To rapidly communicate information on the global clinical effort against Covid-19, the Journal has initiated a series of case reports that offer important teaching points or novel findings. The case reports should be viewed as observations rather than as recommendations for evaluation or treatment. In the interest of timeliness, these reports are evaluated by in-house editors, with peer review reserved for key points as needed.
A 65-year-old woman with hypertension, autoimmune hypothyroidism, and known Covid-19 exposure presented to the emergency department with a 4-day history of fatigue, fever, dry cough, and abdominal discomfort. She was afebrile and had a respiratory rate of 28 breaths per minute and an oxygen saturation of 89% while she was breathing ambient air; breath sounds were diminished bilaterally with bibasilar rales. The abdominal examination was normal.
Laboratory tests showed a normal white-cell count, hemoglobin level (14.2 g per deciliter), and platelet count (183,000 per cubic millimeter). The C-reactive protein level was elevated at 55 mg per liter, and liver-function tests showed cholestasis. An oropharyngeal swab for Covid-19 testing was positive. Chest computed tomography (CT) showed ground-glass opacities in the lower zones.
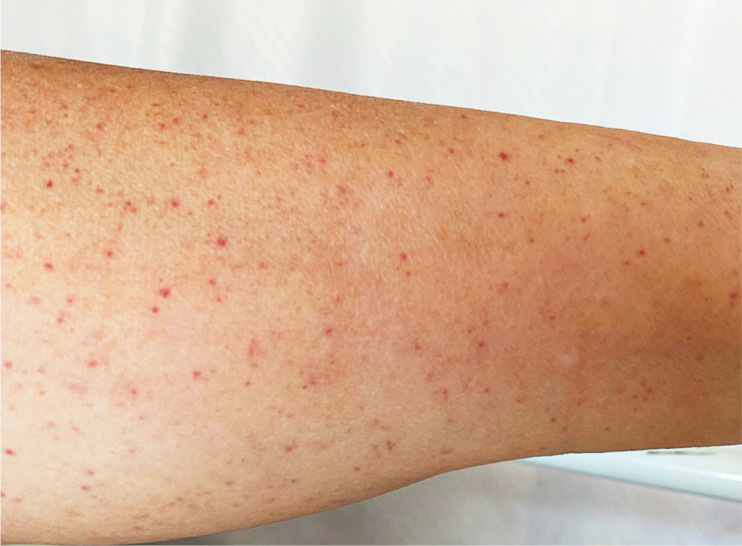
The patient was admitted and began to receive treatment with intravenous amoxicillin–clavulanic acid, low-molecular-weight heparin, and oxygen. On day 4, lower-extremity purpura (Figure 1) appeared and epistaxis occurred. Isolated thrombocytopenia (platelet count, 66,000 per cubic millimeter) was noted; these findings prompted discontinuation of heparin and antibiotics. On day 5, the platelet count was 16,000 per cubic millimeter, and on day 7, it was 8000 per cubic millimeter.
Figure 1. Purpuric Lesions on the Patient’s Lower Extremity.
The prothrombin and activated partial thromboplastin times were normal; the fibrinogen level was 5 g per liter (normal range, 2 to 4). A peripheral-blood smear showed less than 1% schistocytes. The level of thyroid peroxidase antibodies was 245 U per milliliter (normal value, <35); antiplatelet factor 4, antiplatelet antibodies, and antinuclear antibodies were not detected.
Intravenous immune globulin was administered at a rate of 1 g per kilogram of body weight. After 48 hours, the platelet count decreased to 1000 per cubic millimeter and the purpuric lesions progressed; this prompted a second infusion of immune globulin at a dose of 1 g per kilogram.1,2
Bone marrow aspiration showed normal cellularity with an increase in pleomorphic megakaryocytes. Erythroblast and granulocyte cell lines were normal, without evidence of hemophagocytosis.
On day 9, a right frontal headache developed in the patient, without fever, vomiting, or focal neurologic deficit. CT of the head showed a subarachnoid microhemorrhage in the right frontal lobe. The platelet count was 2000 per cubic millimeter, and a platelet transfusion was administered with 100 mg of prednisolone; eltrombopag (75 mg per day) was initiated.1,2
On day 10, the headache had resolved, there were no new neurologic findings, and the platelet count had increased to 10,000 per cubic millimeter. All the other laboratory tests had normalized except for the fibrinogen level, which remained elevated (3.5 g per liter). On day 13, the platelet count was 139,000 per cubic millimeter, and the purpura had disappeared.
The temporal sequence in this case suggests,3 but does not prove, that Covid-19 was a causal factor in immune thrombocytopenia in this patient. Fortunately, she had a response to treatment, albeit in a delayed fashion. Although the cerebral bleeding did not have major sequelae, this case illustrates the need to be vigilant for complications associated with Covid-19.
Disclosure Forms
This case was published on April 15, 2020, at NEJM.org.
Footnotes
Disclosure forms provided by the authors are available with the full text of this case at NEJM.org.
References
- 1.Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv 2019;3:3829-3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Provan D, Arnold DM, Bussel JB, et al. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv 2019;3:3780-3817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lippi G, Plebani M, Henry BM. Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: a meta-analysis. Clin Chim Acta 2020;506:145-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.