Abstract
Acute myeloid leukemia (AML) in older patients is often associated with biologic and clinical characteristics that predict poor outcomes to cytarabine and anthracycline based induction chemotherapy (IC). The impact of hypomethylating agents (HMA) in the treatment of these high-risk patients is unknown. Here we retrospectively examined the remission rates and survival outcomes of 201 newly diagnosed patients ≥ 60 years old with therapy-related (t-AML), secondary (s-AML), or AML with myelodysplasia-related changes (AML-MRC). Ninety-eight patients received IC, and 103 received HMA. Patients in the IC cohort were younger than those who received HMA (68 vs. 74 years; p<0.01) with lower comorbidity burden. Composite complete remission rates (CR) were 39% in IC and 27% in the HMA cohorts (p=0.10). Overall survival (OS) was not significantly different between the two cohorts (7.59 mos vs. 5.49 mos; HR 0.75 95% CI 0.55–1.02) despite the fact that more patients in the IC cohort (33% versus 5%, p<0.01) underwent allogeneic stem cell transplant. Patients with t-AML (HR 0.56; 95% CI 0.33–0.97) and complex karyotype without monosomal karyotype (CK+MK-; HR 0.37; 95% CI 0.19–0.75) had better OS following IC. Patients with CK+MK+ (HR 2.00; 95% CI 1.08–3.70) had improved OS following HMA. Our results support the use of HMA as an alternative upfront regimen in older individuals with newly diagnosed high-risk AML based on similar clinical outcomes to IC.
Keywords: secondary AML, high-risk, epigenetic therapy, hypomethylating agents, azacitidine, decitabine, intensive chemotherapy
Introduction
Tremendous progress in our understanding of the biology of acute myeloid leukemia (AML) has yet to be translated into improved patient outcomes, as evidenced by a 5-yr survival rate of only 30%. This dismal outcome is driven by certain subgroups of AML patients, informally referred to as high-risk AML, characterized by advanced age, poor risk cytogenetics, and secondary AML (s-AML), therapy-related AML (t-AML), or AML with myelodysplastic related changes (AML-MRC). It is well recognized that AML patients with an adverse cytogenetic profile have worse survival than those with favorable or intermediate risk cytogenetic profiles[1, 2]. Monosomal karyotype (MK), defined as two or more monosomies, or a single monosomy in the presence of additional structural abnormalities, has recently been identified to define a distinct subset of AML with extremely poor prognosis[3–5]. In fact, MK+ve AML confers a worse prognosis than AML characterized by traditionally defined complex karyotype (CK; ≥ three cytogenetic abnormalities) and various specific individual adverse cytogenetic abnormalities[5]. Beyond cytogenetics, s-AML arising from antecedent hematologic disorder such as myelodysplastic syndrome (MDS) or myeloproliferative neoplasm (MPN), or t-AML occurring in patients with a history of prior myelotoxic chemotherapy also carry worse prognoses following intensive chemotherapy (IC). Therapy-related myeloid neoplasms now constitute a distinct subcategory in the 2016 revision to the World Health Organization (WHO) classification of myeloid neoplasms[6]. Another subcategory of AML associated with poor prognosis is AML with myelodysplasia-related changes (AML-MRC), first introduced in the 2008 WHO classification, and consists of AML arising in patients with a history of MDS, presence of one or more MDS-related cytogenetic abnormalities, or multilineage dysplasia defined as presence of ≥ 50% dysplastic cells in at least 2 cell lines[6].
Importantly, there is a complex interplay between these high-risk subsets of AML and advanced patient age. These high-risk biological features occur most frequently in older patients who are also at increased risk as compared with their younger counterparts to succumb to treatment- and disease-related complications. Newer treatment modalities appear to have done little to improve outcomes in this patient population. Indeed, a survival analysis of 61,000 AML patients in the Surveillance, Epidemiology, and End Results (SEER) database diagnosed between 1973 to 2016 demonstrated an improvement in the median overall survival (mOS) of younger AML patients aged < 60 years (by 18.36 days/year) with no such improvement (a mere 0.36 days/year) in AML patients ≥ 60 years[7]. Older patients with high-risk AML in particular, tend to fare especially poorly following IC with a mOS of only 6 months and treatment related mortality rates of up to 30%. An alternative induction strategy of a hypomethylating agent (HMA; decitabine and azacitidine) has been widely adopted as a less intensive and safer induction option for older unfit patients. To date, however, data comparing the outcomes of IC vs. HMA therapy in geriatric high risk AML patients has been lacking. Here, we performed a retrospective analysis of the outcomes of IC versus HMA induction therapy in newly diagnosed older individuals with high-risk AML at our institute.
Methods
Patients, treatment, and data collected:
The clinical leukemia database of Roswell Park Comprehensive Cancer Center was queried to identify newly diagnosed AML patients between 01/01/2008 and 12/31/2016. The study was approved by the institutional review board of the Roswell Park Comprehensive Cancer Center, Buffalo, NY and was carried out according to the principles of the Declaration of Helsinki. High-risk AML was defined as AML in a patient with prior history of cytotoxic chemotherapy (t-AML), myeloid malignancy (s-AML) like MDS or MPN, or the presence of cytogenetics indicative of AML-MRC as per the 2016 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia. Patients ≥ 60-yrs of age at the time of AML diagnosis meeting the above study criteria for high-risk AML were included. Patients receiving induction therapy with an infusional cytarabine and anthracycline containing IC backbone or HMA (decitabine or azacitidine) were included. Additional therapies administered on- or off- clinical trial, were allowed as long as the backbone remained IC or HMA therapy. Patients with acute promyelocytic leukemia (APL), history of suspected but unconfirmed MDS or MPN prior to development of AML, and those with presence of ≥ 50% dysplastic cells in at least 2 cell lines in bone marrow specimen but without poor risk cytogenetics were excluded. Baseline characteristics included demographics, hematologic parameters, blast counts, mutational status of fms-like tyrosine kinase 3 (FLT3) and nucleophosmin (NPM1), comorbidities, and Eastern Cooperative Oncology Group (ECOG) performance status scores were recorded. Comorbidity burden was derived using online calculators for Charlson Comorbidity Index (CCI), Hematopoietic Cell Transplantation-Comorbidity Index (HCT-CI), and treatment related mortality (TRM) scoring systems. These scores were dichotomized as low (CCI: ≤ 1, TRM: < 7, and HCT-CI: ≤ 2) or high (CCI: ≥ 2, TRM: ≥ 7, and HCT-CI: ≥ 3).
Efficacy and mortality endpoints:
All patients who received at least one cycle of IC or HMA therapies were included in the efficacy and mortality analysis. For efficacy, the primary endpoint was overall survival (OS). Secondary endpoints included composite complete response rates (CR: complete response + complete remission with incomplete hematologic recovery), duration of remission (DOR), and proportion of patients receiving allogeneic stem cell transplantation (alloSCT). Treatment response was assessed using the 2003 revised International Working Group response criteria[8]. Mortality end points included mortality rates at 30-days, 180-days, 1-yr, and 2-yrs from diagnosis.
Statistical analysis:
Baseline imbalances between the therapy groups were assessed using descriptive statistics. Between-treatment differences of categorical factors and continuous variables were compared using Fisher’s exact test and Wilcoxon rank sum test respectively. Logistic regression model was used to assess effect of therapies on complete response. This effect was described using odds ratio along with 95% CI estimates. Mortality from therapies were compared using Fischer’s test at the above stated time-points; those alive who had not reached the above mentioned specific time points were excluded from analysis. The therapy effects on OS were described using proportional hazards modeling with and without alloSCT as a time-dependent covariate. OS was calculated in months from the date of diagnosis to the date of death from any cause. For patients who achieved CR, DOR was defined as the time from CR to relapse or death, whichever was earlier. Patients alive were censored at the time of their last follow-up. Time-to-event outcomes (OS and DOR) were also described with Kaplan–Meier curves and the therapy differences were assessed using the log rank test. Median survival times were estimated by the reverse Kaplan–Meier method.
Multivariable models were obtained by reducing a full model containing several patient and disease characteristics as possible confounders of the treatment effect estimate. These factors were eliminated from the model using backward selection with a P value retention threshold of 0.30. The induction therapy indicator was retained regardless of P value.
The results of this single-institution, convenience sample study were considered hypothesis generating only. P values <0.05 were considered statistically significant. No multiple testing adjustments were performed to control the overall Type I error rate. All statistical analyses were performed using SAS/STAT software version 9.4 (Copyright 2012, SAS Institute Inc., Cary, NC).
Results
Baseline characteristics:
A total of 415 patients ≥ 60 years of age at the time of diagnosis were seen at the center during the study time frame. Of these, 201 patients (48.4%) met criteria for inclusion in the study; 98 patients received IC while 103 patients received HMA as induction therapy (Table 1). The median age of the patients was 68 years in IC cohort and 74 years in the HMA cohort (p<0.01). The median white blood count (6.2 x 109/L for IC vs. 3.9 x 109/L for HMA; p=0.01) and marrow blast burden (53.4% for IC vs. 43% for HMA; p=0.0017) differed statistically significantly between the two groups but the difference between the peripheral blast burden (18% for IC vs. 11% for HMA; p=0.11) did not reach statistical significance. A very small fraction of the patients had mutated FLT3 (fms-like tyrosine kinase 3; 6.3% vs. 4.4%; p=0.02) or NPM1 (nucleophosmin; 5.8% vs. 2.6%; p=0.05). Almost half (48%) of the patients in the IC cohort had s-AML in comparison to 31% in the HMA (p=0.01). On the contrary, the IC cohort had less patients with t-AML (25% vs. 45%; p=0.01) or AML-MRC (62% vs. 73%; p=0.18) than the HMA cohort. Similarly the IC cohort had fewer patients with complex karyotype (49% vs. 58%; p=0.19) or monosomal karyotype (24% vs. 48%; p<0.01). Amongst the HMA cohort, 34% received azacitidine while 66% received decitabine as induction HMA therapy. Patients in the IC cohort tended to have lower comorbidity burden as compared to those in the HMA cohort (Table 1) as determined using the HCT-CI (median score of 3 in IC vs. 4 in HMA cohort; p=0.03) and CCI scoring models (56% in IC cohort had score of 0 or 1 vs. 37% in HMA cohort; p=0.01). A similar trend was noted using the TRM model but did not reach significance (median score of 7.4 in IC cohort vs. 8.6 in HMA cohort; p=0.29).
Table 1:
Baseline characteristics including reasons for consideration as high-risk AML, cytogenetic make-up, hematologic parameters, mutation profile, specific HMA therapy administered, and comorbidity burden of patients included in the study
| IC | HMA | p | |
|---|---|---|---|
| Pts | 98 | 103 | |
| Gender (M/F) | 69/29 | 65/38 | 0.27 |
| Median age (years) | 68 (60–85) | 74 (63–93) | < 0.01 |
| High-risk AML due to: | |||
| antecedent MDS/MPN (s-AML) | 47 (48%) | 32 (31%) | 0.01 |
| prior chemotherapy (t-AML) | 26 (27%) | 46 (45%) | 0.01 |
| myelodysplasia related changes (AML-MRC) | 61 (62%) | 75 (73%) | 0.18 |
| Cytogenetics: | |||
| complex karyotype (CK) | 48 (49%) | 60 (58%) | 0.19 |
| monosomal karyotype (MK) | 24 (24%) | 49 (48%) | < 0.01 |
| Hematologic parameters (median): | |||
| White blood count (x 109/L) | 6.2 (0.6–222.7) | 3.9 (0.5–118.0) | 0.01 |
| Peripheral blood blasts (%) | 18 (0–99) | 11 (0–95) | 0.11 |
| Marrow blasts (%) | 53.4 (18–96) | 43 (10–91) | 0.0017 |
| Hemoglobin (mg/dL) | 8.9 (4.7–17.0) | 8.8 (4.7–12.4) | 0.43 |
| Platelets (x 109/L) | 67 (5–696) | 48 (5–887) | 0.19 |
| Mutation profile: | |||
| FLT3 (fms-like tyrosine kinase 3) mutation | 6/96 (6.3%) | 4/91 (4.4%) | 0.02 |
| NPM1 (nucleophosmin) mutation | 5/86 (5.8%) | 2/78 (2.6%) | 0.05 |
| Induction HMA therapy with: | |||
| azacitidine | N.A. | 35 (34%) | |
| decitabine | N.A. | 68 (66%) | |
| Treatment Related Mortality (TRM); median (IQR1-IQR3) | |||
| considering all cases as “secondary AML” | 7.4 (3.37–15.56) |
8.6 (5.13–14.71) |
0.29 |
| considering s-AML/t-AML as “secondary AML” | 6.47 (3.18–13.71) |
7.34 (4.42–13.84) |
0.24 |
| Charlson Comorbidity Index (CCI) | |||
| 0 or 1 | 55 (56%) | 38 (37%) | 0.01 |
| ≥ 2 | 43 (44%) | 65 (63%) | |
| Hematopoietic Cell Transplantation-Comorbidity Index (HCT-CI); median (IQR1-IQR3) | 3 (1–5) | 4 (2–5) | 0.03 |
Overall comparison of patient outcomes:
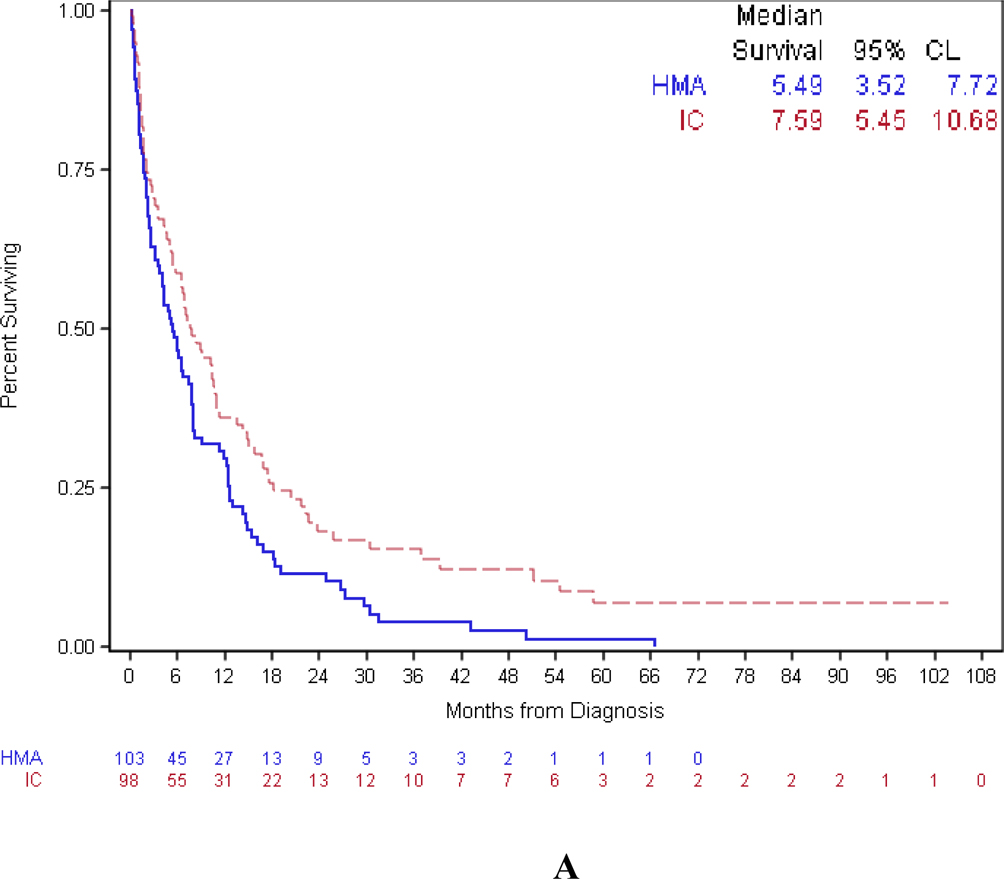
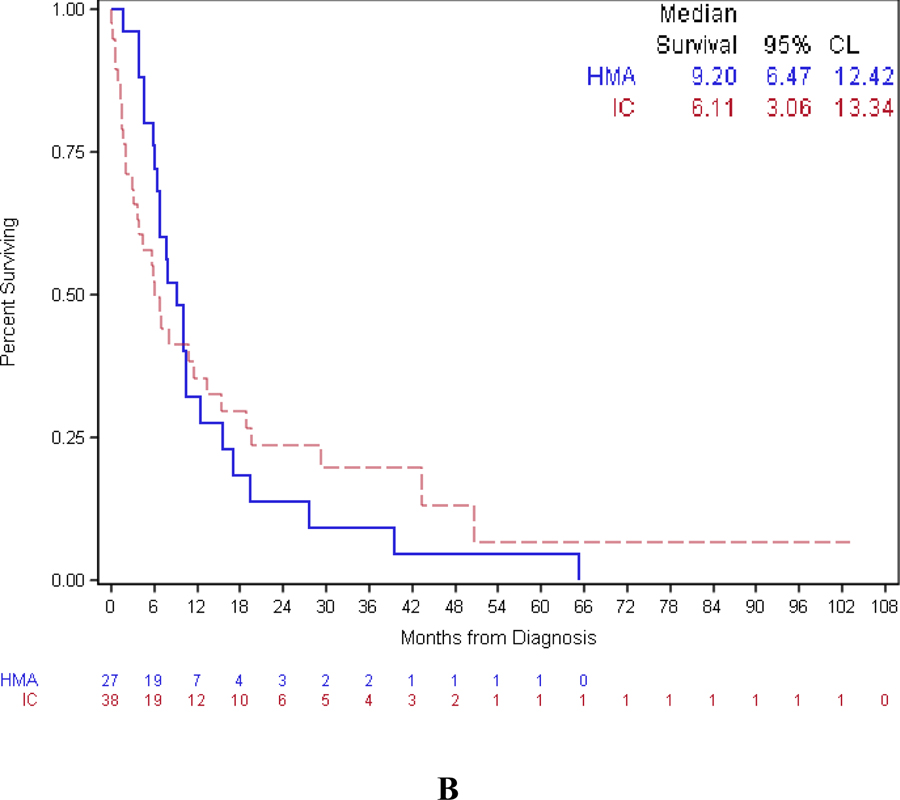
Composite complete remission rates (CR) were 39% in the IC and 27% in the HMA cohorts (p=0.10) (Table 2). More patients in the IC cohort underwent alloSCT as compared to the HMA cohort (33% vs. 5%; p<0.01). As shown in Figure 1, the median DOR was numerically smaller in the IC cohort as compared to the HMA cohort (6.11 mos vs. 9.20 mos) but was not statistically significant. Kaplan Meier estimated OS analysis demonstrated that IC treated patients had prolonged, but not statistically significantly different, mOS than those receiving HMA (7.59 mos vs. 5.49 mos; HR 0.75 95% CI 0.55–1.02; p=0.07 using Cox proportional hazards modelling). The OS and DOR were comparable in patients who received azacitidine vs. decitabine as shown in supplementary figure 1.
Table 2:
Composite complete response (CR) rates, allogeneic stem-cell transplant rates, and mortality from acute myeloid leukemia (AML) directed therapies at specific time-points. Patients alive who had not reached the above mentioned specific time points were excluded from analysis for mortality at time-points analysis.
| IC | HMA | p | |
|---|---|---|---|
| Composite CR: | |||
| Overall | 38 (39%) | 28 (27%) | 0.1 |
| High-risk AML due to: | |||
| antecedent MDS/MPN (s-AML) | 16/47 (34%) | 9/32 (28%) | 0.58 |
| prior chemotherapy (t-AML) | 11/26 (42%) | 11/46 (24%) | 0.10 |
| myelodysplasia related changes (AML-MRC) | 20/61 (33%) | 21/74 (28%) | 0.58 |
| Cytogenetics: | |||
| complex karyotype (CK) | 13/25 (52%) | 4/16 (25%) | 0.09 |
| monosomal karyotype (MK) | 5/23 (22%) | 14/44 (32%) | 0.57 |
| AlloSCT | 32 (33%) | 5 (5%) | <0.01 |
| Mortality at time-points: | |||
| 30 days | 9.2% | 14.7% | 0.28 |
| 180 days | 43.6% | 54.5% | 0.15 |
| 1-yr | 66.3% | 72.2% | 0.43 |
| 2-yrs | 85.4% | 89.6% | 0.5 |
Figure 1:
Kaplan-Meier curves for OS (A) and DOR (B). IC led to an improved OS but results did not reach statistical significance (p=0.07). DOR, similarly, was not statistically different for patients in the two therapy cohorts. OS: overall survival; DOR: duration of response; IC: intensive chemotherapy.
Analysis of mortality from therapies:
Mortality from any cause was not significantly different between the IC and HMA cohorts at 30 days (9.18% vs. 14.7%; p=0.28) and 180 days (43.6% vs. 54.5%; p=0.15). This trend was noted even at 1-yr and 2-yr time-points (Table 2) despite much smaller differences and patient numbers. The causes of mortality at 30 days and 180 days are shown in supplementary figure 2.
Subgroup analysis:
Analysis of outcomes by specific subsets of high risk AML (specifically s-AML, t-AML, AML-MRC, CK+ AML, and MK+ AML) showed no statistically significant difference in composite complete remission rates between the two cohorts (supplementary table 1). The odds of achieving CR were significantly higher only in patients older than 70 years of age who received IC as compared to HMA (OR 2.79; 95% CI 1.17 to 6.60). Patients with t-AML (HR 0.56; 95% CI 0.33 to 0.97) and CK+MK− AML (HR 0.37; 95% CI 0.19 to 0.75) had better OS with IC compared to HMA therapies. Patients with CK+MK+ AML, however, noted improved OS with HMA therapy (HR 2.00; 95% CI 1.08 to 3.70).
Multivariable analysis:
Cox proportional hazards modelling was performed to ascertain the effect of therapy on OS. Factors well known to affect outcomes in AML including age, transplant status, ECOG performance status, and comorbidity burden (CCI) were adjusted as shown in Table 3. CCI based comorbidity burden was the only risk factor that affected OS in a statistically significant manner.
Table 3:
Multivariable regression analysis of prognostic risk factors for overall survival. Only CCI reached statistical significance. CCI: Charlson Comorbidity Index; CI: confidence interval; ECOG-PS: Eastern Cooperative Oncology Group performance status scores; HMA: Hypomethylating agent; HR: hazard ratio; IC: Intensive chemotherapy
| Risk | HR (95% CI) | p |
|---|---|---|
| IC vs. HMA | 0.84 (0.56 to 1.07) | 0.31 |
| Allogeneic stem-cell transplant | 0.67 (0.41 to 1.11) | 0.12 |
| ECOG-PS >1 vs. ≤ 1 | 1.17 (0.81 to 1.68) | 0.39 |
| CCI ≤ 1 vs. ≥ 2 | 0.72 (0.53 to 0.98) | 0.04 |
| Age | 1.02 (0.99 to 1.04) | 0.14 |
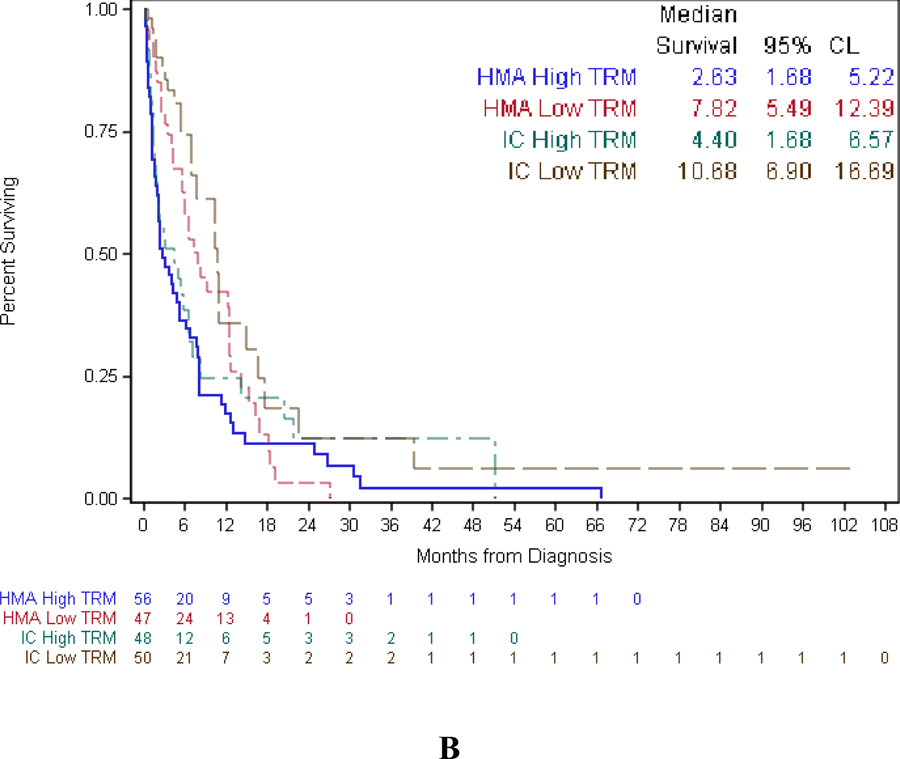
Impact of comorbidities on patient survival:
The effects of adjustment for ECOG performance status, age, and comorbidity burden on the overall survival are demonstrated in Table 4. Patients with t-AML (HR 0.46; 95% CI 0.25 to 0.87) maintained their survival advantage with IC therapy while the statistical significance in favor of IC for the CK+MK− patients was lost (HR 0.50 95% CI 0.22 to 1.11). CK+MK+ AML patients maintained their survival advantage with HMA therapy (HR 2.57 95% CI 1.26 to 5.22). As shown in Figure 2, patients with lower comorbidity burden tended to have better OS than those with higher comorbidity burden across all the modeling systems.
Table 4:
Overall survival of patients (IC vs. HMA) by proportional hazards model using alloSCT as a time-dependent covariate since diagnosis. AML: Acute myeloid leukemia; AML-MRC: AML with myelodysplasia-related changes; CCI: Charlson Comorbidity Index; CI: confidence interval; CK: complex karyotype; ECOG-PS: Eastern Cooperative Oncology Group performance status scores; HMA: Hypomethylating agent; HR: hazard ratio; IC: Intensive chemotherapy; MK: monosomal karyotype; s-AML: secondary AML; t-AML: therapy related AML
| No additional adjustment | Adjusted for ECOG, CCI, and age | |
|---|---|---|
| HR (95% CI) | ||
| Overall population | 0.75 (0.55–1.02) | 0.84 (0.60–1.16) |
| Age group (yrs): | ||
| 60–64 | 0.90 (0.33–2.42) | 1.23 (0.40–3.79) |
| 65–69 | 1.06 (0.55–2.06) | 1.35 (0.67–2.70) |
| 70–95 | 0.67 (0.43–1.03) | 0.77 (0.48–1.22) |
| Type of AML: | ||
| s-AML | 0.96 (0.58–1.59) | 1.17 (0.65–2.10) |
| t-AML | 0.56 (0.33–0.97) | 0.46 (0.25–0.87) |
| AML-MRC | 0.82 (0.56–1.20) | 0.93 (0.63–1.38) |
| Cytogenetics: | ||
| CK+MK− | 0.37 (0.19–0.75) | 0.50 (0.22–1.11) |
| CK+MK+ | 2.00 (1.08–3.70) | 2.57 (1.26–5.22) |
Figure 2:
Kaplan-Meier curves for OS based on therapies and comorbidity burden using CCI (A) and TRM (B) scoring models. Patients with less comorbidity burden had better OS. OS: Overall survival; CCI: Charlson Comorbidity Index; TRM: therapy related mortality
Discussion
The dismal results of IC in adults with secondary or high-risk AML is well known. These outcomes, specifically low CR rates and short disease free survival (DFS), and OS were first reported nearly three decades ago in AML patients with a preleukemic syndrome treated with IC[9]. Multivariate analysis indicated that presence of antecedent preleukemic syndrome (mostly MDS) and age were independent poor prognostic indicators for achieving remission[9]. Attempts to improve these outcomes are exemplified by a large open-label phase III trial of amonafide L-malate plus cytarabine in patients with s-AML which turned out to be negative[10]. Because a substantial proportion of older adults with high risk AML have co-existent comorbidities and/or poor performance status at the time of diagnosis which preclude the use of IC, HMA therapy has emerged as the treatment of choice in many centers (including our own) for the care of elderly “unfit” AML patients. Multiple retrospective studies have sought to compare the outcomes of older AML patients receiving upfront IC vs. HMA[11–13]. While the results have varied somewhat, all of these analyses noted negligible absolute numerical differences in OS achieved using IC compared with HMA. However, because these studies were performed in unselected population of older AML, it is unclear if these results are relevant for specific clinical and/or biologic subsets of patients.
Given that high-risk AML patients (defined as s-AML, t-AML, or AML-MRC) fare especially poorly with IC, we performed this retrospective single institute study to compare the outcomes of IC vs. HMA induction therapy in these older patients. Of note, we did not include patients who met the WHO definition of AML-MRC solely because of ≥ 50% morphologic dysplasia since it is unclear if the survival outcomes are worse as a result[14]. Our results demonstrated no statistically significant difference in OS between patients treated with IC vs. HMA although there was a trend favoring the IC cohort. OS did not differ significantly even after accounting for comorbidity scores, suggesting that high risk older AML with lower comorbidity burdens may be appropriate for HMA in the absence of alloSCT option. Higher treatment related mortality in the HMA cohort most likely reflects the more advanced age and higher comorbidity burdens than the IC cohort as this was significantly different between the two groups. Although there was a survival advantage for IC in t-AML and for HMA in AML with CK+MK+, the reasons for this are not clear. Still, the majority of the AML patients, either with t-AML or MK AML, received HMA in comparison to IC, probably because they were unfit for more intensive treatments, and the therapeutic approach with HMA was considered milder than and as effective as possible. Information on the mutational profile of these patients aside from FLT-3 and NPM-1 was not available. As the mutation profiles of s-AML and t-AML patients are known to be different, this may have potentially played a role in our study findings[15].
It is pertinent to note the results of two prior retrospective studies of outcomes in elderly high-risk AML patients. In a French study, the mOS with IC and HMA (all azacitidine) were also similar at 9.6 and 10.8 months respectively (p=0.899)[16]. Researchers from the University of Texas MD Anderson Cancer Center (MDACC) examined the outcomes of five treatment cohorts (IC, HMA, liposomal cytarabine and daunorubicin (CPX-351), low dose cytarabine (LDAC), and investigational agents)[17]. The mOS in the IC, HMA, and LDAC cohorts were 5.4 mos, 6.7 mos, and 7.1 mos respectively and were statistically significantly different favoring the latter two groups. The authors concluded that lower intensity approaches (HMA or LDAC) were associated with lower early mortality rates and improved OS in comparison with intensive regimens. However, all three of these retrospective studies (including our own) treated significantly different patients with IC versus HMA therapy as reflected by the significantly different median ages and rates of subsequent alloSCT between the two cohorts reflecting physician treatment selection bias. Furthermore, the effects of additional therapies administered on the backbone of the IC or HMA therapies cannot be ascertained. In our study, for example, 9 patients in each cohort (Table 5) received additional AML directed therapy on the backbone of IC (9.2%) or HMA (8.7%). In the MDACC study, the number of patients who received additional therapies was markedly higher. IC cohort was highly heterogeneous while 61.5% (136 of 221 patients) in the HMA cohort and virtually all patients in the LDAC cohort received additional AML directed therapies which may have contributed to their improved outcomes[17].
Table 5:
Addition therapies received on backbone of primary induction therapy. HMA: Hypomethylating agent; IC: Intensive chemotherapy; SMAC: second mitochondrial-derived activator of caspases
| Therapy class | IC (n=98) | HMA (n=103) |
|---|---|---|
| Proteasome inhibitor | 5 | 5 |
| SMAC mimetic | 0 | 1 |
| Antibody-drug conjugate | 0 | 3 |
| Hedgehog inhibitor | 2 | 0 |
| HMA priming | 2 | 0 |
Of note, our analysis only evaluated patients treated at our institute between 2008 and 2016. In Aug 2017, CPX-351, a liposomal formulation of cytarabine and daunorubicin packaged at a 5:1 molar ratio (Vyxeos™; Jazz Pharmaceuticals), was approved for treatment of high risk patients including t-AML or AML-MRC. Approval was based on results in 309 older patients in a phase III trial[18]. In comparison to traditional “7+3” regimen, CPX-351 improved median OS (OS 9.56 vs. 5.95 mos; HR=0.69; p=0.005), event-free survival (HR=0.74; p=0.021), complete remission rate (47.7% vs. 33.3%; p=0.016) as well as 60-day mortality (13.7% vs. 21.2%). The impressive outcomes notwithstanding, grade 3–5 AEs were equal between the two arms (92% vs. 91%). Therefore we were unable to determine how the use of CPX-351 in place of standard 7+3 infusional cytarabine and daunorubicin could have impacted on outcomes of the IC treated patients. However, in our study, the OS in the IC cohort (median 7.59 mos, 95% CI 5.45–10.69) was similar to that obtained by CPX-351 treated patients (median 9.56, 95% CI 6.60. 11.86) and higher than that achieved by the 7+3 patients (median 5.95 mos, 95% CI 4.99, 7.75) on the phase III clinical trial, thereby serving as an indirect external validation of our study findings[18]. Unlike the phase 3 trial, we also included s-AML patients with previous history of MPN in our analysis. Given these differences and the limitations inherent to retrospective analyses, any conclusions about the potential outcomes of IC (either 7+3 or CPX-351) compared to HMA in older high-risk AML patients should be interpreted cautiously in the absence of a randomized clinical trial.
In conclusion, the overall survival of older AML patients with high-risk AML remains dismal and continues to be an area of significant unmet need. Although the recent approval of CPX-351 is a welcome addition to our treatment arsenal, this drug still represents a formulation of cytarabine and daunorubicin with similar rate of high-grade toxicities as traditional “7+3” regimen. Based on our data, HMA therapy constitutes a valid induction treatment option with potentially similar survival results as IC and should be highly considered as frontline therapy in older high-risk AML patients with high comorbidity burden or when alloSCT is not an option. It is important to not restrict alloSCT for fit patients based on age alone since it remains the only curative option[19]. Efforts to bridge older patients to this endpoint should be highly pursued. Additionally, clinical trial participation should be highly encouraged in order to gain any additional therapeutic benefits. Recently newer epigenetic therapies including SGI-110 (guadecitabine, Astex/Otsuka Pharmaceuticals) have shown markedly better CR rates as compared to that achieved with historical decitabine or azacitidine alone in single arm studies for newly diagnosed unfit AML[20]. If this improvement is confirmed in phase III clinical trial (ClinicalTrials.gov Identifier: NCT02348489) along with demonstration of low or similar rate of toxicities as decitabine or azacitidine, then SGI-110 could well replace these other agents as the new standard of care HMA for newly diagnosed older AML patients. In this context, eventually prospective studies comparing SGI-110 therapy against CPX-351 may be warranted to reflect current practice. Other less intensive approaches like immune checkpoint inhibitors and targeted therapies are currently under investigation in various subtypes of AML. Although very exciting conceptually, their role in high-risk AML will need more elucidation. In the present day, given the possibility of equivalency of IC and HMA outcomes in these patients, the likelihood of alloSCT and the effects of therapies (IC or HMA) on quality of life (QoL) may be the deciding factors for treating providers in selecting a treatment regimen. The effect on QoL is especially important because the survival advantage achieved with IC over less intensive approaches is not always clinically relevant.. Results from a large multicenter prospective study may help compare the therapy related QoL changes.
Supplementary Material
Acknowledgements:
This work was supported by National Cancer Institute (NCI) grant P30CA016056 involving the use of Roswell Park Comprehensive Cancer Center’s Biostatistics Shared Resource and Pathology Resource Network (Hematologic Procurement Shared Resource). ES Wang is also supported by the RPCI Alliance Foundation (Jacquie Hirsch Leukemia Research Fund).
Financial support: No financial support was utilized in the preparation of this manuscript.
Footnotes
Conflict of interest disclosure: The authors have no relevant conflicts of interest to report.
REFERENCES
- [1].Dohner H, Weisdorf DJ, Bloomfield CD, Acute Myeloid Leukemia, The New England journal of medicine 373(12) (2015) 1136–52. [DOI] [PubMed] [Google Scholar]
- [2].Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, Wheatley K, Harrison CJ, Burnett AK, Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials, Blood 116(3) (2010) 354–65. [DOI] [PubMed] [Google Scholar]
- [3].Fang M, Storer B, Estey E, Othus M, Zhang L, Sandmaier BM, Appelbaum FR, Outcome of patients with acute myeloid leukemia with monosomal karyotype who undergo hematopoietic cell transplantation, Blood 118(6) (2011) 1490–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Medeiros BC, Othus M, Fang M, Roulston D, Appelbaum FR, Prognostic impact of monosomal karyotype in young adult and elderly acute myeloid leukemia: the Southwest Oncology Group (SWOG) experience, Blood 116(13) (2010) 2224–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Breems DA, Van Putten WL, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KB, Mellink CH, Nieuwint A, Jotterand M, Hagemeijer A, Beverloo HB, Lowenberg B, Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype, Journal of clinical oncology : official journal of the American Society of Clinical Oncology 26(29) (2008) 4791–7. [DOI] [PubMed] [Google Scholar]
- [6].Arber DA, Orazi A, Hasserjian R, Thiele J, Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M, Vardiman JW, The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia, Blood 127(20) (2016) 2391–405. [DOI] [PubMed] [Google Scholar]
- [7].Patel SS, Radivoyevitch T, Gerds AT, Majhail NS, Carraway HE, Advani AS, Nazha A, Maciejewski JP, Kalaycio M, Sekeres MA, Mukherjee S, Forty-Year Analysis of Randomized Clinical Trials in Patients with Acute Myeloid Leukemia Treated with Remission Induction Chemotherapy, Blood 128 (2016). [Google Scholar]
- [8].Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH, Schiffer CA, Doehner H, Tallman MS, Lister TA, Lo-Coco F, Willemze R, Biondi A, Hiddemann W, Larson RA, Lowenberg B, Sanz MA, Head DR, Ohno R, Bloomfield CD, Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia, Journal of clinical oncology : official journal of the American Society of Clinical Oncology 21(24) (2003) 4642–9. [DOI] [PubMed] [Google Scholar]
- [9].Gajewski JL, Ho WG, Nimer SD, Hirji KF, Gekelman L, Jacobs AD, Champlin RE, Efficacy of intensive chemotherapy for acute myelogenous leukemia associated with a preleukemic syndrome, Journal of clinical oncology : official journal of the American Society of Clinical Oncology 7(11) (1989) 1637–45. [DOI] [PubMed] [Google Scholar]
- [10].Stone RM, Mazzola E, Neuberg D, Allen SL, Pigneux A, Stuart RK, Wetzler M, Rizzieri D, Erba HP, Damon L, Jang JH, Tallman MS, Warzocha K, Masszi T, Sekeres MA, Egyed M, Horst HA, Selleslag D, Solomon SR, Venugopal P, Lundberg AS, Powell B, Phase III open-label randomized study of cytarabine in combination with amonafide L-malate or daunorubicin as induction therapy for patients with secondary acute myeloid leukemia, Journal of clinical oncology : official journal of the American Society of Clinical Oncology 33(11) (2015) 1252–7. [DOI] [PubMed] [Google Scholar]
- [11].Quintas-Cardama A, Ravandi F, Liu-Dumlao T, Brandt M, Faderl S, Pierce S, Borthakur G, Garcia-Manero G, Cortes J, Kantarjian H, Epigenetic therapy is associated with similar survival compared with intensive chemotherapy in older patients with newly diagnosed acute myeloid leukemia, Blood 120(24) (2012) 4840–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Gupta N, Miller A, Gandhi S, Ford LA, Vigil CE, Griffiths EA, Thompson JE, Wetzler M, Wang ES, Comparison of epigenetic versus standard induction chemotherapy for newly diagnosed acute myeloid leukemia patients >/=60 years old, American journal of hematology 90(7) (2015) 639–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sorror ML, Storer BE, Elsawy M, Fathi AT, Brunner AM, Gerds AT, Sekeres MA, Mukherjee S, Medeiros BC, Wang ES, Vachhani P, Shami PJ, Peña E, Wardyn S, Whitten J, Moore R, Becker PS, McCune J, Lee SJ, Sandmaier BM, Appelbaum FR, Estey EH, Intensive Versus Non-Intensive Induction Therapy for Patients (Pts) with Newly Diagnosed Acute Myeloid Leukemia (AML) Using Two Different Novel Prognostic Models, Blood 128 (2016). [Google Scholar]
- [14].Miesner M, Haferlach C, Bacher U, Weiss T, Macijewski K, Kohlmann A, Klein HU, Dugas M, Kern W, Schnittger S, Haferlach T, Multilineage dysplasia (MLD) in acute myeloid leukemia (AML) correlates with MDS-related cytogenetic abnormalities and a prior history of MDS or MDS/MPN but has no independent prognostic relevance: a comparison of 408 cases classified as “AML not otherwise specified” (AML-NOS) or “AML with myelodysplasia-related changes” (AML-MRC), Blood 116(15) (2010) 2742–51. [DOI] [PubMed] [Google Scholar]
- [15].Lindsley RC, Mar BG, Mazzola E, Grauman PV, Shareef S, Allen SL, Pigneux A, Wetzler M, Stuart RK, Erba HP, Damon LE, Powell BL, Lindeman N, Steensma DP, Wadleigh M, DeAngelo DJ, Neuberg D, Stone RM, Ebert BL, Acute myeloid leukemia ontogeny is defined by distinct somatic mutations, Blood 125(9) (2015) 1367–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Dumas PY, Bertoli S, Berard E, Mediavilla C, Yon E, Tavitian S, Leguay T, Huguet F, Forcade E, Milpied N, Sarry A, Sauvezie M, Bories P, Pigneux A, Recher C, Azacitidine or intensive chemotherapy for older patients with secondary or therapy-related acute myeloid leukemia, Oncotarget 8(45) (2017) 79126–79136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Boddu PC, Kantarjian HM, Ravandi F, Garcia-Manero G, Verstovsek S, Jabbour EJ, Takahashi K, Bhalla K, Konopleva M, DiNardo CD, Ohanian M, Pemmaraju N, Jain N, Pierce S, Wierda WG, Cortes JE, Kadia TM, Characteristics and outcomes of older patients with secondary acute myeloid leukemia according to treatment approach, Cancer 123(16) (2017) 3050–3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Lancet JE, Uy GL, Cortes JE, Newell LF, Lin TL, Ritchie EK, Stuart RK, Strickland SA, Hogge D, Solomon SR, Stone RM, Bixby DL, Kolitz JE, Schiller GJ, Wieduwilt MJ, Ryan DH, Hoering A, Banerjee K, Chiarella M, Louie AC, Medeiros BC, CPX-351 (cytarabine and daunorubicin) Liposome for Injection Versus Conventional Cytarabine Plus Daunorubicin in Older Patients With Newly Diagnosed Secondary Acute Myeloid Leukemia, Journal of clinical oncology : official journal of the American Society of Clinical Oncology 36(26) (2018) 2684–2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Pratz KW, Levis M, How I treat FLT3-mutated AML, (2017). [DOI] [PMC free article] [PubMed]
- [20].Kantarjian HM, Roboz GJ, Kropf PL, Yee KWL, O’Connell CL, Tibes R, Walsh KJ, Podoltsev NA, Griffiths EA, Jabbour E, Garcia-Manero G, Rizzieri D, Stock W, Savona MR, Rosenblat TL, Berdeja JG, Ravandi F, Rock EP, Hao Y, Azab M, Issa JJ, Guadecitabine (SGI-110) in treatment-naive patients with acute myeloid leukaemia: phase 2 results from a multicentre, randomised, phase 1/2 trial, The Lancet. Oncology 18(10) (2017) 1317–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.