Abstract
Circulating tumor DNA (ctDNA), which carries tumor-specific mutations, is an emerging candidate biomarker for malignancies and for monitoring disease status in various human tumors. Recently, BRAF V595E mutation has been reported in 80% of dogs with urothelial carcinoma. This study investigates the BRAF V595E allele concentration in circulating cell-free DNA (cfDNA) and assesses the clinical significance of BRAF-mutated ctDNA levels in canines with urothelial carcinoma. A total of 15 dogs with urothelial carcinoma were included. cfDNA concentration was measured using a real-time polymerase chain reaction (PCR) of the LINE-1 gene. To measure the concentration of the mutated BRAF gene in cfDNA, allele-specific real-time PCR with a locked nucleic acid probe was performed. BRAF mutations were detected in 11 (73%) of the 15 tested tumor samples. BRAF-mutated ctDNA concentrations were significantly higher in dogs with the BRAF mutation (14.05 ± 13.51 ng/ml) than in wild-type dogs (0.21 ± 0.41 ng/ml) (p = 0.031). The amount of BRAF-mutated ctDNA in plasma increased with disease progression and responded to treatment. Our results show that BRAF-mutated ctDNA can be detected using allele-specific real-time PCR in plasma samples of canines with urothelial carcinoma with the BRAF V595E mutation. This ctDNA analysis may be a potentially useful tool for monitoring the progression of urothelial carcinoma and its response to treatment.
Introduction
Urothelial carcinoma, also known as transitional cell carcinoma, is the most common form of bladder cancer and an aggressive lower urinary tract tumor in dogs. Reported treatments for urothelial carcinoma include chemotherapy, cyclooxygenase (COX) inhibitors, surgery, and radiation therapy. Urothelial carcinoma is characterized by its invasion of surrounding tissues and its high metastatic potential. Therefore, systemic medical treatment is the mainstay of therapy for urothelial carcinoma in dogs [1]. Although medical therapy is not often curative, remission or stable disease can be accomplished, and median survival times have reached 1 year or greater [2]. Ultrasonography is commonly used for tumor monitoring and measurement in veterinary medicine [1]. However, distension of the urinary bladder can vary over time, making accurate tumor size estimations difficult. Therefore, computed tomography (CT) imaging has been suggested to be more suitable for monitoring of these tumors, especially those with irregular shapes [3]. Unfortunately, this imaging modality can be costly and frequently requires anesthetization.
Circulating cell-free DNAs (cfDNA) are extracellular DNAs that are released into the bloodstream from both normal and tumor cells through apoptosis, necrosis, or direct secretion [4]. Circulating tumor DNAs (ctDNA) released by cancer cells have been found within the cfDNA. These ctDNAs contain the same genetic alterations present in the source tumor and therefore may help clinicians evaluate tumor features in patients with cancer. These ctDNAs may also be useful for monitoring response to therapy through obtaining a simple blood sample known as a liquid biopsy [5]. CtDNAs with PIK3CA, EGFR, KRAS, or BRAF mutations have been detected in human patients, and the levels of these ctDNAs have been shown to be useful for the monitoring of disease progression [6, 7].
Recent studies have identified the canine BRAF V595E mutation (cBRAF reference sequence ENSCAFT00000006306), which is homologous to the human BRAF V600E mutation, in several canine cancers and at least 80% of canine urothelial carcinoma [8, 9]. In humans, approximately 50% of patients with melanoma have the BRAF V600E mutation, and BRAF-mutated ctDNA levels have been shown to serve as specific biomarkers in these patients [10]. In veterinary medicine, testing for the presence of the BRAF mutation using urine or tissue samples is a sensitive and noninvasive method for the diagnosis of canine urothelial carcinoma [11]. However, to our knowledge, no studies have analyzed the use of ctDNA for diagnosis or disease monitoring in canines with urothelial carcinoma. The aim of this study is to measure the BRAF-mutated ctDNA levels in plasma and to assess its clinical significance in canines with urothelial carcinoma.
Materials and methods
Patients and follow-up
This study was reviewed and approved by the Institutional Animal Care and Use Committee at the Obihiro University of Agriculture and Veterinary Medicine (Permission number: 18–2 and 19–7). Written informed consent was obtained from owners for animal participation in this study. A total of 15 dogs with urothelial carcinoma were included in this study, and all diagnoses were confirmed by histology or cytology at the Veterinary Medical Center at the Obihiro University of Agriculture and Veterinary Medicine (VMC-OUAVM) between February 2018 and May 2019. Staging of the urothelial carcinoma was performed according to the World Health Organization (WHO) staging system [12], which incorporates the use of CT imaging, thoracic radiography with three views, and abdominal ultrasonography. Patients were treated at the discretion of their owners and veterinarians, as appropriate for their disease stage. Tumor responses were assessed at each visit by Response Evaluation Criteria in Solid Tumors (cRECIST) version v1.0 [13], and were classified as having a complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD).
Blood collection and cell-free DNA extraction
Two milliliters of peripheral blood in ethylenediaminetetraacetic acid were collected from each dog. Plasma was then separated by centrifugation at 2000 g for 10 min at 4 ˚C, transferred to new tubes, and centrifuged at 16,000 g for 10 min at 4 ˚C to remove cell debris. Plasma was stored at -30 ˚C prior to DNA extraction. All samples were processed within 4 h of blood collection. cfDNA was isolated from 500 μl of plasma using the MagMAX Cell-Free DNA Isolation Kit (Thermo Fisher Scientific, Inc., Waltham, MA, USA) according to the manufacturer’s instructions. The cfDNA preparations were eluted in 50 μl of elution buffer and stored at -30 ˚C until further analysis.
BRAF mutation status
The BRAF mutation status was available for all dogs and was obtained from DNA from biopsy or surgical specimens using the QIAamp DNA Mini Kit (QIAGEN, Hilden, Germany). To determine the sequence of cBRAF, a polymerase chain reaction (PCR) was performed, as previously described [9]. Sequencing was performed at Eurofins Genomics (https://www.eurofinsgenomics.jp/), and data were analyzed for the presence of the cBRAF V595E mutation using Sequencher (Sequencher® version 4.7 DNA sequence analysis software, Gene Codes Corporation, Ann Arbor, MI, USA).
Quantification of cfDNA using the LINE-1 gene
The plasma cfDNA concentration was measured using a quantitative real-time PCR (qPCR) reaction of long interspersed nuclear element-1 (LINE-1), as previously described [14]. The results of this assay were used for the normalization of DNA volume to be used in the qPCR for the BRAF mutation. Primer sequences were as follows: forward primer 5’-AAATGCAATGAAACGCCGGG-3’ and reverse primer 5’-TCTTTCGTTGGACACCGAGG-3’ [15]. The qPCR reaction was performed in a 20 μl total volume, containing 500 nM of each primer, 1 μl of cfDNA template, and 10 μl of PowerUp SYBR Green Master Mix (ABI; Thermo Fisher Scientific, Inc., Waltham, MA, USA), using a StepOne Real-Time PCR System (ABI). Initial incubation was performed at 50°C for 2 min and 95°C for 2 min, followed by 40 cycles of denaturation at 95°C for 3 sec and annealing/extension at 60°C for 30 sec. A melt curve (60–95°C) was generated at the end of each run to verify specificity. A standard curve generated by a 10-fold serial dilution (from 1.0–10,000 ng/ml) of genomic DNA obtained from peripheral blood leukocytes of a healthy dog was used to determine the absolute equivalent amount of cfDNA in each sample. All samples were evaluated in duplicate, and a negative control (without template) was included in each plate.
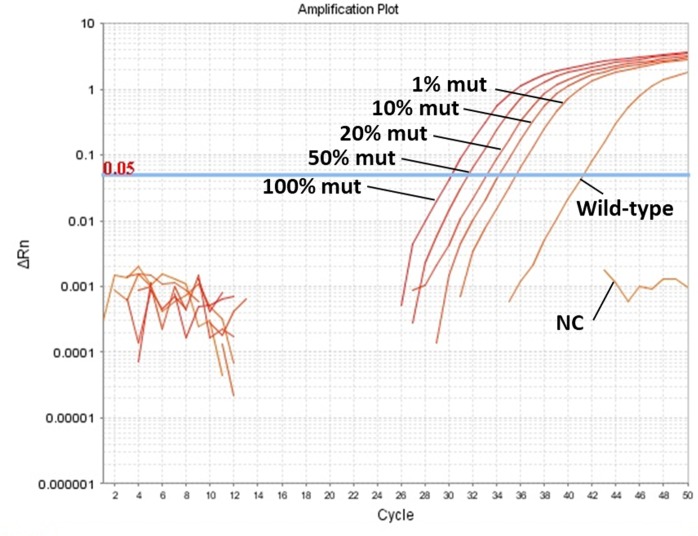
Allele-specific qPCR to measure percentage of the BRAF mutation
Primer pairs were designed for the measurement of the BRAF mutation in cfDNA. Forward primer (5’- TTCATGAAGACCTCACAGTAAA-3’) was common to wild-type, while the reverse primer (5’-CCCACTCCATCGAGATTTCT-3’) was specific to the mutated sequence. A dual-labeled locked nucleic acid (LNA) probe (5’-FAM-CCA[+C]A[+G][+A][+G]A[+A]A[+T]C-IABkFQ-3’, Integrated DNA Technologies, Coralville, Iowa, USA) for detecting the BRAF mutation gene sequence was also designed (Fig 1).
Fig 1. Primer and LNA probe position for amplification of mutated BRAF DNA.
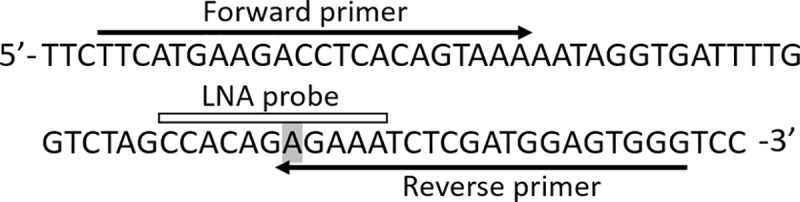
Gray area indicates the mutated allele.
To measure the percentage of the BRAF mutation in plasma samples, qPCR was performed in duplicate with 0.5 ng plasma cfDNA in a 20 μl total volume, containing 500 nM of each primer, 250 nM of LNA probe, 5 μl of cfDNA template, and 10 μl of PrimeTime Gene Expression Master Mix (Integrated DNA Technologies). Initial incubation was performed at 95°C for 3 min, followed by 50 cycles of denaturation at 95°C for 5 sec and annealing/extension at 63°C for 30 sec. The standard curve for the BRAF mutation consisted of six dilutions (100%, 50%, 20%, 10%, 1%, and 0% of BRAF mutated samples) obtained by mixing DNA from a mutant transitional cell carcinoma cell line (LC-TCC) and wild-type genomic DNA obtained from peripheral blood leukocytes of a healthy dog (Fig 2). Sample results were expressed as percentages of mutation. Because canine TCC is heterozygous for the BRAF mutation, mutated BRAF concentrations were calculated as follows: mutated BRAF ctDNA (ng/ml) = (% mutated BRAF × total cfDNA)/100/2 [16]. Analysis of 3 different runs provided the following values (mean± S.D.): slope = –3.36±0.11 (efficiency = 98.67±4.40), R2 = 0.96±0.04, and Y-intercept = 38.97±0.94.
Fig 2. Amplification plots obtained for wild-type and for samples containing known percentages (100%, 50%, 20%, 10%, and 1%) of BRAF mutated samples (mut).
NC means negative control using distilled water.
Statistical analyses
Statistical analyses were carried out using JMP 13 software (SAS Institute, Cary, NC). The Mann-Whitney U test and Kruskal-Wallis test were applied to compare plasma cfDNA concentrations between groups. The Steel-Dwass test was performed on each pair of groups after the Kruskal-Wallis test. Survival time was defined as the time from study entry to date of death or last follow-up. Dogs alive at the last follow-up were censored for survival analysis. Survival curves were calculated by the Kaplan-Meier method using median values as the cut-off. The generalized Wilcoxon test was used for survival estimates. A p-value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
This study included 15 patients with 7 males (nonintact) and 8 females (1 intact). Patients had a median age of 12 years (range 8–15 years). Ten dogs were diagnosed with urothelial carcinoma by histology, and five dogs were diagnosed by cytology. BRAF mutations were detected in 11 (73%) of the 15 tested tumor tissue or urine samples (S1 Fig). Metastases at sampling time were observed in six dogs (lymph node, n = 3; lung, n = 2; and bone, n = 1). The location of the primary tumor was noted in all patients. Eleven tumors were located purely in the bladder, three were located in the urethra with extension into the bladder, and one was located in the prostate. The clinical characteristics of each patient are summarized in Table 1.
Table 1. Characteristics of patients.
| Characteristics | Total (n = 15) | V595E (n = 11) | Wild-type (n = 4) |
|---|---|---|---|
| Sex | |||
| Female | 8 | 6 | 2 |
| Male | 7 | 5 | 2 |
| Age* | 12 (range; 8–15) | 12 (range; 8–15) | 12 (range; 10–13) |
| Location | |||
| Bladder | 11 | 9 | 2 |
| Bladder+urethra | 3 | 1 | 2 |
| Prostate | 1 | 1 | 0 |
| Tumor stagea | |||
| T2 | 11 | 8 | 3 |
| T3 | 4 | 3 | 1 |
| Lymph nodea | |||
| N0 | 12 | 9 | 3 |
| N1 | 3 | 2 | 1 |
| Metastasisa | |||
| M0 | 12 | 9 | 3 |
| M1 | 3 | 2 | 1 |
a) According to the WHO staging system [12]. T2, tumour invading the bladder wall; T3, tumor invading neighboring organs; N0, no evidence of lymph node involvement; N1, lymph node involvement; M0, no evidence of distant metastasis; M1, distant metastasis.
*: years
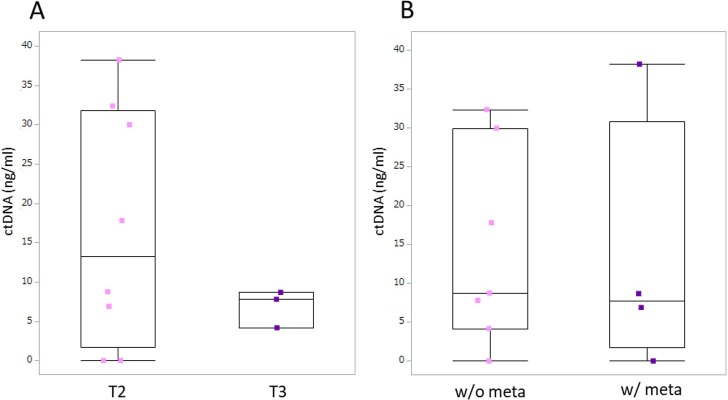
CfDNA concentration
The median cfDNA concentration of LINE-1 in all dogs at presentation was 724.3 ng/ml (range 122.2–5487.6 ng/ml). We compared cfDNA concentrations of dogs with different tumor stages and found no significant difference between T2 stage (n = 11; mean ± SE: 1819.07 ± 1790.95 ng/ml) and T3 stage (n = 4; 612.63 ± 131.32 ng/ml) (p = 0.240) (Fig 3). Plasma cfDNA concentration was higher in dogs with metastasis (2433.05 ± 2227.92 ng/ml) than in dogs without metastasis (873.55 ± 594.00 ng/ml); however, no significant difference was found (p = 0.195) (Fig 3).
Fig 3. Box-plot of plasma cell-free DNA concentrations in dogs with urothelial carcinoma.
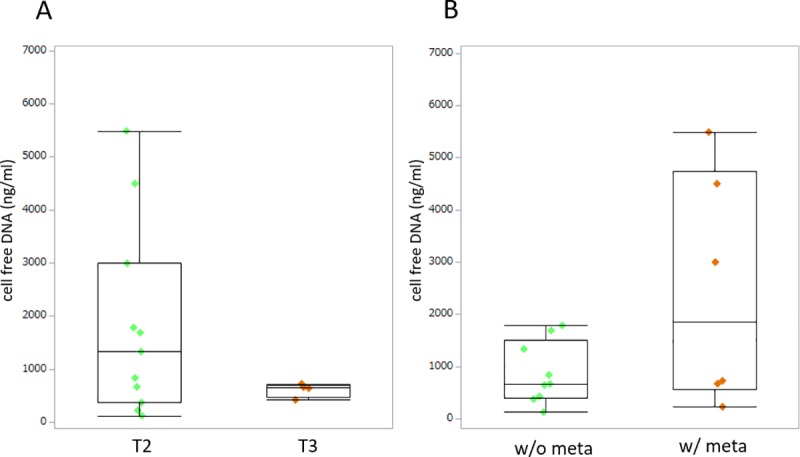
Each box indicates the 25th and 75th percentiles. The horizontal line inside the box indicates the median, and the whiskers indicate the extreme measured values. A. Local tumor stage. T2: tumor invading the bladder wall; T3: tumor invading neighboring organs. B. Metastasis condition. w/o meta: no evidence of metastasis; w/ meta: metastasis present.
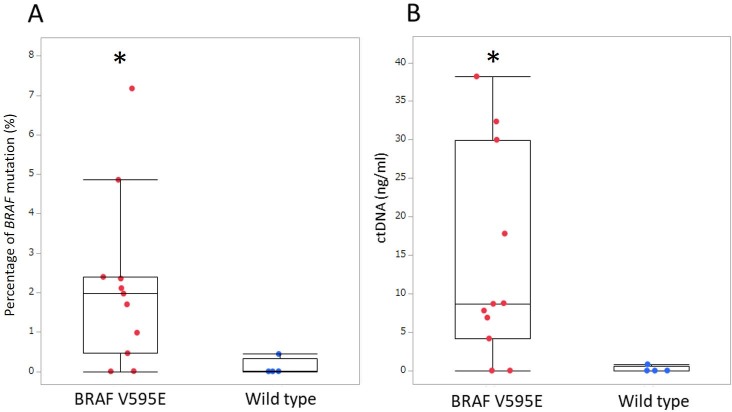
Mutated BRAF percentage and concentrations
In order to evaluate the sensitivity of the qPCR assay, we performed 3 replicates using the standard in the same assay run. The theoretical detection limit of the assay was determined to be 0.13% BRAF-mutated ctDNA. The mean percentage of the BRAF mutation in cfDNA was 2.18 ± 2.15% in dogs with the BRAF mutation and 0.11 ± 0.22% in wild-type dogs (p = 0.022). BRAF-mutated ctDNA concentration was significantly higher in dogs with the BRAF mutation (14.05 ± 13.51 ng/ml) than in wild-type dogs (0.21 ± 0.41 ng/ml) (p = 0.031) (Fig 4).
Fig 4.
Box-plot of (A) percentage of the BRAF mutation and (B) BRAF-mutated ctDNA concentration in plasma obtained from dogs with urothelial carcinoma. Each box indicates the 25th and 75th percentiles. The horizontal line inside the box indicates the median, and the whiskers indicate the extreme measured values. * p < 0.05.
We compared the BRAF-mutated ctDNA concentrations in 11 dogs with the BRAF mutation with different tumor stages. No significant difference was found in BRAF-mutated ctDNA concentrations identified between dogs with T2 (n = 8; 16.75 ± 15.13 ng/ml) or T3 (n = 3; 6.88 ± 2.39 ng/ml) (p = 0.475) disease. Dogs with metastasis (n = 4) also had no significant difference in their BRAF-mutated ctDNA concentration (13.44 ± 16.92 ng/ml) compared to dogs without metastasis (n = 7; 14.41 ± 12.68 ng/ml) (p = 0.777) (Fig 5).
Fig 5. Box-plot of BRAF-mutated ctDNA concentrations in plasma obtained from dogs with urothelial carcinoma.
Each box indicates the 25th and 75th percentiles. The horizontal line inside the box indicates the median, and the whiskers indicate the extreme measured values. A. Local tumor stage. T2: tumor invading the bladder wall; T3: tumor invading neighboring organs. B. Metastasis condition. w/o meta: no evidence of metastasis; w/ meta: metastasis present.
Plasma DNA dynamics and tumor progression
The levels of BRAF-mutated ctDNA were assessed in six patients during the treatment course (Table 2). In several patients, the concentration of BRAF-mutated ctDNA in plasma increased with disease progression and responded to the treatment.
Table 2. Clinical characteristics of six patients assessed by follow-up study.
| Patient | Breed | Age | Gender | Tumor site | Stagea | Metastasis site | Treatment | ST (days) |
|---|---|---|---|---|---|---|---|---|
| 1 | MP | 9 | Spayed | Bladder | T2N0M0 | No | Surgery+cox2i | 22 |
| 2 | PM | 13 | Spayed | Bladder | T2N0M0 | No | Surgery+cox2i | 228* |
| 3 | PM | 8 | Spayed | Bladder | T2N0M0 | No | Chemotherapy+cox2i | 305 |
| 4 | Pug | 11 | Spayed | Bladder+ urethra | T3N0M1 | Pelvic bone | Chemotherapy+cox2i | 217 |
| 5 | MD | 13 | Spayed | Bladder | T3N0M0 | No | Chemotherapy+cox2i | 340* |
| 6 | SS | 12 | Castrated | Bladder | T2N0M1 | Lung | Chemotherapy+cox2i | 335* |
a) According to the WHO staging system [12].
*: censored case
MP, miniature pinscher; PM, pomeranian; MD, miniature dachshund; SS, shetland sheepdog; ST, survival time; cox2i, cyclooxygenase2 inhibitor
Patients 1 and 2 underwent partial cystectomy after first blood sampling. BRAF-mutated ctDNA levels decreased after resection on postoperative day 3 and 32, respectively. Patient 1 died of pneumonia on day 22, and local recurrence was confirmed by necropsy (Fig 6A). In patient 2, bladder recurrence was observed on day 114, and an increase in the mutated ctDNA level was identified (Fig 6B). Both patients were administrated piroxicam, an oral cyclooxygenase-2 inhibitor, after resection.
Fig 6. Monitoring of BRAF-mutated ctDNA concentrations according to treatment response.
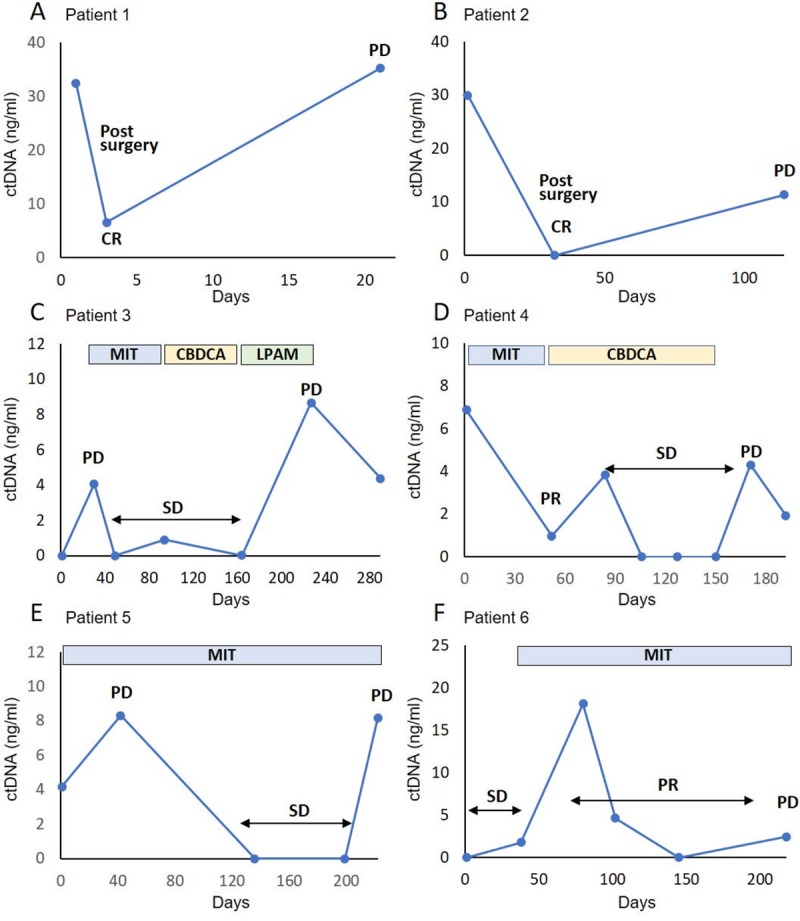
Mutated BRAF ctDNA levels at various time points in six patients. The vertical axis represents mutated BRAF ctDNA concentration, and the horizontal axis represents the time points of plasma-sampling days. All patients were administrated oral cyclooxygenase-2 inhibitors during treatment. CR, complete response; SD, stable disease; PD, progressive disease; PR, partial response; MIT, mitoxantrone; CBDCA, carboplatin; LPAM, Melphalan.
The owners of patients 3, 4, 5, and 6 chose medical therapy. Patient 3 presented with a lung metastasis on day 30, and an increased BRAF-mutated ctDNA level was observed. Progressive primary tumor and lung metastases were observed on day 227 with a substantial increase in the ctDNA levels. The patient’s condition gradually deteriorated, and she died on day 305 (Fig 6C).
Patient 4 presented with a pelvic bone metastasis, and a high level of BRAF-mutated ctDNA was detected at first sampling. Reduction of the primary tumor was observed after carboplatin administration, and the ctDNA level significantly decreased on day 52. Skin metastasis appeared on day 150, and rapid tumor progression was seen after day 171. The ctDNA level increased again, and the patient died on day 217 (Fig 6D).
Patient 5 developed PD of her primary tumor, and BRAF-mutated ctDNA was detected on day 42. The primary tumor stabilized between days 42 and 199 with mitoxantrone administration, and the DNA level was undetectable. However, tumor progression and bilateral hydronephrosis were observed on day 222, and the ctDNA level increased (Fig 6E).
Patient 6 presented with lung metastases detected on CT scan. Although tumor response was classified as PR on day 80, the BRAF-mutated ctDNA level increased between days 80 and 102. Tumor regrowth was detected on day 218, and the ctDNA level increased (Fig 6F).
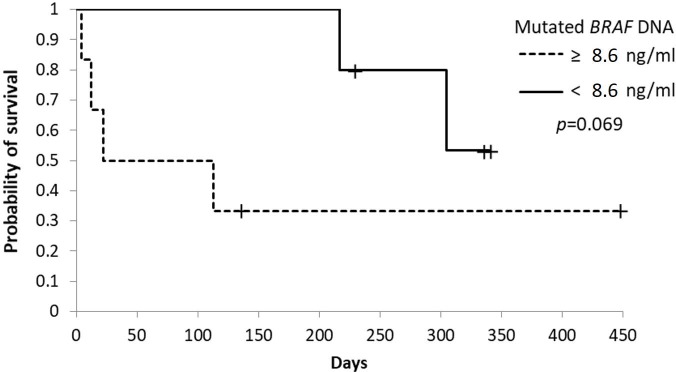
Mutated BRAF concentrations and survival
The 11 patients who tested positive for the BRAF mutation in their primary tumor were divided into two groups according to their plasma concentrations of BRAF-mutated ctDNA (< 8.3 ng/ml vs. ≥ 8.3 ng/ml) at first sampling. These thresholds were selected based on the median value of BRAF-mutated ctDNA.
Although no significant difference was found, the median overall survival duration of the five patients with a BRAF-mutated ctDNA concentration of < 8.6 ng/ml was longer than that of the six patients with a BRAF-mutated ctDNA concentration of ≥ 8.6 ng/ml (305 vs. 67.5 days, p = 0.069) (Fig 7).
Fig 7. Kaplan-Meier curves of survival time in dogs with urothelial carcinoma according to the cut-off value based on mutated BRAF ctDNA concentrations.
Cut-off and p-values are shown. + censored case.
Discussion
CtDNAs carrying tumor-specific mutations have been found in the bloodstream. In humans, ctDNA levels in the plasma or serum are potentially useful noninvasive biomarkers for several tumor types [5]. Recently, studies have reported that the canine BRAF V595E mutation, a single nucleotide T to A transversion at nucleotide 1349, is detectable in 80% of canines with urothelial carcinomas [9, 11]. No previous studies have evaluated the measurement of ctDNA levels of this mutation in the plasma of canines with these tumors. In this study, we developed a real-time PCR method using a forward primer common to both wild-type and mutated BRAF sequences and a mutation-specific reverse primer. A dual-labelled LNA probe was designed on the strand complementary to that recognized and hybridized by the BRAF V595E allele-specific primer. We found that the ctDNA concentration in patients with BRAF-mutated urothelial carcinoma is increased compared to that in wild-type patients, demonstrating that the BRAF mutation in urothelial carcinoma may be detectable in the plasma of these canines. CtDNAs with mutations in several genes have been detected in human patients with cancer, and ctDNA analysis provides critical clinical information to improve diagnosis in these patients [6, 7, 17].
In this study, the BRAF mutation was detected in 11 of the 15 tested tissue or urine samples. Mutated BRAF ctDNA was detected in 9 of these 11 patients’ plasma at the time of the first blood collection. BRAF-mutated ctDNA was detected in the three other dogs later in the course of their diseases. This study suggests that the quantification of mutated BRAF ctDNA in plasma may represent a useful biomarker for the noninvasive diagnosis of canine urothelial carcinoma when the tumor has the BRAF mutation. This study also shows that the concentration of mutated BRAF ctDNA does not correlate with the clinical stage or the presence of metastases. Past studies have found that ctDNA levels of mutated target genes are higher in patients with more advanced-stage disease [18, 19]. Further studies with larger sample sizes will be necessary to explore this discrepancy. Interestingly, mutated BRAF ctDNA was also detected above the cut-off value in one wild-type patient (mutated BRAF percentage, 0.44%). In this study, determination of BRAF mutant cases was made by Sanger sequencing. Some of cases classified as wild type may have had BRAF mutations present at a level below the limit of detection for Sanger sequencing. Furthermore, it is possible that ctDNA in plasma of the dog could be indicative of a BRAF mutation originating from other neoplasms that have been undiagnosed because BRAF V595E mutation has been detected in not only urothelial carcinoma but also many other neoplasms [9]. In addition, recently, study has reported that low levels of common cancer gene mutations may be present even in healthy individuals [20]. Further clinical validation is essential, however, before being incorporated into clinical practice.
In this study, we observed that mutated BRAF ctDNA levels in plasma are approximately correlated with the response to treatment, suggesting that the BRAF-mutated ctDNA level may serve as a useful therapeutic biomarker. In humans, previous studies have indicated that mutated ctDNA levels correlate with tumor burden in several tumor types and that mutated ctDNA levels are consistent with the patient’s overall clinical condition [20, 21]. In addition, detection of ctDNA following chemoradiotherapy is associated with tumor progression and postoperative ctDNA detection is associated with recurrence [22, 23]. Detection of mutated BRAF cfDNA in plasma may be a potentially useful biomarker for noninvasive follow-up of canines with urothelial carcinoma. In contrast, we also found that mutated ctDNA levels do not reflect the observed disease progression in some patients. From our analysis, whether ctDNA quantification provides useful information for tumor monitoring is still unknown because of our small number of included patients.
Although no significant difference was found, we show that low levels of baseline mutated BRAF ctDNA (< 8.6 ng/ml) are predictive of prolonged survival time compared to patients with a high baseline level of mutated BRAF ctDNA. Previous reports have showed high or positive baseline levels of ctDNA in various human cancers, which are associated with shorter overall survival and progression-free survival [24, 25, 26]. Since evaluation of ctDNA levels as a prognostic biomarker for canines with urothelial carcinoma has not been reported previously, larger cohort studies are needed to validate our findings.
Since mutated ctDNA derived from malignant tumors exists only at low concentrations in patients, highly sensitive assays are required for assessment. Most PCR methods that detect BRAF mutation are limited by the presence of a large proportion of wild-type BRAF, which interferes with ctDNA mutation assays [27]. Currently, digital PCR and next-generation sequencing are the main methods used to detect mutation abundance in cfDNA due to their high sensitivities and specificities [20]. However, both methods require specialized instruments and high costs to perform multiple tests for regular tumor monitoring. For this study, we developed an allele-specific real-time PCR method with a dual-labelled LNA probe. The method has already been used to detect BRAF mutations in plasma samples of human patients with melanoma [16]. Although we included only a small number of patients, changes in plasma mutated BRAF ctDNA levels associated with tumor progression were successfully detected by our method. Further studies are needed to assess the clinical value of ctDNA quantification using this method in dogs with urothelial carcinoma.
A limitation of the present study was the small number of patients. The small sample size used for each analysis may have limited the extent to which differences between groups could be detected. Additionally, our study was a retrospective analysis, and therapeutic methods were not consistent. Therefore, a future large-scale prospective study using standardized treatment modalities will be necessary for adequate evaluation.
In conclusion, our results show that mutated BRAF ctDNA can be detected using allele-specific real-time PCR in plasma samples of canines with urothelial carcinoma harboring the BRAF V595E mutation. This technique may be useful for monitoring disease progression and treatment response. Further research is required to establish the true clinical value of plasma mutated BRAF ctDNA as a biomarker for canine urothelial carcinoma.
Supporting information
(TIFF)
Acknowledgments
We appreciate Dr. Tatsuya Deguchi, Dr. Sangho Kim, and Dr. Masahiro Okumura (Laboratory of Veterinary Surgery, Graduate School of Veterinary Medicine, Hokkaido University, Japan) for providing canine transitional cell carcinoma cell lines and the dog's owners for their availability in this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Fulkerson CM, Knapp DW. Management of transitional cell carcinoma of the urinary bladder in dogs: a review. Vet J. 2015;205: 217–225. 10.1016/j.tvjl.2015.01.017 [DOI] [PubMed] [Google Scholar]
- 2.Griffin MA, Culp WTN, Rebhun RB. Lower Urinary Tract Neoplasia. Vet Sci. 2018;5 pii: E96 10.3390/vetsci5040096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leffler AJ, Hostnik ET, Warry EE, Habing GG, Auld DM, Green EM, et al. Canine urinary bladder transitional cell carcinoma tumor volume is dependent on imaging modality and measurement technique. Vet Radiol Ultrasound. 2018;59: 767–776. 10.1111/vru.12652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jahr S, Hentze H, Englisch S, Hardt D, Fackelmayer FO, Hesch RD, et al. DNA fragments in the blood plasma of cancer patients: quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Res. 2001;61: 1659–1665. [PubMed] [Google Scholar]
- 5.Ossandon MR, Agrawal L, Bernhard EJ, Conley BA, Dey SM, Divi RL, et al. Circulating Tumor DNA Assays in Clinical Cancer Research. J Natl Cancer Inst. 2018;110: 929–934. 10.1093/jnci/djy105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fan G, Zhang K, Ding J, Li J. Prognostic value of EGFR and KRAS in circulating tumor DNA in patients with advanced non-small cell lung cancer: a systematic review and meta-analysis. Oncotarget. 2017;8: 33922–33932. 10.18632/oncotarget.15412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Butler TM, Spellman PT, Gray J. Circulating-tumor DNA as an early detection and diagnostic tool. Curr Opin Genet Dev. 2017;42: 14–21. 10.1016/j.gde.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 8.Decker B, Parker HG, Dhawan D, Kwon EM, Karlins E, Davis BW, et al. Homologous Mutation to Human BRAF V600E Is Common in Naturally Occurring Canine Bladder Cancer—Evidence for a Relevant Model System and Urine-Based Diagnostic Test. Mol Cancer Res. 2015;13: 993–1002. 10.1158/1541-7786.MCR-14-0689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mochizuki H, Kennedy K, Shapiro SG, Breen M. BRAF Mutations in Canine Cancers. PLoS One. 2015;10: e0129534 10.1371/journal.pone.0129534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schreuer M, Meersseman G, Van Den Herrewegen S, Jansen Y, Chevolet I, Bott A, et al. Quantitative assessment of BRAF V600 mutant circulating cell-free tumor DNA as a tool for therapeutic monitoring in metastatic melanoma patients treated with BRAF/MEK inhibitors. J Transl Med. 2016;14: 95 10.1186/s12967-016-0852-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mochizuki H, Shapiro SG, Breen M. Detection of BRAF Mutation in Urine DNA as a Molecular Diagnostic for Canine Urothelial and Prostatic Carcinoma. PLoS One. 2015;10: e0144170 10.1371/journal.pone.0144170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Owen LN. TNM Classification of Tumours in Domestic Animals, World Health Organization, Geneva, Switzerland; 1980 [Google Scholar]
- 13.Nguyen SM, Thamm DH, Vail DM, London CA. Response evaluation criteria for solid tumours in dogs (v1.0): a Veterinary Cooperative Oncology Group (VCOG) consensus document. Vet Comp Oncol. 2015;13: 176–183. 10.1111/vco.12032 [DOI] [PubMed] [Google Scholar]
- 14.Tagawa M, Shimbo G, Inokuma H, Miyahara K. Quantification of plasma cell-free DNA levels in dogs with various tumors. J Vet Diagn Invest. 2019;31: 836–843. 10.1177/1040638719880245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beffagna G, Sammarco A, Bedin C, Romualdi C, Mainenti M, Mollo A, et al. Circulating Cell-Free DNA in Dogs with Mammary Tumors: Short and Long Fragments and Integrity Index. PLoS One. 2017;12: e0169454 10.1371/journal.pone.0169454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pinzani P, Salvianti F, Cascella R, Massi D, De Giorgi V, Pazzagli M, et al. Allele specific Taqman-based real-time PCR assay to quantify circulating BRAFV600E mutated DNA in plasma of melanoma patients. Clin Chim Acta. 2010;411: 1319–1324. 10.1016/j.cca.2010.05.024 [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez BJ, Córdoba GD, Aranda AG, Álvarez M, Vicioso L, Pérez CL, et al. Detection of TP53 and PIK3CA Mutations in Circulating Tumor DNA Using Next-Generation Sequencing in the Screening Process for Early Breast Cancer Diagnosis. J Clin Med. 2019;8: E1183 10.3390/jcm8081183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhu YJ, Zhang HB, Liu YH, Zhang FL, Zhu YZ, Li Y, et al. Quantitative cell-free circulating EGFR mutation concentration is correlated with tumor burden in advanced NSCLC patients. Lung Cancer. 2017;109: 124–127. 10.1016/j.lungcan.2017.05.005 [DOI] [PubMed] [Google Scholar]
- 19.Zhou Y, Xu Y, Gong Y, Zhang Y, Lu Y, Wang C, et al. Clinical factors associated with circulating tumor DNA (ctDNA) in primary breast cancer. Mol Oncol. 2019;13: 1033–1046. 10.1002/1878-0261.12456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kunnath AP and Priyashini T. Potential Applications of Circulating Tumor DNA Technology as a Cancer Diagnostic Tool. Cureus. (2019) 11:e4907 10.7759/cureus.4907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamakawa T, Kukita Y, Kurokawa Y, Miyazaki Y, Takahashi T, Yamasaki M, et al. Monitoring gastric cancer progression with circulating tumour DNA. Br J Cancer. 2015;112: 352–356. 10.1038/bjc.2014.609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azad TD, Chaudhuri AA, Fang P, Qiao Y, Esfahani MS, Chabon JJ, et al. Circulating tumor DNA analysis for detection of minimal residual disease after chemoradiotherapy for localized esophageal cancer. Gastroenterology. 2019; pii: S0016–5085(19)41530-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee B, Lipton L, Cohen J, Tie J, Javed AA, Li L, et al. Circulating tumor DNA as a potential marker of adjuvant chemotherapy benefit following surgery for localized pancreatic cancer. Ann Oncol. 2019;30: 1472–1478. 10.1093/annonc/mdz200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahlborn LB, Tuxen IV, Mouliere F, Kinalis S, Schmidt AY, Rohrberg KS, et al. Circulating tumor DNA as a marker of treatment response in BRAF V600E mutated non-melanoma solid tumors. Oncotarget. 2018;9: 32570–32579. 10.18632/oncotarget.25948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Phallen J, Sausen M, Adleff V, Leal A, Hruban C, White J, et al. Direct detection of early-stage cancers using circulating tumor DNA. Sci Transl Med. 2017;9: pii: eaan2415 10.1126/scitranslmed.aan2415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee JS, Rhee TM, Pietrasz D, Bachet JB, Laurent-Puig P, Kong SY, et al. Circulating tumor DNA as a prognostic indicator in resectable pancreatic ductal adenocarcinoma: A systematic review and meta-analysis. Sci Rep. 2019;9: 16971 10.1038/s41598-019-53271-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ashida A, Sakaizawa K, Mikoshiba A, Uhara H, Okuyama R. Quantitative analysis of the BRAF V600E mutation in circulating tumor-derived DNA in melanoma patients using competitive allele-specific TaqMan PCR. Int J Clin Oncol. 2016;21: 981–988. 10.1007/s10147-016-0976-y [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIFF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.