Severe acute respiratory syndrome coronavirus 2 is spreading rapidly worldwide, and coronavirus disease 2019 (COVID-19) has been declared a pandemic by the World Health Organization on March 11, 2020 [1]. This outbreak hit Europe deeply, with 582 554 cases and 47 741 deaths having been reported as of April 6, 2020 [2]. Despite the containment efforts implemented by the national political and health authorities of each Country, the pandemic has not reached its peak yet.
The exponential increase in the number of cases translated into an urgent need to reallocate medical resources to the assistance of COVID-19 patients, with redistribution of medical/surgical activities not primarily involved in the management of COVID-19 patients [3]. In the last month, in many European centers, the urological activity has been limited to urgent procedures and oncological priorities. However, what is to be considered a uro-oncological priority remains debatable, despite some recommendations having recently been published [3], [4]. What is even less clear is to what extent the postponement of uro-oncological procedures will impact patients and health care systems, given that the duration of the crisis is unpredictable and likely prolonged [5].
To provide a snapshot of the current uro-oncological management in Europe during the COVID-19 emergency and to estimate its future consequences, we conducted a survey involving 57 European urological referral centers. Urologists were asked to report on their activity concerning prostate, bladder, and kidney cancer from March 1 to March 31, 2020, as compared with a regular month before the COVID-19 outbreak.
Our results showed that the management of the main urological cancers has been altered dramatically by COVID-19 pandemic, with most European centers (82%) declaring to be “much” or “very much” affected. Uro-oncological consultations for newly diagnosed cancers and follow-up were more than halved or almost suspended, in 55% and 71% of centers, respectively. Prostate biopsies were reduced by 62%, with an average decrease of 23 biopsies per month. Given the aggressive nature of urothelial cancers, the restriction for transurethral resections of bladder tumors was smaller but still significant (46%), with a mean decrease of 12 procedures per month. In March 2020, a dramatic reduction was seen in major uro-oncological surgeries across Europe: radical prostatectomies, radical cystectomies, radical/partial nephrectomies, and nephroureterectomies decreased by 53%, 41%, 53%, and 52%, respectively. The majority of radical prostatectomies nowadays are performed with the robotic technique at referral centers, but the restrictions have specifically affected the access to the robot [4]. Centers estimate that >50% of uro-oncological procedures will have a delay well beyond 30 d from diagnosis, which is the recommended time frame within which newly diagnosed cases should definitely be treated [5].
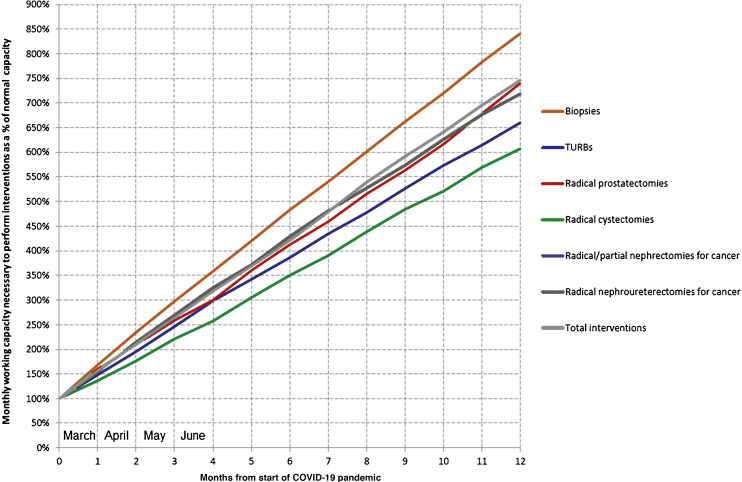
This is of special concern as the delay in a timely treatment will jeopardize oncological outcomes and have a ripple effect on future patients who will also suffer due to lengthening of waiting lists. After the end of the COVID-19 crisis, health systems will have to develop strategies to catch up with these delays. Given similar reduction rates from normal activity to what was seen in March, we tried to estimate the medical working capacity, which would be needed in order to absorb uro-oncological interventions that have been postponed second to the pandemic. The result has been derived from random simulation of monthly reductions in each type of intervention, as well in their total, based on the statistical distribution of survey reduction rates.
We found that, in the near future, uro-oncological surgeries should dramatically increase to treat all patients accumulated on waiting lists (Fig. 1 ). From patients’ point of view, the waiting time for uro-oncological procedures in Europe is estimated to double by the end of April and triple by the end of June. As surgical volumes of each institution cannot increase beyond a certain point, this will be a challenging but important issue to be addressed, specifically as the access to resources will be phased and competitive. In the meantime, delays in the waiting list might also have important implications in terms of patient anxiety and related depression.
Fig. 1.
Estimation of the medical working capacity needed to absorb uro-oncological interventions as a function of pandemic duration. COVID-19 = coronavirus disease 2019; TURB = transurethral resections of bladder tumor.
Our work may not provide precise estimates, as there are slight differences between European regions in terms of the pandemic’s course and effects. Different health care system resources, sociocultural backgrounds, and restrictive governmental measures also act as confounders. However, we provide a first timely estimate of the indirect effect of COVID-19 pandemic on the uro-oncological care based on real-time, first-hand reports of urological case patterns in Europe. In the time of crisis, uro-oncological surgeries should be centralized in tertiary urological centers that should ideally remain COVID-19–free sanctuaries, to guarantee high-quality, timely, and safe treatments to oncological patients. The health care fallout of the COVID-19 pandemic will surely be measured by the direct morbidity/mortality of the virus as well as the secondary effect that will include significant harm from delay of urgent oncological therapies, including surgeries.
Conflicts of interest: The authors have nothing to disclose.
Acknowledgments: We are thankful to all centers that participated in the Covid-19 European Uro-Oncology (CoEUrO) group survey, from Italy (n = 18), France (n = 9), Spain (n = 7), Belgium (n = 5), Germany (n = 5), UK (n = 4), Switzerland (n = 3), Austria (n = 1), Czech Republic (n = 1), the Netherlands (n = 1), Norway (n = 1), Portugal (n = 1), and Turkey (n = 1).
References
- 1.Sohrabi C., Alsafi Z., O’Neill N. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.European Centre for Disease Prevention and Control. Situation update for the EU/EEA and the UK, as of 1 April 2020. https://www.ecdc.europa.eu/en/cases-2019-ncov-eueea.
- 3.Ficarra V, Novara G, Abrate A, et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. In press. 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed]
- 4.Mottrie A. ERUS (EAU Robotic Urology Section) guidelines during COVID-19 emergency. https://uroweb.org/eau-robotic-urology-section-erus-guidelines-during-covid-19-emergency/.
- 5.Naspro R, Da Pozzo L. Urology in the time of corona. Nat Rev Urol. In press. 10.1038/s41585-020-0312-1. [DOI] [PMC free article] [PubMed]