Abstract
Background
Stent thrombosis (ST) is a rare, but potentially fatal complication. Procedural problems, such as stent under-dimension/under-expansion or dual antiplatelet drug resistance may result into ST. These conditions are more frequent during primary percutaneous coronary intervention for ST-elevation myocardial infarction (STEMI).
Case summary
A 60-year-old male patient presented to our hospital with an inferior STEMI. In the emergency department, a dual antiplatelet therapy was administered with ticagrelor 180 mg and aspirin 250 mg IV. During the observation, the patient experienced a ventricular fibrillation. Urgent coronary angiography showed an occlusion of the proximal right coronary artery. Thrombus aspiration was performed followed by implantation of one drug-eluting stent. After 45 min early ST occurred and was treated by immediate thrombus aspiration and post-dilatation. Intravascular ultrasound sonography (IVUS) showed severe strut malapposition due to a partial crush after post-dilatation. Since it was not possible to directly insert the first guidewire in the stent lumen, the IVUS probe was placed between the vessel wall and the crushed stent to guide the manoeuvre.
Discussion
Crushed stent is a rare complication, being caused by an incorrect passage of the guidewire between the stent’s struts and the vessel wall in case of severe underexpansion. In this case, an IVUS-guided re-entry could be an option to gain the stent true lumen and avoid a second stent implantation.
Keywords: Case report, STEMI, Crushed stent, IVUS
Learning points
Crushed stent is a rare complication, being caused by an incorrect passage of the guidewire between the stent’s struts and the vessel wall due to a severe underexpansion.
Placing an intravascular ultrasound sonography probe in ‘live view’ between the vessel wall and the crushed stent in order to see the initial section of the crashed struts, can help the operator to gain the stent true lumen thus avoiding a second stent implantation.
Introduction
ST-segment elevation myocardial infarction (STEMI) is a medical emergency that requires primary percutaneous coronary intervention (pPCI). In this setting stent thrombosis (ST) is a rare but potentially fatal complication, with a higher occurrence rate compared with PCI in stable coronary artery disease.1 It is mainly due to intraprocedural issues (such as under-dimensioned/under-expanded stenting) or resistance to dual antiplatelet therapy combined with the unfavourable setting of vasospasm and high thrombus burden.2
Timeline
| Admission to Emergency Department | Presented with typical acute chest pain and an electrocardiogram registration with acute inferior ST-elevation myocardial infarction |
| 40 min after admission | Primary percutaneous coronary intervention with implantation of drug-eluting stent in proximal right coronary artery |
| 1.2 h after admission | Recurrent inferior ST-segment elevation |
| 1.5 h after admission | Thrombus aspiration and post-dilatation complicated by stent crushing |
| 2.5 h after admission | Intravascular ultrasound sonography-guided in-stent re-entry and correct post-dilatation |
| 7 days after admission | Patient discharged without complications |
Case presentation
A 60-year-old male with a background of hypertension, smoking, and no known drug allergies, was admitted in our hospital with an inferior STEMI. He remained haemodynamically stable (Killip 1) with normal blood pressure (140/80 mmHg) and heart rate without need of drug support. In the emergency department, heparin 5000 IU, ticagrelor 180 mg, and aspirin 250 mg were administered. While preparing him for urgent coronary angiography (CA), he experienced a ventricular fibrillation immediately treated with direct current (DC)-shock and followed by vomiting. The CA showed an occlusion of proximal right coronary artery which was successfully treated with thrombus aspiration and direct implantation of one drug-eluting stent (Ultimaster, Terumo Corporation) 3.5 × 20 mm (Supplementary material online, Videos S1 and S2). After 45 min, back in the ICU, the patient reported chest pain with evidence of inferior ST-segment elevation. A new CA revealed an early acute intrastent thrombosis (ST, Supplementary material online, Video S3), which was treated by wiring of the artery, thrombus aspiration followed by post-dilatation with 3.75 mm non-compliant (NC) balloon. He was then reloaded with ticagrelor 180 mg and an intracoronary bolus of GP2b3a inhibitors was administered. Intravascular ultrasound sonography (IVUS, OptiCross™ Boston Scientific) was performed, showing severe strut malapposition in the mid-portion of the stent (about 6–14 mm from the proximal edge) due to a partial stent crushing occurred after the post-dilatation with the NC balloon in the second procedure (Supplementary material online, Video S4). Since the first guidewire wire could not gain the true stent lumen, the IVUS probe was placed between the vessel wall and the crushed stent (see Figure 1A). In order to see the initial section of the crushed struts, the ‘live view’ was set. After several IVUS-guided attempts, a Sion Black wire (Asahi Intecc) successfully gained its way through nearly all the stent true lumen (Supplementary material online, Video S5, see Figure 1B). Subsequent post-dilatation with 1.0 balloon up to 4.25 NC balloon permitted a good final angiographic and IVUS result. (The total time from the beginning of the first CA to the end of the second coronary intervention procedure was 2 h and 40 min, see Timeline; see Supplementary material online, Videos S6–S8; Figure 1C.) Four days later the patient was discharged asymptomatic with normal ejection fraction and at 1 year of follow-up he did not experience further events.
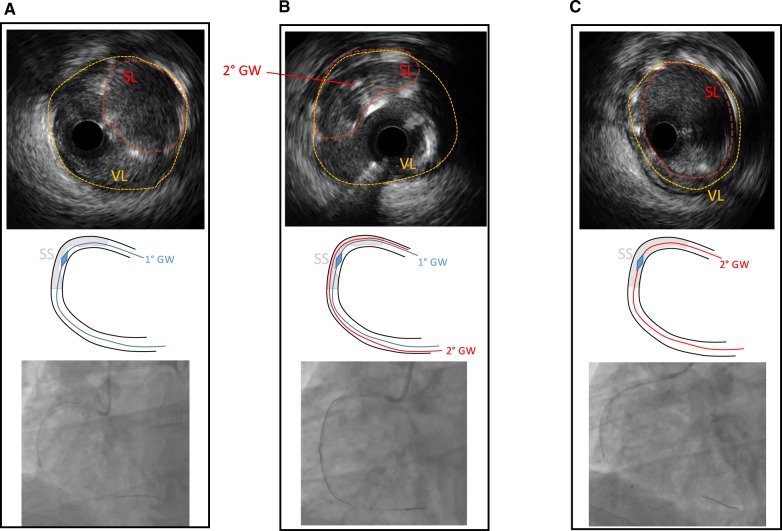
Figure 1.
(A) In the upper part, the intravascular ultrasound sonography image shows clearly the vessel lumen (highlighted in yellow) and the partially crushed stent lumen (highlighted in red) at 3 o’clock while the intravascular ultrasound sonography probe is the black dot in the centre; in the mid-part the cartoon shows the stent struts (in grey) partially crushed in the middle and the intravascular ultrasound sonography probe in blue, while in the bottom part the angiographic view. (B) In the upper part, the intravascular ultrasound sonography view shows the stent partially crushed at 11 o’clock with the second guidewire in the middle, mid-part the cartoon represents the passage of the second guidewire which is shown in angiographic view at the bottom. (C) The final result in the intravascular ultrasound sonography view in the upper part, cartoon in the middle, and angiographic in the bottom are shown with a full stent apposition. GW, guide wire; SL, stent lumen; SS, stent struts; VL, vessel lumen.
Discussion
Stent thrombosis, especially in the early phase post stent implantation, represents an infrequent event. It can be triggered by early antiplatelet therapy discontinuation, extensive atherosclerotic burden, and high stent number/length. To a lesser extent, diabetes, smoking status, and bifurcation/ostial disease could also provoke ST.2 ST-elevation myocardial infarction presentation is known to be one of the most powerful predictors of ST, due to the thrombotic burden, which can enhance inflammatory response if stent malapposition comes with subsequent thrombosis.3 In the Swedish Coronary Angiography and Angioplasty Registry, for example, the risk of ST in STEMI patients was increased 2.5 times compared to patients without.4
In this specific case, the incorrect sizing of the stent based on equivocal angiographical picture due to vasospasm and hyper-adrenergic condition5 was probably the initial stimulus of ST. Moreover, because of the vomit, the first ticagrelor loading dose was probably worthless, and together these two variables may have contributed to ST. Furthermore, because of this severe stent malapposition, the guidewire in the second procedure passed between the stent struts and the vessel wall before entering the stent in its middle portion, thus leading to its partial crush during the subsequent post-dilatation (as shown in Figure 1A the stent is compressed at 3 o’clock).
In these cases, IVUS-guided re-entry could be an option because the guidewire (ideally hydrophilic) can be seen ‘in live view’ along its course and the passage in the stent lumen can be detected quite easily; Moreover, the IVUS probe actually fills the space in between the stent and the vessel wall, thus facilitating the correct passage of the wire. In our patient, this technique avoided the implantation of a second ‘stent in stent’ thus reducing the future risk of restenosis and thrombosis. The main limitation of this technique lies in the deliverability of the IVUS probe, a problem that could be partially be overcome using specific devices (such as Eagle Eye Short Tip, Philips Volcano). However, in this particular case, this trouble was avoided because the ‘partial crush’ of the stent with a 3.75 mm balloon created enough space to easily deliver the probe.
Despite the high procedural volume of our centre [with more than 1000 PCI/year (250 primary PCI] with an IVUS rate use of about 15% and 90 chronic total occlusion (CTO) PCI/year both antegrade or retrograde), this was the first with such a complication, stressing the added value in interventional cardiology practice of a deep knowledge of CTO techniques even in non-CTO setting.
Conclusion
Stent thrombosis following STEMI PCI is an important issue due a multifactorial aetiology. Crushed stent is a rare complication in this setting, in some cases IVUS-guided re-entry could be an option to solve the situation avoiding a second stent implantation.
Lead author biography

Dr Mario Iannaccone acquired his medical degree at ‘Second University of Neaples’, and Specialization in Cardiology at the University of Turin. He had some period of fellowship in Strasburg and in Stockholm at Karolinska Institute. Actually, he is an interventional cardiology working in Turin (Italy) in San Giovanni Bosco hospital (head of the Cath Lab Dr. Roberto Garbo), principal field of interest is percutaneous coronary intervention, IVUS, rotational atherectomy, and CTO PCI.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Supplementary Material
References
- 1.Iannaccone M, Vadalà P, D'ascenzo F, Montefusco A, Moretti C, D'amico M, Gaita F. Clinical perspective of optical coherence tomography and intravascular ultrasound in STEMI patients. J Thorac Dis 2016;8:754–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. D'Ascenzo FBollati M, Clementi F, Castagno D, Lagerqvist B, de la Torre Hernandez JM, ten Berg JM, Brodie BR, Urban P, Jensen LO, Sardi G, Waksman R, Lasala JM, Schulz S, Stone GW, Airoldi F, Colombo A, Lemesle G, Applegate RJ, Buonamici P, Kirtane AJ, Undas A, Sheiban I, Gaita F, Sangiorgi G, Modena MG, Frati G, Biondi-Zoccai G.. Incidence and predictors of coronary stent thrombosis: evidence from an international collaborative meta-analysis including 30 studies, 221,066 patients, and 4276 thromboses. Int J Cardiol 2013;167:575–584. [DOI] [PubMed] [Google Scholar]
- 3.Brugaletta S, Sabate M, Martin-Yuste V, Masotti M, Shiratori Y, Alvarez-Contreras L, Cequier A, Iñiguez A, Serra A, Hernandez-Antolin R, Mainar V, Valgimigli M, Tespili M, den Heijer P, Bethencourt A, Vazquez N, Gomez-Lara J, Backx B, Serruys PW. Predictors and clinical implications of stent thrombosis in patients with ST-segment elevation myocardial infarction: Insights from the EXAMINATION trial. Int J Cardiol 2013;168:2632–2636. [DOI] [PubMed] [Google Scholar]
- 4. Lagerqvist B, Carlsson JRG, Fröbert O, Lindbäck J, Scherstén F, Stenestrand U, James SK; Swedish Coronary Angiography and Angioplasty Registry Study Group. Stent thrombosis in Sweden: a report from the Swedish Coronary Angiography and Angioplasty Registry. Circ Cardiovasc Interv 2009;2:401–408. [DOI] [PubMed] [Google Scholar]
- 5. Taniwaki M, Stefanini G, Räber L, Brugaletta S, Cequier A, Heg D, Iñiguez A, Kelbæk H, Serra A, Ostoijic M, Hernandez-Antolin R, Baumbach A, Blöchlinger S, Jüni P, Mainar V, Sabate M, Windecker S. Predictors of adverse events among patients undergoing primary percutaneous coronary intervention: insights from a pooled analysis of the COMFORTABLE AMI and EXAMINATION trials. EuroIntervention 2015;11:391–398. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.