Microscopy and rapid diagnostic tests (RDTs) are the main diagnostic tools for malaria but fail to detect low-density parasitemias that are important for maintaining malaria transmission. To complement existing diagnostic methods, an isothermal reverse transcription-recombinase polymerase amplification and lateral flow assay (RT-RPA) was developed. We compared the performance with that of ultrasensitive reverse transcription-quantitative PCR (uRT-qPCR) using nucleic acid extracts from blood samples (n = 114) obtained after standardized controlled human malaria infection (CHMI) with Plasmodium falciparum sporozoites.
KEYWORDS: CHMI, Plasmodium falciparum, diagnostics, elimination, isothermal, mass screen and treat, submicroscopic
ABSTRACT
Microscopy and rapid diagnostic tests (RDTs) are the main diagnostic tools for malaria but fail to detect low-density parasitemias that are important for maintaining malaria transmission. To complement existing diagnostic methods, an isothermal reverse transcription-recombinase polymerase amplification and lateral flow assay (RT-RPA) was developed. We compared the performance with that of ultrasensitive reverse transcription-quantitative PCR (uRT-qPCR) using nucleic acid extracts from blood samples (n = 114) obtained after standardized controlled human malaria infection (CHMI) with Plasmodium falciparum sporozoites. As a preliminary investigation, we also sampled asymptomatic individuals (n = 28) in an area of malaria endemicity (Lambaréné, Gabon) to validate RT-RPA and assess its performance with unprocessed blood samples (dbRT-RPA). In 114 samples analyzed from CHMI trials, the positive percent agreement to uRT-qPCR was 90% (95% confidence interval [CI], 80 to 96). The negative percent agreement was 100% (95% CI, 92 to 100). The lower limit of detection was 64 parasites/ml. In Gabon, RT-RPA was 100% accurate with asymptomatic volunteers (n = 28), while simplified dbRT-RPA showed 89% accuracy. In a subgroup analysis, RT-RPA detected 9/10 RT-qPCR-positive samples, while loop-mediated isothermal amplification (LAMP) detected 2/10. RT-RPA is a reliable diagnostic test for asymptomatic low-density infections. It is particularly useful in settings where uRT-qPCR is difficult to implement.
INTRODUCTION
Light microscopy (LM) and antigen-detecting rapid diagnostic tests (RDTs) are the primary diagnostic tools for the confirmation and management of suspected clinical malaria (1). Nucleic acid amplification tests (NAATs) based on PCR are commonly used for studies that require detection of low-density malaria infections, below the limit of detection of LM or RDTs, such as in controlled human malaria infection (CHMI) for early treatment decisions (2) and in low-transmission areas for epidemiological research and surveys (1).
In CHMI trials, volunteers are purposely infected either by the bite of infectious mosquitoes, direct intravenous injection of Plasmodium falciparum sporozoites (PfSPZ), or by injection of blood-stage parasites (3). In both cases, the asexual blood-stage infection starts with an extremely low parasitemia, below the detection threshold of conventional PCR assays or expert microscopists. In sporozoite-induced CHMI, the first-cycle blood-stage parasites can be detected by ultrasensitive quantitative real-time PCR (qPCR) around day 7, when hepatic merozoites are released into the bloodstream (4, 5), while expert microscopists require about 3 cycles of multiplication (∼day 11, 100- to 1,000-fold higher parasitemia) before thick blood smears are read as positive (5, 6). The qPCR sensitivity is enhanced by the inclusion of reverse transcriptase (RT-qPCR) and use of a higher blood volume enabling ultrasensitive detection (≤20 parasites/ml) (4, 5).
Sensitive diagnostics are fundamental for transmission intervention campaigns, particularly in areas of low endemicity or regions with declining transmission intensity, where a large proportion of P. falciparum infections are asymptomatic with very low parasite densities (7). These “hidden” submicroscopic infections constitute up to one-half of all infections detected by PCR (8). Without proper diagnosis and treatment, these highly prevalent asymptomatic infections represent an important infectious reservoir for malaria transmission (8).
Malaria control and prevention in the most vulnerable and high-risk groups (e.g., pregnant women) include intermittent preventive treatment (IPTp) with sulfadoxine-pyrimethamine (SP) (9). Screening with RDTs and treatment (intermittent screening and treatment in pregnancy [ISTp]) with artemisinin-based combination have been evaluated as an alternative approach to IPTp in areas with SP-resistant parasites (10). Highly sensitive diagnostics will be essential to improve clinical management and outcome of ISTp, since sequestration frequently leads to peripheral parasitemias below the diagnostic thresholds of microscopy and RDTs (10).
In recent years, non-PCR-based NAATs for use in low-resource settings have been developed. Best known are loop-mediated isothermal amplification (LAMP) and nucleic acid sequence-based amplification (NASBA) techniques. Recombinase polymerase amplification (RPA) is one of the most versatile isothermal amplification techniques which works at a fixed temperature between 37°C and 42°C, using minimally prepared samples in less than 20 min (11). Furthermore, RPA can be integrated with lateral flow strips for a quick read out without any complex equipment. These features potentially make RPA the preferred choice for use at the point-of-need, especially in low-resource settings, as a PCR substitute.
In this study, the application of reverse transcription-RPA (RT-RPA) as a robust, highly sensitive, and rapid diagnostic test for P. falciparum is described. The approach utilized abundant asexual stage-expressed rRNA and the coding genes (GenBank AL844504 and AL844506) as the template for amplification and the lateral flow strip for the readout. The diagnostic performance was evaluated in healthy volunteers with low-density parasitemia induced by standardized controlled human malaria infection (CHMI) with cryopreserved P. falciparum sporozoites (Sanaria PfSPZ challenge) (5, 6, 12, 13). A further simplified direct blood amplification approach was tested in Lambaréné, Gabon, to evaluate the assay in asymptomatic individuals from a setting where malaria is endemic.
MATERIALS AND METHODS
RPA primers and probe design.
Nucleotide sequence domains unique to P. falciparum were scanned by aligning large-subunit rRNA genes (28S), including those from human and other non-falciparum species. Amplification primers and the probe for lateral flow detection by a so-called “sandwich assay” were designed based on the guidelines from TwistDx (TwistAmp DNA amplification kits, combined instruction manual [2016]). The most efficient primer pair specific for P. falciparum RT-RPA was determined by testing three forward primers and reverse primers in different combinations analyzed by endpoint capillary electrophoresis (QIAxcel; Qiagen). Specificity of the primers was tested using malaria-naive samples as well as PCR-confirmed non-falciparum monospecies infection with Plasmodium vivax, P. malariae, P. ovale curtisi, and P. ovale wallikeri. The amplification was confirmed by direct sequencing using an ABI 3130XL DNA sequencer and homology search (BLAST) against NCBI GenBank. After working out the best pair of primers, a probe was designed along with modifications for lateral flow detections. The forward primer (Pfal28S_F1) was an unmodified oligonucleotide, while the reverse primer (Pfal28S_R1-Bio) was labeled with biotin at the 5′ end. The probe (Pfal28S_LF2) consists of an oligonucleotide backbone with a 5′ antigenic label (6-carboxyfluorescein), an internal abasic nucleotide analogue (dSpacer), and a polymerase extension blocking group (SpC3) at the 3′ end. All primers and probes were ordered from Eurofins Genomics (Ebersberg, Germany) and are shown in Table 1.
TABLE 1.
Primer and probe sequences
| Primer IDa | 5′→3′ sequence | Length (bp) |
|---|---|---|
| RPA_Pfal28S_F1 | GGAGTAGAAACTGAAATATGTTTTTACGACAG | 32 |
| RPA_Pfal28S_R1_Bio | Biotin-GAAATTGGGAGAAAGATAAGAAACAAGTTTC | 31 |
| RPA_Pfal28S_F2 | FAM-GTTGTTTTACTTATCCATTTATAGGGAAAT [dSpacer]TATTATGCTTTATCCTTCG-SpC3b | 50 |
ID, identifier.
The probe consists of 5′ antigenic label (6-carboxyfluorescein [FAM]), an internal abasic nucleotide analogue (dSpacer), and a polymerase extension blocking group (SpC3) at the 3′ end.
RT-RPA lateral flow test.
RT-RPA was performed using a TwistAmp nfo kit (TwistDx, TANFOO2) with the addition of SensiFAST reverse transcriptase (Bioline). The assay was performed in a total volume of 50 μl containing 420 nM each primer, 120 nM probe, 1× reverse transcriptase, 20 U RNase inhibitor, rehydration buffer, 4 μl template, and 14 mM magnesium acetate (MgAc). The master mix was prepared without the template and magnesium acetate and was distributed into each tube of a 0.2-ml 8-tube strip containing freeze-dried enzyme pellet followed by the addition of 4 μl template into the tubes. Magnesium acetate was pipetted into the tube lids and centrifuged into the reaction mix using a benchtop centrifuge. The reaction tubes were immediately incubated at 40°C for 20 min in a thermoblock-shaker (ThermoMixer Comfort; Eppendorf) with constant shaking at 300 rpm. After 6 min of incubation, the reaction tubes were removed and mixed by inverting 2 to 3 times, centrifuged, and reincubated for another 14 min. External positive- and negative-amplification controls were included in each run. The positive-amplification control consisted of nucleic acids prepared from confirmed P. falciparum-infected blood. The no-template control (NTC) consisted of nucleic acids extracted from blood of healthy malaria-naive volunteers. To eliminate carryover contamination, pre- and postamplification steps were performed in a separate room using pipettors for each work. Sterile aerosol protection filter tips (Nerbe plus, Winsen, Germany) were used in all assay setups. Amplification products were detected by nucleic acid lateral flow immunoassays using either HybriDetect 1 (Milenia Biotec, Germany) or PCRD (Abingdon Health, UK). For detection using HybriDetect 1, products were diluted 1 in 20 with 1× phosphate-buffered saline with 0.5% Tween (PBST) in a microcentrifuge tube. Strips were dipped into the diluted product, and the readout was observed within 10 min. Detection with PCRD was performed by diluting the product with the kit buffer (1 in 15), and the readout was observed within 10 min. Interpretation of results was based on a semiquantitative scoring system for the test line: none (no line visible), weak (barely visible), medium (similar to control line), strong (stronger than control line). Absence of the control line was considered an invalid result. Readings were performed by two investigators. In the case where the two readings were not concordant due to a weakly stained test band, the lateral flow assay was repeated with a new dipstick. A smartphone camera was used to capture the test results for electronic data storage and record keeping.
CHMI sample background.
Samples for evaluation of the RT-RPA were collected from volunteers enrolled in CHMI trials conducted in Tübingen, Germany (n = 39), and Lambaréné, Gabon (n = 36). Details of the three studies in Tübingen are published elsewhere (5, 6, 13). CHMI samples from Lambaréné included volunteers recruited for a malaria vaccine trial (PACTR201503001038304) published recently (12). All CHMI samples were collected following direct venous inoculation (DVI) of 3,200 aseptic, purified, cryopreserved Plasmodium falciparum sporozoites (strain NF54) as shown in Table 2. From the three studies conducted in Tübingen, samples were collected from three time points (days 6, 7, and 7.5) postinoculation of PfSPZ challenge; the time point of parasite egress from the liver. This time represents the subpatent period of low-density parasitemia in malaria-naive volunteers, approximately 4 days prior to malaria symptoms and microscopic detection of parasites by expert readers (5, 6, 13).
TABLE 2.
CHMI samples
| Study (no. of specimens) | No. of specimens |
Ethical approval | ||
|---|---|---|---|---|
| Aparasitemica | Subpatent parasitemicb | Patent parasitemicc | ||
| NCT02115516 (38) | 17 | 18 | 3 | The ethics committee of the Eberhard Karls University and the University Clinics of Tübingen |
| NCT02450578 (16) | 12 | 4 | 0 | The ethics committee of the Eberhard Karls University and the University Clinics of Tübingen |
| EudraCT-2017-002723-16 (24) | 13 | 11 | 0 | The ethics committee of the Eberhard Karls University and the University Clinics of Tübingen |
| PACTR201503001038304 (36) | 4 | 17 | 15 | The national ethics committee of Gabon and the Gabonese Ministry of Health |
Aparasitemic, uninfected, negative by RT-qPCR and TBS.
Subpatent parasitemic, positive by RT-qPCR only.
Patent parasitemic, positive by both RT-qPCR and TBS.
In a subset of samples (n = 5), the performance of RT-RPA was also compared to that of the Loopamp Malaria Pf detection kit (lot 49001; Eiken Chemical) at time points corresponding to second and third blood-stage cycles (days 9 and 11). Lastly, the assay was tested on semi-immune volunteers enrolled in a CHMI study conducted in Lambaréné. This included volunteers who became thick-smear positive and those who remained negative until the end of the follow-up period (day 35).
Blood samples from these volunteers were purified and previously tested by a validated RT-qPCR assay during the studies (5). Purification was either performed manually or automated using QIAsymphony SP (Qiagen). For manual extraction, 0.5-ml aliquots of EDTA-anticoagulated blood were processed using a QIAamp DNA blood minikit (catalog number [no.] 51306; Qiagen) and eluted into 100 μl of nuclease-free water (catalog no. 129114; Qiagen). With automation by QIAsymphony, nucleic acids were purified using 0.4 ml blood and eluted in 100 μl elution buffer.
Thick blood smear (TBS) microscopy and RT-qPCR methods have been implemented as the primary diagnostic tools for CHMI studies at the clinical trial platform in Tübingen. The TBS procedures are standardized to allow detection of at least 10 parasites/μl (14). Quantification of parasitemia by RT-qPCR relies on a standard curve obtained from laboratory P. falciparum 3D7 culture and is expressed as parasites per milliliter (p/ml) of blood (detailed standard operating procedures available upon request from the corresponding author) (5).
Direct blood RT-RPA.
For direct blood RPA, 28 blood samples were collected from asymptomatic, healthy Gabonese children (7 to 12 years) and adults after informed consent was given to be screened for prospective malaria drug/vaccine trials at CERMEL, Lambaréné, in October 2018. Volunteers willing to participate were screened for plasmodial infection with RDTs and microscopy. In parallel, those screening samples were evaluated for the diagnostic accuracy testing of the RPA. Inclusion criteria were provision of consent and being healthy, the exclusion criterion was clinically diagnosed or reported illness. The screening samples were collected in 1.2-ml blood collection tubes (Sarstedt S-Monovette 1.2 ml, K3 EDTA) for parasitological testing. From this, 100-μl blood aliquots were obtained from the study team for RPA. Direct blood RT-RPA was performed as mentioned above except that 4 μl fresh blood instead of purified nucleic acid was used in the reaction. All direct blood assays were performed in Lambaréné, and the test operators were blinded from any laboratory test results. The remaining 96 μl blood was used for purification (QIAamp DNA blood minikit). Both RT-RPA and RT-qPCR were performed using purified nucleic acids for comparison between the three tests.
Malaria LAMP assay.
From a subset of CHMI volunteers (n = 5), 1 ml heparin-anticoagulated whole blood was collected separately at days 9 and 11 after intravenous injection of P. falciparum sporozoites (PfSPZ) for LAMP, because EDTA interferes with the assay’s fluorescence readout (calcein). DNA extraction was performed by the boil method as described in the malaria LAMP standard operating procedure (SOP) by FIND’s malaria program (ver. AUG2012) and by spin columns (QIAamp DNA blood minikit; Qiagen). Amplification of P. falciparum DNA was carried out using the Loopamp Malaria Pf detection kit (lot 49001; Eiken Chemical) following the protocol by FIND’s malaria program (ver. AUG2012). For detection and interpretation of results, amplified products were visualized under a UV transilluminator. Calcein contained in the reagent mix emitted green fluorescence under UV light for a positive sample, while no light is emitted in a negative sample. For comparison, the same set of nucleic acid preparations were amplified by RT-RPA.
Data analysis.
The estimates of sensitivity and specificity of the assay were reported as positive percent agreement (PPA) and negative percent agreement (NPA), respectively, as the comparator RT-qPCR assay was a nonreference standard. The metrics to assess the diagnostic accuracy of the assay were calculated in R (version 3.5.1) using the epibasix package. The PPA was calculated as true positives/(true positives + false negatives) × 100 and the NPA as true negatives/(true negatives + false positives) × 100. The overall percent agreement was calculated as (true positives + true negatives)/(true positives + false negatives + true negatives + false positives) × 100.
RESULTS
Laboratory validation.
We designed primers from P. falciparum 28S rRNA genes located on chromosomes 5 and 7. Newly designed primers showed high specificity to P. falciparum. No cross-reactivity was observed with four non-falciparum species (P. vivax, P. malariae, P. ovale curtisi, and P. ovale wallikeri) as well as human DNA controls. Direct sequencing of the RPA amplicon showed 100% sequence similarity to GenBank P. falciparum (PF3D7_0726000).
Detection of submicroscopic low-density P. falciparum.
The analytical sensitivity was first tested on samples from CHMI volunteers at time points 6 to 7.5 days after inoculation with PfSPZ challenge. The median parasitemia during these time points by the reference RT-qPCR was 43 parasites/ml (95% confidence interval [CI], 20 to 76). From the total of 68 samples measured, the diagnostic accuracy was 95.6% compared to the reference. The positive percent agreement (PPA) and the negative percent agreement (NPA) were 88% (95% CI, 70 to 98) and 100% (95% CI, 92 to 100), respectively (Table 3).
TABLE 3.
Agreement between RT-RPA and RT-qPCR in detecting ultra-low-density parasitemia
| RT-RPA result | RT-qPCR reference (n) |
PPAa (95% CI) | NPAb (95% CI) | Median parasite density (no. parasites/ml) | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Positive | 23 | 0 | 88 (70–98) | 100 (92–100) | 43 |
| Negative | 3 | 42 | |||
PPA, positive percent agreement.
NPA, negative percent agreement.
Overall performance of RT-RPA with CHMI samples.
In total, 114 analyses were performed using nucleic acids prepared from aparasitemic, subpatent parasitemic, and patent parasitemic volunteers across four CHMI studies (in Tübingen and Lambaréné). The overall percent agreement between the reference and the RT-RPA was 93.9%, while the PPA and the NPA were 90% (95% CI, 80 to 96) and 100% (95% CI, 92 to 100), respectively. The kappa estimates of 0.88 suggested an excellent agreement between the tests (Table 4). Diagnoses of RT-RPA with 15 microscopically confirmed volunteers in Lambaréné were all positive (100% agreement). In total, seven volunteers with low-density infections were missed by the RT-RPA (median parasitemia, 24; 95% CI, 6 to 36) as shown in Fig. 1. Based on logistic regression model, the limit of detection in 95% of RT-qPCR positives was 64 parasites per ml (Fig. 1).
TABLE 4.
Overall performance of RT-RPA compared to that of RT-qPCR for the detection of Plasmodium falciparum using purified nucleic acids
| RT-RPA result | RT-qPCR reference (n) |
PPAa (95% CI) | NPAb (95% CI) | Accuracy (%) | κ value (95% CI) | |
|---|---|---|---|---|---|---|
| Positive | Negative | |||||
| Positive | 61 | 0 | 90 (80–96) | 100 (92–100) | 94 (88–97) | 0.88 (0.79–0.96) |
| Negative | 7 | 46 | ||||
PPA, positive percent agreement.
NPA, negative percent agreement.
FIG 1.
Logit analysis of RT-RPA diagnosis compared to that with RT-qPCR. Logit regression analysis using R on data sets of 114 RT-RPAs. The limit of detection in 95% of RT-qPCR positives was 64 parasites per ml.
Validation of direct blood RT-RPA in asymptomatic subjects.
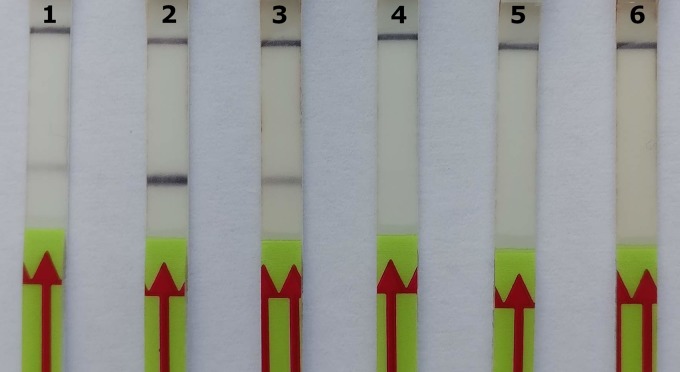
To simplify the assay further, the direct use of blood was first tested in the laboratory using frozen blood from a volunteer with confirmed low-density malaria infection. RPA worked with three EDTA-blood concentrations tested, and 8% blood in the reaction showed the best amplification with minimal inhibition (Fig. 2). Of 28 asymptomatic individuals tested in Lambaréné, nine were positive with the simplified RPA (dbRT-RPA). RT-qPCR later confirmed seven were truly positive and, in addition, showed one false negative by dbRT-RPA. The diagnostic accuracy of dbRT-RPA was 89% with fair to good agreement with the reference test (κ = 0.75). However, when RPA was performed on purified nucleic acids from the same blood aliquot of 100 μl, the test agreement was 100% with the reference (Table 5).
FIG 2.
Direct blood RT-RPA optimization with different blood volumes. Lateral flow detection test strips (HybriDetect; Milenia Biotec GmbH). Strip 1, reaction with 4% (vol/vol) malaria-positive blood; strip 2, reaction with 8% (vol/vol) malaria-positive blood; strip 3, reaction with 16% (vol/vol) malaria-positive blood; strip 4, reaction with 4% (vol/vol) malaria-negative blood; strip 5, reaction with 8% (vol/vol) malaria-negative blood; strip 6, reaction with 16% (vol/vol) malaria-negative blood.
TABLE 5.
Performance of direct blood RT-RPA for malaria screening test in healthy subjects
| Method | Result | RT-qPCR reference (n) |
PPAa (95% CI) | NPAb (95% CI) | Accuracy (%) | κ value (95% CI) | |
|---|---|---|---|---|---|---|---|
| Positive | Negative | ||||||
| dbRT-RPA | Positive | 7 | 2 | 88 (47–100) | 90 (68–99) | 89 (72–98) | 0.75 (0.48–1.02) |
| Negative | 1 | 18 | |||||
| RT-RPA | Positive | 8 | 0 | 100 (63–100) | 100 (83–100) | 100 (88–100) | 1 |
| Negative | 0 | 20 | |||||
PPA, positive percent agreement.
NPA, negative percent agreement.
Comparison of isothermal techniques.
LAMP kit for P. falciparum detection was originally evaluated during a PfSPZ vaccine trial (5) from five placebo-immunized control volunteers. For the purpose, blood samples were collected at two time points that coincided with peak parasitemia at day 9 (second-cycle blood stage) and day 11 (thick-smear patent period). RT-qPCR showed early blood-stage parasitemia in all five volunteers from day seven. Three became positive by thick smear at day 11, and the remaining became positive at days 12 and 18. By LAMP assay, clear positive amplification of P. falciparum DNA was seen only from two thick-smear-positive volunteers at day 11. The estimated parasitemia by thick smear were 4 and 14 parasites/μl. The same sample sets were analyzed with RT-RPA, and Table 6 shows the comparative results. All but one was positive by RT-RPA, showing 90% agreement with the reference RT-qPCR results (Fig. 3).
TABLE 6.
Performance of RT-RPA, LAMP, and microscopy compared to that of RT-qPCR
| Method | Result | RT-qPCR reference (n) |
PPAa (95% CI) | |
|---|---|---|---|---|
| Positive | Negative | |||
| RT-RPA | Positive | 9 | 0 | 90 (55–100) |
| Negative | 1 | 0 | ||
| LAMP | Positive | 2 | 0 | 20 (3–56) |
| Negative | 8 | 0 | ||
| TBSb | Positive | 3 | 0 | 30 (7–65) |
| Negative | 7 | 0 | ||
PPA, positive percent agreement.
TBS, thick blood smear.
FIG 3.
Recombinase polymerase amplification of P. falciparum NF54. Strip 1, volunteer 1, day 9 post-CHMI; strip 2, volunteer 2, day 9 post-CHMI; strip 3, volunteer 3, day 9 post-CHMI; strip 4, volunteer 4, day 9 post-CHMI; strip 5, volunteer 5, day 9 post-CHMI; strip 6, volunteer 1, day 11 post-CHMI; strip 7, volunteer 2, day 11 post-CHMI; strip 8, volunteer 3, day 11 post-CHMI; strip 9, volunteer 4, day 11 post-CHMI; strip 10, volunteer 5, day 11 post-CHMI; strip 11, malaria-naive healthy control.
DISCUSSION
Despite the need for improved diagnostics to enable the shift from malaria control to elimination, investment in research to accelerate the development and delivery of new diagnostics is minimal compared to the investment in drugs and vaccine development (15). Even though investments have grown since 2007, diagnostics comprised the smallest portion (2.8%) of all funding allocations available for malaria research and development during the period from 2014 through 2016 (16).
While preventing morbidity and death on the individual level can be achieved with treatment guided by LM and RDTs, malaria elimination requires targeting the infectious reservoir on a population level, which includes “asymptomatic carriers,” often with low-density parasitemia (17). The situation is most critical in low-endemicity settings, where such carriers constitute a large proportion of infections and contribute to malaria transmission (8). Current strategies to interrupt transmission, such as mass screening and treatment (MSAT) and focal testing and treatment, rely on the sensitivity of the diagnostics used to screen infected individuals for treatment (18). An effective outcome is modeled with a diagnostics test sensitivity at or below 0.1 parasites/μl (19), a threshold that can be easily achieved with RT-RPA. In the absence of field diagnostics with such a threshold, many of these trials rely on LM or RDTs; the results so far have not proven to influence transmission due to the high proportion of asymptomatic carriers that were not detected (18).
While asymptomatic malaria infection, first observed by Robert Koch in 1900 (20), has recently gained renewed interest in the context of malaria elimination and eradication, little is known about the clinical and long-term health consequences of harboring submicroscopic parasitemia. Generally, this gap in knowledge is attributed to the lack of efficient diagnostic tools and the notion of benefit conferred as “premunition” to superinfection among such carriers, thus impeding the urge to investigate the infection outcome (21). On the contrary, recent studies suggest that chronic asymptomatic infections can have an important impact, at least in high-risk groups, and has been associated with low birth weight and premature births in pregnancy (22). Hence, new sensitive diagnostics may have a role beyond epidemiology and guide treatment decision not only in CHMI trials. Depending on the primary endpoint, detecting and clearing asymptomatic parasitemia is essential to reduce the confounding factors of vaccine efficacy measurement and could also be improved by a quick point-of-need test (23).
Some advances were made in 2017 with the launch of a new-generation ultrasensitive RDT (uRDT) to corroborate screening tools in the field (24). However, its performance in settings of low endemicity with low-density parasitemia is still not good, wherein up to 56% of PCR-detectable P. falciparum infections were missed by uRDT (25). The performance of standard RDT as well as uRDT has been tested recently in the framework of CHMI studies for early diagnosis. However, RDTs do not meet the diagnostic sensitivity required to detect early blood-stage parasitemia (<1,000 parasites/ml). The sensitivity of RDTs is similar to that of expert microscopists (limit of detection [LOD] = ∼10 parasites/μl) in the CHMI trial platform (26). Therefore, in this study, we used ultrasensitive RT-qPCR as the only comparator to RPA.
LAMP is another diagnostic tool recommended by the WHO Global Malaria Programme for use in low-transmission settings (1). More than 26 malaria LAMP assays have been developed, and two are commercially available as a ready-to-use kit: the Loopamp MALARIA kit (Eiken Chemical Co.) and the Illumigene malaria LAMP (Meridian Bioscience) (27). Similar to the results from the previous field evaluations in Uganda (28) and Zanzibar (29), our result showed the performance of Loopamp MALARIA Pan/Pf detection kit (Eiken Chemical Co.) is not reliable for pre-elimination settings especially for screening low-density infections. Recently, RT-LAMP with increased diagnostic sensitivity compared to that of commercial LAMP kit has been developed (30). Together with our findings, this corroborates that targeting highly abundant and stable rRNA could greatly benefit malaria diagnosis of low parasite levels for malaria control and elimination efforts.
This is the first study to evaluate the diagnostic performance of RT-RPA for the detection of P. falciparum infections. RT-RPA far exceeded the sensitivity of the LAMP kit evaluated in this study. Notably, this study demonstrated that RT-RPA worked using unprocessed blood for the rapid detection of P. falciparum, i.e., without any nucleic acid extraction step, although purification of nucleic acids improved the diagnostic sensitivity. Further optimization is needed to improve the direct use of blood for malaria diagnosis as well as determine the diagnostic performance using nucleic acid purification from standard dried blood spots (DBS).
The assay limitations include a reduction in specificity of the lateral flow assay with incubation time. Thus, results should be interpreted immediately (within 10 min), which may be a hindrance to large sample analyses. However, we observed improved specificity by using 1× PBST buffer (with 0.5% Tween) as diluent for lateral flow assays. The other is a residual risk of carryover contamination using the lateral flow strips employed in this study. To detect the RPA product, the amplified product was first diluted and pipetted to a dipstick for analysis. This inevitable step thereby increases the risk of contamination of work surfaces and equipment with abundant amplicons from the reaction tube. Minimizing the chance of contamination is likely to be the major challenge for routine use of the assay with the current lateral flow strips, especially outside the laboratory. As an alternative, the new disposable lateral flow cassette (USTAR01, TwistDx) allows direct detection in a sealed cartridge without the need for dilution and opening of tubes, thus minimizing the chance of cross-contamination, suitable for field use. In addition, with modification in probe design, real-time detection of amplification is possible, e.g., by fluorescent probes and use of a real-time PCR instrument (or a fluorometer at 40°C). Hence, the technique is amenable to nucleic acid quantification and is compatible to standard high-throughput setups when a fully equipped laboratory is available.
In conclusion, this study highlighted steps taken toward the development of a simplified molecular test that shows potential as an effective screening tool for the rapid and accurate detection of submicroscopic P. falciparum infections.
ACKNOWLEDGMENTS
We thank all the patients and participants who agreed to participate in the CHMI studies, the staff of the Institute of Tropical Medicine, Tübingen, and Centre de Recherches Médicales de Lambaréné (CERMEL), Lambaréné, Gabon.
This work was supported by the German Center for Infection research (DZIF) and the National Institutes of Health (grant numbers 5R44AI055229 and 5R44AI058375) for the production of P. falciparum sporozoites (PfSPZ Challenge).
We report no conflicts of interest.
REFERENCES
- 1.World Health Organization. 2014. Policy recommendation on malaria diagnostics in low transmission settings. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 2.Walk J, Schats R, Langenberg MCC, Reuling IJ, Teelen K, Roestenberg M, Hermsen CC, Visser LG, Sauerwein RW. 2016. Diagnosis and treatment based on quantitative PCR after controlled human malaria infection. Malar J 15:398. doi: 10.1186/s12936-016-1434-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roestenberg M, Hoogerwerf M-A, Ferreira DM, Mordmüller B, Yazdanbakhsh M. 2018. Experimental infection of human volunteers. Lancet Infect Dis 18:e312–e322. doi: 10.1016/S1473-3099(18)30177-4. [DOI] [PubMed] [Google Scholar]
- 4.Hodgson SH, Douglas AD, Edwards NJ, Kimani D, Elias SC, Chang M, Daza G, Seilie AM, Magiri C, Muia A, Juma EA, Cole AO, Rampling TW, Anagnostou NA, Gilbert SC, Hoffman SL, Draper SJ, Bejon P, Ogutu B, Marsh K, Hill AVS, Murphy SC. 2015. Increased sample volume and use of quantitative reverse-transcription PCR can improve prediction of liver-to-blood inoculum size in controlled human malaria infection studies. Malar J 14:33. doi: 10.1186/s12936-015-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mordmüller B, Surat G, Lagler H, Chakravarty S, Ishizuka AS, Lalremruata A, Gmeiner M, Campo JJ, Esen M, Ruben AJ, Held J, Calle CL, Mengue JB, Gebru T, Ibáñez J, Sulyok M, James ER, Billingsley PF, Natasha KC, Manoj A, Murshedkar T, Gunasekera A, Eappen AG, Li T, Stafford RE, Li M, Felgner PL, Seder RA, Richie TL, Sim BKL, Hoffman SL, Kremsner PG. 2017. Sterile protection against human malaria by chemoattenuated PfSPZ vaccine. Nature 542:445–449. doi: 10.1038/nature21060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sulyok M, Rückle T, Roth A, Mürbeth RE, Chalon S, Kerr N, Samec SS, Gobeau N, Calle CL, Ibáñez J, Sulyok Z, Held J, Gebru T, Granados P, Brückner S, Nguetse C, Mengue J, Lalremruata A, Sim BKL, Hoffman SL, Möhrle JJ, Kremsner PG, Mordmüller B. 2017. DSM265 for Plasmodium falciparum chemoprophylaxis: a randomised, double blinded, phase 1 trial with controlled human malaria infection. Lancet Infect Dis 17:636–644. doi: 10.1016/S1473-3099(17)30139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.malERA Refresh Consultative Panel on Tools for Malaria Elimination. 2017. malERA: an updated research agenda for diagnostics, drugs, vaccines, and vector control in malaria elimination and eradication. PLoS Med 14:e1002455. doi: 10.1371/journal.pmed.1002455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.malERA Refresh Consultative Panel on Characterising the Reservoir and Measuring Transmission. 2017. malERA: an updated research agenda for characterising the reservoir and measuring transmission in malaria elimination and eradication. PLoS Med 14:e1002452. doi: 10.1371/journal.pmed.1002452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. 2018. Intermittent preventive treatment in pregnancy (IPTp). Last Modif 1. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 10.Desai M, Hill J, Fernandes S, Walker P, Pell C, Gutman J, Kayentao K, Gonzalez R, Webster J, Greenwood B, Cot M, Ter Kuile FO. 2018. Prevention of malaria in pregnancy. Lancet Infect Dis 18:e119–e132. doi: 10.1016/S1473-3099(18)30064-1. [DOI] [PubMed] [Google Scholar]
- 11.Piepenburg O, Williams CH, Stemple DL, Armes NA. 2006. DNA detection using recombination proteins. PLoS Biol 4:e204. doi: 10.1371/journal.pbio.0040204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dejon-Agobe JC, Ateba-Ngoa U, Lalremruata A, Homoet A, Engelhorn J, Paterne Nouatin O, Edoa JR, Fernandes JF, Esen M, Mouwenda YD, Betouke Ongwe EM, Massinga-Loembe M, Hoffman SL, Sim BKL, Theisen M, Kremsner PG, Adegnika AA, Lell B, Mordmüller B. 2019. Controlled human malaria infection of healthy lifelong malaria-exposed adults to assess safety, immunogenicity and efficacy of the asexual blood stage malaria vaccine candidate GMZ2. Clin Infect Dis 69:1377–1384. doi: 10.1093/cid/ciy1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Metzger WG, Theurer A, Pfleiderer A, Molnar Z, Maihöfer-Braatting D, Bissinger AL, Sulyok Z, Köhler C, Egger-Adam D, Lalremruata A, Esen M, Lee Sim K, Hoffman S, Rabinovich R, Chaccour C, Alonso P, Mordmüller BG, Kremsner PG. 6 December 2019. Ivermectin for causal malaria prophylaxis: a randomized controlled human infection trial. Trop Med Int Health doi: 10.1111/tmi.13357. [DOI] [PubMed] [Google Scholar]
- 14.Mordmüller B, Supan C, Sim KL, Gómez-Pérez GP, Ospina Salazar CL, Held J, Bolte S, Esen M, Tschan S, Joanny F, Lamsfus Calle C, Löhr SJZ, Lalremruata A, Gunasekera A, James ER, Billingsley PF, Richman A, Chakravarty S, Legarda A, Muñoz J, Antonijoan RM, Ballester MR, Hoffman SL, Alonso PL, Kremsner PG. 2015. Direct venous inoculation of Plasmodium falciparum sporozoites for controlled human malaria infection: a dose-finding trial in two centres. Malar J 14:117. doi: 10.1186/s12936-015-0628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peeling RW, McNerney R. 2014. Emerging technologies in point-of-care molecular diagnostics for resource-limited settings. Expert Rev Mol Diagn 14:525–534. doi: 10.1586/14737159.2014.915748. [DOI] [PubMed] [Google Scholar]
- 16.PATH. 2018. Bridging the gaps in malaria R&D: an analysis of funding—from basic research and product development to research for implementation. PATH, Seattle, WA. [Google Scholar]
- 17.Bell D, Fleurent AE, Hegg MC, Boomgard JD, McConnico CC. 2016. Development of new malaria diagnostics: matching performance and need. Malar J 15:406. doi: 10.1186/s12936-016-1454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. 2015. Mass drug administration, mass screening and treatment and focal screening and treatment for malaria. World Health Organization, Geneva, Switzerland. [Google Scholar]
- 19.Gerardin J, Eckhoff P, Wenger EA. 2015. Mass campaigns with antimalarial drugs: a modelling comparison of artemether-lumefantrine and DHA-piperaquine with and without primaquine as tools for malaria control and elimination. BMC Infect Dis 15:144. doi: 10.1186/s12879-015-0887-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Müller I, Bockarie M, Alpers M, Smith T. 2003. The epidemiology of malaria in Papua New Guinea. Trends Parasitol 19:253–259. doi: 10.1016/s1471-4922(03)00091-6. [DOI] [PubMed] [Google Scholar]
- 21.Laishram DD, Sutton PL, Nanda N, Sharma VL, Sobti RC, Carlton JM, Joshi H. 2012. The complexities of malaria disease manifestations with a focus on asymptomatic malaria. Malar J 11:29. doi: 10.1186/1475-2875-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen I, Clarke SE, Gosling R, Hamainza B, Killeen G, Magill A, O'Meara W, Price RN, Riley EM. 2016. “Asymptomatic” malaria: a chronic and debilitating infection that should be treated. PLoS Med 13:e1001942. doi: 10.1371/journal.pmed.1001942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bejon P, Mwangi T, Lowe B, Peshu N, Hill AVS, Marsh K. 2007. Clearing asymptomatic parasitaemia increases the specificity of the definition of mild febrile malaria. Vaccine 25:8198–8202. doi: 10.1016/j.vaccine.2007.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Das S, Jang IK, Barney B, Peck R, Rek JC, Arinaitwe E, Adrama H, Murphy M, Imwong M, Ling CL, Proux S, Haohankhunnatham W, Rist M, Seilie AM, Hanron A, Daza G, Chang M, Nakamura T, Kalnoky M, Labarre P, Murphy SC, McCarthy JS, Nosten F, Greenhouse B, Allauzen S, Domingo GJ. 2017. Performance of a high-sensitivity rapid diagnostic test for Plasmodium falciparum malaria in asymptomatic individuals from Uganda and Myanmar and naive human challenge infections. Am J Trop Med Hyg 97:1540–1550. doi: 10.4269/ajtmh.17-0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hofmann NE, Gruenberg M, Nate E, Ura A, Rodriguez-Rodriguez D, Salib M, Mueller I, Smith TA, Laman M, Robinson LJ, Felger I. 2018. Assessment of ultra-sensitive malaria diagnosis versus standard molecular diagnostics for malaria elimination: an in-depth molecular community cross-sectional study. Lancet Infect Dis 18:1108–1116. doi: 10.1016/S1473-3099(18)30411-0. [DOI] [PubMed] [Google Scholar]
- 26.Mpina MG, Raso J, Deal A, Pupu LA, Nyakarungu EL, Davis M. d C, Schindler T, Urbano V, Mtoro A, Hamad A, Lopez MSA, Pasialo BN. 2019. Sensitivity and specificity of a novel highly sensitive rapid diagnostic test for detecting low density Plasmodium falciparum infection during a controlled human malaria infection study in Equatorial Guinea, abstr P-292, p 89, Abstr ASTMH 68th Annual Meeting National Harbor, MD. [Google Scholar]
- 27.Lucchi NW, Ndiaye D, Britton S, Udhayakumar V. 2018. Expanding the malaria molecular diagnostic options: opportunities and challenges for loop-mediated isothermal amplification tests for malaria control and elimination. Expert Rev Mol Diagn 18:195–203. doi: 10.1080/14737159.2018.1431529. [DOI] [PubMed] [Google Scholar]
- 28.Katrak S, Murphy M, Nayebare P, Rek J, Smith M, Arinaitwe E, Nankabirwa JI, Kamya M, Dorsey G, Rosenthal PJ, Greenhouse B. 2017. Performance of loop-mediated isothermal amplification for the identification of submicroscopic Plasmodium falciparum infection in Uganda. Am J Trop Med Hyg 97:1777–1781. doi: 10.4269/ajtmh.17-0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Aydin-Schmidt B, Morris U, Ding XC, Jovel I, Msellem MI, Bergman D, Islam A, Ali AS, Polley S, Gonzalez IJ, Mårtensson A, Björkman A. 2017. Field evaluation of a high throughput loop mediated isothermal amplification test for the detection of asymptomatic Plasmodium infections in Zanzibar. PLoS One 12:e0169037. doi: 10.1371/journal.pone.0169037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohon AN, Getie S, Jahan N, Alam MS, Pillai DR. 2019. Ultrasensitive loop mediated isothermal amplification (US-LAMP) to detect malaria for elimination. Malar J 18:350. doi: 10.1186/s12936-019-2979-4. [DOI] [PMC free article] [PubMed] [Google Scholar]