Abstract
Background:
The Veterans Affairs Healthcare System implemented a computer-based tool (iMedConsent™) to improve the quality of informed consent in 2004. The impact of this tool on the process of informed consent remains unknown. Our aim was to determine the impact of iMedConsent™ on patient information preference, anxiety, trust in the surgeon, ambivalence about the surgical decision, and comprehension of procedure-specific risk, benefits and alternatives.
Materials and Methods:
We prospectively enrolled a consecutive cohort of patients presenting to a general surgery clinic for possible cholecystectomy or inguinal herniorrhaphy from October 2009 to August 2010. We administered questionnaires before and after the clinic visit.
Results:
75 patients completed pre-visit questionnaires. After evaluation by the surgeon, 42 patients were offered surgery and documented their informed consent using iMedConsent™, of which 38 (90%) also completed a post-visit questionnaire. Among the participants who completed both pre- and post-visit questionnaires, participant comprehension of procedure-specific risks benefits and alternatives improved from 50% at baseline to 60% after the clinic visit (p<.001). No differences were noted in ambivalence, trust or anxiety. After the clinic visit, significantly more patients expressed a preference for participating in decision making with their surgeon (98% vs. 71%, p=.008). However, significantly fewer expressed a preference for knowing all possible details about their illness (25% to 83%, p=<.001).
Conclusions:
The informed consent process using iMedConsent™ improves patient comprehension of procedure-specific risks, benefits and alternatives. It also increases patient preferences for participating more actively in the decision-making process. However, the process may provide more detail than patients want regarding their illness.
Keywords: informed consent, decision-making, information preference, participation preference, ethics, trust, anxiety
Introduction
Informed consent (IC) is a legal, ethical and regulatory requirement for the practice of surgery.(1–3) The legal concept of IC was developed to protect patients’ rights to self-determination with regard to health care decisions. Ethically, the practice of IC extends beyond the narrow legal definition to empower patients to exercise their autonomy and participate in shared decision making. Despite efforts to implement IC, evidence indicates that the process of IC has limited impact on clinical care. For example, patients do not remember much of the information disclosed during the IC process,(4–7) and they often over-estimate their level of comprehension.(8–10) Data also suggest that the IC process can inadvertently increase patient anxiety.(11–14) Finally, the impact of the IC process can be compromised when clinicians and administrators approach IC as merely a signature on a form.(15)
To improve the quality of the IC process, the Veterans Affairs Healthcare System implemented a system-wide computer-based tool, iMedConsent™ in 2004.(16) iMedConsent™ (iMed) is designed to standardize the IC process and create high-quality IC documents. iMed promotes the delivery of standardized information regarding the surgical risks, benefits and alternatives while documenting the details of the IC discussion in the patient’s electronic record. iMed also contains educational resources such as anatomical diagrams and instructions that can function as decision-aids for patients and providers. The program is integrated within the VA’s electronic medical record system, and it is launched by the clinician. After selecting the IC template for the appropriate procedure, the clinician may then modify the form to suit the needs of the particular patient. The IC document can be viewed online by both the physician and the patient, and it can be printed if so desired. When the document is complete, a signature pad is used to capture the electronic signature of the clinician, patient and witness before a signed version is uploaded into the patient record.
Fink, et al. studied iMed and found that patient comprehension of the elements of IC improved when iMed was programmed to prompt clinicians to request patients to repeat back in their own words the relevant risks, benefits and alternatives to surgical treatment.(17) They also found that comprehension improved as patients and providers together spent more time with iMed, though the improvement plateaued after 15 minutes.(18) However, Fink, et al. did not measure the change in patient comprehension before and after using iMed, thus limiting the evidence that iMed leads to improved comprehension. Our prospective cohort study aimed to provide stronger evidence of iMed’s effects by measuring patient comprehension of procedure-specific risks, benefits and alternatives before and after using iMed to document IC for either cholecystectomy or inguinal herniorrhaphy. We also tried to understand how iMed affected patients’ information preferences, anxiety, trust in their surgeon and ambivalence about their decision to have surgery. We hypothesized that when compared to baseline, patient comprehension of procedure-specific risks, benefits and alternatives would improve after documenting IC with iMed. We further hypothesized that patients’ anxiety, trust in their physician and ambivalence about their decision to have surgery would vary according to their information preferences (e.g., patients who preferred less information would experience increased anxiety after the IC process).
Materials and Methods
Participants were recruited from the General Surgery Clinic at the VA Pittsburgh Healthcare System from October 2009 to August 2010. We approached consecutively all patients presenting for elective inguinal herniorrhaphy or cholecystectomy for benign biliary disease. To avoid bias from participants’ previous experience with IC for inguinal herniorrhaphy, we excluded patients presenting with recurrent or contralateral hernias who had had previous inguinal herniorrhaphies. We also excluded patients who: (1) required surrogate consent; (2) underwent non-elective surgery; (3) could not communicate in English; (4) had uncontrolled psychiatric illness limiting their capacity to participate in the study; (5) were younger than 18 years old; (6) were prisoners; (7) had severe visual impediments that limit their capacity to read written material; or (8) did not complete the iMed IC document during the course of the study.
Enrolled participants completed questionnaires immediately before meeting the surgical providers to assess demographics, health literacy, health related functional status, information preferences, anxiety, trust in the surgical provider, ambivalence about the decision for surgery and comprehension of procedure-specific risks, benefits and alternatives. Participants then proceeded with their scheduled clinic visit. Participants who did not need surgery or otherwise chose not to have surgery were subsequently excluded from the study per protocol. Those participants who elected to have surgery and documented IC with iMed were then given a second questionnaire to measure changes in information preferences, anxiety, trust in the surgical provider, ambivalence about the decision for surgery and comprehension of procedure-specific risks, benefits and alternatives. This second questionnaire was completed immediately following the clinic visit during which the participant documented IC with iMed.
The questionnaires took approximately 30 minutes to complete at baseline and 15 minutes to complete in follow up. The primary outcome was comprehension of procedure-specific risks, benefits and alternatives measured using a 23-item Consent Comprehension Questionnaire specific to either cholecystectomy or herniorrhaphy. Fink, et al. developed the instrument for cholecystectomy,(17) and we developed a similar instrument for patients consenting to inguinal herniorrhaphy. Each instrument included questions about the nature of the surgery, the potential benefits and alternatives to surgery, and both common and key risks of the surgery. Each participant’s comprehension score was calculated as the percent of the total questions answered correctly. Using the methods of Fink, et al., we calculated subscales for comprehension of the nature of the operation, surgical benefits, alternatives, common risks and key risks.(17)
Secondary outcomes were trust in the surgical provider, anxiety state and ambivalence (or confidence) about the decision for surgery. These variables were measured by the Trust in Physician Scale(19, 20) (11 items using a 5 point Likert scale), the Short Form State Scale of the State Trait Anxiety Index(21) (6 items using a 4 point Likert scale), and the Ambivalence Scale(22–25) (7 items using a 4 point Likert scale). The Trust in Physician Scale was modified to reference the surgeon specifically. The Ambivalence Scale was also modified to make the questions contextually appropriate to the decision to have surgery.
Patient preferences were measured with three previously validated instruments to explore if these preferences mediated the changes in primary and secondary outcomes. The Cassileth Information Styles Questionnaire(26) used two, single-item questions on a 5 point Likert scale to assess Information Preference (the preferred amount of detail regarding health status) and Participation Preference (preference for making healthcare decisions independently from, in collaboration with or in deference to the doctor). The Information Seeking subscale of the Autonomy Preference Index(27) used 8 items on a 5 point Likert scale to assess the preference for seeking information about health status. The Michigan Assessment of Decision Style(28, 29) measured the preferred style of decision making and consists of four independently analyzed factors: information seeking, deliberation, avoidance and deferring responsibility. Each factor was measured with 4 items on a 5 point Likert scale (16 items total).
Covariates included age, race, marital status, religiousness, income, and education level assessed with standard items. Health Literacy was measured with the REALM-7(30, 31) that tests the accurate pronunciation of 7 medical terms and corresponds to grade level: 4th–6th grade (1–3 correct); 7th–8th grade (4–6 correct); 9th grade or higher (7 correct). Health Related Functional Status was measured with the SF-12 v.2(32) consisting of 12 items on a 6 point scale scored according to 2 factors (physical and mental health) with a range from 6–36.
We calculated mean values for each of the multi-item instruments except for the REALM-7 and the SF-12 which are reported as counts. We then compared baseline characteristics for those participants who completed both the pre- and post-visit questionnaires and those who completed only the pre-visit questionnaire. We used Chi-square statistics for categorical measures and t-tests for continuous measures. In cases where the cell frequencies for categorical variables were < 10, we used Fishers exact tests. For categorical measures, we used repeated measure chi-square tests to assess changes pre to post. For continuous measures (e.g., knowledge, anxiety, trust and ambivalence), we used random effects regressions to assess change. The regression models were then expanded to include both the time variable (pre or post) and either decision style, information seeking preference, participation preference or information preference. The interactions of decision style and time were included in subsequent more complex models. The complex models should be considered exploratory because of the small number of subjects in the study. All analyses were conducted with STATA v. 11 (Stata Corp, College Station, Texas 2009). Significance was defined as p<.05 (two-sided). This research was approved by the Institutional Review Board of the VA Pittsburgh Healthcare System and was conducted in accordance with the Helsinki Declaration of 1975.
Results
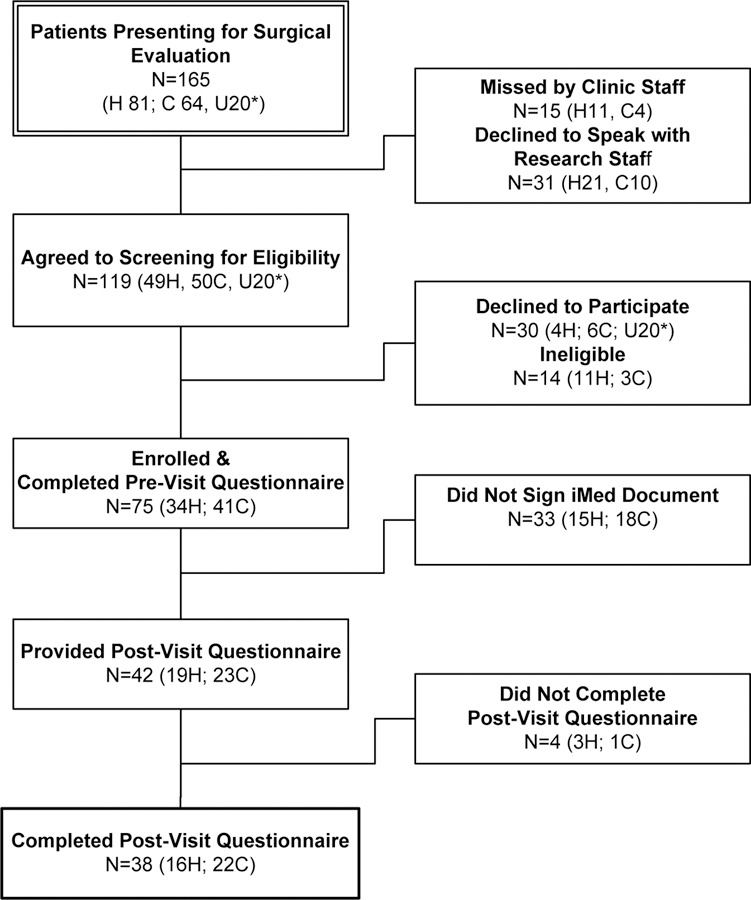
75 of the 165 consecutive patients presenting to the general surgery clinic for either inguinal herniorrhaphy or cholecystectomy agreed to participate and completed the baseline, pre-visit questionnaire (Figure 1). There were no statistically significant differences in age, race or gender between the 75 enrolled participants and the 90 patients who did not enroll (data not shown). 42 of the enrolled participants elected to have the recommended surgery, documented IC using iMed, and were given the post-visit questionnaire. 38 completed the post-visit questionnaire. The 33 patients who did not sign the iMed IC document were not suitable candidates for surgey, and were therefore not offered an operation (e.g., the referring diagnosis was not confirmed or the patient’s comorbidities made operative intervention too risky).
Figure 1: Flow chart of participant screening and enrollment.
Participants included patients presenting for surgical evaluation of either Inguinal Herniorrhaphy (H) or Cholecystectomy (C). The type of procedure (H or C) is indicated at each step of the flow chart except in those cases where the procedure type is unknown (U). Procedure type is unknown because the initial protocol was not designed to record data about patients who declined to participate. However, during the course of data collection, the protocol was modified to record data about patients who declined to participate.
Table 1 contains demographic characteristics for both the 38 participants who completed both the pre and post-visit questionnaires as well as the 37 participants who only completed the pre-visit questionnaire. There were no statistically significant differences between these groups. In the 38 who completed both questionnaires, there were 2 female and 3 African American participants, the mean age was 56.2 (range 28–81), 92% completed high school and 40% had an income >$30,000.
Table 1:
Comparison of the pre-visit characteristics of participants who did and did not complete the post-visit questionnaire.
| Pre-Visit Characteristic† | Completed Pre and Post-Visit Questionnaires | Completed Only Pre-Visit Questionnaire | p value* | ||
|---|---|---|---|---|---|
| (N=38) | (N=37) | ||||
| Age (Mean Years±SD) | 56.2±12.8 | 61.0±11.0 | 0.09 | ||
| n | % | n | % | ||
| Sex Male | 35 | 95 | 34 | 97 | 1.00 |
| Female | 2 | 5 | 1 | 3 | |
| Race White | 30 | 79 | 31 | 84 | 0.49 |
| Black | 3 | 8 | 4 | 11 | |
| Other (includes missing†) | 5 | 13 | 2 | 5 | |
| Hispanic/Latino Yes | 2 | 5 | 0 | 0 | |
| Do you live alone? Yes | 12 | 33 | 13 | 39 | 0.60 |
| No | 24 | 67 | 20 | 61 | |
| Marital Status | |||||
| Never Married | 9 | 24 | 6 | 17 | 0.42 |
| Currently Married | 18 | 47 | 15 | 42 | |
| Living with Partner | 5 | 13 | 3 | 8 | |
| Separated | 0 | 0 | 2 | 6 | |
| Divorced | 6 | 16 | 10 | 28 | |
| Education | |||||
| Less than high school | 3 | 8 | 1 | 3 | 0.74 |
| High School/GED | 12 | 33 | 14 | 39 | |
| Trade school or some college | 15 | 42 | 16 | 44 | |
| At least a BA/BS/BFA | 6 | 17 | 5 | 14 | |
| Income <$13,000 | 10 | 29 | 8 | 22 | 0.35 |
| $13,000-$19,000 | 5 | 14 | 9 | 24 | |
| $20,000-$29,999 | 6 | 17 | 10 | 27 | |
| >$30,000 | 14 | 40 | 10 | 27 | |
| Health Literacy (mean±SD) | 6.3±0.2 | 6.2±0.2 | 0.61 | ||
| Health Related Quality of Life (mean±SD) | |||||
| SF-12 Physical Health | 33.1±11.8 | 34.5±11.9 | 0.61 | ||
| SF-12 Mental Health | 49.8±11.5 | 52.1±9.4 | 0.35 | ||
For any single question, missing data were < 5% of the study sample and were censored before calculating reported means and proportions.
p values were calculated using t-tests for comparison of means, chi-square tests for comparisons of proportions across groups, and Fisher Exact test for comparison of proportions across groups when cell frequencies were small (<5).
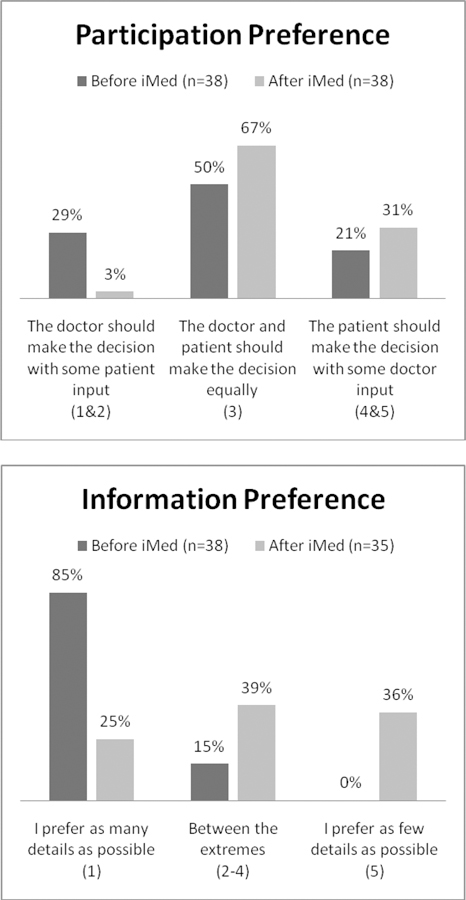
Figure 2 demonstrates that after the clinic visit during which they signed the iMed IC document, more Veterans expressed a preference for participating in decision making with their doctor (98% vs. 71%, p=.008). However, fewer expressed a preference for knowing all possible details about their illness (25% vs. 85%, p=<.001). Patients’ comprehension of procedure-specific risks benefits and alternatives improved from 50% at baseline to 60% after the clinic visit (p<.001, see Table 2). There were statistically significant improvements in all comprehension subscales except comprehension of alternatives to surgical treatment. No pre-and post-visit differences were noted in ambivalence, trust or anxiety.
Figure 2: Comparison of patient preferences before and after signing iMed.
Bar graphs show changes in preferences before (dark) and after (light) signing iMed. After signing iMed participants expressed preferences for more participation (p=0.008), but less information (p<.001). Each preference was measured on a 5 point Likert scale. Based on data distribution, the response categories were aggregated as indicated in parentheses. P values were calculated with the repeated measures chi-square test for symmetry.
Table 2:
Comparison of outcomes before and after signing iMedConsent™.
| Outcome | Before iMed (N=38) |
After iMed (N=38) |
p value* |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Procedure-specific knowledge‡ | 0.50±0.20 | 0.60±0.18 | < 0.001 |
| Understanding operation | 0.33±0.31 | 0.74±0.32 | < 0.001 |
| Alternatives | 0.43±0.25 | 0.38±0.26 | 0.29 |
| Benefits | 0.66±0.29 | 0.76±0.25 | 0.02 |
| Overall risks | 0.50±0.27 | 0.60±0.21 | 0.002 |
| Key risks | 0.38±0.42 | 0.68±0.35 | 0.001 |
| Trust in the surgeon | 3.67±0.50 | 3.84±0.60 | 0.11 |
| Ambivalence about the decision to have surgery | 2.21±0.66 | 2.24±0.54 | 0.67 |
| Anxiety State | 1.97±0.56 | 1.91±0.57 | 0.29 |
| Decision Style (Range 1–4)† | |||
| Defer Responsibility | 3.98±0.92 | ||
| Information Seeking | 2.91±1.24 | ||
| Deliberation | 3.68±0.83 | ||
| Avoidance | 1.78±0.75 | ||
| Information Seeking Preference (Range 1–5)† | 4.49±0.56 | ||
Changes assessed with random effects regression models; p values calculated using the Wald z-test for paired data.
The measures of procedure-specific knowledge contained questions testing five separate subscales as described in the text. Knowledge scores are reported as the proportion of correct answers. The proportion of correct answers on all items is reported first, and then the proportion of correct answers is reported for each subscale.
These characteristics were assessed only on the post-iMed questionnaire as potential mediators of changes in outcomes; no statistical comparison is indicated.
Table 2 also shows the mean values for decision style and information seeking preference as assessed in the post-visit questionnaire administered after signing iMed. These variables were measured once to explore how they might mediate observed changes in the primary and secondary outcomes. Random effects multivariable regression analyses suggest that the observed improvement in knowledge scores was primarily found among those patients endorsing a deferring decision-making style (they arrive knowing less than others, but leave knowing the same as others, p=.058). In contrast, those endorsing a deliberative decision-style arrived knowing 9% more than others (p=.009), but did not improve after the clinic visit. The information seeking decision style was associated with lower trust in the physician (p=.01) and increased anxiety (p=.05). The deferring decision style was associated with increased trust (p=.07) and lower comprehension of the nature of the operation (p=.001). The avoiding decision style was associated with worse comprehension of the nature of the operation (p =.05).
Discussion
There are three key findings from our study. First, the IC process using iMed improved overall patient comprehension of procedure-specific risks, benefits and alternatives from 50% to 60% before and after using iMed to document IC for cholecystectomy and herniorrhaphy. Improvements were found in all comprehension subscales except for comprehension of alternatives to recommended surgery. This suggests that surgeons might pay more attention to explaining relevant alternatives to cholecystectomy and herniorrhaphy. Second, our data also demonstrated that documenting IC with iMed changes patient preferences for participating in medical decision making. Before the clinic visit, 29% of patients preferred that the doctor be the primary decision-maker, but after documenting IC with iMed only 3% of patients had this preference. Third, at the same time that the IC process appears to empower patient participation, it may overwhelm some patients with more information than they want. Fully 85% of patients arrived in the clinic wanting to know as many details as possible about their health status, but after the clinic visit, only 25% continued to report this preference. At the same time, the proportion of patients preferring as few details as possible increased from 0% to 36%. These preliminary findings may warrant reconsidering the amount of detail disclosed in the iMed documents and the IC process.
Exploratory analyses of our data also suggested that patient comprehension of procedure-specific risks, benefits and alternatives improved primarily in those patients endorsing a deferring decision-making style. On the other hand, an information-seeking decision-making style was associated with increased anxiety and decreased trust. These results may explain why previous studies of IC and anxiety had mixed findings.(11–14) The impact of IC on anxiety may depend on the patient’s decision making style, suggesting that a one-size-fits-all approach to IC may not serve all patients equally well.
In the only other study of iMed in a Veteran population, Fink, et al reported a post-visit comprehension score of 68% among patients documenting IC for cholecystectomy. This comprehension score increased to 69.5% among those patients asked to repeat back the relevant risks, benefits and alternatives(17). This improvement in comprehension attributable to “repeat back” is similar in magnitude to the other enhancements of IC recently reviewed by Schenker, et al.(33) Fink, et al conclude that the improvements in patient comprehension attributable to repeating back relevant risks, benefits and alternatives warrants consideration of “repeat back” as a routine enhancement of IC.(17) However, we note that the incremental improvement is only modest (1.5%), especially when compared to the improvement attributable to “standard” iMed reported here (10%). Indeed, the data from Fink, et al suggest that the incremental improvement in comprehension varied with time spent with iMed: patients spending less than 5 minutes on consent scored 65% whereas those spending 15 minutes or more scored 78%.(18) Future research might include examine ways to optimize the time spent with iMed and modeling the cost-effectiveness of implementing “repeat back” or other enhancements to the basic iMed application.
It is of some concern that the absolute levels of comprehension reported here are not good. The Consent Comprehension Questionnaire was designed by Fink, et al with the intention that a score of 70% would indicate adequate comprehension.(17) Despite attempts to inform patients adequately regarding the risks, benefits and alternatives relevant to their surgery, patient comprehension in this cohort remains below what some would consider a minimum standard.(33) This finding is similar to other studies that demonstrate that patients do not remember much of the information disclosed during the IC process.(4–7) Although iMed increases patient comprehension, there is still room for improvement.
The primary limitation of this study is the small sample size that limits the number of variables that can be modeled in the regression analyses and the generalizability of the findings. The data also reflect a single site, and may not represent findings in other Veteran populations, further limiting the generalizability of the findings.
In conclusion, the informed consent process using iMed improves patient comprehension of procedure-specific risks, benefits and alternatives. It also empowers patients to participate more actively in the decision-making process. However, the process may provide more detail than patients want regarding their illness. It also suggests that patients experience the standardized iMed IC process differently according to individual patient preferences for decision-making style. Future research could be directed to better understanding how patient preferences influence relevant outcomes like anxiety, trust in the surgeon, and comprehension of relevant risks, benefits and alternatives. The IC process could then be explicitly adapted to meet the specific preferences of particular patients by tailoring the type and quantity of information disclosed.
Acknowledgement:
The authors wish to thank Drs. Aaron Fink and Alan Prochazka for their gracious advice regarding the design of this study. This research was funded by grants from VA HSR&D (CDA 08-281), VISN4 Competitive Pilot Project Fund (XVA 72-057), and the CHERP Pilot Project Program (LIP 72-043).
Financial Support: This research was funded by grants from VA HSR&D (CDA 08-281), VISN4 Competetive Pilot Project Fund (XVA 72-057), and the CHERP Pilot Project Program (LIP 72-043).
Footnotes
Presentation: This research was presented as a poster at the VA Health Services Research and Development National Meeting on February 17, 2011 in National Harbor, Maryland
References
- 1.Beauchamp TL, and Childress JF Principles of Biomedical Ethics. New York: Oxford University Press, 1989. [Google Scholar]
- 2.Office of the General Counsel AMA Infomed Consent. 1998.
- 3.American Medical Association Informed Consent. Code of Medical Ethics, 1981.
- 4.Lloyd A, Hayes P, Bell P, and AR N The role of risk and benefit perception in informed consent for surgery. Med Decis Making 21: 141–149, 2001. [DOI] [PubMed] [Google Scholar]
- 5.Leeb D, Bowers DG Jr., and Lynch JB Observations on the myth of “informed consent”. Plast Reconstr Surg 58: 280–282, 1976. [DOI] [PubMed] [Google Scholar]
- 6.Lavelle-Jones C, Byrne DJ, Rice P, and Cuschieri A Factors affecting quality of informed consent. BMJ 306: 885–890, 1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hutson MM, and Blaha JD Patients’ recall of preoperative instruction for informed consent for an operation. J Bone Joint Surg Am 73: 160–162, 1991. [PubMed] [Google Scholar]
- 8.Lashley M, Talley W, Lands LC, and Keyserlingk EW Informed proxy consent: communication between pediatric surgeons and surrogates about surgery. Pediatrics 105: 591–597, 2000. [DOI] [PubMed] [Google Scholar]
- 9.Tait AR, Voepel-Lewis T, and Malviya S Do they understand? (part II): assent of children participating in clinical anesthesia and surgery research. Anesthesiology 98: 609–614, 2003. [DOI] [PubMed] [Google Scholar]
- 10.Tait AR, Voepel-Lewis T, and Malviya S Do they understand? (part I): parental consent for children participating in clinical anesthesia and surgery research. Anesthesiology 98: 603–608, 2003. [DOI] [PubMed] [Google Scholar]
- 11.Lankton J, Batchelder B, and Ominsky A Emotional responses to detailed risk disclosure for anesthesia: A propsective randomized study. Anesthesiology 46: 294–296, 1977. [DOI] [PubMed] [Google Scholar]
- 12.Goldberger JJ, Kruse J, Parker MA, and Kadish AH Effect of informed consent on anxiety in patients undergoing diagnostic electrophysiology studies. Am Heart J 134: 119–126, 1997. [DOI] [PubMed] [Google Scholar]
- 13.Yucel A, Gecici O, Emul M, Oyar O, Gulsoy UK, Dayanir YO, Acar M, Degirmenci B, and Haktanir A Effect of informed consent for intravascular contrast material on the level of anxiety: how much information should be given? Acta Radiol 46: 701–707, 2005. [DOI] [PubMed] [Google Scholar]
- 14.Hyodo I, Eguchi K, Takigawa N, Segawa Y, Hosokawa Y, Kamejima K, and Inoue R Psychological impact of informed consent in hospitalized cancer patients. A sequential study of anxiety and depression using the hospital anxiety and depression scale. Support Care Cancer 7: 396–399, 1999. [DOI] [PubMed] [Google Scholar]
- 15.Meisel A From tragedy to catastrophe: Lawyers and the bureaucratization of informed consent. Yale Journal of Health Policy, Law and Ethics 6: 479–483, 2006. [Google Scholar]
- 16.VHA Handbook 1004.05: IMedConsent(TM). In 2009.
- 17.Fink AS, Prochazka AV, Henderson WG, Bartenfeld D, Nyirenda C, Webb A, Berger DH, Itani K, Whitehill T, Edwards J, Wilson M, Karsonovich C, and Parmelee P Enhancement of surgical informed consent by addition of repeat back: a multicenter, randomized controlled clinical trial. Ann Surg 252: 27–36, 2010. [DOI] [PubMed] [Google Scholar]
- 18.Fink AS, Prochazka AV, Henderson WG, Bartenfeld D, Nyirenda C, Webb A, Berger DH, Itani K, Whitehill T, Edwards J, Wilson M, Karsonovich C, and Parmelee P Predictors of comprehension during surgical informed consent. J Am Coll Surg 210: 919–926, 2010. [DOI] [PubMed] [Google Scholar]
- 19.Anderson LA, and Dedrick RF Development of the Trust in Physician Scale: A measure to assess interpersonal trust in patient-physician relationships. Psychological Reports 67: 1091–1100, 1990. [DOI] [PubMed] [Google Scholar]
- 20.Thom DH, Ribisl KM, Stewart AL, Luke DA, and Physicians STS Further validation and reliability testing of the trust in physician scale. Medical Care 37: 510–517, 1999. [DOI] [PubMed] [Google Scholar]
- 21.Marteau TM, and Bekker H The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventory (STAI). Br J Clin Psychol 31 (Pt 3): 301–306, 1992. [DOI] [PubMed] [Google Scholar]
- 22.Simmons RG, Marine SK, and Simmons RL Gift of Life: The Effect of Organ Transplantation on Individual, Family and Societal Dynamics. Transaction Books, 1987. [Google Scholar]
- 23.Switzer GE Helping unrelated strangers: Physical and psychological reactions to the bone marrow donation process among anonymous donors. Journal of Applied Social Psychology 26: 469–490, 1996. [Google Scholar]
- 24.Switzer GE, Dew MA, Goycoolea JM, Myaskovsky L, Abress L, and Confer DL Attrition of potential bone marrow donors at two key decision points leading to donation. Transplantation 77: 1529–1534, 2004. [DOI] [PubMed] [Google Scholar]
- 25.Switzer GE, Myaskovsky L, Goycoolea JM, Dew MA, Confer DL, and King R Factors associated with ambivalence about bone marrow donation among newly recruited unrelated potential donors. Transplantation 75: 1517–1523, 2003. [DOI] [PubMed] [Google Scholar]
- 26.Cassileth BR, Zupkis RV, Sutton-Smith K, and March V Information and participation preferences among cancer patients. Ann Intern Med 92: 832–836, 1980. [DOI] [PubMed] [Google Scholar]
- 27.Ende J, Kazis L, Ash A, and Moskowitz MA Measuring patients’ desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med 4: 23–30, 1989. [DOI] [PubMed] [Google Scholar]
- 28.Pierce P Michigan assessment of decision style (MADS). Ann Arbor: University of Michigan, 1995. [Google Scholar]
- 29.Pierce PF Deciding on breast cancer treatment: a description of decision behavior. Nurs Res 42: 22–28, 1993. [PubMed] [Google Scholar]
- 30.Arozullah AM, Yarnold PR, Bennett CL, Soltysik RC, Wolf MS, Ferreira RM, Lee SY, Costello S, Shakir A, Denwood C, Bryant FB, and Davis T Development and validation of a short-form, rapid estimate of adult literacy in medicine. Med Care 45: 1026–1033, 2007. [DOI] [PubMed] [Google Scholar]
- 31.Wolf MS, Heckinger EA, Arozullah A, Costello SR, Yarnold PR, Soltysik RC, and Bennett CL Identifying persons with poor health literacy in 7-seconds: An important adjunct to improving cancer screening and treatment. J Clin Oncol (Meeting Abstracts) 22: 6007–, 2004. [Google Scholar]
- 32.Ware J Jr., Kosinski M, and Keller SDA 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34: 220–233, 1996. [DOI] [PubMed] [Google Scholar]
- 33.Schenker Y, Fernandez A, Sudore R, and Schillinger D Interventions to Improve Patient Comprehension in Informed Consent for Medical and Surgical Procedures: A Systematic Review. Med Decis Making. [DOI] [PMC free article] [PubMed]