Abstract
The emergence of multidrug-resistant (MDR) strains is a major health problem worldwide. There is an urgent need for novel strategies to combat bacterial infections caused by MDR strains like Pseudomonas aeruginosa and Acinetobacter baumannii. Quorum sensing (QS) is a critical communication system in bacterial community controlling survival and virulence. The awareness of the importance of QS in bacterial infections has stimulated research to identify QS inhibitors (QSIs) to defeat microbes. In this study, four FDA-approved drugs (besides azithromycin as positive QSI) were tested for potential QS inhibition against clinical A. baumannii isolates and P. aeruginosa (PAO1) standard strain. The inhibitory effect of these drugs on virulence factors of both microbes has been investigated. The studied virulence factors include biofilm formation, twitching and swarming motilities, proteolytic enzyme production, and resistance to oxidative stress. The four tested drugs (erythromycin, levamisole, chloroquine, and propranolol) inhibited QS in Chromobacterium violaceum by 84, 72, 55.1, and 37.3%, respectively. They also significantly inhibited virulence factors in both PAO1 and A. baumannii at sub-inhibitory concentrations. These findings were confirmed by qRT-PCR and mice mortality test, where tested drugs highly repressed the expression of abaI gene and showed significantly improved mice survival rates. In addition, molecular docking studies against AbaI and AbaR proteins of QS system in A. baumannii revealed the potential inhibition of QS by tested drugs. Beside their known activities, the tested drugs could be given new life as QSIs to combat A. baumannii nosocomial infections (alone or in combination with antimicrobials).
Electronic supplementary material
The online version of this article (10.1007/s10096-020-03882-z) contains supplementary material, which is available to authorized users.
Keywords: Acinetobacter baumannii, Quorum sensing, Chloroquine, Erythromycin, Levamisole, Propranolol
Introduction
Acinetobacter baumannii and Pseudomonas aeruginosa are two of the main superbug bacteria responsible for nosocomial infections in severely ill patients. They cause a wide spectrum of infections from skin and wound infections to septicemia and hospital outbreaks worldwide; both organisms are resistant to several classes of antibiotics making their treatment very difficult [1]. The MDR pattern can be transferred to the other organisms that initially do not show such resistance [2]. In addition, biofilm production in A. baumannii and P. aeruginosa encourages increased colonization and persistence in hospital environments leading to higher rates of device-related infections [3]. To solve the problem of limited therapeutic options, it is very vital to find new therapeutic strategy to combat A. baumannii infections.
It is well known now that quorum sensing (QS), a cell-to-cell communication system, regulates the expression of several virulence and survival genes in many organisms at high cell densities using N-acyl-homoserine lactone (AHL) signaling molecules; thus, QS plays key role in the establishment of microbial infections [4]. Therefore, interfering with QS is considered as a promising strategy to combat bacterial infections by inhibiting bacterial virulence hence affecting the ability of pathogens to cause diseases rather than affecting their growth which does not impose a selection pressure and helps to avoid emergence of resistance [5]. Consequently, QSI would increase the susceptibility of the pathogen to host defense and clearance by the host immune system [6].
A. baumannii has one chromosomally encoded AHL-dependent signaling system, comprising of LuxI and LuxR homologs. abaI gene is responsible for the synthesis of 3-hydroxy-dodecanoyl-(L) homoserine lactone (3-OH-C12 HSL), and the cognate receptor of this ligand is synthesized by abaR [7].
P. aeruginosa has at least three QS systems; QS inhibition in P. aeruginosa has been reported using either natural or synthetic compounds. Any QSI used in P. aeruginosa would be efficient in inhibiting QS in other pathogens [8]. Many compounds that function as QSIs can successfully inhibit P. aeruginosa and A. baumannii pathogenesis, but some of them have toxicity in human-like halogenated furanone compounds [9, 10]. Thus, it is more reliable to screen the approved drugs used for human therapy which already found in the market and have a known safety profile. The idea of repurposing of old drug is an attractive idea that has been applied for many drugs [11].
Several studies have illustrated the QS inhibitory activity of antibiotics in P. aeruginosa including ceftazidime, ciprofloxacin, and azithromycin [12, 13]. Moreover, streptomycin was found to inhibit QS in A. baumannii [14]. The macrolide antibiotic, erythromycin, is a hydrophobic and large-sized molecule and active against Gram-positive bacteria, but has much narrower spectrum against Gram-negative bacteria as it is believed to be ineffective against Enterobacteriaceae. While azithromycin, another macrolide, exerts greater antimicrobial activity than erythromycin [15].
Propranolol was reported to inhibit morphogenesis and germ tube formation in Candida albicans which are essential for its virulence [16]. Also, it was found that lesions of EHEC were not formed on epithelial cells in the presence of propranolol, which suggests that QS can specifically inhibit using β-adrenergic receptor antagonists [17].
Chloroquine (CQ) is known for its antimalarial activity. Chloroquine derivatives were found to exhibit QS inhibition in Serratia marcescens and Pseudomonas aeruginosa [18]. Recently, CQ showed antiviral activity against coronavirus causing COVID 19 disease [19].
The anthelmintic drug niclosamide inhibited Pseudomonas aeruginosa QS and virulence [9]. Levamisole is another anthelmintic drug that was found to be successful in treating chronic mucocutaneous candidiasis in combination with oral antifungals [20].
This study aimed to investigate the potential role of a number of FDA-approved drugs with different pharmacological activities including (erythromycin (antibiotic), chloroquine (antimalarial), levamisole (antiparasitic), and propranolol (adrenergic blocker), in interfering with QS and virulence in both PAO1 standard strain and MDR A. baumannii clinical isolates. In addition, the QS inhibitory activity was evaluated in vivo by a mouse model of peritoneal sepsis, and evaluated at the molecular level by qRT-PCR. Moreover, docking analysis was also performed against the two proteins of QS system found in A. baumannii, AbaI, and AbaR.
Materials and methods
Bacterial strains and drugs
Twenty QS-positive clinical A. baumannii isolates were selected for this study. They were obtained from different intensive care units (ICUs) of Zagazig University Hospitals, and the International Medical Center, Egypt. All strains have been identified and confirmed to be QS-positive MDR A. baumannii. The isolates were of 3 clinical sources, 14 from tracheal aspirate, 3 from blood, and 3 from wound (supplementary Table 1). They were maintained routinely on Luria-Bertani (LB) agar. Two reference strains were used in this study: Pseudomonas aeruginosa O1 (PAO1) as a QS-positive strain and Chromobacterium violaceum 026 (CV026), a biosensor for QS which is violacein-negative strain, and its violacein purple pigment is induced by AHLs (acyl-homoserine lactones).
Chloroquine (CQ), erythromycin (E), levamisole (LEV), and propranolol (PPL) were obtained from the National Organization of Drug Control and Research (NODCAR) Cairo, Egypt. The antibiotic azithromycin (AZ) was used as QSI-positive control in all experiments. All drugs were dissolved in water except erythromycin and azithromycin which were dissolved in dimethylsulfoxide (DMSO).
Screening some drugs for the quorum sensing inhibitory activity
Overnight-grown C. violaceum CV026 cells (15 mL) were added into 200 mL of 1.5% molten LB agar (Oxoid, Hampshire, England) that has been supplemented with N-hexanoyl homoserine lactone (C6-HSL, 0.25 μg/mL) purchased from Sigma-Aldrich Chemie GmbH (Steinheim, Germany). CV026 agar suspension was poured into Petri dishes and allowed to solidify; wells were made using sterile pipette tips. The tested drug solutions (30 μL of 32 mg/mL) were placed in each well and the solvent served as negative control. The plates were incubated at 28 °C for 24 h. Halo formation on a purple background suggested that the tested drugs exhibited anti-QS activity [21].
Quantification of the inhibition of violacein pigment production
First, minimum inhibitory concentration (MIC) of the potential QSIs was determined by broth microdilution according to CLSI methodology [22]. Briefly, four morphologically similar colonies from CV026 were touched with a sterile loop and transferred to Müller Hinton broth (MHB), Oxoid (Hampshire, England), and broth was incubated with shaking at 28–30 °C until the visible turbidity was equivalent to 0.5 McFarland. The bacterial suspension was diluted 1:100 in MHB, so the final concentration of bacteria will be approximated 5 × 105 CFU/mL. Twofold serial dilutions of each drug were prepared directly in 96-well microtiter plates (double strength of the required concentrations) in a final volume of 50 μL per well. One well was left without drug to serve as a positive growth control. Each well was inoculated with 50 μL of inoculum and incubated at 30 °C for 18 to 20 h. The microtiter plates were examined for growth; MIC was considered as the lowest concentration of QSI at which there was no visible growth of the organism.
The inhibition of violacein pigment production using sub-MIC of tested drugs was quantified spectrophotometrically [23]. Briefly, 10 mL of LB broth supplemented with C6-HSL (0.25 μg/mL) either in the absence or presence of and ¼ MIC of the 4 drugs were inoculated with 200 mL of overnight culture of CV026 (diluted to 106 CFU/mL) and incubated at 30 °C for 24 h. One milliliter of culture from each sample was centrifuged at 13,000 rpm for 10 min. Then, culture supernatant was discarded, and the pellet was solubilized in 1 mL of DMSO, vortexed until the violacein was extracted, and centrifuged at 13,000 rpm for 10 min. Optical density (OD) of each violacein-containing supernatant was measured at 585 nm using micro-titer plate reader (Biotek Spectrofluorimeter, Biotek, USA); results were expressed as percentage of violacein production inhibition with respect to negative controls. The control sample was CV026 inoculated in LB medium containing C6-HSL without QSIs.
Measurement of P. aeruginosa and A. baumannii virulence factors in presence of MIC of QSIs
The MICs of four QSIs (erythromycin, chloroquine, levamisole, propranolol) against PAO1 and clinical QS positive A. baumannii isolates were first determined by broth micro-dilution method in addition to azithromycin as positive QSI control. The virulence factors were detected in absence and presence of MIC of potential QSIs. Assay of biofilm formation, twitching motility, sensitivity to oxidative stress and protease, and gelatinase activity were performed for both P. aeruginosa (PAO1) and A. baumannii isolates. Pyocyanin production, swarming motility, and rhamnolipid production were done only for P. aeruginosa, while surface-associated motility, esterase, and phospholipase C production were performed only for A. baumannii clinical isolates.
Quantification of biofilm formation
The modified method of Stepanovic et al. [24] was used to test biofilm formation. Overnight culture of PAO1 and A. baumannii either with and without MIC of QSIs were prepared, diluted with MHB, and adjusted to a cell density of 1 × 106 CFU/mL. Aliquots of 100 μL of adjusted bacterial suspension were inoculated to the wells of sterile 96-well polystyrene micro-titer plates. After incubation for 24 h at 37 °C, the contents of the wells were gently aspirated, and the wells were washed three times with sterile phosphate buffered saline (PBS, pH 7.2). The adherent cells were fixed with 100 μL of 99% methanol for 20 min and then stained with 100 μL crystal violet (1%) for 20 min. The excess dye was then removed under running distilled water, and then the plates were left to air-dry. The bound dye was extracted by the addition of 80 μL of 33% glacial acetic acid, and the optical densities were read at 600 nm using micro-titer plate reader. The experiment was performed in triplicate, and the mean optical densities were calculated, wells using media only was used as negative control. The cut-off OD (ODc) was defined as three times standard deviations above the mean OD of the negative control. According to the criteria of Stepanovic et al. [24], the test isolates were categorized into four groups: non-biofilm forming (OD ≤ ODc), weak biofilm forming (OD > ODc, but ≤ 2× ODc), moderate biofilm forming (OD > 2× ODc, but ≤ 4× ODc), and strong biofilm forming (OD > 4× ODc).
Twitching motility assay
Semisolid LB media (LB broth with 1% agar) either with or without QSIs were used for the motility assay [25]. Plates were made by pouring 15 mL medium into a 90-mm petri dish, and allowing the medium to air-dry with the lid off for 20 min in a laminar flow hood, plates were prepared on the same day as the inoculation. A 2 μL of freshly grown cultures, adjusted to 0.5 McFarland, were stab-inoculated into semisolid agar to enable spread of bacteria on the interphase between the bottom of the Petri dish and the LB medium. After inoculation, plates were sealed with parafilm and incubated at 37 °C for 48 h. To visualize the bacteria at the interface, agar was removed from each plate, and the plates were air-dried and stained with 1% CV. For each isolate, assays were performed at least three times. Results interpreted according to the criteria of Vijayakumar et al. [26]. The average diameter of zone of twitching was determined; isolates are classified as non-motile (NM, < 5 mm), intermediately motile (IM, 5–20 mm), and highly motile (HM, > 20 mm).
Protease activity
First, sterile supernatant was prepared according to Gupta et al. [27]. Briefly, 0.5 mL of 0.5 MacFarland overnight cultures was inoculated in 5-mL LB broth with and without 1/8 MIC of QSIs and incubated at 37 °C for 18 h. The supernatants were separated by centrifugation at 8500g for 15 min and were filtered using 0.45-μm syringe filter. This sterile supernatant was used in testing protease, gelatinase, and rhamnolipid production.
Protease activity was tested using skimmed milk agar media [28]. The media consists of 5% skimmed milk in 1.5% LB agar. Skimmed milk agar plates were prepared, and 100 μL of sterile supernatants were added to the wells made in the plates using a sterile pipette tip. The plates were incubated overnight at 37 °C for 24 h, and the clear zones surrounding the wells were measured which indicates positive proteolytic activity in presence and absence of QSIs. The experiment was performed in triplicate.
Gelatinase activity
The method of Su et al. [29] was used to detect gelatinase production. Briefly, 1.5% LB agar supplemented with 3% gelatin with a final pH 7.2 was prepared, and isolate culture was spot inoculated on the surface of the plates and incubated for 24 h at 37 °C. The plates were observed for growth and subsequently flooded with 10 mL of Frazier’s solution (15.0 g mercuric chloride, 20 ml hydrochloric acid (37% v/v), and distilled water to 100 mL) to precipitate the unhydrolyzed gelatin. The plates which showed area of opaque layer with zone of clearance (transparent halo) around the colonies were taken as positive for gelatin hydrolysis. The experiment was performed in triplicate. AZ was used as control QSI. The results were recorded as Gz values by calculating the ratio between the colony diameter and the gelatin hydrolysis zone diameter, and the isolates were classified according to the method of Sanchez et al. [30], where Gz of 1.0 was evaluated as negative (−), 0.99–0.7 as low (+), 0.5–0.69 as moderate activity (++), and < 0.5 as high (++++) activity.
Sensitivity to oxidative stress (sensitivity to H2O2)
Sensitivity to oxidative stress was carried out by the modified disk assay [31]. Briefly, 100-μL aliquots from LB broth cultures in mid-log or stationary phases of growth were uniformly spread on the surface of MHA plates containing 2% agar with and without sub-MIC of QSIs. Sterile 6-mm diameter filter paper disks were placed on the surface, and the disks were spotted with 10 μL of 1.5% H2O2. The diameter of the zone of growth inhibition around each disk was measured after 24 h of incubation at 37 °C. The experiment was performed in triplicate. The increase in the diameter of the inhibition zone indicates the ability of potential QSIs to inhibit resistance or tolerance to oxidative stress (i.e., augment susceptibility to oxidative stress).
Pyocyanin production assay
Pyocyanin production by untreated and QSI-treated PAO1 was assayed as described previously [32]. PAO1 overnight culture in LB broth was prepared and diluted to OD600 of 0.4. Luria-Bertani broth (1 mL) with and without QSIs was inoculated with 10 μL of diluted culture suspension, and the cultures were incubated at 37 °C for 48 h. To remove the cells and obtain the supernatants, the tubes were centrifuged at 10,000 rpm for 10 min, and the pyocyanin was quantified in the supernatants by measuring the absorbance at 691 nm by Biotek spectrofluorimeter (Biotek, USA). The experiment was performed in triplicate.
Swarming motility
Swarming motility was detected according to Rashid and Kornberg [33]. LB medium used for assay and contained 0.5% agar, tryptone 10 g/L, NaCl 1.25 g/L, and yeast extract 5 g/L with or without potential QSIs. Swarm plates were typically allowed to dry at room temperature before being used. The swarm LB agar plates were spot inoculated by 2 μL of 0.5 McFarland solution of PAO1 overnight culture, and incubated for 24 h at 37 °C. This assay was performed three times, and the average of the diameter of swarm colony was recorded in mm.
Rhamnolipid production
The oil spreading technique was carried out as described by Youssef et al. [34]. Briefly, 20-mL distilled water was added to 90-mm Petri dish followed by addition of 10-μL crude oil to the surface of water. Then, 10-μL PAO1 supernatant with and without sub-MIC of QSIs was dropped onto the crude oil surface. The diameter of the clear zone on the oil surface was measured. The experiment was performed in triplicate, and the average was calculated.
Surface-associated motility
Surface motility plates were prepared according to Vijayakumar et al. [26] with modification (tryptone 10 g/L, NaCL 1.25 g/L, yeast extract 5 g/L, 0.05% triphenyl tetrazolium chloride (TTC), 0.4% agar). In order to reduce variation between plates, plates were prepared on the same day, by pouring 15 ml of surface motility medium in each plate in a laminar flow hood with the lids off and allowing it to dry for 30 min and then quickly used for motility assays. Two microliters of a bacterial suspension normalized to 0.5 McFarland standard were surface inoculated. After inoculation, the plates were sealed with parafilm and incubated for 48 h at 37 °C. Surface-associated motility assays were conducted on at least three separate occasions. Swarming positive isolates were defined as those strains that showed a zone of > 10 mm around the site of inoculation.
Esterase production (Tween 80 opacity test)
The esterase production assay was performed according to Slifkin [35]. Two microliters of overnight cultures of A. baumannii isolates grown on LB broth and adjusted to 0.5 McFarland turbidity were transferred to Tween 80 medium (containing 0.5% Tween 80) with or without sub-MIC of QSIs. The inoculated agar plates were incubated at 37 °C for 3 days. The tests were performed in triplicate. The presence of an opaque halo around an inoculated site on the medium, viewed with transmitted light, indicated a positive result. Esterase activity (Ez) was calculated as the ratio of the diameter of the colony to the diameter of the colony plus that of the opaque zone, which correlates with hydrolysis of Tween 80. The isolates were classified according to the method of Sanchez et al. [30], where Ez of 1.0 was evaluated as negative (−), 0.99–0.7 as low (+), 0.5 to 0.69 as moderate activity (++), and < 0.5 as high (++++) activity.
Phospholipase C production
Phospholipase C (lecithinase) activity was done by inoculating 2 μL of overnight cultures (on LB) equivalent to 0.5 McFarland turbidity of each isolate into egg yolk agar (1.5% LB agar containing 0.5% egg yolk and 0.11% calcium chloride) with or without sub-MIC of QSIs [36]. Inoculated plates were incubated at 37 °C for 48 h. The experiment was performed in triplicate. Phospholipase C positive colonies were clearly marked by dense white zone of precipitation extending from the edge of the colony. Colony diameter and colony diameter plus precipitation zone were measured for each isolate, and the zone of phospholipase activity (Pz value) was calculated. Pz value was calculated as the ratio of the diameter of the colony to the diameter of the colony plus that of the precipitation zone. The isolates were classified according to the method of Sanchez et al. [30], where a Pz of 1.0 was evaluated as negative (−), 0.99–0.7 as low (+), 0.5 to 0.69 as moderate activity (++), and < 0.5 as high (++++) activity.
RNA isolation and quantitative real-time PCR for autoinducer synthase gene in A. baumannii
Real-time PCR was performed in absence of the potential QSIs on the 20 QS positive isolates while qRT-PCR was performed in presence of 1/8 MICs of 4 potential QSIs for A. baumannii isolate number 1 (AB1). AZ was used as control. Total RNA was extracted using GeneJET RNA extraction Kit (Thermo Fisher Scientific Inc., Germany) according to the manufacturer’s instructions. Briefly, 5-mL LB broth of A. baumannii isolates was inoculated with 0.5-mL culture equivalent to 0.5 Macfarland and incubated at 37° for 18 h. cDNA was generated by reverse transcription of 2 μg of total RNA using oligo dT primers and 0.2 μL reverse transcriptase in a total reaction volume of 20 μL. Primers for abaI (abaIF 5′CCGCCTTCCTCTAGCAGTCA3′ abaIR 5′AAAACCCGCAGCACGTAATAA 3′) and 16SrRNA (forward 5′ ACTCCTACGGGAGGCAGCAGT 3′ and reverse 5′ TATTACCG CGGCTGCTGGC 3′) were adapted from Selasi et al. [37] and Clifford et al. [38], respectively.
The RT-PCR master mix was prepared in 20-μL final volume comprised of the following: 10 μL of 2× SensiFAST™ SYBR (Bioline, London, UK), 0.8 μL of each primer (10 μM), 0.2 μL reverse transcriptase, 0.4 μL RiboSafeRNase Inhibitor, water up to 16 μL, and 4 μL of RNA template. The reaction mix was applied in RT-PCR (StepOne Applied Biosystem, Foster City, USA). Three-step cycling was used as follows: 1 cycle reverse transcription at 45 °C for 10 min, then PCR consists of initial activation cycle of 95 °C at 2 min followed by 40 cycles of 95 °C for 15 s, 55 °C for 30s, and 72 °C for 1 min. Fold changes in gene expression were calculated using the comparative Ct method (2−ΔΔCT), and samples were normalized to 16S rRNA expression [39].
Mice mortality test using a peritoneal sepsis model
A murine model of peritoneal sepsis by A. baumannii was established by intra-peritoneal inoculation of bacteria in mice [40]. An overnight culture of A. baumannii AB1 was inoculated in LB medium with and without the 4 QSIs (at 1/8-MIC concentration) at 37 °C for 18 h. Ten milliliters of the culture (adjusted to 0.5 McFarland) was harvested by centrifugation at 12,000 g at 4 °C for 10 min. The pellet was resuspended in 1.25 mL PBS by vortexing. A 250 μL of the suspended cells, equivalent to 2 × 108 cells, was injected into the abdominal cavity of four to 5-week-old-specific pathogen-free Swiss albino (15–23 g weight) female mice. Mortality was observed during 3 days period for 5 mice for each treatment. DMSO, DMF, and PBS were injected into mice as negative control groups (n = 5/group). Experimental design and animal handling procedures were performed according to the guidelines for animal use of the Ethical Committee of the Faculty of Pharmacy, Zagazig University.
Molecular docking analysis
The structure of autoinducer synthase AbaI protein model (Code: B0FLN1) was retrieved from Swiss-model (B0FLN1 (ABAI_ACIBA) Acinetobacter baumannii, Acyl-homoserine-lactone synthase. https://swissmodel.expasy.org/repository/uniprot/B0FLN1).
The active site was identified through protein structure alignment tool in the Molegro Virtual Docker (MVD Version 6.0) with the template structure (PDB Code: 3P2H) [41], and the ligand S-adenosyl methionine (SAM) was transferred to the model active site. This study was carried out on erythromycin, propranolol, chloroquine, and levamisole along with SAM. The studied compounds were drawn into Marvin Sketch (V5.11.5). The most energetically favored conformer was saved as (*.mol2) file format for docking. The optimal geometry of the ligand was determined during the docking process. MolDock optimizer algorithm in Molegro Virtual Docker software (MVD) was chosen to perform docking process with 10 runs per ligand, 200 population size, 4000 max iteration, and 5 poses for each ligand. MolDock docking engine using the optimized ligands was executed [42]. Finally, the top-returned poses were chosen for analysis.
The structure of AbaR receptor model (Code: A0A2C9TFV2) was retrieved from swiss-model (A0A2C9TFV2 (A0A2C9TFV2_ACIBA) Acinetobacter baumannii, https://swissmodel.expasy.org/repository/uniprot/A0A2C9TFV2). The docking study was carried out on erythromycin, propranolol, chloroquine, and levamisole along with natural ligand N-(3-Hydroxydodecanoyl)-L-homoserine lactone OH-DHL) with the same docking procedure as previously mentioned.
Results
Screening some drugs for quorum sensing inhibitory activity
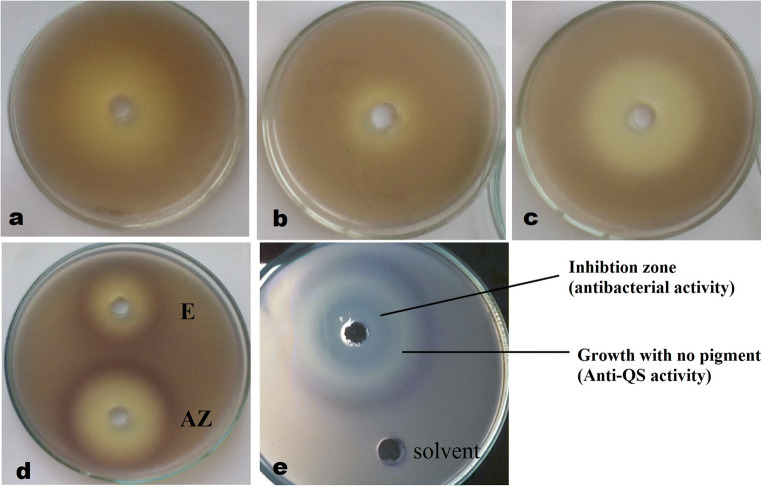
In presence of C6-HSL (cognate signal), CV026 produces violacein purple pigment, which inhibited in presence of QSI that can affect the signal production or signal reception. Among the tested drugs, erythromycin, levamisole, propranolol, and chloroquine showed the highest inhibition of quorum sensing in CV026 as they produced a large clear zone around each well on a purple background (Fig. 1); hence, these four drugs were tested in the further experiments. Azithromycin was used as a positive QSI. It was noticed that drugs had antibacterial activity that appeared as growth inhibition zone beside the anti-QS activity. Erythromycin and azithromycin also produce darker ring of purple color after the anti-QS zone.
Fig. 1.
Screening some drugs for QS inhibition in CV026. Positive QS inhibition by chloroquine (a), levamisole (b), propranolol (c), erythromycin, and azithromycin (d, e) is antibacterial and anti-QS activity of QSIs. There is a zone of growth inhibition due to antibacterial activity then a halo zone of growth with no purple color due to the QS inhibition
Quantification of the inhibition of violacein pigment production
The MICs of the four QSIs and azithromycin against CV026 were determined by broth microdilution method. The MICs were 0.5, 256, 128, 2048, and 10,000 μg/mL for azithromycin, erythromycin, propranolol, levamisole, and chloroquine, respectively.
The inhibition of violacein pigment production in CV026 in presence of (1/4, 1/8 MIC of QSIs) was quantified spectrophotometrically. OD values at 585 nm were used to calculate the percentage of inhibition of pigment production (Table 1). The results revealed that all tested drugs had high percentage of QSI; the most effective drug was erythromycin (84% at 1/4 MIC, 80.9% at 1/8 MIC) followed by azithromycin, levamisole, chloroquine, and propranolol.
Table 1.
Percentage inhibition of violacein pigment production by CV026 in presence of QSIs
| QSI | % inhibition at 1/4 MIC | % inhibition at 1/8 MIC |
|---|---|---|
| Azithromycin | 75.6 | 72.8 |
| Erythromycin | 84 | 80.9 |
| Chloroquine | 55.1 | 48.5 |
| Levamisole | 72 | 68.1 |
| Propranolol | 37.3 | 38.5 |
Measurement of P. aeruginosa virulence factors in presence of QSIs
All tested drugs inhibited PAO1 growth at different values, 0.5 μg/ml for azithromycin, 128 μg/mL for propranolol, 256 μg/mL for erythromycin, 512 μg/mL for levamisole, and 7.5 mg/mL for chloroquine. To evaluate the anti-QS and anti-virulence activity of tested drugs, 1/8 MIC of each drug was used.
Inhibition of biofilm formation in PAO1
The obtained results revealed that PAO1 biofilm (strong) was markedly inhibited in presence of 1/8 MIC of tested drugs (> 68%); the highest inhibition was observed with erythromycin (82.7%) as shown in Table 2 and Fig. 2a.
Table 2.
Percentage inhibition of virulence factors of PAO1 in presence of QSIs
| Percentage inhibition of | ||||||||
|---|---|---|---|---|---|---|---|---|
| QSI | Biofilm | Twitching motility | Swarming motility | Protease | Gelatinase | Pyocyanin production | Resistance to H2O2 | Rhamnolipid production |
| Azithromycin | 76.5 | 41.5 | 67.1 | 30.4 | 50.7 | 49.8 | 16.7 | 66.7 |
| Erythromycin | 82.7 | 53.8 | 84.3 | 39.1 | 54.8 | 53.9 | 36.7 | 66.7 |
| Levamisole | 74.6 | 32.3 | 67.1 | 13 | 43.1 | 41.4 | 16.7 | 53.3 |
| Chloroquine | 68.8 | 32.3 | 64.3 | 13 | 25 | 16 | 13.3 | 33.3 |
| Propranolol | 73 | 12.3 | 80 | 30.4 | 53.5 | 34.8 | 13.3 | 60 |
Fig. 2.
Measurement of PAO1 virulence factors in presence of 1/8 MIC of QSIs. a Biofilm. b Twitching motility. c Swarming motility. d Protease production. e Gelatinase production. f Resistance to H2O2. g Pyocyanin production. h Rhamnolipid production. AZ, azithromycin; E, erythromycin; LEV, levamisole; CQ, chloroquine; PPL, propranolol. Control is PAO1 without QSIs
Inhibition of PAO1 motilities
The effect of the tested drugs on twitching and swarming of PAO1 was determined. Swarming motility was more inhibited than twitching; the highest inhibition of twitching and swarming motility was reported in presence of erythromycin (53.8% and 84.3%, respectively), and the lowest inhibition in both motilities was observed with propranolol (Table 2 and Fig. 2b, c).
Inhibition of protease and gelatinase production in PAO1
PAO1 was found to be strong gelatinase producer as Gz value was 0.33. Gelatinase production was highly inhibited in presence of erythromycin and chloroquine (54.8% and 53.5%, respectively), while protease activity was moderately inhibited in presence of QSIs. The lowest inhibition in protease activity was recorded in presence of levamisole and propranolol (Table 2 and Fig. 2d, e).
H2O2 oxidative stress response in PAO1
The effect of H2O2 was highly augmented in presence of erythromycin as tolerance to oxidative stress was reduced by 36.7% (Table 2 and Fig. 2f); lower augmentation was observed with azithromycin and levamisole (16.7% for both) and propranolol and chloroquine (13.3% for both).
Inhibition of pyocyanin production in PAO1
The pyocyanin production was significantly inhibited in presence of erythromycin, azithromycin, levamisole, and chloroquine with percentages of 53.9, 49.8, 41.4, and 34.8%, respectively. Lower inhibition (16%) was observed with propranolol (Table 2 and Fig. 2g).
Inhibition of rhamnolipid production
The rhamnolipid production was highly inhibited in presence of all QSIs (Table 2 and Fig. 2h) as spreading of oil on water surface was decreased. Azithromycin and erythromycin showed very significant inhibition (66.7%) followed by chloroquine (60%) and levamisole (53.3%), while propranolol showed the lowest inhibition (33.3%).
Assay of A. baumannii virulence factors in presence of 1/8 MIC of QSIs
The MICs of QSIs against QS-positive MDR A. baumannii isolates were determined by broth micro-dilution method (supplementary Table 2). MIC50 was calculated; azithromycin had the lowest MIC (4 μg/mL) while chloroquine had the highest (1875 μg/mL). To evaluate the anti-QS and anti-virulence activity of tested drugs, 1/8 MIC of each drug was used (see supplementary Tables S3–S8 for detailed results of virulence inhibition and supplementary Fig. S1 for representative examples of virulence inhibition in A. baumannii).
Inhibition of biofilm formation in A. baumannii
Quantification of biofilm in presence of 1/8 MIC of QSIs was performed. More than 50% inhibition of biofilm formation appeared in 15 of 20 A. baumannii isolates with all tested drugs (Table 3 and Fig. 3). Chloroquine showed the highest range of percentage inhibition of biofilm (67.4–93.5%).
Table 3.
Percentage inhibition of virulence factors of A. baumannii isolates in presence of QSIs
| Virulence factor | Azithromycin | Erythromycin | Levamisole | Chloroquine | Propranolol | |
|---|---|---|---|---|---|---|
| Biofilm | % inhibition range | 33.6–93.3 | 20.2–93.3 | 33.8–92.9 | 67.4–93.5 | 37.8–92.9 |
| % of isolates with ≥ 50% inhibition | 80% | 95% | 85% | 100% | 75% | |
| Twitching motility | % inhibition range | 7.7–75 | 19.3–81.8 | 11.7–89.5 | 8.3–77.3 | 16.7–80 |
| % of isolates with ≥ 50% inhibition | 30% | 30% | 50% | 40% | 35% | |
| Surface-associated motility | % inhibition range | 7.7–40 | 7.7–40 | 7.7–40 | 6.7–40 | 6.7–40 |
| % of isolates with ≥ 50% inhibition | 60% | 70% | 50% | 20% | 30% | |
| Esterase production | % inhibition range | 5–56.5 | 21.9–66.7 | 5.5–59.2 | 5.5–59.2 | 13.4–38.1 |
| % of isolates with ≥ 50% inhibition | 10.5% | 31.5% | 5% | 10.5% | 0% | |
| Sensitivity to H2O2 | % inhibition range | 6.3–50 | 10–100 | 3.3–100 | 6.7–50 | 6.3–40 |
| % of isolates with ≥ 50% inhibition | 5% | 25% | 10% | 15% | 0% | |
| Phospholipase production | % inhibition range | 18.2–100 | 13–100 | 26.1–100 | 13–100 | 21.7–100 |
| % of isolates with ≥ 50% inhibition | 62.5% | 37.5% | 62.5% | 50% | 62.5% | |
Fig. 3.
Percentage of isolates with ≥ 50% inhibition in virulence factors production in A. baumannii isolates treated with sub-MIC of QSIs. AZ, azithromycin; E, erythromycin; LEV, levamisole; CQ, chloroquine; PPL, propranolol
Inhibition of twitching motility in A. baumannii
Twitching motility was tested in A. baumannii isolates, 40% of isolates were intermediately motile, and 60% were highly motile. All QSIs inhibited the twitching motility in all isolates with varying degrees more than 50% inhibition in twitching motility noticed in 6 isolates. The highest inhibition was recorded with levamisole. In addition, ≥ 80% inhibition was detected in 2 isolates in presence of erythromycin and one isolate in presence of propranolol and levamisole (Table 3 and Fig. 3).
Inhibition of surface-associated motility in A. baumannii
The results revealed that 50% of the A. baumannii isolates were positive for surface-associated motility. All QSIs inhibited surface motility; the inhibition was ranged from 7.7 to 40% in presence of azithromycin, erythromycin, and levamisole; and most of the isolates showed inhibition ≥ 20%. In addition, the highest number (n = 7) of isolates showing inhibition ≥ 20% in surface motility was recorded in presence of erythromycin (Table 3 and Fig. 3).
Inhibition of esterase production in A. baumannii
All A. baumannii isolates strongly produced esterase enzyme, except one isolate. The highest inhibition range was recorded in presence of erythromycin; esterase was inhibited in a range of 21.9–66.7%, with 6 isolates being inhibited by ≥ 50% (Table 3 and Fig. 3).
A. baumannii sensitivity to oxidative stress in presence of QSIs
The effect of hydrogen peroxide was highly augmented in presence of sub-MIC of erythromycin and levamisole. The augmentation ranged from 10 to 100% in case erythromycin and from 3.3 to 100% in case of levamisole (Table 3 and Fig. 3).
Inhibition of phospholipase production in A. baumannii
Only 8 isolates (40%) were phospholipase producers, two isolates were strong producers (Pz = 0.67), and the other 6 isolates were low producers (Pz = 0.71–0.77). The highest inhibition range was recorded in presence of levamisole, propranolol, and azithromycin in a range of 26.1–100%, 21.7–100%, and 18.2–100%, respectively (Table 3 and Fig. 3).
Protease and gelatinase production by A. baumannii
Protease and gelatinase activities were not detected in any of the tested isolates.
RNA isolation and quantitative PCR for acyl-homoserine lactone synthase (abaI) gene in A. baumannii
Relative expression of QS regulatory gene abaI to the reference gene 16S rRNA was tested. All tested isolates were positive for the expression of the abaI gene. In addition, qRT-PCR was performed on isolate no. 1 (AB1) either treated with the four QSIs or untreated culture as negative control. AZ was used as positive control. Relative expression levels of abaI gene was calculated using the 2^−ΔΔCt method according to Livak and Schmittgen (2001). At sub-inhibitory concentrations, erythromycin, azithromycin, levamisole, chloroquine, and propranolol highly repressed the expression of abaI gene by 92, 86.9, 83.32, 67, and 49%, respectively (Fig. 4). The fold decrease in the expression of abaI gene was 12.5, 7.7, 5.88, 3, and 2 times in presence of erythromycin, azithromycin, levamisole, chloroquine, and propranolol, respectively.
Fig. 4.
Fold decrease in abaI gene expression in AB1 isolate. AZ, azithromycin; E, erythromycin; LEV, levamisole; CQ, chloroquine; PPL, propranolol
Mice mortality test by using a peritoneal sepsis model
In mice mortality test, the 5 mice injected with AB1 alone started to die after 18 h of injection, and all of them were dead after 48 h. The control mice groups which were injected with solvents and saline were 100% alive throughout the experiment period. Mice groups injected with AB1 treated with sub-MIC of 4 potential QSIs showed significant improvement in survival rates; 100% survival was recorded in the group injected with culture grown with erythromycin (Fig. 5).
Fig. 5.
Survival rates in mice following inoculation with A. baumannii (AB1). Groups of mice (n = 5) were i.p. inoculated with AB1 alone or AB1 overnight treated with 4 potential QSIs as indicated and their clinical outcome monitored daily for 72 h
Molecular docking studies
Molecular docking of potential QSIs with AbaI
The molecular docking study ranked the activity of compounds (Moldock score) as inhibitors for autoinducer synthase AbaI as follows: erythromycin (− 169.34), propranolol (− 114.23), chloroquine (− 108.51), and levamisole (− 89.94). The binding interactions with the receptor are shown in Fig. 6a–e. The MolDock score for SAM was − 151.54, and the interacting residues were shown in supplementary Table S9. From the docking scores, the erythromycin showed higher binding affinity than SAM and the other studied compounds.
Fig. 6.
The molecular docking of QSIs into the active site of AbaI protein model (a–e). a Erythromycin. b SAM. c Propranolol. d Chloroquine. e Levamisole. And AbaR receptor model (f–j). f Chloroquine. g OH-DHL. h Propranolol. i Levamisole. j Erythromycin
Molecular docking of potential QSIs with AbaR
The molecular docking study ranked the activity of compounds (Moldock score) as inhibitors for AbaR receptor as follows: chloroquine (− 144.83), propranolol (− 131.89), levamisole (− 104.43), and erythromycin (− 55.09). The binding interactions with the receptor are shown in Fig. 6f–j. The MolDock score for N-(3-Hydroxydodecanoyl)-L-homoserine lactone was − 135.74, and the interacting residues are shown in supplementary Table S10. From the docking scores, chloroquine showed the highest binding affinity among the studied compounds.
Discussion
It is well known that QS controls virulence and pathogenicity of microbes; hence, it is a good target to design novel antimicrobial therapeutics by developing QSIs that target virulence through either inhibiting QS signal production, signal reception, or degrading AHLs [43]. In the present study, it was found that the tested drugs have inhibited QS in CV026 biosensor as indicated by inhibition of violacein pigment production. CV026 responds to C6-HSL and produces violacein, but in presence of QSIs, no pigment is produced. It is noticed that azithromycin and erythromycin formed an intense violet ring around the inhibition zone. This may be attributed to a potentiating effect for violacein production with a certain concentration of these inhibitors. This finding was in accordance with that of Liu et al. [44].
The highest inhibition of violacein pigment was recorded for erythromycin and azithromycin followed by levamisole, chloroquine, and propranolol; erythromycin has the highest QS inhibitory activity. This was consistent with several reports which reported that antibiotics interfere with QS by blocking C12-HSL production in P. aeruginosa [13, 45].
Pseudomonas aeruginosa has three major QS systems LasI/R, RhlI/R, and pseudomonas quinolone system (PQS) [46] which work together to control cell survival, biofilm formation, and virulence [47, 48]. It is very critical to inhibit biofilm as it is responsible for high antibiotic resistance rates [49], and it participates in serious infections [50]. The 4 tested drugs significantly reduced the ability of PAO1 to form biofilm as they had very strong anti-biofilm activities, with erythromycin being the most powerful QS inhibitor. Many reports stated the high inhibition of biofilm in PAO1 by other QSIs [51–53].
In the current study, sub-MIC of tested drugs highly inhibited both types of motility in PAO1. The swarming motility was significantly inhibited in a range of 64.3–84.3%; erythromycin had the strongest inhibitory activity. Consistent with our results, other studies reported high reduction in PAO1 swarming using other drugs [54, 55]. Twitching motility was inhibited in a range of 12.3–53.8%, and the highest inhibition was also in presence of erythromycin, which was comparable with previous work [51]. It was reported that swarming motility is affected by QS, rhamnolipid production, type IV pili, and flagella [56]. This may explain the higher inhibition in swarming motility than twitching that was observed in the current study.
In the present study, the effect of QSIs on hydrolytic enzymes like protease and gelatinase was investigated. These enzymes are very crucial for degrading host tissue components which aid in bacterial colonization [57]. The protease production by PAO1 was inhibited by 13–39.1% in presence of tested drugs. Similarly, other QSIs reduced PAO1 proteolytic activity [53, 55]. Moreover, gelatinase production by PAO1 was much more inhibited than protease enzyme by a range of 25–57.1%. In accordance with our results, macrolides inhibited gelatinase in P. aeruginosa [58].
Pyocyanin is responsible for tissue damage due to hydroxyl radical formation and also it suppresses the acute inflammatory response [59, 60]. The tested drugs inhibited pyocyanin production in PAO1 by a range of 16–53.9%. Erythromycin and levamisole were the most effective inhibitors. Consistent to our findings, several reports showed reduction in pyocyanin production by other drugs [53, 61].
Rhamnolipid (biosurfactant) is a key virulence determinant regulated by QS. It has antimicrobial activity against different bacteria and fungi [62, 63]. In the present study, rhamnolipid production was markedly inhibited in a range of 33.3–66.7%. Similar to our findings, baicalin demonstrated significant suppression in PAO1 rhamnolipid production [61].
PAO1 resistance to oxidative stress is under the control of QS [64]. In the current study, QSIs showed moderate increase in the sensitivity of PAO1 to H2O2; the highest reduction in tolerance to oxidative stress was obtained with erythromycin (36.7%). Similar to our findings, metformin and glyceryl trinitrate caused augmentation in the effect of H2O2 [52, 53].
It is well known that azithromycin and erythromycin (macrolide antibiotics) act mainly on Gram-positive bacteria. So, their inhibitory effect in P. aeruginosa and A. baumannii is not due to their antimicrobial activity, but due to their inhibitory activity on QS system [15]. In this study, several virulence factors in A. baumannii clinical isolates were investigated. Biofilm and twitching motility were detected in all 20 isolates (100%), followed by esterase (n = 19) then surface-associated motility (n = 10). The least detected virulence was phospholipase (n = 8), while none of the 20 isolates produced proteolytic enzymes. Five isolates produced all these factors including isolate (no. 1) which has the highest virulence expression; hence, it was used in animal study and RT-PCR experiments.
Biofilm formation is considered one of the main virulence factors in A. baumannii [65]. In the present study, QSIs markedly reduced biofilm formation in A. baumannii clinical isolates as 50% inhibition was observed in 75% of A. baumannii isolates. Chloroquine showed the highest range of inhibition (67.4–93.5%). This finding was consistent with many reports that linked QS to biofilm formation in A. baumannii [7, 66]. Also, chloroquine sensitizes biofilm of Candida to azoles [67].
Twitching motility allows A. baumannii to spread rapidly on semisolid surfaces; twitching is mediated by type IV pili (TFP) system [25, 68]. All of our isolates showed twitching motility, while Vijaykumar et al. [26] found that 58.3% of isolates had twitching motility. Twitching motility is regulated by several environmental factors [25, 69, 70]. The 4 tested QSIs inhibited twitching motility in all A. baumannii isolates with varying degrees. The highest inhibition was recorded in presence of levamisole (11.7–89.5%). The difference in results between this work and other studies may be related to different factors including source and nature of isolates, and experimental conditions.
Many strains of A. baumannii have been found to exhibit unique surface-associated motility on semisolid surface that resembles swarming motility of P. aeruginosa; however, swarming motility is flagellum-coordinated movement [71]. A. baumannii surface-associated motility is a flagellum-independent, complex process that is dependent on many factors including QS [25, 69, 72]. It has been speculated that TFP might be involved in the surface-associated motility of A. baumannii [68]. In the present study, 50% of A. baumannii isolates were positive in surface-associated motility. In agreement with our results, Eraç et al. [73] reported that 44% of A. baumannii isolates were motile. At the contrary, Vijaykumar et al. [26] reported that only 10% of isolates swarm, while Skiebe et al. [72] reported nearly all isolates had swarming-like motility on 0.5% agarose-containing media; however, we used 0.4% agar. Any variation in the physical factors could have effect on motility; we also found that using low salt concentration in the media gives better motility. All the tested QSIs inhibited surface motility; ≥ 20% inhibition was observed in presence of azithromycin, erythromycin, and levamisole. In addition, ≥ 50% inhibition was recorded in 7 isolates in presence of erythromycin. At the contrary, 60% of A. baumannii isolates underwent a decrease in surface-associated motility in presence of virstatin [74].
In the present study, 95% of A. baumannii isolates were strong esterase producers. Valli and Gopinath [75] found that 70% of isolates were esterase positive which agreed with our results to some extent. In the current study, the highest inhibition range of esterase production was recorded in presence of erythromycin (21.9–66.7%) with the highest number of isolates being inhibited by ≥ 50%, followed by chloroquine and levamisole.
Pathogens are exposed to killing by host via various reactive oxygen species (ROS). Pathogen is able to resist ROS and persist under oxidative stress by production of superoxide dismutase (SOD) and catalase enzymes. SOD was found to play vital role in resistance to oxidative stress in A. baumannii [70]. Autoinducer synthase mutant was found to produce small amount of antioxidant enzymes indicating the importance of QS in response to oxidative stress [70]. In the current study, the effect of H2O2 was highly augmented (tolerance to oxidative stress was reduced) in presence of sub-MIC of erythromycin (10–100%) and levamisole (3.3–100%). A recent study showed that curcumin enhances the therapeutic efficacy of antibiotics by increasing ROS and compromising oxidative stress defense [76].
In the current study, results revealed that only 40% of A. baumannii were phospholipase producers. In agreement with our results, two previous studies found similar percentage of PLC production [77, 78]. Regarding the inhibition of PLC, our results revealed that at least one isolate had 100% inhibition in phospholipase production in presence of some tested drugs. The highest number of isolates inhibited by ≥ 50% was recorded with levamisole, propranolol, and azithromycin. In our study, both protease and gelatinase activities were not detected in A. baumannii, in accordance with Abdulla et al. [79]. However, other studies reported proteolytic activity in A. baumannii [75, 78].
The qRT-PCR was used to study the relative expression of QS regulatory gene abaI in A. baumannii isolates, and to calculate the relative expression of abaI gene before and after treatment with sub-MIC of QSIs. It was found that erythromycin, azithromycin, levamisole, chloroquine, and propranolol highly repressed expression of abaI by 92, 86.9, 83.32, 67, and 49%, respectively. These results confirm the QS inhibitory activity of the 4 drugs at molecular level. This finding provides a basis to explain the remarkable decrease in the production of QS-regulated virulence factors. Similarly, significant downregulation of QS regulator systems of PAO1 treated with sub-inhibitory concentration of QSIs was reported [51, 55].
It is worth mentioning that the concentrations of the drugs used as QSIs do not always meet the pharmacological limits for human use. Levamisole and propranolol therapeutic plasma levels 0.8–1.6 μg/mL and 0.134 μg/mL, respectively [80, 81], are much lower than their concentrations as QSIs in this study. On the contrary, erythromycin and azithromycin therapeutic plasma levels are 3.5 μg/mL and 0.24 μg/mL, respectively [82], and are higher than the concentrations used as QSIs in this study. The in vitro results must not be considered as final applicable conclusions in clinical situations. Moreover, the behavior of bacteria in lab differs from that in human body, and characteristics of drugs in lab also differ from those in human body where the drug may undergo degradation, conformational changes, re-arrangement, and plasma protein binding. Therefore, all in vitro studies are considered as a beginning step and must be fulfilled with in vivo studies. To compensate this shortage in reaching the drug therapeutic plasma level with some drugs, it could be possible to use QSIs with high MIC values in topical formulations like dressings or ointments for skin and soft-tissue infections and aerosols for respiratory infections. Also, QSIs with high MIC can be tested in future study in combination with antibiotics using low concentration of these QSIs that not exceed their accepted therapeutic levels.
To evaluate the effect of the 4 QSIs in vivo, the mice mortality test was performed. First, mice were injected with 250 μL of A. baumannii (AB1) grown without QSIs, which cause 100% mortality within 48 h. Several studies have reported other numbers of bacteria injected in the mice, some agree with our number, and others differ [40, 83, 84]. This was strain-dependent, and many reports account this to the probable negative correlation between MDR phenotype and virulence [85, 86]. The obtained results revealed that mice which were injected with AB1 grown with sub-MIC of QSIs showed significant improvement in survival rates, which reached 100% in case of erythromycin followed by 80% in presence of propranolol.
A more confirmation of QS inhibitory mechanism of the tested drugs was done using the molecular docking study. It was revealed that erythromycin showed higher binding affinity than SAM (the natural ligand of AbaI) while levamisole had the lowest binding affinity. Moreover, all drugs bound with the active site of the ligand-binding domain of AbaI by hydrophobic interactions and H-bonding. In addition, molecular docking study ranked the activity of the compounds as inhibitors for AbaR receptor with chloroquine being the most active, followed by propranolol with a score similar to the natural ligand. The binding interactions with the receptor were by hydrophobic interactions and H-bonding except levamisole, which had no H-bonding. Erythromycin exhibited the lowest inhibition for AbaR receptor. Therefore, the potential mechanism of QS inhibition by the 4 tested drugs may be due to either binding to the AbaI autoinducer synthase preventing AHL synthesis, or binding to AbaR receptor preventing AHL signal reception. Finally, erythromycin markedly inhibited QS in vivo and in vitro in A. baumannii isolates. This may be due to inhibiting the synthesis of AHL signals by erythromycin more than inhibiting signal reception. In addition, chloroquine inhibited QS in A. baumannii by inhibiting AHL signal reception more than AHL signal synthesis. Several studies performed the docking of QSIs against either LasR or RhlR of PAO1, and a significant binding potential to the active site of these proteins was revealed confirming the QS inhibitory activity [51, 53, 55].
Conclusion
The study demonstrated that QS could control the virulence, as most of virulence factors of both PAO1 and A. baumannii clinical isolates were highly inhibited by QSIs. The most effective drug as QSIs was erythromycin. To the best of our knowledge, this study showed that antibiotics like erythromycin can inhibit QS beside their antimicrobial activity; the other tested drugs (i.e., chloroquine, levamisole, and propranolol) were studied for the first time as inhibitors for QS in A. baumannii. Results obtained from qRT-PCR, in vivo study, and molecular docking of 4 QSIs against AbaI and AbaR proteins could give a more confirmation of the mechanism of QS inhibition by the tested drugs. In addition, inhibition of QS using FDA-approved drugs present in the market is a promising strategy for inhibiting virulence without affecting microbial growth which could be used as a therapeutic alternative for traditional antibiotics. This could help in decreasing the selective pressure causing antibiotic resistance development. Future studies are needed to formulate the tested drugs in suitable dosage forms and to study their effects in vivo.
Electronic supplementary material
(DOCX 320 kb)
Acknowledgements
We would like to thank Islam Mohsen and Fatma Yehia (assistant lectures in Microbiology & Immunology Department, Zagazig University) for providing Acinetobacter baumannii isolates, and the Department of Microbiology and Immunology, Ain Shams University, for providing the CVO26 strain.
Authors’ contributions
NMS, HKA, and AE conceived and designed the experiments. NMS performed the experiments except the molecular docking studies which were done by MAS. AE and NMS analyzed and interpreted the data. NMS wrote the manuscript draft. HKA and AE revised and edited the manuscript. All the authors approved the final manuscript.
Compliance with ethical standards
Ethics approval
Experimental design and animal handling procedures were performed according to the guidelines of the Ethical Committee of for animal use in the Faculty of Pharmacy, Zagazig University.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Castillo-Juarez I, Lopez-Jacome LE, Soberón-Chávez G, Tomás M, Lee J, Castañeda-Tamez P, et al. Exploiting quorum sensing inhibition for the control of Pseudomonas aeruginosa and Acinetobacter baumannii biofilms. Curr Top Med Chem. 2017;17(17):1915–1927. [PubMed] [Google Scholar]
- 2.Dijkshoorn L, Nemec A, Seifert H. An increasing threat in hospitals: multidrug resistant Acinetobacter baumannii. Nat Rev Microbiol. 2007;5:939–951. doi: 10.1038/nrmicro1789. [DOI] [PubMed] [Google Scholar]
- 3.Navon-Venezia S, Ben-Ami R, Carmeli Y. Update on Pseudomonas aeruginosa and Acinetobacter baumannii infections in the health care setting. Curr Opin Infect Dis. 2005;18:306–313. doi: 10.1097/01.qco.0000171920.44809.f0. [DOI] [PubMed] [Google Scholar]
- 4.Rutherford ST, Bassler BL. Bacterial quorum sensing: its role in virulence and possibilities for its control. Cold Spring Harb Perspect Med. 2012;2(11):1–25. doi: 10.1101/cshperspect.a012427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rasko DA, Sperandio V. Anti-virulence strategies to combat bacteria-mediated disease. Nat Rev Drug Discov. 2010;9:117–128. doi: 10.1038/nrd3013. [DOI] [PubMed] [Google Scholar]
- 6.Bjarnsholt T, Givskov M. Quorum-sensing blockade as a strategy for enhancing host defences against bacterial pathogens. Philos Trans R Soc B. 2007;362:1213–1222. doi: 10.1098/rstb.2007.2046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Niu C, Clemmer KM, Bonomo RA, Rather PN. Isolation and characterization of an autoinducer synthase from Acinetobacter baumannii. J Bacteriol. 2008;190:3386–3392. doi: 10.1128/JB.01929-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imperi F, Massai F, Pillai CR, Longo F, Zennaro E, Rampioni G, et al. New life for an old drug: the anthelmintic drug niclosamide inhibits Pseudomonas aeruginosa quorum sensing. Antimicrob Agents Chemother. 2013;57(2):996–1005. doi: 10.1128/AAC.01952-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Givskov M, de Nys R, Manefield M, Gram L, Maximilien R, Eberl L, et al. Eukaryotic interference with homoserine lactonemediated prokaryotic signalling. J Bacteriol. 1996;178:6618–6622. doi: 10.1128/jb.178.22.6618-6622.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kjelleberg S, Steinberg P, Givskov M, Gram L, Manefield M, de Nys R. Do marine natural products interfere with prokeryotic AHL regulatory systems? Aquat Microb Ecol. 1997;13:85–93. [Google Scholar]
- 11.Pushpakom S, Iorio F, Eyers PA, Escott KJ, Hopper S, Wells A, et al. Drug repurposing: progress, challenges and recommendations. Nat Rev Drug Discov. 2019;18(1):41–58. doi: 10.1038/nrd.2018.168. [DOI] [PubMed] [Google Scholar]
- 12.Tateda K, Comte R, Pechere J, Köhler T, Yamaguchi K, Van Delden C (2001) Azithromycin inhibits quorum sensing in Pseudomonas aeruginosa. 45:1930–1933 [DOI] [PMC free article] [PubMed]
- 13.Skindersoe ME, Alhede M, Phipps R, Yang L, Jensen PO, Rasmussen TB, et al. Effects of antibiotics on quorum sensing in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2008;52:3648–3663. doi: 10.1128/AAC.01230-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saroj SD, Rather PN. Streptomycin inhibits quorum sensing in Acinetobacter baumannii. Antimicrob Agents Chemother. 2013;57(4):1926–1929. doi: 10.1128/AAC.02161-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hof H. Macrolides, a group of antibiotics with a broad spectrum of activity. Immun Infekt. 1994;22(2):66–71. [PubMed] [Google Scholar]
- 16.Baker CA, Desrosiers K, Dolan JW. Propranolol inhibits hyphal development in Candida albicans. Antimicrob Agents Chemother. 2002;46(11):3617–3620. doi: 10.1128/AAC.46.11.3617-3620.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sperandio V, Torres AG, Jarvis B, Nataro JP, Kaper JB. Bacteria–host communication: the language of hormones. PNAS USA. 2003;100(15):8951–8956. doi: 10.1073/pnas.1537100100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aleksić I, Šegan S, Andrić F, Zlatović M, Moric I, Opsenica DM, et al. Long-chain 4-aminoquinolines as quorum sensing inhibitors in Serratia marcescens and Pseudomonas aeruginosa. ACS Chem Biol. 2017;12(5):1425–1434. doi: 10.1021/acschembio.6b01149. [DOI] [PubMed] [Google Scholar]
- 19.Devaux CA, Rolain JM, Colson P, Raoult D (2020) New insights on the antiviral effects of chloroquine against coronavirus: what to expect for COVID-19? Int J Antimicrob Agents 105938 [DOI] [PMC free article] [PubMed]
- 20.Sinha S, Sarkar R, Garg VK. Successful treatment of chronic mucocutaneous candidiasis with oral antifungals and levamisole. Indian J Paediatr Dermatol. 2015;16:159–162. [Google Scholar]
- 21.Tan LY, Yin W, Chan K. Silencing quorum sensing through extracts of Melicope lunu-ankenda. Sensors. 2012;12:4339–4351. doi: 10.3390/s120404339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clinical and Laboratory Standards Institute (2012) Performance standards for antimicrobial disk susceptibility tests; approved standard—11th edition. CLSI document M02-A11. Wayne: CLSI
- 23.Choo JH, Rukayadi Y, Hwang JK. Inhibition of bacterial quorum sensing by vanilla extract. Lett Appl Microbiol. 2006;42(6):637–641. doi: 10.1111/j.1472-765X.2006.01928.x. [DOI] [PubMed] [Google Scholar]
- 24.Stepanovic S, Vukovic D, Hola V, Di Bonaventura G, Djukić S, Cirković I, Ruzicka F. Quantification of biofilm in microtiter plates: overview of testing conditions and practical recommendations for assessment of biofilm production by staphylococci. APMIS. 2007;115(8):891–899. doi: 10.1111/j.1600-0463.2007.apm_630.x. [DOI] [PubMed] [Google Scholar]
- 25.Clemmer KM, Bonomo RA, Rather PN. Genetic analysis of surface motility in Acinetobacter baumannii. Microbiol. 2011;157(9):2534–2544. doi: 10.1099/mic.0.049791-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vijayakumar S, Rajenderan S, Laishram S, AnandanS BV, Biswas I. Biofilm formation and motility depend on the nature of the Acinetobacter baumannii clinical isolates. Front Public Health. 2016;4(105):1–9. doi: 10.3389/fpubh.2016.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta RK, Setia S, Harjai K. Expression of quorum sensing and virulence factors are interlinked in P. aeruginosa: an in vitro approach. Am J Biomed Sci. 2011;3:116–125. [Google Scholar]
- 28.Vijayaraghavan P, Vincent SGP. A simple method for the detection of protease activity on agar plate using bromocresolgreen dye. J Biochem Tech. 2013;4(3):628–630. [Google Scholar]
- 29.Su YA, Sulavik MC, He P, Mäkinen KK, Mäkinen P-L, Fiedler S, et al. Nucleotide sequence of the gelatinase gene (gele) from Enterococcus faecalis subsp. Liquefaciens. Infect Immun. 1991;59(1):415–420. doi: 10.1128/iai.59.1.415-420.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanchez A, Escandon P, Castaneda E. In vitro determination of virulence factors activity associated with several Cryptococcus neoformans clinical isolates. Rev Iberoam Micol. 2008;25:145–149. doi: 10.1016/s1130-1406(08)70034-2. [DOI] [PubMed] [Google Scholar]
- 31.Hassett DJ, Schweizer HP, Ohman DE. Pseudomonas aeruginosa soda and sodb mutants defective in manganese- and iron-cofactored superoxide dismutase activity demonstrate the importance of the iron-cofactored form in aerobic metabolism. J Bacteriol. 1995;177:6330–6337. doi: 10.1128/jb.177.22.6330-6337.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Das T, Manefield M. Pyocyanin promotes extracellular DNA release in Pseudomonas aeruginosa. PLoS One. 2012;7:e46718. doi: 10.1371/journal.pone.0046718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rashid MH, Kornberg A. Inorganic polyphosphate is needed for swimming, swarming, and twitching motilities of Pseudomonas aeruginosa. PNAS. 2000;97(9):4885–4890. doi: 10.1073/pnas.060030097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Youssef N, Duncan KE, Savage KN. Comparison of methods to detect biosurfactant production by diverse microorganisms. J Microbiol Methods. 2004;56:339–347. doi: 10.1016/j.mimet.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 35.Slifkin M. Tween 80 opacity test responses of various Candida species. J Clin Microbiol. 2000;38(12):4626–4628. doi: 10.1128/jcm.38.12.4626-4628.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Esselmann MT, Liu PV. Lecithinase production by gram-negative bacteria. J Bacteriol. 1961;81:939–945. doi: 10.1128/jb.81.6.939-945.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Selasi GN, Nicholas A, Jeon H, Na SH, Kwon HI, Kim YJ, et al. Differences in biofilm mass, expression of biofilm-associated genes, and resistance to desiccation between epidemic and sporadic clones of carbapenem-resistant Acinetobacter baumannii sequence type. PLoS One. 2016;11(9):e0162576. doi: 10.1371/journal.pone.0162576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clifford RJ, Milillo M, Prestwood J, Quintero R, Zurawski DV, et al. Detection of bacterial 16S rRNA and identification of four clinically important bacteria by real-time PCR. PLoS One. 2012;7:e48558. doi: 10.1371/journal.pone.0048558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2-ΔΔct method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 40.Lood R, Winer BY, Pelzek AJ, Diez-Martinez R, Thandar M, Euler CW, et al. Novel phage lysin capable of killing the multidrug-resistant gram-negative bacerium Acinetobacter baumannii in a mouse bacteremia model. Antimicrob Agents Chemother. 2015;59(4):1983–1991. doi: 10.1128/AAC.04641-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chung J, Goo E, Yu S, Choi O, Lee J, Kim J, et al. Small-molecule inhibitor binding to an N-acyl-homoserine lactone synthase. PNAS. 2011;108(29):12089–12094. doi: 10.1073/pnas.1103165108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomsen R, Christensen MH, Moldock A new technique for high-accuracy molecular docking. J Med Chem. 2006;49:3315–3321. doi: 10.1021/jm051197e. [DOI] [PubMed] [Google Scholar]
- 43.Hentzer M, Givskov M. Pharmacological inhibition of quorum sensing for the treatment of chronic bacterial infections. J Clin Invest. 2003;112:1300–1307. doi: 10.1172/JCI20074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu Z, Weishan W, Zhu Y, Gong Q, Yu W, Lu X. Antibiotics at sub-inhibitory concentrations improve the quorum sensing behavior of Chromobacterium violaceum. FEMS Microbiol Lett. 2013;341(1):37–44. doi: 10.1111/1574-6968.12086. [DOI] [PubMed] [Google Scholar]
- 45.Tateda K, Standiford TJ, Pechere JC, Yamaguchi K. Regulatory effects of macrolides on bacterial virulence: potential role as quorum-sensing inhibitors. Curr Pharm Des. 2004;10:3055–3065. doi: 10.2174/1381612043383377. [DOI] [PubMed] [Google Scholar]
- 46.Heeb S, Fletcher MP, Chhabra SR, Diggle SP, Williams P, Cámara M. Quinolones: from antibiotics to autoinducers. FEMS Microbiol Rev. 2011;35:247–274. doi: 10.1111/j.1574-6976.2010.00247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pearson JP, Feldman M, Iglewski BH, Prince A. Pseudomonas aeruginosa cell-to-cell signaling is required for virulence in a model of acute pulmonary infection. Infect Immun. 2000;68(7):4331–4334. doi: 10.1128/iai.68.7.4331-4334.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kipnis E, Sawa T, Wiener-Kronish J. Targeting mechanisms of Pseudomonas aeruginosa pathogenesis. Med Mal Infect. 2006;36:78–91. doi: 10.1016/j.medmal.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 49.Høiby N, Bjarnsholt T, Givskov M, Molin S, Ciofu O. Antibiotic resistance of bacterial biofilms. Int J Antimicrob Agents. 2010;35(4):322–332. doi: 10.1016/j.ijantimicag.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 50.Høiby N. Recent advances in the treatment of Pseudomonas aeruginosa infections in cystic fibrosis. BMC Med. 2011;9(32):1–7. doi: 10.1186/1741-7015-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.El-Mowafy SA, Abd El Galil KH, El-Messery SM, Shaaban MI. Aspirin is an efficient inhibitor of quorum sensing, virulence and toxins in Pseudomonas aeruginosa. Microb Pathog. 2014;74:25–32. doi: 10.1016/j.micpath.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 52.Abbas HA, Shaldam MA. Glyceryl trinitrate is a novel inhibitor of quorum sensing in Pseudomonas aeruginosa. Afr Health Sci. 2016;16(4):1107–1116. doi: 10.4314/ahs.v16i4.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Abbas HA, Elsherbini AM, Shaldam MA. Repurposing metformin as a quorum sensing inhibitor in Pseudomonas aeruginosa. Afr Health Sci. 2017;17(3):808–819. doi: 10.4314/ahs.v17i3.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ulusoy S, Tinaz G. Nonsteroidal anti-inflammatory drugs reduce the production of quorum sensing regulated virulence factors and swarming motility in human pathogen Pseudomonas aeruginosa. Drug Res. 2013;63(8):409–413. doi: 10.1055/s-0033-1343430. [DOI] [PubMed] [Google Scholar]
- 55.Abbas HA, Soliman WEE, Shaldam MA. Perturbation of quorum sensing in Pseudomonas aeruginosa by febuxostat. Adv Microbiol. 2018;8:650–664. [Google Scholar]
- 56.Déziel E, Lépine F, Milot S, Villemur R. rhlA is required for the production of a novel biosurfactant pro-moting swarming motility in Pseudomonas aeruginosa: 3-(3-hydroxyalkanoyloxy) alkanoic acids (HAAs), the precursors of rhamnolipids. Microbiol. 2003;149:2005–2013. doi: 10.1099/mic.0.26154-0. [DOI] [PubMed] [Google Scholar]
- 57.Bandara BM, Zhu H, Sankaridurg PR, Willcox MD. Salicylic acid reduces the production of several potential virulence factors of P. aeruginosa associated with microbial keratitis. Invest Ophthalmol Vis Sci. 2006;47:4453e60. doi: 10.1167/iovs.06-0288. [DOI] [PubMed] [Google Scholar]
- 58.Mizukane R, Hirakata Y, Kaku M, Ishii Y, Furuya N, Ishida K, et al. Comparative in vitro exoenzyme-suppressing activities of azithromycin and other macrolide antibiotics against Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1994;38:528–533. doi: 10.1128/aac.38.3.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Britigan BE, Roeder TL, Rasmussen GT, Shasby DM, McCormick ML, Cox CD. Interaction of the Pseudomonas aeruginosa secretory products pyocyanin and pyochelin generates hydroxyl radical and causes synergistic damage to endothelial cells. Implications for Pseudomonas-associated tissue injury. J Clin Invest. 1993;90(6):2187–2196. doi: 10.1172/JCI116104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hall S, McDermott C, Anoopkumar-Dukie S, McFarland AJ, Forbes A, Perkins AV, et al. Cellular effects of pyocyanin, a secreted virulence factor of Pseudomonas aeruginosa. Toxins. 2016;8(236):1–14. doi: 10.3390/toxins8080236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Luo J, Dong B, Wang K, Cai S, Liu T, Cheng X, et al. Baicalin inhibits biofilm formation, attenuates the quorum sensing controlled virulence and enhances Pseudomonas aeruginosa clearance in a mouse peritoneal implant infection model. PLoS One. 2017;12(4):e0176883. doi: 10.1371/journal.pone.0176883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ochsner UA, Koch AK, Fiechter A, Reiser J. Isolation and characterization of a regulatory gene affecting rhamnolipid biosurfactant synthesis in Pseudomonas aeruginosa. J Bacteriol. 1994;176:2044–2054. doi: 10.1128/jb.176.7.2044-2054.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Haba E, Pinazo A, Jauregui O, Espuny MJ, Infante MR, Manresa A. Physicochemical characterization and antimicrobial properties of rhamnolipids produced by Pseudomonas aeruginosa 47T2 NCBIM 40044. Biotechnol Bioeng. 2003;81:316–322. doi: 10.1002/bit.10474. [DOI] [PubMed] [Google Scholar]
- 64.Bjarnsholt T, Jensen PO, Burmolle M, Hentzer M, Haagensen JAJ, Hougen HP, et al. Pseudomonas aeruginosa tolerance to tobramycin, hydrogen peroxide and polymorphonuclear leukocytes is quorum-sensing dependent. Microbiol. 2005;151:373–383. doi: 10.1099/mic.0.27463-0. [DOI] [PubMed] [Google Scholar]
- 65.Gurung J, Annie BK, Banik A, Lyngdoh WV, Choudhury B, Bhattacharyya P. Association of biofilm production with multidrug resistance among clinical isolates of Acinetobacter baumannii and Pseudomonas aeruginosa from intensive care unit. Indian J Crit Care Med. 2013;17:214–218. doi: 10.4103/0972-5229.118416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gaddy JA, Actis LA. Regulation of Acinetobacter baumannii biofilm formation. Future Microbiol. 2009;4:273–278. doi: 10.2217/fmb.09.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Shinde RB, Raut JS, Chauhan NM, Karuppayil SM. Chloroquine sensitizes biofilms of Candida albicans to antifungal azoles. Braz J Infect Dis. 2013;17(4):395–400. doi: 10.1016/j.bjid.2012.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Harding CM, Tracy EN, Carruthers MD, Rather PN, Actis LA, Munson RS. Acinetobacter baumannii strain M2 produces type IV pili which play a role in natural transformation and twitching motility but not surface-associated motility. mBio. 2013;4(4):e00360–e00313. doi: 10.1128/mBio.00360-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mcqueary CN, Kirkup BC, Si Y, Barlow M, Actis LA, Craft DW, et al. Extracellular stress and lipopolysaccharide modulate Acinetobacter baumannii surface-associated motility. J Microbiol. 2012;50(3):434–443. doi: 10.1007/s12275-012-1555-1. [DOI] [PubMed] [Google Scholar]
- 70.Heindorf M, Kadari M, Heider C, Skiebe E, Wilharm G. Impact of Acinetobacter baumannii superoxide dismutase on motility, virulence, oxidative stress resistance and susceptibility to antibiotics. PLoS One. 2014;9(7):e101033. doi: 10.1371/journal.pone.0101033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Henrichsen J. Bacterial surface translocation: a survey and a classification. Bacteriol Rev. 1972;36:478–503. doi: 10.1128/br.36.4.478-503.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Skiebe E, de Berardinis V, Morczinek P, Kerrinnes T, Faber F, Lepka D, et al. Surface-associated motility, a common trait of clinical isolates of Acinetobacter baumannii, depends on 1,3-diaminopropane. Int J Med Microbiol. 2012;302(3):117–128. doi: 10.1016/j.ijmm.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 73.Eraç B, Yılmaz FF, Hoşgör Limoncu M, Oztürk I, Aydemir S. Investigation of the virulence factors of multidrug-resistant Acinetobacter baumannii isolates. Mikrobiyol Bul. 2014;48(1):70–81. [PubMed] [Google Scholar]
- 74.Chabane YN, Mlouka MB, Alexandre S, Nicol M, Pestel-Caron M, Vila J, et al. Virstatin inhibits biofilm formation and motility of Acinetobacter baumannii. BMC Microbiol. 2014;14(62):1–7. doi: 10.1186/1471-2180-14-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Valli B, Gopinath P. Detection of gelatinase and lipase among clinical isolates of Acinetobacter baumannii. J Chem Pharm Sci. 2016;9(4):3245–3247. [Google Scholar]
- 76.Kaur A, Sharma P, Capalash N. Curcumin alleviates persistence of Acinetobacter baumannii against colistin. Sci Rep. 2018;8(1):11029. doi: 10.1038/s41598-018-29291-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.AL-Warid RJM, AL-Thahab AAL. Isolation and identification of Acinetobacter baumannii in Hilla city. IJABR. 2014;4(1):4–8. [Google Scholar]
- 78.Tektook NK. Study the virulence factors and patterns of antibiotics resistance in Acinetobacter baumannii isolated from hospitalized patients in Baghdad city. Pak J Biotechnol. 2018;15(1):19–23. [Google Scholar]
- 79.Abdulla AA, Althahab AA, Abed TA, Mahdi RK, Fadhil S. Screening of virulence factors in Acintobacter baumannii isolated from clinical samples. Int J Curr Res Aca Rev. 2015;3(6):128–134. [Google Scholar]
- 80.Pine M, Favrot L, Smith S, Mcdonald K, Chidsey CA. Correlation of plasma propranolol concentration with therapeutic response in patients with angina pectoris. Circulation. 1975;52:886–893. doi: 10.1161/01.cir.52.5.886. [DOI] [PubMed] [Google Scholar]
- 81.Luyckx M, Rousseau F, Cazin M, Brunet C, Cazin JC, Haguenoer JM, et al. Pharmacokinetics of levamisole in healthy subjects and cancer patients. Eur J Drug Metab Pharmacokinet. 1982;7(4):247–254. doi: 10.1007/BF03189626. [DOI] [PubMed] [Google Scholar]
- 82.Kaneko T, Dougherty TJ, Magee TV. Macrolide Antibiotics. In: Taylor JB, Triggle DJ, editors. Comprehensive medicinal chemistry II. Amsterdam: Elsevier; 2007. pp. 519–566. [Google Scholar]
- 83.Ko WC, Lee HC, Chiang SR, Yan JJ, Wu JJ, Lu CL, et al. In vitro and in vivo activity of meropenem and sulbactam against a multidrug-resistant Acinetobacter baumannii strain. J Antimicrob Chemother. 2004;53:393–395. doi: 10.1093/jac/dkh080. [DOI] [PubMed] [Google Scholar]
- 84.Gaddy JA, Arivett BA, McConnell MJ, López-Rojas R, Pachón J, Actis LA. Role of acinetobactin-mediated iron acquisition functions in the interaction of Acinetobacter baumannii ATCC 19606T with human lung epithelial cells, Galleria mellonella caterpillars and mice. Infect Immun. 2012;80:1015–1024. doi: 10.1128/IAI.06279-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.López-Rojas R, McConnell MJ, Jiménez-Mejías ME, Domínguez-Herrera J, Fernández-Cuenca F, Pachón J. Colistin resistance in a clinical Acinetobacter baumannii strain appearing after colistin treatment: effect on virulence and bacterial fitness. Antimicrob Agents Chemother. 2013;57(9):4587–4589. doi: 10.1128/AAC.00543-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Geisinger E, Isberg RR. Interplay between antibiotic resistance and virulence during disease promoted by multidrug-resistant bacteria. J Infect Dis. 2017;215(1):S9–S17. doi: 10.1093/infdis/jiw402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 320 kb)