Abstract
Background and Aims:
The Ultrasound (USG)-guided internal jugular vein (IJV) cannulation can be performed using different approaches like short axis (SAX), long axis (LAX), oblique axis (OAX) or medial oblique axis (M-OAX). We aimed to determine which view was optimal for IJV cannulation.
Methods:
After ethical committee approval and written informed consent, this prospective, randomised, controlled trial was conducted on 108 patients. Patients were allocated into one of the three groups: A (SAX), B (LAX) and C (M-OAX approach) for USG-guided IJV cannulation. The number of needle passes, the success of IJV cannulation and its diameter, venous access time, guidewire time, catheterisation time and complications if any were recorded. Statistical analysis was performed by SPSS version 17.0.
Results:
First needle pass success rate was highest in M-OAX (97.2%) followed by SAX (88.9%) and then LAX (77.8%) but it was statistically insignificant among the groups. Mean venous access, guidewire insertion and catheterisation time were shortest in M-OAX followed by SAX and then LAX approach. It was statistically significant between LAX and SAX and between LAX and M-OAX group. (P < 0.001). The carotid puncture was noticed in two patients in the LAX group. The overall success rate and the number of needle passes were comparable among the groups.
Conclusion:
The M-OAX approach is a safe and effective technique for USG-guided IJV cannulation when compared to SAX and LAX approaches.
Key words: Internal jugular vein cannulation, long axis, medial oblique axis, short axis, ultrasound
INTRODUCTION
Internal jugular venous (IJV) cannulation is the most commonly performed central venous cannulation procedure both in the perioperative period and critical care settings.[1] The use of the ultrasound for IJV access provides quick, safe and reliable guidance for needle placement in elective routine and difficult cases. It also results in a higher proportion of successful cannulations on the first attempt with a shorter average time for cannulation and reductions in mechanical complications when compared to the landmark approach.[2]
Ultrasound (USG)-guided IJV cannulation can be performed using different approaches like short axis (SAX), long axis (LAX), combination of short and long axes (SAX to start off with, followed by rotation to LAX to visualise needle entry into vein), oblique axis (OAX) or medial oblique axis (M-OAX).[3,4] Each of the techniques has its own advantages and disadvantages.
There are limited studies in the literature comparing different approaches for USG-guided IJV cannulation and as to which scanning axis provides optimal conditions for vascular access.[3,4,5,6] Therefore, we conducted this study to compare three approaches viz SAX, LAX and M-OAX for USG-guided IJV cannulation. The purpose of this study was to assess and compare the performance of these approaches (SAX, LAX and M-OAX) in terms of successful cannulation on first needle pass and overall success rate. The diameter of IJV, number of needle passes, venous access time (VAT), guidewire time, catheterisation time and complications if any were observed as secondary objectives.
METHODS
This prospective, randomised, controlled trial was conducted after obtaining institutional ethics committee (IEC) approval and registering the study with the Clinical Trials Registry of India (CTRI/2019/01/023696). The study was conducted between October 2017 and February 2019 in accordance with the principles of the Declaration of Helsinki. One hundred and eight patients of either sex of age 18 years or above scheduled for elective surgery or admitted in the intensive care unit (ICU) and requiring IJV cannulation were included in the study. Patients with signs of infection or subcutaneous hematoma at or close to the puncture site, history of IJV cannulation during the past 72 h at the same site, previous surgical interventions on the cannulation site, severe coagulopathy, recent cervical trauma with neck immobilisation, subcutaneous emphysema with cervical extension, thrombus in the IJV, inability to obtain formal informed consent from the patient/attendant were excluded from the study. Written informed consent was obtained from all participants after explaining the study. The enrolled patients were allocated into one of the three groups A, B and C using block randomisation method by taking block size as 9. Enrolment and allocation of the patients into the three groups was done by an anaesthesiologist not involved in USG-guided IJV cannulation. IJV cannulation was done using the SAX approach in group A, LAX approach in group B and M-OAX approach in group C.
After the establishment of an intravenous line and attachment of monitors for non-invasive blood pressure, electrocardiography and pulse oximetry in the operating room, general anaesthesia was induced. All intubated patients were placed in Trendelenburg position (20°–30°) with a rolled towel under the shoulders and the head turned to the opposite side for cannulation. All cannulations were done in right IJV with 7 F (15 cm) triple lumen catheter by an anaesthesiologist with experience of 50 or more USG-guided IJV cannulations. The procedure was performed by a Seldinger technique, using an 18 G, 7 cm introducer needle with a 5 ml syringe attached to it. The probe marker was oriented to patients' left side, corresponding marker on the screen. Adjustments were made to obtain optimal images to identify the IJV and the carotid artery and diameter of IJV were noted in the anteroposterior plane and then the vascular puncture was performed under ultrasound guidance, using a single person technique (with the same operator handling the transducer and the needle). A linear array high-frequency transducer 6-13 MHz attached to a 2D image display of the ultrasound machine (M- Turbo Sonosite, Japan) was used.
With SAX approach, the transducer was placed transversely over the neck (parallel and superior to the clavicle), and once the vein was visible in the middle of the ultrasound image the needle attached with a syringe was introduced at a 45° angle with gentle aspiration in a plane perpendicular to the LAX of the transducer. The needle tip was visualised as a white dot on the screen. With LAX, the transducer was placed longitudinally over the neck and once the vein was identified, the needle was inserted just underneath the footprint of the probe following its LAX from cranial to caudal. With M-OAX, a SAX view of the vein was obtained first and then the transducer was rotated 30° counterclockwise in a medial-cephalad to the lateral-caudad direction. The introducer needle was inserted directly at the proximal end of the ultrasound probe and the needle was advanced in a plane directed laterally toward ipsilateral nipple.
When the needle appeared to be in the vein as evidenced by ultrasound image and return of venous blood into the syringe, then a guidewire was placed through the needle into the vein by an assistant. Confirmation of the venous placement of guidewire was done by visualising guidewire in the lumen of the vein using an ultrasound probe, after which the needle was withdrawn. The guidewire was seen as a dot in the lumen of the vessel in SAX [Figure 1] whereas the path of the guidewire was visualised in long and M-OAX [Figures 2 and 3], ECG was continuously monitored for any arrhythmias. After identifying the guidewire inside the jugular vein using ultrasound, the Seldinger technique was continued until catheter insertion. After the catheter was fixed in place, a chest X-ray was conducted to verify the correct catheter tip position and check for other mechanical complications.
Figure 1.
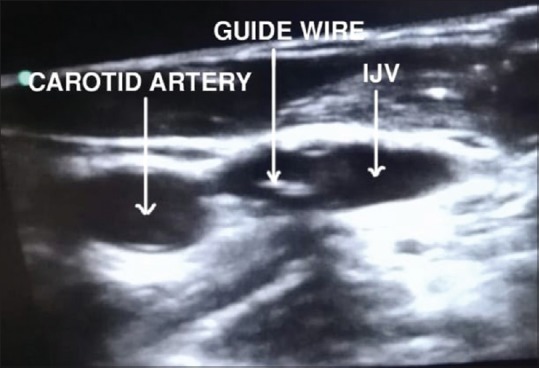
Short axis approach with guidewire seen as white dot
Figure 2.
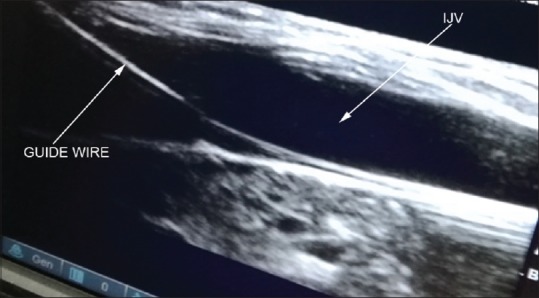
Long axis approach showing guidewire seen as a bright line
Figure 3.
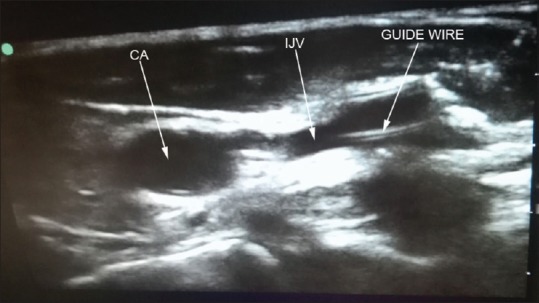
Medial oblique axis view showing both artery, vein and path of the guidewire as a bright line
Diameter of IJV in anteroposterior plane, number of needle passes, success of cannulation, VAT (time from starting of insertion of introducer needle to return of venous blood into the attached syringe), guidewire time (time from starting of insertion of introducer needle to crossing the second marker of the guidewire from beginning of needle's body), catheterisation time (time from starting of insertion of introducer needle to end of catheter placement, not including the suturing and fixation time) and complications like carotid artery puncture, hematoma formation, arrhythmias, haemothorax, pneumothorax and catheter malposition if any were recorded. A needle pass was considered successful if the Seldinger needle was advanced forward without any backward movement. Every needle withdrawal with subsequent advance was considered another needle pass whether or not a new skin puncture site was chosen. A maximum of four needle passes was allowed. Cannulation was considered successful if guidewire was advanced without resistance and detected ultrasonographically inside the vein. It was considered unsuccessful if guide wire can't be inserted into the vein in four needle passes. Then, an alternative approach was used for the cannulation of IJV.
Statistical analysis was performed by the SPSS programme for Windows, version 17.0. Continuous variables are presented as mean ± SD and categorical variables are presented as absolute numbers and percentages. Data were checked for normality before statistical analysis using the Shapiro–Wilk test. Normally distributed continuous variables like venous access, guidewire and catheterisation time were compared using ANOVA. Categorical variables were analysed using the Chi-square test. For all statistical tests, a P value less than 0.05 was taken to indicate a significant difference.
RESULTS
In the present study, a total of 108 patients with 36 patients in each group were randomised between October 2017 and February 2019. All three groups were comparable with respect to demographic profiles [Table 1].
Table 1.
Demographic profile of the patients in different groups
| Group A (SAX) (n=36) | Group B (LAX) (n=36) | Group C (M-OAX) (n=36) | P | |
|---|---|---|---|---|
| Age (year) | 48.72±14.26 | 49.14±17.52 | 44.81±15.68 | 0.445 |
| Sex F/M | 12/24 | 19/17 | 17/19 | 0.947 |
| Place of cannulation OT/ICU | 25/11 | 26/10 | 24/12 | 0.877 |
| AP diameter of IJV (cm) | 1.03±0.19 | 0.93±0.22 | 0.93±0.17 | 0.098 |
SAX – Short axis, LAX – Longitudinal axis, M-OAX – Medial oblique
The first needle pass success rate was highest in M-OAX (97.2%) followed by SAX (88.9%) and then LAX (77.8%). But it was not statistically significant. The mean VAT was shortest in M-OAX (14.78 ± 5.45) followed by SAX (17.07 ± 3.81) and then LAX (23.83 ± 7.32) approach. It was statistically significant between LAX and SAX and between LAX and M-OAX group with a mean difference of 11.70 s (95% CI 2.26, 21.12). No significant difference was found between SAX and M-OAX groups. Similarly, guidewire insertion and catheterisation time were also highest for LAX (37.29 ± 6.61; 106.72 ± 22.42) followed by SAX (31.97 ± 4.49; 96.5 ± 15.29) and then M-OAX (27.22 ± 5.55; 89.17 ± 11.46) approach. It was also statistically significant among different approaches (P < 0.001). Although the complications developed were minor and there was no significant difference among all the groups, the rate of carotid wall puncture was higher in the LAX group as compared to SAX and M-OAX group. The incidence of arrhythmias was more in the SAX group (19.4%) followed by the LAX group (11.1%) than the M-OAX group (8.3%) but the difference was insignificant (P = 0.48). All the groups were comparable in terms of overall success rate and a number of needle passes [Tables 2 and 3].
Table 2.
Venous cannulation/catheterisation characteristics among different groups
| Parameters | Group A (SAX) (n=36) | Group B (LAX) (n=36) | Group C (M-OAX) (n=36) | P |
|---|---|---|---|---|
| First pass success rate (%) | 32 (88.9%) | 28 (77.8%) | 35 (97.2%) | 0.122 |
| Cannulation attempts/number of needle passes 1/2/3/4 | 32/4/0/0 | 28/7/1/0 | 35/1/0/0 | 0.122 |
| Venous access time (s) | 17.07±3.81 | 23.83±7.32 | 14.78±5.45 | <0.001*# |
| Guide wire insertion time (s) | 31.97±4.49 | 37.29±6.61 | 27.22±5.55 | <0.001*#$ |
| Catheterisation time (s) | 96.5±15.29 | 106.72±22.42 | 89.17±11.46 | <0.001*# |
*Significant between groups A and B; #significant between groups B and C; $significant between groups A and C
Table 3.
Complications among different groups
| Complications | Group A (n=36) | Group B (n=36) | Group C (n=36) | P |
|---|---|---|---|---|
| Carotid artery puncture | 0 (0.0%) | 2 (5.6%) | 0 (0.0%) | 0.130 |
| Haematoma | 0 (0.0%) | 1 (2.8%) | 0 (0.0%) | 0.364* |
| Pneumothorax | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Haemothorax | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - |
| Arrhythmias | 7 (19.4) | 4 (11.1%) | 3 (8.3%) | 0.344 |
DISCUSSION
Real-time USG-guided IJV cannulation has become the standard of care and is recommended by numerous societies.[7,8,9] USG-guided IJV cannulation is performed using different approaches like SAX, LAX, OAX or M-OAX and each technique has its own advantages and disadvantages.[3,4] In the SAX approach, the vessel is viewed in cross-section and allows the simultaneous visualisation of both the artery and the vein but makes the control of needle tip difficult.[3] In LAX view, the probe is centred on the IJ vein and rotated through 90° in a clockwise direction resulting in an LAX image of the vein. The probe needle and the blood vessel are in the plane of the ultrasound beam and therefore can optimise the needle visualisation, but it displays only the vein in the ultrasound image and does not allows the visualisation of relevant surrounding anatomic structures.[3] M-OAX technique combines the benefits of the above two techniques. M-OAX view is obtained by initially obtaining SAX view and then the probe is rotated 30° counterclockwise. With this technique, IJV and carotid artery can be seen beside each other and the needle shaft and tip are observable in its entire direction. Further, the risk of carotid artery puncture is decreased in this approach as the direction of the needle is from medial (cephalad) to lateral (caudad), that is, away from the carotid artery.[4]
The main objective of the present study was to compare three approaches SAX, LAX and M-OAX for USG-guided IJV cannulation and as to which scanning axis provides optimal condition for vascular access. We found that M-OAX and SAX are better than LAX in terms of significantly shorter venous access, guidewire and catheterisation time. The medial oblique and SAX approach were also associated with a higher first-pass success rate with a lesser incidence of complications as compared to the LAX approach though it was not significant statistically.
Kamalipour et al. compared the SAX and M-OAX approach using USG-guided right IJV cannulation in 80 patients. Similar to our study, they reported higher first-attempt success rate in M-OAX group 87.5% than SAX group 85% and it was statistically insignificant (P = 0.289). The overall success rate of cannulation in both groups was similar (100%). Mean VAT and catheterisation time in the M-OAX group (14.35 ± 8.93; 93.22 ± 26.02) was less as compared to SAX group (17.72 ± 12.59, 98.1 ± 27.75 s) but was statistically insignificant (P = 0.376). In contrast to the present study, guidewire insertion time in M-OAX group (36.02 ± 22.92 s) was larger as compared to SAX group (31.12 ± 13.12 s) but was statistically insignificant. This can be attributed to the difference in the angulation between patients' heads with the trunk in the SAX technique. There was no incidence of carotid artery puncture and hematoma in both SAX and M-OAX group.[10]
Batllori et al. compared short, LAX and OAX approach of USG-guided IJV cannulation in 220 patients. They noted a higher first-pass success rate in SAX as compared to the LAX approach and the difference was statistically significant (P = 0.005). The success rate of cannulation was similar in both groups (97%). Guidewire insertion time was also shorter in SAX (35 s) than the LAX (46.1 s) group and it was statistically significant (P = 0.039). In contrast to our study, the incidence of carotid artery puncture was less in the LAX group (0%) as compared to the SAX group (11%) and was statistically significant (P = 0.001).[3] This could be due to the difference in the experience of the anaesthesiologist performing the specific technique of USG-guided IJV cannulation.
Chittodan et al. compared the SAX and LAX approach of USG-guided IJV cannulation in 99 patients. First pass success rate was more in SAX (98%) as compared to the LAX approach (78%) and the difference was statistically significant (P < 0.006). The overall success rate of cannulation was similar in both groups (100%). Guidewire insertion time was shorter in SAX group (39.6 s) as compared to LAX (46.9 s) group (P = 0.59). The incidence of carotid artery puncture was also less in the SAX group (0%) as compared to the LAX group (4%) but the difference was insignificant (P = 0.48).[11]
Baidya et al. compared the SAX and M-OAX approach using USG-guided right IJV cannulation in 200 patients. Similar to our study, the first attempt success rate was higher in the M-OAX group 87% as compared to SAX group 85% and it was statistically insignificant (P = 0.538). The overall success rate of cannulation in both groups was similar (100%). The guidewire insertion time in both the groups was similar (14 s) but catheterisation time in the M-OAX group (128 s) was less as compared to the SAX group (134 s) (P = 0.165). There was no incidence of hematoma in both SAX and M-OAX group.[1] In their other study, Baidya et al. found that the transverse diameter of the IJV was significantly higher and the percentage of overlap was also significantly lower in the medial-oblique probe position (48.7 ± 10.7% in short-axis vs 36.3 ± 13.2% in medial-oblique probe position (P = 0.000). However, there was no statistically significant difference in the anteroposterior diameter of the IJV between the two probe positions (1.11 ± 0.26 cm in SAX vs 1.07 ± 0.25 cm in medial oblique; P = 0.631). They mentioned that the medial-oblique probe position for IJV cannulation provides sonoanatomic superiority over the classic SAX probe position.
Tamman et al. and Shresta et al. also compared SAX and LAX approach using USG-guided IJV cannulation and noted a similar overall success rate of cannulation (100%) in both groups.[12,13]
Stone et al. compared the landmark vs ultrasound (SAX and LAX) technique. They found that the VAT was lesser in the SAX group (12.4 s) as compared to the LAX group (14.8 s) but it was statistically insignificant (P = 0.48).[14]
The present study is in contrast to the study done by Vogel et al. who compared the LAX and SAX approaches using ultrasound. They noted that the mean access time in LAX (9.5 s) was lesser as compared to SAX (14.5 s).[15] Similarly, Chaudhari et al. compared the SAX and LAX approach of IJV cannulation using ultrasound in 50 patients. In their study, first-pass success rate was more in LAX (92%) as compared to SAX (76%) approach but the difference was statistically insignificant (P = 0.128).[16] The difference in the results can be attributed to the experience of the anaesthetists (experience of more than 50 USG-guided IJV cannulations in our study).
We found that M-OAX and SAX are better than LAX in terms of significantly shorter venous access, guidewire and catheterisation time. The M-OAX and SAX approach were also associated with the higher first attempt and overall success rate with lesser incidence of complications as compared to the LAX approach though it was not statistically significant. The M-OAX approach also had significantly shorter guidewire insertion time as compared to SAX. The present study has some limitations. The difference in the ability of each anaesthesiologist to manage each of the three approaches may be a possible source of bias in the present study. Another limitation is that this study had a limited number of patients (sample size of 108) over a limited period of time. Larger sample studies are required to further validate the superiority of a particular approach of USG-guided IJV cannulation over the other. Moreover, due to the nature of the study, it was impossible to blind the operator to the three approaches of USG-guided IJV cannulation.
CONCLUSION
We conclude that the M-OAX approach is a safe and effective approach for performing USG-guided IJV cannulation because of better visibility of both artery and vein and continuous real-time visualisation of the LAX of the needle. Thus, the use of this approach for USG-guided IJV cannulation is encouraged. Further clinical studies with large sample size are needed to confirm this conclusion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Baidya DK, Arora MK, Ray BR, Mohan VK, Anand Rk, Khanna P, et al. Comparison between short axis and medial oblique view for ultrasound guided internal jugular vein cannulation: A randomized controlled trial. Acta Anaesth Belg. 2018;69:107–12. [Google Scholar]
- 2.Hrics P, Wilber S, Bland MP, Gallo U. Ultrasound assisted internal jugular vein catheterization in the ED. Am J Emerg Med. 1998;16:401–3. doi: 10.1016/s0735-6757(98)90140-1. [DOI] [PubMed] [Google Scholar]
- 3.Batllori M, Urra M, Uriarte E, Romero C, Pueyo J, Olaondo LL, et al. Randomized comparison of three transducer orientation approaches for ultrasound guided internal jugular venous cannulation. Br J Anaesth. 2016;116:370–6. doi: 10.1093/bja/aev399. [DOI] [PubMed] [Google Scholar]
- 4.Dilisio R, Mittnacht AJC. The medial-oblique approach to ultrasound-guided central venous cannulation- Maximize the view, minimize the risk. Cardiothorac Vascu Anesth. 2012;26:982–4. doi: 10.1053/j.jvca.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 5.Phelan M, Hagerty D. The oblique view: An alternative approach for ultrasound-guided central line placement. J Emerg Med. 2009;37:403–8. doi: 10.1016/j.jemermed.2008.02.061. [DOI] [PubMed] [Google Scholar]
- 6.Baidya DK, Chandralekha, Darlong V, Pandey R, Goswami D, Maitra S. Comparative Sonoanatomy of Classic “Short Axis” Probe Position with a Novel “Medial-oblique” probe position for ultrasound guided internal jugular vein cannulation: A crossover study. J Emerg Med. 2015;48:590–6. doi: 10.1016/j.jemermed.2014.07.062. [DOI] [PubMed] [Google Scholar]
- 7.Troianos CA, Hartman GS, Glask E, Skubas NJ, Eberhardt RT, Warker JD, et al. Guidelines for performing ultrasound guided vascular cannulation: Recommendations of the American Society of Echocardiograghy and the Society of Cardiovascular Anaesthesiologists. J Am Soc Echocardiogr. 2011;24:1291–318. doi: 10.1016/j.echo.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 8.Lamperti M, Bordenham AR, Pittiniti M, Blaisvas M, Augoustides JG, Elbarbary M, et al. International evidence-based recommendations on ultrasound-guided vascular access. Intensive Care Med. 2012;38:1105–17. doi: 10.1007/s00134-012-2597-x. [DOI] [PubMed] [Google Scholar]
- 9.National Institute for Clinical Excellance. Guidance on the use of ultrasound locating devices for placing central venous catheters. [Last accessed on 2014 May 08];Internet J Anesthesiol [serial on the Internet] 2008 20(2):5. Available from: http://ispub.com/IJA/20/2/8060 . [Google Scholar]
- 10.Kamalipour H, Shahbazi S, Derakhshan MM, Moinvaziri MT, Allahyar E. Comparision of US-guided catheterization of the right internal jugular vein using medial oblique and short axis techniques. Intcardiovasc Res J. 2015;9:210–5. [Google Scholar]
- 11.Chittodan S, Breen D, O2Donnell BD, Iohom G. Long versus short axis ultrasound guided approach for internal jugular vein cannulation. Med Ultrasono. 2011;13:21–5. [PubMed] [Google Scholar]
- 12.Tammam TF, El-Shafey EM, Tammam HF. Ultrasound-guided internal jugular vein access: Comparison between short axis and long axis techniques. Saudi J Kidney Dis Transpl. 2013;24:707–13. doi: 10.4103/1319-2442.113861. [DOI] [PubMed] [Google Scholar]
- 13.Shrestha GS, Gurung A, Koirala S. Comparision between long and short axis techniques for ultrasound guided cannulation of internal jugular vein. Ann Card Anaesth. 2016;19:288–92. doi: 10.4103/0971-9784.179629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stone MB, Moon C, Sutijono D, Blaivas M. Needle tip visualization during ultrasound-guided vascular access: Short-axis vs long-axis approach. Am J Emerg Med. 2010;28:343–7. doi: 10.1016/j.ajem.2008.11.022. [DOI] [PubMed] [Google Scholar]
- 15.Vogel JA, Haukoos JS, Erickson CL, Liao MM, Theoret J, Sanz GE, et al. Is long-axis view superior to short-axis view in ultrasound-guided central venous catheterization? Crit Care Med. 2015;43:832–9. doi: 10.1097/CCM.0000000000000823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaudhari MS, Shah SB, Kamat HV. Ultrasound guided internal jugular vein cannulation with short and long axis approach. Technical ease and complications. Indian J Clin Anaesth. 2016;3:546–50. [Google Scholar]


