Abstract
Eating disorders (EDs) are more common among younger women compared to older women and in women compared to men. As such, most ED research focuses on late adolescent and young adult females resulting in limited prospective research on gender differences in eating disorder psychopathology across the lifespan. The present study addresses this gap by examining gender differences in ED diagnoses, eating pathology, and the impact of putative risk factors on eating pathology in women (n = 624) and men (n = 276) over a 30-year period from late adolescence (Mean(SD) = 20[2] years) to later mid-life (Mean(SD) = 50[2] years). Four assessment waves were conducted, beginning with baseline participation during college and subsequent 10-, 20-, and 30-year follow-up. Retention at 30-year follow-up was 72% (n = 440) for women and 67% (n = 181) for men. Prevalence of DSM-5 ED diagnoses decreased over the 30-year span for women and remained stable for men, with no significant gender difference in point prevalence by age 50. Drive for thinness decreased for women through age 50 and increased for men, while bulimic symptoms decreased as both genders aged. Multilevel models demonstrated that the impact of dieting as a risk factor on drive for thinness decreased prospectively as men aged and remained stable as women aged. Results imply that current risk models require refinement to account for developmental trajectories in which dramatic gender differences observed in late adolescence diminish over time.
Keywords: eating disorders, gender differences, longitudinal study, prevalence, lifespan
Research supports that eating disorders (EDs) are more prevalent in females compared to males during adolescence and young adulthood (Hudson, Hiripi, Pope, & Kessler, 2007), however, it is unclear whether these patterns of gender differences persist into mid-life. While evidence suggests that a substantial proportion of women age out of EDs (Keel & Brown, 2010), most studies have relied on cross-sectional (e.g., Hudson et al., 2007; Udo & Grilo, 2018) or clinical samples (e.g., Eddy et al., 2017) and few include men. Epidemiological data suggest that EDs are increasing in women and men over age 45 (Mitchison, Hay, Slewa-Younan, & Mond, 2014). This pattern underscores the importance of prospective data in understanding the natural course of eating pathology between genders, as previous cross-sectional samples may reflect cohort effects. Greater understanding of gender differences in developmental trajectories can inform etiological models and identify at-risk populations across the lifespan. Thus, the current study sought to compare gender differences in the natural course of EDs, eating pathology, and the impact of ED risk factors on eating pathology from late adolescence (20s) through mid-life (50s) in a nonclinical sample of women and men, building upon our previous work (Keel, Baxter, Heatherton, & Joiner Jr, 2007; Keel, Gravener, Joiner, & Haedt, 2010).
The Course of Eating Disorder Diagnoses from Adolescence to Mid-Life
EDs most often onset in females during adolescence and young adulthood, and decrease in the transition from adulthood to mid-life (Keel et al., 2010). Cross-sectional data support that older women are significantly less likely to develop or currently experience an ED compared to younger women (Hudson et al., 2007; Preti et al., 2009). This pattern is consistent with the hypothesis that women age out of their EDs. However, recent research suggests that EDs in mid-life may be more common than previously thought (Mangweth-Matzek et al., 2014; Micali et al., 2017). Problematically, the studies of mid- to late-adulthood conducted to date are confounded by cohort effects, as the large majority of women in these studies were born and entered adulthood before the observed increase in ED incidence in Western cultures around the 1970s to 1990s (Keel & Klump, 2003). Thus, research is needed to confirm that epidemiological patterns reflect developmental effects, rather than cohort effects.
More limited epidemiological data exist on patterns of EDs in men, though research consistently suggests that EDs are less common in this group (Hudson et al., 2007; Udo & Grilo, 2018). Research examining men is often cross-sectional (Mangweth-Matzek, Kummer, & Pope, 2016) and/or collapses across age groups (Hay, Girosi, & Mond, 2015), making it difficult to infer changes associated with aging. Existing prospective studies including males and comparing gender differences are often limited to young adulthood (Liechty & Lee, 2013), limiting generalizability to mid-life adults. Importantly, recent data suggest that men may have a later age of ED onset than women (Mitchison & Mond, 2015). Such findings underscore the importance of examining men as well as gender differences in later life as these may impact understanding of how risk factors for EDs change over the lifespan.
Data implicating the role of ovarian hormones in the development of eating pathology (Klump, Culbert, & Sisk, 2017) and the rarity of ED onset before puberty and after menopause suggest that age and the hormonal environment play an important role in the etiology of EDs in females. Consequently, changes occurring for women in later mid-life may dramatically decrease gender differences in eating pathology. While no study to date has prospectively and formally examined gender differences in DSM-5 ED diagnoses from late adolescence to later mid-life, our group (Keel et al., 2010) examined prospective changes in DSM-III-R diagnoses of bulimia nervosa (BN) and related EDNOS cross-sectionally at ages 20, 30, and 40 in women and men. Bulimic syndrome point prevalence declined significantly in women, but remained stable in men, from late adolescence to early mid-life, supporting that gender differences in prevalence in late adolescence are decreased in adulthood at 30 and 40 years of age. However, at approximately 40 years of age, women were still significantly more likely to have a current ED compared to men (Keel et al., 2010). Cross-sectional research supports that women demonstrate higher ED point prevalence compared to men between ages 18–29 (women = 3.6%, men = 0.7%), but gender differences in point prevalence disappear in those over age 45 (women = 2.3%, men = 2.5%; Hudson et al., 2007). These results support the need to prospectively evaluate gender differences in ED trajectory into later mid-life.
The Course of Disordered Eating Attitudes and Behaviors
In addition to the need for understanding gender differences in the course of EDs, it is important to examine gender differences in the course of disordered eating attitudes and behaviors dimensionally. Dimensional approaches may provide more accurate reflection of underlying pathophysiology and tend to demonstrate greater sensitivity and reliability compared to categorical assessments (Brown & Barlow, 2005; Helzer, Kraemer, & Krueger, 2006; Luo, Donnellan, Burt, & Klump, 2016). In our previous description of a 20-year longitudinal study of women and men from their 20s to their 40s, women demonstrated higher drive for thinness and bulimia scores across time compared to men (Keel et al., 2007). Importantly, there were also gender differences in the trajectory of eating pathology over time; drive for thinness decreased over time for women and increased over time for men, while bulimia scores decreased over time for both genders (Keel et al., 2007). These results are relatively consistent with recent epidemiological data from Project EAT supporting declines for females and increases for males in unhealthy weight control behaviors from adolescence to adulthood, with unhealthy behaviors being more common for women across time (Neumark-Sztainer et al., 2018). Continued examination of gender differences in eating pathology during the transition from 40 to 50 may be particularly important given the hypothesized role of ovarian hormones in eating pathology (Klump et al., 2014), the hormonal changes associated with menopause (Rannevik et al., 1995), and the weight gain associated with aging for both women and men (Guo, Zeller, Chumlea, & Siervogel, 1999). While the hormonal changes associated with menopause for women should reduce risk for EDs, age-related weight gain for both genders may increase body image and eating concerns.
The Differential Impact of Eating Disorder Risk Factors over Time between Genders
Previous research from our group supports that ED risk factors (weight, weight perception, and dieting) may differ between genders over time (Keel et al., 2007). Although BMI increased significantly as both men and women aged, both weight perception and dieting frequency decreased in women while increasing in men as the cohort transitioned from their 20’s to their 40’s. These results for men are consistent with research from Project EAT supporting that high frequency dieting (i.e., 5+ times/year) increased in a cohort of men, but not women, from adolescence to adulthood (Haynos et al., 2018). Changes in levels of risk factors may further explain changes in eating pathology. It is also important to understand if the impact of those risk factors changes between genders as individuals age (Slevec & Tiggemann, 2011). For example, the impact of a particular risk factor may remain stable (e.g., the impact of BMI on eating pathology remains the same across time) or alternatively, the impact of the risk factor may change over time (e.g., the impact of BMI on eating pathology becomes weaker/stronger over time). Similarly, the trajectory of the impact of risk factors on eating pathology may differ between genders.
Regarding the impact of weight on eating pathology, higher body mass index (BMI) has been associated with increased body dissatisfaction and eating pathology cross-sectionally from adolescence to midlife for women (Slevec & Tiggemann, 2011; Stice, 2002) and men (Keel et al., 2007; Lavender, De Young, & Anderson, 2010; Patrick & Stahl, 2009). Prospective data from Project EAT suggest that dieting and unhealthy weight control behaviors track with trajectories of both rapid and gradual weight gain from adolescent to adulthood for both females and males (Goldschmidt et al., 2018). However, one study found that BMI was a significant predictor of increased drive for thinness in women at younger ages (25–35), but not at older ages (over 65; Pruis & Janowsky, 2010). Thus, the potency of BMI as a risk factor for eating pathology may decrease for women as they age, but it is unclear if this would be true for men. The importance of weight perception in affecting eating pathology may also differ between genders over time. As men and women age, they develop additional roles and responsibilities that affect their self-worth outside of body image and body perception (e.g., marriage, parenthood, career; Halliwell & Dittmar, 2003; Keel et al., 2007). Onset of these adult life roles has been associated with decreases in eating pathology in women, but not men (Keel et al., 2007). Thus, over time, weight perception may have a decreasing impact on eating pathology for women, but not men. Finally, the impact of dieting on eating pathology may decrease over time across genders, as dieting in older ages may reflect a more normative response to weight gain or medical conditions versus pursuit of an aesthetic ideal linked to EDs. While our group (Keel et al., 2007) previously examined how these putative risk factors (BMI, weight perception, dieting) impact eating pathology over time in women and men separately, we did not conduct a formal statistical test of gender as a moderator of associations between risk factors and disordered eating over time. Additionally, the final assessment wave occurred before the majority of women would have entered menopause, which may trigger dramatic changes in gender differences.
Aims of the Present Study
The present study had two aims. First, we sought to describe the point prevalence of DSM-5 ED diagnoses (Aim 1a) and the developmental course of eating pathology (Aim 1b) in a community-based sample of women and men from their 20s to their 50s. This extends our prior findings with this cohort by examining DSM-5 versus DSM-III-R diagnoses derived via survey data (Keel et al., 2010; Keel, Heatherton, Dorer, Joiner, & Zalta, 2006) and by adding the transition of participants as they moved from early mid-life (Keel et al., 2006) to later mid-life. Based on previous research (Hudson et al., 2007; Keel et al., 2010), we hypothesized that point prevalence estimates would decrease in women from late adolescence to later mid-life and remain stable in men. Regarding eating pathology, we hypothesized that drive for thinness would decrease for women and increase for men as they aged, while bulimic symptoms would decrease for both genders. For our second aim, we sought to determine the relative impact of risk factors on eating pathology across age between genders (Aim 2). Our first question was, does the influence of BMI, weight perception, and dieting frequency differ between women and men? We hypothesized that weight perception and dieting frequency, but not BMI, would have a greater impact on eating pathology in women compared to men. Our second question was, does the influence of these risk factors on eating pathology change across age? We hypothesized that collapsing across gender, BMI, weight perception, and dieting frequency would have a decreasing impact on eating pathology as people aged. Our final question was, does the change in influence of these risk factors differ between women and men as they age? We hypothesized that: (1) BMI would exhibit decreasing impact on eating pathology for women as they age; (2) the impact of weight perception on eating pathology would decrease in women as they age, and remain stable for men; and (3) dieting would have a decreasing impact on eating pathology for both genders as they age. Results will contribute to our understanding of ED etiology and the influence of risk factors from late adolescence to mid-life in order to inform prevention and intervention efforts.
Methods
Participants
Participants for the present study were N = 900 college students (n = 624 women, n = 276 men) at a prestigious northeastern university in 1982. The average age at 30-year follow-up in 2012 was 50.53 (±2.06) years. The racial and ethnic breakdown of the sample was as follows: 81.4% Caucasian, non-Hispanic, 8.6% Asian, 5.1% African American, 4.6% Hispanic, and 0.2% Other.
Procedure
Baseline data were collected in the spring of 1982, during which participants were randomly sampled from the freshman and senior classes of the university. The baseline participation rate for the study was strong for both women (n = 624 [78%]) and men (n = 276 [69%]). Participants were followed at 10-year intervals, resulting in 10-, 20-, and 30-year follow-up data. Surveys at all waves of data collection were mailed up to three times. In 2002 and 2012, participants were also provided the option of completing surveys online. No differences were observed on psychometric properties between paper and online surveys in 2002 (Keel et al., 2006). Participation rates were strong at 10- (women: 82%; men: 76%) and 20-year follow-up (women: 75%; men: 70%; Heatherton, Mahamedi, Striepe, Field, & Keel, 1997; Keel et al., 2007). All study procedures were approved by the Institutional Review Board.
In the spring of 2012, we attempted to contact each individual who participated in the baseline survey who was not deceased. At the time of 30-year follow-up, 15 participants (9 women, 6 men) were deceased. One of the deceased individuals had an ED at baseline and 10-year follow-up, as determined by their survey responses. Of those still living, 72% of women (N = 440) and 67% of men (N = 181) participated at 30-year follow-up.
Measures
As noted previously (Heatherton et al., 1997; Keel et al., 2007), the same questions were included in surveys at each wave of data collection. Therefore, we were able to assess the variables described below through 30-year follow-up.
Body Weight
Participants’ self-reported current height and weight were used to calculate body mass index (BMI; kg/m2). Self-reported height between baseline and 30-year follow-up demonstrated high stability (r[606] = .95, p <.001), and rank ordering for self-reported weight status demonstrated a significant association across time (Spearman’s r[602] = .38, p <.001). These findings support the validity of using self-reported height and weight in large, geographically diverse samples where direct assessment is not feasible (Burton, Brown, & Dobson, 2010).
Weight Perception
Weight perception was assessed through a single item asking participants to describe their current weight using one of five response options (“Very Underweight,” “Underweight,” “Average,” “Overweight,” and “Very Overweight”). Previous research supports the use of single-item measures of weight perception (Dorsey, Eberhardt, & Ogden, 2009).
Dieting Frequency
Dieting frequency was measured using a single item that asked participants to rate how often they are currently dieting, with four response options (“Never,” “Rarely,” “Sometimes,” and “Often”). Single-item assessments of dieting behavior have demonstrated similar associations to multi-item measures of dietary restraint (Neumark-Sztainer, Jeffery, & French, 1997). Importantly, self-report measures of dieting may be a better measure of intention to diet rather than actual dieting behaviors (Stice, Fisher, & Lowe, 2004).
Eating Disorder Inventory (EDI; Garner, Olmstead, & Polivy, 1983)
Eating pathology was assessed using the Drive for Thinness (DT) and Bulimia subscales from the EDI available at the inception of the study in 1982. Measurement invariance for the EDI across gender and age groups through age 40 was previously demonstrated in this cohort (Keel et al., 2007) and the current study sought to extend these results through age 50. In the present sample, both subscale scores discriminated between individuals who did and did not meet criteria for an ED at all time points (all p-values <.001). The internal consistency of the DT subscale within the present study ranged from α=.87-.90 for women and α=.83-.88 for men over time, and the internal consistency of the Bulimia subscale was between α=.80-.86 for women and α=.72-.77 for men.
Eating Disorder Diagnoses
To determine current ED diagnostic status, we used survey-based diagnostic algorithms, following methods used by Keel and colleagues (2006) who had applied DSM-III-R criteria (e.g., BN diagnoses included a) current self-reported binge eating twice or more per week, b) loss of control during binge episodes, c) self-induced vomiting, fasting, diet pills, laxatives, and/or diuretics once or more per week, and d) overconcern with weight/shape.) Previous data from this cohort supports the sensitivity, specificity, and kappa agreement between diagnoses based on survey algorithms and diagnoses based on structured clinical interview (Keel et al., 2010). Algorithms for anorexia nervosa (AN), BN, binge eating disorder (BED) were updated to reflect changes in the diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5; APA, 2013). We also determined the point prevalence of DSM-5 Other Specified Feeding or Eating Disorder (OSFED) presentations. Given that DSM-5 does not specific a diagnostic hierarchy for OSFED, we determined OSFED presentations as follows: atypical AN only (AAN), subthreshold BN only, subthreshold BED only, purging disorder only (PD), and mixed OSFED (having symptoms of multiple OSFED categories).
Data Analyses
Data were determined to be not missing completely at random and were imputed in SPSS 24.0 using expectation-maximization (EM) to prevent biases due to attrition (Schafer & Graham, 2002) and consistent with our prior research (Keel et al., 2007). Missing values were not imputed for nonparametric analyses, including ED diagnosis.
Aim 1: Eating Disorder Diagnoses and Eating Disorder Attitudes and Behaviors between Genders across Time and Age
To address Aim 1a, chi-square analyses compared ED point prevalence estimates between genders. McNemar chi-square tests compared point prevalence estimates within gender across timepoints.
Aim 1b requires that our measures of eating disorder attitudes and behaviors assess the same construct between genders and across age. Thus, prior to conducting analyses for Aim 1b, we evaluated factor invariance for the EDI between genders through age 50. We compared models in which factor loadings were allowed to vary between gender/age (unconstrained models) with models in which factor loadings were constrained to be equal between gender/age groups (constrained models), using the lavaan package in R (Rosseel, 2012).
To test hypotheses for Aim 1b, multilevel models were run using the Mixed Models module of the Statistical Package for the Social Sciences (IBM SPSS, Version 25) to examine changes in eating pathology (EDI DT and EDI Bulimia scores) between genders across age. Within-person changes in eating pathology were modeled at Level 1, and gender and the interaction between gender and age were modeled at Level 2. A linear distribution was specified for dependent variables. A random intercept, random slopes model was fit to the data, such that the intercept for each person and their rate of change across age were allowed to vary. Full information maximum likelihood estimation (FIML) was used (Schafer & Graham, 2002). Predictor variables were grand-mean centered across waves to permit tests of between-person differences in risk factors over time. While we considered within-person centering of predictor variables (Curran & Bauer, 2011), which could result in additional information on how individual trajectories of EDI scores change over time, this approach was beyond the scope of our identified aims. Thus, we chose to use grand-mean centering, as our central research question reflected specific interest in between-person, rather than within-person changes over time. To provide the least restrictive approach, unstructured covariance matrixes were employed across models.
Aim 2: Changes in Putative Risk Factors between Genders over Age 20 to 50
To address Aim 2, separate time-lagged linear mixed effect models were run in SPSS to examine the differential impact of putative risk factors between genders on eating pathology over 30 years. Age and dependent variables (EDI DT, EDI Bulimia) were time-lagged to establish temporal precedence, such that predictor variables at age 20 were aligned with EDI scores at age 30, predictor variables at age 30 were aligned with EDI scores at age 40, and predictor variables at age 40 were aligned with EDI scores at age 50. Within-person changes in eating pathology were modeled at Level 1, and between-person differences in putative risk factors and interactions between risk factors, gender, and age were modeled at Level 2. Comparable to the models described in Aim 1b, random intercept, random slopes models were fit to the data, linear distributions were specified for dependent variables, FIML was used as an estimator, predictors were grand-mean centered, and an unstructured covariance matrix was used. Models were run in a 3-stage approach, such that Model 1 for both DT and Bulimia included main effects and the two-way interactions between risk factors and gender, Model 2 added the two-way interactions between risk factors and age, and Model 3 added the three-way interactions between risk factor, gender, and age (see Table 3). The family-wise error rate for post-hoc comparisons in multilevel models was set at p =.01.
Table 3.
Impact of Putative Risk Factors on Eating Pathology between Genders across Age
| EDI Drive for Thinness | EDI Bulimia | |||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Fixed Effects | γ (SE) | γ (SE) | γ (SE) | γ (SE) | γ (SE) | γ (SE) |
| Intercept (γ00) | 11.59 (0.14)*** | 11.65 (0.15)*** | 11.67 (0.15)*** | 10.41 (0.11)*** | 10.45 (0.11)*** | 10.45 (0.11)*** |
| Age (γ10) | 0.02 (0.01) | 0.01 (0.01) | <0.005 (0.01) | −0.03 (0.01)*** | −0.04 (0.01)*** | −0.04 (0.01)*** |
| Gender | 2.40 (0.32)*** | 2.39 (0.33)*** | 2.35 (0.33)*** | 1.15 (0.24)*** | 1.17 (0.24)*** | 1.13 (0.24)*** |
| BMI | 0.10 (0.04)* | 0.12 (0.04)** | 0.12 (0.04)** | 0.12 (0.03)*** | 0.13 (0.03)*** | 0.13 (0.03)** |
| Weight Perception | 0.80 (0.18)*** | 0.72 (0.18)*** | 0.74 (0.18)*** | 0.53 (0.13)*** | 0.52 (0.13)*** | 0.53 (0.13)** |
| Dieting Frequency | 0.82 (0.10)*** | 0.78 (0.10)*** | 0.80 (0.10)*** | 0.46 (0.07)*** | 0.46 (0.07)*** | 0.47 (0.07)*** |
| Gender X Age | 0.06 (0.02)** | 0.06 (0.02)* | 0.08 (0.03)** | 0.01 (0.01) | 0.01 (0.02) | 0.02 (0.02) |
| BMI X Gender | −0.10 (0.09) | −0.08 (0.09) | −0.10 (0.09) | 0.07 (0.06) | 0.08 (0.06) | 0.06 (0.07) |
| Weight Perception X Gender | 0.46 (0.40) | 0.38 (0.39) | 0.43 (0.40) | 0.18 (0.28) | 0.17 (0.28) | 0.20 (0.28) |
| Dieting Frequency X Gender | 0.19 (0.24) | 0.14 (0.24) | 0.14 (0.24) | −0.01 (0.17) | −0.02 (0.17) | −0.04 (0.16) |
| BMI X Age | <0.005 (<0.005) | <0.005 (<0.005) | <0.005 (<0.005) | <0.005 (<0.005) | ||
| Weight Perception X Age | −0.01 (0.02) | −0.01 (0.02) | 0.02 (0.01) | 0.02 (0.01) | ||
| Dieting Frequency X Age | −0.02 (0.01) | −0.02 (0.01) | −0.01 (0.01) | −0.01 (0.01) | ||
| BMI X Gender X Age | <0.005 (0.01) | <0.005 (<0.005) | ||||
| Weight Perception X Gender X Age | <0.005 (0.04) | <0.005 (0.03) | ||||
| Dieting Frequency X Gender X Age | 0.06 (0.02)** | 0.02 (0.02) | ||||
| Variance | ||||||
| Within-Person | 7.08 (0.43)*** | 6.98 (0.43)*** | 6.99 (0.43)*** | 3.29 (0.21)*** | 3.30 (0.21)*** | 3.31 (0.21)*** |
| Intercept | 12.02 (0.82)*** | 12.30 (0.85)*** | 12.25 (0.85)*** | 6.86 (0.43)*** | 6.89 (0.44)*** | 6.88 (0.44)*** |
| Slope | 0.01 (<0.005)** | 0.01 (<0.005)** | 0.01 (<0.005)** | 0.01 (<0.005)** | <0.005 (<0.005)** | <0.005 (<0.005)** |
Note. EDI=Eating Disorder Inventory.
p < .05
p < .01
p < .001
Results
Participants at 30-year follow-up did not differ from non-participants on gender, baseline BMI, EDI scale scores, dieting frequency, or weight perception (all p-values >.10). However, racial/ethnic minority participants were less likely to participate compared to non-Hispanic White participants at follow-up (non-Hispanic White: 82.01%; Other Race/Ethnicity: 68.33%, χ2[1, n=648] = 11.21, p = .001).1
Eating Disorder Diagnoses between Genders over Time
Table 1 describes changes in DSM-5 ED diagnoses from age 20 to 50. The percentage of women meeting criteria for any ED diagnosis decreased from age 20 to 30 (p <.001) and remained stable from 30 to 50 (p-values >.22), while the percentage of men meeting criteria for any ED diagnosis did not change significantly from age 20 to 50 (all p-values >.13). Women were more likely to have AN, BN, BED, AAN, and PD in their 20s and AAN in their 40s compared to men. Women were also more likely to have any ED from their 20s to their 40s compared to men, but no significant gender differences in ED point prevalence were found at age 50.2 Among participants at 30-year follow-up, 74.8% of women (n=329/440), and 68.5% of men (n=124/276) provided data to determine diagnoses at all four assessment waves. Of these women who had an ED at age 20, 84.3% (n = 59/70) had recovered and 15.7% (n = 11/70) had relapsed at age 50. For men, 83.3% (n = 5/6) had recovered and 16.7% (n = 1/6) had relapsed. Across genders, no cases persisted from age 20 to age 50.
Table 1.
Point Prevalence of DSM-5 Eating Disorders over Time for Women and Men
| AN | BN | BED | AAN | subBN | subBED | PD | Mixed OSFED | Any ED | |
|---|---|---|---|---|---|---|---|---|---|
| Age | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) | n(%) |
| Women | |||||||||
| 20s | 12(1.9)* | 52(8.3)* | 25(4.0)* | 19(3.0)* | 2(0.3) | 0(0) | 11(1.8)* | 0(0) | 121(19.4)* |
| 30s | 1(0.2) | 7(1.4) | 19(3.7) | 17(3.3) | 2(0.4) | 3(0.6) | 5(1.0) | 1(0.2) | 55(10.8)* |
| 40s | 0(0) | 3(0.6) | 9(1.9) | 12(2.6)* | 0(0) | 3(0.6) | 5(1.1) | 3(0.6) | 35(7.5)* |
| 50s | 0(0) | 1(0.2) | 9(2.0) | 12(2.7) | 1(0.2) | 4(0.9) | 4(0.9) | 3(0.7) | 34(7.7) |
| Men | |||||||||
| 20s | 0(0) | 7(2.5) | 1(0.4) | 2(0.7) | 0(0) | 0(0) | 0(0) | 0(0) | 10(3.6) |
| 30s | 0(0) | 1(0.5) | 3(1.5) | 2(1.0) | 0(0) | 0(0) | 1(0.5) | 0(0) | 7(3.4) |
| 40s | 0(0) | 0(0) | 1(0.5) | 0(0) | 0(0) | 1(0.5) | 1(0.5) | 1(0.5) | 4(2.1) |
| 50s | 0(0) | 0(0) | 2(1.1) | 2(1.1) | 0(0) | 0(0) | 3(1.7) | 0(0) | 7(3.9) |
Note. Given differences in participation, sample sizes varied across time (age 20 women n=624, men n=276; age 30 women n=509, men n=206; age 40 women n=466, men n=189; age 50 women n=440, men n=181). Missing data were not imputed to determine diagnoses. AN=anorexia nervosa; BN=bulimia nervosa, BED=binge eating disorder, AAN=Atypical AN, PD=purging disorder; OSFED=other specified feeding or eating disorder; ED=eating disorder.
p < .05
Of the individuals who had an ED at age 50 and provided data to determine diagnosis at all four assessment waves, 25% (n = 7/28) of women and 33.3% (n = 2/6) of men had an onset at an earlier wave that persisted though age 50. Additionally, 46.4% (n = 13/28) of women and 16.7% (n=1/6) of men onset at an early age, remitted, and then relapsed at age 50. Of the individuals who had an ED at age 50, 28.6% of women (n = 8/28) and 50.0% of men (n = 3/6) represented new onset cases. The point prevalence of new onset cases did not differ significantly by gender (χ2[1, n=532] = 0.42, p = .84).
Regarding ED typology, the majority of overall and new onset cases at age 50 were diagnosed with OSFED for both women (overall: 70.6%, new onset: 62.5%) and men (overall: 71.4%, new onset: 66.7%, see Table 1). Over time, the proportion of OSFED cases increased for women (age 20 = 26.4%, age 30 = 47.3%, age 40 = 67.6%, age 50 = 70.6%) and men (age 20 = 20.0%, age 30 = 42.9%, age 40 = 75.0%, age 50 = 71.4%). This suggests that DSM-5 AN, BN, and BED may better capture EDs as experienced by younger individuals and fail to reflect how EDs present at older ages.
Establishing Measurement Invariance for the EDI between Genders through Age 50
Fit statistics for the unconstrained model for gender were χ2(86, N=610) = 404.13, p <.001; RMSEA (90% CI) =.110 (.099-.121), p <.001, SRMR = .060; CFI = .893 and fit statistics for the constrained model were χ2(95, N=610) = 424.94, p <.001; RMSEA (90% CI) = .107 (.096-.117), p <.001, SRMR = .067; CFI = .889. Fit statistics for the unconstrained model for age were χ2 (172, N=610) = 1119.70, p <.001; RMSEA (90% CI) = .099(.094-.105), p <.001, SRMR = .051; CFI = .925 and fit statistics for the constrained model were χ2(199, N=610) = 1271.22, p <.001; RMSEA (90% CI) = .098(.093-.104), p <.001, SRMR = .077; CFI = .915. Constraining factor loadings to be equal did degrade model fit for gender and age according to chi-square difference testing (gender: χ2diff=20.81, Δdf =9, p = .01; age: χ2diff=151.52, Δdf =27, p <.001). As chi-square testing is highly sensitive to sample size, we examined change in CFI between the models, based on recommendations by Cheung & Rensvold (2002), with ΔCFI < .01 supporting equivalent factor loadings. CFI values differed between the constrained and unconstrained models by .004 for gender and .01 for age, SRMR values did not differ appreciably, and 90% CIs for RMSEA overlapped. Taken together, these results extend previous research supporting factor invariance for the EDI across men and women through age 40 (Keel et al., 2007) to age 50.
Changes in Eating Disorder Attitudes and Behaviors between Genders across Age
Table 2 presents results from multilevel models examining differences in eating pathology between women and men across ages. The model for drive for thinness demonstrated a significant decrease in EDI DT scores for participants as they aged. A significant effect of gender indicated that females had higher EDI DT scores compared to males. There was a significant gender by age interaction, such that EDI DT scores marginally increased for men as they aged (b = .02, t = 2.00, p = .046; Cohen’s d age 20–50 = .14), while scores decreased for women as they aged (b = −.10, t = −12.53, p < .001; Cohen’s d age 20–50 = .56).
Table 2.
Changes in Estimated EDI Drive for Thinness and Bulimia scores in Men and Women across Ages 20 to 50
| Women | Men | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age 20 | Age 30 | Age 40 | Age 50 | Age 20 | Age 30 | Age 40 | Age 50 | ||
| EDI Subscale | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | M (SE) | |
| Fixed Effects Estimate γ (SE) | |||||||||
| Drive for Thinness | 14.68 (0.21) | 13.67 (0.18) | 12.66 (0.18) | 11.66 (0.22) | 9.12 (0.31) | 9.37 (0.27) | 9.62 (0.27) | 9.87 (0.33) | Intercept: 14.19 (0.27)*** |
| Age: −0.06 (0.01)*** | |||||||||
| Gender : 8.06 (0.59)*** | |||||||||
| Age*Gender : −0.13 (0.11)*** | |||||||||
| Bulimia | 13.34 (0.17) | 12.08 (0.13) | 10.82 (0.13) | 9.56 (0.15) | 10.27 (0.25) | 9.84 (0.20) | 9.40 (0.20) | 8.97 (0.24) | Intercept: 14.40 (0.22)*** |
| Age: −0.10 (0.01)*** | |||||||||
| Gender : 4.71 (0.49)*** | |||||||||
| Age*Gender : −0.08 (0.01)*** | |||||||||
Note. Fixed effects estimates are from multilevel models with age in years. Estimated marginal means are probed at ages 20, 30, 40, and 50. EDI=Eating Disorder Inventory.
p < .05
p < .01
p < .001
Results from the model for bulimic symptoms also demonstrated a significant decrease in EDI Bulimia scores for all participants as they aged, and women had higher EDI Bulimia scores overall compared to men. Males had a slower rate of reduction in EDI Bulimia scores compared to women as they aged (men: b = −.04, t = −4.40, p < .001; Cohen’s d age 20–50 = .32; women: b = −.13, t = −19.61, p <.001; Cohen’s d age 20–50 = .94).
Do Putative Risk Factors Differentially Affect Eating Pathology between Women and Men Over 30 Years?
Model 1: Does the Influence of Risk Factors Differ between Women and Men?
Results from the time-lagged model for drive for thinness (see Table 3) including main effects of risk factors and risk factor by gender interactions indicated significant main effects of gender, BMI, weight perception, and dieting frequency, such that being a woman, having a higher BMI, weight perception, and dieting frequency all predicted higher EDI DT scores over time. There was also a significant two-way interaction between gender and age, such that there were no significant changes in EDI DT scores for women as they aged (b = −.02, t = −1.21, p =.23), while EDI DT scores increased for men as they aged (b = .04, t = 3.16, p =.002). There were no significant two-way interactions between risk factor and gender.
Results from the time-lagged model for bulimic symptoms demonstrated a significant decrease in EDI Bulimia scores over time for all participants (see Table 3). Similar to DT models, there were also significant main effects of gender, BMI, weight perception, and dieting frequency in predicting increased EDI Bulimia scores across age. There were no significant two-way interactions between risk factor and gender.
Model 2: Does the Influence of Risk Factors Change Across Age?
Results from the model adding in the 2-way interactions between risk factors and age did not reveal any significant two-way risk factor by age interactions, collapsing across gender, for EDI DT or Bulimia (see Table 3).
Model 3: Does the Change in Risk Factor Influence Differ between Women and Men across Age?
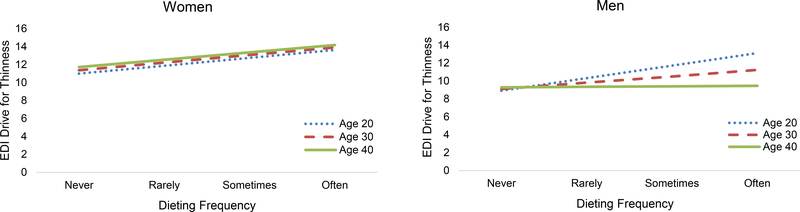
Results from models adding the three-way interactions between risk factors, gender, and age for EDI DT indicated a significant three-way interaction between gender, age, and dieting frequency (see Table 3; Figure 1). Specifically, for women, age did not have a significant impact on the association between dieting frequency and EDI DT scores (b <.005, t = 0.01, p = .80), with higher dieting frequency predicting higher EDI DT at all ages (b range = .82-.88, all p-values <.001). However, for men, the impact of dieting frequency on EDI DT scores decreased prospectively across age at the level of significance (b = −.06, t = −2.55, p = .01). Specifically, while higher dieting frequency at ages 20 and 30 predicted increased EDI DT scores, the impact of this association decreased across age in men to the point that there was no longer a significant association between dieting at age 40 and DT at age 50 (20s to 30s: b = 1.40, p <.001; 30s to 40s: b = .70, p =.001; 40s to 50s: b = .06, p =.85). No significant three-way interactions were found for the model of EDI Bulimia scores.
Figure 1.
Depiction of the three-way interaction between dieting frequency, gender, and age in prospectively predicting drive for thinness. For women (left), the relationship between dieting frequency and drive for thinness did not differ across age, with higher dieting frequency predicting higher drive for thinness at all ages. For men (right), the impact of dieting frequency on drive for thinness decreased prospectively across age, to the point that there was no longer a significant association between dieting at age 40 and drive for thinness at age 50.
Discussion
ED research has often focused on females in adolescence, in part due to assumptions regarding periods of peak risk. This focus has reinforced that EDs are more common in females than males by ignoring EDs in males or only examining gender differences within a limited age range. Results from the present study provide a more nuanced understanding of gender differences. EDs are not simply more common in women; instead, dramatic gender differences in this sample in late adolescence and young adulthood largely diminish in later mid-life. Indeed, the point prevalence of DSM-5 ED diagnoses in women decreased dramatically from age 20 to 30 and remained stable through 50, while point prevalence remained stable over time in men. Importantly, by age 50, there were no significant gender differences in ED point prevalence. Regarding eating pathology more broadly, drive for thinness decreased for women and increased for men across age, while bulimic symptoms decreased for both genders across age. Multilevel models demonstrated that the impact of dieting as a risk factor on drive for thinness decreased prospectively as men aged, to the point where it had no impact in mid-life on drive for thinness, whereas, the impact of dieting on drive for thinness remained stable and significant as women aged.
Results support that most women age out of their EDs. However, a significant minority (28.6%) of cases at age 50 represented new ED onset. Thus, there is no clear evidence that menopause exerts a specific influence on the prevalence of EDs in women. For men, the stable point prevalence over time may suggest a more extended period of risk through mid-life, with over half of the diagnoses at age 50 representing new ED onset. Notably, the number of men with EDs at age 50 was small (n=6), which limits our ability to draw definitive conclusion regarding potentially delayed onset in this group. Results should also be interpreted with caution, given missing data to determine diagnoses across waves. Thus, replication of these results in larger samples is needed. Across genders, the proportion of new onset cases around age 50 signifies the importance of additional research on EDs in mid-life and factors that may contribute to later-age onset. Further, consistent with and extending previous research (Mangweth-Matzek et al., 2014; Micali et al., 2017), the majority of new onset cases were OSFED presentations. This reinforces that EDs may present atypically in mid-life, making detection of these cases more challenging and more likely to be overlooked and/or untreated (Mangweth-Matzek & Hoek, 2017).
The patterns of ED point prevalence imply that dramatic gender differences in prevalence observed in late adolescence diminish over time. This is consistent with cross-sectional research demonstrating similar ED point prevalence estimates between genders in those over 45 (Hudson et al., 2007). Our point prevalence estimates for women in their 50s are generally comparable to estimates reported by Mangweth-Matzek and colleagues (2014); DSM-IV threshold disorders: 4.6%, DSM-IV subthreshold disorders: 4.8%) and slightly higher than those reported by Micali and colleagues (2017) in a longitudinal follow-up study of pregnant women (3.6%). While few studies have examined ED diagnoses in men, point prevalence estimates in the present study are generally comparable to 12-month DSM-IV prevalence estimates from a community sample of men ages 45–59 (2.5%; Hudson et al., 2007) and slightly lower than rates of EDs symptoms in a community-based sample of men in their 50s (6.8%; Mangweth-Matzek et al., 2016). Supporting that changes to DSM-5 criteria reduced the preponderance of residual ED diagnoses compared to prior editions of the DSM, the point prevalence of BN at baseline in this cohort was higher in the present study than when using DSM-III-R criteria in Keel et al. (2006) (women: 8.3% vs. 4.5%; men: 2.5% vs. 1%, respectively), and the point prevalence of OSFED was lower (women: 5.1% vs. 12.5%; men: 0.7% vs. 3.1%). Regarding trends in eating pathology, consistent with patterns observed in previous work with this cohort (Keel et al., 2007), bulimic symptoms continued to decrease through 30-year follow-up for both genders, and drive for thinness continued to decrease for women and increase for men. These results extend the growing literature on the incidence of EDs and eating pathology in mid-life (Mangweth-Matzek et al., 2014; Mangweth-Matzek et al., 2016; Micali et al., 2017; Mitchison et al., 2014) and support narrowed gender differences in symptoms through mid-life.
Prospective model results support that for women, dieting frequency exerts a stable and significant influence on drive for thinness from young adulthood to later mid-life. To the extent that dieting prospectively exerts these influences in models that include both BMI and weight perception, women’s motivation to diet for non-weight reasons may contribute to drive for thinness. Such non-weight related motivations may include a desire for control or for potential health effects (e.g., reducing HDL cholesterol; LaRose, Leahey, Hill, & Wing, 2013). In contrast, for men, dieting frequency conferred less risk for drive for thinness across age, to the point where dieting no longer predicted drive for thinness in later mid-life. For men, the influence of dieting may be overshadowed by the increasing impact of BMI across age. Thus, increases in dieting frequency for men later in mid-life may reflect a normative response to natural weight gain and accurate weight perception. It is important to note that individuals may interpret the term “dieting” in a myriad of ways, ranging from healthful to unhealthful behaviors. Further, it is possible that the term dieting may not capture the same set of behaviors and/or intentions as individuals age; thus, results should be interpreted with these considerations in mind. Additional research is needed to replicate gender differences in how the relationship between risk factors and eating pathology changes over the lifespan.
The present study has important implications for developmental perspectives on eating pathology beyond adolescence. Research has demonstrated that males and females report equivalent levels of disordered eating prior to pubertal onset, with gender differences emerging during and after puberty (Klump et al., 2012; Rozzell, Moon, Klimek, Brown, & Blashill, 2019). While the assumption has been that these patterns of gender differences persist into mid-life (Keel et al., 2007), results imply that current models of, and assumptions regarding, ED risk require refinement to account for developmental trajectories in which dramatic gender differences observed in late adolescence disappear during the approach to later mid-life. From a psychosocial perspective, these patterns may be influenced by differential effects of life role transitions between genders over time. For women in college, living with other women may increase vulnerability for eating pathology given peer influences on eating behavior (Keel, Forney, Brown, & Heatherton, 2013). As women age and move beyond college, changing life roles (e.g., marriage, motherhood), may impact their self-worth beyond appearance-related concerns, contributing to sharp declines in eating pathology after late adolescence (Keel et al., 2007). In contrast, for men, marriage and parental status may be less tied to eating and appearance-related concerns over time (Keel et al., 2007).
Our results also have important implications for ED intervention between genders. Among women, results support and reinforce the importance of prevention programs during late adolescence (Le, Barendregt, Hay, & Mihalopoulos, 2017), when ED risk factors and diagnoses are at their highest. While our results were generally encouraging regarding long-term prognosis for women, consistent with previous research, a substantial minority remained ill into their 30s (Eddy et al., 2017), underscoring the need for effective early interventions to help young women with EDs recover more quickly. Further, given that a substantial minority of ED cases at age 50 for women were new onset, cognitive-behavioral preventive intervention efforts (e.g., McLean, Paxton, & Wertheim, 2011) focused on acceptance of age-related weight gain and healthy ways to manage weight outside of restrictive dieting may also be relevant for a subset of mid-life women (Lewis-Smith, Diedrichs, Rumsey, & Harcourt, 2016). For men, prevalence patterns suggest prevention and intervention efforts may be beneficial across a broader range of ages (Haynos et al., 2018). In particular, for older men, given age-related weight gain and the decreasing impact of dieting on eating pathology over time, adapting interventions aimed at encouraging healthy dietary changes and physical activity (e.g., healthy weight interventions; Stice, Shaw, Burton, & Wade, 2006) for older men may be beneficial.
The current study had several noteworthy methodological strengths including the inclusion of both women and men, the 30-year length of follow-up from late adolescence to mid-life, repeated assessment waves, a strong retention rate across time, and an analytic approach that accounts for nested longitudinal data and minimizes type I error. Importantly, the present study provides much needed data regarding the point prevalence of EDs and the developmental course of eating pathology in mid-life between genders.
Despite these strengths, there are also some important limitations to note. First, the sample was drawn from a prestigious northeastern university and results may not generalize to other demographic populations. Relatedly, results may not generalize across other age cohorts, given that previous research demonstrating the decreasing point prevalence of bulimia nervosa over time (Keel et al., 2006). While the inclusion of males within the sample represents a strength, the undersampling of men in the 1982 cohort represents an important limitation, which may have reduced power to detect changes over time for this group. Given that the parent study was designed to address epidemiological questions about eating and health behaviors, all items were based on self-report and many key measures relied on single-item, self-report assessments (i.e., dieting frequency, weight perception). Additionally, measures included within the present study were developed for, and initially validated in, samples of women and thus may not capture all aspects of eating pathology relevant for men (e.g., muscularity concerns). ED diagnoses were also determined through algorithms applied to self-report data, which may have overestimated rates of EDs within the current sample. As such, future studies should replicate these results within other samples using interview-based assessments.
Conclusions
ED research has often overlooked male populations at all ages and females beyond adolescence, due to epidemiological data supporting that EDs predominantly occur in young women. This focus has seriously limited our understanding of ED risk within understudied groups and inadvertently reinforced expectations about gender differences in ED psychopathology. Results from the present study help close this gap and support a paradigm shift in understanding that gender differences in EDs are age-dependent, with significant gender differences in ED prevalence and psychopathology in late adolescence narrowing in later mid-life. Continued research on how eating pathology and risk factors may differ between genders across the lifespan is essential to help inform intervention efforts for all those who suffer from EDs.
General Scientific Summary.
This study suggests that while eating disorder prevalence and eating pathology is elevated in women compared to men during late adolescence, these gender differences diminish by later mid-life.
Acknowledgments
Funding: This work was supported by grants from the Milton Fund and National Institute of Mental Health (R01MH63758, PI: Keel; F31MH105082, PI: Forney). Portions of this work have been previously presented at the 2017 annual International Conference on Eating Disorders in Prague, Czech Republic. We thank the Henry Murray Center of the Radcliffe Institute for providing access to data from Todd Heatherton’s Follow-up and Replication of Prevalence among College Students (baseline data) and the Alumni Office of Harvard University for supplying addresses for participants at follow-up.
Research ethics committee approval: This study, “Bulimic Syndromes: Secular & Longitudinal Trends II” was approved by the Florida State University Institutional Review Board.
Footnotes
Given that racial/ethnic minority participants were less likely to participate at follow-up, we examined race/ethnicity as a covariate in multilevel models. Race/ethnicity was not a significant predictor of EDI DT or Bulimia scores (p-values >.05) and the overall pattern of results remained unchanged
Post-hoc power analyses for a χ2 goodness of fit test supported that the total sample provided > 80% power at alpha=.05 to detect the small-medium effect size observed at age 50 (w=.28).
Contributor Information
Tiffany A. Brown, Department of Psychiatry, University of California San Diego
K. Jean Forney, Department of Psychology, Ohio University
Kelly M. Klein, VA Boston Healthcare System, Brockton Division
Charlotte Grillot, Department of Psychology, Florida State University
Pamela K. Keel, Department of Psychology, Florida State University
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Burton NW, Brown W, & Dobson A (2010). Accuracy of body mass index estimated from self-reported height and weight in mid-aged Australian women. Australian and New Zealand Journal of Public Health, 34, 620–623. doi: 10.1111/j.1753-6405.2010.00618.x [DOI] [PubMed] [Google Scholar]
- Cheung GW, & Rensvold RB (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling, 9, 233–255. doi: 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- Curran PJ, & Bauer DJ (2011). The disaggregation of within-person and between-person effects in longitudinal models of change. Annual Review of Psychology, 62, 583–619. doi: 10.1146/annurev.psych.093008.100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorsey RR, Eberhardt MS, & Ogden CL (2009). Racial/ethnic differences in weight perception. Obesity, 17, 790–795. doi: 10.1038/oby.2008.603 [DOI] [PubMed] [Google Scholar]
- Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, … Keel PK (2017). Recovery from Anorexia Nervosa and Bulimia Nervosa at 22-year follow-up. The Journal of Clinical Psychiatry, 78, 184–189. doi: 10.4088/JCP.15m10393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, & Polivy J (1983). Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders, 2, 15–34. doi: [DOI] [Google Scholar]
- Guo SS, Zeller C, Chumlea WC, & Siervogel RM (1999). Aging, body composition, and lifestyle: The Fels longitudinal study. The American Journal of Clinical Nutrition, 70, 405–411. doi: 10.1093/ajcn/70.3.405 [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Wall MM, Choo T-HJ, Evans EW, Jelalian E, Larson N, & Neumark-Sztainer D (2018). Fifteen-year weight and disordered eating patterns among community-based adolescents. American Journal of Preventive Medicine, 54, e21–e29. doi: 10.1016/j.amepre.2017.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halliwell E, & Dittmar H (2003). A qualitative investigation of women’s and men’s body image concerns and their attitudes toward aging. Sex Roles, 49, 675–684. doi: 10.1023/B:SERS.0000003137.71080.97 [DOI] [Google Scholar]
- Hay P, Girosi F, & Mond J (2015). Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian population. Journal of Eating Disorders, 3, 19. doi: 10.1186/s40337-015-0056-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynos AF, Wall MM, Chen C, Wang SB, Loth K, & Neumark-Sztainer D (2018). Patterns of weight control behavior persisting beyond young adulthood: Results from a 15-year longitudinal study. International Journal of Eating Disorders, 51, 1090–1097. doi: 10.1002/eat.22963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Mahamedi F, Striepe M, Field AE, & Keel P (1997). A 10-year longitudinal study of body weight, dieting, and eating disorder symptoms. Journal of Abnormal Psychology, 106, 117–125. doi: 10.1037/0021-843X.106.1.117 [DOI] [PubMed] [Google Scholar]
- Helzer JE, Kraemer HC, & Krueger RF (2006). The feasibility and need for dimensional psychiatric diagnoses. Psychological Medicine, 36, 1671–1680. doi: 10.1017/S003329170600821X [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG Jr., & Kessler RC (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61, 348–358. doi: 10.1016/j.biopsych.2006.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Baxter MG, Heatherton TF, & Joiner TE Jr (2007). A 20-year longitudinal study of body weight, dieting, and eating disorder symptoms. Journal of Abnormal Psychology, 116, 422–432. doi: 10.1037/0021-843X.116.2.422 [DOI] [PubMed] [Google Scholar]
- Keel PK, & Brown TA (2010). Update on course and outcome in eating disorders. International Journal of Eating Disorders, 43, 195–204. doi: 10.1002/eat.20810 [DOI] [PubMed] [Google Scholar]
- Keel PK, Forney KJ, Brown TA, & Heatherton TF (2013). Influence of college peers on disordered eating in women and men at 10-year follow-up. Journal of Abnormal Psychology, 122, 105–110. doi: 10.1037/a0030081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel PK, Gravener JA, Joiner TE Jr., & Haedt AA (2010). Twenty-year follow-up of bulimia nervosa and related eating disorders not otherwise specified. International Journal of Eating Disorders, 43, 492–497. doi: 10.1002/eat.20743 [DOI] [PubMed] [Google Scholar]
- Keel PK, Heatherton TF, Dorer DJ, Joiner TE, & Zalta AK (2006). Point prevalence of bulimia nervosa in 1982, 1992, and 2002. Psychological Medicine, 36, 119–127. doi: 10.1017/S0033291705006148 [DOI] [PubMed] [Google Scholar]
- Keel PK, & Klump KL (2003). Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychological Bulletin, 129, 747–769. doi: 10.1037/0033-2909.129.5.747 [DOI] [PubMed] [Google Scholar]
- Klump KL, Culbert KM, & Sisk CL (2017). Sex differences in binge eating: Gonadal hormone effects across development. Annual Review of Clinical Psychology, 13, 183–207. doi: 10.1146/annurev-clinpsy-032816-045309 [DOI] [PubMed] [Google Scholar]
- Klump KL, Culbert KM, Slane JD, Burt SA, Sisk CL, & Nigg J (2012). The effects of puberty on genetic risk for disordered eating: Evidence for a gender difference. Psychological Medicine, 42, 627–637. doi: 10.1017/S0033291711001541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klump KL, Racine SE, Hildebrandt B, Burt SA, Neale M, Sisk CL, … Keel PK (2014). Influences of ovarian hormones on dysregulated eating: A comparison of associations in women with versus women without binge episodes. Clinical Psychological Science, 2, 545–559. doi: 10.1177/2167702614521794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRose JG, Leahey TM, Hill JO, & Wing RR (2013). Differences in motivations and weight loss behaviors in young adults and older adults in the National Weight Control Registry. Obesity, 21, 449–453. doi: 10.1002/oby.20053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, De Young KP, & Anderson DA (2010). Eating Disorder Examination Questionnaire (EDE-Q): Norms for undergraduate men. Eating Behaviors, 11, 119–121. doi: 10.1016/j.eatbeh.2009.09.005 [DOI] [PubMed] [Google Scholar]
- Le LK-D, Barendregt JJ, Hay P, & Mihalopoulos C (2017). Prevention of eating disorders: A systematic review and meta-analysis. Clinical Psychology Review, 53, 46–58. doi: 10.1016/j.cpr.2017.02.001 [DOI] [PubMed] [Google Scholar]
- Lewis-Smith H, Diedrichs PC, Rumsey N, & Harcourt D (2016). A systematic review of interventions on body image and disordered eating outcomes among women in midlife. International Journal of Eating Disorders, 49, 5–18. doi: 10.1002/eat.22480 [DOI] [PubMed] [Google Scholar]
- Liechty JM, & Lee MJ (2013). Longitudinal predictors of dieting and disordered eating among young adults in the US. International Journal of Eating Disorders, 46, 790–800. doi: 10.1002/eat.22174 [DOI] [PubMed] [Google Scholar]
- Luo X, Donnellan MB, Burt SA, & Klump KL (2016). The dimensional nature of eating pathology: Evidence from a direct comparison of categorical, dimensional, and hybrid models. Journal of Abnormal Psychology, 125, 715–726. doi: 10.1037/abn0000174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangweth-Matzek B, & Hoek HW (2017). Epidemiology and treatment of eating disorders in men and women of middle and older age. Current Opinion in Psychiatry, 30, 446–451. doi: 10.1097/YCO.0000000000000356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangweth-Matzek B, Hoek HW, Rupp CI, Lackner-Seifert K, Frey N, Whitworth AB, … Kinzl J (2014). Prevalence of eating disorders in middle-aged women. International Journal of Eating Disorders, 47, 320–324. doi: 10.1002/eat.22232 [DOI] [PubMed] [Google Scholar]
- Mangweth-Matzek B, Kummer KK, & Pope HG (2016). Eating disorder symptoms in middle-aged and older men. International Journal of Eating Disorders, 49, 953–957. doi: 10.1002/eat.22550 [DOI] [PubMed] [Google Scholar]
- McLean SA, Paxton SJ, & Wertheim EH (2011). A body image and disordered eating intervention for women in midlife: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79, 751–758. doi: 10.1037/a0026094 [DOI] [PubMed] [Google Scholar]
- Micali N, Martini MG, Thomas JJ, Eddy KT, Kothari R, Russell E, … Treasure J (2017). Lifetime and 12-month prevalence of eating disorders amongst women in mid-life: A population-based study of diagnoses and risk factors. BMC Medicine, 15, 12. doi: 10.1186/s12916-016-0766-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison D, Hay P, Slewa-Younan S, & Mond J (2014). The changing demographic profile of eating disorder behaviors in the community. BMC Public Health, 14, 943. doi: 10.1186/1471-2458-14-943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison D, & Mond J (2015). Epidemiology of eating disorders, eating disordered behaviour, and body image disturbance in males: A narrative review. Journal of Eating Disorders, 3, 20. doi: 10.1186/s40337-015-0058-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall MM, Chen C, Larson NI, Christoph MJ, & Sherwood NE (2018). Eating, activity, and weight-related problems from adolescence to adulthood. American Journal of Preventive Medicine, 55, 133–141. doi: 10.1016/j.amepre.2018.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Jeffery RW, & French SA (1997). Self-reported dieting: How should we ask? What does it mean? Associations between dieting and reported energy intake. International Journal of Eating Disorders, 22, 437–449. doi: [DOI] [PubMed] [Google Scholar]
- Patrick JH, & Stahl ST (2009). Understanding disordered eating at midlife and late life. The Journal of General Psychology, 136, 5–20. doi: 10.3200/GENP.136.1.5-20 [DOI] [PubMed] [Google Scholar]
- Preti A, de Girolamo G, Vilagut G, Alonso J, de Graaf R, Bruffaerts R, … Morosini P (2009). The epidemiology of eating disorders in six European countries: Results of the ESEMeD-WMH project. Journal of Psychiatric Research, 43, 1125–1132. doi: 10.1016/j.jpsychires.2009.04.003 [DOI] [PubMed] [Google Scholar]
- Pruis TA, & Janowsky JS (2010). Assessment of body image in younger and older women. The Journal of General Psychology: Experimental, Psychological, and Comparative Psychology, 137, 225–238. doi: 10.1080/00221309.2010.484446 [DOI] [PubMed] [Google Scholar]
- Rannevik G, Jeppsson S, Johnell O, Bjerre B, Laurell-Borulf Y, & Svanberg L (1995). A longitudinal study of the perimenopausal transition: Altered profiles of steroid and pituitary hormones, SHBG and bone mineral density. Maturitas, 21, 103–113. doi: 10.1016/0378-5122(94)00869-9 [DOI] [PubMed] [Google Scholar]
- Rosseel Y (2012). Lavaan: An R package for structural equation modeling and more Version 0.5–12 (BETA). Ghent, Belgium: Ghent University. [Google Scholar]
- Rozzell K, Moon DY, Klimek P, Brown T, & Blashill AJ (2019). Prevalence of eating disorders among US children aged 9 to 10 years: Data from the adolescent brain cognitive development (ABCD) study. JAMA Pediatrics, 173, 100–101. doi: 10.1001/jamapediatrics.2018.3678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. doi: 10.1037/1082-989X.7.2.147 [DOI] [PubMed] [Google Scholar]
- Slevec JH, & Tiggemann M (2011). Predictors of body dissatisfaction and disordered eating in middle-aged women. Clinical Psychology Review, 31, 515–524. doi: 10.1016/j.cpr.2010.12.002 [DOI] [PubMed] [Google Scholar]
- Stice E (2002). Risk and maintenance factors for eating pathology: A meta-analytic review. Psychological Bulletin, 128, 825–848. doi: 10.1037/0033-2909.128.5.825 [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, & Lowe MR (2004). Are dietary restraint scales valid measures of acute dietary restriction? Unobtrusive observational data suggest not. Psychological Assessment, 16, 51–59. doi: 10.1037/1040-3590.16.1.51 [DOI] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, & Wade E (2006). Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology, 74, 263–275. doi: 10.1037/0022-006X.74.2.263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udo T, & Grilo CM (2018). Prevalence and correlates of DSM-5–defined eating disorders in a nationally representative sample of US adults. Biological Psychiatry, 84, 345–354. doi: 10.016/j.biopsych.2018.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]