Abstract
Rationale: Cough and phlegm are common symptoms of chronic obstructive pulmonary disease (COPD) and may significantly affect quality of life. This study assessed the burden of cough and phlegm on clinical outcomes and quality of life among people with a self-reported physician diagnosis of COPD.
Methods: Patient-reported data from the COPD Foundation’s Patient-Powered Research Network (COPD PPRN) were utilized. Cough and phlegm severity and frequency were assessed by responses to questions on the COPD Assessment Test (CAT) and categorized into none/low, moderate and severe. Quality of life domains were evaluated using the Patient-Reported Outcome Measurement Information System (PROMIS-29). Associations between cough and phlegm levels and PROMIS-29 domains were examined using multivariate analysis of variance (MANOVA).
Results: The 5286 participants were average age 64.4 years (SD=11.4), 87.9% white, 60.4% female, 51.2% married, and 42.2% with caregivers. Approximately three-fourths of the participants had moderate or severe cough or phlegm levels. Respondents with moderate and high cough or phlegm had significantly worse dyspnea (p<0.0001), more exacerbations in the previous one year (p<0.0001), worse physical and social functioning, and more symptoms of anxiety and depression on PROMIS-29 compared to those with no/low cough and phlegm.
Conclusions: In this group of people with COPD, higher levels of cough and phlegm are associated with worse clinical and quality of life outcomes.
Keywords: chronic obstructive pulmonary disease, patient-reported outcomes, symptom burden, COPD, cough, phlegm, PROMIS-29
Introduction
This article contains supplemental material.
Chronic obstructive pulmonary disease (COPD) affects between 15 and 25 million adults in the United States, and is the fourth leading cause of death and the second leading cause of disability.1-3 COPD is estimated to be responsible for over 10 million office visits, 1.5 million emergency department (ED) visits, and 700,000 hospitalizations annually.3,4 The estimated U.S. direct and indirect cost of COPD is over $50 billion3,5 but is likely higher when considering that patients with COPD often have multiple comorbiditites.6
COPD patients experience high rates of morbidity and disability based on multiple symptoms, exacerbations, and severity of airflow obstruction.3,7 The COPD symptom experience is closely related to health outcomes.8,9 Cough and mucus production (phlegm) are common reasons for people with COPD to seek medical care, yet COPD-associated cough and phlegm have few effective therapies compared to other common symptoms, such as dyspnea.10 Negative association between overall COPD symptom severity and health-related quality of life (HRQoL), including an adverse impact on physical and social function as well as mood, has been reported previously.11 Nighttime symptoms including cough and phlegm further contribute to increased morbidity in this patient population.12,13
Limited research has been conducted to understand the burden of cough and phlegm on functional status, role fulfillment abilities and impact on mood and sleep in those with COPD with most research focusing only on the subgroup diagnosed with chronic bronchitis.14 Yet chronic bronchitis is not often diagnosed within primary care.15,16 While some characteristics of COPD can be studied using medical records and database information, cough and phlegm severity and their burden are best assessed by patient-reported experience and evaluated using patient-reported outcomes (PROs) instruments.17
The main objectives of this study were to estimate the patient-reported prevalence and severity of cough and phlegm and to assess the associated impact and burden among individuals with a diagnosis of COPD. We used data available from the COPD Foundation’s Patient-Powered Research Network (COPD PPRN)18 community to determine if an association is present between reported levels of phlegm and cough, clinical outcomes and quality of life.
Materials and Methods
Our study used PROs data collected from individuals with self-reported physician diagnoses of COPD who are enrolled in the COPD PPRN. This study utilized data from the COPD PPRN Registry established in 2013, maintained by the COPD Foundation and funded by the Patient-Centered Outcomes Research Institute (PCORI) and the Foundation. This online patient research registry has over 7700 consented adults with self-reported COPD enrolled nationally. Each enrolled individual completed baseline surveys querying them about their COPD, presence of comorbid conditions including diabetes, cardiovascular disease and co-existing lung diseases (asthma, bronchiectasis), and COPD exacerbation occurrence as well as completing the COPD Assessment Test (CAT) and the Patient Reported Outcome Measurement Information System (PROMIS-29) that covers emotional, physical and social role functioning. Each PPRN member has an account on a secure platform where they provided electronic consent agreeing to be informed of additional PPRN-sponsored surveys, facilitated by a personalized dashboard. Eligibility criteria for COPD PPRN membership includes being a U.S. resident, 18 years or older and having a self-reported physician diagnosis of COPD/chronic bronchitis/emphysema. The data for this study were taken from the baseline CAT completed at the time of enrollment.
Responses to the first 2 questions of the CAT were used to assess the frequency and severity of cough (question 1) and phlegm (question 2).19 This is a novel method of assessing overall frequency/severity of cough and phlegm on a commonly used COPD management tool, although individual components of the CAT have been explored in previous research.20,21 CAT is a validated patient-completed questionnaire that measures 8 symptoms of COPD on a 0–5 point Likert-type scale.19 For the purposes of this study, frequency and severity of cough and phlegm, questions 1 and 2 of the CAT, were stratified into 3 categories: (1) no/low (CAT scores of 0–1), (2) moderate (CAT scores of 2–3) and (3) high (CAT scores 4–5). The modified Medical Research Council (mMRC) Dyspnea Scale was used to assess dyspnea severity on a 0–4 Likert-type scale.22,23 The Charlson Age-Comorbidity Index (CACI) was calculated using information on self-reported illnesses to measure the burden of comorbidities.24 For the purposes of this study, exacerbations were defined and calculated as the highest number among antibiotic or prednisone use or ED or hospital visits.
The PROMIS-29 instrument was used to evaluate respondents’ quality of life and specific functional abilities such as social and physical role functioning.25,26 PROMIS-29 (v2.0) was designed specifically for use in people with chronic conditions. It encompasses 7 domains (Depression, Anxiety, Physical Function, Pain Interference, Fatigue, Sleep Disturbance, and Ability to Participate in Social Roles and Activities) with 4 questions in each domain.27,28 Per PROMIS-29 scoring guidelines, for 5 out of 7 domains, a score of 50 represents the average for the general U.S. population, and for Ability to Participate in Social Roles and Activities, and Sleep Disturbance, a score of 50 represents the average of a calibration sample enriched for chronic morbidities.27 For negatively worded concepts, such as Depression or Fatigue, a higher PROMIS-29 T-score (above 50) is worse as it represents more of the negative concept being measured. Whereas, for positively worded concepts such as Ability to Participate in Social Roles and Activities, a higher PROMIS-29 T-score (above 50) is better.
Approval for this study was obtained from the Western Institutional Review Board (protocol number: 20141136).
Statistical Analyses
Descriptive statistics were computed and reported as mean (standard deviation [SD]) for continuous variables, and frequencies and proportions for categorical variables. Stratified analyses of main demographic and clinical characteristics were performed by severity levels of cough and phlegm. Values between the strata were compared using Chi-square tests for categorical variables and analysis of variance (ANOVA) for continuous variables. The significance level was set at 0.05. Correlations between cough and phlegm severity levels were evaluated using Kendall's tau-b (τb). Standardized scores of PROMIS-29 domains were calculated and reported as mean (SD) in the overall sample and stratified by cough and phlegm severity levels. Correlations between the 7 domains of PROMIS-29 were assessed using Pearson correlation coefficients. Frequency and patterns of missing PROMIS-29 data were evaluated using the Mutual Imputation procedure in SAS software. One-way multivariate analysis of variance (MANOVA)29 was conducted to identify mean differences of standardized scores of the 7 PROMIS-29 domains across the severity levels of cough and phlegm. Adjusted associations between PROMIS-29 domains and severity levels of both cough and phlegm were controlled for age, gender, and smoking status.
All statistical analyses were performed using SAS 9.4 (SAS Institute, Inc., Cary, North Carolina).
Results
Of the 5314 respondents with self-reported physician-diagnosed COPD in the COPD PPRN at time of analysis, 5286 (99.5%) had sufficient data to assess the severity of cough and phlegm and were included in the analyses. The majority of the participants were women (60.4%) with a mean age of 64.4 years (SD=11.4), predominantly white (87.9%) and approximately half of them were married (51.2%) and 42.2% had caregivers. Most of the respondents (88.2%) reported ever smoking with an average of 45.5 pack years, and 17.8% of ever smokers were current smokers.
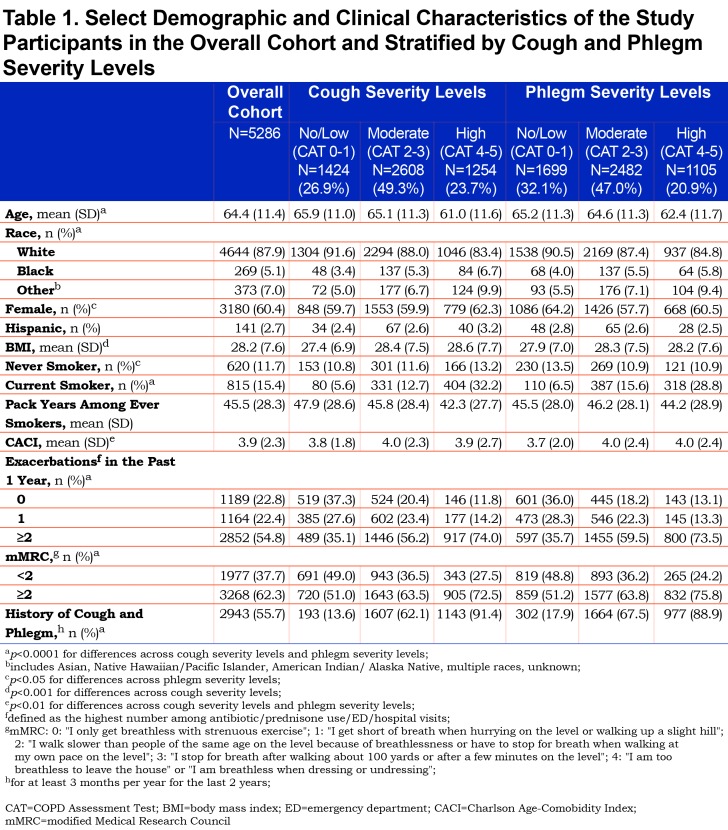
High levels of cough were reported by 23.7%, and moderate levels of cough by 49.3% of the respondents. Approximately a quarter (26.9%) of the participants had no or low cough severity. Phlegm severity levels had similar distribution (Table 1). Respondents with high cough and phlegm frequency/severity were younger compared to those with moderate or no/low severity of these symptoms (p<0.0001) (Table 1). A significantly greater proportion of respondents with high levels of cough (32.2%) reported being current smokers compared to those with moderate or no/low cough (12.7% and 5.6% respectively, p<0.0001). A similar greater proportion of current smokers was detected comparing respondents with high and moderate or no/low levels of phlegm (28.8% versus. 15.6% and 6.5%, p<0.0001) (Table 1). Those with high and moderate cough and phlegm had significantly worse self-reported dyspnea on mMRC (p<0.0001), and greater numbers of exacerbations in the past 1 year compared to those with no/low cough and phlegm (p<0.0001). Two or more exacerbations per year were reported by 74.0% of respondents with high cough severity and 73.5% of those with high phlegm severity, compared to 35.1% among those with no/low cough and 35.7% with no/low phlegm. There was a strong, positive correlation between frequency/severity levels of cough and phlegm as measured by τb (τb=0.599, p<0.01) (online supplement Table 1 (118.4KB, pdf) ). Significantly more respondents with high levels of cough (91.4%) and high levels of phlegm (88.9%) also reported having a history of cough and phlegm for at least 3 months per year for the last 2 years compared to only 13.6% and 17.9% of those with no or low severity of cough and phlegm respectively (p<0.0001) (Table 1).
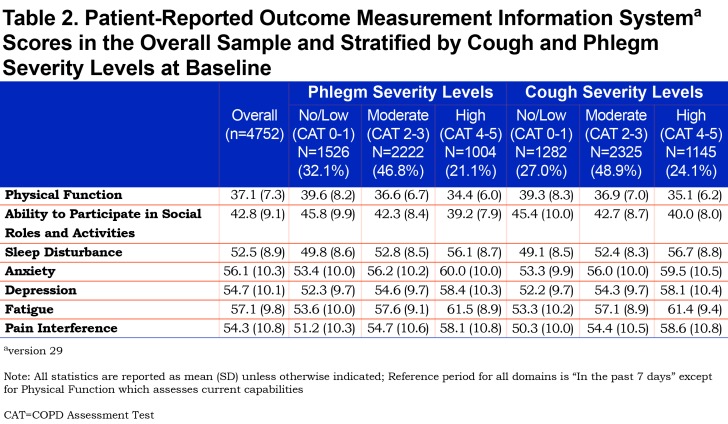
A total of 4752 respondents had complete data on all items in 7 domains of PROMIS-29 and were included in the analyses of quality of life. Analysis of missing data (n=534, 10.1%) did not reveal any obvious patterns. Pearson correlations between the 7 domains of PROMIS-29 were significant (p<0.0001) and ranged from r = -0.27 to r = 0.77. Overall, compared to the average PROMIS-29 scores of 50 (SD=10) for the general U.S. population, our study participants reported significantly lower Physical Function (over 1 SD less than the general U.S. population) and Ability to Participate in Social Roles and Activities, and over half an SD higher score for Anxiety and Fatigue (Table 2).
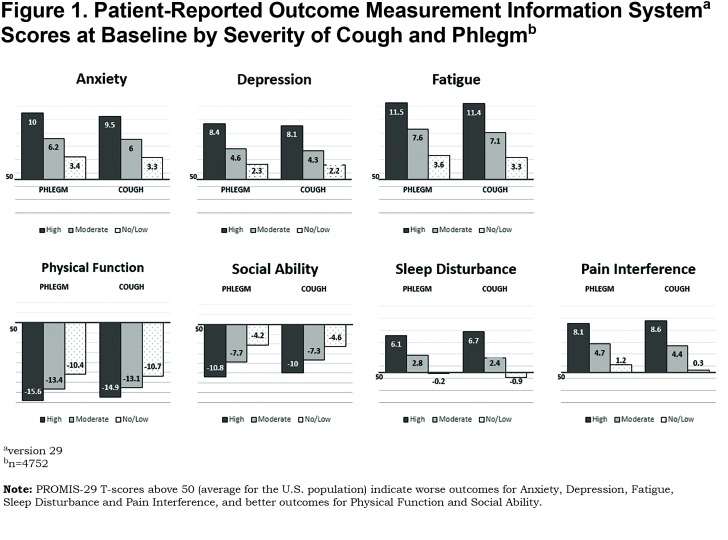
Mean scores of PROMIS-29 domains differed by levels of severity of cough and phlegm (p<0.0001) (Figure 1). There was a stepwise increase in anxiety, depression, fatigue, sleep disturbance and pain interference scores as the severity levels of cough and phlegm increased from no/low to moderate and high. Scores for these domains were on average 1 SD higher in participants with high cough and phlegm compared to the standard U.S. population. Similarly, scores for positively worded domains, such as Physical Function and Ability to Participate in Social Roles and Activities decreased as the severity of cough and phlegm increased. (Figure 1).
The results of the one-way MANOVA29 identified significant mean differences (1 or more) in 7 PROMIS-29 domains’ scores across the severity of cough and phlegm categories (cough: Pillai’s Trace=0.14, F (14, 9488) =49.87, p<0.0001, phlegm: Pillai’s Trace=0.12, F (14, 9488) =44.30, p<0.0001). Adjusted association between severity levels of both cough and phlegm and PROMIS-29 scores from all 7 domains remained significant, controlling for age, gender and smoking status (p<0.0001).
Discussion
In our study, patient-reported cough and phlegm burden was high among these individuals with COPD, with approximately three-fourths of the participants reporting moderate to high levels of cough and/or phlegm. Our findings support previously reported frequency of cough (70%) and phlegm (60%) in patients with COPD in a large international survey and suggests the importance of assessing these symptoms in all COPD patients.10,30 The recent Global initiative for chronic Obstructive Lung Disease (GOLD) statement acknowledged that cough and sputum production in the COPD population may be underreported, perhaps due to limitations of database studies.31 This underlines the importance of symptom burden estimates based on patient-reported data.
Not only were cough and phlegm common in our study cohort, the greater severity and frequency of these 2 symptoms were associated with higher levels of fatigue, anxiety, and depression, greater pain interference and sleep disturbance, and lower social abilities and physical function as measured by PROMIS-29. Recent work by Miravitlles and Ribera also highlighted the association between greater burden of COPD symptoms and high levels of anxiety and depression and worse patient outcomes.32 However, they did not specifically focus on cough and phlegm, aggregating them into overall “COPD symptoms”. Previous work specifically related to the burden of cough and phlegm is limited in the overall COPD population.10 Research that did focus on frequent and persistent cough and sputum production was usually limited to the chronic bronchitis phenotype of COPD in which cough and phlegm are part of the diagnostic criteria and often diagnosed only within lung specialists’ practices.32-34
In this study, over a half of the overall cohort had 2 or more exacerbations in the past year with significantly more exacerbations among individuals with greater cough and phlegm severity.
The large multicenter COPD Genetic Epidemiology study identified significant association between presence of chronic bronchitis symptoms in patients with COPD and history of exacerbations and hospitalizations.14 Similar to our study, the authors also identified that individuals with symptoms of chronic bronchitis were younger and had a greater smoking history and dyspnea.14 A recent study by Kim et al further highlighted the association between cough and phlegm production and exacerbations.35 One of the suggested hypotheses supporting this association was that these 2 symptoms serve as markers of a specific mucus-producing COPD endotype.36
Recent research in Sweden reported that productive cough in COPD patients was associated with exacerbations and risk for death.37 Cough has also been shown to be associated with decline in general health status of patients with airflow obstruction and with disability in COPD.10 Similar associations between chronic bronchitis symptoms and higher exacerbation frequency, dyspnea and worse general health status including physical activity limitations were reported by the researchers of the PLATINO study.38 A recent prospective SPIROMICS study of patients with COPD reported only 10% of the participants having 2 or more exacerbations in the preceding year.39 Of note, less than a quarter of patients in that cohort were reported as having a chronic bronchitis.
In patients with COPD, morning difficulties with cough (60.1%) and phlegm (70.9%) are common and have been shown to affect activities such as washing (41.0%) and dressing (40.7%) among participants in a large European study.40 Both early-morning and nighttime symptoms such as cough and phlegm have been shown to be associated with worse HRQoL.32,41,42
The results of the patient-reported decline in social and physical role functioning and increase in anxiety and depression symptoms compared to the general population and those with other chronic diseases is of special interest in better understanding the burden of cough and phlegm. Findings of a multicenter cross-sectional study supported the validity of PROMIS in patients with COPD and identified that among all domains, physical functioning was most negatively affected compared to the general population across all COPD severity grades.43 Consistent with these findings, our study results also indicate the worst standardized scores in Physical Function (over 1 SD worse than the average scores for the general U.S. population) among all 7 PROMIS-29 domains across all cough and phlegm severity levels.
Despite the repeatedly demonstrated negative impact of cough and phlegm in people with COPD, currently only a few pharmacotherapies directly address either of these symptoms.7,31 The findings of our study highlight the need to review and renew the search for therapies designed to reduce cough and phlegm. Symptom relief has been highlighted as one of the main goals of COPD management.44,45 Few and perhaps only 1 effective cough medication has been developed by the pharmaceutical industry in over a century.10,46 Only about a third of the participants in our study had either no or low severity of cough or phlegm. Higher frequency and severity of these symptoms was associated with worse mood, pain, sleep and physical and social functioning. High levels of cough and phlegm might also be explored as a proxy for COPD disease severity or an independent association in risk prediction models. The consistent association between high burden of cough and phlegm and worse quality of life suggests the need for further research in this area.47
Strengths and Limitations
The main strengths of our study include the large number of individuals enrolled in the COPD PPRN with data available for these analyses as well as unique and rich patient assessed data on seldom-addressed patient-reported outcomes such as ability to participate in social roles and activities, physical function, anxiety, depression, and sleep disturbance. Limitations of the study include potential selection bias in view of the self-reported nature of physician-diagnosed COPD. Patient-reported clinical information including presence of comorbidities, frequency of physician visits, ED visits and hospitalizations are subject to a potential recall bias. Classification of cough and phlegm frequency/severity levels were based on a novel use of the individual questions of the CAT which have only been validated for use as a total score. Use of the 2 items from the CAT to assess the burden of these 2 symptoms (cough and phlegm) is not meant to substitute for a diagnostic evaluation. CAT has been developed specifically to assess symptom burden in individuals with COPD. The findings of this study may not be generalizable to all individuals with COPD due to the age, COPD severity, ethnic and racial distribution of the study population.
Conclusion
In this population of people with self-reported, physician diagnosed COPD, severity of cough and phlegm is associated with more exacerbations, greater dyspnea, and worsened patient-reported quality of life including physical and social functioning. Further work in this area is needed including exploration of new treatments aimed at improvement of cough and phlegm severity in this patient population.
Abbreviations
chronic obstructive pulmonary disease, COPD; COPD Patient-Powered Research Network, COPD-PPRN; Patient-Reported Outcome Measurement Information System, PROMIS-29; multivariate analysis of variance, MANOVA; emergency department, ED; health-related quality of life, HRQoL; patient-reported outcomes, PROs; Patient-Centered Outcomes Research Institute, PCORI; modified Medical Research Council, mMRC; Charlson Age-Comorbidity Index, CACI; standard deviation, SD; analysis of variance, ANOVA; Kendall’s tau-b, τb Global initiative for chronic Obstructive Lung Disease, GOLD
Funding Statement
This study was funded through a Patient-Centered Outcomes Research Institute® (PCORI®) Award (PPRN-1306-04748 Phase II) for the development of the National Patient-Centered Clinical Research Network, known as PCORnet® and through the COPD Foundation, Washington, DC. The statements presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute® (PCORI®), its Board of Governors or Methodology Committee or other participants in PCORnet®.
References
- 1.Foster TS,Miller JD,Marton JP,Caloyeras JP,Russell MW,Menzin J. Assessment of the economic burden of COPD in the US: a review and synthesis of the literature. COPD. 2006;3(4):211-218. doi: https://doi.org/10.1080/15412550601009396 [DOI] [PubMed] [Google Scholar]
- 2.Kochanek K,Murphy S,Xu J,Arias E. Mortality in the United States, 2016. NCHS Data Brief. 2017;293. [PubMed] [Google Scholar]
- 3.Choate R,Mannino DM. Chronic obstructive pulmonary disease: epidemiology, clinical presentation, and evaluation. J Clin Outcomes Manag. 2017;24(4):172-180. [Google Scholar]
- 4.Ford ES,Croft JB,Mannino DM,Wheaton AG,Zhang X,Giles WH. COPD surveillance-United States, 1999-2011. Chest. 2013;144(1):284-305. doi: https://doi.org/10.1378/chest.13-0809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller JD,Foster T,Boulanger L,et al. Direct costs of COPD in the US: an analysis of Medical Expenditure Panel Survey (MEPS) data. COPD. 2005;2(3):311-318. doi: https://doi.org/10.1080/15412550500218221 [DOI] [PubMed] [Google Scholar]
- 6.Mannino DM,Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007;370(9589):765-773. doi: https://doi.org/10.1016/S0140-6736(07)61380-4 [DOI] [PubMed] [Google Scholar]
- 7.Vogelmeier CF,Criner GJ,Martinez FJ,et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 Report. GOLD executive summary. Am J Respir Crit Care. 2017;195(5):557-582. doi: https://doi.org/10.1164/rccm.201701-0218PP [DOI] [PubMed] [Google Scholar]
- 8.Ding B,DiBonaventura M,Karlsson N,Bergström G,Holmgren U. A cross-sectional assessment of the burden of COPD symptoms in the US and Europe using the National Health and Wellness Survey. Int J Chron Obstruct Pulmon Dis. 2017;12:529-539. doi: https://doi.org/10.2147/COPD.S114085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones PW,Agusti AG. Outcomes and markers in the assessment of chronic obstructive pulmonary disease. Eur Respir J. 2006;27(4):822-832. doi: https://doi.org/10.1183/09031936.06.00145104 [DOI] [PubMed] [Google Scholar]
- 10.Smith J,Woodcock A. Cough and its importance in COPD. Int J Chron Obstruct Pulmon Dis. 2006;1(3):305-314. doi: https://doi.org/10.2147/copd.2006.1.3.305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srivastava K,Thakur D,Sharma S,Punekar YS. Systematic review of humanistic and economic burden of symptomatic chronic obstructive pulmonary disease. Pharmaco Econ. 2015;33(5):467-488. doi: https://doi.org/10.1007/s40273-015-0252-4 [DOI] [PubMed] [Google Scholar]
- 12.Bhullar S,Phillips B. Sleep in COPD patients. COPD. 2005;2(3):355-361. doi: https://doi.org/10.1080/15412550500274836 [DOI] [PubMed] [Google Scholar]
- 13.Miravitlles M,Worth H,Cataluña JJS,et al. Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Resp Res. 2014;15(1):122. doi: https://doi.org/10.1186/s12931-014-0122-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim V,Han MK,Vance GB,et al. The chronic bronchitic phenotype of COPD: an analysis of the COPDGene study. Chest. 2011;140(3):626-633. doi: https://doi.org/10.1378/chest.10-2948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Van Schayck C,Loozen J,Wagena E,Akkermans R,Wesseling G. Detecting patients at a high risk of developing chronic obstructive pulmonary disease in general practice: cross sectional case finding study. BMJ. 2002;324(7350):1370. doi: https://doi.org/10.1136/bmj.324.7350.1370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takahashi T,Ichinose M,Inoue H,Shirato K,Hattori T,Takishima T. Underdiagnosis and undertreatment of COPD in primary care settings. Respirology. 2003;8(4):504-508. doi: https://doi.org/10.1046/j.1440-1843.2003.00501.x [DOI] [PubMed] [Google Scholar]
- 17.Mocarski M,Zaiser E,Trundell D,Make BJ,Hareendran A. Evaluation of the psychometric properties of the Nighttime Symptoms of COPD instrument. Int J Chron Obstruct Pulmon Dis. 2015;10:475-487. doi: https://doi.org/10.2147/COPD.S75776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daugherty SE,Wahba S,Fleurence R,et al. (for the PCORnet PPRN Consortium). Patient-powered research networks: building capacity for conducting patient-centered clinical outcomes research. J Am Med Inform Assoc. 2014;21(4):583-586. doi: https://doi.org/10.1136/amiajnl-2014-002758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones PW,Harding G,Berry P,Wiklund I,Chen WH,Leidy NK. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648-654. doi: https://doi.org/10.1183/09031936.00102509 [DOI] [PubMed] [Google Scholar]
- 20.Houben-Wilke S,Janssen DJA,Franssen FME,Vanfleteren LEGW,Wouters EFM,Spruit MA. Contribution of individual COPD assessment test (CAT) items to CAT total score and effects of pulmonary rehabilitation on CAT scores. Heal Qual Life Outcome. 2018;16(1):205. doi: https://doi.org/10.1186/s12955-018-1034-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Raghavan N,Lam Y-M,Webb KA,et al. Components of the COPD Assessment Test (CAT) associated with a diagnosis of COPD in a random population sample. COPD. 2012;9(2):175-183. doi: https://doi.org/10.3109/15412555.2011.650802 [DOI] [PubMed] [Google Scholar]
- 22.Stenton C. The MRC breathlessness scale. Occup Med. 2008;58(3):226-227. doi: https://doi.org/10.1093/occmed/kqm162 [DOI] [PubMed] [Google Scholar]
- 23.Hsu KY,Lin JR,Lin MS,Chen W,Chen YJ,Yan YH. The modified Medical Research Council dyspnoea scale is a good indicator of health-related quality of life in patients with chronic obstructive pulmonary disease. Singapore Med J. 2013;54(6):321-327. doi: https://doi.org/10.11622/smedj.2013125 [DOI] [PubMed] [Google Scholar]
- 24.Charlson M,Szatrowski TP,Peterson J,Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245-1251. doi: https://doi.org/10.1016/0895-4356(94)90129-5 [DOI] [PubMed] [Google Scholar]
- 25.Cella D,Riley W,Stone A,et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179-1194. doi: https://doi.org/10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rose M,Bjorner JB,Gandek B,Bruce B,Fries JF,Ware JE. The PROMIS Physical Function item bank was calibrated to a standardized metric and shown to improve measurement efficiency. J Clin Epidemiol. 2014;67(5):516-526. doi: https://doi.org/10.1016/j.jclinepi.2013.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Health Measures; PROMIS Adult Profile Instruments. Health Measures website. http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Adult_Profile_Scoring_Manual.pdf Published 2018 Accessed September 2018. [Google Scholar]
- 28.Cook KF,Jensen SE,Schalet BD,et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J Clin Epidemiol. 2016;73:89-102. doi: https://doi.org/10.1016/j.jclinepi.2015.08.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cole PJ. Inflammation: a two-edged sword--the model of bronchiectasis. Eur J Resp Dis-Suppl. 1986;147:6-15. [PubMed] [Google Scholar]
- 30.Rennard S,Decramer M,Calverley PMA,et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J. 2002;20(4):799. doi: https://doi.org/10.1183/09031936.02.03242002 [DOI] [PubMed] [Google Scholar]
- 31.Gao Y-h,Guan W-j,Zhu Y-n,Chen R-c,Zhang G-j. Antibiotic-resistant Pseudomonas aeruginosa infection in patients with bronchiectasis: prevalence, risk factors and prognostic implications. Int J Chron Obstruct Pulmon Dis. 2018;13:237. doi: https://doi.org/10.2147/COPD.S150250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miravitlles M,Ribera A. Understanding the impact of symptoms on the burden of COPD. Resp Res. 2017;18(1):67. doi: https://doi.org/10.1186/s12931-017-0548-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Landis SH,Muellerova H,Mannino DM,et al. Continuing to confront COPD international patient survey: methods, COPD prevalence, and disease burden in 2012-2013. Int J Chron Obstruct Pulmon Dis. 2014;9:597. doi: https://doi.org/10.2147/COPD.S61854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miravitlles M. Cough and sputum production as risk factors for poor outcomes in patients with COPD. Respir Med. 2011;105(8):1118-1128. doi: https://doi.org/10.1016/j.rmed.2011.02.003 [DOI] [PubMed] [Google Scholar]
- 35.Kim V,Zhao H,Regan E,et al. The St. George's Respiratory Questionnaire definition of chronic bronchitis may be a better predictor of COPD exacerbations compared with the classic definition. Chest. 2019;156(4):685-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martin C,Burgel P-R. Do cough and sputum production predict COPD exacerbations?: The evidence is growing. Chest. 2019;156(4):641-642. doi: https://doi.org/10.1016/j.chest.2019.06.023 [DOI] [PubMed] [Google Scholar]
- 37.Lindberg A,Sawalha S,Hedman L,Larsson L-G,Lundbäck B,Rönmark E. Subjects with COPD and productive cough have an increased risk for exacerbations and death. Respir Med. 2015;109(1):88-95. doi: https://doi.org/10.1016/j.rmed.2014.12.001 [DOI] [PubMed] [Google Scholar]
- 38.de Oca MM,Halbert RJ,Lopez MV,et al. The chronic bronchitis phenotype in subjects with and without COPD: the PLATINO study. Eur Respir J. 2012;40(1):28-36. doi: https://doi.org/10.1183/09031936.00141611 [DOI] [PubMed] [Google Scholar]
- 39.Han MK,Quibrera PM,Carretta EE,et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5(8):619-626. doi: https://doi.org/10.1016/S2213-2600(17)30207-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kessler R,Partridge MR,Miravitlles M,et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J. 2011;37(2):264-272. doi: https://doi.org/10.1183/09031936.00051110 [DOI] [PubMed] [Google Scholar]
- 41.Price D,Small M,Milligan G,Higgins V,Gil EG,Estruch J. Impact of night-time symptoms in COPD: a real-world study in five European countries. Int J Chron Obstruct Pulmon Dis. 2013;8:595. doi: https://doi.org/10.2147/COPD.S48570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stephenson JJ,Cai Q,Mocarski M,Tan H,Doshi JA,Sullivan SD. Impact and factors associated with nighttime and early morning symptoms among patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:577. doi: https://doi.org/10.2147/COPD.S76157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lin F-J,Pickard AS,Krishnan JA,et al. Measuring health-related quality of life in chronic obstructive pulmonary disease: properties of the EQ-5D-5L and PROMIS-43 short form. BMC Med Res Meth. 2014;14(1):78. doi: https://doi.org/10.1186/1471-2288-14-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Global Initiative for Chronic Obstructive Lung Disease (GOLD) Pocket guide to COPD diagnosis, management and prevention. A guide for health care professionals. 2018 report. GOLD website. https://goldcopd.org/wp-content/uploads/2018/02/WMS-GOLD-2018-Feb-Final-to-print-v2.pdf Published 2018 Accessed December 5, 2018. [Google Scholar]
- 45.Agusti A,Calverley PMA,Celli B,et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Resp Res. 2010;11(1):122. doi: https://doi.org/10.1186/1465-9921-11-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dicpinigaitis PV,Morice A,Birring S,et al. Antitussive drugs-past, present, and future. Pharm Rev. 2014;66(2):468-512. doi: https://doi.org/10.1124/pr.111.005116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Birring SS,Kavanagh JE,Irwin RS,et al. Treatment of interstitial lung disease associated cough: CHEST guideline and expert panel report. Chest. 2018;154(4):904-917. doi: https://doi.org/10.1016/j.chest.2018.06.038 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This article contains supplemental material.