Abstract
Introduction
An increased metabolic demand during pregnancy is fulfilled by gaining sufficient gestational weight. Women who gain inadequate-weight are at a high-risk of premature birth or having a baby with low-birth weight. However, women who gain excessive-weight are at a high-risk of having a baby with macrosomia. The aim of this review was to determine the distribution of gestational weight gain and its association with birth-outcomes in Sub-Saharan Africa.
Methods
For this systematic review and meta-analysis, we performed a literature search using PubMed, Medline, Embase, Scopus, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases. We searched grey-literature from Google and Google Scholar, and region-specific journals from the African Journals Online (AJOL) database. We critically appraised the included studies using the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies. Two independent reviewers evaluated the quality of the studies and extracted the data. We calculated pooled relative-risks (RR) with 95% confidence intervals.
Results
Of 1450 retrieved studies, 26 met the inclusion criteria. Sixteen studies classified gestational weight gain according to the United States Institute of Medicine recommendations. The percentage adequate amount of gestational weight ranged from 3% to 62%. The percentage of inadequate weight was >50% among nine studies. Among underweight women, the percentage of women who gained inadequate gestational weight ranged from 67% to 98%. Only two studies were included in the meta-analyses to evaluate the association of gestational weight gain with pre-eclampsia and macrosomia. No difference was observed among women who gained inadequate and adequate gestational weight regarding experiencing pre-eclampsia (RR, 0.71; 95% CI: 0.22, 2.28, P = 0.57). Excessive gestational weight gain was not significantly associated with macrosomia compared to adequate weight gain (RR, 0.68; 95% CI: 0.38, 1.22, P = 0.20).
Conclusion
A substantial proportion of sub-Saharan African women gain inadequate gestational weight particularly high among underweight women. Future interventions would need to design effective pre-pregnancy weight management strategies.
Introduction
Desirable gestational weight gain (GWG) supports the increased metabolic demands required for positive pregnancy outcomes [1]. Guidelines regarding appropriate levels of GWG have been promoted worldwide [2]. A variety of guidelines about the GWG exist; their approach in GWG management also varies [3, 4]. More than a half (54%) of the GWG guidelines are similar to the 2009 United State Institutes of Medicine (IOM) recommendations [3]. The IOM recommends that women gain between 0.5 and 2.0 kg in the first trimester of pregnancy. In the second and third trimester, the weight gain recommendation is 0.44 to 0.58 kg per week for women who were underweight during the pre-pregnancy period (body mass index (BMI) ≤18.5 kg/m2); 0.35 to 0.50 kg per week for women of normal-weight (BMI is 18.5 to <25 kg/m2); 0.23 to 0.33 kg per week for over-weight women (BMI 25 to 30 kg/m2); and 0.17 to 0.27 kg per week for obese women (BMI ≥30 kg/m2). In total, the IOM recommends weight gain of 12.5 to 18 kg for underweight women; 11.5 to 16 kg for normal weight women, 7 to 11 kg for overweight women and 5 to 9 kg for obese women [5].
The amount of weight gained during pregnancy is determined by factors including the mother’s age [2, 6, 7], parity [2, 6, 7], income status [2, 8], educational status [7], social class [6], and pre-pregnancy maternal weight [2, 9]. Other factors include antenatal care (ANC) [2, 6], physical activity during pregnancy [10] and perinatal depression[11–13].
A desirable GWG is essential for optimal outcomes for both the mother and her baby [14]. Inappropriate GWG can pose health risks for mother and baby [15, 16]. Women who do not gain enough weight during pregnancy are at risk of having a baby with low birth weight (LBW) [17, 18] and pre-term birth [19]. Women who gain excessive weight are at an increased risk of hypertension in pregnancy, as well as an increased risk of pre-eclampsia [20–22], gestational diabetes [15, 20], caesarean sections [20, 22, 23], postpartum haemorrhage [22], postpartum weight retention [24], and development of long-term obesity [25].
The World Health Organization (WHO) defines low birth weight as a birth weight less than 2500g [26]. Globally, LBW contributes to 60% to 80% of all neonatal deaths [27]. About 95% of the 20.6 million LBW infants born each year are in low-income countries [26, 27]. Inadequate GWG in combination with low pre-pregnancy weight is associated with higher rates of LBW and prematurity [28].
To date, there are few systematic reviews and meta-analyses of research in sub-Saharan Africa (SSA) on the weight of pregnant women [29–31]. None addressed how much weight is gained during pregnancy by women in this population, or the effect on birth outcomes. Therefore, this systematic review and meta-analysis presents available evidence on the amount of GWG, factors affecting GWG and the association of GWG with birth outcomes, in sub-Saharan Africa.
Methods
The protocol and registration
The method of this systematic review and meta-analysis was reported using the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement recommendations [32] (S1 Table). We followed the flowchart from the PRISMA-P 2015 guideline recommendation to demonstrate the selection process from initially identified records to finally included studies [33]. The protocol for this review was registered on the International Prospective Register of Systematic Reviews (PROSPERO) registration number CRD42018085499 [34].
Search strategy
We identified literature from PubMed, Medline, Embase, Scopus, and CINAHL databases (S2 Table). We also accessed the African Journals Online (AJOL) database for papers published in country-specific or region-specific journals. A supplementary search was conducted to find grey literature from the Google search engine and Google Scholar. In addition, we contacted six authors to request additional information missing from their papers. However, only one author [35] responded to the email request. The search was limited to papers published since 1990 (when the IOM guideline was published [36]) to 2019 in sub-Saharan Africa and published in English. We employed the Medical Subject Headings (MeSH) terms, Emtree, CINAHL headings and combined keywords to identify studies in these databases. The search terms emerged from the following keywords (GWG, Weight gain during pregnancy, Birth outcome, Birth weight, Low birth weight, sub-Saharan Africa).
Eligibility criteria
We included cross-sectional, case-control, cohort and randomized controlled trials. We included studies that defined GWG as inadequate, adequate, or excess according to IOM recommendations, or mean GWG in total or in each trimester, and that explicitly reported for underweight, normal weight, overweight and obese women (based on pre-pregnancy BMI). We also included studies that classified GWG based on the researchers’ categories and studies that assessed the association of GWG with birth outcomes. We excluded the studies if they were duplicates; anonymous reports; not published in English language; systematic reviews and meta-analyses or studies that were unable to provide information about the adequacy of GWG. The primary outcome of interest in this study is GWG. Other outcomes were factors affecting GWG and the association between GWG and birth outcomes.
Study selection procedure
We located an initial set of studies by using the search terms and applying filters to the databases. We exported the identified studies to Covidence, a systematic review software [37], and we excluded duplicates. Two reviewers independently screened the studies based on titles and abstracts as per the inclusion criteria. During the screening process, we resolved any disagreements between the two reviewers through discussion. However, in the case of further disagreement, other authors made the final decisions.
Quality assessment
Two independent appraisers appraised the quality of the included studies. We used the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies [38] is to appraise the studies critically and to report the level of the strength of a study’s quality. The quality assessment tool uses a number of criteria to rate the strength of the studies. These criteria include the presence of selection bias, the strength of the study design, withdrawals and dropout rate, data collection practices, blinding as part of a controlled trial and how confounders were controlled. Each examined practice paper marked as “strong,” “moderate,” or “weak”. During appraisal, attention was given to the clear description of objectives, inclusion criteria, precision of measurement of the outcome (the time and how pre-pregnancy BMI and GWG were measured) and the appropriateness of statistical analyses.
Data extraction process
We used an excel spreadsheet for data extraction. Two reviewers extracted the data using a data extraction format which includes authors, year of publication, study design, sample size, the country of the study, objectives of the study, how GWG was measured, time at which pre-pregnancy BMI was measured, and the pre-pregnancy weight status of the women (underweight, normal-weight, overweight, and obese). We extracted data on GWG (mean for each category of pre-pregnancy weight, the percentage of inadequate, adequate or excess), factors affecting GWG and effects of GWG on birth-outcomes. Where the GWG categorisation did not follow the IOM categories, we used the categorisation used in the study.
Data analysis
Findings from each study were described by the country of the studies, population characteristics, women’s pre-pregnancy BMI, study design, study objectives, and outcomes. Outcomes, GWG, were reported using the IOM classification. For studies that used arbitrary classifications (for example, ≤ 8.0 kg (inadequate GWG), 8.1 to 16.0 kg (adequate GWG), and ≥16.1 kg (excessive GWG) [39]; or <7 kg (inadequate GWG), 7 to 12 kg (adequate t GWG), and >12 kg (excessive GWG) [40]), we used the authors’ own classifications.
We used forest plots to report the results graphically. We checked the presence of heterogeneity among studies using the chi-squared test where statistical significance with a p-value <0.05. The I2 statistic was used to quantify the level of heterogeneity among the studies. We assumed substantial heterogeneity among studies when the value of I2 was ≥50%. We used the Mantel–Haenszel fixed effects model to conduct meta-analyses where the studies did not have substantial heterogeneity (i.e. I2 statistic < 50%). We used random effects model while assessing the effect of gaining inadequate gestational weight on pre-eclampsia although the I2 value is <50%, because we have observed considerable heterogeneity among included studies. We pooled the percentages of inadequate, adequate and excess GWG. However, substantial heterogeneity was detected among studies (I2 value for inadequate, adequate and excess weight gain were 99.7%, 98.9% and 99.1% respectively) (S1 to S3 Figs). We stratified women into underweight, normal-weight, overweight and obese women to pool their GWG, but the I2 value within each group of the women was >95.0% (S4 to S6 Figs). The association between GWG and birth outcomes (LBW, Macrosomia, APGAR-score, caesarean section, obstetric hemorrhage, pre-eclampsia, and episiotomy) was determined using the Review Manager Software (RevMan version 5.3 for windows) [41]. We calculated risk ratios with 95% confidence intervals. However, due to high heterogeneity among studies and the limited number of studies (S3 and S4 Tables), we reported only the association between GWG and macrosomia and pre-eclampsia. Factors associated with GWG were classified differently among different studies. We used narrative synthesis to describe factors associated with GWG.
Results
Results of the screening process
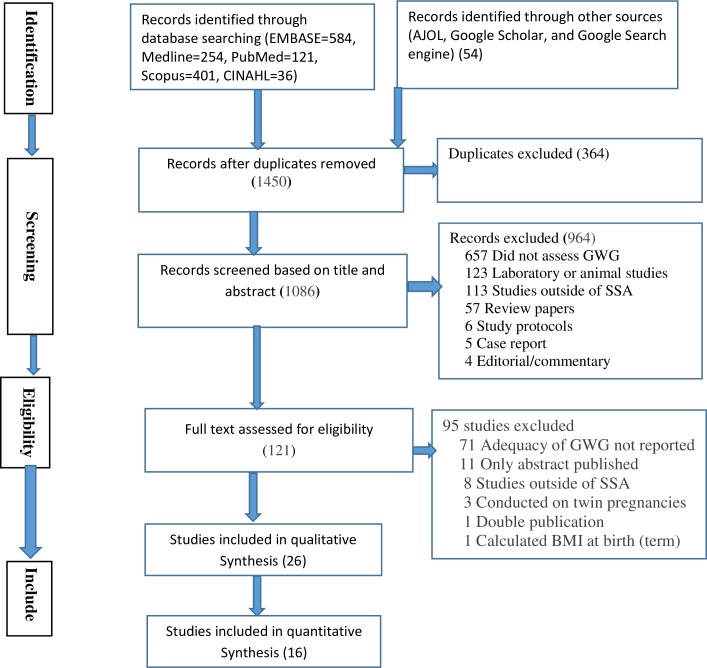
The search retrieved a total of 1450 studies. A total of 1086 articles were reviewed after removal of 364 duplicates. Based on title and abstract screening, we excluded 964 articles, and we conducted a full-text review on the remaining 121 studies left. We included 26 studies in the review. The most common reasons for exclusion were failure to report GWG according to IOM recommendations or failure to explicitly report pre-pregnancy weight specific GWG or only reporting weight gain that did not indicate the adequateness of GWG (Fig 1).
Fig 1. PRISMA flow diagram for article selection and screening.
Study characteristics
Table 1 describes the characteristics of the studies included in this review. Five studies were from Nigeria [6, 7, 42–44]; four from Cameroon [45–48]; four each from Ethiopia [2, 35, 49, 50] and Ghana [39, 51–53]; two studies from South Africa [54, 55] and Malawi [28, 56]; and one each from Uganda [9], Kenya [57], Niger [58], Benin [40], and the Democratic Republic of Congo [59]. Based on a country’s income status [60], two studies were from upper middle-income countries [54, 55]; fourteen from lower middle-income countries [6, 7, 39, 42–48, 51–53, 57] and ten from low-income countries [2, 9, 28, 35, 40, 49, 50, 56, 58, 59].
Table 1. Characteristics of the 21 studies reporting on gestational weight gain in relation to pre-pregnancy weight in sub-Saharan Africa, 2019.
| Author and year |
Country | Study design | Study settings | Sample size | Objective of the study | GWG Measure | Time at which pre-pregnancy BMI measured | Underweight (UW), normal-weight (NW), Overweight(OW and Obese (O) women Number (%) |
|---|---|---|---|---|---|---|---|---|
| Fouelifack FY et al 2015 [45] | Cameroon | Retrospective Cohort | Urban Referral hospital |
465 | To assess associations of BMI and GWG with pregnancy outcomes | IOM 2009 | Self-reported pre-pregnancy weight | UW = 17 (3.7) NW = 228(49) OW = 152(32.7) O = 65(14) |
| Mbu RE et al 2013 [46]* | Cameroon | Cross-sectional study | Urban Maternity hospital (type of the hospital is indicated) |
220 | To determine pregnancy outcomes among women who gained normal and excess gestational weight | IOM 2009 with modifications | Not clearly stated | Not clearly stated |
| Asefa F et al 2016 [2] | Ethiopia | Cross-sectional study |
Urban Both primary and referral hospitals |
411 | To assess GWG and associated factors | IOM 2009 | Before 16 weeks of gestation | UW = 39 (9.5) NW = 296(72) OW = 60(14.6) O = 16(3.9) |
| Halle-Ekane GE et al 2015 [47] | Cameroon | Cross-sectional study | Urban District hospitals |
350 | To determine the prevalence of excessive GWG, its risk factors, and effects on pregnancy outcomes | IOM 2009 | Before 13 weeks of gestation | UW = 8 (2.3) NW = 176 (50.3) OW = 115(32.8) O = 51(14.6) |
| Seifu B 2017 [35] | Ethiopia | Cross-sectional study | Urban Health centre, primary and referral hospitals |
549 | To compare GWG and its associated factors among HIV-positive and HIV-negative women | IOM 2009 | Before 16 weeks of gestation | UW = 107 (19.5) NW = 371 (67.6) OW = 65 (11.8) O = 6 (1.1) |
| Abubakari A et al 2015 [51] | Ghana | Cross-sectional study | Urban, peri-urban and rural Both primary and referral hospitals |
419 | To assess the association between pre-pregnancy BMI, GWG, maternal socio economic and demographic factors and birth weight | IOM 2009 | First trimester |
UW = 16 (3.8) NW = 242 (57.8) OW = 105 (25.0) O = 56 (13.3) |
| Wanyama R et al. 2016 [9] | Uganda | Cross-sectional study | Urban Health centre |
192 | To determining the prevalence of inadequate, adequate and excessive GWG | IOM 2009 | Self-reported pre-pregnancy weight | UW = 28 (14.6) NW = 143 (74.5) OW = 21 (10.9) O = 0 |
| Wrottesley SV et al 2017 [54] | South Africa | Prospective cohort study | Urban Teaching hospitals |
538 | To assess patterns of habitual dietary intake and their associations with first trimester BMI and GWG | IOM 2009 | Before 20 weeks of gestation | UW = 0 NW = 182 (33.8) OW = 190 35.3) O = 166 (30.9) |
| Chithambo SET 2017 [56] | Malawi | Longitudinal study (Cohort) | Rural Community based |
257 | To identify factors associated with the rate of GWG | IOM 2009 | Before 24 weeks of gestation | UW = 18 (7.0) NW = 201 (78.2) OW = 38 (14.8) O = 0 |
| Esimai OA et al 2014 [7] | Nigeria | Longitudinal (cohort)study | Urban vs rural is not clearly stated Primary health facilities |
590 | To determine correlates of gestational weight gain and infant birth weight | IOM 2009 with some operational definition (<7 kg low, >7 kg high) | First 2 months of pregnancy |
UW = 47 (8.0) NW = 482 (81.7) OW = 46 (7.8) O = 15 (2.5) |
| Iyoke CA et al 2013 [42] | Nigeria | Retrospective cohort | Urban Teaching hospitals |
648 | To compare GWG and obstetric outcomes between obese and normal weight women | IOM 2009 | First trimester | UW = NA NW = 324 (50.0) OW = NA O = 324 (50.0) |
| Adu-Afarwuah S et al 2017 [52] | Ghana | Randomized Controlled Trial | Semi-urban Primary hospitals and poly clinic |
1320 | To determine the association of SQ-LNSs with differences in GWG or maternal anthropometric characteristics, including risk of overweight or obesity | IOM 2009 and INTERGROWTH-21st guidelines | Before 20 weeks of gestation | UW = 50 (3.8) NW = 743 (56.3) OW = 354 (26.8) O = 143 (10.8) |
| Nomomsa D et al 2014 [49] | Ethiopia | Cross-sectional study | Urban Both primary and referral hospitals |
411 | To assess the association of GWG and LBW | IOM 2009 | Before 16 weeks of gestation | UW = 39 (9.5) NW = 296(72) OW = 60(14.6) O = 16(3.9) |
| Muyayalo KP et al 2017 [59] | Democratic Republic of Congo | Prospective Cohort |
Urban Referral hospitals |
199 | To determine proportion of post-partum weight retention and its average level; to identify its risk factors; to determine the proportion of obese women 6 weeks after delivery. | IOM 2009 | Before 20 weeks of gestation | UW = 11 (5.5) NW = 111 (55.8) OW = 56 (28.1) O = 21 (10.6) |
| Ismail LC et al 2016 [57] | Kenya | longitudinal (cohort) study | Urban (institution where the study collected was not clearly indicated) | Varies§ | To describe patterns in maternal gestational weight gain in healthy pregnancies with good maternal and perinatal outcomes | Mean GWG at each month of follow-up and INTERGROWTH-21st† | Before 14 weeks of gestation | All were normal weight women |
| Addo VN 2010 [39] | Ghana | Cross-Sectional study | Urban vs rural is not clearly stated Private specialist Hospital |
1755 | To find out the effects of pregnancy weight gain in different BMI groups on maternal and neonatal outcomes | Operationally defined (Low weight gain ≤ 8.0 kg, Normal weight gain 8.1 to 16.0 kg, High weight gain ≥16.1 kg) |
Between 10 and 13 weeks of Gestation |
UW = 77 (4.4) NW = 832 (47.4) OW = 609 (34.7) O = 314 (17.9)‡ |
| Onwuka CI et al. 2017 [6] | Nigeria | Longitudinal (cohort) study | Urban Teaching hospitals |
200 | To determine the pattern of GWG and its association with birth weight | Operationally defined (<10 kg inadequate, 10 to 15 kg adequate, >15 kg excess) | Before 14 weeks of gestation | UW = 7 (3.5) NW = 102 (51.0) OW = 35 (17.5) O = 56 (28.0) |
| Elie N et al 2015 [48] | Cameroon | Cross-sectional study | Urban University teaching hospital |
232 | To identify risk factors for a baby born with macrosomia | Operationally defined (<16 kg and ≥16 kg) | Before 20 weeks of gestation but from maternal recall before she realized pregnancy | UW = 0 NW = 114 (49.1) OW & O = 118(50.9) |
| Onyiriuka A.N 2006 [43] | Nigeria | Cross-sectional study | Urban Referral Hospital |
408 | To determine the incidence of delivery of HBW (macrosomia) |
Operationally defined (<10 kg, 10 to 12 kg, 13 to 15 and >15 kg) | First trimester | Not reported |
| Akindele RL et al 2017 [44] | Nigeria | Case–control study | Urban Major public hospitals (type of the hospitals are not indicated) |
240 | To determine the incidence of macrocosmic new-borns, their maternal socio-biologic predictors, the neonatal complications attributable to the mode of delivery, and their early neonatal outcome |
Operationally defined (<15 kg and ≥15 kg) | Self-reported pre-pregnancy weight | UW, NW & OW = 172 (71.7) O = 68 (28.3) |
| Ward E et al 2007 [55] | South Africa | Longitudinal (cohort) study | Urban vs rural is not clearly stated Primary health care clinic |
89 | To evaluate the association between pre-pregnancy BMI and maternal pregnancy weight gain and pregnancy outcome | IOM 1990 | 14 weeks of Gestation | UW = 14 (15.7) NW = 45 (50.6) OW & O = 28 (31.5) |
| Ouédraogo CT et al 2019 [58] | Niger | Cross-sectional study | Community‐based survey | 1386 | To estimate the prevalence and the determinants of low GWG and low mid-upper arm circumference | IOM 2009 and INTERGROWTH-21st guidelines | Not clear (women included regardless of their gestational age) | Not reported |
| Gondwe A et al 2018 [28] | Malawi | Retrospective cohort nested with randomized controlled trial | Semi-urban and semi-rural Private hospital and public health centre |
1287 | To examined whether maternal pre-pregnancy BMI and GWG are associated with birth outcomes | IOM 2009 | Before 20 weeks of gestation | UW = 76 (5.9) NW = 1071 (83.2) OW & O = 140 (10.9) |
| Agbayizah DE 2017 [53] | Ghana | Cross-sectional study | Urban Semi-urban Rural General Hospital |
322 | To assess the prevalence of inadequate, adequate and excessive GWG and its associated factors | IOM 2009 | Before 20 weeks of gestation | UW = 3 (1.0) NW = 164 (50.9) OW = 119 (36.9) O = 56 (11.2) |
| Agbota G et al 2019 [40] | Benin | Longitudinal (cohort) study | Semi-urban and Rural; institution where the study collected was not clearly indicated |
260 | To assess the effect of maternal anthropometric status before conception and during pregnancy on fetal and postnatal growth, up to 12 months of age | Operationally defined (<7 kg, 7 to 12 kg and >12 kg) | Before 7 weeks of gestation | UW = 23 (8.9) NW = 175 (67.3) OW = 43 (16.5) O = 19 (7.3) |
| Tela FG et al 2019 [50] | Ethiopia | Cross-sectional study | Urban Private clinics |
309 | To determine the prevalence of macrosomia and investigate the associated risk factors | Operationally defined (<16 kg, ≥16 kg) | Around 12 weeks of gestation | UW = 28 (9.0) NW = 173 (56.0) OW = 76 (24.6) O = 32(10.4) |
*intentionally included equal number of women who gained excessive gestational weight and who gained adequate gestational weight to compare their birth outcomes
†International Fetal Newborn Growth Standards for the 21st Century -INTERGROWTH-21st (This study is a multicenter study including one sub-Saharan African country, Kenya. However, the GWG according to the INTERGROWTH-21st standard was not explicitly reported for Kenya)
‡ the summation of the described numbers of UW, NW, OW and O women is greater than the described total sample size.
§Varies across Gestational ages (355 for 14–18+6 weeks, 356 for 19–23+6 weeks, 360 for 24–28+6 weeks, 355 for 29–33+6 weeks, 388 for 34–40+0 weeks)
Sixteen studies [2, 7, 9, 28, 35, 42, 45, 47, 51–56, 58, 59] classified the outcome (GWG) according to the IOM recommendations, but for seven studies [6, 39, 40, 43, 44, 48, 50] standard criteria were not used to measure and classify the outcome, that is the authors classified weight gain using their own method. Three studies reported according to the International Fetal Newborn Growth Standards for the 21st Century (INTERGROWTH-21st) guidelines [52, 57, 58], of which two studies [52, 58] used both IOM 2009 and INTERGROWTH-21st guidelines. The authors of one study stated that they used the IOM classification, but they also reported normal weight gain as “women with BMIs between 18.5 kg/m2 and 30 kg/m2 and who gained 9 to 16 kg; excessive weight gain for those who gained weight above these ranges” [46]. Eight studies reported GWG separately for each category of woman’s pre-pregnancy weight [2, 7, 9, 35, 42, 53, 54, 56], and the author of one study provided these data upon email request [35]. Four studies [9, 44, 45, 48] used self-reported pre-pregnancy weight while three studies [52, 54, 59] used weight after 20 weeks of gestation and one study [56] used weight at 24 weeks of gestation. It was not clear when and how pre-pregnancy weight was measured in two studies [46, 58] (Table 1).
Critical appraisal results
In two studies, loss to follow-up was not well described. In one of these studies [7], a cohort of 1000 women was recruited, but the authors reported the results of 590 women, but there was not an adequate description of loss to follow-up of the remaining 410 women. Poor control of confounding factors was also an issue affecting the quality of the studies [6, 9, 39, 42, 43, 46–48]. These studies either did not control for confounding factors at all or did not include all necessary variables into the analysis (partially controlled) or did not report how confounding was controlled. According to our quality assessment, 17 studies had moderate quality, while the remaining 10 studies had weak quality. Except for one study [52], all included studies were observational studies (Table 2).
Table 2. Summary of the quality of included studies according to the Effective Public Health Practice Project Quality Assessment Tool for Quantitative Studies, 2019.
| Author and year |
Selection bias | Study design | Confounder | Blinding | Data collection method | Withdrawal and dropout | Overall strength |
|---|---|---|---|---|---|---|---|
| Fouelifack FY et al 2015 [45] | Moderate | Weak | Moderate | NA* | Moderate | Strong | Moderate |
| Mbu RE et al 2013 [46] | Weak | Weak | Weak | NA | Moderate | Weak | Weak |
| Asefa F et al 2016 [2] | Moderate | Weak | Strong | NA | Moderate | Strong | Moderate |
| Halle-Ekane GE et al 2015 [47] | Strong | Weak | Weak | NA | Strong | Strong | Weak |
| Seifu B 2017 [35] | Moderate | Weak | Moderate | NA | Moderate | Strong | Moderate |
| Abubakari A et al 2015 [51] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Wanyama R et al. 2016 [9] | Moderate | Weak | Weak | NA | Strong | Strong | Weak |
| Wrottesley SV et al 2017 [54] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Chithambo SET 2017 [56] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Esimai OA et al 2014 [7] | Moderate | Weak | Moderate | NA | Strong | Weak | Weak |
| Iyoke CA et al 2013 [42] | Moderate | Weak | Weak | NA | Strong | Strong | Weak |
| Adu-Afarwuah S et al 2017 [52] | Strong | Strong | Strong | Weak | Strong | Strong | Moderate |
| Nemomsa D et al 2014 [49] | Moderate | Weak | Strong | NA | Moderate | Strong | Moderate |
| Muyayalo KP et al 2017 [59] | Moderate | Weak | Strong | NA | Moderate | Strong | Moderate |
| Ismail LC et al 2016 [57] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Addo VN 2010 [39] | Moderate | Weak | Weak | NA | Moderate | Strong | Weak |
| Onwuka CI et al. 2017 [6] | Moderate | Weak | Weak | NA | Strong | Strong | Weak |
| Elie N et al 2015 [48] | Strong | Weak | Weak | NA | Strong | Strong | Weak |
| Onyiriuka A.N 2006 [43] | Strong | Weak | Weak | NA | Strong | Strong | Weak |
| Akindele RL et al 2017 [44] | Moderate | Weak | Strong | NA | Strong | Strong | Moderate |
| Ward E et al 2007 [55] | Moderate | Weak | Moderate | NA | Moderate | Strong | Moderate |
| Ouédraogo CT et al 2019 [58] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Gondwe A et al 2018 [28] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Agbayizah DE 2017 [53] | Moderate | Weak | Moderate | NA | Strong | Strong | Moderate |
| Agbota G et al 2019 [40] | Strong | Weak | Strong | NA | Strong | Strong | Moderate |
| Tela FG et al 2019 [50] | Moderate | Weak | Moderate | NA | Moderate | Strong | Moderate |
*Not-applicable
Gestational weight gain classifications
Gestational weight gain according to IOM classification
Sixteen studies reported the percentage of GWG according to IOM recommendations. The percentage of women with inadequate GWG ranged from 15.7% to 96.6% [7, 55]. The percentage of women with adequate GWG ranged from 3% to 62% [7, 42]. Nine of the 16 studies reported the percentage of women with inadequate GWG as >50% [2, 7, 9, 28, 35, 52, 56, 58, 59] and the percentage of women with adequate GWG as <30% [2, 7, 28, 35, 52–54, 56, 58, 59]. The smallest percentage of inadequate GWG (15.7%)[55] and the highest percentage of excessive GWG (55.5%) [54] were from South Africa. In 11 of the 16 studies, the percentage of women with excessive GWG was <20% [2, 7, 9, 28, 35, 42, 51, 52, 56, 58, 59] (Table 3).
Table 3. Studies describing proportions of inadequate, adequate and excess gestational weight gain in Sub-Saharan Africa according to the United State Institute of Medicine recommendations, 2019.
| Authors and year | Sample Size | Inadequate GWG n (%) | Adequate GWG n (%) | Excess GWG n (%) |
|---|---|---|---|---|
| Chithambo SET et al. 2017 [56] | 257 | 206 (80.2) | 51 (19.8) | 0 (0.0) |
| Asefa F et al. 2016 [2] | 411 | 285 (69.3) | 115 (28.0) | 11 (2.7) |
| Seifu B et al. 2017 [35] | 549 | 369 (67.2) | 160 (29.2) | 20 (3.6) |
| Wanyama R et al. 2016 [9] | 192 | 120 (62.5) | 66 (34.4) | 6 (3.1) |
| Esimai OA et al 2014 [7] | 590 | 570 (96.6) | 18 (3.1) | 2 (0.3) |
| Abubakari A et al 2015 [51] | 419 | 208 (49.6) | 180 (43.0) | 31 (7.4) |
| Adu-Afarwuah S et al 2017 [52] | 1030 | 646 (62.7) | 277 (26.9) | 107 (10.4) |
| Muyayalo K P et al 2017 [59] | 199 | 117 (58.8) | 52 (26.1) | 30 (15.1) |
| Iyoke CA et al 2013 [42] | 648 | 121 (18.7) | 400 (61.7) | 127 (19.6) |
| Halle-Ekane GE et al 2015 [47] | 350 | 129 (36.9) | 114 (32.6) | 107 (30.6) |
| Fouelifack FY et al 2015 [45] | 462 | 131 (28.0) | 186 (40.0) | 145 (32.0) |
| Wrottesley SV et al 2017 [54] | 538 | 128 (24.0) | 113 (21.0) | 297 (55.5) |
| Ward E et al 2007 [55] | 89 | 14 (15.7) | 46 (51.7) | 29 (29.6) |
| Ouédraogo CT et al 2019 [58] | 911 | 574 (63.0) | 218 (24.0) | 119 (13.0) |
| Gondwe A et al 2018 [28] | 1287 | 924 (71.8) | 296 (23.0) | 67 (5.2) |
| Agbayizah ED 2017 [53] | 322 | 73 (22.7) | 94 (29.2) | 155 (48.1) |
Of the eight studies [2, 7, 9, 35, 42, 53, 54, 56] that reported GWG separately for each category of women’s pre-pregnancy weight, two studies had no underweight women [42, 54] or obese women [9, 56], while one study had no overweight women [42]. According to the six studies that had underweight women [2, 7, 9, 35, 53, 56], more than 67% of underweight women were reported to have gained inadequate gestational weight. In four studies [2, 7, 9, 56], more than two-thirds of normal weight women gained inadequate gestational weight, but in three studies [42, 53, 54], nearly one -third of normal weight women gained inadequate gestational weight. As pre-pregnancy BMI of the women increased, the percentage of those with adequate GWG increased (7.7% among underweight women and 62.5% among obese women [2]; 2.1% among underweight women and 93.3% among obese women [7]) (Table 4).
Table 4. Proportions of inadequate, adequate and excess gestational weight gain according to pre-pregnancy weight of the women in Sub-Saharan Africa, 2019.
| Authors and year | Pre-pregnancy weight status of the women | Inadequate GWG n (%) | Adequate GWG n (%) | Excess GWG n (%) |
Total n |
|---|---|---|---|---|---|
| Asefa F et al 2016 [2] | Underweight | 35 (89.7) | 3 (7.7) | 1 (2.6) | 39 |
| Normal weight | 222 (75.0) | 71(24.0) | 3 (1.0) | 296 | |
| Overweight | 23 (38.3) | 31 (51.7) | 6 (10.0) | 60 | |
| Obese | 5(31.2) | 10 (62.5) | 1(6.3) | 16 | |
| Total | 285(69.3) | 115 (28.0) | 11(2.7) | 411 | |
| Wanyama R et al 2016 [9] | Underweight | 20 (71.4) | 8 (28.6) | 0 (0.0) | 28 |
| Normal weight | 98 (68.5) | 43 (30.1) | 2 (1.4) | 143 | |
| Overweight | 2 (9.5) | 15 (71.4) | 4 (19.1) | 21 | |
| Obese | 0(0.0) | 0(0.0) | 0(0.0) | 0 | |
| Total | 120 (62.5) | 66 (34.4) | 6 (3.1) | 192 | |
| Wrottesley SV et al 2017 [54] | Underweight | 0(0.0) | 0(0.0) | 0(0.0) | 0 |
| Normal weight | 54 (29.7) | 54 (29.7) | 74 (40.6) | 182 | |
| Overweight | 38 (20.0) | 32 (16.8) | 120 (63.2) | 190 | |
| Obese | 36 (21.7) | 27 (16.3) | 103 (62.0) | 166 | |
| Total | 128 (23.8) | 113 (21.0) | 297 (55.2) | 538 | |
| Chithambo SET et al 2017 [56] | Underweight | 16 (88.9) | 2 (11.1) | 0(0.0) | 18 |
| Normal weight | 163 (81.1) | 38 (18.9) | 0(0.0) | 201 | |
| Overweight | 27 (71.1) | 11 (28.9) | 0(0.0) | 38 | |
| Obese | 0(0.0) | 0(0.0) | 0(0.0) | 0 | |
| Total | 206 (80.2) | 51 (19.8) | 0(0.0) | 257 | |
| Esimai OA et al 2017 [7] | Underweight | 46 (97.9) | 1 (2.1) | 0(0.0) | 47 |
| Normal weight | 479 (99.4) | 2 (0.4) | 1 (0.2) | 482 | |
| Overweight | 45(97.8) | 1 (2.2) | 0(0.0) | 46 | |
| Obese | 0(0) | 14 (93.3) | 1 (6.7) | 15 | |
| Total | 570 (96.6) | 18 (3.1) | 2 (0.3) | 590 | |
| Iyoke CA et al 2013 [42] | Underweight | NA* | NA* | NA* | NA* |
| Normal weight | 109 (33.6) | 126 (38.9) | 89 (27.5) | 324 | |
| Overweight | NA* | NA* | NA* | NA* | |
| Obese | 12 (3.7) | 274 (84.6) | 38 (11.7) | 324 | |
| Total | 121 (18.7) | 400 (61.7) | 127 (19.6) | 648 | |
| Seifu B 2017 [35] | Underweight | 84 (78.5) | 20 (18.7) | 3 (2.8) | 107 |
| Normal weight | 268 (72.2) | 94 (25.4) | 9 (2.4) | 371 | |
| Overweight | 15 (23.1) | 44 (67.7) | 6(9.2) | 65 | |
| Obese | 2 (33.3) | 2 (33.3) | 2 (33.3) | 6 | |
| Total | 369 (67.2) | 160 (29.1) | 20 (3.7) | 549 | |
| Agbayizah ED 2017 [53] | Underweight | 2 (66.7) | 1 (33.3) | 0 (0.0) | 3 |
| Normal weight | 52 (31.7) | 62 (37.8) | 50 (30.5) | 164 | |
| Overweight | 9 (7.6) | 25 (21.0) | 85 (71.4) | 119 | |
| Obese | 10 (27.8) | 6 (16.7) | 20 (55.5) | 36 | |
| Total | 73 (22.7) | 94 (29.2) | 155 (48.1) | 322 |
NA*-Not applicable- because the authors (Iyoke et al) intended to compare GWG among normal weight and obese women, and they intentionally excluded underweight and overweight women
Mean gestational weight gain
According to one study, mean GWG (± standard deviation) was 1.52±1.65 kg during 14 to 18+6 weeks; 2.57±1.46kg during 19 to 23+6 weeks; and 2.48±1.29 kg during 24 to 28+6 weeks. Similarly, GWG during 29 to 33+6 weeks, and 34 to 40+0 weeks was 2.18 ±1.39 kg and 2.42±2.41 kg, respectively [57]. According to the study from Uganda weekly mean GWG of 0.32 kg, 0.30 kg and 0.28 kg were reported among underweight, normal-weight and overweight women, respectively [9]. In another study, the mean GWG was 9.14±3.46 among underweight women; 9.26±3.14 kg among normal-weight women; 8.03±3.64 kg among overweight women, and 6.44±3.46 kg among obese-women [2]. Onwuka et al also reported a mean GWG of 10.21±2.90 kg among underweight women; 11.50±2.82 kg among normal-weight women; 10.30±3.98 kg among overweight women; and 9.54±3.65 kg among obese women [6].
Gestational weight gain according to INTERGROWTH-21st standard
Three studies reported GWG according to the INTERGROWTH-21st standard [52, 57, 58]. One study reported that 27.5% of pregnant women gained gestational weight less than the third centile which is considered insufficient; 82.7% gained gestational weight less than the 50th centile; and 2.0% gained gestational weight above the 97th centile which is considered excess [58]. The other study reported that 26.8% of women with normal weight gained gestational weight less than the third centile, and none gained above the 97th centile [52].
Gestational weight gain according to authors’ classifications
Akindele et al reported that 72.9% of women gained < 15 kg [44]; Onyiriuka reported that 42.9% of women gained < 10 kg [43]; Nkwabong reported that 75% of women gained <16 kg. [48]; Onwuka et al reported that 36.0% of women gained <10 kg [6], and Addo reported 14.8% of women gained ≤ 8.0 kg [39] (Table 5).
Table 5. Proportions gestational weight gain in sub-Saharan Africa according to authors’ classification, 2019.
| Authors and year | Sample size | GWG classifications in kilogram | N (%) |
|---|---|---|---|
| Akindele et al 2017 [44] | 240 | <15 | 175 (72.9) |
| ≥15 | 65 (27.1) | ||
| Onyiriuka 2006 [43] | 408 | <10 | 175(42.9) |
| 10 to 13 | 95 (23.3) | ||
| 13.1 to 15 | 129 (31.6) | ||
| ≥15 | 9 (2.2) | ||
| Elie N et al 2015 [48] | 232 | <16 | 174 (75.0) |
| ≥16 | 58 (25.0) | ||
| Onwuka et al 2017 [6] | 200 | <10 | 72 (36.0) |
| 10 to15 | 107 (53.5) | ||
| ≥15 | 21 (10.5) | ||
| Addo VN 2010 [39] | 1755 | ≤8 | 259 (14.8) |
| 8.1 to 16 | 1385 (78.1) | ||
| ≥16 | 111 (6.3) | ||
| Agbota G et al 2019 [40] | 253 | <7 kg | 65 (25.7) |
| 7 to 12 kg | 132 (52.2) | ||
| >>12 kg | 56 (22.1) | ||
| Tela FG et al 2019 [50] | 309 | <16 kg | 276 (89.3) |
| ≥16 kg | 33 (10.7) |
Factors associated with gestational weight gain
Four studies reported factors associated with gaining weight according to IOM recommendations [2, 35, 52, 56]. These factors include pre-pregnancy weight [2, 35], having at least four ANC visits [2], engaging in physical activity [2, 35], income [2, 35], type of food consumption [2], knowledge about the importance of fruit [35], education [7, 35], type of food supplementation [52], and seasonality [56]. These factors are described below.
Maternal pre-pregnancy weight
According to two studies from Ethiopia [2, 35], women’s early pregnancy BMI was associated with GWG. Asefa et al reported that overweight and obese women were three times more likely to gain adequate gestational weight as compared to underweight women [2]. Similarly, Seifu reported that overweight and obese women were fourteen times more likely to have adequate GWG than those who were underweight [35].
Food consumption and physical activity
Mothers’ knowledge of the inclusion of fruits as a main food type during pregnancy was associated with gaining adequate gestational weight [35]. The women who ate fruit, vegetables, and meat at least once a week were more likely to gain adequate gestational weight compared with their counterparts [2]. According to Adu-Afarwuah et al, the percentage of women with adequate GWG was significantly higher in the group of women who received lipid-based nutrition supplementation than in a group who received multiple micronutrients and iron and folic acid supplementation [52]
Asefa et al reported that undertaking physical activity at least once a week for no less than 30 minutes was associated with higher likelihood of gaining adequate gestational weight [2]. Saifu also reported that engaging in physical activity up-to six hours a week was associated with gaining adequate gestational weight [35].
Income, occupation, and social class
One study reported that having a monthly family income of > $US100 was associated with gaining adequate gestational weight, while another study reported monthly income >$US150 as a factor associated with adequate GWG [2, 35]. According to Onwuka et al, women from a higher social class were more likely to gain weight of 10 to15 kg [6]. Being employed was reported as associated with gaining gestational weight of >7 kg [7].
Maternal age and parity
One study reported that being an adolescent (≤18 years of age) was associated with gaining gestational weight greater than 7 kg [7]. Another study reported that being younger than 35 years of age was associated with gaining gestational weight of 10 to 15 kg [6]. These two studies reported that being nulliparous was associated with gaining gestational weight of >7 kg [7] and 10 to 15 kg [6]. However, these associations are crude associations (not adjusted for confounders). According to Ouédraogo et al one increase in the number of pregnancies that a woman had was associated with increased odds of GWG below the 50th centile (OR, 1.11, 95% CI: 1.03, 1.20) [58]
ANC visits
Attending ANC four or more times was associated with gaining adequate gestational weight [2]. In addition, another study identified that having had regular ANC visits was associated with gaining gestational weight of 10 to 15 kg [6].
Effect of GWG on birth outcomes
Low birthweight
An association between GWG and LBW was reported in some studies from SSA [42, 49, 51, 61].
Nemomsa et al reported that 17.5% of women who gained inadequate gestational weight gave birth to LBW babies, while 1.7% of women who gained adequate gestational weight gave birth to LBW babies[49]. Gondwe et al also reported that 15.6% of women who gained inadequate gestational weight gave birth to LBW babies; 7.6% of women who gained adequate gestational weight gave birth to LBW babies [28]; and none of the women who gained excess gestational weight in Nemomsa et al [49] and Gondwe et al [28] gave birth to LBW babies. In another study, 8.6% of women who gained inadequate weight, 11.5% of women who gained adequate weight, and 6.9% of women who gained excess gestational weight gave birth to LBW babies [45]. In another study, the proportion of LBW was 9.7% and 2.3% among women who gained < 10 kg and 10 to 15 kg, respectively [6].
Macrosomia
Seven studies reported an association between GWG and macrosomia [6, 43–47, 50]. Of these, five studies defined macrosomia as birth weight of ≥ 4 kg [6, 43–45, 50], while two studies did not clearly show how they defined macrosomia [46, 47]. Of the total seven studies, three studies classified GWG according to IOM [45–47], while the remaining four studies classified GWG according to their authors own classification [6, 43, 44, 50]. The percentage of a baby born with macrosomia was 30.9% [46], 11.0% [45] and 9.3% [47] among women who gained excessive gestational weight, while it was 3.9% [47] and 3.2% [45] among women who gained inadequate gestational weight. In other studies, the percentage was 83.1% [44], 66.7% [43], and 38.1% [6] among women who gained >15 kg, while it was 2.8% [6] and 20% [43] among women who gained <10 kg. Tela et al reported that 54.5% of women who gained ≥16 kg gave birth to a baby born with macrosomia while 16% of women who gained <16 kg gave birth to a baby born with macrosomia [50]. There was no statistically significant difference regarding giving birth to a baby born with macrosomia among women who gained adequate and excess gestational weight (RR, 0.68; 95% CI: 0.38, 1.50, P = 0.20), but this was based on two studies only (Fig 2).
Fig 2. The association of excess gestational weight gain and macrosomia in sub-Saharan Afric.

Caesarean section and episiotomy
The percentage of caesarean section in two studies was 17% [47] and 26% [45] among women who gained inadequate gestational weight. The percentage was 10% [46], 16.7% [47], and 37% [45] among women who gained adequate weight; and 17.8% [47], 27.3% [46] and 50.3% [45] among women who gained excess gestational weight. According to Halle-Ekane et al, the percentages of episiotomy were 13.2%, 8.8% and 7.5% among women who gained inadequate, adequate and excess gestational weigh, respectively [47].
Pre-eclampsia
Pre-eclampsia was reported among 3.1% [47] and 7.5% [45] of women who gained inadequate gestational weight; 1.8% [47] and 6.4% [46] among those who gained adequate gestational weight; 15% [47], 18.2% [46], and 12.4% [45] among women who gained excess gestational weight. However, no significant difference was observed among women who gained inadequate compared with women who gained adequate gestational weight regarding predisposition to pre-eclampsia (RR, 0.71; 95% CI: 0.22, 2.28, P = 0.57) (Fig 3).
Fig 3. The association of inadequate GWG and pre-eclampsia in sub-Saharan Africa.

Discussion
The percentage of inadequate GWG was >50% among nine of the 16 studies that classified GWG according IOM recommendations, and the percentage of inadequate GWG was particularly high among underweight women, ranging from 67% to 98%. High percentages of inadequate GWG were reported from low-income Sub-Saharan African countries (80% and 71.8% from Malawi [28, 56], 69.3% and 67.2% from Ethiopia [2, 35], 63% from Niger [58], 62.7% from Uganda [9], and 58.8% from Democratic Republic of Congo [59]) compared to middle-income countries (28% and 36.9% from Cameroon [45, 47], 15.7% and 24% from South Africa [54, 55]). Unlike in other high-income [20, 24, 62, 63] and middle-income [64] countries where many pregnant women experience excessive GWG, all of the studies from low-income Sub-Saharan countries [2, 9, 28, 35, 56, 58, 59] reported that more than 58% of pregnant women experienced inadequate GWG. This could be due to the inability of women to consume adequate food because of accessibility and affordability problems [65]. Pregnant women in low-income Sub-Saharan African countries suffer from a wide range of nutritional problems due to poverty, food insecurity and frequent infections [66]. Among seven of the sixteen studies, the percentages of women who gained excessive gestational weight were <10%. Five of these seven studies were from low-income countries (Ethiopia, Uganda and Malawi), and the percentage of excessive GWG among these studies were reported to be <6%. Seven studies where more than 10% the women gained excessive were from middle-income countries of Sub-Saharan Africa (Ghana, Nigeria, Cameroon, and South Africa). In South Africa, the percentage of women with excessive GWG was as high as 55%, which is even higher than for some studies from high-income countries such as Canada (49%) [67] and Australia (46%) [68]. The high percentage of excessive GWG may be explained by South Africa being an upper-middle income country [60], and 66% of participants in the South African study [54] were either overweight or obese. The finding of high levels of GWG in middle-income countries suggests the importance of low-income Sub-Saharan African countries designing strategies to prevent excessive GWG before it becomes a public health problem as these countries transition to middle-income countries.
While we pooled the percentages of the percentages of inadequate, adequate and excess GWG, substantial heterogeneity have been detected among studies, which may be explained by a number of factors. Firstly, the GWG classifications were inconsistent. Some authors classified GWG using the IOM recommendations while others used their own classifications. Secondly, studies were in different sub-Saharan African countries that had very different income levels, including upper middle- income, lower middle-income and lower-income countries. For example, a study from South Africa [54] reported that 55% of pregnant women gained excess gestational weight, whereas no women from Malawi [56] and <3% of pregnant women from Ethiopia [2, 35] and Uganda [9] gained excess gestational weight. Thirdly, some studies were conducted in urban settings and in tertiary hospitals [42, 45], while others were conducted in semi-urban and rural [28, 51, 52, 56] settings in primary health care facilities. A study conducted in Nigeria in primary health care facilities [7] reported that 96.6% of pregnant women gained inadequate gestational weight. A study conducted in rural Malawi [56] showed that 80.2% of the pregnant women gained inadequate weight. By contrast the percentage of inadequate gestational weight gain was <30% among studies conducted in urban settings and tertiary hospitals [42, 45]. Finally, the difference in the pre-pregnancy weight of the participants may have affected the heterogeneity among studies. A study from South Africa [54] reported no underweight women; 66.2% of study participants were overweight and obese; and 55% of the participants gained excessive gestational weight. By contrast, studies from Malawi [56] and Uganda [9] had no obese women, and reported ≤ 3% of their participants gained excessive gestational weight.
This review identified that a number of factors that were associated with GWG including pre-pregnancy weight [2, 35], number and frequency of ANC visits [2], engaging in physical activity [2, 35], income [2, 35], type of food consumption [2], knowledge about the importance of fruit [35], education [7, 35], and type of food supplementation [52]. However, the inconsistent classification of the factors and poor control for confounding effects among the included studies made the findings of this review inconclusive.
The pre-pregnancy weight of women is associated with the amount of weight gained during pregnancy. Other studies have also reported that pre-pregnancy BMI is strongly associated with GWG [69–71]. This is because pre-gestational BMI is closely linked to maternal nutrition, lifestyle and socio-cultural factors, which could have an impact on the amount of GWG [72]. In this review, studies that have reported higher percentage of excessive GWG (for example, >30%) had a higher percentage of overweight and obese women (>46%) [45, 47, 53, 54]. Studies that have reported lower percentage of excessive GWG (<6%) had lower percentage of overweight and obese women (<15%) [2, 7, 9, 28, 35, 56]. These findings are supported by other studies that reveal a high BMI (overweight or obese) at the inception of pregnancy is associated with gaining weight above the IOM recommendations [70, 71]. In this review, the percentage of inadequate GWG ranged from 67% to 98% among underweight women [2, 7, 9, 35, 53, 56]. It may be difficult for underweight women to gain a sufficient amount of gestational weight, particularly if they tend to be underweight due to metabolic or food security factors [2]. Despite the association between pre-pregnancy weight and GWG, interventions on GWG managements took place mainly during pregnancy and focussed on reducing in GWG [73–76]. This implies that future interventions would need to focus on pre-pregnancy weight management strategies and its effectiveness. Weight management strategies should be inclusive by encouraging the reduction in GWG for women who are susceptible to excessive weight gain or encouraging weight gain for women who are susceptible to inadequate weight gain.
An association between GWG and birth weight has been reported by several studies [17, 77–79], and women who gain inadequate gestational weight are at an increased risk of having a baby with LBW or a pre-term birth [21, 80–82]. In the studies in this review, the majority of LBW babies were born to women who gained inadequate gestational weight. By contrast, a large percentage of women who gained excessive gestational weight (30%) gave birth to a baby born with macrosomia. However, the association between GWG and birth weight (LBW and macrosomia) were not statistically significant in the review that could be because of the small numbers of studies (only two studies) and small sample size (for example, only 6 of 196 [45], and 5 of 134 [47] pregnant women who gained inadequate gestational weight gave birth to a baby born with macrosomia). Several studies have reported that gaining GWG outside of IOM recommendations is associated with different adverse pregnancy outcomes such as caesarean section [23, 69], episiotomy, low Apgar score at first and fifth minutes [83–85], antepartum haemorrhage, and pre-eclampsia [21]. However, given the inclusion of a limited number of studies in the meta-analyses, large differences in the settings among studies, and the inconsistent classification of GWG, these factors were not significantly associated with GWG outside of IOM recommendations in this analysis.
There were several issues relating to the quality of studies in the review. Firstly, the measurement of pre-pregnancy weight of the women was problematic, with four studies [9, 44, 45, 48] using self-reported pre-pregnancy weight. However, there is a typically a difference between self-reported weight and actual measured weight [86–88]. Women may be misclassified as gaining inadequate, adequate or excess based on self-reported pre-pregnancy weight [89]. Three studies [52, 54, 59] in this review used the weight of the women at 20 weeks of gestation and one study [56] used the weight of the women at 24 weeks of gestation as a proxy for pre-pregnancy weight. At this stage of pregnancy, there could be significant physiologic changes that may have resulted in weight gain, which may affect the measurement of GWG. In two studies [46, 58], it was unclear when or how the pre-pregnancy weight of the women was measured. The arbitrary classification of the outcome [6, 39, 40, 43, 44, 48, 50] and unclear classification of BMI and GWG were identified as a major quality issue in the review. Thirdly, there was poor control of confounding factors in many studies [6, 9, 39, 42, 43, 46–48]. These studies either did not control for confounding factors at all or did not include all necessary variables into the analysis (partially controlled). The identification of a number of quality issues in most of the included studies suggest the need for methodologically rigorous studies in sub-Saharan Africa to answer GWG related research questions including what factors affect GWG and the association between GWG and birth outcomes.
This review has a number of limitations. Firstly, the studies included in the review were highly heterogeneous and only two studies were eligible for the meta-analyses. Secondly, some of the included studies did not use standard GWG classifications. Thirdly, the pre-pregnancy weight of the women was assessed using different methods and at different stages (for example, pre-pregnancy or at 20 weeks). Fourthly, factors associated with GWG were classified inconsistently across studies. Finally, confounding factors were poorly controlled in most of the included studies.
Conclusion
The percentage of inadequate GWG was as high as 80% in low-income Sub-Saharan countries while it was as low as 15% in upper middle-income Sub-Saharan African countries. In all studies from low-income Sub-Saharan countries, the percentage of inadequate GWG was greater than 58%. The percentage of inadequate GWG ranged from 67% to 98% among underweight women. Studies with a higher percentage of women with excessive GWG had a higher percentage of women who were overweight or obese, and those with a lower percentage of women with a lower percentage of excessive GWG had a lower percentage of women with high BMI (overweight or obese). Future interventions would need to give attention to design effective pre-pregnancy weight management strategies. Sub-Saharan African countries may need to develop regional GWG guidelines.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
(TIF)
Acknowledgments
We acknowledge Beklecho Geleta’s contribution in critically appraising papers.
Abbreviations
- AJOL
African Journal Online
- ANC
Antenatal Care
- BMI
Body Mass Index
- CI
Confidence Interval
- GWG
Gestational Weight Gain
- IOM
Institute of Medicine
- LBW
Low Birth Weight
- PRISM-P
Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols
- RR
Relative Risk
- SSA
sub-Saharan Africa
- WHO
World Health Organization
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Raatikainen K, Heiskanen N, Heinonen S. Transition from Overweight to Obesity Worsens Pregnancy Outcome in a BMI-dependent Manner. Obesity. 2006;24(1):166–71. [DOI] [PubMed] [Google Scholar]
- 2.Asefa F, Nemomsa D. Gestational weight gain and its associated factors in Harari Regional State: Institution based cross-sectional study, Eastern Ethiopia. Reproductive Health. 2016;13(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alavi N, Haley S, Chow K, McDonald SD. Comparison of national gestational weight gain guidelines and energy intake recommendations. Obesity Review. 2013;14:68–85. [DOI] [PubMed] [Google Scholar]
- 4.Scott C, Andersen CT, Valdez N, Mardones F, Nohr EA, Poston L, et al. No global consensus: a cross-sectional survey of maternal weight policies. BMC Pregnancy Childbirth. 2014;14(167):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.IOM (Institute of Medicine), NRC (National Research Council). Weight gain during pregnancy: reexamining the guidelines. Washington D.C:National Academy Press: 2009. Accessed on September 30, 2017, from: https://www.cbsnews.com/htdocs/pdf/052809_pregnancy.pdf [Google Scholar]
- 6.Onwuka C, Ugwu E, Onah H, Obi S, Onwuka C, Menuba I, et al. Patterns of Gestational Weight Gain and Its Association with Birthweight in Nigeria. Nigerian Journal of Clinical Practice. 2017;20:754–60. 10.4103/1119-3077.208958 [DOI] [PubMed] [Google Scholar]
- 7.Esimai OA, Ojofeitimi E. Pattern and Determinants of Gestational Weight Gain an Important Predictor of Infant Birth Weight in a Developing Country. Global Journal of Health Science. 2014;6(4):148–54. 10.5539/gjhs.v6n4p148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill B, McPhie S, Skouteris H. The Role of Parity in Gestational Weight Gain and Postpartum Weight Retention. Womens Health Issues. 2016;26(1):123–9. 10.1016/j.whi.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 9.Wanyama R, Obai G, Odongo P, Kagawa MN, Baingana RK. Are Women In Low Income Setting Gaining Adequate Gestational Weight? A Prospective Cross Sectional Study In Urban Uganda. Research journali’s Journal of Public Health. 2016;2(11):1–14. [Google Scholar]
- 10.McDonalda SM, Liub J, Wilcoxa S, Laua EY, Archerc E. Does dose matter in reducing gestational weight gain in exercise interventions? A systematic review of literature. Journal of Science and Medicene in Sport. 2016;19:323–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bodnar LM, Wisner KL, Moses-Kolko E, Sit DKY, Hanusa BH. Prepregnancy body mass index, gestational weight gain and the likelihood of major depression during pregnancy. Journal Clinical Psychiatry. 2009;70(9):1290–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casanueva E, Labastida J, Sanz C, Morales-Carmona F. Depression and Body Fat Deposition in Mexican Pregnant Adolescents. Arch Med Res. 2000;31:48–52. 10.1016/s0188-4409(00)00041-2 [DOI] [PubMed] [Google Scholar]
- 13.Web GJB, Siega-Riz AM, Dole N4. Psychosocial Determinants of Adequacy of Gestational Weight. Obesity. 2009;17(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Artal R, Lockwood CJ, Brown HL. Weight Gain Recommendations in Pregnancy and the Obesity Epidemic. Obstetrics and Gynecology. 2010;115(1):152–5. 10.1097/AOG.0b013e3181c51908 [DOI] [PubMed] [Google Scholar]
- 15.Hedderson MM, Gunderson EP, Ferrara A. Gestational Weight Gain and Risk of Gestational Diabetes Mellitus. Obstetrics and Gynecology. 2010;115(3):597–604. 10.1097/AOG.0b013e3181cfce4f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nehring I, Schmoll S, Beyerlein A, Hauner H, Kries Rdv. Gestational weight gain and long-term postpartum weight retention: a meta-analysis. American Journal of Clinical Nutrition. 2011;94:1225–31. 10.3945/ajcn.111.015289 [DOI] [PubMed] [Google Scholar]
- 17.Zhao R, Xu L, Wu M.L, Huang S.H, Cao X.J. Maternal pre-pregnancy body mass index, gestational weight gain influence birth weight. Women and Birth. 2018;31:e20–e5. 10.1016/j.wombi.2017.06.003 [DOI] [PubMed] [Google Scholar]
- 18.Guan P, Tang F, Sun G, Ren W. Effect of maternal weight gain according to the Institute of Medicine recommendations on pregnancy outcomes in a Chinese population. Journal of International Medical Research. 2019;47(9):4397–412. 10.1177/0300060519861463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huang A, Ji Z, Zhao W, Hu H, Yang Q, Chen D. Rate of gestational weight gain and preterm birth in relation to prepregnancy body mass indices and trimester: a follow-up study in China. Reproductive Health. 2016;13(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson J, Clifton RG, Roberts JM, Myatt L, Hauth JC, Spong CY, et al. Pregnancy Outcomes With Weight Gain Above or Below the 2009 Institute of Medicine Guidelines. Obstetrics and Gynecology. 2013;121(5):969–75. 10.1097/AOG.0b013e31828aea03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ldl Torre, Flick AA, Istwan N, Rhea D, Cordova Y, Dieguez C, et al. The Effect of New Antepartum Weight Gain Guidelines and Prepregnancy Body Mass Index on the Development of Pregnancy-Related Hypertension. American Journal Perinatology. 2011;28(4):285–91. [DOI] [PubMed] [Google Scholar]
- 22.Mochhoury L, Razine R, Kasouati J, Kabiri M, Barkat A. Body Mass Index, Gestational Weight Gain, and Obstetric Complications in Moroccan Population. Journal of Pregnancy. 2013:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung JGY, Taylor RS, Thompson JMD, Ngaire H. Anderson a, Dekker GA, Kenny LC, et al. Gestational weight gain and adverse pregnancy outcomes in a nulliparous cohort. European Journal of Obstetrics and Gynecology. 2012. [DOI] [PubMed] [Google Scholar]
- 24.Ashley-Martin J, Woolcott C. Gestational Weight Gain and Postpartum Weight Retention in a Cohort of Nova Scotian Women. Maternal Child Health Journal. 2014;18:1927–35. 10.1007/s10995-014-1438-7 [DOI] [PubMed] [Google Scholar]
- 25.Mamun AA, Kinarivala M, O’Callaghan MJ, Williams GM, Najman JM, Callaway LK. Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: evidence from 21 y postpartum follow-up. American Journal of Clinical Nutrition. 2010;91:1336–41. 10.3945/ajcn.2009.28950 [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Low Birth Weight; Country, Regional and Global Estimates Geneva, Switzerland and New York, USA: World Health Organization and United Nations Children’s Fund, 2004. Accessed on November 5, 2018, from:http://www.who.int/iris/handle/10665/43184 [Google Scholar]
- 27.World Health Organization. Guideline on optimal feeding of low birth weight infants in low and middle income countries. Geneva, Switzerland: World Health Organization, 2011. Accessed on November 5, 2018, from: https://www.who.int/maternal_child_adolescent/documents/9789241548366.pdf [PubMed] [Google Scholar]
- 28.Gondwe A, Ashorn P, Ashorn U, Dewey KG, Maleta K, Nkhoma M, et al. Pre-pregnancy body mass index (BMI) and maternal gestational weight gain are positively associated with birth outcomes in rural Malawi. PLoS One. 2018;13(10):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ayensu J, Annan RA, Edusei A, Badu E. Impact of maternal weight on pregnancy outcomes: a systematic review. Nutrition and Food Science. 2016;46(4):542–56. [Google Scholar]
- 30.Mukona D, Munjanja SP, Zvinavashe M, Stray-Pederson B. Physical activity in pregnant women in Africa: A systematic review. International Journal of Nursing and Midwifery. 2016;8(4):28–34. [Google Scholar]
- 31.Onubi OJ, Marais D, Aucott L, Friday Okonofua, Poobalan AS. Maternal obesity in Africa: a systematic review and meta-analysis. Journal of Public Health 2015;38(3):e218–e31. 10.1093/pubmed/fdv138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine. 2009;6(7):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews 2015;4(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asefa F, Foureur M, Hayen A, Cummins A, Dessie Y. Gestational weight gain and its effect on birth outcomes in sub-Saharan Africa: a protocol for systematic review and meta-analysis. PROSPERO 2018. CRD42018085499 Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018085499. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Seifu B. Assesment Of Gestational Weight Gain And Associated Factors Among HIV Negative And HIV Positive Women In Addis Ababa, Ethiopia. Addis Ababa, Ethiopia: Addis Ababa Univesity; 2017. Accessed on December 12, 2017, from: http://etd.aau.edu.et/handle/123456789/6784 [Google Scholar]
- 36.Institute of Medicine. Nutrition During Pregnancy: Part I: Weight Gain, Part II: Nutrient Supplements. Washington, DC: The National Academies Press; 1990. Accessed on December 12, 2017, from: https://www.ncbi.nlm.nih.gov/pubmed/25144018 [PubMed] [Google Scholar]
- 37.Covidence systematic review software. Melbourne, Australia, Veritas Health Innovation. Available from: www.covidence.org
- 38.Evans N, Lasen M, Tsey K. A Systematic Review of Rural Development Research Characteristics, Design Quality and Engagement with Sustainability Springer Briefs in Public Health. Accessed on June 25, 2018, from: https://www.springer.com/gp/book/9783319172835. [Google Scholar]
- 39.Addo VN. Body Mass Index, Weight Gain During Pregnancy And Obstetric Outcomes. Ghana Medical Journal. 2010;44(2):64–9. 10.4314/gmj.v44i2.68886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agbota G, Fievet N, Heude B, Accrombessi M, Ahouayito U, Yovo E, et al. Poor maternal anthropometric status before conception is associated with a deleterious infant growth during the first year of life: a longitudinal preconceptional cohort. Pediatric Obesity. 2019;15(1):1–11. [DOI] [PubMed] [Google Scholar]
- 41.Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- 42.Iyoke CA, Ugwu GO, Ezugwu FO, Lawani OL, Onyebuchi AK. Retrospective cohort study of the effects of obesity in early pregnancy on maternal weight gain and obstetric outcomes in an obstetric population in Africa. International Journal of Women's Health. 2013;5(1):501–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Onyiriuka AN. High birth weight babies: incidence and foetal outcome in a mission hospital in Benin City, Nigeria. Nigerian journal of clinical practice. 2006;9(2):114–9. [PubMed] [Google Scholar]
- 44.Akindele R, Audu L, O M. Macrosomic Births in Abuja: A Case–Control Study of Predisposing Factors and Early Neonatal Outcome. Nigerian journal of clinical practice. 2017;20(3):320–7. 10.4103/1119-3077.196060 [DOI] [PubMed] [Google Scholar]
- 45.Fouelifack FY, Fouedjio JH, Fouogue JT, Sando Z, Fouelifa LD, Mbu RE. Associations of body mass index and gestational weight gain with term pregnancy outcomes in urban Cameroon: a retrospective cohort study in a tertiary hospital. BMC research notes. 2015;8(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mbu RE, Fouedjio HJ, Tabot M, Fouelifack FY, Tumasang FN, Tonye RN, et al. Effects of gestational weight gain on the outcome of labor at the Yaounde central hospital maternity, Cameroon. Open Journal of Obstetrics and Gynecology. 2013;(3):648–52. [Google Scholar]
- 47.Halle-Ekane GE, Nsom JB, Atashili J, Palle JN, Nsagha DS, Nguefack CT, et al. Outcome of Pregnancy in Patients with Excessive Gestational Weight Gain in Two District Hospitals in Douala, Cameroon. SM Journal of Gynecology Obstetrics. 2015;1(1):1–6. [Google Scholar]
- 48.Elie N, Tangho N, Roge G. Risk Factors for Macrosomia. The Journal of Obstetrics and Gynecology of India. 2015;65(4):226–9. 10.1007/s13224-014-0586-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nemomsa D, Mesfin F, Damena M, Asefa F. Early-pregnancy Body Mass Index and GestationalWeightGain are important Maternal Markers of LowBirth Weight in Harar town,Eastern Ethiopia East African Journal of Health and Biomedical Sciences. 2018;2(1):1–9. [Google Scholar]
- 50.Tela FG, Bezabih AM, Adhanu AK, Tekola KB. Fetal macrosomia and its associated factors among singleton live-births in private clinics in Mekelle city, Tigray, Ethiopia. BMC Pregnancy Childbirth. 2019;19(1):1–6. 10.1186/s12884-018-2145-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abubakari A, Kynast-Wolf G, Jah A. Maternal Determinants of Birth Weight in Northern Ghana. PLoS One. 2015;10(8):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adu-Afarwuah S, Lartey A, Okronipa H, Ashorn P, Ashorn U, Zeilani M, et al. Maternal supplementation with small-quantity lipid-based nutrient supplements compared with multiple micronutrients, but not with iron and folic acid, reduces the prevalence of low gestational weight gain in semi-urban Ghana: A randomized controlled trial. Journal of Nutrition and Dietetics. 2017;147(4):697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Agbayizah ED. Gestational Weight Gain and it’s Contributing Factors Among Post-Natal Women At Tema General Hospital, Greater Accra. Accra, Ghana: University of Ghana; 2017. Accessed on December 10, 2019, from:http://ugspace.ug.edu.gh/handle/123456789/23355?show=full [Google Scholar]
- 54.Wrottesley SV, Pisa PT, Norris SA. The Influence of Maternal Dietary Patterns on Body Mass Index and Gestational Weight Gain in Urban Black South African Women. Nutrients. 2017;9(732):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ward E, Kruger HS, Graan AV. The influence of pre-pregnancy BMI and weight gain during pregnancy on pregnancy outcome South African Journal of Clinical Nutrition. 2007;20(3):112–7. [Google Scholar]
- 56.Chithambo SET. Factors associated with the rate of gestational weight gain in the rural Mangochi district of Malawi. Oslo, Norway: University Of Oslo; 2017. Accessed on December 12, 2017, from: https://www.duo.uio.no/handle/10852/58269 [Google Scholar]
- 57.Ismail LC, Bishop DC, Pang R, Ohuma EO, Kac G, Abrams B, et al. Gestational weight gain standards based on women enrolled in the Fetal Growth Longitudinal Study of the INTERGROWTH-21st project: A Prospective longitudinal cohort study. BMJ. 2016;352(i555):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ouédraogo CT, Wessells KR, Young RR, Faye MT, Hess SY. Prevalence and determinants of gestational weight gain among pregnant women in Niger. Maternal and Child Nutrition 2019:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Muyayalo KP, Olivia NA, Mbungu MR. Postpartum Weight Retention in Congolese Pregnant in Kinshasa. International Journal of Current Research Review 2017;9(18):29–35. [Google Scholar]
- 60.World Bank Country and Lending Groups. World Bank Country and Lending Groups, Country Classification. Accessed on February 20, 2019, from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- 61.Tela FG, Bezabih AM, Adhanu AK. Effect of pregnancy weight gain on infant birth weight among mothers attending antenatal care from private clinics in Mekelle City, Northern Ethiopia: A facility based follow-up study. PLoS One. 2019;14(3):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Begum F, Colman I, McCargar LJ, Bell RC. Gestational Weight Gain and Early Postpartum Weight Retention in a Prospective Cohort of Alberta Women. Journal of Obstetrics and Gynaecology Canada. 2012;34(7):637–47. 10.1016/s1701-2163(16)35316-6 [DOI] [PubMed] [Google Scholar]
- 63.Restall A, Taylor RS, Thompson JD, Flower D, Dekker GA, Kenny LC, et al. Risk Factors for Excessive Gestational Weight Gain in a Healthy, Nulliparous Cohort. Journal of Obesity. 2014;2014(ID 148391):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fraga ACSA Filha MMT. Factors associated with gestational weight gain in pregnant women in Rio de Janeiro, Brazil, 2008. Cad Saúde Pública, Rio de Janeiro. 2014;30(3):633–44. [DOI] [PubMed] [Google Scholar]
- 65.Food And Agriculture Organization. Regional Overview of Food Insecurity Africa; African Food Security Prospects Brighter Than Ever 2015. Accessed on November 5, 2018, from: http://www.fao.org/3/a-i4635e.pdf.
- 66.Lindsay KL, Gibney ER, McAuliffe FM. Maternal nutrition among women from Sub-Saharan Africa, with a focus on Nigeria, and potential implications for pregnancy outcomes among immigrant populations in developed countries. Journal of Human Nutrition and Dietetics. 2012;25:534–46. 10.1111/j.1365-277X.2012.01253.x [DOI] [PubMed] [Google Scholar]
- 67.Jarman M, Yuan Y, Pakseresht M, Shi Q, Robson PJ, Bell RC, et al. Patterns and trajectories of gestational weight gain: a prospective cohort study. Canadian Medical Association Journal. 2016;4(2):338–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hill B, Skouteris H, McCabe M, Fuller-Tyszkiewicz M. Body Image and Gestational Weight Gain: A Prospective Study. Journal of Midwifery and Womens Health. 2013;58(2):189–94. [DOI] [PubMed] [Google Scholar]
- 69.Godoy AC, Nascimento SLd, SuritaI FG. A systematic review and meta-analysis of gestational weight gain recommendations and related outcomes in Brazil. Clinics (Sao Paulo). 2015;70(11):758–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Beyerlein A, Nehring I, Rzehak P, Heinrich J, ller MJM, Plachta-Danielzik S, et al. Gestational Weight Gain and Body Mass Index in Children: Results from Three German Cohort Studies. PLoS One. 2012;7(3):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schlaff RA, Holzman C, Mudd LM, Pfeiffer K, Pivarnik J. Body Mass Index is Associated With Appropriateness of Weight Gain But Not Leisure-Time Physical Activity During Pregnancy. Journal of Physical Activity and Health. 2014;11(8):1593–9. 10.1123/jpah.2013-0090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Mohannad A, Rizvi F, Irfan G. Impact of Maternal Education, and Socioeconomic Status on Maternal Nutritional Knowledge and Practices Regarding Iron Rich Foods and Iron Supplements. Annals of Pakistan Institute of Medical Sciences. 2012;8(2):101–5. [Google Scholar]
- 73.Streuling I, Beyerlein A, Kries Rdv. Can gestational weight gain be modified by increasing physical activity and diet counseling? A meta-analysis of interventional trials. American Journal of Clinical Nutrion 2010;92(4):678–87. [DOI] [PubMed] [Google Scholar]
- 74.Gardner B, Wardle J, Poston L, Croker H. Changing diet and physical activity to reducegestational weight gain: a meta-analysis. Obesity Reveiw 2011;12(7):e602–20. [DOI] [PubMed] [Google Scholar]
- 75.Agha M, Agha RA, Sandell J. Interventions to Reduce and Prevent Obesity in Pre-Conceptual and Pregnant Women: A Systematic Review and Meta-Analysis. PLoS One. 2014;9(5):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rogozińska E, Marlin N, Betrán AP, Astrup A, Barakat R, Bogaerts A, et al. Effect of diet and physical activity based interventions in pregnancy on gestational weight gain and pregnancy outcomes: meta-analysis of individual participant data from randomised trials. BMJ. 2017;358 (8119):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.LimaI RJCP, Batista RFL, Ribeiro MRC, Ribeiro CCC, Simões VMF, Neto PML, et al. Prepregnancy body mass index, gestational weight gain, and birth weight in the BRISA cohort. Rev Saude Publica. 2018;52(48):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hunt KJ, Alanis MC, Johnson ER, Mayorga ME, Korte JE. Maternal pre-pregnancy weight and gestational weight gain and their association with birthweight with a focus on racial differences. Maternal and Child Health Journal. 2013;17(1):85–94. 10.1007/s10995-012-0950-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.McDonald SD, Han Z, Mulla S, Lutsiv O, Lee T, Beyene J. High Gestational Weight Gain and the Risk of Preterm Birth and Low Birth Weight: A Systematic Review and Meta-Analysis. Journal of Obstetrics and Gynaecology Canada. 2011;33(12):1223–33. 10.1016/S1701-2163(16)35107-6 [DOI] [PubMed] [Google Scholar]
- 80.Ehrenberg HM, Dierker L, Milluzzi C, Mercer BM. Low maternal weight, failure to thrive in pregnancy, and adverse pregnancy outcomes. American Journal of Obstetrics and Gynecology. 2003;189(6):1726–30. 10.1016/s0002-9378(03)00860-3 [DOI] [PubMed] [Google Scholar]
- 81.Haugen M, Brantsæter AL, Winkvist A, Lissner L, Alexander J, Bente Oftedal1, et al. Associations of pre-pregnancy body mass index and gestational weight gain with pregnancy outcome and postpartum weight retention: a prospective observational cohort study. BMC Pregnancy Childbirth. 2015;14(201):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hickey CA. Sociocultural and behavioral influences on weight gain during pregnancy. American Journal of Clinical Nutrition. 2000;71(suppl):1364S–70S. [DOI] [PubMed] [Google Scholar]
- 83.Gante I, Amaral N, Dores J, Almeida MC. Impact of gestational weight gain on obstetric and neonatal outcomes in obese diabetic women. BMC Pregnancy Childbirth. 2015;15(249):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhu T, Jun Tang, Zhao F, Qu Y, Mu D. Association between maternal obesity and offspring Apgar score or cord pH: a systematic review and meta-analysis. Scientific Report 2015;5(1–6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Çalik KY, Yildiz NK, Erkaya R. Effects of gestational weight gain and body mass index on obstetric outcome. Saudi Journal of Biological Science. 2018:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shin D, Chung H, Weatherspoon L, O. Song W. Validity of Prepregnancy Weight Status Estimated from Self-reported Height and Weight. Maternal and Child Health Journal. 2014;18(7):1667–74. 10.1007/s10995-013-1407-6 [DOI] [PubMed] [Google Scholar]
- 87.Natamba BK, Sanchez SE, Gelaye B, Williams MA. Concordance between self-reported pre-pregnancy body mass index (BMI) and BMI measured at the first prenatal study contact BMC Pregnancy Childbirth. 2016;16(187):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Han E, Abrams B, Sridhar S, Xu F, Heddersona M. Validity of Self-Reported Pre-Pregnancy Weight and Body Mass Index Classification in an Integrated Health Care Delivery System. Paediatrics and Perinatal Epidemiology. 2016;30:314–9. [DOI] [PubMed] [Google Scholar]
- 89.Mandujano A, Huston-Presley L, Waters TP, Catalano PM. Women’s reported weight: is there a discrepancy? The Journal of Maternal-Fetal and Neonatal Medicine. 2012;25(8):1395–8. 10.3109/14767058.2011.636099 [DOI] [PubMed] [Google Scholar]