The coronavirus disease 2019 (COVID-19) pandemic has presented health care professionals with extraordinary challenges. As of April 13, 2020, there are about 555,000 confirmed cases in the United States and about 22,000 deaths; almost half of the deaths to date are in the state of New York. In New York City, with a population density of 26,430 people per square mile, the densest of any American municipality with a population greater than 100,000.1 social distancing may mitigate the strain on existing health care systems. Furthermore, the absence of widely available testing has resulted in additional use of already limited resources, including hospital beds, personal protective equipment, and staff. As nephrologists, we see our primary goals as 2-fold: (1) keeping our existing patients safe both at home and in their dialysis units, and (2) meeting the needs of patients who require hospitalization, both COVID-19 related and unrelated.
The Mount Sinai Hospital, located in East Harlem, NY, has been at the forefront of patient care during the COVID-19 pandemic. It is also home to a large home dialysis unit with 80 peritoneal dialysis (PD) and 20 home hemodialysis (HD) patients. We report our experience with caring for this patient population during this crisis in the outpatient setting, as well as our procedures to use acute PD to combat the inexorable increase in the number of admitted patients requiring kidney replacement therapy in the inpatient setting.
Home Dialysis
As of March 16, a number of changes were implemented in the home dialysis unit to avoid the unnecessary exposure of staff and patients to infection while still continuing to provide care and support to our patients. Within a span of a few days, our PD unit obtained 2 iPads, arranged courier services, and contracted with a laboratory company to obtain, deliver, and process patients’ monthly blood work to effectively provide telemedicine services.
Each patient was contacted 24 to 48 hours before their scheduled appointment by a clinic coordinator to confirm their appointment date and time and to explain that their monthly visits would be conducted in the comfort of their own homes with the use of our telehealth capabilities. Because the government expanded telehealth capabilities and waived penalties for HIPAA (Health Insurance Portability and Accountability Act of 1996) violations, we used platforms such as FaceTime, WhatsApp, and Zoom to expedite this process. A contracted laboratory company provided home visits, with laboratory results available within 24 hours of the blood draw.
Dialysis staff called patients on the day and time of their clinic appointments. Patients were asked to take their temperature, pulse, and blood pressure. Visual examinations were performed, including inspection of the exit site and evaluation for respiratory distress and edema. A thorough review of systems was also performed. The majority of our patients use Baxter’s Amia cycler with the remote Sharesource connectivity platform, which has been an invaluable resource to get patients’ daily treatment information. Patients also spoke with the dietician and social worker. Patients’ medications and prescriptions were adjusted. Monthly medications for anemia and mineral bone disease provided by the dialysis unit were delivered to patients’ homes by a contracted courier company. The same company picked up urine and dialysate samples if needed to assess dialysis adequacy (Kt/V) and delivered them to the dialysis unit.
Situations in which it was deemed necessary for the patient to be physically present in the clinic included incident home patients, patients with PD catheter complications (such as exit-site or tunnel infections), patients with suspected peritonitis, and patients deemed unstable. These patients were triaged over the telephone by the clinical staff for potential COVID-19 infection risk factors and symptoms, and if negative, they were instructed to come in to the dialysis unit for further evaluation. After this system was implemented, we successfully managed >80% of our patients remotely.
Inpatient Dialysis
There has been an increase in hospital demands for HD, due to maintenance HD patients being admitted with COVID-19 disease, severe acute kidney injury (AKI) with COVID-19 infection requiring urgent dialysis, and the increasing number of maintenance dialysis patients throughout the city who missed their regularly scheduled dialysis sessions and present to hospitals. Given this surge in dialysis needs and an increase in the number of clotted dialysis systems resulting in either prolonged treatment time or inadequate treatments due to the prothrombotic nature of COVID-19,2 and decreased HD nursing staff availability due to COVID-19 infection, our current dialysis setup has been insufficient to handle the load. As a result, we developed an acute PD program at the Mount Sinai Hospital with the major goal of maximizing our ability to provide dialysis resources for this surge.
Acute PD
Acute PD is a viable alternative to HD, not only reducing the number of central venous catheters being placed and therefore the number of central line–associated bloodstream infections, but also providing patients with a viable long-term solution for their dialysis needs if they continue to require it in the outpatient setting at the time of discharge.
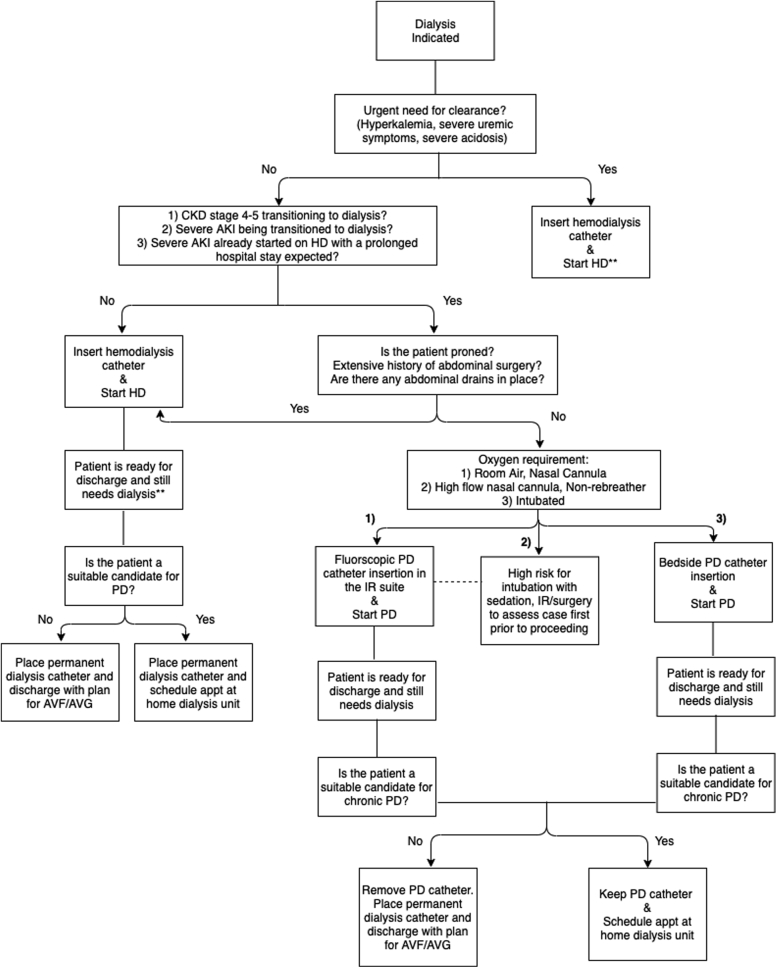
As of April 14, 2020, we have treated 10 patients with acute PD. This program is mainly focused on transitioning hospitalized patients with new dialysis needs to PD (Fig 1). Targeted patient groups include: (1) admitted patients with chronic kidney disease stages 4 to 5 who were transitioned to HD during their current admission and who are expected to have a prolonged hospital stay, and (2) patients with unresolved AKI who have not been started on kidney replacement therapy and who are appropriate candidates for PD. In the event that we still cannot meet our dialysis demands, we would then consider switching maintenance HD patients temporarily to PD while in the inpatient setting. The acute PD program is being applied to all admitted patients regardless of their COVID-19 infection status. Patients with AKI who require urgent clearance (hyperkalemia, with potassium level > 6.0 mEq/L; severe uremic symptoms such as pericardial effusions or seizures; and severe acidosis, with pH < 7.2), as well as prone patients, were not considered good candidates for acute PD and it was recommended that they have HD catheters placed instead. A major challenge was timing, specifically when the acute PD program would be implemented. We elected to transition to acute PD when we reached 75% of maximal HD (including continuous HD) capacity.
Figure 1.
Dialysis decision tree. Abbreviations: AKI, acute kidney injury; appt, appointment; AVF/AVG, arteriovenous fistula/arteriovenous graft; CKD, chronic kidney disease; HD, hemodialysis; IR, interventional radiology; PD, peritoneal dialysis.
A major advantage of PD in this crisis was our ability to train non-nursing staff in the PD procedure, which is not technically challenging but requires strict sterile technique. This differs from the technical requirements needed to provide HD and is particularly important should we encounter staff shortages of existing dialysis nurses and technicians.
We are using an automated cycler that can be set up in 10 to 15 minutes and allows for daily retrospective monitoring of patients’ treatments. We also plan to use manual exchanges if the demand for dialysis exceeds our supply of cyclers. In that situation, fairly minimal dialysis with 3 to 4 exchanges per day (starting with low-volume fills such as 1 L and gradually increasing to 1.5-2 L in a couple of days) may be necessary. We have had extensive experience with the use of a manifold system, a multiline tubing set that allows for the connection of 5 to 9 dialysate bags (any volume bags may be used).3
An acute PD program is a 24/7 operation; as a result, we proposed the training of licensed practical nurses (LPNs) and technicians to help troubleshoot treatments overnight. The LPNs/technicians are available to the hospital nurses during the cycler treatments and can communicate any issues directly with the nephrologist on call. We have surgeons and an interventional nephrologist on staff at Mount Sinai with expertise in PD catheter placement. They are committed to providing their support through the timely placement of double-cuff PD catheters.
Patients who are breathing room air or use a nasal cannula are transported to the interventional radiology suite for fluoroscopic catheter placement by the interventional nephrologist, whereas patients who are intubated have their catheters placed at the bedside by the surgery team. Patients who are using a high-flow nasal cannula, bilevel positive airway pressure, or a nonrebreather mask would be assessed by the radiology team for suitability of catheter placement given their high risk for decompensation with sedation, potentially resulting in intubation and mechanical ventilation. A decision would then be taken by them as to whether the patient is a suitable candidate for the procedure.
Our acute PD implementation protocol follows.
-
1.
The nephrologist(s) assesses the patient’s suitability for PD, then communicates with the surgeon/interventional radiologist for catheter placement.
-
2.
PD catheter insertion is followed by initiation within 48 to 72 hours with low volumes and a high number of exchanges.
-
3.
PD is performed overnight or throughout the day (according to individual patient needs).
-
4.
At the end of each treatment session, an LPN collects data from the cyclers (initial drain, ultrafiltration, average dwell time, number of cycles, and average drain time) and documents this information in the electronic medical record, which can be reviewed by the covering nephrologist, with prescription changes made accordingly.
For patients treated with acute PD catheter insertion who are still dialysis dependent at the time of discharge, the nephrology team will evaluate their suitability for outpatient PD. If deemed suitable, the patient would have an urgent appointment scheduled with the home dialysis unit. If the patient is deemed an unsuitable candidate, a tunneled HD catheter will be placed and the patient would be set up with an outpatient HD unit. The PD catheter would then be removed before discharge. Further access plans will depend on the likelihood of kidney recovery.
The COVID-19 pandemic is rapidly evolving, and these planning steps have helped prepare us for the surge that we have been confronted with in April 2020. Circumstances will continue to change in the coming weeks, and we will pursue finding creative ways to combat and deal with them. The success of our proposed changes remains to be seen, but it is a work in progress that will hopefully meet the demands that we are anticipating.
Article Information
Authors’ Full Names and Academic Degrees
Osama El Shamy, MD, Shuchita Sharma, MD, Jonathan Winston, MD, and Jaime Uribarri, MD.
Support
None.
Financial Disclosure
Dr Winston reports consulting fees for Relypsa, Inc and Sarepta Therapeutics. The remaining authors declare that they have no relevant financial interests.
Peer Review
Received March 31, 2020. Direct editorial input by the Editor-in-Chief. Accepted in revised form April 14, 2020.
References
- 1.Demographics of New York City. February 22, 2020. Wikipedia. https://en.wikipedia.org/wiki/Demographics_of_New_York_City Accessed March 28, 2020.
- 2.Alberici F., Delbarba E., Manenti C. on behalf of the Brescia Renal COVID Task Force. Management of patients on dialysis and with kidney transplant during SARS-COV-2 (COVID-19) pandemic in Brescia, Italy. Kidney Int Rep. 2020;5(5):580–585. doi: 10.1016/j.ekir.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mallipattu S., Duffoo M., Fallahi A., Uribarri J. Manifold exchange: a delivery option in managing patients on peritoneal dialysis. Perit Dial Int. 2014;34(6):657–663. doi: 10.3747/pdi.2013.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]