9.Evenepoel P, Claes K, Kuypers D, Maes B, Bammens B, Vanrenterghem Y. Natural history of parathyroid function and calcium metabolism after kidney transplantation: a single-centre study. Nephrol Dial Transplant. 2004;19:1281–1287. [DOI] [PubMed] [Google Scholar]
- 10.Pihlstrom H, Dahle DO, Mjoen G, et al. Increased risk of all-cause mortality and renal graft loss in stable renal transplant recipients with hyperparathyroidism. Transplantation. 2015;99:351–359. [DOI] [PubMed] [Google Scholar]
- 11.Inabnet WB 3rd, Dakin GF, Haber RS, Rubino F, Diamond EJ, Gagner M. Targeted parathyroidectomy in the era of intraoperative parathormone monitoring. World J Surg. 2002;26:921–925. [DOI] [PubMed] [Google Scholar]
- 12.Carneiro DM, Irvin GL 3rd. New point-of-care intraoperative parathyroid hormone assay for intraoperative guidance in parathyroidectomy. World J Surg. 2002;26:1074–1077. [DOI] [PubMed] [Google Scholar]
- 13.Pitt SC, Panneerselvan R, Chen H, Sippel RS. Secondary and tertiary hyperparathyroidism: the utility of ioPTH monitoring. World J Surg. 2010;34:1343–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma J, Weber C. Early versus late parathyroidectomy for tertiary (posttransplant) hyperparathyroidism. Difficult Decisions Endocr Surg. 2018;7:209–216. [Google Scholar]
- 15.Milas M, Weber CJ. Near-total parathyroidectomy is beneficial for patients with secondary and tertiary hyperparathyroidism. Surgery. 2004;136:1252–1260. [DOI] [PubMed] [Google Scholar]
- 16.Tang JA, Friedman J, Hwang MS, Salapatas AM, Bonzelaar LB, Friedman M. Parathyroidectomy for tertiary hyperparathyroidism: a systematic review. Am J Otolaryngol. 2017;38:630–635. [DOI] [PubMed] [Google Scholar]
- 17.Kebebew E, Duh QY, Clark OH. Tertiary hyperparathyroidism: Histologic patterns of disease and results of parathyroidectomy. Arch Surg. 2004;139:974–977. [DOI] [PubMed] [Google Scholar]
- 18.Haustein SV, Mack E, Starling JR, Chen H. The role of intraoperative parathyroid hormone testing in patients with tertiary hyperparathyroidism after renal transplantation. Surgery. 2005;138:1066–1071 [discussion 1071]. [DOI] [PubMed] [Google Scholar]
- 19.Andrade JS, Mangussi-Gomes JP, Rocha LA, et al. Localization of ectopic and supernumerary parathyroid glands in patients with secondary and tertiary hyperparathyroidism: surgical description and correlation with preoperative ultrasonography and Tc99m-Sestamibi scintigraphy. Braz J Otorhinolaryngol. 2014;80:29–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schneider R, Waldmann J, Ramaswamy A, Fernandez ED, Bartsch DK, Schlosser K. Frequency of ectopic and supernumerary intrathymic parathyroid glands in patients with renal hyperparathyroidism: analysis of 461 patients undergoing initial parathyroidectomy with bilateral cervical thymectomy. World J Surg. 2011;35:1260–1265. [DOI] [PubMed] [Google Scholar]
- 21.Roodnat JI, van Gurp EA, Mulder PG, et al. High pretransplant parathyroid hormone levels increase the risk for graft failure after renal transplantation. Transplantation. 2006;82:362–367. [DOI] [PubMed] [Google Scholar]
- 22.Patel TV, Singh AK. Kidney disease outcomes quality initiative guidelines for bone and mineral metabolism: emerging questions. Semin Nephrol. 2009;29:105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Araujo M, Ramalho JAM, Elias RM, et al. Persistent hyperparathyroidism as a risk factor for long-term graft failure: the need to discuss indication for parathyroidectomy. Surgery. 2018;163:1144–1150. [DOI] [PubMed] [Google Scholar]
- 24.Lou I, Schneider DF, Leverson G, Foley D, Sippel R, Chen H. Parathyroidectomy is underused in patients with tertiary hyperparathyroidism after renal transplantation. Surgery. 2016;159:172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kerby JD, Rue LW, Blair H, Hudson S, Sellers MT, Diethelm AG. Operative treatment of tertiary hyperparathyroidism: a single-center experience. Ann Surg. 1998;227:878–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baia LC, Humalda JK, Vervloet MG, Navis G, Bakker SJ, de Borst MH. Fibroblast growth factor 23 and cardiovascular mortality after kidney transplantation. Clin J Am Soc Nephrol. 2013;8:1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]