Abstract
The double burden of malnutrition (DBM), defined as the simultaneous manifestation of both undernutrition and overweight/obesity, affects most low- and middle-income countries (LMICs). This paper describes the dynamics of DBM in LMICs and how it differs by socioeconomic level. The paper shows that DBM has increased in the poorest LMICs, mainly due to overweight/obesity increases. Indonesia is the largest country experiencing severe levels of the DBM, but many other Asian and sub-Saharan African countries also face this problem. We also discuss that overweight increases are mainly due to rapid changes in the food system, particularly the availability of cheap ultra-processed food and beverages in LMICs while there are major reductions in physical activity at work, transportation, home and even leisure related to introductions of activity-saving technologies. Understanding that the lowest income LMICs face severe levels of DBM and that the major direct cause is rapid increases in overweight allows identifying selected critical drivers and possible options for addressing DBM at all levels.
INTRODUCTION
The global health community has been slow to acknowledge the challenge of the large proportion of low- and middle-income countries (LMICs) facing the double burden of malnutrition (DBM) – the coexistence of undernutrition (i.e., micronutrient deficiencies, underweight and childhood stunting and wasting) and overweight/obesity and diet-related non communicable diseases. Current estimates are that 2.28 billion1 or more children and adults are overweight and more than 150 million children are stunted.2,3
There are a number of studies that describe double burden of nutritional deficiencies (childhood stunting/wasting and micronutrient deficiencies) and overweight/obesity affecting countries, households, and individuals. This includes the very first set of studies,4–6 but is represented by a growing literature that has focused on understanding the dimensions of the problem and the causes, consequences, and possible solutions.7–13 The analysis has pinpointed several reasons for this health crisis, many related to the stage of the nutrition transition dominated by reduced physical activity and increased access to less healthful, highly processed foods and beverages14–21. However, there is a gap on how to translate this evidence into effective actions.
Building on the 2013 Lancet Series on Maternal and Child Nutrition and complementing other major scientific initiatives such as The EAT-Lancet Commission on Food, Planet, Health and the Lancet Commission on The Global Syndemic of Obesity, Undernutrition, and Climate Change,22–24 this series highlights the new nutrition reality: that there are multiple forms of malnutrition that overlap in different ways and in different places13 and that addressing malnutrition in all its forms will require new ways of designing, targeting, and implementing programs and policies to accelerate progress in improving nutrition globally. We also want to acknowledge that the impact of undernutrition over the past 4–5 decades will impact our health for many future years. While stunting has declined greatly from the early 1990’s, we must understand that the stunting of last 3–4 decades will subsequently have a great effect on subsequent increases decades later in the way of increased visceral fat and greater risks of major NCDs.25 as discussed in the Wells et al paper and the key cohorts studies.25–29
This 2019 series is timely, with the recent UN Decade of Action on Nutrition and the Sustainable Development Goals shifting focus from predominantly undernutrition, or single ‘sides’ of malnutrition, to all forms of malnutrition.30,31 Further, major UN and other international institutions and donors are revisiting their strategies to reconsider the scope of nutrition priorities, developing strategy documents and formulating initiatives to focus on overweight/obesity as well as undernutrition.32
The papers in this series take this a step further and focus on not only the epidemiology and larger societal changes in the food system and other major demographic and economic dimensions but also the biological underpinnings of stunting and subsequent adiposity and NCD risk33They also take this issue into the program and policy area34 by building on the work on double duty inventions11 which focus on reducing both undernutrition and overweight/obesity but also how ignoring obesity in programs focused on malnutrition prevention at various ages has affected obesity and the DBM34 and focus on the economic impacts of health programs and policies.35
This first paper in the series introduces the epidemiology of the DBM, presents changes in global estimates of the DBM and its components and uses repeated household surveys to explore aspects of the DBM. It then provides an overview of the nutrition and food system transitions that explain the large increase in the DBM, particularly among the lowest-income LMICs. The final section discusses the4–6consequences of the problem and possible solutions.7,8,12,36–38,34,39,14,40–43,14,16,44–48,39,34,38,35
PART 1: THE DOUBLE BURDEN AND ITS PREVALENCE: COUNTRY AND HOUSEHOLD EPIDEMIOLOGY
In this and the subsequent papers of this series we use malnutrition to refer to both wasting/stunting/thinness and overweight/obesity. Although micronutrient malnutrition is recognized as a component of undernutrition, we have not been able to include it in our DBM estimates, due to the lack of sufficient data.49,50,51,52–58,51,50
Country-level double burden
DBM at the country level was defined as having a high prevalence of both undernutrition and overweight/obesity in at least one population group. We examined which countries had DBM [DBM; prevalence wasting >15% or stunting > 30% or women’s thinness (prevalence >20%)]and adult or child overweight(prevalence >20, 30, 40%). The cutoffs for undernutrition ares defined as wasting (WHZ<−2) or stunting (HAZ<−2) for children age 0–4 and thinness (BMI<18.5) for adult women. For overweight (BMI Z >+2 in children under age 18 and BMI>25 for adults36 exceeds 20%, 30%, or 40% prevalence (Figure 1 and Supplemental Tables S1 and S2). We use a combination of overweight and obesity because extensive epidemiological research associates BMI of 25 or even lower to the risks of noncommunicable diseases (NCDs) across LMICs.37–43
Figure 1. The global double burden of malnutrition in low- and middle-income countries based on 1990s and 2010s weight and height data*.
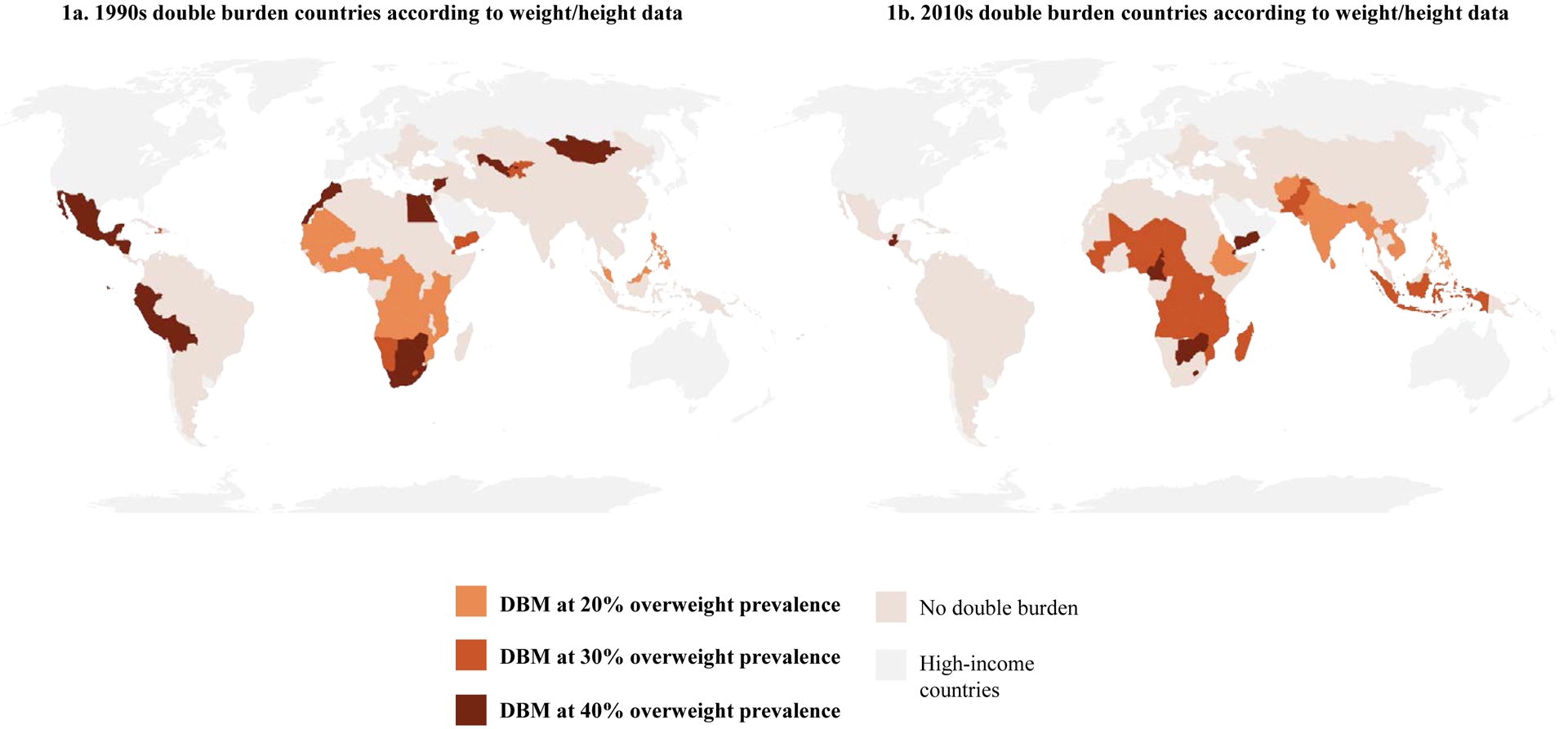
(using UNICEF, WHO, World Bank, and NCD-RisC estimates, supplemented with selected DHS and other country direct measures)
* Double burden of malnutrition (DBM) = at least 1 child, adolescent, or adult in household with severe levels of wasting/stunting/thinness and 1 with overweight/obesity (shown at 20%, 30%, or 40% overweight prevalence)
Among 123 countries with 1990s data, the number with DBM based on 20, 30, and 40% overweight prevalence was 45, 22, and 15, respectively (Figure 1a, Supplemental Table S1). Of the 126 countries with data from the 2010s, 48, 35, or 10 countries face DBM with overweight prevalence exceeding 20%, 30%, or 40%, respectively (Figure 1b and Supplemental Table S2). DBM is especially concentrated in Sub-Saharan Africa, South Asia, and East Asia and Pacific. In countries with data for both time periods, increases and decreases were roughly balanced, using the 30% and 40% cutoffs. Increases in DBM were observed particularly in Asia, whereas improvements were observed in Latin America/Caribbean and Middle East/North Africa.
Economic Development and DBM at the National Level
Examining the changes in DBM status by quartile of GDP/capita in 1990, we can see that increases in DBM from the 1990s to 2010s are concentrated in the lowest quartile countries, whereas the number of countries with DBM has declined in the top three income quartiles (Figure 2). The largest increases in number of DBM countries were observed using the 20% and 30% adult overweight prevalence cutoffs. This highlights the driving role of overweight in shaping countries now facing a high DBM, with the greatest effect among the lowest quartile of GDP/capita countries. Figure 3 further highlights these changes in DBM by income quartile. At the same time, the total number of countries with severe levels of DBM declined using the 40% overweight cutoff, related mainly to significant declines in wasting and stunting.
Figure 2. Countries with high double burden of malnutrition* in 1990s and 2010s, by time period and GDP/capita (PPP) quartile**.
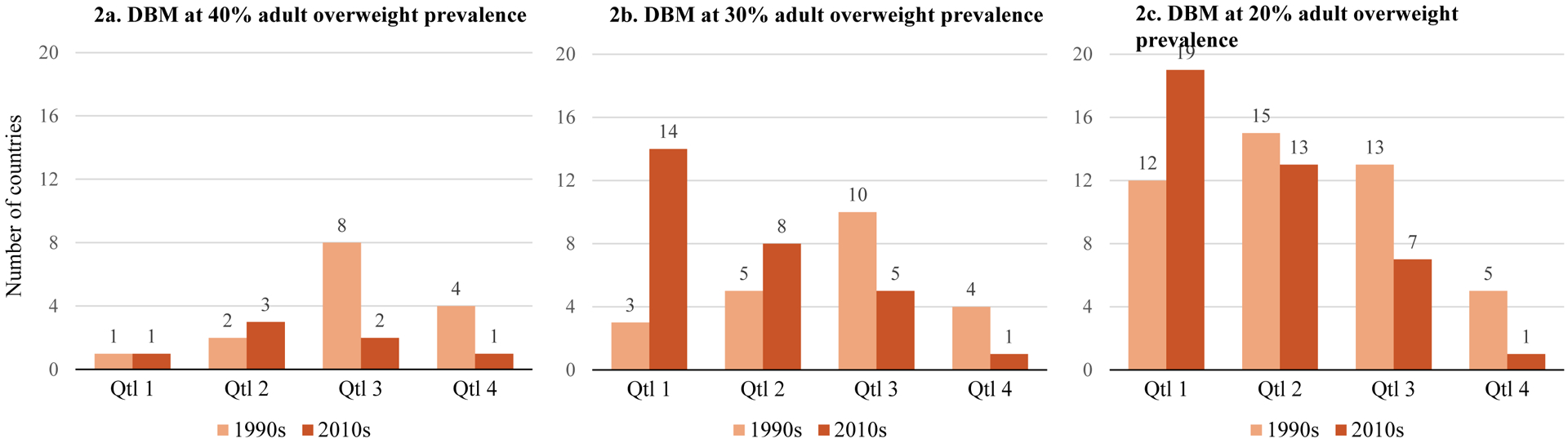
* Double burden of malnutrition (DBM) = at least 1 child, adolescent, or adult in household with severe levels of wasting/stunting/thinness and 1 with overweight/obesity(shown at 20%, 30%, or 40% adult overweight prevalence); countries only included here if they had DBM data available for bothtime periods (1990s and 2010s)
** Quartile (Qtl) 1 is lowest-wealth, Qtl4 is highest-wealth
Data sources: Based on UNICEF, WHO, World Bank, and NCD-RisCestimates supplemented with selected DHS and other country direct measures for the 1990’s
Figure 3. Number of countries that changed double burden of malnutrition* status from 1990s to 2010s, by GDP/capita (PPP) quartile.
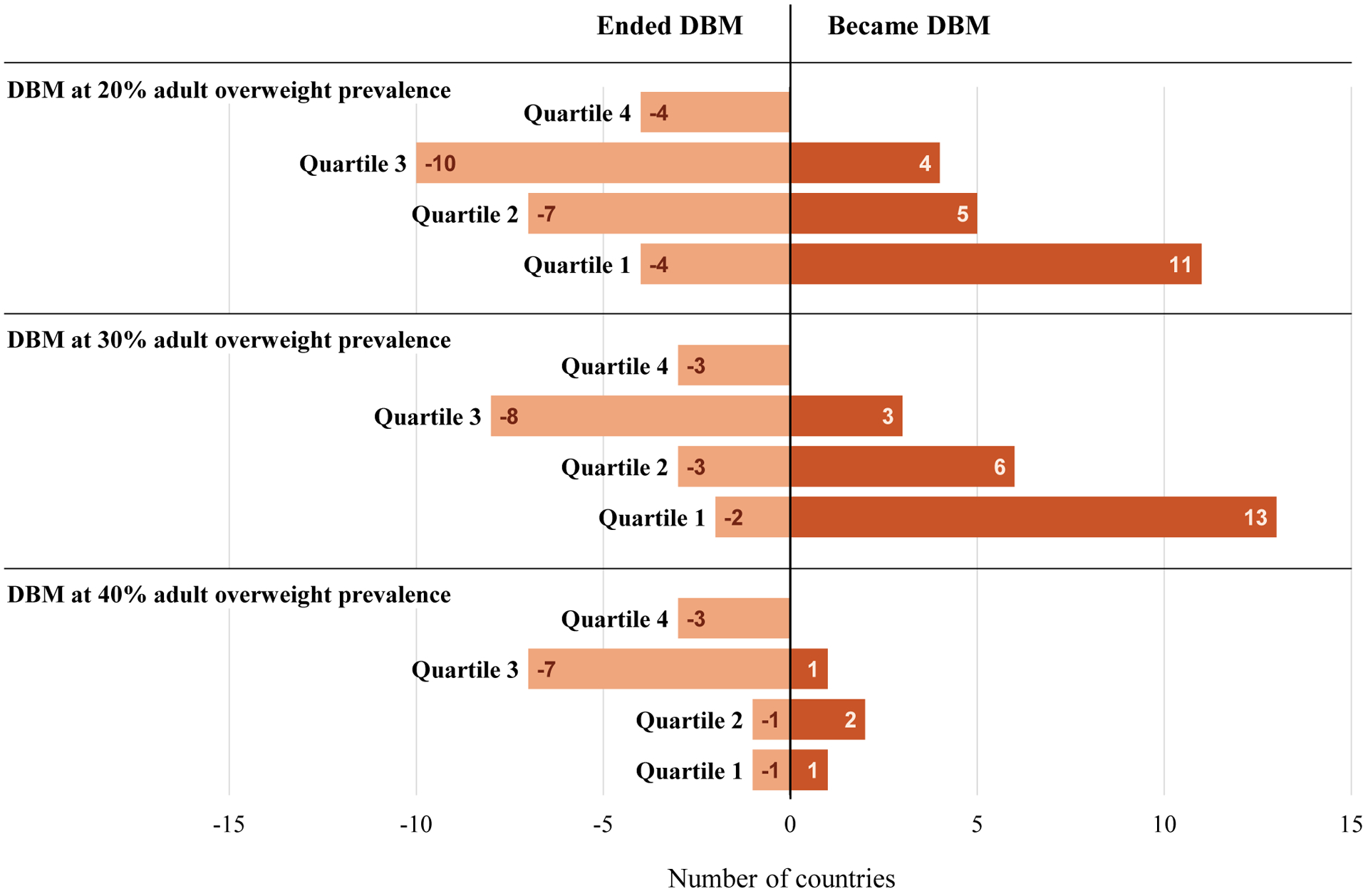
* Double burden of malnutrition (DBM) = at least 1 child, adolescent, or adult in household with severe levels of wasting/stunting/thinness and 1 with overweight/obesity(shown at 20%, 30%, or 40% adult overweight prevalence); countries only included here if they had DBM data available for bothtime periods (1990s and 2010s)
** Quartile (Qtl) 1 is lowest-wealth, Qtl4 is highest-wealth
Data sources: Based on UNICEF, WHO, World Bank, and NCD-RisCestimates supplemented with selected DHS and other country direct measures for the 1990’s
Household-level double burden
DBM at the household level was defined as one or more individuals with wasting/stunting/thinness and one or more individuals with overweight/obesity within the same household. It can occur in one of four ways: 1) a child is both stunted and overweight; 2) the mother is overweight and one of her children under 5 is wasted; 3) the mother is overweight and one of her children under age five is stunted; or 4) the mother is thin and one of her children is overweight. Supplemental Table S4 shows the prevalence of each of these scenarios as well as the total prevalence of household DBM. Household-level DBM is driven primarily by the combination of women with overweight and children with stunting (highest prevalence of all four possible combinations in every country with the highest growth rate where increases are occurring). In contrast, the contribution of the fourth category of DBM (mother with thinness and child with overweight) is extremely small (less than 1% prevalence in most countries).
The prevalence of total household-level DBM ranges from <3 percent to nearly 35 percent, with over a quarter of households experiencing DBM in Azerbaijan, Guatemala, Egypt, Comoros, and Sao Tome and Principe. The total household-level DBM is shown in Supplemental Figure S1a for countries with at least two surveys more than 15 years apart. Comparing the earliest and latest surveys in these countries, five countries showed declining levels of DBM and 15 (including India, China, and Indonesia) showed increases (Supplemental Figure S1a and S1b).
Economic Development and DBM at the Household Level
In Supplemental Table S3–4, we see that the general shape of the GDP/capita and household level DBM relationship is similar in the two time periods examined (1990s and 2010s), with the highest levels of household DBM seen in the middle of the income range (Figure 4). However, the entire curve has shifted slightly upward (about 2–3 additional percentage points) in the most recent time period at all income levels.
Figure 4. The association between GDP-PPP and regressions relating GDP per capita to household double burden.
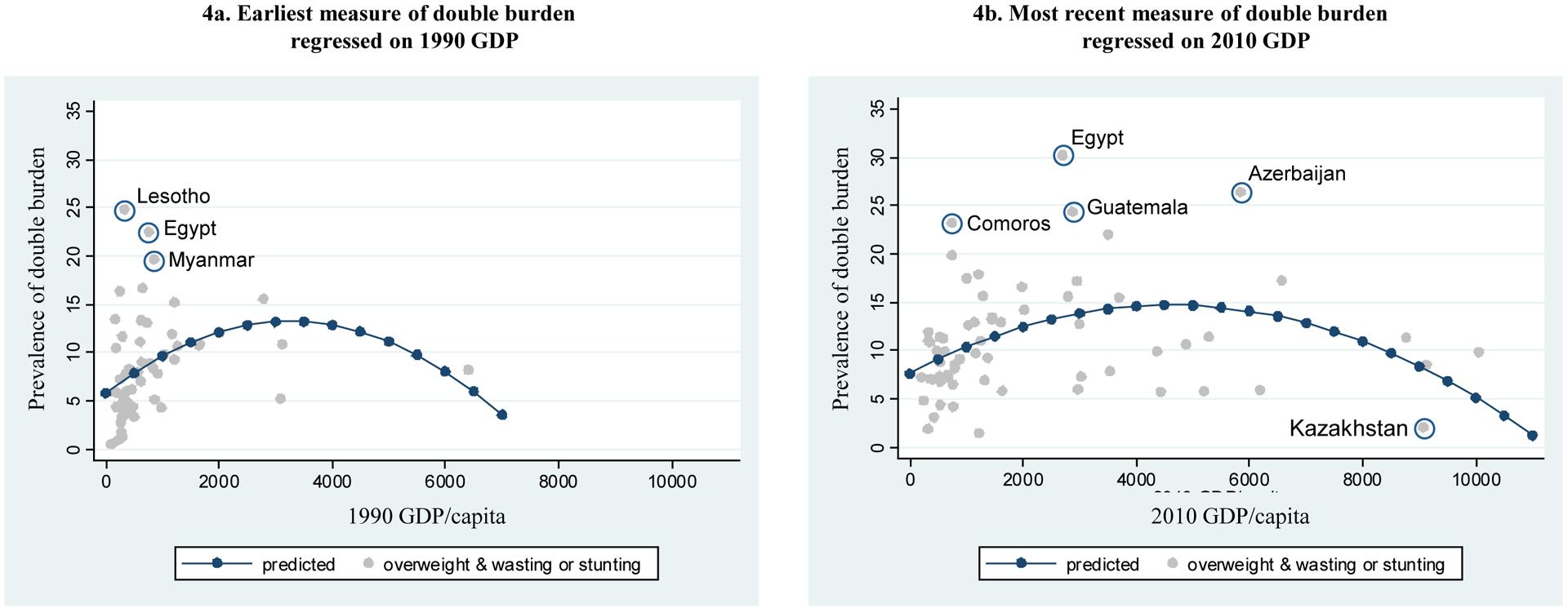
Sources: The data are from the Demographic and Health Surveys (DHS, https://dhsprogram.com/), with the exceptions of China (China Health and Nutrition Survey), Indonesia (Indonesian Family Life Survey), Mexico (Mexico National Survey of Health and Nutrition), Brazil (Brazil National Health Survey), and Vietnam (Vietnam Living Standards Survey).
Individual-level double burden
The Wells et al. paper addresses the underlying developmental origins biology that can lead to a child who has both stunting and overweight44. The prevalence of individual-level DBM for children ages 0–4 years is shown in Supplemental Table S4 and Supplemental Figure S1c. The percent of children who have both stunting and overweight ranges from <1% in Myanmar, Colombia, and Nepal to >15% in Albania. Among the 20 countries with earliest-to-latest-year data spanning 15 or more years, about half showed a decline in individual child DBM and half showed an increase (Supplemental Figure S1d).
Changes in malnutrition over time: equity considerations
Nearly all countries saw declines in child wasting or stunting, with a third of them declining by more than one percentage point per year (Supplemental Table S5). On the other hand, nearly all countries saw an increase in overweight among women, with over a third of countries increasing by more than one percentage point per year (Supplemental Table S6).
From a public health perspective, it is important to know where this overweight is emerging and whether the burden is now, or in the future, greater among the poor. To provide some sensitivity to where increased overweight is occurring, we looked at the prevalence and annualized changes in prevalence in all countries with two years of anthropometric data and we examined the differences in the changes in overweight/obesity prevalence between the poorest and the highest-wealth quintiles in the earliest and most recent survey periods (Figure 5). A positive annualized difference indicates that the poor face greater overweight/obesity prevalence and suggests increasing disparities between the lowest and the highest wealth quintiles. (See Supplemental Table S7 for the data and Appendix 1 for the methodology.) We show growing rates of overweight/obesity among the poor in most countries in LAC, EECA, and East Asia (led by China and Indonesia). In contrast, sub-Saharan Africa and South Asia have the largest increases in overweight/obesity prevalence among higher-wealth households (Supplemental Table S7). We cannot predict with extant data if these regions will see a shift toward greater overweight among the poor in the future. A recent study shows that in all low and middle income countries other than South Asia and sub-Saharan Africa, rural overweight and obesity is growing faster than in urban areas and also highlights the need for shared solutions targeted to both urban and rural areas.45
Figure 5. The shifting burden of overweight/obesity from higher- to lower-wealth populations in sample countries**.
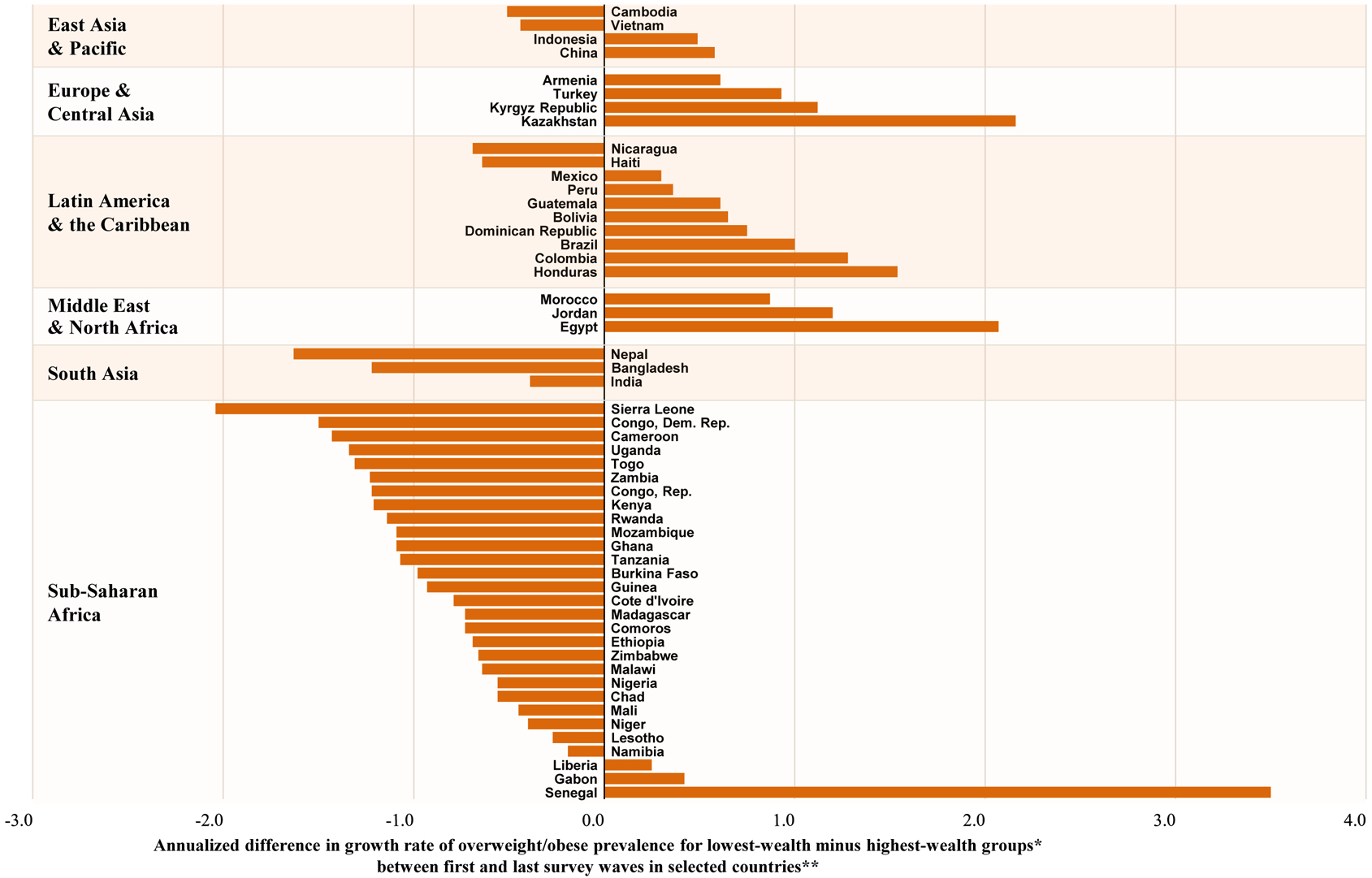
* Positive difference indicates higher annualized growth in overweight/obesity prevalence for the lowest-wealth quartile.
** Countries presented here had earliest-to-latest-year data spanning 15 or more years, latest-year data after 2010, and a population greater than ≈15 million (with the exception of Jordan andKyrgyz Republic, which both had smaller populations but were included for regional representation). The data presented is from years spanning 1988 to 2016, but exact years vary by country.The span of earliest-to-latest years collected ranges from 15 years to 24 years. All data are from the Demographic and Health Surveys (DHS, https://dhsprogram.com/) with the exceptions ofChina (China Health and Nutrition Survey), Indonesia (Indonesian Family Life Survey), Mexico (Mexico National Survey of Health and Nutrition), Brazil (Brazil National Health Survey), andVietnam (Vietnam Living Standards Survey).
The next section explores the global food systems linked with a new nutrition reality now affecting even the poorest LMICs.
PART 2: TRANSITIONS THAT EXPLAIN THE CURRENT SHIFTS IN THE DOUBLE BURDEN TOWARD THE LOWER INCOME COUNTRIES
We found that all the new DBM countries (14) were among the lowest quartile GDP/capita (PPP). At the same time, the number of countries in the upper income quartiles with DBM decreased. This reflects increasing overweight among lower-income countries that have not reduced stunting or wasting or thinness below the WHO-UNICEF cutoff levels. We focus the following discussion on the changing food system and new nutrition reality that these poorest LMICs are facing.
Economic change certainly has been critical to both the reductions in wasting/stunting/thinness as well as declines in physical activity and major shifts in the food system that have resulted in an increase in ultra-processed foods consumption.16,20,21,46–51 In longitudinal studies in China, the increases in overweight were fueled by massive reduction in physical activity and most likely also in energy expenditure derived from the introduction of modern technology in market economic work, home production (e.g., rice cookers, refrigerators, stoves) and transportation systems.18–21,50,52 However, it is in the diets and the food systems of most LMICs where most of the recent change in energy imbalance that causes weight gain is focused. It is very difficult for example, to offset the effects of any ultra-processed food, e.g., a 355 ml bottle of sugar-sweetened beverage, as the consumer would be required to undertake a 1.5 mile walk or run for at least 15 minutes.5,48, 57, 61, 62 Thus, we discuss below mainly the shifts in the food system and diet changes overtime.15,48,66–68,40,41,43,60–63,18–21,64,65,53
We conceptualize the food system as the entire process from production to the consumer.54–56 This system includes the activities, infrastructure, and people involved in feeding the global population. Over the past several decades we have seen not only greater relative influence and power among the various actors who affect and direct production but also the penetration of modern food retailing and marketing throughout most LMICs. Here we touch on these dramatic changes only briefly. A more in-depth discussion of these changes can be found elsewhere16 and in more detail for LAC.56 These food system changes are clearly important for weight gain and overweight status but the literature on how these changes affect undernutrition is less clear and very understudied.
The general concept of the nutrition transition is that in each region of the world (not only countries but subregions within countries), a transformation in the way people eat, drink, and move at work, at home, in transport, and in leisure has affected the distribution of body composition and created nutritional problems.57,58 The transition has produced remarkable shifts in physical activity and diets in LMICs and a rapid increase in overweight, obesity, and nutritionrelated NCDs.20,21,50,52 As noted above, we only have suggestive information on ways this transition affects infant diets for those facing a high risk of stunting and wasting.47,49,51,59 We have no studies in recent years on the exact causes of country-level or even household-level DBM. But we will describe briefly a new nutrition reality that is rapidly becoming the major driver of overweight and obesity among lower income countries and also has unclear but increasing effects on undernutrition.
The new nutrition reality
The new nutrition reality is particularly important to acknowledge, because diet is an important driver of DBM.60,61 While we understand that changes in the last several decades in food marketing, access, and purchase of packaged processed foods have demarcated a new nutrition reality across the globe, this paper focuses on the impact on all LMICs while attempting to understand the effects on countries in different regions and with varying income levels.62–64 The growth in retail food62,65,66 and the control of the entire food chain in many countries by agribusinesses, food retailers, food manufacturers, and food service companies have changed markedly.56,67 This has been accompanied the increased consumption of ultra-processed food purchases in LMICs.68,69 Ultra-processed, packaged foods rich in refined carbohydrates, fat, sugar, and salt are relatively inexpensive and often ready to eat.70. Recent evidence suggests these ultra-processed foods play a major role in increased obesity and NCD’s. A randomized controlled trial conducted by a team at the U.S. National Institutes of Health showed that normalweight adults lost 0.9 kilograms in two weeks when fed a real food diet and gained 2.1 kilograms when fed a diet composed of ultra-processed foods, following a cross-over design.14 It is unclear from this study if it is the hyperpalatability of ultra-processed food or the much higher energy density of such foods. Additionally, two large European cohorts have recently shown a strong positive relation between ultra-processed foods and cardiovascular disease and all-cause mortality (Lawrence and Baker 2019; Rico-Campà et al. 2019; Srour et al. 2019). The role of ultra-processed foods on stunting remains less clear. though we would expect they are replacing nutrient-rich, energy dense foods.14,71,72 Intake of ultra-processed foods during the first thousand days is increasing and represent a newly emerging likely contributor of stunting,46–49,51,53,59,73 therefore perpetuating the DBM.
The retail revolution
The retail revolution, where fresh markets have increasingly disappeared, and large and small food retailers have replaced them, has swept the globe, as a series of studies by T. Reardon and others shows.62,63,65–67,74 In LAC, packaged processed food sales increased from about 10% of all food expenditures (both in cash and in-kind sales) in 1990 to 60% in 2000. The bulk of this increase appears to be in ultra-processed unhealthy foods and beverages. That growth continues in the Latin American and Caribbean region. with large increases in ultra-processed categories of foods and beverages56,65,75 Similar increases in the penetration of modern food retailer emerged at different rates across Asia, Africa, and the Middle East.66 The Persian Gulf states66 have not been studied as carefully, though we presume they experienced similar growth even earlier as the area urbanized and experienced rapid growth in incomes. The changes vary across sub-Saharan Africa, North Africa, East, Southeast, and South Asian countries but change is accelerating in most countries.62,63,76. which in urban areas was already dominated by a modern food retail sector in the mid-1990s, most growth in the African market has occurred in the twenty-first century.64
Controlling the food supply
The actors who control the food supply are changing. At the time of the green revolution and the development of the global agricultural research sector, countries, large agribusiness firms in the seed and fertilizer area and global foundations generated the change.54,56,67,74,75,77 While they still play major roles in producing new technology, control of the food chain is transforming. Case studies from China, Bangladesh, and India were the first to remark on this67 and later research showed similar trends in Africa.63 These studies showed that the global and national public sectors were no longer the major influences in LMIC diets. Rather, food retailers, food agribusinesses, global food companies, and the food service sector and their domestic cloned counterparts directly impacted farmers.
Nonessential foods and beverages
Sales of nonessential foods and beverages are growing rapidly. Sales volume data from Euromonitor International demonstrates trends in increasing sales of nonessential or junk foods and SSBs in Chile, South Africa, the Philippines, and Malaysia (Supplemental Figure S2).78 Supplemental Tables S8 and S9 present the sales data from Euromonitor International used to model the GDP relationship with both sales volumes and annualized changes in sales of SSBs (Supplemental Figure S3) and junk foods (Supplemental Figure S4) in LMICs using data regressions.78 These results show how large SSB sales already were in lower-income countries by 2017. The rapid growth of junk foods and SSBs in these countries exemplifies how aggressive this food sector is. India and China are two of the top five markets for sugary beverage manufacturers (Supplemental Figures S5 and S6) and are expected to become their major markets in the next decade. The speed of change is particularly important in understanding how this nutrition reality is shifting.
Key drivers of the new nutrition reality
In LMICs urbanization, migration to cities, income growth, infrastructure improvements, and global trade policy liberalization have spurred private investment in the food sector.56,63,74,77 The roles of income growth79 and other drivers associated with diet changes should not be downplayed. Equally important, women working outside the home56,80 and their opportunity costs of time have shaped the demand for food that is ready to eat or ready to heat.81 C.A. Monteiro calls this convenience in food preparation and consumption the ultra-processed food revolution.68,69 Modern marketing and access to mass media have added to changes in conceptions of the ideal set of foods. But while power is shifting to large-scale food retailers, manufacturers, and food service companies,56,67 the informal sector and smaller local companies remain understudied components of the food sector who are often important sources of food for low-income and rural populations.
CONCLUSION
This paper has shown that LMICs countries continue to experience high levels of DBM; however, those countries with the current higher levels of DBM are lower income levels than in the early 1990s. The analysis of the dynamics of undernutrition and obesity suggest that it is the rapid increases in prevalence of overweight/obesity occurring in these lower income countries which are also experiencing a slower decline in the prevalence of undernutrition. A greater number of new countries with high levels of DBM were in the lowest GNP/capita (PPP) quartile of LMICs than in the 1990’s. We show that this new nutrition reality is driven by important and rapid changes that have taken place in the food system. Conversion of the global and domestic retail food, food service, and agribusiness sectors of the economy, along with other transformations,55,56,63,67 have resulted in an important increased availability of ultra-processed foods in LMICs. Ultra-processed food consumption has been linked to overweight/obesity and NCDs risk and there is preliminary evidence that its consumption during the first 1,000 period (pregnancy and infancy) early-life window could be also linked to stunting. There is an urgent need for understanding and tackling the drivers of the food system shift and enacting effective policies that address the challenges of the DBM.48,67,71,78
Supplementary Material
Supplemental Table S1. Country burdens by age, sex, and region in 1990s UNICEF and NCD-RisC surveys with DHS for preschoolers where gaps existed
Supplemental Table S2. Country burdens by age, sex, and region in 2010s UNICEF and NCD-RisC surveys
Supplemental Table S3. Number of households with children and women, mean age for women, and GDP per capita (PPP) by country for earliest and latest survey years
Supplemental Table S4. Prevalence of household double burdens for children with underweight (ages 0–4) and women with overweight (ages 15–49 years) and annualized change in prevalence from earliest to latest survey years
Supplemental Table S5. Prevalence of wasting, stunting, and overweight or obesity for children (ages 0–4 years) and annualized change in prevalence from earliest to latest survey years
Supplemental Table S6. Prevalence of thinness and overweight for women (ages 15–49 years) and annualized change in prevalence from earliest to latest survey years
Supplemental Table S7. Prevalence of overweight and obesity for lowest and highest wealth quintiles, differences in the earliest and latest years, and annualized changes in disparity
Supplemental Table S8. Total estimated sales volumes and annualized change in sales volumes of sugar-sweetened beverages, 2004 to 2017
Supplemental Table S9. Total estimated sales volumes and annualized change in sales volumes of nonessential junk foods, 2004 to 2017
Supplemental Figure S1. Changes in nationally representative prevalence of individual preschooler and household double burden from selected countries’ earliest to latest survey years, weighted by 2010 populations
Supplemental Figure S1a. Total double burden: Overweight in woman or child + wasting or stunting in child or thinness in woman
Supplemental Figure S1b. Annualized change in overweight in woman or child + wasting or stunting in child or thinness in woman
Supplemental Figure S1c. Overweight + stunting in single child
Supplemental Figure S1d. Annualized Change in overweight + stunting in single child
Supplemental Figure S2. Trends in estimated total SSB and junk food sales volumes, 2004–2017
Supplemental Figure S3. Regressions of global trends in estimated total SSB sales in LMICs
Supplemental Figure S3a. Annualized change in SSB sales, 2004–2017
Supplemental Figure S3b. 2017 SSB sales
Supplemental Figure S4. Regressions of global trends in estimated total junk food sales in LMICs
Supplemental Figure S4a. Annualized change in junk food sales, 2004–2017
Supplemental Figure S4b. 2017 junk food sales
Supplemental Figure S5. Trends in estimated total SSB and junk food sales and restaurant banner sales in China
Supplemental Figure S5a. Trends in estimated total retail + foodservice sales volumes for SSBs and junk foods, 2004–2017
Supplemental Figure S5b. Trends in total banner sales from quick-service, café, and full-service restaurant retailers, 2006–2017
Supplemental Figure S6. Trends in estimated total SSB and junk food sales and restaurant banner sales in India
Supplemental Figure S6a. Trends in estimated total retail + foodservice sales volumes for SSBs and junk foods, 2004–2017
Supplemental Figure S6b. Trends in total banner sales from quick-service, café, and full-service restaurant retailers, 2006–2017
Key messages:
In low- and middle-income countries (LMICs), stunting, wasting and thinness in women are declining while overweight increases in most age groups. A total of 48, 35, or 10 countries presented severe levels of double burden of malnutrition (DBM; wasting >15% or stunting > 30%, women’s thinness (and women’s thinness(BMI< 18.5 >20%)and adult or child overweight(>20, 30, 40%) according to most recent survey years.
Severe levels of the DBM shifted to the countries in the poorest income quartile. Whereas several decades ago, the double burden was typically seen more in the higher-income LMICs, today it predominates in countries with much lower gross domestic products per capita, particularly in South and East Asia and sub-Saharan Africa.
Increases in overweight are the results of changes in the global food system that make less nutritious food cheaper and more accessible while physical activity is decreasing due to major technological shifts in market, home production and transportation. In South Asia and Sub-Saharan Africa countries, the risk of overweight/obesity is greater among the higher wealth households and urban areas while in many other LMICs the risk is starting to concentrate among low-income people and rural areas.
LMICs face a new nutrition reality. The shifts in the global food system are accelerating increases in overweight. Concurrently these same shifts have changed the diet of infants and pre-schoolers but the impact on stunting needs further research. LMICs need to implement interventions to improve diet quality in order to address under- and overnutrition across the lifecycle.
Acknowledgments:
Thanks to Karen Ritter and Emily Busey for great programming, research, and graphics support and Frances Burton for administrative support and Francesco Branco and the authors of the DBM series for suggestions. Funding is from the National Institutes of Health (R01DK108148 and P2C HD050924), and the and the World Health Organization, through a grant from the Bill and Melinda Gates Foundation. The providers of the grants had no direct role in the study design, analysis, interpretation of the evidence or manuscript preparation nor in the decision to submit for publication. None of the authors have conflicts of interest of any type with respect to this manuscript.
Funding:
The World Health Organization, and the National Institutes of Health (R01DK108148 and P2C HD050924).
Acronyms
- GDP/cap (PPP)
gross domestic product per capita based on purchasing power parity
- PPP
purchasing power parity
- LAC
Latin America and the Caribbean
- MENA
Middle East and North Africa
- EECA
Eastern Europe and Central Asia
- LMICs
low- and middle-income countries
- SSBs
sugar-sweetened beverages
- DBM
double burden of malnutrition
- SES
socioeconomic status
- NCDs
noncommunicable diseases
- WHO
World Health Organization
- UNICEF
United Nations Children’s Fund
- NCD-RisC
Non-communicable Disease Risk Factor Collaboration (generated the data found on the Institute of Health Metrics and Evaluation website)
- DHS
Demographic and Health Surveys
Footnotes
Declaration of interest of the authors: None.
REFERENCES
- 1.World Health Organization. Obesity and overweight Factsheet. 2016. http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed May 1 2017).
- 2.International Food Policy Research Institute. 2017 Global Food Policy Report. Washington, DC: International Food Policy Research Institute (IFPRI), 2017. [Google Scholar]
- 3.FAO, IFAD, UNICEF, WFP, WHO. The State of Food Security and Nutrition in the World 2018: Building climate resilience for food security and nutrition. Rome: Food and Agricultural Organization; 2018. p. 182. [Google Scholar]
- 4.Doak CM, Adair LS, Bentley M, Monteiro C, Popkin BM. The dual burden household and the nutrition transition paradox. Int J Obes 2005; 29(1): 129–36. [DOI] [PubMed] [Google Scholar]
- 5.Doak CM, Adair LS, Monteiro C, Popkin BM. Overweight and underweight coexist within households in Brazil, China and Russia. J Nutr 2000; 130(12): 2965–71. [DOI] [PubMed] [Google Scholar]
- 6.Garrett J, Ruel M. Stunted child-overweight mother pairs: Prevalence and association with economic development and urbanization. Food Nutr Bull 2005; 26(2): 209–21. [DOI] [PubMed] [Google Scholar]
- 7.Victora CG, Rivera J. Optimal child growth and the double burden of malnutrition: research and programmatic implications. Am J Clin Nutr 2014; 100(6): 1611S–2S. [DOI] [PubMed] [Google Scholar]
- 8.Rivera JA, Pedraza LS, Martorell R, Gil A. Introduction to the double burden of undernutrition and excess weight in Latin America. Am J Clin Nutr 2014; 100(6): 1613S–6S. [DOI] [PubMed] [Google Scholar]
- 9.Kroker-Lobos MF, Pedroza-Tobías A, Pedraza LS, Rivera JA. The double burden of undernutrition and excess body weight in Mexico. A J Clin Nutr 2014; 100(6): 1652S–8S. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Double-duty actions for nutrition: policy brief. In: Nutrition, editor. Geneva: WHO; 2017. p. 10. [Google Scholar]
- 11.Hawkes C, Demaio AR, Branca F. Double-duty actions for ending malnutrition within a decade. The Lancet Global Health 2017. [DOI] [PubMed] [Google Scholar]
- 12.Tzioumis E, Adair LS. Childhood dual burden of under- and overnutrition in low- and middle-income countries: A critical review. Food Nutr Bull 2014; 35(2): 230–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Global Nutrition Report independent expert group. 2018 Global Nutrition Report: Shining a light to spur action on nutrition. 2018. p. 166.
- 14.Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: A one-month inpatient randomized controlled trial of ad libitum food intake. Cell Matab 2019. 30(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Popkin BM. Nutrition, agriculture and the global food system in low and middle income countries. Food Policy 2014; 47: 91–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Popkin BM. Relationship between shifts in food system dynamics and acceleration of the global nutrition transition. Nutr Rev 2017; 75(2): 73–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Popkin BM, Reardon T. Obesity and the food system transformation in Latin America. Obes Rev 2018; 19(8): 1028–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Monda KL, Adair LS, Zhai F, Popkin BM. Longitudinal relationships between occupational and domestic physical activity patterns and body weight in China. Eur J Clin Nutr 2008; 62: 1318–25. [DOI] [PubMed] [Google Scholar]
- 19.Monda KL, Popkin BM. Cluster analysis methods help to clarify the activity-BMI relationship of Chinese youth. Obes Res 2005; 13(6): 1042–51. [DOI] [PubMed] [Google Scholar]
- 20.Ng SW, Norton EC, Guilkey DK, Popkin BM. Estimation of a dynamic model of weight. Empirical Econ 2012; 42(2): 413–43. [Google Scholar]
- 21.Ng SW, Popkin BM. Time use and physical activity: a shift away from movement across the globe. Obes Rev 2012; 13(8): 659–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Springmann M, Clark M, Mason-D’Croz D, et al. Options for keeping the food system within environmental limits. Nature 2018; 562(7728): 519–25. [DOI] [PubMed] [Google Scholar]
- 23.Swinburn BA, Kraak VI, Allender S, et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. The Lancet 2019; 393(10173): 791–846. [DOI] [PubMed] [Google Scholar]
- 24.Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT–Lancet Commission on healthy diets from sustainable food systems. The Lancet 2019; 393(10170): 447–92. [DOI] [PubMed] [Google Scholar]
- 25.Wells J, Wibaek R, Poullas M. The dual burden of malnutrition increases the risk of cesarean delivery: evidence from India. Front Public Health 2018; 6: 292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adair LS, Fall CH, Osmond C, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet 2013; 382(9891): 525–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stein AD, Wang M, Martorell R, et al. Growth patterns in early childhood and final attained stature: data from five birth cohorts from low- and middle-income countries. Am J Hum Biol 2010; 22(3): 353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008; 371(9609): 340–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wells J, Sawaya A, Wibaek R, et al. Emerging biological pathways in the double burden of malnutrition. The Lancet In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. United Nations Decade of Action. 2016. http://www.who.int/nutrition/decade-of-action/en/ (accessed March 1 2019).
- 31.Nilsson M, Griggs D, Visbeck M. Policy: map the interactions between Sustainable evelopment Goals. Nature News 2016; 534(7607): 320–2. [DOI] [PubMed] [Google Scholar]
- 32.United Nations Children’s Fund. Implementing taxes on sugar-sweetened beverages: An overview of current approaches and the potential benefits for children. 2019. https://scalingupnutrition.org/news/implementing-taxes-on-sugar-sweetened-beverages-anoverview-of-current-approaches/ (accessed March 19 2019).
- 33.Wells JC, Wibaek R, Poullas M. The Dual Burden of Malnutrition Increases the Risk of Cesarean Delivery: Evidence From India. Frontiers in Public Health 2018; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hawkes C, Ruel M, Salms L, Sinclair B, Bazán K, Branca F. Double-duty actions: seizing program and policy opportunities to address malnutrition in all its forms. The Lancet 2019. [DOI] [PubMed] [Google Scholar]
- 35.Nugent R, Levin C, Hale J, Hutchison B. Economic impacts of the double burden of malnutrition. The Lancet 2019. [DOI] [PubMed] [Google Scholar]
- 36.de Onis M, Borghi E, Arimond M, et al. Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Health Nutr 2018; 22(1): 175–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Colin Bell A, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol 2002; 155(4): 346–53. [DOI] [PubMed] [Google Scholar]
- 38.Albrecht SS, Mayer-Davis E, Popkin BM. Secular and race/ethnic trends in glycemic outcomes by BMI in US adults: the role of waist circumference. Diabetes Metab Res Rev 2017; 33(5). [DOI] [PubMed] [Google Scholar]
- 39.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004; 363(9403): 157–63. [DOI] [PubMed] [Google Scholar]
- 40.Wells JC, Pomeroy E, Walimbe SR, Popkin BM, Yajnik CS. The elevated susceptibility to diabetes in India: an evolutionary perspective. Front Public Health 2016; 4(145). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Misra A Ethnic-specific criteria for classification of body mass index: a perspective for Asian Indians and American Diabetes Association position statement. Diabetes Technol Ther 2015; 17(9): 667–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nair M, Prabhakaran D. Why do South Asians have high risk for CAD? Global Heart 2012; 7(4): 307–14. [DOI] [PubMed] [Google Scholar]
- 43.Joshi P, Islam S, Pais P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007; 297(3): 286–94. [DOI] [PubMed] [Google Scholar]
- 44.Wells JC, Sawaya A, Wibeak R, et al. The double burden of malnutrition: etiological pathways and consequences for health. The Lancet 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.NCD Risk Factor Collaboration Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature 2019; 569(7755): 260–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pries AM, Huffman SL, Mengkheang K, et al. Pervasive promotion of breastmilk substitutes in Phnom Penh, Cambodia, and high usage by mothers for infant and young child feeding. Matern Child Nutr 2016; 12: 38–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pries AM, Huffman SL, Mengkheang K, et al. High use of commercial food products among infants and young children and promotions for these products in Cambodia. Matern Child Nutr 2016; 12(Suppl 2): 52–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vitta BS, Benjamin M, Pries AM, Champeny M, Zehner E, Huffman SL. Infant and young child feeding practices among children under 2 years of age and maternal exposure to infant and young child feeding messages and promotions in Dar es Salaam, Tanzania. Matern Child Nutr 2016; 12(Suppl 2): 77–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huffman SL, Piwoz EG, Vosti SA, Dewey KG. Babies, soft drinks and snacks: a concern in low- and middle-income countries? Matern Child Nutr 2014; 10(4): 562–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bell A, Ge K, Popkin B. Weight gain and its predictors in Chinese adults. Int J Obes Relat Metab Disord 2001; 25(7): 1079–86. [DOI] [PubMed] [Google Scholar]
- 51.Pries A, Filteau S, Ferguson E. Snack food and beverage consumption and young child nutrition in low- and middle-income countries: a systematic review. Matern Child Nutr 2019; 15(S4): e12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bell AC, Ge K, Popkin BM. The road to obesity or the path to prevention: motorized transportation and obesity in China. Obes Res 2002; 10(4): 277–83. [DOI] [PubMed] [Google Scholar]
- 53.Pries AM, Rehman AM, Filteau S, Sharma N, Upadhyay A, Ferguson EL. Unhealthy snack food and beverage consumption is associated with lower dietary adequacy and length-forage z-scores among 12–23-month-olds in Kathmandu Valley, Nepal. J Nutr 2019; pii: nxz140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Anand SS, Hawkes C, de Souza RJ, et al. Food consumption and its impact on cardiovascular disease: Importance of solutions focused on the globalized food system: A report from the workshop convened by the World Heart Federation. J Am Coll Cardiol 2015; 66(14): 1590–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reardon T, Timmer CP. The economics of the food system revolution. Ann Rev Resource Econ 2012; 4(1): 225–64. [Google Scholar]
- 56.Popkin BM, Reardon T. Obesity and the food system transformation in Latin America. Obes Rev 2018. 19(8): 1028–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Popkin BM. The shift in stages of the nutrition transition in the developing world differs from past experiences! Public Health Nutr 2002; 5(1A): 205–14. [DOI] [PubMed] [Google Scholar]
- 58.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev 2012; 70(1): 3–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pries AM, Huffman SL, Adhikary I, et al. High consumption of commercial food products among children less than 24 months of age and product promotion in Kathmandu Valley, Nepal. Matern Child Nutr 2016; 12(Suppl 2): 22–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 2015; 386(10010): 2287–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. The Lancet 2013; 371(9608): 243–60. [DOI] [PubMed] [Google Scholar]
- 62.Reardon T, Timmer CP, Minten B. Supermarket revolution in Asia and emerging development strategies to include small farmers. Proc Natl Acad Sci USA 2012; 109(31): 12332–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Reardon T, Tschirley D, Minten B, et al. Transformation of African agrifood systems in the new era of rapid urbanization and the emergence of a middle class In: Badiane O, Makombe T, editors. ReSAKSS Annual Conference “Beyond a Middle Income Africa”, Transforming African Economies for Sustained Growth with Rising Employment and Incomes; 2015; Addis Ababa, Ethiopia; 2015. [Google Scholar]
- 64.Tschirley D, Reardon T, Dolislager M, Snyder J. The rise of a middle class in East and Southern Africa: Implications for food system transformation. J Int Dev 2015; 27(5): 628–46. [Google Scholar]
- 65.Reardon T, Berdegué JA. The rapid rise of supermarkets in Latin America: challenges and opportunities for development. Dev Policy Rev 2002; 20(4): 371–88. [Google Scholar]
- 66.Reardon T, Timmer CP, Barrett CB, Berdegue JA. The rise of supermarkets in Africa, Asia, and Latin America. Am J Agri Econ 2003; 85(5): 1140–6. [Google Scholar]
- 67.Reardon T, Chen KZ, Minten B, et al. The quiet revolution in Asia’s rice value chains. Annals NY Acad Sci 2014; 1331(1): 106–18. [DOI] [PubMed] [Google Scholar]
- 68.Monteiro CA, Levy RB, Claro RM, de Castro IR, Cannon G. Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr 2011; 14(1): 5–13. [DOI] [PubMed] [Google Scholar]
- 69.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev 2013; 14(S2): 21–8. [DOI] [PubMed] [Google Scholar]
- 70.Poti JM, Mendez MA, Ng SW, Popkin BM. Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am J Clin Nutr 2015; 99(1): 162–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ 2019; 365: l1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rico-Campà A, Martínez-González MA, Alvarez-Alvarez I, et al. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ 2019; 365: l1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Feeley AB, Ndeye Coly A, Sy Gueye NY, et al. Promotion and consumption of commercially produced foods among children: situation analysis in an urban setting in Senegal. Matern Child Nutr 2016; 12(S2): 64–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Reardon T, Barrett CB, Berdegué JA, Swinnen JFM. Agrifood industry transformation and small farmers in developing countries. World Dev 2009; 37(11): 1717–27. [Google Scholar]
- 75.Reardon TA, Berdegué JA, Farrington J. Supermarkets and farming in Latin America: pointing directions for elsewhere?: Overseas Development Institute; 2002. [Google Scholar]
- 76.Hu D, Reardon T, Rozelle S, Timmer P, Wang H. The emergence of supermarkets with Chinese characteristics: challenges and opportunities for China’s agricultural development. Dev Policy Rev 2004; 22: 557–86. [Google Scholar]
- 77.Neven D, Odera MM, Reardon T, Wang H. Kenyan supermarkets, emerging middle-class horticultural farmers, and employment impacts on the rural poor. World Dev 2009; 37(11): 1802–11. [Google Scholar]
- 78.Euromonitor. Market Sizes- Historical- Total Volume- Kilograms or litres per capita-Packaged Food, Soft Drinks, and Hot Drinks. [Statistics] Euromonitor Passport International London, United Kingdom: Euromonitor; 2018. [Google Scholar]
- 79.Bennett M The World’s Food. New York: Harper & Brothers; 1954. [Google Scholar]
- 80.Novta N, Wong J. Women at work in Latin America and the Caribbean. International Monetary Fund; Washington; 2017. [Google Scholar]
- 81.Mincer J Market prices, opportunity costs, and income effects In: Christ CF, Friedman M, Goodman LA, et al. , eds. Measurement in economics: studies in mathematical economics and econometrics in memory of Yehuda Grunfeld. Stanford, CA: Stanford University Press; 1963. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table S1. Country burdens by age, sex, and region in 1990s UNICEF and NCD-RisC surveys with DHS for preschoolers where gaps existed
Supplemental Table S2. Country burdens by age, sex, and region in 2010s UNICEF and NCD-RisC surveys
Supplemental Table S3. Number of households with children and women, mean age for women, and GDP per capita (PPP) by country for earliest and latest survey years
Supplemental Table S4. Prevalence of household double burdens for children with underweight (ages 0–4) and women with overweight (ages 15–49 years) and annualized change in prevalence from earliest to latest survey years
Supplemental Table S5. Prevalence of wasting, stunting, and overweight or obesity for children (ages 0–4 years) and annualized change in prevalence from earliest to latest survey years
Supplemental Table S6. Prevalence of thinness and overweight for women (ages 15–49 years) and annualized change in prevalence from earliest to latest survey years
Supplemental Table S7. Prevalence of overweight and obesity for lowest and highest wealth quintiles, differences in the earliest and latest years, and annualized changes in disparity
Supplemental Table S8. Total estimated sales volumes and annualized change in sales volumes of sugar-sweetened beverages, 2004 to 2017
Supplemental Table S9. Total estimated sales volumes and annualized change in sales volumes of nonessential junk foods, 2004 to 2017
Supplemental Figure S1. Changes in nationally representative prevalence of individual preschooler and household double burden from selected countries’ earliest to latest survey years, weighted by 2010 populations
Supplemental Figure S1a. Total double burden: Overweight in woman or child + wasting or stunting in child or thinness in woman
Supplemental Figure S1b. Annualized change in overweight in woman or child + wasting or stunting in child or thinness in woman
Supplemental Figure S1c. Overweight + stunting in single child
Supplemental Figure S1d. Annualized Change in overweight + stunting in single child
Supplemental Figure S2. Trends in estimated total SSB and junk food sales volumes, 2004–2017
Supplemental Figure S3. Regressions of global trends in estimated total SSB sales in LMICs
Supplemental Figure S3a. Annualized change in SSB sales, 2004–2017
Supplemental Figure S3b. 2017 SSB sales
Supplemental Figure S4. Regressions of global trends in estimated total junk food sales in LMICs
Supplemental Figure S4a. Annualized change in junk food sales, 2004–2017
Supplemental Figure S4b. 2017 junk food sales
Supplemental Figure S5. Trends in estimated total SSB and junk food sales and restaurant banner sales in China
Supplemental Figure S5a. Trends in estimated total retail + foodservice sales volumes for SSBs and junk foods, 2004–2017
Supplemental Figure S5b. Trends in total banner sales from quick-service, café, and full-service restaurant retailers, 2006–2017
Supplemental Figure S6. Trends in estimated total SSB and junk food sales and restaurant banner sales in India
Supplemental Figure S6a. Trends in estimated total retail + foodservice sales volumes for SSBs and junk foods, 2004–2017
Supplemental Figure S6b. Trends in total banner sales from quick-service, café, and full-service restaurant retailers, 2006–2017


