Difficulties making a fist in patients presenting with recent-onset arthralgia of small joints without clinically detectable arthritis, is considered a risk factor for progression to inflammatory arthritis (IA) and Rheumatoid Arthritis (RA). This is also reflected by this sign being incorporated in the EULAR-definition of arthralgia suspicious for progression to RA.[1] However, to date there is barely scientific evidence for its predictive value and little comprehension on the underlying mechanism in recent-onset arthralgia. We studied if difficulties making a fist is indeed predictive for the development of IA and RA, and whether this sign is associated with subclinical inflammation.
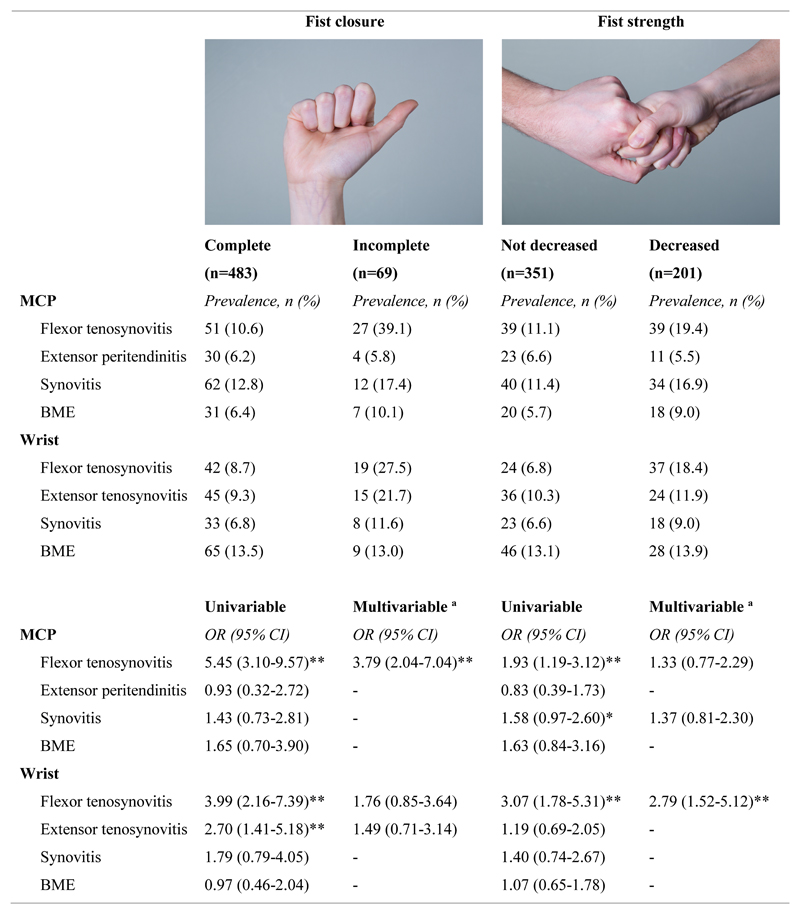
Patients presenting with recent-onset (<1 year) arthralgia of the small joints were consecutively included in the Leiden Clinically Suspect Arthralgia (CSA)-cohort.[2] At baseline the ability to completely close the fist (actively close the fist with all fingertips touching the palm) and fist strength (measured by a patient squeezing the assessor’s fingers) were determined (Figure 1). It was determined by trained research nurses in all patients, and for reliability purposes also by rheumatologists in a subset of patients. Contrast-enhanced 1.5T MRI of wrist and 2nd-5th metacarpophalangeal (MCP)-joints was performed and scored for synovitis, bone marrow edema (BME), tenosynovitis and MCP extensor peritendinitis. Patients were followed on development of clinically apparent IA, determined by rheumatologists (median follow-up 16 months (IQR 4-25)). Detailed description of the cohort, MRI-protocol and statistics are presented supplementary. Cox regression was performed with IA and RA (1987- or 2010-criteria-positivity) as primary and secondary outcome respectively; time-to-event was time from first presentation until IA-development. Associations between difficulties making a fist and subclinical inflammation in the same hand at baseline were assessed with logistic regression.
Figure 1. MRI-detected subclinical inflammation and associations with two components of diffulties making a fist, fist closure and fist strength, in patients with CSA.
At baseline data of diffulties making a fist and MRI-detected subclinical inflammation were available in 552 patients (see flowchart in the supplement).
a Multivariable logistic regression analyses were adjusted for age, gender and MRI inflammatory features from both wrist- and MCP joints with associations of p<0.1 in univariable logistic regression.
* p-value<0.1, ** p-value<0.01.
CSA: clinically suspect arthralgia, MCP: metacarpophalangeal joint, BME: bone marrow edema, OR: odds ratio, CI: confidence interval
Flowchart and baseline characteristics are presented supplementary. From 606 CSA-patients, 86 (14%) had incomplete fist closure, 233 (38%) had decreased fist strength. In univariable Cox regression, the hazard ratio (HR) of incomplete fist closure was 2.22 (95% CI 1.36-3.64) and of decreased fist strength 1.33 (0.87-2.05). In multivariable analyses, corrected for age, gender, CRP- and ACPA-status, both signs were independently associated with IA-development; incomplete fist closure HR 2.33 (1.38-3.93) and decreased strength HR 1.62 (1.04-2.54). Similar findings were obtained with RA-development as outcome (supplement).
To better understand the underlying pathology, as clinical arthritis was absent and therefore not the explanation, we evaluated whether fist problems were related to subclinical inflammation. Incomplete fist closure was associated with MCP flexor tenosynovitis and wrist flexor and extensor tenosynovitis in univariable analysis, and MCP flexor tenosynovitis in multivariable analysis (OR 3.79 (2.04-7.04), Figure 1). Decreased fist strength was associated with MCP and wrist flexor tenosynovitis in univariable analysis, and wrist flexor tenosynovitis in multivariable analysis (OR 2.79 (1.52-5.12), Figure 1).
Finally the two tests were assessed by different observers in a subset of patients. Agreement was substantial for fist closure (n=324, Cohen’s Kappa 0.61), but only fair for fist strength (n=318, Kappa 0.28; supplement).
Difficulties making a fist in recent-onset arthralgia in the absence of clinically apparent arthritis is considered a sign of imminent RA. This is the first study providing scientific support for the predictive value of this sign; incomplete fist closure in particular had better reliability and higher predictive value.
Intuitively, assessment of fist strength (normal/decreased) by physicians who get pinched may be more subject to interobserver variation than visual evaluation if the fist is completely closed, this was illustrated by lower values of agreement. The lower reliability may also have contributed to lower HRs for fist strength.
The association between fist problems and tenosynovitis is plausible as tenosynovitis can hamper tendon gliding within its sheath, limiting tendon excursion and the ability to distribute muscle strength to the fingers. It is reasonable that fist closure was especially associated with MCP flexor tenosynovitis and fist strength with wrist flexor tenosynovitis as these respective tendons are important for these movements.
Thus, difficulties making a fist in CSA is a sign of underlying flexor tenosynovitis. Incomplete fist closure in particular is predictive for RA-development. In contrast to MRI, fist closure is simple to assess, also by physicians with little experience in joint examination. Therefore fist closure, a component of the EULAR definition of arthralgia suspicious for progression to RA,[1] is a feasible and valuable sign for use in daily clinical practice. However, as predictive values are dependent on prevalence, the value of this test in different patient populations (e.g. primary care) needs further investigation.
Supplementary Material
Acknowledgements
The authors thank G. Kracht, photographer at the Department of Radiology of the Leiden University Medical Center, for making and processing the pictures.
Funding This work was supported by the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (Starting grant, agreement No 714312), and the Dutch Arthritis Society.
Footnotes
Contributors FW, FJvdG, EN and AHMvdHvM developed the study concept and design. FW and XMEM contributed to the data acquisition. FW performed the data analyses. FW, EN and AHMvdHvM wrote the first version of the manuscript. All authors critically reviewed the paper and approved the final manuscript.
Competing interests None declared.
Patient consent Obtained.
Ethics approval Local Medical Ethics Committee, named ‘Commissie Medische Ethiek’.
Data sharing statement Data can be requested from the corresponding author.
References
- [1].van Steenbergen HW, Aletaha D, Beaart-van de Voorde LJ, et al. EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis. Ann Rheum Dis. 2017;76:491–6. doi: 10.1136/annrheumdis-2016-209846. [DOI] [PubMed] [Google Scholar]
- [2].van Steenbergen HW, van Nies JA, Huizinga TW, et al. Characterising arthralgia in the preclinical phase of rheumatoid arthritis using MRI. Ann Rheum Dis. 2015;74:1225–32. doi: 10.1136/annrheumdis-2014-205522. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.