Background: The coronavirus disease 2019 (COVID-19) pandemic originated in China in late 2019 and continues to spread globally (1). At the time of writing, there were nearly 2 million COVID-19 cases causing approximately 110 000 deaths across more than 200 affected countries and territories (2). As some health care systems approach collapse, a pressing need exists for tools modeling the capacity of acute and critical care systems during the COVID-19 pandemic.
Objective: To develop an online tool to estimate the maximum number of COVID-19 cases that could be managed per day within the catchment area served by a health care system, given acute and critical care resource availability.
Methods: We modeled steady-state patient-flow dynamics constrained by the number of acute care beds, critical care beds, and mechanical ventilators available for COVID-19–infected patients seeking health care during the pandemic. Parameters for patient-flow dynamics were extracted from evolving data on COVID-19 and assumptions based on expert guidance. We used the package shiny within R, version 3.5.3 (R Foundation for Statistical Computing), to create the interactive tool.
The tool determines the maximum number of COVID-19 cases that could be managed per day within the catchment area served by a health care system, where the rate of patients with COVID-19 who are being admitted or transferred to acute care or critical care or requiring mechanical ventilation (“patients in”) equals the maximum daily turnover of each of those resources available for patients with COVID-19 (“patients out”). These estimates represent the maximum steady-state constraints imposed by these limited resources being managed by a health care system or hospital. Resources available for patients with COVID-19 should account for the proportion of existing staffed resources that could be made maximally available to support patients with COVID-19 plus any additional staffed surge capacity.
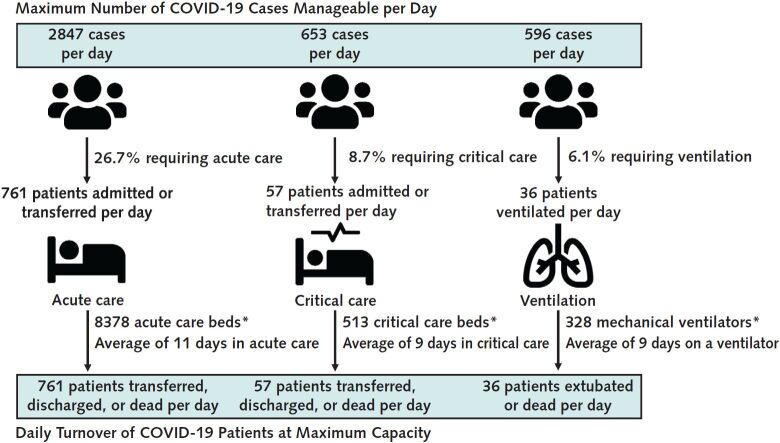
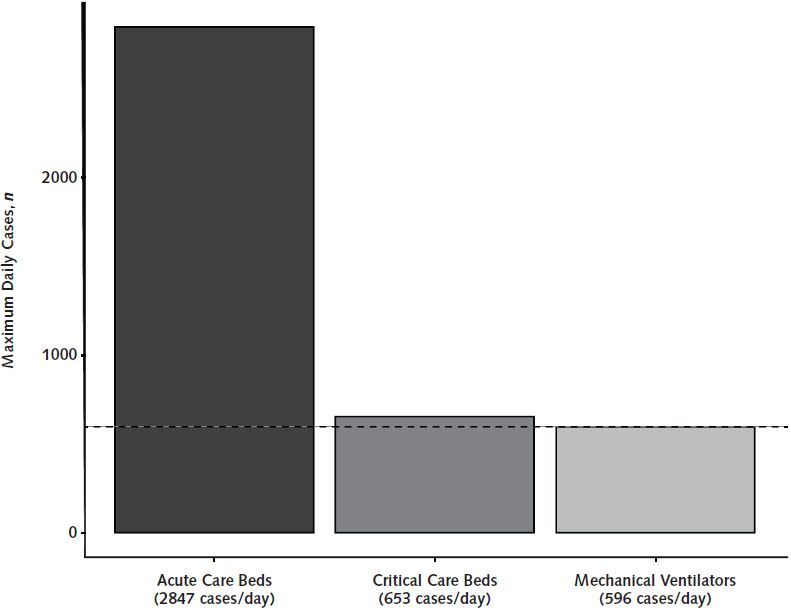
The tool first calculates the maximum daily turnover of acute care beds, critical care beds, and mechanical ventilators available for patients with COVID-19 by taking the maximally available number of each of those resources for these patients and dividing it by the expected duration of their use for patients with COVID-19. On the basis of published data, the average length of stay in acute care and critical care was set at 11 and 9 days, respectively, whereas the average length of time for mechanical ventilation was set at 9 days (1, 3, 4). The tool then calculates the population-weighted age-stratified probabilities of COVID-19 cases requiring acute care hospitalization and critical care, and in the base case assumes that 70% of critical care patients will be mechanically ventilated (3–5). Finally, the maximum number of new COVID-19 cases per day that a health care system could manage is calculated by dividing the daily turnover of maximally available acute care beds, critical care beds, or mechanical ventilators by the probability of each resource being used among COVID-19 cases. The tool outputs maximum numbers of manageable cases per day separately for acute care beds, critical care beds, and mechanical ventilators (Figure 1), so that health systems can determine the limiting resource at steady state (Figure 2) and consider system adjustments, such as allocating more acute and critical care resources to COVID-19.
Figure 1.
The CAIC-RT default output.
The default output of CAIC-RT is the maximum number of COVID-19 cases per day manageable by the health care system in Ontario, Canada, on the basis of resource constraints. The tool outputs steady-state estimates of the maximum number of cases based on existing acute care bed, critical care bed, and mechanical ventilator capacities so that health care systems can determine the limiting resource. In Ontario, the current limiting health care resource for the pandemic is mechanical ventilators (dashed line). CAIC-RT = COVID-19 Acute and Intensive Care Resource Tool.
Figure 2.
Maximum number of manageable COVID-19 cases per day on the basis of resource constraints in the Ontario health care system.
* Number of existing acute or critical care resources for patients with COVID-19.
All inputs and parameters of the tool (namely total resource capacity, percentage of resources available for COVID-19 and potential additional surge capacity, age distribution, age-stratified probability of resource use, and proportion of critical care patients requiring ventilation) can be tailored for use in any region of the world and applied to either a large health care system (such as a national or state-level system) or to an individual hospital. Although the default parameters for age-based case distribution and severity reflect data from the United States and acute and critical care resource availability inputs reflect provincial data from Canada's most populous province of Ontario (5), users can modify these parameters to match their local data.
Findings: The COVID-19 Acute and Intensive Care Resource Tool (CAIC-RT) is open access and available at https://caic-rt.shinyapps.io/CAIC-RT. As a demonstration, the maximum number of new COVID-19 cases per day that could be managed by the Ontario health care system (default output of the tool) is detailed in Figures 1 and 2.
Discussion: By using an online tool, health care systems can estimate the maximum number of COVID-19 cases per day that could be managed on the basis of age-based case distribution and severity and the number of maximally available acute and critical care resources. Unlike forecasting instruments, our tool determines a sustainable threshold for resource use during the pandemic rather than forecasting when resources might become depleted on the basis of assumptions about reporting, epidemic growth, and reproduction numbers.
Outputs from the tool allow planners to examine how increases in acute and critical resources available for patients with COVID-19 can affect health care system sustainability. Finally, the tool allows customization of age-based case distribution and severity, which is essential for countries with differing population demographics and health care systems.
Limitations of this tool include the steady-state assumption; assumptions that patients with COVID-19 are hospitalized instantaneously and that all beds and ventilators can be adequately staffed; and the application of Canadian, Chinese, Italian, and U.S. data for default parameters, which may not be generalizable to all health care systems. Further, if the tool is applied to a single hospital in a region with several hospitals receiving patients with COVID-19, the proportion of cases directed to that hospital must be considered.
Although we intentionally left the tool modifiable, we will update the default values as new data emerge to account for the ramp-up of diagnostic testing in such countries as the United States, with the understanding that most persons tested will not be hospitalized.
Biography
Disclaimer: The tool, available at https://caic-rt.shinyapps.io/CAIC-RT, was developed by the authors for this article by using a third-party application, which may have limited access and functionality. Neither Annals of Internal Medicine nor the American College of Physicians is responsible for the content and functionality of this online application. Questions regarding the use of the application should be addressed to Dr. Stall (e-mail, nathan.stall@sinaihealth.ca).
Disclosures: Disclosures can be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M20-1169.
Reproducible Research Statement: Study protocol and statistical code: Described in Methods and in the figure legends. Data set: Not applicable.
Corresponding Author: Nathan M. Stall, MD, Division of General Internal Medicine and Geriatrics, Mount Sinai Hospital, Suite 475, 600 University Avenue, Toronto, Ontario M5G 1X5, Canada; e-mail, nathan.stall@sinaihealth.ca.
Previous Posting: This manuscript was posted as a preprint on medRxiv on 25 March 2020. doi:10.1101/2020.03.25.20043711
Footnotes
This article was published at Annals.org on 16 April 2020.
References
- 1. doi: 10.1016/S0140-6736(20)30566-3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [PMID: 32171076] doi:10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed]
- 2. World Health Organization. Coronavirus disease 2019 (COVID-19). Situation Report – 84. Accessed at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200413-sitrep-84-covid-19.pdf?sfvrsn=44f511ab_2. on 13 April 2020.
- 3. doi: 10.1001/jama.2020.1585. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. [PMID: 32031570] doi:10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed]
- 4. doi: 10.1001/jama.2020.5394. Grasselli G, Zangrillo A, Zanella A, et al; COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020. [PMID: 32250385] doi:10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed]
- 5. doi: 10.15585/mmwr.mm6912e2. CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343-346. [PMID: 32214079] doi:10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed]