Abstract
Objective:
Insight and avoidance are commonly discussed factors in obsessive compulsive disorder (OCD) that have demonstrated associations with increased severity as well as reduced treatment response in adults, but have not been sufficiently examined in pediatric OCD. The present study examines the impacts of avoidance, insight, and impairment recognition concordance, on cognitive behavioral therapy (CBT) outcomes, as well as impacts of CBT on insight and avoidance, in a large sample of OCD-affected youth.
Method:
Data from 573 OCD-affected youth enrolled in CBT trials was aggregated. The Children’s Yale-Brown Obsessive Compulsive Scale items measured treatment response, insight, and avoidance. Standardized differences between child- and parent-ratings of impairment were used to calculate impairment recognition concordance. Binary logistic regression was utilized to identify variables associated with treatment response.
Results:
Greater avoidance, limited child recognition of impairment, older age, and lower baseline severity predicted reduced likelihood of treatment response, but insight did not. Both insight and avoidance improved significantly following CBT. Response rates were lower when post-treatment insight and avoidance were worse.
Conclusion:
Contrasting with prevailing belief, poor insight does not appear to limit CBT response potential in pediatric OCD. Avoidance and impairment recognition are understudied CBT response predictors and warrant further consideration in pediatric OCD. Clinicians should attend to these factors to optimize outcomes for children affected by this common, debilitating illness.
Keywords: symptom recognition, exposure and response prevention, mega-analysis, predictors, treatment response
Lay Summary
Combining data from four programs, the present study features an international sample of 573 youth with obsessive compulsive disorder who received cognitive behavioral therapy (CBT). Youths’ symptom insight at baseline was not related to their likelihood of responding to treatment, but youth were less likely to have responded to treatment if they were older, had lower baseline severity, had greater baseline avoidance, and reported much less OCD-related impairment compared to their parent. Improvement in insight and avoidance over treatment was common, but lower rates of treatment response were observed among youth with worse post-treatment avoidance and insight. Youth denial of OCD-related impairment, but not poor baseline insight, may represent a signal of treatment resistance and tracking/targeting of avoidance and insight throughout CBT is recommended.
Introduction
Obsessive compulsive disorder (OCD) is an impairing psychiatric condition that is associated with reduced quality of life,1 impairment in functioning,1–3 and a chronic course if untreated.4 Consistently found to be efficacious and tolerable, cognitive behavioral therapy (CBT) emphasizing exposure and response prevention (ERP) is a first line approach for treating pediatric OCD; however, a sizable proportion of youth receiving CBT do not achieve response and/or remission.5–7 Identification of vulnerability factors associated with suboptimal response may provide additional treatment targets to improve eventual outcomes.
OCD-related avoidance, symptom insight, and recognition of impairment may represent such factors. Avoidance (i.e., an individual’s attempts to minimize or circumvent triggering of distress/symptoms) is a common behavioral coping strategy employed by youth with OCD.8–11 Symptom insight (i.e., an individual’s recognition that obsessions/compulsions are problematic symptoms of an OCD diagnosis rather than true, natural, or protective beliefs/behaviors) is an important clinical feature of OCD.12–14 Given that the presence of impairment is included in diagnostic criteria for OCD, failure to recognize or admit impairment observed by other family members may also represent an additional marker of illness awareness that has not been adequately explored in pediatric OCD. Prior to intervention, insight and avoidance are strongly correlated,15 and both factors are associated with greater OCD severity.15–19
Given that ERP requires the patient to directly approach their feared stimuli without the use of safety behaviors, reducing avoidance and improving insight are likely fundamental in achieving optimal treatment outcomes. Avoidance is the opposite of the approach encouraged through exposure and therefore will be addressed throughout treatment. In addition, insight may be expected to improve as individuals learn to face the threat of obsessional content via ERP and build confidence managing their compulsive urges despite that perceived threat. In fact, although rarely examined as an outcome, prior research has indicated that insight improves and avoidance is reduced following CBT.20–22
However, insight, avoidance and divergent family perspectives regarding illness impact may also present barriers to treatment success. Given that CBT for pediatric OCD generally requires parent involvement, failure of either the child or the parent to recognize negative impacts of OCD may limit motivation to engage in treatment. Youth with poor insight and/or severe avoidance also may be less likely to engage, or more likely to subvert, ERP exercises due to a perception that their behaviors are protective (e.g., “if I don’t hide the knives, I might really hurt myself”; “I can’t handle my distress”) or functional, rather than problematic (e.g., “my compulsions/avoidance help me to feel okay and get on with my day”). In support of this, both poorer insight and greater avoidance at baseline have been associated with reduced response to CBT/ERP in a number of adult OCD studies,23–26 although contradictory results have also been reported with respect to baseline insight.27,28 Further, when measured again at post-treatment, two small studies (n = 41; n = 78) of adults with OCD found that failure to improve insight during treatment, rather than baseline levels of insight, was associated with attenuated response.20,21 In pediatric OCD, one treatment study has suggested that poorer baseline insight was associated with reduced response across SSRI, CBT, combined SSRI plus CBT, or pill placebo treatment groups.29 Specific to CBT, a recent study noted better baseline insight was associated with greater improvements in global severity (Clinical Global Impression – Severity Scale) but not OCD severity as measured by the Children’s Yale Brown Obsessive Compulsive Scale (CY-BOCS).30 No pediatric OCD studies were identified that examined changes in insight or avoidance and CBT outcomes.
Given that insight and avoidance are domains directly influenced during ERP, and that initial evidence suggests they may predict treatment response, further examination within the context of pediatric OCD treatment is warranted. In addition, examination of parent- and child- concordance regarding impairment warrants exploration as an additional construct that may impact CBT response. Therefore, utilizing a well powered, multi-site aggregated sample of youth receiving CBT, the present study addressed the following two primary and one exploratory aims:
Primary Aim 1.
To examine whether baseline avoidance, insight or impairment recognition concordance, predicted response to CBT at post-treatment. It was hypothesized that greater avoidance, poorer insight, and limited impairment recognition would be associated with reduced likelihood of response to CBT.
Primary Aim 2.
To examine whether OCD-related insight and avoidance changed following CBT. It was hypothesized that both insight and avoidance would significantly improve following CBT.
Exploratory Aim 1.
To explore whether post-treatment insight and avoidance were associated with CBT response.
Method
Participants and Procedures
Data for 573 OCD-affected youth was obtained from four international pediatric OCD programs that implemented CBT trials (see Table S1, available online for program/study details). This sample represents a subsample of participants previously combined and included in Selles et al (2018).15 Participants had a confirmed diagnosis of OCD and a baseline CY-BOCS total score ≥ 16 and an insight rating. The sample was 53.2% female and aged 7 to 19 years old (M = 12.67; SD = 2.87). See Table 1 for an overview of participant characteristics for individual programs and the combined sample.
Table 1.
Demographic Characteristics of the Combined Sample
| All Sites (n = 573) |
DCS-CBT (n = 158) |
Griffith (n = 77) |
Nord-LOTS (n = 266) |
UBC-POP (n = 72) |
Site Differences | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | N | M (SD) | F | |
| Age | 573 | 12.67 (2.87) | 158 | 12.36 (3.07) | 77 | 12.83 (2.75) | 266 | 12.83 (2.75) | 72 | 13.39 (2.82) | 3.52*a |
| Baseline CY-BOCS Total | 573 | 24.95 (5.24) | 158 | 25.42 (5.94) | 77 | 26.52 (4.17) | 266 | 24.62 (5.11) | 72 | 23.43 (4.68) | 5.18*a,b |
| Baseline Insight (Q11) | 573 | 1.20 (1.02) | 158 | 1.14 (1.08) | 77 | 1.52 (0.94) | 266 | 1.12 (0.98) | 72 | 1.26 (1.08) | 3.37*c, d |
| Baseline Avoidance (Q12) | 572 | 1.77 (1.11) | 158 | 1.52 (1.20) | 77 | 2.05 (0.92) | 266 | 1.83 (1.08) | 71 | 1.82 (1.13) | 4.76*d,e |
| Change CY-BOCS | 573 | 11.42 (8.28) | 158 | 10.09 (7.92) | 77 | 13.74 (8.29) | 266 | 12.13 (8.78) | 72 | 9.21 (5.96) | 5.88*a,f |
| N | n (%) | N | n (%) | N | n (%) | N | n (%) | N | n (%) | X2 | |
| Female Gender | 573 | 305 (53) | 158 | 79 (50) | 77 | 46 (60) | 266 | 137 (52) | 72 | 43 (60) | 3.51 |
| Treatment History | 289 | 200 (69) | 158 | 103 (65) | 74 | 59 (77) | - | - | 57 | 38 (67) | 5.21 |
| Past Psychosocial | 115 | 70 (61) | - | - | 73 | 50 (69) | - | - | 42 | 20 (48) | 4.88* |
| Past Meds | 292 | 117 (40) | 157 | 80 (51) | 77 | 11 (14) | - | - | 58 | 26 (45) | 29.61** |
| Current Meds | 277 | 99 (36) | 158 | 59 (37) | 77 | 26 (34) | - | - | 42 | 14 (33) | 0.41 |
| Any Other Disorder | 546 | 298 (55) | 153 | 90 (57) | 77 | 69 (90) | 263 | 98 (37) | 53 | 41 (77) | 82.14** |
| Any Anxiety | 549 | 199 (36) | 155 | 62 (40) | 77 | 62 (81) | 265 | 49 (18) | 53 | 26 (49) | 106.30** |
| GAD | 553 | 115 (21) | 156 | 35 (22) | 77 | 42 (55) | 265 | 19 (7) | 56 | 19 (34) | 89.28** |
| Social Phobia | 554 | 63 (11) | 156 | 20 (13) | 77 | 22 (29) | 265 | 12 (5) | 56 | 9 (16) | 36.47** |
| Sep Anxiety | 555 | 27 (5) | 157 | 9 (6) | 77 | 9 (12) | 265 | 6 (2) | 56 | 3 (5) | 11.90* |
| Specific Phobia | 552 | 70 (13) | 157 | 16 (10) | 77 | 32 (42) | 265 | 20 (8) | 53 | 2 (4) | 68.97** |
| Externalizing | 551 | 95 (17) | 156 | 39 (25) | 77 | 14 (18) | 265 | 29 (11) | 53 | 13 (25) | 15.97* |
| ADHD | 551 | 74 (13) | 156 | 30 (19) | 77 | 9 (12) | 265 | 23 (9) | 53 | 12 (23) | 13.73* |
| ODD | 552 | 37 (7) | 157 | 17 (11) | 77 | 8 (10) | 265 | 10 (4) | 53 | 2 (4) | 10.31* |
| Major Depression | 550 | 33 (6) | 157 | 17 (11) | 77 | 5 (7) | 263 | 8 (3) | 53 | 3 (6) | 10.61* |
| Tic Disorder | 549 | 77 (14) | 157 | 7 (5) | 74 | 9 (12) | 265 | 49 (18) | 53 | 12 (23) | 19.77** |
| Impairment Recognition | 482 | - | 134 | - | 67 | - | 227 | - | 55 | - | 2.51 |
| Limited Parent | - | 69 (14) | - | 21 (16) | - | 11 (16) | - | 30 (13) | - | 7 (13) | - |
| Concordant | - | 349 (72) | - | 97 (72) | - | 44 (66) | - | 168 (74) | - | 40 (73) | - |
| Limited Child | - | 64 (13) | - | 16 (12) | - | 12 (18) | - | 29 (13) | - | 8 (15) | - |
Note: ADHD = Attention-deficit/hyperactivity disorder; CBT = Cognitive Behavior Therapy; DCS = D-cycloserine; GAD = Generalized Anxiety Disorder; Nord-LOTS = Nordic long-term OCD Treatment Study; ODD = Oppositional defiant disorder; UBC-POP = University of British Columbia Provincial OCD Program.
Griffith vs UBC-POP
DCS-CBT vs UBC-POP
Nord-LOTS vs Griffith
DCS-CBT vs Griffith
DCS-CBT vs Nord-LOTS
Nord-LOTS vs UBC-POP
p < .05;
p < .001.
Measures
Diagnostic Assessments:
Sites utilized either the Kiddie Schedule for Affective Disorders and Schizophrenia – Present and Lifetime Version31 or the Anxiety Disorder Interview Schedule for Children – Parent Version32 to establish baseline diagnoses.
OCD Severity:
CY-BOCS:33
The CY-BOCS is a 10-item clinician-rated measure of OCD severity in youth. Items (time spent, interference, distress, resistance, control) across two subscales (obsessions and compulsions) are rated from 0 to 4, with higher scores indicating more severe symptoms. The psychometric properties of the CY-BOCS have been well established.33,34
Avoidance:
The CY-BOCS includes a clinician-rated extension item (Q12) that measures avoidance. Youth are asked the extent to which they avoid doing things, going places, or being with people because of obsessions or compulsions. Using provided detailed descriptors as reference, answers are rated on a five-point scale, specifically 0) None; 1) Mild; 2) Moderate; 3) Severe; and 4) Extreme. Only one youth was missing an avoidance rating at baseline.
Insight:
The CY-BOCS includes a clinician-rated extension item (Q11) which assesses insight, most specifically, overvalued ideation/fixity of belief. In particular, youth are asked whether they believe their concerns or behaviors are reasonable as well as whether they believe their feared outcome may occur if they do not perform their compulsions. Using provided detailed descriptors as reference, answers are rated on a five-point Likert scale, specifically 0) Excellent; 1) Good; 2) Fair; 3) Poor; and 4) Lacks Insight/Delusional.33 In youth, Q11 is the primary measure used in prior studies of insight in pediatric OCD15,19,29,35 and when assessed, Q11 demonstrated strong inter-rater reliability.35
Impairment Recognition Concordance:
In pediatric OCD, discordance of child and parent-reported impairment suggests that one of the parties may underestimate (or overestimate) impacts of this illness. Therefore, to supplement analyses, impairment recognition concordance was calculated using parent- and child-ratings on versions of the Child Obsessive-Compulsive Impact Scale (COIS) at baseline. A total of 482 youth had available child- and parent-ratings on the COIS. Sites varied in utilizing the original 52-item,3 the revised 33-item,36 or a brief 20-item, version (see Supplemental Table 1 for utilization of measure by program). As such, prior to calculation, raw COIS total scores were converted into standardized z-scores within each site and then combined across sites. The difference between parent-rated impairment and child-rated impairment was then calculated, with concordant impairment recognition indicated by a z-score difference between −1 and 1, and discordant impairment recognition indicated by all other z-score differences. Discordance possibilities included limited parent recognition of impairment (relative to child report) indicated by z-score difference scores below −1 (i.e. child reported substantially more impairment than the parent), and limited child recognition of impairment (relative to parent report) indicated by difference z-scores above 1 (i.e. parent reported substantially more impairment than the child). Due to the method of measurement, impairment recognition could not be recalculated at post-treatment.
Analytic Plan
Relationships between baseline OCD severity, avoidance, and insight were examined using Pearson correlation coefficients. One-way ANOVAs were used to examine relationships between impairment recognition concordance and OCD severity, avoidance, and insight.
An intent-to-treat approach was utilized to address missing post-treatment CY-BOCS total scores. Of the 573 youth assessed at baseline, 90% (n = 517) had complete post-treatment CY-BOCS scores. When missing, post-treatment CY-BOCS total scores were replaced with CY-BOCS scores from (in order of priority) 1-month follow-up assessment (n = 6), mid-point assessment (n = 12), or baseline assessment (n = 38). The predictive impact of avoidance, insight, and impairment recognition concordance on treatment response (≥ 35% reduction in CY-BOCS score)37 was calculated using binary logistic regression. Due to associations with poorer insight at baseline,15 child age and baseline symptom severity were included as covariates along with study site. Due to the small number of youth with absent insight (n = 8), youth with absent and poor insight were combined for the regression analysis.
Improvements in insight and avoidance were evaluated using chi-square testing and the measured effect size of change from baseline to post-treatment (Cohen’s d). As post-treatment insight and avoidance were measured simultaneously with post-treatment severity, their associations with treatment response were examined only descriptively. Post-treatment insight and avoidance ratings were available for 89% of youth (n = 510).
Results
Baseline Outcomes
At baseline, distribution of insight ratings were as follows: excellent (29.7%; n = 170); good (34.0%; n = 195); fair (24.6%; n = 141); poor (10.3%; n = 59); and absent (1.4%; n = 8). Distribution of avoidance ratings at baseline were: none (16.8%; n = 96), mild (19.9%; n = 114), moderate (37.6%; n = 215), severe (20.6%; n = 118), and extreme (5.1%; n = 29).
Relationships between baseline OCD severity, insight, avoidance, and impairment recognition concordance are presented in Table 2. Increased OCD severity was noted among poor/absent youth although the overall correlation between insight and OCD severity is small (r = .15, p < .001). Avoidance was significantly positively correlated with OCD severity (r = .40, p < .001). Insight had a small but significant negative correlation with age (r = −.13, p = .001), while avoidance was not correlated with age (r = .08, p = .054). Insight and avoidance were significantly positively correlated with each other (r = .20, p < .001). No significant relationships were found between impairment recognition concordance and baseline OCD severity [F (2, 480) = 2.48, p = .09], child age [F (2, 480) = 0.87, p = .42], insight [F (2, 480) = 1.20, p = .30], or avoidance [F (2, 479) = 1.21, p = .30].
Table 2.
Baseline Ratings and Treatment Response by Insight, Avoidance, Impairment Recognition Concordance, and Age (n = 573)
| Factor | Rating | N | Child Age | Baseline CY-BOCS | Baseline Insight | Baseline Avoidance | Responders | Δ CY-BOCS | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | n | % | M | SD | |||
| Insight | Excellent | 170 | 13.01 | 3.02 | 24.88 | 5.31 | - | - | 1.55 | 1.21 | 103 | 60.6 | 11.41 | 8.52 |
| Good | 195a | 12.87 | 2.78 | 23.99 | 4.77 | - | - | 1.75 | 0.96 | 118 | 60.5 | 10.54 | 7.27 | |
| Fair | 141 | 12.45 | 2.77 | 24.94 | 5.13 | - | - | 1.81 | 1.06 | 91 | 64.5 | 11.21 | 8.18 | |
| Poor | 59 | 11.66 | 2.69 | 27.58 | 5.75 | - | - | 2.22 | 1.20 | 39 | 66.1 | 14.15 | 9.68 | |
| Absent | 8 | 11.88 | 3.48 | 30.88 | 3.27 | - | - | 3.13 | 0.64 | 6 | 75.0 | 16.50 | 12.33 | |
| Avoidance | None | 96 | 12.43 | 2.72 | 22.86 | 5.14 | 0.90 | 1.00 | - | - | 69 | 71.9 | 12.23 | 8.68 |
| Mild | 114 | 12.35 | 3.03 | 23.24 | 4.54 | 1.04 | 0.87 | - | - | 76 | 66.7 | 11.93 | 7.95 | |
| Moderate | 215 | 12.61 | 2.84 | 24.32 | 4.76 | 1.23 | 0.93 | - | - | 133 | 61.9 | 10.75 | 7.75 | |
| Severe | 118 | 13.29 | 2.85 | 27.92 | 4.66 | 1.41 | 1.15 | - | - | 64 | 54.2 | 11.28 | 8.55 | |
| Extreme | 29 | 12.52 | 2.83 | 31.35 | 3.96 | 1.69 | 1.37 | - | - | 14 | 48.3 | 12.28 | 10.77 | |
| Impairment Recognition | Limited Parent | 69 | 13.09 | 2.72 | 26.12 | 5.29 | 1.22 | 0.92 | 1.70 | 0.97 | 43 | 62.3 | 12.62 | 9.26 |
| Concordant | 349a | 12.66 | 2.84 | 24.70 | 5.08 | 1.24 | 1.03 | 1.77 | 1.12 | 233 | 66.8 | 12.03 | 7.87 | |
| Limited Child | 64 | 12.49 | 2.79 | 25.45 | 5.23 | 1.03 | 1.06 | 1.97 | 1.15 | 30 | 46.2 | 8.09 | 7.81 | |
| Age | Child (7–12) | 265 | 10.05 | 1.63 | 24.77 | 5.48 | 1.33 | 1.07 | 1.71 | 1.12 | 179 | 67.5 | 12.58 | 8.50 |
| Adolescent (13–19) | 308a | 14.92 | 1.44 | 25.12 | 5.03 | 1.08 | 0.96 | 1.82 | 1.10 | 178 | 57.8 | 10.41 | 7.96 | |
N – 1 for Baseline Avoidance
Impact on CBT Response
Table 3 presents the distribution of CBT responders (≥ 35% reduction in CY-BOCS score)37 versus CBT non-responders in addition to the mean CY-BOCS score change across baseline levels of insight, avoidance, and impairment recognition convergence. Results from the binary logistic regression analysis indicated that the model accounted for a small but statistically significant portion of the variance in likelihood of response [Adjusted R2 = .14, X2 (15, 467) = 51.65, p < .001; see Table 3]. Regarding control variables, site was significantly associated with response rate and a greater likelihood of response was predicted by younger age and higher baseline severity.
Table 3.
Outcomes of Logistic Regression Predicting Response to Cognitive Behavioral Therapy (n = 482)
| Variables | B (SE) | OR | 95% CI | Wald | p |
|---|---|---|---|---|---|
| Site | 11.82 | .008 | |||
| Child Age | −0.10 (.04) | 0.90 | 0.84 – 0.97 | 7.38 | .006 |
| Baseline CY-BOCS | 0.05 (.02) | 1.05 | 1.00 – 1.10 | 4.33 | .034 |
| Baseline Insight | 1.91 | .59 | |||
| Baseline Avoidance | 17.51 | .002 | |||
| None vs. Mild | −0.03 (.35) | 0.97 | 0.49 – 1.94 | 0.01 | .94 |
| None vs. Moderate | −0.56 (.32) | 0.57 | 0.31 – 1.06 | 3.14 | .076 |
| None vs. Severe | −1.11 (.36) | 0.33 | 0.16 – 0.67 | 9.34 | .002 |
| None vs. Extreme | −1.67 (.55) | 0.19 | 0.06 – 0.56 | 9.06 | .003 |
| Impairment Recognition | 10.85 | .004 | |||
| Equal vs. Limited Parent | −0.28 (.29) | 0.76 | 0.43 – 1.33 | 0.93 | .34 |
| Equal vs. Limited Child | −0.95 (.29) | 0.39 | 0.22 – 0.68 | 10.67 | .001 |
| Constant | 2.43 | .12 |
Baseline insight was not significantly related to response rates. Greater baseline avoidance and limited child recognition of impairment predicted reduced likelihood of achieving response to CBT. Response rates steadily declined with worsening avoidance from a 71.9% (n = 69) response rate for youth with no avoidance down to a 48.3% (n = 14) response rate for youth with extreme avoidance. Only 46.2% (n = 30) of youth with limited recognition of impairment (relative to the parent’s recognition) responded to treatment, in comparison to 62.3 – 66.8% of youth with either concordant, or limited parent, impairment recognition.
Impact of CBT on OCD-Related Insight and Avoidance
Changes in insight and avoidance levels over treatment were evaluated using chi-square analyses. Results indicated that insight ratings significantly changed over treatment [X2 (16, 494) = 67.14, p < .001] with most youth maintaining, or improving towards, excellent insight (see Figure 1). Avoidance ratings also significantly changed with treatment [X2 (16, 494) = 116.00, p < .001] with most youth exhibiting reductions in avoidance (see Figure 1). Restricted by limited room for improvement (e.g., youth cannot improve on excellent insight or no avoidance), overall effect sizes were moderate for insight improvement (d = 0.67) and avoidance improvement (d = 0.94); however, very large improvements were observed when only examining youth who had poor or absent baseline insight (d = 2.85; n = 60) or severe/extreme baseline avoidance (d = 2.36; n = 127).
Figure 1.
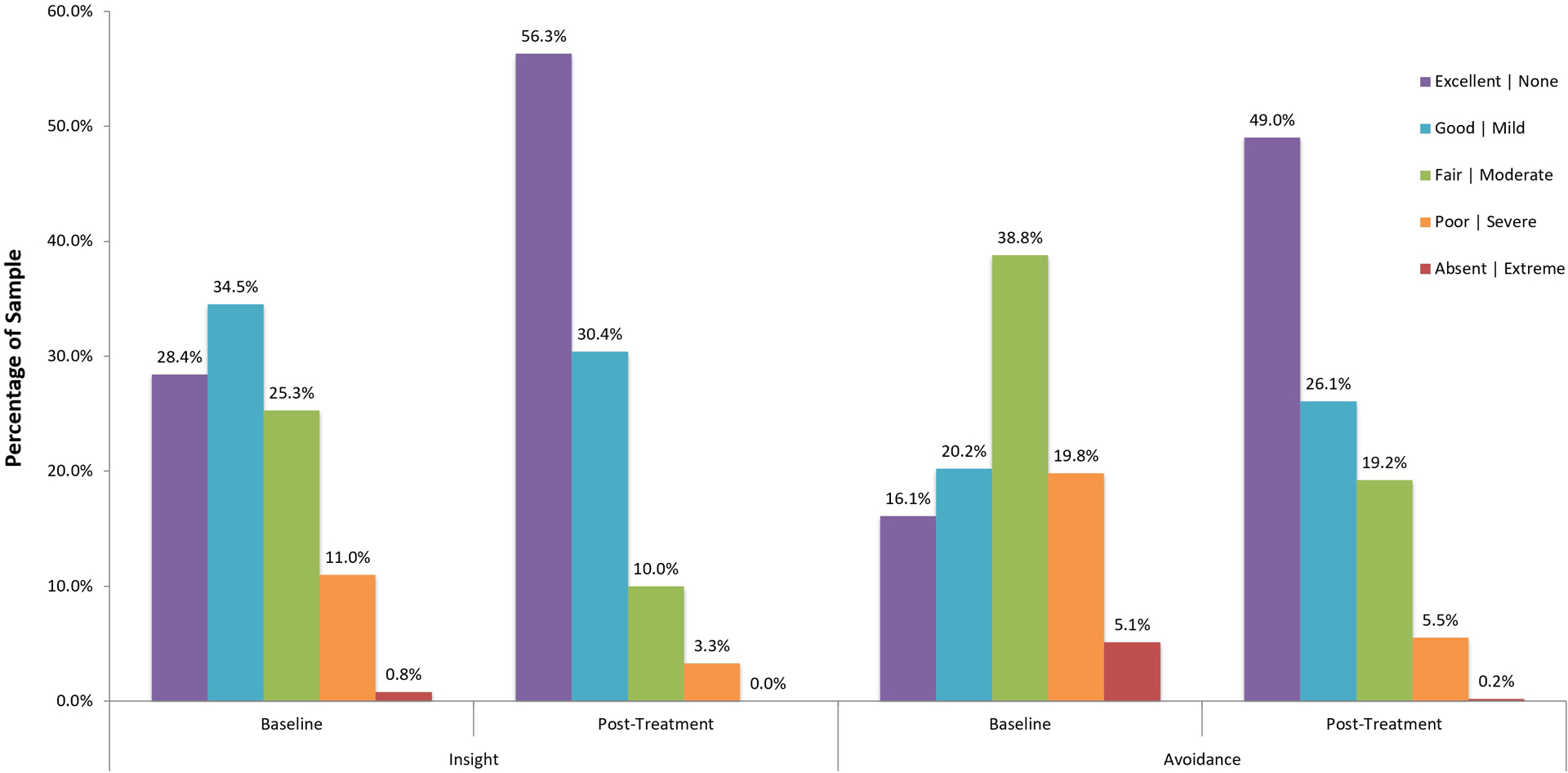
Insight and Avoidance Ratings Prior To, and Following, Treatment (n = 510)
Post-Treatment Insight and Avoidance and Response
Table 4 presents the distribution of responders to CBT and the mean CY-BOCS Change across post-treatment insight and avoidance ratings. Lower response rates presented with each level of declining insight and increasing avoidance at post-treatment, decreasing from 78.0% (n = 224) response among youth with excellent insight (n = 287) to 23.5% (n = 4) response among youth with poor insight (n = 17) and from 87.6% (n = 219) response among youth with no avoidance (n = 250) to 3.4% (n = 1) response among youth with severe/extreme avoidance (n = 29).
Table 4.
Treatment Response by Post-treatment Insight and Avoidance (n = 510)
| Factor | Rating | N | Response | Δ CY-BOCS | ||
|---|---|---|---|---|---|---|
| n | % | M | SD | |||
| Insight | Excellent | 287 | 224 | 78.0 | 14.31 | 8.02 |
| Good | 155 | 98 | 63.2 | 10.89 | 6.58 | |
| Fair | 51 | 17 | 33.3 | 8.47 | 7.28 | |
| Poor | 17 | 4 | 23.5 | 4.18 | 6.79 | |
| Avoidance | None | 250 | 219 | 87.6 | 16.23 | 7.29 |
| Mild | 133 | 86 | 64.7 | 10.38 | 6.07 | |
| Moderate | 98 | 36 | 36.7 | 7.70 | 5.49 | |
| Severe | 28 | 1 | 3.6 | 3.21 | 5.76 | |
| Extreme | 1 | 0 | 0.0 | −2.00 | - | |
Discussion
The present study elucidates roles of insight, avoidance and concordance of parent-child reported impairment in the context of CBT for pediatric OCD. Baseline insight did not predict treatment response while greater baseline avoidance, limited child impairment recognition (relative to parent), older age, and lower baseline severity, were associated with a reduced likelihood of treatment response. Insight and avoidance were identified as factors that substantially improve with CBT. Finally, individuals with worse insight and more avoidance following CBT also demonstrated lower response rates to CBT, indicating improvements in these factors is related to symptom improvement.
These results contrast with both adult OCD findings and conventional thinking, by suggesting that baseline insight does not have a substantial impact on the likelihood of treatment response. Regardless of youth’s awareness that their beliefs may be excessive, unrealistic, and/or a manifestation of their OCD, it appears that CBT is equally efficacious. In addition, youth typically maintained, or moved towards, higher levels of insight over CBT. Given that, prior to treatment, youth with poor insight demonstrate greater distress, avoidance and reduced symptom resistance,15 results of the present study may indicate that through ERP tasks (i.e. approaching fear, increasing resistance), the youth may begin to understand the nonsensical or excessive nature of their symptoms and change their dysfunctional beliefs.38 If so, it seems possible that poorer insight may still be expected to negatively impact the efficacy of placebo and medication (i.e., despite reductions in perceived distress, poorer insight does not lead to changes in behaviors or beliefs) which may partially explain the present study’s differences from the findings that poorer insight predicted worse outcomes across treatments in the Pediatric OCD Treatment Study.29
Regarding differences from adult findings,23–26 pediatric OCD has been proposed as a developmental subtype that is distinct from adult OCD.39 Among adult samples, poor insight has been associated with earlier age of onset,16,40 longer symptom duration,40 and more chronic course.16,41 Given the low observed frequency of absent insight in the present sample, it seems possible this subgroup may delay seeking assessment/treatment until adulthood, at which point their symptoms may be further entrenched and their likelihood of response to intervention reduced. In addition, limitations in the assessment of insight among youth as compared to adults (e.g., youth may be incorrectly identified as having poor insight due to issues in identifying or describing core fears, impulsivity toward compulsive urges despite no strong beliefs, extensive avoidance) may have contributed to the lack of associations between insight and outcome. Overall, the findings suggest that poor insight should not be considered a contraindication for CBT in youth.
In contrast to insight findings, limited child impairment recognition (relative to the parent) was associated with reduced treatment response and smaller mean CY-BOCS reductions. As limited child impairment recognition captures denial of OCD-related problems, it may represent a better proxy for “poor insight” in youth compared to Q11 of the CY-BOCS. Completion of CBT is a difficult and time-consuming process that requires experiencing distress, extensive behavioral changes, and potential temporary reductions in functioning. A child’s minimizing of OCD-related impairment relative to his/her parent may be an early marker that the child is lacking motivation to engage in treatment. An individual who does not recognize or believe the negative impacts of OCD would likely provide less effort towards, expect less benefit from, or be more easily turned away by initial negative experiences of, treatment. As impairment recognition was calculated via discrepancies in parent and child reports, family factors, such as accommodation (e.g., accommodations shift impairment from child to parent) and conflict/dysfunction/blame (e.g., parent blames child, so child denies symptoms), may also play a role in the observed associations.42–44 Regardless, these findings suggest that impairment recognition concordance is likely an important variable to be evaluated and considered at the onset of treatment.
Greater baseline avoidance was also associated with decreased likelihood of treatment response. Consistent with insight, ratings of avoidance improved significantly over the course of treatment, perhaps demonstrating both direct (e.g., successful targeting of avoidance) and indirect (e.g., less avoidance due to reduced symptom severity) benefits from CBT. As a barrier to CBT response, extensive avoidance may mask a youth’s symptom severity at baseline (e.g., patient under reports time spent, distress, and interference associated with symptoms due to persistent avoidance of triggers) and prevent, or slow, youth’s engagement in both planned and naturalistic ERP. As a result, clinicians should ensure that initial estimates of severity and impairment adequately reconcile the role that avoidance may play (e.g., wearing gloves may temporarily reduce hand-washing) and, if the youth is engaged in avoidant behaviors, clinicians should monitor their use within the context of ERPs and ensure that the patient is directly/fully engaging with the feared stimulus. For some youth, extensive avoidance may also signal the presence of other factors, such as poor distress tolerance45 and unwillingness to experience unpleasant thoughts, emotions, and/or bodily sensations46 which may have a more direct impact on inhibiting treatment success and warrant slight modifications to treatment (e.g., utilizing interoceptive exposures,47 pharmaceutical augmentation).
While not the focus of the present study, it is worth noting that older age was also associated with a reduced likelihood of treatment response. While older youth may have additional cognitive and communication capacities for treatment, one might hypothesize that younger youth are more malleable to intervention (e.g., symptoms less entrenched, faster learning). The utility and impact of parent/family involvement in treatment, which was included in all trials in the present study, may also be more substantial for younger youth (e.g., greater parental involvement in symptoms and opportunity for control over behavior).
Following CBT, results indicated that individuals who finished treatment with poorer insight or more avoidance were also less likely to have responded to treatment. As avoidance and insight were measured simultaneously to symptom severity at post-treatment, it is not clear whether this outcome implicates these domains as possible mediators of treatment improvement or if these domains are simply secondary outcomes of treatment response. These results are particularly difficult to interpret given that most youth made large improvements in avoidance and insight, and that post-treatment ratings included youth whose insight or avoidance worsened rather than simply failed to improve. It is possible that difficulties in assessing insight at baseline (e.g., patient reports excellent insight at baseline but reveals absent insight once ERPs became challenging) prevented the study’s ability to detect youth who display the trait-like resistant insight observed in adult studies. However, worse post-treatment ratings in these domains could be a reflection of other patient factors associated with non-response (e.g., distress tolerance, motivation), a failure of the intervention or clinician (e.g., ERPs did not adequately target the core fear), or other unknown factors. Regardless of the relationship direction or other factors contributing to its association, the above findings suggest that clinicians may be advised to monitor insight and avoidance throughout treatment and, if failing to improve or deteriorating, consider adjusting treatment to better target these domains (e.g., reconceptualization of core fear, enhanced focus on avoidance behaviors and acceptance of obsessions, and consideration of treatment alternatives including medication augmentation).
The study has several limitations. The participants included in the present study were recruited at OCD specialty centers for a variety of clinical trials examining ERP-focused CBT and combined retrospectively. With a broad distribution of patients in regard to nationality, age, baseline severity, treatment history, and comorbidity, the study sample is highly representative of treatment-seeking youth with primary OCD; however, study results may not generalize to all youth experiencing OCD, particularly those who may have OCD within the context of a different primary disorder, those experiencing excluded comorbidities (e.g., psychosis, active suicide risk), and/or those not presenting for assessment/treatment. This limitation may partially explain the particularly small number of youth with absent insight (n = 8) included in the present study and, as a result, reduced the likelihood of finding a relationship between absent insight and reduced treatment response. Second, although all sites provided ERP-focused CBT, they differed in exact delivery (e.g., dosing amount and frequency, components, individual versus group, extent of family/parent involvement). These differences reflect how varied CBT provision can be, even within the context of OCD specialty centers/treatment trials, and further supports the generalizability of the present study’s findings; however, these differences limit the ability to draw specific conclusions about study findings within the context of any one approach to treatment delivery. Third, insight and avoidance were measured by single items that are not comprehensive or truly continuous and limited impairment recognition was assessed indirectly. Finally, while in comparison to individual sample studies, data aggregation reduced the number of statistical tests, multiple testing was conducted increasing the chance of type-I error.
In conclusion, avoidance, insight, and parent-child concordance on impairment, all appear to be variables relevant to CBT. As a result, it is recommended that clinicians assess and monitor these factors prior to, and throughout, treatment. Future studies are needed to understand the emergence of problematic presentations, such as limited child impairment recognition, and extreme avoidance, in youth prior to treatment. In addition, the use of more comprehensive and frequent assessment of these domains throughout the treatment process is recommended to identify reasons for lack of change in, or worsening of, insight and/or avoidance over treatment.
Supplementary Material
Clinical Guidance.
Poor symptom insight at baseline does not appear related to CBT outcome; however, research using a more comprehensive measure of insight is needed in pediatric OCD to be more conclusive
Greater avoidance at baseline may slow/complicate treatment progress, but should not be considered a barrier to CBT participation.
Clinicians are recommended to measure and contrast child- and parent-reports of OCD-related impairment, as limited impairment recognition by the child as compared to their parent may limit improvement.
Avoidance and insight should be tracked and targeted throughout CBT and if youths’ avoidance and/or insight does not improve with treatment, alternate conceptualizations or treatment approaches should be considered.
Footnotes
Presentation Information: This study was presented as an abstract at the American Academy of Child and Adolescent Psychiatry’s 65th Annual Meeting; October 22–27, 2018; Seattle, WA.
Facebook: Mega-analytic study of pediatric OCD treatment data finds baseline insight not associated with response to CBT. Instead, reduced likelihood of treatment response predicted by greater baseline avoidance, limited child recognition of impairment (as compared to parent), older age, and lower baseline severity. Both insight and avoidance improved significantly following CBT. When post-treatment insight and avoidance were worse, response rates were also lower. #ocd #cbt
Twitter: In new mega-analytic study, baseline insight was not found to predict CBT response in pediatric OCD. Greater baseline avoidance and limited child recognition of impairment (as compared to parent) predicted lower likelihood of CBT response. #ocd #cbt
References
- 1.Storch EA, Small BJ, McGuire JF, Murphy TK, Wilhelm S, Geller DA. Quality of life in children and youth with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart SE, Hu YP, Leung A, et al. A multisite study of family functioning impairment in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 2017;56(3):241–249 e243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piacentini J, Bergman RL, Keller M, McCracken J. Functional impairment in children and adolescents with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol 2003;13 Suppl 1:S61–69. [DOI] [PubMed] [Google Scholar]
- 4.Stewart SE, Geller DA, Jenike M, et al. Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr Scand 2004;110(1):4–13. [DOI] [PubMed] [Google Scholar]
- 5.Geller D, March J, Issues TACoQ. Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 2012;51(1):98–113. [DOI] [PubMed] [Google Scholar]
- 6.Torp NC, Dahl K, Skarphedinsson G, et al. Effectiveness of cognitive behavior treatment for pediatric obsessive-compulsive disorder: Acute outcomes from the Nordic Long-term OCD Treatment Study (NordLOTS). Behav Res Ther 2015;64:15–23. [DOI] [PubMed] [Google Scholar]
- 7.Freeman J, Benito K, Herren J, et al. Evidence base update of psychosocial treatments for pediatric obsessive-compulsive disorder: Evaluating, improving, and transporting what works. J Clin Child Adolesc Psychol 2018;47(5):669–698. [DOI] [PubMed] [Google Scholar]
- 8.Gillan CM, Morein-Zamir S, Urcelay GP, et al. Enhanced avoidance habits in obsessive-compulsive disorder. Biol Psychiatry. 2014;75(8):631–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGuire JF, Storch EA, Lewin AB, Price LH, Rasmussen SA, Goodman WK. The role of avoidance in the phenomenology of obsessive-compulsive disorder. Compr Psychiatry. 2012;53(2):187–194. [DOI] [PubMed] [Google Scholar]
- 10.Starcevic V, Berle D, Brakoulias V, et al. The nature and correlates of avoidance in obsessive-compulsive disorder. Aust N Z J Psychiatry. 2011;45(10):871–879. [DOI] [PubMed] [Google Scholar]
- 11.Endrass T, Kloft L, Kaufmann C, Kathmann N. Approach and avoidance learning in obsessive-compulsive disorder. Depress Anxiety. 2011;28(2):166–172. [DOI] [PubMed] [Google Scholar]
- 12.Kozak MJ, Foa EB. Obsessions, overvalued ideas, and delusions in obsessive-compulsive disorder. Behav Res Ther. 1994;32(3):343–353. [DOI] [PubMed] [Google Scholar]
- 13.Neziroglu F, McKay D, Yaryura-Tobias JA, Stevens KP, Todaro J. The Overvalued Ideas Scale: Development, reliability and validity in obsessive-compulsive disorder. Behav Res Ther. 1999;37(9):881–902. [DOI] [PubMed] [Google Scholar]
- 14.Foa EB, Abramowitz JS, Franklin ME, Kozak MJ. Feared consequences, fixity of belief, and treatment outcome in patients with obsessive-compulsive disorder. Behav Ther. 1999;30(4):717–724. [Google Scholar]
- 15.Selles RR, Hojgaard D, Ivarsson T, et al. Symptom insight in pediatric obsessive-compulsive disorder: Outcomes of an international aggregated cross-sectional sample. J Am Acad Child Adolesc Psychiatry 2018;57(8):615–619 e615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Catapano F, Perris F, Fabrazzo M, et al. Obsessive-compulsive disorder with poor insight: A three-year prospective study. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(2):323–330. [DOI] [PubMed] [Google Scholar]
- 17.Visser H, van Megen H, van Oppen P, et al. The impact of poor insight on the course of Obsessive-Compulsive Disorder in patients receiving naturalistic treatment. J Obsess-Compuls Rel. 2017;13:42–48. [Google Scholar]
- 18.Borda T, Neziroglu F, Taboas W, McKay D, Frenkiel L. Overvalued ideation in adolescents with obsessive-compulsive disorder. Psychiatry Res. 2017;255:66–71. [DOI] [PubMed] [Google Scholar]
- 19.Storch EA, Milsom VA, Merlo LJ, et al. Insight in pediatric obsessive-compulsive disorder: Associations with clinical presentation. Psychiat Res. 2008;160(2):212–220. [DOI] [PubMed] [Google Scholar]
- 20.Matsunaga H, Kiriike N, Matsui T, et al. Obsessive-compulsive disorder with poor insight. Compr Psychiatry. 2002;43(2):150–157. [DOI] [PubMed] [Google Scholar]
- 21.Lelliott PT, Noshirvani HF, Basoglu M, Marks IM, Monteiro WO. Obsessive-compulsive beliefs and treatment outcome. Psychol Med. 1988;18(3):697–702. [DOI] [PubMed] [Google Scholar]
- 22.Barrett P, Healy L, March JS. Behavioral avoidance test for childhood obsessive-compulsive disorder: A home-based observation. Am J Psychother. 2003;57(1):80–100. [DOI] [PubMed] [Google Scholar]
- 23.Wheaton MG, Gershkovich M, Gallagher T, Foa EB, Simpson HB. Behavioral avoidance predicts treatment outcome with exposure and response prevention for obsessive-compulsive disorder. Depress Anxiety. 2018;35(3):256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tolin DF, Maltby N, Diefenbach GJ, Hannan SE, Worhunsky P. Cognitive-behavioral therapy for medication nonresponders with obsessive-compulsive disorder: A wait-list-controlled open trial. J Clin Psychiatry. 2004;65(7):922–931. [DOI] [PubMed] [Google Scholar]
- 25.Raffin AL, Fachel JMG, Ferrão YA, de Souza FP, Cordioli AV. Predictors of response to group cognitive-behavioral therapy in the treatment of obsessive-compulsive disorder. European Psychiatry. 2009;24(5):297–306. [DOI] [PubMed] [Google Scholar]
- 26.Himle JA, Van Etten ML, Janeck AS, Fischer DJ. Insight as a predictor of treatment outcome in behavioral group treatment for obsessive-compulsive disorder. Cognit Ther Res. 2006;30:661–666. [Google Scholar]
- 27.Stewart SE, Yen CH, Stack DE, Jenike MA. Outcome predictors for severe obsessive-compulsive patients in intensive residential treatment. J Psychiatr Res 2006;40(6):511–519. [DOI] [PubMed] [Google Scholar]
- 28.Maher MJ, Wang Y, Zuckoff A, et al. Predictors of patient adherence to cognitive-behavioral therapy for obsessive-compulsive disorder. Psychother Psychosom. 2012;81(2):124–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garcia AM, Sapyta JJ, Moore PS, et al. Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I). J Am Acad Child Adolesc Psychiatry. 2010;49(10):1024–1033; quiz 1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilhelm S, Berman N, Small BJ, Porth R, Storch EA, Geller D. D-Cycloserine augmentation of cognitive behavior therapy for pediatric OCD: Predictors and moderators of outcome. J Affect Disord. 2018;241:454–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 1997;36(7):980–988. [DOI] [PubMed] [Google Scholar]
- 32.Silverman WK, Albano AM. The Anxiety Disorders Interview Schedule for DSM-IV: Child and parent versions. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- 33.Scahill L, Riddle MA, McSwiggin-Hardin M, et al. Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36(6):844–852. [DOI] [PubMed] [Google Scholar]
- 34.Storch EA, Murphy TK, Geffken GR, et al. Psychometric evaluation of the Children’s Yale-Brown Obsessive-Compulsive Scale. Psychiatry Res. 2004;129(1):91–98. [DOI] [PubMed] [Google Scholar]
- 35.Lewin AB, Bergman RL, Peris TS, Chang S, McCracken JT, Piacentini J. Correlates of insight among youth with obsessive-compulsive disorder. J Child Psychol Psychiatry. 2010;51(5):603–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M. BRIEF REPORT: Functional impairment in childhood OCD: Development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale-Revised (COIS-R). J Clin Child Adolesc Psychol. 2007;36(4):645–653. [DOI] [PubMed] [Google Scholar]
- 37.Skarphedinsson G, De Nadai AS, Storch EA, Lewin AB, Ivarsson T. Defining cognitive-behavior therapy response and remission in pediatric OCD: A signal detection analysis of the Children’s Yale-Brown Obsessive Compulsive Scale. Eur Child Adolesc Psychiatry. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wolters LH, Prins PJM, Garst GJA, et al. Mediating Mechanisms in Cognitive Behavioral Therapy for Childhood OCD: The Role of Dysfunctional Beliefs. Child Psychiatry Hum Dev. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Geller D, Biederman J, Jones J, et al. Is juvenile obsessive-compulsive disorder a developmental subtype of the disorder? A review of the pediatric literature. J Am Acad Child Adolesc Psychiatry. 1998;37(4):420–427. [DOI] [PubMed] [Google Scholar]
- 40.Kishore VR, Samar R, Reddy YJ, Chandrasekhar C, Thennarasu K. Clinical characteristics and treatment response in poor and good insight obsessive–compulsive disorder. European Psychiatry. 2004;19(4):202–208. [DOI] [PubMed] [Google Scholar]
- 41.Bellino S, Patria L, Ziero S, Bogetto F. Clinical picture of obsessive-compulsive disorder with poor insight: a regression model. Psychiatry Res. 2005;136(2–3):223–231. [DOI] [PubMed] [Google Scholar]
- 42.Lebowitz ER, Panza KE, Su J, Bloch MH. Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother. 2012;12(2):229–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Keeley ML, Storch EA, Merlo LJ, Geffken GR. Clinical predictors of response to cognitive-behavioral therapy for obsessive-compulsive disorder. Clin Psychol Rev. 2008;28(1):118–130. [DOI] [PubMed] [Google Scholar]
- 44.Peris TS, Sugar CA, Bergman RL, Chang S, Langley A, Piacentini J. Family factors predict treatment outcome for pediatric obsessive-compulsive disorder. J Consult Clin Psychol. 2012;80(2):255–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Selles RR, Franklin M, Sapyta J, et al. Children’s and parents’ ability to tolerate child distress: Impact on cognitive behavioral therapy for pediatric obsessive compulsive disorder. Child Psychiatry Hum Dev. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Reid AM, Garner LE, Van Kirk N, et al. How willing are you? Willingness as a predictor of change during treatment of adults with obsessive-compulsive disorder. Depress Anxiety. 2017;34(11):1057–1064. [DOI] [PubMed] [Google Scholar]
- 47.Boswell JF, Farchione TJ, Sauer-Zavala S, Murray HW, Fortune MR, Barlow DH. Anxiety sensitivity and interoceptive exposure: A transdiagnostic construct and change strategy. Behav Ther. 2013;44(3):417–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Storch EA, Wilhelm S, Sprich S, et al. Efficacy of Augmentation of Cognitive Behavior Therapy With Weight-Adjusted d-Cycloserine vs Placebo in Pediatric Obsessive-Compulsive Disorder: A Randomized Clinical Trial. JAMA psychiatry. 2016;73(8):779–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.de Diaz NAN, Farrell LJ, Waters AM, Donovan C, McConnell HW. Sleep-related problems in pediatric obsessive-compulsive disorder and intensive exposure therapy. Behav Ther. 2019;50(3):608–620. [DOI] [PubMed] [Google Scholar]
- 50.Torp NC, Dahl K, Skarphedinsson G, et al. Predictors associated with improved cognitive-behavioral therapy outcome in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 2015;54(3):200–207 e201. [DOI] [PubMed] [Google Scholar]
- 51.Thomsen PH, Torp NC, Dahl K, et al. The Nordic long-term OCD treatment study (NordLOTS): rationale, design, and methods. Child and adolescent psychiatry and mental health. 2013;7(1):41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ivarsson T, Thomsen PH, Dahl K, et al. The rationale and some features of the Nordic Long-Term OCD Treatment Study (NordLOTS) in childhood and adolescence. Child Youth Care Forum. 2010;39(2):91–99. [Google Scholar]
- 53.Schuberth DA, Selles RR, Stewart SE. Coercive and disruptive behaviors mediate group cognitive-behavioral therapy response in pediatric obsessive-compulsive disorder. Compr Psychiatry. 2018;86:74–81. [DOI] [PubMed] [Google Scholar]
- 54.Selles RR, Belschner L, Negreiros J, et al. Group family-based cognitive behavioral therapy for pediatric obsessive compulsive disorder: Global outcomes and predictors of improvement. Psychiat Res. 2017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


