Abstract
Aims
People with psychotic disorders face impairments in their global functioning and their quality of life (QoL). The relationship between the two outcomes has not been systematically investigated. Through a systematic review, we aim to explore the presence and extent of associations between global functioning and QoL and establish whether associations depend on the instruments employed.
Methods
In May 2016, ten electronic databases were searched using a two-phase process to identify articles in which associations between global functioning and QoL were assessed. Basic descriptive data and correlation coefficients between global functioning and QoL instruments were extracted, with the strength of the correlation assessed according to the specifications of Cohen 1988. Results were reported with reference to the Meta-analysis of Observational Studies in Epidemiology guidelines and PRISMA standards. A narrative synthesis was performed due to heterogeneity in methodological approaches.
Results
Of an initial 15 183 non-duplicate articles identified, 756 were deemed potentially relevant, with 40 studies encompassing 42 articles included. Fourteen instruments for measuring global functioning and 22 instruments for measuring QoL were used. Twenty-nine articles reported linear associations while 19 assessed QoL predictors. Correlations between overall scores varied in strength, primarily dependent on the QoL instrument employed, and whether QoL was objectively or subjectively assessed. Correlations observed for objective QoL measures were consistently larger than those observed for subjective measures, as were correlations for an interviewer than self-assessed QoL. When correlations were assessed by domains of QoL, the highest correlations were found for social domains of QoL, for which most correlations were moderate or higher. Global functioning consistently predicted overall QoL as did depressive and negative symptoms.
Conclusions
This review is the first to explore the extent of associations between global functioning and QoL in people with psychotic disorders. We consistently found a positive association between global functioning and QoL. The strength of the association was dependent on the QoL instrument employed. QoL domains strongly associated with global functioning were highlighted. The review illustrates the extensive array of instruments used for the assessment of QoL and to a lesser extent global functioning in people with psychotic disorders and provides a framework to understand the different findings reported in the literature. The findings can also inform the future choice of instruments by researchers and/or clinicians. The observed associations reassure that interventions for improving global functioning will have a positive impact on the QoL of people living with a psychotic disorder.
Key words: Functioning, psychosis, quality of life, Schizophrenia
Introduction
Psychotic disorders are of special interest due to the severity of their symptoms, the surrounding stigma and the consequences of dysfunction, discrimination and costs. The importance of functioning to psychotic disorders was reaffirmed when psychosis was described as an imprecise group of symptoms, of sufficient severity to disrupt everyday functioning (Petho and Ban, 1988).
According to the International Classification of Functioning, Disability and Health (World Health Organization, 2001), functioning denotes the positive features of the relationship between a health condition and the environmental and personal context of the individual, while disability indicates negative features of that relationship. Thus, functioning is concerned with the ability of an individual to perform their roles and participate in life (Bowling, 2005). Global functioning should encompass the measurement of several types of functioning (Aas, 2010). Since 1962, a number of instruments have been created to measure global functioning, as well as specific dimensions (or types) of functioning e.g., social functioning, executive functioning, etc. (see Fig. 1).
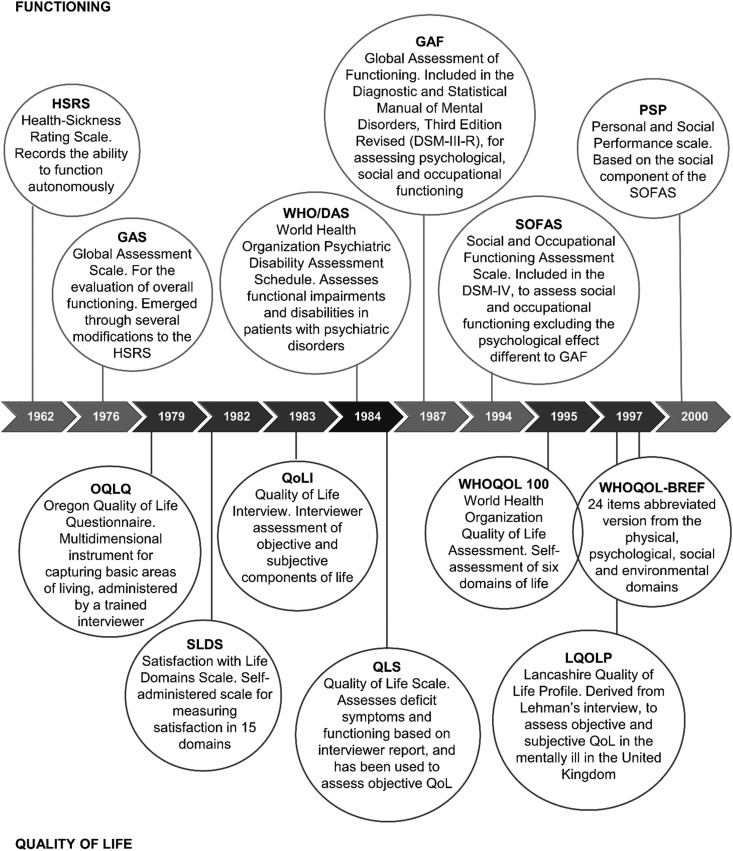
Fig. 1.
Timeline of functioning and quality of life instruments development.
Almost parallel to the development of instruments to assess functioning, and shortly after quality of life (QoL) in health care was raised by Elkinton, when he asked: ‘What is the harmony within a man, and between a man and his world –the quality of life– to which the patient, the physician, and society aspires?’ (Elkinton, 1966), interest in QoL as an outcome of people with psychosis began to emerge (Fig. 1). This interest occurred alongside the implementation of community support programmes after deinstitutionalisation (Baker and Intagliata, 1982; Lehman, 1988). QoL has been defined as ‘an individual's perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns’ (World Health Organization, 1997). Despite this, there is no agreement on what aspects and how QoL should be assessed. More than 50 QoL instruments have been used in patients with mental disorders (Prigent et al., 2014).
Functioning and more recently QoL have thus been identified as important outcomes in people with psychosis. Reviews focused on the assessment of global functioning and QoL in people with psychotic disorders are scarce (Awad et al., 1997; Pinikahana et al., 2002) and the relationship between them has not been systematically assessed. As impairment in the global functioning of people with psychosis is expected, it is important to understand the impact of this impairment on QoL. Establishing the relationship between global functioning and QoL measures would support the future choice of instruments for the assessment of these outcomes and, in turn, identify strategies to diminish the societal burden of psychotic disorders.
The aim of the present study is to explore the presence and extent of associations between global functioning and QoL in people with psychotic disorders and establish whether this relationship is dependent on the instruments employed.
Methods
Selection criteria
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al., 2009). Studies included for data extraction were full-text articles with a cross-sectional design or a follow-up design that provided required information at baseline. Baseline information only was sought, as changes in the functioning of people with psychosis over time is well documented (Harvey and Davidson, 2002; Ascher-Svanum et al., 2013; Harvey, 2014). Articles could be written in English or Spanish (given native English and Spanish speakers within the authorship team). The sample needed to comprise people with schizophrenia and schizophrenia spectrum disorders with or without people with mood disorders with psychotic symptoms (bipolar disorder type I, major or severe depressive disorder with psychotic symptoms) assessed according to the Ninth/Tenth Revision of the International Classification of Diseases (ICD 9/10) or the Diagnostic and Statistical Manual of Mental Disorders Fourth/Fifth Edition (DSM-IV/5), and aged between 18 and 64 years, in which associations between global functioning and QoL were assessed. There were no time-period restrictions.
Due to the lack of a universal definition of global functioning, instruments that assessed several dimensions of functioning as an inclusive outcome were deemed a global functioning instrument. Likewise, given the absence of a universally accepted definition of QoL, instruments reporting on a group of outcomes that contribute to an individual's satisfaction with life and/or overall health (Fayers and Machin, 2016) were accepted for inclusion in the review.
Intervention studies, reviews and meta-analyses were excluded as well as studies based on populations with organic or induced psychosis, psychosis due to other mental disorders or other medical conditions and populations at high risk of psychosis but not yet diagnosed. Intervention studies were excluded as functioning levels differ in artificial environments such as clinical trials (Patterson et al., 2001; Bellack et al., 2007; Ascher-Svanum et al., 2013).
Search strategy
In May 2016 Annual Reviews, Cochrane Library, CINAHL, EconLit, Embase, Medline, PsycARTICLES, PsycINFO, PubMed and ScienceDirect were searched using a two-phase identification process. Search terms were introduced with corresponding MeSH Terms, synonyms and stem words, as well as appropriate filters and use of Boolean operators. The detailed search strategy is available as Supplementary material.
Searches were divided into phases in order to identify potential publication bias. This approach was adopted because of concern that only strong associations would be reported in title and abstract. In Phase A, all keyword terms were searched in title and abstract. In Phase B, all keyword terms except functioning were searched in title and abstract, with stem ‘function’ then searched for in the main text.
Study selection
Two independent reviewers (ANF and AN) assessed studies for inclusion, with inconsistencies and disagreements resolved by consensus. After deletion of duplicates, Phase A records were screened for inclusion criteria in their titles and abstracts. Full-text articles of included studies were obtained and assessed in full for eligibility. A similar process was used for Phase B records, except that screening for inclusion included a search for functioning in the main text. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement (von Elm et al., 2007) was used to assess whether analytical observational studies reported STROBE elements determined a priori as essential. These items were 3, 7, 12, 16 and 18 (i.e., objectives, variables, statistical methods, main and key results).
Data extraction
Data extracted from each article encompassed basic descriptive data and correlation coefficients between global functioning and QoL instruments. Extraction was undertaken by ANF under the guidance of AN. After extraction, socio-demographic variables were coded for summarisation in frequency tables.
The correlation coefficients between global functioning and QoL extracted were: correlations between global functioning and other variables; and correlations between QoL and other variables comprising the domains and items covered for each instrument. This analysis reports on the strength of the correlation between global functioning and QoL and between global functioning and individual domains of QoL. Strength of correlation was assessed according to the specifications of Cohen (1988) established as 0.10⩽r < 0.3 small effect, 0.3⩽r < 0.5 medium effect and 0.50⩽r large effect.
A narrative synthesis was performed given the heterogeneity in methodological approaches, including instruments employed in the assessment of global functioning and QoL, and statistical analyses employed. QoL instruments were defined as an objective if comprised objective items only (usually intended for interviewer-assessment), subjective if comprised subjective items only (usually intended for self-assessment), or subjective and objective. Results were reported with reference to the Meta-analysis of Observational Studies in Epidemiology guidelines (Stroup et al., 2000) and PRISMA standards.
Results
Search results
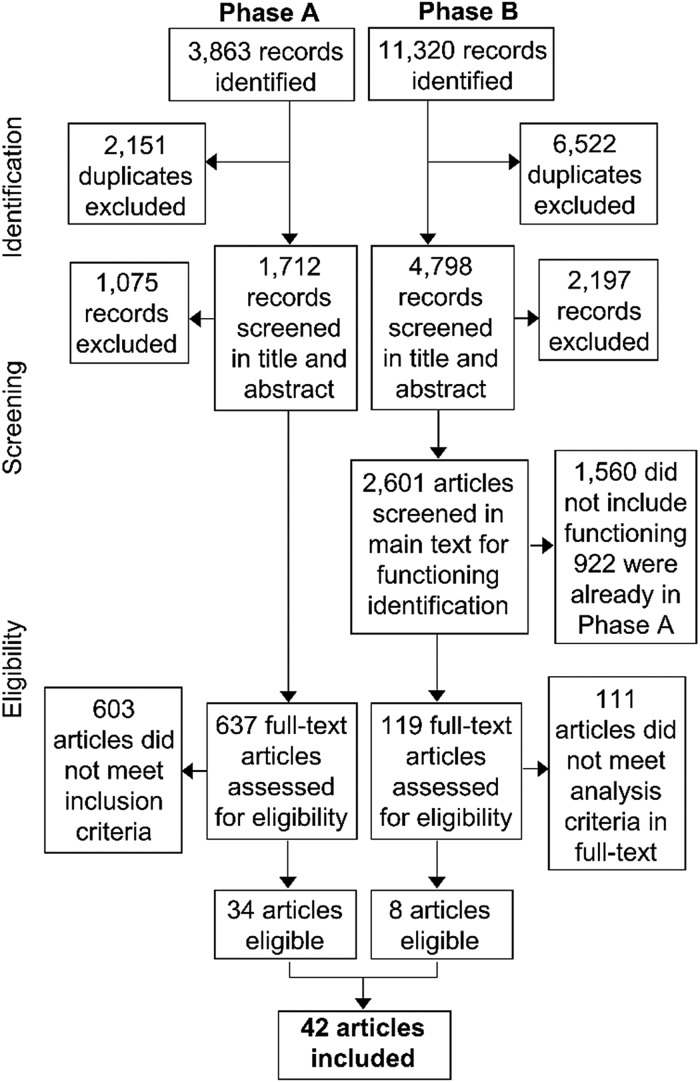
Across Phases A and B 15 183 records were initially identified, of which 8673 were duplicates and excluded from further review. In Phase A, upon screening of title and abstract, 637 articles were then assessed as requiring full-text review for eligibility, with 34 articles assessed as eligible. In Phase B upon screening of title and abstract, 2601 articles were assessed as requiring full-text screening for functioning, with 119 then identified as requiring full-text review for eligibility. Eight additional articles were identified as eligible for inclusion (see Fig. 2). Thus 42 articles were included in this review as listed in Table 1.
Fig. 2.
PRISMA flow diagram of Phase A and Phase B search.
Table 1.
Main characteristics of included studies
| Study | Conducted | Participants | Instruments | ||||
|---|---|---|---|---|---|---|---|
| Country of publication | N | Age range | Dxa (%) | Functioning | Quality of Life | ||
| Greenley et al. (1997) | NA | USA | 971 | NA | NS | GAF | QLQ |
| ELCCT: Holloway and Carson (1999) | NA | England | 70 | NA | NS | WHO/DAS | LQOLP; LEC |
| Norman et al. (2000) | 1989-1993 | Canada | 128 | 17–57 | 100 | LSP | QLS; GWB |
| EPSILON: Gaite et al. (2002) Becker et al. (2005) |
1997–1998 | Denmark; England; Italy; Spain; The Netherlands | 404 | 18–65 | NS | GAF | LQoLP-EU (European version) |
| Meijer et al. (2009, 2002) | 1997–1998 | The Netherlandsb | 143 | 18–65 | 100 | GAF | SF-36; LQoLP Dutch version |
| Mubarak (2005) | NA | Malaysia | 258 | NA | 100 | WHO/DAS | QoLI |
| Reine et al. (2005) | 2000 | France | 205 | 18–70 | 100 | GAF | SF-36; QoLI brief version; S-QoL |
| Ritsner et al. (2005) | NA | Israel | 133 | 18–60 | 100 | GAF | QLS; Q-LES-Q |
| König et al. (2007) | 2003–2004 | Germany | 166 | 21–80 | 72 | GAF; SOFAS | EQ-5D; WHOQOL-BREF |
| UK-SCAP: Kusel et al. (2007) | 1999–2000 | UK | 442 | NA | NS | GAF | QLS; MANSA |
| Prince (2007) | 1994–1996 | USA | 264 | 17–65 | NS | GAS | QoLI |
| Miclutia et al. (2008) | NA | Romania | 50 | 18–55 | 100 | GAF | WHOQOL-BREF |
| Adewuya and Makanjuola (2009) | 2006 | Nigeria | 99 | NA | 100 | GAF | WHOQOL-BREF |
| Chino et al. (2009) | NA | Japan | 36 | NA | 100 | GAF | WHOQOL-BREF |
| Kuo et al. (2009) | NA | Taiwan | 100 | 18–65 | 100 | GAF | SQLS-R4; LQOLP Taiwanese |
| Galuppi et al. (2010) | 2008 | Italy | 104 | NA | 100 | FPS | WHOQOL-BREF |
| Woon et al. (2010) | NA | Singapore | 83 | NA | 100 | GAF | WHOQOL-BREF |
| PSP Portuguese validation study: Brissos et al. (2011) | 2009–2010 | Portugal | 76 | 18–65 | 100 | PSP Portuguese version | WHOQOL-BREF Portuguese version |
| Hosseini and Yousefi (2011) | 1999–2000 | Iran | 100 | 21–60c | 100 | GAF | QLS |
| Karadayi et al. (2011) | NA | Turkey | 102 | 18–65 | 100 | PSP | QLS |
| Mas-Exposito et al. (2011) | 2006–2008 | Spain | 241 | NA | 100 | GAF; WHO DAS-S | WHOQOL-BREF |
| Riedel et al. (2011) | 2007 | Germany | 136 | 18–65 | 78 | GAF | QLS; RSM-Scale |
| Roe et al. (2011) | 2007–2008 | Israel | 159 | 19–66 | NS | GAF | MANSA |
| Guilera et al. (2012) | 2007–2009 | Spain | 352 | 18–55 | 88 | WHODAS II; SOFAS | EQ-5D |
| EGOFORS: Hunter and Barry (2012) | NA | Belgium; France; Germany; Israel; Italy; Spain; Sweden; Turkey; UK | 295 | NA | 100 | GAF; PSP | QLS |
| Nafees et al. (2012) | NA | UK | 73 | 18–65 | 100 | PSP; GAF | QLS |
| Pitkanen et al. (2012) | 2005–2006 | Finland | 311 | 18–65 | 41 | GAF | EQ-5D; Q-LES-Q short form |
| Razali and Wahid (2012) | NA | Malaysia | 206 | 18–60 | 100 | PSP | QoLI brief version |
| Medeiros-Ferreira et al. (2013) | 2008–2009 | Spain | 76 | NA | NS | GAF | EQ-5D |
| Akinsulore et al. (2014) | 2010 | Nigeria | 100 | NA | 100 | GAF | WHOQOL-BREF |
| Bai et al. (2014) | NA | Taiwan | 108 | 20–60 | 100 | PSP; SRG-PSP | WHOQOL-BREF |
| Rocca et al. (2014) | 2009–2011 | Italy | 92 | 18–65 | 100 | PSP | QLS |
| Zendjidjian et al. (2014) | NA | France | 91 | NA | 100 | GAF | SF-36 |
| Dima et al. (2015) | 2009–2010 | Romania | 131 | 18–65 | NS | GAF | SF-36; Q-LES-Q short form |
| Ito et al. (2015) | 2008–2011 | Japan | 168 | 16–55 | NS | GAF | WHOQOL-BREF |
| Lasebikan and Owoaje (2015) | 2008 | Nigeria | 652 | NA | 56 | GAF | WHOQOL-BREF |
| Stubbs et al. (2015) | 2010–2012 | UK | 438 | NA | NS | GAF | EQ-5D 3 levels |
| Alessandrini et al. (2016) | 2010–2014 | France | 271 | NA | 100 | FROGS | S-QoL 18 |
| Fujino et al. (2016) | NA | Japan | 93 | NA | 100 | UPSA-B; SFS | JSQLS |
| Rocca et al. (2016) | 2008–2011 | Italy | 323 | 18–65 | 100 | GAF | QLS |
EGOFORS, European Group on Functional Outcomes and Remission in Schizophrenia study; ELCCT, East Lambeth Continuing Care Team study; EPSILON, European Psychiatric Services: Inputs Linked to Outcome Domains and Needs study; EQ-5D, EuroQol five dimensions questionnaire; FPS, Personal and Social Functioning Scale; FROGS, Functional Remission Of General Schizophrenia; GAF, Global Assessment of Functioning; GAS, Global Assessment Scale; GWB, General Well-Being Scale; JSQLS, Schizophrenia Quality of Life Scale Japanese version; LEC, Life Experiences Checklist; LQOLP, Lancashire Quality of Life Profile; LSP, Life Skills Profile; MANSA, Manchester Short Assessment of Quality of Life; NS, not specified; PSP, Personal and Social Performance scale; Q-LES-Q, Quality of Life Enjoyment and Satisfaction Questionnaire; QLQ, Quality of Life Questionnaire; QLS, Quality of Life Scale; QoLI, Lehman’s Quality of Life Interview; RSM-Scale, Riedel-Spellmann-Musil-Scale; SF-36, Medical Outcomes Study (MOS) 36-Item Short-Form Health Survey; SFS, Social Functioning Scale; SOFAS, Social and Occupational Functioning Assessment Scale; SQLS-R4, Schizophrenia Quality of Life Scale Revision 4 Chinese version; S-QoL, Schizophrenia Quality of Life; SRG-PSP, Self-reported version of the graphic PSP; UK-SCAP, United Kingdom Schizophrenia Care and Assessment Programme; UPSA-B, University of California, San Diego (UCSD) Performance-based Skills Assessment-Brief version; USA, United States of America; WHO DAS-S, World Health Organization Short Disability Assessment Schedule; WHO/DAS, World Health Organization Disability Assessment Schedule; WHOQOL-BREF, World Health Organization Quality of Life abbreviated version; NA, not available.
Percentage of schizophrenia diagnosis.
Including EPSILON's participants from Amsterdam and other participants from The Netherlands.
Lower – Upper age of participants included in the study.
The articles
Articles were published between 1997 and 2016, all met the required STROBE criteria for inclusion. Three-fifths (25 articles) were from Europe. Four articles related to the European Psychiatric Services: Inputs Linked to Outcome Domains and Needs (EPSILON) study: Gaite et al. (2002) and Becker et al. (2005) reported on the entire sample while Meijer et al. (2002) reported on the Amsterdam participants at baseline, and at 18 months follow up (2009), as part of a broader Netherlands’ study. Each of these articles undertook different analyses of the data and as there was no pooling of results, the results for each are reported to maximise the comprehensiveness of the narrative synthesis. Four more articles (Holloway and Carson, 1999; Kusel et al., 2007; Brissos et al., 2011; Hunter and Barry, 2012) were published as part of larger studies. The systematic review thus comprised articles from 40 independent studies.
Data extracted overview
The median number of participants across all studies was 135, with the range 36–971. Schizophrenia was the single diagnosis in 26 articles (62%), only four articles (Greenley et al., 1997; Holloway and Carson, 1999; Lasebikan and Owoaje, 2015; Stubbs et al., 2015) (10%) included participants with bipolar disorder or depressive disorder with psychotic symptoms. Over half of the articles (57%) utilised one instrument for measuring functioning and one for measuring QoL. Six articles, employed two functioning instruments, 11 articles two QoL instruments and one article (Reine et al., 2005) three QoL instruments. Fujino et al. (2016) utilised two instruments, which together assessed global functioning.
Within the included studies, we identified 14 instruments for measuring global functioning and 22 for QoL. The Global Assessment of Functioning (GAF) was the most utilised functioning instrument (29 articles) and the WHO Quality of Life Instruments (WHOQOL-BREF) together with its Portuguese version the most utilised QoL instrument (12 articles) (see Supplementary material).
Of the 42 articles, 29 (69%) reported linear associations between global functioning and QoL overall scores and/or domain scores and presented correlation coefficients, four articles (10%) assessed associations between global functioning and QoL using alternate statistical methods; and 19 articles (45%) assessed predictors of QoL (Table 2). Outcomes for each are examined below.
Table 2.
Summary of associations provided by article
| Articles (total 42) | N | % | References |
|---|---|---|---|
| Correlations | |||
| Overall global functioning– Overall quality of life (QoL) | 20 | 48 | Karadayi et al. (2011), Mas-Exposito et al. (2011), Riedel et al. (2011), Hosseini and Yousefi (2011), Roe et al. (2011), Hunter and Barry (2012), Nafees et al. (2012), Gaite et al. (2002), Reine et al. (2005), König et al. (2007), Kusel et al. (2007), Miclutia et al. (2008), Galuppi et al. (2010), Dima et al. (2015), Chino et al. (2009), Greenley et al. (1997), Ritsner et al. (2005), Norman et al. (2000), Bai et al. (2014), Ito et al. (2015). |
| Overall global functioning – Domains of QoL | 13 | 31 | Mas-Exposito et al. (2011), Riedel et al. (2011), Meijer et al. (2002), Reine et al. (2005), Miclutia et al. (2008), Galuppi et al. (2010), Rocca et al. (2014), Dima et al. (2015), Kuo et al. (2009), Woon et al. (2010), Akinsulore et al. (2014), Bai et al. (2014), Fujino et al. (2016). |
| Domains of global functioning – Overall QoL | 5 | 12 | Mas-Exposito et al. (2011), Guilera et al. (2012), Holloway and Carson (1999), Chino et al. (2009), Bai et al. (2014). |
| Domains of global functioning– Domains of QoL | 5 | 12 | Mas-Exposito et al. (2011), Rocca et al. (2014), Alessandrini et al. (2016), Bai et al. (2014), Fujino et al. (2016). |
| Alternate statistical methods | 4 | 10 | Mubarak (2005), Pitkanen et al. (2012), Becker et al. (2005), Medeiros-Ferreira et al. (2013). |
| Associations estimated by multivariate analysis | |||
| Global functioning – Overall QoL | 10 | 24 | Roe et al. (2011), Meijer et al. (2009), Kusel et al. (2007), Stubbs et al. (2015) Alessandrini et al. (2016), Rocca et al. (2016), Norman et al. (2000), Woon et al. (2010), Prince (2007), Lasebikan and Owoaje (2015). |
| Global functioning – Domains of QoL | 4 | 10 | Brissos et al. (2011), Zendjidjian et al. (2014), Woon et al. (2010), Akinsulore et al. (2014). |
Linear associations between global functioning and QoL (overall scores)
Twenty articles (48%) provided correlations between overall scores of global functioning and QoL instruments. Two of these articles (Mas-Exposito et al., 2011; Bai et al., 2014) also provided correlations between global functioning with QoL domains and among global functioning and QoL domains (Table 2).
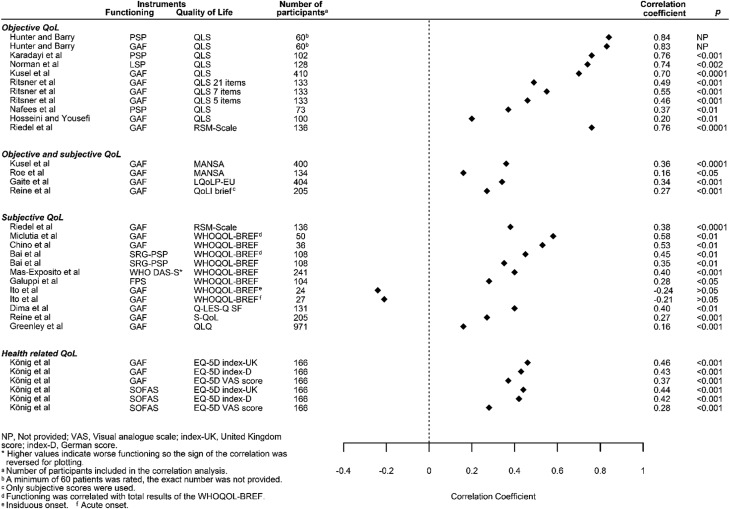
Correlations between overall scores ranged in strength from strong to weak with nearly half of the correlations reported as moderate (r = 0.34 to 0.49). Most moderate correlations involved the GAF which is consistent with the frequent use of the instrument. The two largest correlations assessed QoL using the QoL Scale (QLS), the largest assessed functioning with the Personal and Social Performance (PSP) (r = 0.84), the second largest with the GAF (r = 0.83). The smallest correlation reported as significant were for the GAF and the QoL Questionnaire (QLQ) and the GAF and Manchester Short Assessment of QoL (MANSA) (r = 0.16 for each) (Fig. 3).
Fig. 3.
Correlations between global functioning and quality of life.
Amongst the QoL instruments, nearly one-third of the correlations were assessed in relation to the QLS primarily the complete 21-item version, with the 7-item and 5-item versions also assessed in Ritsner et al. (2005). Half the correlations were large, including that for the 7-item version. One-quarter of correlations were assessed in relation to the self-assessed WHOQOL-BREF. Correlations were reported for four domain scores and two separate scored items that assessed the individual's overall perception of QoL and health (World Health Organization, 1998; The WHOQOL Group, 1998) in Galuppi et al. (2010), and just for overall QoL in three articles (Chino et al., 2009; Bai et al., 2014; Ito et al., 2015). Some articles reported correlations for the four domains and a total score (Miclutia et al., 2008; Mas-Exposito et al., 2011; Bai et al., 2014). Ito et al. (2015) reported non-significant associations for the overall score in insidious onset and acute onset (r = −0.24, −0.21), respectively. Correlations observed for objective QoL measures such as QLS were consistently larger (r = 0.20 to 0.84) than those observed for subjective measures such as WHOQOL-BREF (r = −0.21 to 0.58). Interviewer-assessment was also associated with larger correlations than self-assessment as reflected in Riedel et al. (2011).
Linear association between overall scores of global functioning and QoL domains
Thirteen articles (31%) provided correlations between global functioning and QoL domains, as listed in Table 3. Global functioning was measured with GAF in over half of the articles (62%), and with the exception of Bai et al. (2014) which employed the self-reported version of the graphic PSP (SRG-PSP), the interviewer undertook all assessments of functioning. The most utilised QoL instrument was the WHOQOL-BREF, followed by the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36). Assessments of QoL were self-assessed, with four exceptions (Meijer et al., 2002; Reine et al., 2005; Riedel et al., 2011; Rocca et al., 2014).
Table 3.
Correlations between overall scores of global functioning and domains scores of quality of life
| Components | QoL instrument construct | Subjective | Both | Objective | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Articles | Woon et al. (2010) | Akinsulore et al. (2014) | Miclutia et al. (2008) | Mas−Exposito et al. (2011) | Galuppi et al. (2010) | Bai et al. (2014) | Fujino et al. (2016) | Kuo et al. (2009) | Dima et al. (2015) | Reine et al. (2005) | Meijer et al. (2002) | Riedel et al. (2011) | Rocca et al. (2014) | |
| Instruments | GAF | GAF | GAF | WHODAS-S | FPS | SRG-PSP | UPSA-B | GAF | GAF | GAF | GAF | GAF | PSP | |
| QoL domains (number of items) | WHOQOL-BREF | JSQLS | SQLS -R4 | SF-36 Q-LES-Q SF |
SF-36 QoLI S-QoL |
SF-36 LQoLP Dutch |
RSM-Scaled | QLS | ||||||
| Environmental | Environment (8) | 0.34♦ | 0.19 | 0.42** | −0.36♦ | 0.43♦ | 0.39** | |||||||
| Living conditions (11) (RSM Sub_3) | 0.26♦
0.47♦e |
|||||||||||||
| Living situation (4) | 0.04 | |||||||||||||
| Residence (3) | 0.07b | |||||||||||||
| Finances (4) | 0.11 | |||||||||||||
| Disposable income (3) | −0.05b | |||||||||||||
| Personal security (3) | 0.10b | |||||||||||||
| Safety (2) | 0.08 | |||||||||||||
| Life in general | Subjective well-being (16) (RSM Sub_1) | 0.36♦
0.72♦e |
||||||||||||
| Life satisfaction (1) | 0.23* | |||||||||||||
| Goals (Fulfilment) (13) | 0.21** | |||||||||||||
| Framework (10) | 0.14 | |||||||||||||
| Symptoms/Side Effects (8) | −0.34** | |||||||||||||
| Satisfaction with treatment (1) | 0.23* | |||||||||||||
| Occupational | Occupational functioning (8) | 0.34♦
0.59♦e |
||||||||||||
| Instrumental role (4) | 0.44♦ | |||||||||||||
| Job satisfaction (3) | −0.10b | |||||||||||||
| Common Objects and activities (2) | 0.17 | |||||||||||||
| Leisure activities (4) | 0.12b | |||||||||||||
| Psychological | Psychological (6) | 0.31♦ | 0.42** | 0.58** | −0.31♦ | 0.34* | 0.39** | |||||||
| Psychological wellbeing (10) | 0.26c♦ | |||||||||||||
| Mental health (5) | 0.28a** | 0.24a♦ | 0.38a** | |||||||||||
| Composite Mental score | 0.21a** | |||||||||||||
| Resilience (5) | 0.26c♦ | |||||||||||||
| Emotional functioning (10) | 0.35♦
0.65♦e |
|||||||||||||
| Role Emotional (3) | 0.12a* | 0.17a* | 0.25a** | |||||||||||
| Self-esteem (6) | 0.24c♦ | |||||||||||||
| Negative esteem (5) | 0.35** | |||||||||||||
| Positive esteem (5) | 0.21* | |||||||||||||
| Psychosocial (15) | −0.17 | −0.03 | ||||||||||||
| Physical | Health (7) | 0.33** | ||||||||||||
| Health (1) | 0.30* | |||||||||||||
| General Health Perceptions (5) | 0.15a* | 0.20a* | ||||||||||||
| Physical Health (7) | 0.29** | 0.42** | 0.29** | −0.30♦ | 0.57 ∻ | 0.44** | ||||||||
| Physical functioning (10) | 0.40a** | 0.14a | 0.28a** | |||||||||||
| Physical functioning (7) | 0.22♦
0.41♦e |
|||||||||||||
| Physical well-being (4) | 0.21c♦ | |||||||||||||
| Role physical (4) | 0.20a** | 0.18a* | 0.26a** | |||||||||||
| Composite physical score | 0.14a | |||||||||||||
| Cognition (4) | 0.28♦
0.61♦e |
|||||||||||||
| Autonomy (4) | 0.28c♦ | |||||||||||||
| Energy/Fatigue (4) | 0.21a** | 0.24a♦ | 0.17a* | |||||||||||
| Motivation energy (7) | −0.16 | −0.11 | ||||||||||||
| Bodily Pain (2) | 0.15a* | 0.19a** | ||||||||||||
| Mental and physical health (3) | 0.10b** | |||||||||||||
| Social | Interpersonal relationships (8) | 0.56♦ | ||||||||||||
| Social relationships (3) | NP | 0.21* | 0.47** | −0.31♦ | 0.37* | 0.37** | ||||||||
| Social relations (3) | 0.20b** | |||||||||||||
| Functioning in social roles (9) (RSM Sub_2) | 0.35♦
0.65♦e |
|||||||||||||
| Social functioning (7) | 0.38♦
0.65♦e |
|||||||||||||
| Social functioning (2) | 0.32a** | 0.18a* | 0.37a** | |||||||||||
| Sentimental life (2) | 0.23c♦ | |||||||||||||
| Leisure and social (6) | 0.18* | |||||||||||||
| Friends relationships (5) | 0.16c* | |||||||||||||
| Family relationships (5) | 0.09c | |||||||||||||
| Family relations (2) | 0.12 | |||||||||||||
| Family relations (2) | −0.05b | |||||||||||||
*p < 0.05, **p < 0.01, ∻ p < 0.005, ♦p < 0.001.
Note: Quality of life domains were extracted from each of the QoL instruments. The number of items for the assessment of every domain is within parenthesis.
NP, not provided.
SF-36.
QoLI brief. Only subjective items were used.
S-QoL.
RSM-scale allocates their 36 items into the five-dimensions model, it also assigns the items to three subscores: Items 1–16 (Sub_1), items 17–20, 23, 32–35 (Sub_2), items 21–22, 24–31, 36 (Sub_3).
Interviewer-assessment.
In total, we recorded 100 correlation coefficients across 39 domains within included QoL instruments. The strength of correlations varied widely and were primarily weak (48%). Just over one-quarter of correlations were presented in a single article (Reine et al., 2005), with the GAF compared with three different QoL instruments, the SF-36, Schizophrenia QoL (S-QoL) and Lehman's QoL Interview brief version (QoLI brief) (subjective items). All associations reported in this study were weak and in some instances lower than for other comparable assessments.
The largest correlation coefficient (r = 0.72) was between functioning assessed with GAF and ‘subjective wellbeing’ assessed by the interviewer with the Riedel-Spellmann-Musil-Scale (RSM-Scale) (Riedel et al., 2011). The next four highest correlations were also assessed between these instruments (r = 0.61 to 0.65) (Riedel et al., 2011). The smallest significant correlation (r = 0.10) was between functioning assessed with GAF and interviewer-assessed ‘mental and physical health’ of the QoLI brief, subjective items only (Reine et al., 2005).
Most correlations between global functioning and QoL domains were positive. Exceptions were for Mas-Exposito et al. (2011), which employed the WHO Short Disability Assessment Schedule (WHO DAS-S) for evaluating functioning, and Fujino et al. (2016) and Kuo et al. (2009), which employed the Schizophrenia QLS Japanese version (JSQLS) and Revision 4 Chinese version (SQLS-R4) to assess QoL respectively. For each of these three instruments lower scores signify better outcomes.
Correlations for the WHOQOL-BREF tended to be larger than those for the SF-36. The WHOQOL-BREF gave rise to correlations that were primarily moderate in strength for each of the four domains of the instrument, although large correlations were also reported for the physical (Galuppi et al., 2010) and psychological domains (Miclutia et al., 2008). In regard to the SF-36, of the 24 correlations all were small except for four correlations from two of three articles: one correlation for the physical domain (Dima et al., 2015), one for the mental health domain (Meijer et al., 2002) and two for the social domain (Meijer et al., 2002; Dima et al., 2015).
The three most frequently assessed domains of QoL were the physical, psychological and social components. The vast majority of correlations for the physical component were small (70%), half were small for the psychological component and 45% small for the social component. Around a third of these small correlations were assessed in Reine et al. (2005) which reported just over a quarter of all correlations. Over half (56%) of the correlations reported for occupational and environmental issues, as well as for components related to treatment and satisfaction with life, in general, were small.
When correlations were limited to broad domains (i.e., included several items), over half of the correlations were moderate for the environmental, psychological and social components and small for over half the correlations for physical components.
Over two-thirds of the total correlations between global functioning and QoL domains were self-assessed and nearly half were small (r = −0.03 to 0.29). The remaining 29 correlations were interviewer-assessed and over half were small (r = 0.10 to 0.21).
Associations resulting from alternate statistical approaches
In the four articles assessing associations between global functioning and QoL using alternate statistical methods, four separate approaches were used. Mubarak (2005) which compared means of dysfunction with a dichotomisation of QoL found that people with high dysfunction (low functioning) had low QoL. Pitkanen et al. (2012) which compared medians of QoL with a dichotomisation of functioning reported that lower functioning indicated poorer QoL. Becker et al. (2005) which compared the means of QoL across three levels of functioning showed an increase in the mean of QoL across levels of functioning from low to high. Medeiros-Ferreira et al. (2013) which compared the means of HRQoL and functioning in subgroups of people with or without metabolic syndrome reported no association.
Functioning as a predictor of QoL
Nineteen articles (45%) assessed predictors of QoL. Of these, Fujino et al. (2016) and Rocca et al. (2014) did not include global functioning as an initial predictor, 13 modelled global functioning as a predictor in their final models and four (Gaite et al., 2002; Adewuya and Makanjuola, 2009; Kuo et al., 2009; Razali and Wahid, 2012) did not include it in the final models (Table 2).
Of the 13 articles that modelled global functioning as a predictor of QoL, nine considered QoL overall and three specific domains of QoL. Woon et al. (2010) tested both. Global functioning predicted QoL overall in most analyses (Norman et al., 2000; Kusel et al., 2007; Meijer et al., 2009; Woon et al., 2010; Roe et al., 2011; Lasebikan and Owoaje, 2015; Alessandrini et al., 2016; Rocca et al., 2016). Exceptions were Stubbs et al. (2015) and Prince (2007).
Discussion
This systematic review is the first to explore the presence and extent of associations between global functioning and QoL in people with psychotic disorders. The appraisal proved difficult given a lack of similarities between studies, and differences in methodological approaches including instruments employed, and inconsistencies in results for given instruments. Despite these difficulties, we found that most of the included articles reported positive associations between higher global functioning and better QoL, and through a narrative review, we were able to clarify the extent of these associations alongside important explanatory factors.
Our results showed that the strength of the association was primarily dependent on the QoL instrument used and whether QoL was being objectively or subjectively assessed. The largest correlations were given by objective QoL instruments completed by an interviewer, the RSM-Scale in particular. The RSM-Scale covers social, occupational and psychological functioning and includes physical functioning and subjective well-being (Riedel et al., 2011). The other objective QoL instrument, the QLS, covers social (interpersonal relations), occupational (instrumental role) and psychological domains (intrapsychic foundations) as well as common objects and activities (Heinrichs et al., 1984). Thus, domains covered by both objective QoL instruments, overlap with domains encompassed by measures of global functioning, which account for the strong associations observed. Furthermore, both, objective QoL instruments and measures of global functioning were assessed by the one interviewer leading to further consistency in assessment. In contrast, subjective QoL instruments are intended to be completed through self-assessment and given that the patient's perspective can differ from an evaluator's (Sainfort et al., 1996; Atkinson et al., 1997; Bengtsson-Tops et al., 2005), the resulting differences will affect the strength of the correlation.
Even with the application of the same instruments, correlation coefficients will vary as a result of sampling variation. This was evident for studies that used the GAF and MANSA (Kusel et al., 2007; Roe et al., 2011). A smaller correlation was found when participants were all living in a psychiatric rehabilitation residential facility in Israel (Roe et al., 2011) than recruited from inpatient and outpatient settings in the UK (Kusel et al., 2007). Likewise, the importance of country and in turn differences in cultural and possibly health system structure and functioning is arguably reflected in Hosseini and Yousefi (2011). Two-thirds of participants in this study lived in an Iranian institution, and while QoL was measured with an objective QoL instrument (QLS), a small correlation was assessed. In comparison strong to moderate associations were assessed in other studies using the QLS from Europe (Kusel et al., 2007; Karadayi et al., 2011; Hunter and Barry, 2012; Nafees et al., 2012), Canada (Norman et al., 2000) and Israel (Ritsner et al., 2005).
Variation in QoL of people living with psychosis based on sociodemographic characteristics is well documented (Browne et al., 1996; Chan et al., 2003; Caron et al., 2005). Ethnicity has also been acknowledged as a contributor to the QoL of people with psychosis within a given cultural setting (Lehman, 1995; Ben-Zur et al., 2014), which may in part be due to the impact of racism and discrimination on an individual's expectations (Lehman, 1995; Prince, 2007). Religious beliefs and spirituality may also contribute directly to a better QoL (Cohen et al., 2010; Grover et al., 2014; Caqueo-Urízar et al., 2016). It is thus evident that social and demographic issues will affect associations between global functioning and QoL of people living with psychosis.
Our results support respondent burden as a potential confounder in the assessment of associations between functioning and QoL (Ulrich et al., 2005; Fricker et al., 2014). We observed small correlations only when three QoL instruments were employed (Reine et al., 2005), and predominantly small correlations when two QoL instruments were employed (Meijer et al., 2002; Dima et al., 2015).
We also observed that some authors (Miclutia et al., 2008; Mas-Exposito et al., 2011; Bai et al., 2014) reported a total score for the WHOQOL-BREF when there is no such approved score for this instrument. The WHOQOL-BREF generates four domain scores and two separately scored items (overall perception of QoL and health) (World Health Organization, 1998; University of Washington, 2011). As the appropriate use of an instrument is essential for a valid outcome, all results pertaining to the WHOQOL-BREF total score are not considered reliable. In another study (Medeiros-Ferreira et al., 2013), standard scoring techniques for the EQ-5D were not applied. Reine et al. (2005) reported the physical and mental composite scores of the SF-36, and while assessed (Ware et al., 1995), it has been suggested they provide an imprecise summary of profile scores (Taft et al., 2001). For these reasons, results of these studies were not considered reliable, reinforcing the importance of the proper use of an instrument, and the necessity of adhering to standardised scoring protocols.
Another important finding was that the domains covered by an instrument are key to the associations obtained. Further, the items included within an instrument will lead to differences in correlations as reflected in the results for the three variations of the QLS (the complete 21 items and abbreviated 7 and 5 items). We consider that in the assessment of QoL of people with psychosis it is important to include items that broadly encompass the mental or psychological domain, otherwise, the outcome will not fully reflect the potential experiences of this population. Thus, the assessment of mental health in the EQ-5D is considered problematic given that the dimension comprises a single item regarding the presence of anxiety and/or depression. In turn, while moderate correlations were obtained between the EQ-5D and global functioning, correlations themselves should not be considered sufficient in determining a reliable and valid QoL instrument.
Findings regarding the strength of the associations between global functioning and QoL domains highlighted social components. These had the highest correlations, with more than half moderate or higher even when subjectively assessed. However, the breadth of domains also impacted correlations and was smaller for narrow domains. As with comparisons between overall scores, the QoL instrument was the primary determinant of the strength of the correlations between global functioning and QoL domains.
Our systematic review has highlighted the extensive array of instruments for the assessment of QoL, and to a lesser extent global functioning in people living with a psychotic disorder. Further, given that both outcomes are commonly used, our systematic review provides the framework to understand the different findings reported in the literature, and inform the future choice of instruments by researchers and/or clinicians.
We found no patterns in the use of instruments in regard to either year, a country where studies were conducted, diagnostic criteria or other characteristics. This variability could be in part due to the absence of a universal definition of global functioning and QoL. However, the diversity is likely at least in part driven by cultural issues leading to modification of available instruments. Also limiting study findings was the need to undertake a narrative review given the heterogeneity of study findings. We did not include articles published in other than English or Spanish. All articles identified employed English, although over three-quarters were from non-English speaking countries. Therefore, it is considered that this limitation will have minimal impact if any on our findings. We did not register our protocol with PROSPERO: International prospective registered systematic reviews (University of York, 2011) as we considered our review fell under stated exclusion criteria: ‘looking at the reporting of and/or use of outcomes in research would not be included’.
We believe that clearer and precise definitions of global functioning and QoL are required so these outcomes can be concisely and uniformly measured, and we can identify the domains of life that need to be targeted for improving these outcomes. Further, only by having standard/homogeneous instruments, can we consistently assess the impact of interventions aimed at improving these outcomes, and thereby contribute to the ongoing development and implementation of strategies for improving global functioning and QoL in people living with psychotic disorders.
Overall, most articles identified reported moderate and positive associations between global functioning and QoL. The strength of correlation was dependent upon the instruments employed and the respondent (e.g., a clinician or the individual living with psychosis). However, the moderate associations between global functioning and QoL reassure that interventions that improve functioning in people with a psychotic disorder will have a positive impact on their QoL. Policy makers and clinicians should make improvement of QoL of people with psychosis a priority alongside symptom remission. Happiness and satisfaction, fulfilment of goals and expectations, are essential to people living with psychotic illness.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of Interest
None.
Availability of Data and Materials
Data supporting our findings can be available under request.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796018000549.
click here to view supplementary material
References
- Aas IM (2010) Global Assessment of Functioning (GAF): properties and frontier of current knowledge. Annals of General Psychiatry 9, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adewuya AO and Makanjuola ROA (2009) Subjective quality of life of Nigerian schizophrenia patients: sociodemographic and clinical correlates. Acta Psychiatrica Scandinavica 120, 160–164. [DOI] [PubMed] [Google Scholar]
- Akinsulore A, Aloba OO, Mapayi BM, Oloniniyi IO, Fatoye FO and Makanjuola RO (2014) Relationship between depressive symptoms and quality of life in Nigerian patients with schizophrenia. Social Psychiatry and Psychiatric Epidemiology 49, 1191–1198. [DOI] [PubMed] [Google Scholar]
- Alessandrini M, Lançon C, Fond G, Faget-Agius C, Richieri R, Faugere M, Metairie E, Boucekine M, Llorca PM, Auquier P and Boyer L (2016) A structural equation modelling approach to explore the determinants of quality of life in schizophrenia. Schizophrenia Research 171, 27–34. [DOI] [PubMed] [Google Scholar]
- Ascher-Svanum H, Novick D, Haro JM, Aguado J and Cui Z (2013). Empirically driven definitions of “good,” “moderate,” and “poor” levels of functioning in the treatment of schizophrenia. Quality of Life Research 22, 2085–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson M, Zibin S and Chuang H (1997) Characterizing quality of life among patients with chronic mental illness: a critical examination of the self-report methodology. American Journal of Psychiatry 154, 99–105. [DOI] [PubMed] [Google Scholar]
- Awad AG, Voruganti LN and Heslegrave RJ (1997) Measuring quality of life in patients with schizophrenia. PharmacoEconomics 11, 32–47. [DOI] [PubMed] [Google Scholar]
- Bai YM, Hsiao CY, Chen KC, Huang KL, Lee IH, Hsu JW, Chen PS and Yang YK (2014) The development of a self-reported scale for measuring functionality in patients with schizophrenia-Self-reported version of the graphic Personal and Social Performance (SRG-PSP) scale. Schizophrenia Research 159, 546–551. [DOI] [PubMed] [Google Scholar]
- Baker F and Intagliata J (1982) Quality of life in the evaluation of community support systems. Evaluation and Program Planning 5, 69–79. [DOI] [PubMed] [Google Scholar]
- Becker T, Leese M, Krumm S, Ruggeri M and Vazquez-Barquero JL (2005) Needs and quality of life among patients with schizophrenia in five European centres: what is the impact of global functioning scores? Social Psychiatry and Psychiatric Epidemiology 40, 628–634. [DOI] [PubMed] [Google Scholar]
- Bellack AS, Green MF, Cook JA, Fenton W, Harvey PD, Heaton RK, Laughren T, Leon AC, Mayo DJ, Patrick DL, Patterson TL, Rose A, Stover E and Wykes T (2007) Assessment of community functioning in people with schizophrenia and other severe mental illnesses: a white paper based on an NIMH-sponsored workshop. Schizophrenia Bulletin 33, 805–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Zur H, Duvdevany I and Saffoury Issa D (2014) Ethnicity moderates the effects of resources on quality of life for persons with mental illness living in community settings. Psychiatric Rehabilitation Journal 37, 309–315. [DOI] [PubMed] [Google Scholar]
- Bengtsson-Tops A, Hansson L, Sandlund M, Bjarnason O, Korkeila J, Merinder L, Nilsson L, Sørgaard KW, Vinding HR and Middelboe T (2005) Subjective versus interviewer assessment of global quality of life among persons with schizophrenia living in the community: a Nordic multicentre study. Quality of Life Research 14, 221–229. [DOI] [PubMed] [Google Scholar]
- Bowling A (2005) Measuring Health: a Review of Quality of Life Measurement Scales. Berkshire, England: Open University Press. [Google Scholar]
- Brissos S, Balanza-Martinez V, Dias VV, Carita AI and Figueira ML (2011) Is personal and social functioning associated with subjective quality of life in schizophrenia patients living in the community? European Archives of Psychiatry & Clinical Neuroscience 261, 509–517. [DOI] [PubMed] [Google Scholar]
- Browne S, Roe M, Lane A, Gervin M, Morris M, Kinsella A, Larkin C and O'Callaghan E (1996) Quality of life in schizophrenia: relationship to sociodemographic factors, symptomatology and tardive dyskinesia. Acta Psychiatrica Scandinavica 94, 118–124. [DOI] [PubMed] [Google Scholar]
- Caqueo-Urízar A, Urzúa A, Boyer L, Williams D, Caqueo-Urízar A, Urzúa A and Williams DR (2016) Religion involvement and quality of life in patients with schizophrenia in Latin America. Social Psychiatry and Psychiatric Epidemiology 51, 521–528. [DOI] [PubMed] [Google Scholar]
- Caron J, Lecomte Y, Stip E and Renaud S (2005) Predictors of quality of life in schizophrenia. Community Mental Health Journal 41, 399–417, 19p. [DOI] [PubMed] [Google Scholar]
- Chan GWL, Ungvari GS, Shek DTL and Leung JJP (2003) Hospital and community-based care for patients with chronic schizophrenia in Hong Kong quality of life and its correlates. Social Psychiatry & Psychiatric Epidemiology 38, 196–203. [DOI] [PubMed] [Google Scholar]
- Chino B, Nemoto T, Fujii C and Mizuno M (2009) Subjective assessments of the quality of life, well-being and self-efficacy in patients with schizophrenia: regular article. Psychiatry and Clinical Neurosciences 63, 521–528. [DOI] [PubMed] [Google Scholar]
- Cohen J (1988) Statistical Power Analysis for the Behavioral Sciences L. Hillsdale, New Jersey: Erlbaum Associates. [Google Scholar]
- Cohen CI, Jimenez C and Mittal S (2010) The role of religion in the well-being of older adults with schizophrenia. Psychiatric Services 61, 917–922. [DOI] [PubMed] [Google Scholar]
- Dima L, Vasile D, Rogozea L, Zia-Ul-Haq M, Bukhari SA and Moga M (2015) Self-perception of quality of life in patients treated with antipsychotics. Turkish Journal of Medical Sciences 45, 782–788. [DOI] [PubMed] [Google Scholar]
- Elkinton JR (1966) Medicine and the quality of life. Annals of Internal Medicine 64, 711–714. [DOI] [PubMed] [Google Scholar]
- Fayers PM and Machin D (2016) Quality of Life: The Assessment, Analysis and Reporting of Patient-Reported Outcomes. Chichester, Sussex UK: Wiley Blackwell. [Google Scholar]
- Fricker S, Yan T and Tsai S (2014) Response burden: what predicts it and who is burdened out? In AAPOR Proceedings, American Association for Public Opinion Research, Anaheim, California, May 15–18, 2014, pp. 4568–4577.
- Fujino H, Sumiyoshi C, Sumiyoshi T, Yasuda Y, Yamamori H, Ohi K, Fujimoto M, Hashimoto R, Takeda M and Imura O (2016) Predicting employment status and subjective quality of life in patients with schizophrenia. Schizophrenia Research: Cognition 3, 20–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaite L, Vazquez-Barquero JL, Borra C, Ballesteros J, Schene A, Welcher B, Thornicroft G, Becker T, Ruggeri M and Herran A (2002) Quality of life in patients with schizophrenia in five European countries: the EPSILON study. Acta Psychiatrica Scandinavica 105, 283–292. [DOI] [PubMed] [Google Scholar]
- Galuppi A, Turola MC, Nanni MG, Mazzoni P and Grassi L (2010) Schizophrenia and quality of life: how important are symptoms and functioning? International Journal of Mental Health Systems 4, 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenley JR, Greenberg JS and Brown R (1997) Measuring quality of life: a new and practical survey instrument. Social Work 42, 244–254. [DOI] [PubMed] [Google Scholar]
- Grover S, Davuluri T and Chakrabarti S (2014) Religion, spirituality, and schizophrenia: a review. Indian Journal of Psychological Medicine 36, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilera G, Gomez-Benito J, Pino O, Rojo JE, Cuesta MJ, Martinez-Aran A, Safont G, Tabares-Seisdedos R, Vieta E, Bernardo M, Crespo-Facorro B, Franco M and Rejas J (2012) Utility of the World Health Organization Disability Assessment Schedule II in schizophrenia. Schizophrenia Research 138, 240–247. [DOI] [PubMed] [Google Scholar]
- Harvey PD (2014). What is the evidence for changes in cognition and functioning over the lifespan in patients with schizophrenia? The Journal of Clinical Psychiatry 75(Suppl. 2), 34–38. [DOI] [PubMed] [Google Scholar]
- Harvey PD and Davidson M (2002) Schizophrenia: Course Over the Lifetime In Neuropsychopharmacology: The Fifth Generation of Progress (ed. Davis KL, Charney D, Coyle JT and Nemeroff C), pp. 641–655. Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- Heinrichs DW, Hanlon TE and Carpenter WT (1984) The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophrenia Bulletin 10, 388–398. [DOI] [PubMed] [Google Scholar]
- Holloway F and Carson J (1999) Subjective quality of life, psychopathology, satisfaction with care and insight: an exploratory study. International Journal of Social Psychiatry 45, 259–267. [DOI] [PubMed] [Google Scholar]
- Hosseini SH and Yousefi MK (2011) Quality of life and GAF in schizophrenia correlation between quality of life and global functioning in schizophrenia. Iranian Journal of Psychiatry and Behavioral Sciences 5, 120–125. [PMC free article] [PubMed] [Google Scholar]
- Hunter R and Barry S (2012) Negative symptoms and psychosocial functioning in schizophrenia: neglected but important targets for treatment. European Psychiatry 27, 432–436. [DOI] [PubMed] [Google Scholar]
- Ito S, Nemoto T, Tsujino N, Ohmuro N, Matsumoto K, Matsuoka H, Tanaka K, Nishiyama S, Suzuki M, Kinoshita H, Ozawa H, Fujita H, Shimodera S, Kishimoto T, Matsumoto K, Hasegawa T and Mizuno M (2015) Differential impacts of duration of untreated psychosis (DUP) on cognitive function in first-episode schizophrenia according to mode of onset. European Psychiatry 30, 995–1001. [DOI] [PubMed] [Google Scholar]
- Karadayi G, Emiroglu B and Ucok A (2011) Relationship of symptomatic remission with quality of life and functionality in patients with schizophrenia. Comprehensive Psychiatry 52, 701–707. [DOI] [PubMed] [Google Scholar]
- König H-H, Roick C and Angermeyer MC (2007) Validity of the EQ-5D in assessing and valuing health status in patients with schizophrenic, schizotypal or delusional disorders. European Psychiatry 22, 177–187. [DOI] [PubMed] [Google Scholar]
- Kuo PJ, Ma HI, Kuo CC, Huang WC and Chung MS (2009) Factor analysis of the schizophrenia quality of life scale revision 4 (SQLS-R4) Chinese version and related factors. International Journal of Psychiatry in Clinical Practice 13, 278–284. [DOI] [PubMed] [Google Scholar]
- Kusel Y, Laugharne R, Perrington S, McKendrick J, Stephenson D, Stockton-Henderson J, Barley M, McCaul R and Burns T (2007) Measurement of quality of life in schizophrenia: a comparison of two scales. Social Psychiatry and Psychiatric Epidemiology 42, 819–823. [DOI] [PubMed] [Google Scholar]
- Lasebikan VO and Owoaje ET (2015) Quality of life in psychosis: prevalence and associated factors in a Nigerian clinical population. Community Mental Health Journal 51, 491–496. [DOI] [PubMed] [Google Scholar]
- Lehman AF (1988) A quality of life interview for the chronically mentally ill. Evaluation and Program Planning 11, 51–62. [Google Scholar]
- Lehman AF (1995) Demographic influences on quality of life among persons with chronic mental illnesses. Evaluation and Program Planning 18, 155–164. [Google Scholar]
- Mas-Exposito L, Amador-Campos JA, Gomez-Benito J and Lalucat-Jo L (2011) The World Health Organization Quality of Life Scale Brief Version: a validation study in patients with schizophrenia. Quality of life Research 20, 1079–1089. [DOI] [PubMed] [Google Scholar]
- Medeiros-Ferreira L, Obiols JE, Navarro-Pastor JB and Zuniga-Lagares A (2013) Metabolic syndrome and health-related quality of life in patients with schizophrenia. Actas Espanolas de Psiquiatria 41, 17–26. [PubMed] [Google Scholar]
- Meijer CJ, Schene AH and Koeter MW (2002) Quality of life in schizophrenia measured by the MOS SF-36 and the Lancashire Quality of Life Profile: a comparison. Acta Psychiatrica Scandinavica 105, 293–300. [DOI] [PubMed] [Google Scholar]
- Meijer CJ, Koeter MW, Sprangers MA and Schene AH (2009) Predictors of general quality of life and the mediating role of health related quality of life in patients with schizophrenia. Social Psychiatry & Psychiatric Epidemiology 44, 361–368. [DOI] [PubMed] [Google Scholar]
- Miclutia IV, Popescu CA and Macrea RS (2008) Sexual dysfunctions of chronic schizophrenic female patients. Sexual & Relationship Therapy 23, 119–129. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J and Altman DG, and the PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Mubarak AR (2005) Social functioning and quality of life of people with schizophrenia in the northern region of Malaysia. Australian e-Journal for the Advancement of Mental Health 4, 1–10. [Google Scholar]
- Nafees B, van Hanswijck de Jonge P, Stull D, Pascoe K, Price M, Clarke A and Turkington D (2012) Reliability and validity of the Personal and Social Performance scale in patients with schizophrenia. Schizophrenia Research 140, 71–76. [DOI] [PubMed] [Google Scholar]
- Norman RMG, Malla AK, McLean T, Voruganti LPN, Cortese L, McIntosh E, Cheng S and Rickwood A (2000) The relationship of symptoms and level of functioning in schizophrenia to general wellbeing and the Quality of Life Scale. Acta Psychiatrica Scandinavica 102, 303–309. [DOI] [PubMed] [Google Scholar]
- Patterson TL, Goldman S, McKibbin CL, Hughs T and Jeste DV (2001) UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally Ill adults. Schizophrenia Bulletin 27, 235–245. [DOI] [PubMed] [Google Scholar]
- Petho B and Ban TA (1988) DCR Budapest-Nashville in the diagnosis and classification of functional psychoses. Psychopathology 21, 149–240. [DOI] [PubMed] [Google Scholar]
- Pinikahana J, Happell B, Hope J and Keks NA (2002) Quality of life in schizophrenia: a review of the literature from 1995 to 2000. International Journal of Mental Health Nursing 11, 103–111. [DOI] [PubMed] [Google Scholar]
- Pitkanen A, Valimaki M, Endicott J, Katajisto J, Luukkaala T, Koivunen M, Kuosmanen L and Hatonen H (2012) Assessing quality of life in patients with schizophrenia in an acute psychiatric setting: reliability, validity and feasibility of the EQ-5D and the Q-LES-Q. Nordic Journal of Psychiatry 66, 19–25. [DOI] [PubMed] [Google Scholar]
- Prigent A, Simon S, Durand-Zaleski I, Leboyer M and Chevreul K (2014) Quality of life instruments used in mental health research: properties and utilization. Psychiatry Research 215, 1–8. [DOI] [PubMed] [Google Scholar]
- Prince JD (2007) Education, ethnicity, and subjective life quality of recently discharged inpatients with schizophrenia. Journal of Nervous & Mental Disease 195, 560–565. [DOI] [PubMed] [Google Scholar]
- PROSPERO: International prospective register of systematic reviews. Centre for Reviews and Dissemination, University of York. (http://www.crd.york.ac.uk). Accessed 13 August 2018.
- Razali SM and Wahid MA (2012) Quality of life and depressive symptoms in patients with schizophrenia. International Medical Journal 19, 130–134. [Google Scholar]
- Reine G, Simeoni MC, Auquier P, Loundou A, Aghababian V and Lancon C (2005) Assessing health-related quality of life in patients suffering from schizophrenia: a comparison of instruments. European Psychiatry 20, 510–519. [DOI] [PubMed] [Google Scholar]
- Riedel M, Spellmann I, Schennach-Wolff R, Obermeier M and Musil R (2011) The RSM-scale: a pilot study on a new specific scale for self- and observer-rated quality of life in patients with schizophrenia. Quality of Life Research 20, 263–272. [DOI] [PubMed] [Google Scholar]
- Ritsner M, Kurs R, Ratner Y and Gibel A (2005) Condensed version of the Quality of Life Scale for schizophrenia for use in outcome studies. Psychiatry Research 135, 65–75. [DOI] [PubMed] [Google Scholar]
- Rocca P, Montemagni C, Zappia S, Pitera R, Sigaudo M and Bogetto F (2014) Negative symptoms and everyday functioning in schizophrenia: a cross-sectional study in a real world-setting. Psychiatry Research 218, 284–289. [DOI] [PubMed] [Google Scholar]
- Rocca P, Montemagni C, Mingrone C, Crivelli B, Sigaudo M and Bogetto F (2016) A cluster-analytical approach toward real-world outcome in outpatients with stable schizophrenia. European Psychiatry 32, 48–54. [DOI] [PubMed] [Google Scholar]
- Roe D, Mashiach-Eizenberg M and Lysaker PH (2011) The relation between objective and subjective domains of recovery among persons with schizophrenia-related disorders. Schizophrenia Research 131, 133–138. [DOI] [PubMed] [Google Scholar]
- Sainfort F, Becker M and Diamond R (1996) Judgments of quality of life of individuals with severe mental disorders: patient self-report versus provider perspectives. The American Journal of Psychiatry 153, 497–502. [DOI] [PubMed] [Google Scholar]
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA and Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Journal of the American Medical Association 283, 2008–2012. [DOI] [PubMed] [Google Scholar]
- Stubbs B, Gardner-Sood P, Smith S, Ismail K, Greenwood K, Patel A, Farmer R and Gaughran F (2015) Pain is independently associated with reduced health related quality of life in people with psychosis. Psychiatry Research 230, 585–591. [DOI] [PubMed] [Google Scholar]
- Taft C, Karlsson J and Sullivan M (2001) Do SF-36 summary component scores accurately summarize subscale scores? Quality of Life Research 10, 395–404. [DOI] [PubMed] [Google Scholar]
- The WHOQOL Group (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine 28, 551–558. [DOI] [PubMed] [Google Scholar]
- Ulrich CM, Wallen GR, Feister A and Grady C (2005) Respondent burden in clinical research: when are we asking too much of subjects? IRB: Ethics & Human Research 27, 17–20. [PubMed] [Google Scholar]
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC and Vandenbroucke JP (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bulletin of the World Health Organization 85, 867–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH and Raczek A (1995). Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Medical Care 33, AS264-AS279. [PubMed] [Google Scholar]
- Woon PS, Chia MY, Chan WY and Sim K (2010) Neurocognitive, clinical and functional correlates of subjective quality of life in Asian outpatients with schizophrenia. Progress in Neuro-Psychopharmacology and Biological Psychiatry 34, 463–468. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Division of Mental Health and Prevention of Substance Abuse (1997) WHOQOL : measuring quality of life. Geneva: World Health Organization; http://www.who.int/iris/handle/10665/63482 [Google Scholar]
- World Health Organization. Division of Mental Health and Prevention of Substance Abuse (1998) Programme on mental health: WHOQOL user manual. Geneva: WHO. [Google Scholar]
- World Health Organization (2001) International Classification of Functioning, Disability and Health: ICF. Geneva: WHO. [Google Scholar]
- Zendjidjian XY, Baumstarck K, Auquier P, Loundou A, Lançon C and Boyer L (2014) Satisfaction of hospitalized psychiatry patients: why should clinicians care? Patient Preference and Adherence 8, 575–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S2045796018000549.
click here to view supplementary material
Data Availability Statement
Data supporting our findings can be available under request.