A 70-year-old woman, receiving 7.5 mg prednisone as a maintenance therapy for rheumatoid arthritis (RA), presented with a rapidly, bilateral weakness and tingling sensation in all four extremities resulting in a total functional disability within 48 hours. The patient denied any sphincter disturbances, dyspnea or swallowing difficulties. She first received a diagnosis of RA exacerbation but no improvement was seen after corticosteroids increase. At admission to our Neurology department, at the tenth day of symptom's onset (April 13), neurological examination showed quadriplegia, hypotonia, areflexia and bilateral positive Lasègue sign. Cranial nerves were intact. Temperature, lung and cardiac auscultation were, also normal. On April 1st, three days prior to the ongoing symptom's onset, the patient presented an episode of dry cough without dyspnea or fever, spontaneously resolving within 48 hours. Initial blood tests showed no abnormality, except for a lymphocytopenia (520/ml, normal: 1500–5000). A nerve conduction study (NCS), on day 10, revealed a marked reduction or absence of electrical potentials in both motor and sensory nerves in all four limbs, with little or no abnormalities in conduction velocities and latencies. The needle electromyography (EMG) found diffuse and abundant fibrillation potentials at rest. These findings were consistent with an Acute Motor and Sensory Axonal Neuropathy (AMSAN) subtype of Guillain-Barré syndrome (GBS). CSF analysis showed increased protein level at 1 g per liter (normal range: 0,2–0,4) with normal white blood cell count. Chest CT (day 10) revealed ground-glass opacities in the left lung (Fig. 1 ). SARS-CoV-2 on RT-PCR assay was positive at oropharyngeal swab (day 10), negative in CSF. The patient was treated with intravenous immunoglobulin (2 g/kg for 5 days) and a combination of Hydroxychloroquine (600 mg per day) and Azithromycine (500 mg at the first day, then 250 mg per day). No significant neurological improvement is seen after one week of treatment.
Fig. 1.
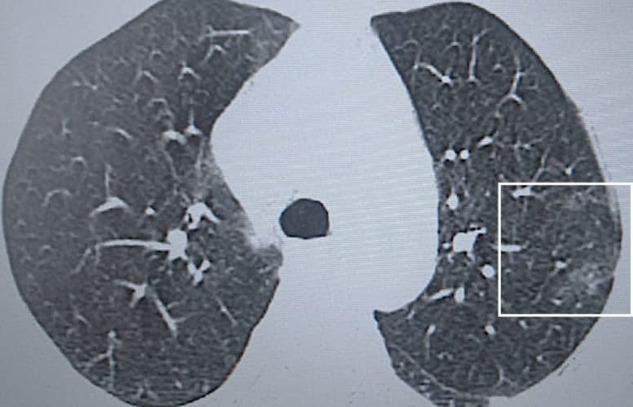
Chest computer tomography revealed a ground-glass opacities in the upper lobe of the left lung.
The Covid-19 infection hides many secrets that are yet to be revealed and little is known about its neurological manifestations. Here, we describe a case of a patient with mild respiratory symptoms linked to a COVID-19 infection, followed by a rapidly evolving quadriplegia arguing for a SARS-Cov-2-induced GBS. A negative PCR analysis in the CSF supports a post infectious, dysimmune mechanism.
Zhao et al. [1] reported the case of a 61-year-old man who presented with an Acute Inflammatory Demyelinating Polyneuropathy (AIDP) subtype of GBS, associated with SARS-Cov-2 infection. Being the first reported case, the authors questioned the cause-effect relationship between both events, since respiratory symptoms appeared after GBS's onset. After this first case, we found three other reports published to date. Camdessanche et al. [2] described a case of AIDP GBS subtype in a 64-year-old man, while the case of Sedaghat and Karim [3] resembled ours, an AMSAN form. Toscano et al. [4] reported a series of five patients from three Italian hospitals. Their findings were consistent with an axonal variant in three patients and with demyelinating process in two patients.
We add to the literature another case of GBS related to a Covid-19 infection. All these cases argues that SARS-Cov-2 virus could be a triggering factor of GBS. Since mild respiratory symptoms were noted in our patient, we suggest that all newly diagnosed Guillain-Barré cases should be tested for a Covid-19 infection in the current pandemic, even if they lack respiratory complaints. This would probably result in larger series and would help clarify the spectrum of this neurological condition.
Disclosure of interest
The authors declare that they have no competing interest.
Acknowledgement
The authors would like to give a special thanks to the colleagues and nurses at the departments of Neurology and Anesthesiology/reanimation and to Dr Mounir Zoubi.
References
- 1.Zhao H., Shen D., Zhou H., Liu J., Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020 doi: 10.1016/S1474-4422(20)30109-5. pii:S1474-4422(20)30109-5 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Camdessanche J.P., Morel J., Pozzetto B., Paul S., Tholance Y., Botelho-Nevers E. COVID-19 may induce Guillain-Barré syndrome. Rev Neurol. 2020 doi: 10.1016/j.neurol.2020.04.003. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sedaghat Z., Karimi N. Guillain Barre syndrome associated with COVID-19 infection: A case report. J Clin Neurosci. 2020 doi: 10.1016/j.jocn.2020.04.062. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toscano G., Palmerini F., Ravaglia S., Ruiz L., Invernizzi P., Cuzzoni M.G. Guillain-Barré syndrome associated with SARS-CoV-2. N Engl J Med. 2020 doi: 10.1056/NEJMc2009191. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]


