Abstract
Introduction
Although residents are on the front lines of patient care, they enter few formal patient safety reports on the adverse events and near misses they witness. Demonstrating the rationale and mechanics of reporting may improve this.
Methods
We designed and implemented an escape room patient safety simulation to incorporate active learning, gamification, and adult learning theory into intern patient safety onboarding. Interns from all sponsoring institution programs participated, identifying, mitigating, and reporting a range of patient safety hazards. Props and faculty time were the major resources required.
Results
One hundred twenty interns participated in this simulation in June 2018. Forty-one percent reported previous training on reporting errors, and only 5% had previously entered an event report. Average confidence in ability to identify patient safety hazards improved after the simulation from 6.35 to 8.00 on a 10-point rating scale. The simulation was rated as relevant or highly relevant to practice by 96% of interns.
Discussion
Several factors contribute to a low error-reporting rate among house staff. We developed a simulation modeled on popular escape room activities to increase awareness of safety hazards and ensure familiarity with the actual online reporting system our interns will use in the clinical environment.
Keywords: Patient Safety, Simulation, Gamification, Risk Management, Error Reporting, Event Reporting
Educational Objectives
After completing this session, learners will be able to:
-
1.
Identify and mitigate patient safety hazards.
-
2.
Enter an event report using an online event-reporting system.
-
3.
Apply teamwork skills to address patient safety issues.
Introduction
Teaching patient safety and error reporting to graduate medical education audiences is challenging. Students and residents are on the front lines of care, which demands training in pertinent safety practices including how to use voluntary error-reporting systems.1–3 If effectively engaged, learners can provide critical information to better identify the drivers of patient harm.4,5 Unfortunately, resident and fellow physicians rarely submit incident reports. The Accreditation Council for Graduate Medical Education clinical learning environment report found that few resident trainees appreciated the benefits of this practice.6 On a more local front, a survey of house staff at Thomas Jefferson University Hospital identified a lack of comfort with how to report an error and what to actually report as significant barriers to reporting, especially for learners in their first year of graduate training.
To engage incoming PGY 1 trainees during orientation to our local safety priorities and the use of our voluntary reporting system, we created a version of a simulated escape room. We hypothesized that creating a patient safety escape room simulation would allow us to address the aforementioned learning objectives more effectively than a simple didactic through the incorporation of active learning and gamification. The decision to use the escape room as the educational medium for this initiative was rooted in adult learning theory. Escape rooms are live-action, team-based games where players must work together, solve clues, and complete a series of mind-bending, fitness-challenging tasks to escape the room in less than 60 minutes.7
Participatory learning experiences such as the escape room8 engage adults both cognitively and affectively. Adults are experiential learners and learn from active participation in, and reflection on, a specific activity or experience. Kolb breaks down experiential learning into four discrete stages: concrete experience, observations and reflections, formalization/generalizations of concepts, and testing concepts in new situations.9 These stages of the learning cycle can be further simplified into the stages of feeling, watching, thinking, and doing, respectively.10 By actively participating in an escape room, the participant is engaged in a concrete experience and then has the opportunity to reflect on that experience in the form of debriefing, which assists in forming a generalization of the experience. Generalizations can then be applied to new situations, as the learning cycle repeats. Escape rooms, which can be facilitated naturally through simulation, authentically support adult learning.9 Our simulation distinguishes itself from Zhang, Lee, Rodriguez, Rudner, Chan, and Papanagnou,8 who describe the onetime use of a commercial escape room experience to foster team-building skills. Our simulation is also different from the patient safety room of horrors of Farnan et al.11 in that, instead of individually and statically identifying safety hazards, our learners actively work in teams to identify and mitigate hazards while solving a puzzle and actively practice entering an error report to document their findings.
In our curriculum, interns from multiple specialties worked together to identify and mitigate patient safety hazards that could potentially be encountered in hospitalized patients’ rooms and enter an error report to ultimately escape the room.
Methods
Development
A working group composed of faculty clinicians, simulation and patient safety experts, and medical education fellows developed two hospital-based cases. The working group identified hospital safety priorities and associated safety hazards by group consensus; standardized chart formatting and content; and aligned chart content, room setup, and patient safety hazards for each scenario. The implementation team also recruited and trained simulation facilitators.
We assigned 120 incoming interns to 16 teams, composed of seven to eight members per team. Teams participated in the escape room challenges as part of their required residency orientation in June 2018. The goal of the escape room was for each team to identify a predetermined set of serious patient safety hazards and successfully log them into the event-reporting system (CS STARS) within 20 minutes to successfully escape the room.
We conducted a pilot of the escape room activity during the week prior to orientation with 35 rising PGY 2 internal medicine (IM) residents to test proof of concept, evaluate necessary timing and flow, and solicit feedback from learners on necessary improvements.
Equipment
Two escape room cases were developed—one of a medical inpatient (the IM case) and the other of a critically ill patient in the emergency department (the emergency medicine [EM] case). See Appendix A for simulation guides and Appendices B and C for schematics and specific instructions on room setup. Because we had to accommodate a large number of learners, four rooms were needed—two for each case. We ran the simulations at our university's simulation center in mock hospital rooms.
Case 1 (IM) equipment list
-
•
Hospital bed.
-
•
Mannequin.
-
•
Computer (with internet connection to enter error report).
-
•
Sequential compression devices.
-
•
Isolation cart with only one gown left.
-
•
Opened lumbar puncture kit (with sharps removed for safety).
-
•
Identification bracelet.
-
•
Falls risk bracelet.
-
•
Adult diaper.
-
•
Yellow falls risk socks.
-
•
Urinal.
-
•
Soft wrist restraints.
-
•
Incentive spirometer.
-
•
Quick Response (QR) codes printed out on paper.
-
•
Door sign.
-
•
Paper chart (Appendix D: IM chart).
-
•
Clipboard with blank list for recording hazards and clues.
Case 2 (EM) equipment list
-
•
Hospital bed.
-
•
Mannequin (with endotracheal tube and central line).
-
•
Computer.
-
•
Ventilator.
-
•
IV pole.
-
•
Saline bag marked as penicillin.
-
•
Saline bag marked as sedation.
-
•
Saline bag marked as nitroglycerin.
-
•
Identification bracelet.
-
•
Allergy bracelet.
-
•
Falls risk bracelet.
-
•
Yellow falls risk socks.
-
•
QR codes printed out on paper.
-
•
Door sign.
-
•
Paper chart (Appendix E: EM chart).
-
•
Clipboard with blank list for recording hazards and clues.
Personnel
Each simulation room required one in-room facilitator as a timekeeper to ensure adequate progress toward the team's escape. (See Appendices F and G for facilitator versions of charts.) A second observer was situated in the simulation control room to accurately evaluate the learning activity. This second observer is not mandatory for the implementation of the simulation. Two supervisors (referred to as traffic controllers) were present to orient each group on arrival and ensure smooth transitions between simulation rooms and then to the final debriefing room. Finally, two faculty cofacilitated closing debriefing sessions after each set of four learner groups completed their second simulation. To accommodate 120 learners in four simulations rooms and effectively debrief them, we required a total 12 facilitators. (See Appendix H for a description of facilitator roles.)
Implementation
During the room setup, we planted 14 patient safety hazards in the EM case and 18 in the IM case. We used QR codes to link a subset of these safety hazards to information sheets containing best practices for the associated safety priority. Three of the information sheets further contained clues. (See Appendix I for an example QR code with clue and teaching pearl; see Appendices B and C for specific instructions on setting up each room.) Clues were either the log-in, password, or patient identifier for the event-reporting system, all three of which were necessary to enter an event report. QR codes were revealed when team members took active steps to mitigate the hazards. For example, lowering a too-high bed to an appropriate height revealed a QR code on the wall behind the bed. Applying the sequential compression device to the mannequin revealed a QR code hidden inside the boot.
We generated QR codes using a free online program (https://www.qr-code-generator.com). Our patient safety office assisted us in creating dummy log-ins for the reporting system, enabling us to use the actual online system the interns would use in their real practice without our simulated error reports being aggregated as actual reports and sent to institutional safety officers.
Prior to the session, all learners heard a 15-minute didactic describing the institutional safety priorities (see Appendix J for the didactic template) and demonstrating the local event-reporting system, including how to navigate the site and how to complete the necessary fields. Setup for the four rooms required approximately 1 hour. We scheduled 16 randomly assigned, mixed-specialty teams of interns throughout the afternoon (Appendix K: sample schedule for 120 learners). Upon arrival, we verbally described the goals and objectives of the session. We explained the logistics and flow of the session and conducted a technology check, using a QR code linking to session instructions. Instructions were limited, asking only that teams identify safety hazards, write them down, and enter an event report containing the hazard list to escape. We described what information was necessary to enter an event report but withheld the association between QR codes and clues.
Groups completed their first case (20 minutes), debriefed on teamwork practices (10 minutes), completed the second case (20 minutes), and then attended the large-group debrief on safety concepts (30 minutes).
Assessment
This exercise was designed to be formative for participating interns. Learners completed pre- and postsurveys regarding their previous training in event reporting, their self-reported comfort with patient safety topics, and whether they had ever entered an event report (i.e., in medical school). Assessment of teams included how many hazards they identified and whether they successfully entered an event report (Appendices L and M).
The simulation exercise was evaluated in a multimodal fashion. We measured how many of the intended hazards were identified, whether additional hazards were noted, and whether teams were able to enter an event report. A voluntary session evaluation, adapted from Brookfield's Critical Incident Questionnaire, captured qualitative feedback about the session (Appendix N). Residents also provided comments recommending improvements for subsequent iterations.
Debriefing
After the first simulation, learners and observers completed a teamwork assessment for their group, using the Jefferson Teamwork Observation Guide (JTOG; Appendix O). We used the JTOG responses to prompt discussion of team dynamics during the debriefing after the first case.
Upon completion of both escape rooms, teams reported to a large conference room for a group debriefing, cofacilitated by two faculty members. The goal for this debriefing was to highlight any trends and observations across groups. The cofacilitators used an objective-oriented approach to their facilitation, focusing on patient safety concerns and teamwork skills.
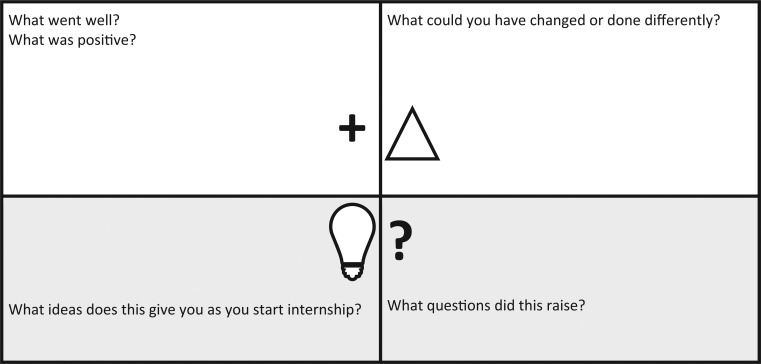
The feedback capture grid (Figure) guided the debriefing. Cofacilitators made use of a dry-erase board in the conference room to capture comments made by resident participants. The debriefing began with a focus on behaviors that were helpful (to reinforce these behaviors); this developed into a conversation on what could have been improved or performed differently to optimize results. Residents commented on any ideas, innovations, or interventions applicable to their internship. Finally, cofacilitators captured questions that came up during the debriefing in the grid's questions quadrant to provide answers and appropriate links to resources.
Figure.
Feedback capture grid for large-group debriefing.
Results
Table 1 shows participant characteristics, including whether learners had received prior training in event reporting and whether they had previously submitted an event report.
Table 1. Participant Characteristics.
| Specialty | No. (%) of PGY 1s Responding | Received Prior Training in Event Reporting | Previously Entered an Event Report |
|---|---|---|---|
| Anesthesiology | 9 (90) | 5 | 0 |
| Emergency medicine | 12 (86) | 1 | 0 |
| Otolaryngology | 3 (60) | 1 | 0 |
| Family medicine | 8 (80) | 5 | 1 |
| Internal medicine | 28 (76) | 17 | 0 |
| Neurology | 8 (89) | 2 | 1 |
| Pediatric neurology | 1 (100) | 1 | 0 |
| Neurosurgery | 1 (33) | 0 | 0 |
| Obstetrics and gynecology | 4 (57) | 1 | 0 |
| Orthopedics | 3 (50) | 2 | 0 |
| Pediatrics | 13 (59) | 5 | 2 |
| Psychiatry | 8 (100) | 3 | 0 |
| General surgery | 7 (70) | 0 | 0 |
| No specialty selected | 1 (N/A) | 0 | 0 |
| Total | 106 (75) | 44a | 5b |
41% of respondents.
5% of respondents.
Participants were asked to rate their confidence in their abilities to identify patient safety hazards both before and after the session. A total of 106 interns completed the presurvey, and 102 interns completed the postsurvey. Mean confidence prior to the session on a 10-point scale (1 = low confidence, 10 = high confidence) was 6.35 and improved to 8.00 after the session (p < .001).
Sixty of the 102 residents (58.8%) strongly agreed and 37 (36.3%) agreed that the session was relevant to their practice. Only four (3.9%) were neutral about its relevance to their practice.
All teams (100%) were able to escape the room within the 20-minute limit, confirmed through the receipt of 32 total event reports. Tables 2 and 3 show the rate of identifying the planned hazards for the IM and EM cases, respectively.
Table 2. Number of Teams That Identified a Planted Hazard in the IM Case.
| Safety Priority | IM Case Hazards | No. Teams Identifying Hazard (out of 16) |
|---|---|---|
| Hand hygiene | Sink broken | 16 |
| Procedure safety | Lumbar puncture tray not cleaned up (sharps) | 16 |
| Falls | Bed rails down | 15 |
| Deep venous thrombosis prophylaxis | Sequential compression boots not on patient | 15 |
| Restraints | Restraints (no order) | 14 |
| Hospital-acquired infection | No gowns in isolation cart | 13 |
| Skin safety | Tourniquet on | 12 |
| Hospital-acquired infection | Spirometry out of reach | 12 |
| Falls | Fall bracelet not on patient | 11 |
| Skin safety | Diaper on patient | 9 |
| Falls | Bed elevated | 9 |
| Falls | Fall socks not on patient | 8 |
| Procedure safety | Consent filled out wrong | 5 |
| Procedure safety | No time-out | 5 |
| Skin safety | Patient not turned | 5 |
| Procedure safety | Incomplete procedure note | 5 |
| Falls | Bed not locked | 5 |
| Documentation | Copy-forward error in chart | 1 |
Abbreviation: IM, internal medicine.
Table 3. Number of Teams That Identified a Planted Hazard in the EM Case.
| Safety Priority | EM Case Hazards | No. Teams Identifying Hazard (out of 16) |
|---|---|---|
| Medication safety | No allergy wristband | 15 |
| Falls | Bed rails down | 13 |
| Falls | Bed elevated | 13 |
| Hospital-acquired infection | Central line not dressed | 13 |
| Medication safety | Penicillin given in an allergic patient | 13 |
| Medication safety | Medication not connected | 11 |
| Hospital-acquired infection | Head of bed flat | 10 |
| Medication safety | Discontinued medication still hanging | 10 |
| Procedure safety | No procedure note for central line | 7 |
| Falls | Fall socks not on | 6 |
| Falls | No fall wristband | 5 |
| Procedure safety | No time-out documented | 1 |
| Airway | Endotracheal tube malpositioned | 1 |
Abbreviation: EM, emergency medicine.
Discussion
Our team-based simulation of an escape room successfully reinforced our hospital's patient safety priorities for the participating 120 incoming interns across all specialties and exposed them to the actual software they will use to enter a report. We demonstrated that it is feasible to get a large number of learners through a complex active learning session and that they enjoyed the exercise and saw its applicability to their future practice.
Most of our incoming interns had not previously received training in entering patient safety event reports into an online system, and only a tiny minority had ever entered a report. This indicates a clear training gap and supports the need for innovative educational strategies at the point of entry into residency. Our simulated escape room was engaging, relevant, and timely, and it improved learner confidence in identifying safety hazards. The requirement that learners mitigate safety hazards to find clues also trained learners in self-efficacy, reinforcing the notion that they can and should take action to prevent patient harm. Interns used our actual patient safety reporting system, exposing them to the mechanism for reporting events and improving their skill, not just their knowledge, in navigating the system.
Learners had useful ideas for improving future sessions. They requested real clinical examples of events reported, which could be done in a deidentified fashion to further engage learners in the importance of reporting. Describing any system changes or improvements resulting from the reported error would be particularly meaningful, reinforcing the cycle of improvement resulting from event reporting. The gamification element could be enhanced by integrating prizes and competition among teams, although this would have to be carefully done to maintain intrinsic motivation for error reporting. Learners requested higher-acuity cases. We would expand that feedback to creating a greater variety of cases (intensive care, operating room, outpatient clinic), which would send a valuable message about the broad applicability of error reporting. Learners noted that this activity provides a great opportunity for interprofessional education, as including colleagues from nursing and other professions would help flatten hierarchy (an enemy to patient safety) and underscore our shared responsibility for maintaining a safety culture. Other learner suggestions included allowing all residents the opportunity to enter concerns into the reporting system (as opposed to one team entry), providing clearer instructions prior to the start of the activity, decreasing the size of the groups, and physically displaying a countdown of the time available to escape each room.
Limitations of this simulation include a deliberate choice to emphasize errors of commission rather than errors of omission. Prior educational curricula suggest that it is harder to identify something that is missing than something done incorrectly.11 The simulations were limited to inpatient room setups, which may have sent an unintended message that inpatient settings are the only places that errors can occur. Feedback and review of event reports indicated that learners were not always clear on exactly what to include in the escape room event report, which is an opportunity for improvement in the simulation instructions. Finally, our evaluation was limited to assessing learner confidence and perception of relevance, and we have not shown whether this training paradigm will lead to increased event-reporting rates in practice. Other barriers, such as work compression, failure of delegation, and lack of feedback about events, may have disproportionate effects on resident engagement in voluntary event reporting.
We found that learners were able to participate actively in this activity, identifying a broad range of potential patient safety hazards. All teams also completed an event report. Successful task completion suggested that PGY 1s are ready to perform these skills in the clinical environment. Learners felt that this activity was enjoyable and highly relevant, which led to excellent engagement during the activity. It is our hope that this will translate to increased event-reporting rates at our institution and a greater confidence among our house staff in their roles as patient safety advocates. If this turns out not to be the case, our experience with this activity shows that resident engagement and ability will not be at fault; rather, it will likely be due to the impact of the additional barriers mentioned above.
Appendices
A. Escape Room Simulation Case Guides.docx
B. Case 1 (IM) Room Schematic & Instructions.docx
C. Case 2 (EM) Room Schematic & Instructions.docx
D. Case 1 (IM) Chart.doc
E. Case 2 (EM) Chart.docx
F. Case 1 (IM) Facilitator Chart.docx
G. Case 2 (EM) Facilitator Chart.docx
H. Facilitator Roles for Simulation.docx
I. Sample Clue QR Code & Teaching.docx
J. Customizable Didactic Error Reporting.pptx
K. Sample Schedule.docx
L. Assessment Worksheet for Case 1 (IM).docx
M. Assessment Worksheet for Case 2 (EM).docx
N. Escape Room Session Evaluation.doc
O. Information on JTOG.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
None to report.
Prior Presentations
Madara JC, Zavodnick J, Diemer G, et al. Patient safety escape! Engaging residents in patient safety education and event reporting. Poster presented at: ACGME Annual Educational Conference; March 7–10, 2019; Orlando, FL.
Ethical Approval
Reported as not applicable.
References
- 1.Wolf ZR, Hughes RG. Error reporting and disclosure. In: Hughes RG, ed. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008:863–909. [PubMed] [Google Scholar]
- 2.Jagsi R, Kitch BT, Weinstein DF, Campbell EG, Hutter M, Weissman JS. Residents report on adverse events and their causes. Arch Intern Med. 2005;165(22):2607–2613. https://doi.org/10.1001/archinte.165.22.2607 [DOI] [PubMed] [Google Scholar]
- 3.Wild D, Bradley EH. The gap between nurses and residents in a community hospital's error-reporting system. Jt Comm J Qual Patient Saf. 2005;31(1):13–20. https://doi.org/10.1016/S1553-7250(05)31003-8 [DOI] [PubMed] [Google Scholar]
- 4.Clemmer TP, Spuhler VJ, Oniki TA, Horn SD. Results of a collaborative quality improvement program on outcomes and costs in a tertiary critical care unit. Crit Care Med. 1999;27(9):1768–1774. https://doi.org/10.1097/00003246-199909000-00011 [DOI] [PubMed] [Google Scholar]
- 5.Baggs J, Ryan SA, Phelps CE, Richeson JF, Johnson JE. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21(1):18–24. [PubMed] [Google Scholar]
- 6.Wagner R, Koh NJ, Patow C, Newton R, Casey BR, Weiss KB; for CLER Program. Detailed findings from the CLER National Report of Findings 2016. J Grad Med Educ. 2016;8(2)(suppl 1):35–54. https://doi.org/10.4300/1949-8349.8.2s1.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nicholson S. Peeking behind the locked door: a survey of escape room facilities [white paper]. Scott Nicholson website. http://scottnicholson.com/pubs/erfacwhite.pdf. Updated May 24, 2015.
- 8.Zhang XC, Lee H, Rodriguez C, Rudner J, Chan TM, Papanagnou D. Trapped as a group, escape as a team: applying gamification to incorporate team-building skills through an “escape room” experience. Cureus. 2018;10(3):e2256 https://doi.org/10.7759/cureus.2256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. Englewood Cliffs, NJ: Prentice Hall; 1984. [Google Scholar]
- 10.Taylor DCM, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35(11):e1561–e1572. https://doi.org/10.3109/0142159X.2013.828153 [DOI] [PubMed] [Google Scholar]
- 11.Farnan JM, Gaffney S, Poston JT, et al.. Patient safety room of horrors: a novel method to assess medical students and entering residents’ ability to identify hazards of hospitalisation. BMJ Qual Saf. 2016;25(3):153–158. https://doi.org/10.1136/bmjqs-2015-004621 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A. Escape Room Simulation Case Guides.docx
B. Case 1 (IM) Room Schematic & Instructions.docx
C. Case 2 (EM) Room Schematic & Instructions.docx
D. Case 1 (IM) Chart.doc
E. Case 2 (EM) Chart.docx
F. Case 1 (IM) Facilitator Chart.docx
G. Case 2 (EM) Facilitator Chart.docx
H. Facilitator Roles for Simulation.docx
I. Sample Clue QR Code & Teaching.docx
J. Customizable Didactic Error Reporting.pptx
K. Sample Schedule.docx
L. Assessment Worksheet for Case 1 (IM).docx
M. Assessment Worksheet for Case 2 (EM).docx
N. Escape Room Session Evaluation.doc
O. Information on JTOG.docx
All appendices are peer reviewed as integral parts of the Original Publication.