To rapidly communicate short reports of innovative responses to Covid-19 around the world, along with a range of current thinking on policy and strategy relevant to the pandemic, the Journal has initiated the Covid-19 Notes series.
A text message from a colleague in mainland China flashed across the screen of one of our cell phones on New Year’s Eve, 2019, notifying us of an emerging cluster of cases of atypical pneumonia in Wuhan. Amid flashbacks to the fearsome severe acute respiratory syndrome (SARS) epidemic in 2002–2003, we immediately reached out to our network of collaborators for further leads. An uncomfortable silence followed over the next few weeks.
By mid-January, we noticed the first reports of exported cases in Bangkok and then Tokyo. These reports were surprising, given the low number of reported cases in Wuhan at that point. They motivated us to “nowcast” the true size of the Wuhan outbreak and then forecast the potential for nationwide spread in China during chunyun, the largest annual human migration in the world, which is associated with the Spring Festival.
Finally, a flurry of WeChat exchanges on January 22, 2020, resulted in our team flying to Beijing the next morning. We spent the next 24 hours working nonstop alongside colleagues from the Chinese Center for Disease Control and Prevention who had already spent 3 weeks frantically collecting and collating data. Our job was to make sense of disparate data sets to tease out the early transmission dynamics of what would subsequently be named Covid-19. Our findings were disseminated in the Journal 6 days later (www.nejm.org/doi/10.1056/NEJMoa2001316).
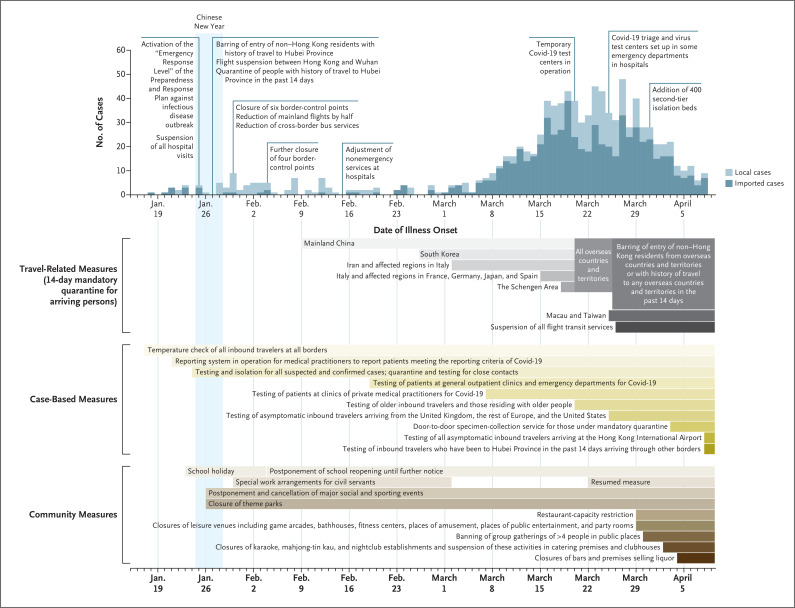
Then, on January 25, the first day of the lunar new year — the most important holiday in the Chinese calendar — one of us spent the day huddled with Hong Kong’s entire cabinet. By evening, Chief Executive Carrie Lam declared that Hong Kong’s Covid-19 response had been raised to the highest “emergency” level. Figure 1 summarizes Hong Kong’s experience so far (www.coronavirus.gov.hk/eng/index.html).
Figure 1. Actions Taken to Suppress Covid-19 Transmission in Hong Kong and Occurrence of Laboratory-Confirmed Cases.
Information is through April 9, 2020. Cases are shown on their date of laboratory confirmation; in 141 cases, patients were asymptomatic at the time of confirmation. Darker shading represents more severe disease-control measures.
In Geneva, the World Health Organization (WHO) had shifted into high gear and gathered leading researchers and public health experts to take stock of the rapidly developing knowledge base for Covid-19 and, more important, to establish a research roadmap for working out what we had yet to learn about the disease. We led the development of the epidemiology track. Midday on February 11, the first day of the 2-day summit, one of us received a message telling us to immediately return to Hong Kong, then travel on to Beijing for the WHO–China Joint Mission on Covid-19. We spent the next 10 days traversing the country and writing a report that summarized the Chinese experience with Covid-19, with the goal of informing and helping to prepare people throughout the rest of the world.
All the while, we were working with colleagues in Boston, in College Park, Maryland, and in Guangzhou to produce evidence to help answer some of the key questions identified in the WHO’s Covid-19 research roadmap, including questions on the disease’s severity and case fatality ratio, the effectiveness of face masks for preventing transmission, and the role of presymptomatic transmission by people incubating the disease, respectively.
As scientists conducting research during a pandemic, we are very much public health practitioners at the same time; we therefore never forget our primary responsibility to the local control effort. We produce daily updates on epidemic progress for the public and weekly reports for authorities, aiming to disseminate the most robust and reliable science to inform decision making. The more successful Hong Kong is at keeping a local epidemic at bay, the harder it will be to maintain effective disease-control measures until the first vaccines against Covid-19 arrive. The three-way tug-of-war between health protection, economic preservation, and social acceptance and well-being will remain unresolved until sufficient population immunity is acquired as a result of infection or vaccination.
SARS brought the three of us together. We matured during the influenza A (H1N1) pandemic in 2009, were further tested by the influenza A (H7N9) avian-to-human outbreak in 2013, and now face Covid-19. Working at frontiers in science to control emerging infections is difficult, but the art of equanimity and resilience is harder still to master. We remain in solidarity with our fellow long-distance runners in this marathon and to face whatever comes next.
Acknowledgments
We thank Tiffany Ng for technical assistance.
Disclosure Forms
This note was published on April 15, 2020, at NEJM.org.
Footnotes
Supported by a commissioned grant from the Health and Medical Research Fund of the Food and Health Bureau, Government of the Hong Kong Special Administrative Region.
Disclosure forms provided by the authors are available with the full text of this note at NEJM.org.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.