Background
The coronavirus disease-2019 (COVID-19) pandemic has placed an unpredictable new strain on the healthcare system. Worldwide, the most affected countries face new, multifaceted COVID-19-specific risks for patients, surgeons, health care workers, institutions, and society. The risk of contagion is not homogeneously distributed among the population: immunocompromised patients, frail and comorbid patients and those with anatomical or surgical alterations of the upper airways seem to be the most prone to contagion. On the other hand, the risk of infection is higher in the hospital environment than in the community: presumed hospital-related transmission has been estimated to occur in more than 40% of cases [1]. For this reason, patients requiring periodical visits still need to access hospitals during this critical period, with potential exposure to SARS-CoV-2.
Head and neck cancer patients are generally at high-risk for COVID-19 infection and severe adverse outcomes. Given the highly contagious nature of the virus in respiratory droplets and aerosolization, it is reasonable to identify patients with tracheostomy or total laryngectomy as possibly those who are most exposed to infection. Laryngectomized patients also experience a high risk for the most severe complications of COVID-19, being in most cases former smokers and alcohol abusers with frequent medical comorbidities including chronic pulmonary disease, peripheral vascular disease, cardiac disease, cerebrovascular disease, diabetes, underlying cancer history, and a propensity for atelectasis due to loss of upper airway resistance [2]. Furthermore, without nasal humidification and filtration, they are also apt to acute infections due to impaired mucociliary function and mucosal irritation from dry and cold inspired air [2], [3]. In case of infection, laryngectomized patients carry a high risk of transmitting viral particles to surrounding people, both to healthcare workers and members of the community, due to their altered airway anatomy and to aerosolization of tracheal secretions [4].
In western countries, over the last 2–3 decades, there has also been a progressive shift from esophageal to prosthetic voice rehabilitation [5]. An intrinsic characteristic of modern voice prostheses is the need for office-based replacement within a median time of 70 days (95% CI 67–73) [5]. For the aforementioned characteristics, management of laryngectomized patients poses a challenge for the otolaryngologist during the current COVID-19 pandemic.
Protecting laryngectomized patients
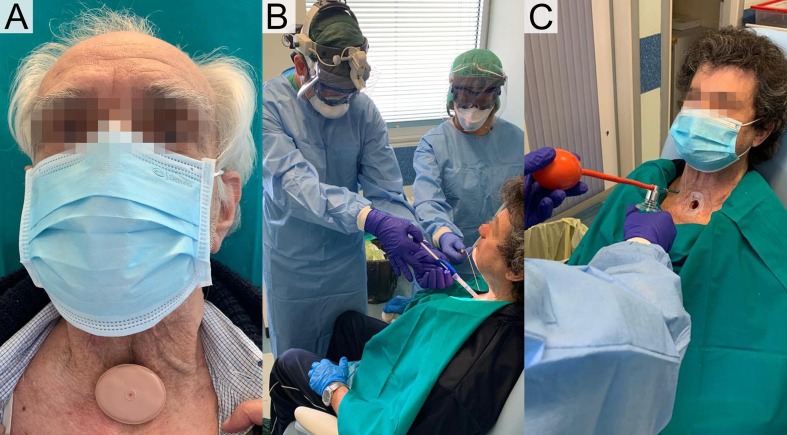
Impairment of nasal humidification and filtrating functions, due to anatomical iatrogenic changes of the upper aerodigestive tract after total laryngectomy, can be partially restored with the adoption of measures such as filtrating bibs or stomal devices with heat and moisture exchangers (HME). The latter, available from many commercial suppliers, are effective in reducing the incidence of tracheobronchial infections in laryngectomized patients [3]. Concerning the best protection of the laryngectomized during daily life in the community during the COVID-19 pandemic, we recommend the use of both facial protection (e.g., masks or scarfs) to reduce the risk of contact with oral or nasal mucosal surfaces and the adoption of filtrating devices to cover the stoma, possibly hidden with bibs or customized masks, to further reduce the risk of spreading droplets (Fig. 1 A).
Fig. 1.
Scenarios regarding safe management of laryngectomized patients during the COVID-19 pandemic. A laryngectomized patient wearing all recommended PPE: surgical mask and a highly efficient filter with a heat and moisture exchanger (A). The clinical setting of prosthetic valve replacement adopting safe PPE, considering all patients as potentially COVID-19 infected (B). Trans-stomal administration of local spray anesthesia to reduce cough reflex before prosthetic valve replacement (C).
Several ventilators’ filters with viral filtering capability are physically couplable with tracheostomy cannulas, but their resistance features, not specific for spontaneous breathing, should advise against their easy use in awaken laryngectomized patients. Among stomal HME filters, since 2007 is available the Provox Micron HME, aimed to reduce the risk of bacterial and viral infections in high-risk laryngectomized patients and to be used during flu epidemics. To the best of our knowledge, the Micron HME is the only specific stomal device with proven virus filtering properties available on the market. This device achieves its filtering activity through an electrostatic mechanism, without the need for a dense texture, and as such does not compromise the quality of life of patients in term of breathing or speaking functions (for voice prosthesis carriers) [6]. The device was developed by investigating the filtering activity against bacteriophage ΦX174, a virus measuring 22–25 nm in size, with 99.9% viral filtration efficiency [7]. These results, considering that SARS-CoV-2 particles are 60–140 nm [8], support the use of a Micron HME filter as further protection during the current ongoing COVID-19 pandemic.
Securing healthcare workers
Even during the COVID-19 pandemic, hospital visits for malfunctioning of voice prostheses i.e., in most cases leakage [5], cannot reasonably be avoided or delayed because of the risk of aspiration through the valve and consequent aspiration pneumonia. Considering the urgent nature of the procedure, patients cannot be tested beforehand for positivity to SARS-CoV-2. This, together with the technique itself which is performed by frontal direct tracheoscopy [9], exposes otolaryngologists and nurses to a high risk of contamination. Nevertheless, patients should be screened at hospital entrance for the presence of cough, sore throat, dyspnea, and fever (anosmia is not reliable in laryngectomies [10]): any patient with suspected COVID-19 positivity should be immediately referred to the emergency department triage.
After admitting the laryngectomized patient to the laryngology department, a safe prosthetic valve replacement procedure should be performed by using all the recommended personal protective equipment (PPE), and still considering the possibility that the patient may be infected but asymptomatic (Fig. 1B). This means that N95/FFP3/FFP2 masks, protective glasses, and gloves together with disposable water-repellent lab coats should be worn by nurses and physicians. The setting and instruments should be prepared in advance, while a small amount of local spray anesthesia (e.g. lidocaine 2%) should be administrated into the trachea to reduce coughing reflexes that are usually triggered by the procedure (Fig. 1C). Before and after the procedure, appropriate stomal filters should be placed by the patient. Finally, the outpatient clinic room should be sanitized at the end of the procedure.
Conclusion
The safe management of laryngectomized patients during the COVID-19 pandemic should be conducted carefully and responsibly, applying unprecedented cautious and preventive measures, with the awareness that there is high risk for both patients and healthcare providers. We recommend the regular use of a surgical face mask to prevent contact with mouth and nose mucosal surfaces and adhesive stomal support coupled with highly efficient HME filtering for all laryngectomized patients, during in-community activities that cannot be deferred (Fig. 1A). Furthermore, urgent procedures such as prosthetic valve replacement should not be delayed, since the risk of aspiration pneumonia is relevant. However, all precautionary measures for suspected COVID-19 patients should be taken (Fig. 1B and C).
Funding
None declared.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA – J Am Med Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hess M.M., Schwenk R.A., Frank W., Loddenkemper R. Pulmonary function after total laryngectomy. Laryngoscope. 1999;109:988–994. doi: 10.1097/00005537-199906000-00027. [DOI] [PubMed] [Google Scholar]
- 3.van den Boer C., van Harten M.C., Hilgers F.J.M., van den Brekel M.W.M., Retèl V.P. Incidence of severe tracheobronchitis and pneumonia in laryngectomized patients: a retrospective clinical study and a European-wide survey among head and neck surgeons. Eur Arch Oto-Rhino-Laryngol. 2014;271:3297–3303. doi: 10.1007/s00405-014-2927-4. [DOI] [PubMed] [Google Scholar]
- 4.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersen J.F., Lansaat L., Timmermans A.J., van der Noort V., Hilgers F.J.M., van den Brekel M.W.M. Postlaryngectomy prosthetic voice rehabilitation outcomes in a consecutive cohort of 232 patients over a 13-year period. Head Neck. 2019;41:623–631. doi: 10.1002/hed.25364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheenstra R.J., Muller S.H., Vincent A., Ackerstaff A.H., Jacobi I., Hilgers F.J.M. Short-term endotracheal climate changes and clinical effects of a heat and moisture exchanger with an integrated electrostatic virus and bacterial filter developed for laryngectomized individuals. Acta Otolaryngol. 2010;130:739–746. doi: 10.3109/00016480903382790. [DOI] [PubMed] [Google Scholar]
- 7.Nystrand R. Bio-TeQ Nystrand Consult; 2007. Test summary Atos Medical HME Micron (Report no. AM 071024) [Google Scholar]
- 8.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hilgers F.J.M., Ackerstaff A.H., Balm A.J.M., Bing Tan I., Aaronson N.K., Persson J.O. Development and clinical evaluation of a second-generation voice prosthesis (Provox®2), designed for anterograde and retrograde insertion. Acta Otolaryngol. 1997;117:889–896. doi: 10.3109/00016489709114220. [DOI] [PubMed] [Google Scholar]
- 10.Riva G., Sensini M., Corvino A., Pecorari G., Garzaro M. Smell and taste impairment after total laryngectomy. Ann Otol Rhinol Laryngol. 2017;126:548–554. doi: 10.1177/0003489417709794. [DOI] [PubMed] [Google Scholar]