Abstract
Background
The importance of management of metabolic syndrome (MetS) for risk reduction of cardiovascular disease (CVD) has been recognized worldwide. Because of the comparatively unique characteristics of bodily figure/obesity and incident CVD in Japan, the relevance of MetS on CVD can be still discussed among Japanese people. The present study aimed to review briefly the relationship of MetS with CVD morbidity/mortality among general Japanese people.
Methods
Population-based prospective cohort studies evaluating the predictive value of MetS on CVD morbidity/mortality via a PubMed search up to 2019 were summarized.
Results
We identified two studies on morbidity that reported MetS to predict CVD morbidity. We identified three studies on mortality, and these studies showed an increased direction of hazard ratio (HR) of CVD mortality, while one study reported an insignificant prediction of MetS for CVD mortality. In the meta-analysis method, MetS significantly predicted CVD morbidity (HR=1.71 [95% confidence interval=1.34–2.18] in men and HR=1.89 [95% confidence interval=1.45–2.46] in women) as well as CVD mortality (HR=1.68 [95% confidence interval=1.37–2.06] in men and HR=1.73 [95% confidence interval=1.39–2.15] in women).
Conclusion
Among general Japanese people, MetS can be a positive predictor of CVD morbidity/mortality. Since the studies are limited, more research is needed to establish the findings.
Keywords: cardiometabolic health, disease morbidity, disease mortality, obesity
Introduction
Metabolic syndrome (MetS) is marked by an accumulation of atherosclerotic risk factors, such as obesity, diabetes mellitus, hypertension and dyslipidemia.1 The biological mechanism underlying the relationship between MetS and cardiovascular disease (CVD) is often explained by obesity-related pathophysiology including insulin resistance and unhealthy lifestyle as a common basis.1–3 The harmful influence of MetS on CVD has been demonstrated in international studies.4–6 Thus, the risk management of MetS for cardiovascular health has been importantly recognized.1–3
Obesity plays a central role in MetS.2,3 Approximately 30% of men and 20% of women are currently classified as obese (body mass index [BMI] ≥25 kg/m2) in Japan.7 Of interest, the proportion of BMI ≥30 kg/m2 in Japan is one tenth that in the United States, while the proportion of pre-obesity (25.0 to 29.9 kg/m2) is similar between the two countries.8,9
While CVD is a leading cause of death in developed countries, Japanese people are characterized by a lower mortality due to coronary heart disease than Western populations.10 The healthcare system of Japan (i.e., a free-access system to any medical institutions providing intensive therapy and close follow-up for CVD patients) may be a reason for such a low CVD mortality.11–13 The characteristics of obesity and CVD in Japan are different from those in Western countries; thus, the relevance of MetS on CVD can be still discussed among Japanese people.7–10,14
The summary of data specific to Japanese people can give an insight into the understanding of MetS on risk management of CVD. Although prior international review papers included the Japanese studies,4–6 all studies of general Japanese people were not always included. Therefore, the current study reviewed briefly, based on available cohort studies, the relationship between MetS and CVD morbidity/mortality in general Japanese people.
Materials and Methods
Candidate articles were searched using a PubMed search engine. The articles were searched for mentions of either morbidity or mortality. In the search of morbidity, the keywords were “metabolic syndrome”, “cardiovascular disease”, “cohort study”, “Japan”, and “morbidity”. In the search of mortality, the keywords were “metabolic syndrome”, “cardiovascular disease”, “cohort study”, “Japan”, and “mortality”. The term CVD basically included coronary heart disease (myocardial infarction, angina pectoris, ischemic heart failure) and stroke (cerebral infarction, cerebral hemorrhage). The search was performed for articles published between January 1966 and December 2019. The exclusion criteria for the selection of articles were as follows: not a human study, not an adult population, and not written in English.
First, the title and the abstract were investigated by two researchers independently. Non-cohort studies and original articles that did not focus on MetS-CVD morbidity/mortality relationship were excluded. When these researcher’s opinions matched, the articles were deemed appropriate for advancing to the next step. If their opinions did not match, they discussed whether or not the articles were appropriate.
Second, the full text was evaluated, and articles that met all of the following inclusion criteria were selected: (1) number of participants ≥1000; (2) ≥10 years of follow-up; (3) MetS defined; (4) CVD morbidity or mortality described; and (5) hazard ratio (HR) and 95% confidence interval (CI) described. When multi-variate estimates were reported, the most fully adjusted estimate was used.
Third, the two researchers reviewed and confirmed, with each other, the content of the articles. The summary tables of the respective articles were then created.
Furthermore, based on the articles, a (mini)meta-analysis of MetS for CVD morbidity/mortality was conducted using the generic inverse variance method with Review Manager (RevMan; computer program) 5.3.15 The results were expressed as HR (95% CI).
Results
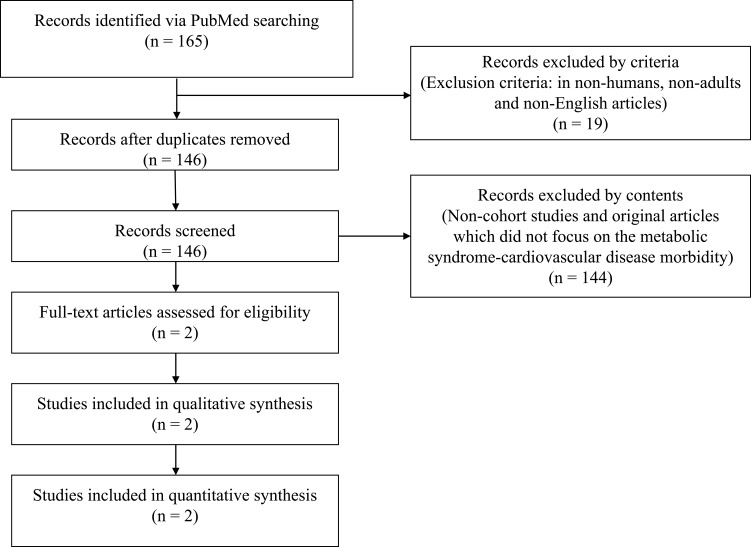
Figure 1 shows the flow for selecting articles that examined the relationship between MetS and CVD morbidity. Of the initial articles identified, 19 were excluded based on the exclusion criteria mentioned above. Of the remaining articles, 146 were further excluded for not being performed in a prospective cohort study design and not focusing on the relationship between MetS and CVD morbidity. Ultimately, two articles that met the criteria were selected.16,17
Figure 1.
Flow chart of article selection: Metabolic syndrome and cardiovascular disease morbidity.
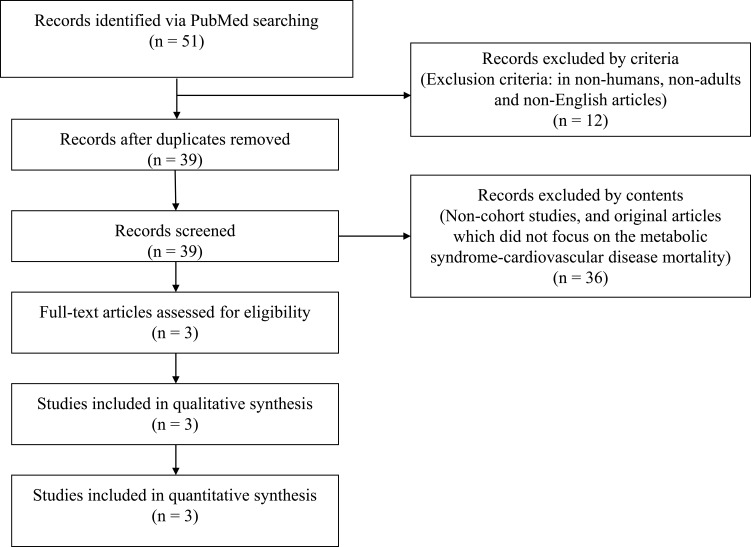
Similar to the selection for CVD morbidity, Figure 2 shows the process used to select articles that examined the relationship between MetS and CVD mortality. Of the initial articles identified, 12 were excluded based on the exclusion criteria mentioned above. Of the remaining articles, 36 were further excluded for not being performed in a prospective cohort study design and not focusing on the relationship between MetS and CVD mortality. Ultimately, three articles that met the criteria were selected.18–20
Figure 2.
Flow chart of article selection: Metabolic syndrome and cardiovascular disease mortality.
MetS and CVD Morbidity
Two cohort studies that examined the predictive value of MetS on CVD morbidity for general Japanese people were summarized (Table 1). In the Suita study,16 the total number of study participants were 5332 (2492 men and 2840 women), and the observation period was 12.5 years. In the Hisayama study,17 the total number of study participants were 2452 (1050 men and 1402 women), and the observation period was 14 years. Both studies reported MetS to predict CVD morbidity.16,17 In both studies, the predictive value of MetS on CVD morbidity might be high especially in women.16,17 Predicting the morbidity of coronary heart disease tended to be similar to that of stroke.16,17 The prediction of morbidity also appeared to be similar regardless of the definition of MetS, even though there were some differences in the definition between the two studies.16,17 Furthermore, MetS significantly predicted CVD morbidity in the meta-analysis (by National Cholesterol Education Program - the third revision of Adult Treatment Panel [NCEP-ATPIII]-based definition) as follows: HR=1.71 (95% CI=1.34–2.18) in men and HR=1.89 (95% CI=1.45–2.46) in women.
Table 1.
Summary of the Predictive Value of MetS on CVD Morbidity
| Study | Participants (n) | Age (Years) | Follow-Up (Years) | Definition of MetS (Abdominal Obesity) | CVD Incidence | Coronary Heart Disease | Stroke | |||
|---|---|---|---|---|---|---|---|---|---|---|
| n | HR (95% CI) | n | HR (95% CI) | n | HR (95% CI) | |||||
| Suita Studya [Kokubo Y, et al]16 | M: 2492 | 30–79 | 12.5 | Japanese | M: 48 | 1.34 (0.96–1.87) | M: 22 | 1.51 (0.91–2.48) | M: 26 | 1.27 (0.81–1.97) |
| W: 2840 | (Waist circumference) | W: 19 | 2.20 (1.31–3.68) | W: 7 | 2.70 (1.15–6.35) | W: 12 | 2.05 (1.07–3.92) | |||
| NCEP-ATPIII (Asian) | M: 55 | 1.75 (1.27–2.41) | M: 26 | 2.12 (1.31–3.43) | M: 29 | 1.58 (1.02–2.43) | ||||
| (Waist circumference) | W: 56 | 1.90 (1.31–2.77) | W: 21 | 2.77 (1.44–5.32) | W: 35 | 1.62 (1.02–2.58) | ||||
| Hisayama Studyb [Doi Y, et al]17 | M: 1050 | ≥40 | 14 | Japanese | M: 34 | 1.28 (0.86–1.91) | – | – | – | – |
| W: 1402 | (Waist circumference) | W: 19 | 1.89 (1.15–3.10) | – | – | – | – | |||
| Modified Japanese | M: 24 | 2.49 (1.57–3.94) | – | – | – | – | ||||
| (Waist circumference) | W: 47 | 2.27 (1.55–3.32) | – | – | – | – | ||||
| Modified NCEP-ATPIII | M: 40 | 1.66 (1.14–2.43) | – | – | – | – | ||||
| (Waist circumference) | W: 62 | 1.88 (1.30–2.74) | – | – | – | – | ||||
Notes: aAdjusted Confounders: age, smoking, drinking. bAdjusted Confounders: age, proteinuria, cholesterol, electrocardiogram abnormalities, alcohol, exercise, smoking. The bold text shows a HR (95% CI) level with a significance of P<0.05.
Abbreviations: MetS, metabolic syndrome; CVD, cardiovascular disease; n, number; M, men; W, women; HR, hazard ratio; CI, confidence interval, NCEP-ATPIII, National Cholesterol Education Program - the third revision of Adult Treatment Panel.
MetS and CVD Mortality
Three cohort studies that examined the predictive value of MetS on CVD mortality for general Japanese people were summarized (Table 2). In the Jichi Medical School Study,18 the total number of study participants were 2176 (914 men and 1262 women), and the observation period was 12.5 years. In the JPHC study,19 the total number of study participants were 34,051 (12,412 men and 21,639 women), and the observation period was 12.3 years. In the Ibaraki Prefectural Health Study,20 the total number of study participants were 91,157 (30,774 men and 60,383 women), and the observation period was 12 years. In the Jichi Medical School Study,18 MetS did not significantly predict CVD mortality, although a trend for its prediction of CVD mortality was observed. In the JPHC study19 and Ibaraki Prefectural Health Study,20 MetS significantly predicted CVD mortality. The predictive values of morbidity for coronary heart disease seemed to be high in comparison to those for stroke.18–20 The prediction of morbidity was not largely influenced by the definition of MetS.18–20 Furthermore, MetS significantly predicted CVD mortality in the meta-analysis (by the Japanese definition for the Jichi Medical School Study18 and NCEP-ATPIII-based definition for the JPHC study19 and the Ibaraki Prefectural Health Study20) as follows: HR=1.68 (95% CI=1.37–2.06) in men and HR=1.73 (95% CI=1.39–2.15) in women.
Table 2.
Summary of the Predictive Value of MetS on CVD Mortality
| Study | Participants (n) | Age (Years) | Follow-Up (Years) | Definition of MetS (Abdominal Obesity) | CVD Mortality | Coronary Heart Disease | Stroke | |||
|---|---|---|---|---|---|---|---|---|---|---|
| n (rate) | HR (95% CI) | n | HR (95% CI) | n | HR (95% CI) | |||||
| Jichi Medical School Studya [Niwa Y, et al]18 | M: 914 | 40–69 | 12.5 | Japanese | M: 5 (5.0d) | 1.84 (0.68–4.96) | - | - | - | - |
| W: 1262 | (Waist circumference) | W: 1 (3.6d) | 1.31 (0.17–9.96) | - | - | - | - | |||
| JPHC Studyb [Saito I, et al]19 | M: 12,412 | 40–69 | 12.3 | Japanese | M: 177 | 1.54 (1.02–2.31) | M: 71 | 1.91 (1.05–3.48) | M: 106 | 1.31 (0.75–2.29) |
| W: 21,639 | (BMI) | W: 127 | 1.31 (0.79–2.18) | W: 38 | 2.56 (1.19–5.48) | W: 89 | 0.88 (0.44–1.77) | |||
| NCEP-ATPIII | M: 177 | 1.41 (0.99–2.02) | M: 71 | 1.76 (1.03–3.01) | M: 106 | 1.20 (0.74–1.94) | ||||
| (BMI) | W: 127 | 1.44 (0.98–2.11) | W: 38 | 1.90 (0.97–3.74) | W: 89 | 1.26 (0.79–2.03) | ||||
| Ibaraki Prefectural Health Studyc [Irie F, et al]20 | M: 30,774 | 40–79 | 12 | NCEP-ATPIII | M: 226 | 1.83 (1.41–2.38) | M: 85 | 2.54 (1.55–4.15) | M: 51 | 1.38 (0.84–2.27) |
| W: 60,383 | (BMI) | W: 322 | 1.90 (1.45–2.49) | W: 79 | 2.20 (1.24–3.89) | W: 79 | 2.37 (1.26–4.46) | |||
Notes: aAdjusted Confounders: age, smoking, alcohol. bAdjusted Confounders: age, dietary, smoking, alcohol, exercise. cAdjusted Confounders: age, smoking, alcohol, dietary, cholesterol. dRates of mortality: adjusted for per 1000 person-years. The bold text shows a HR (95% CI) level with a significance of P<0.05.
Abbreviations: MetS, metabolic syndrome; CVD, cardiovascular disease; n, number; HR, hazard ratio; CI, confidence interval; M, men; W, women; BMI, body mass index; NCEP-ATPIII, National Cholesterol Education Program - the third revision of Adult Treatment Panel.
Discussion
The current review summarized the relationship between MetS and CVD among general Japanese people using population-based prospective cohort studies. Although we must acknowledge the limited numbers of such reliable studies, summarizing the current position will help promote further advances in this research field due to the unique characteristics of obesity and CVD in Japan (i.e., the prevalence of severe obesity and incident CVD has not been historically very high compared to that in Western countries).7–10 In the current review, MetS was found to be a possibly positive predictor of CVD morbidity/mortality. The results in the current review are mostly in accordance with those of prior international studies.2–4 In spite of the unique characteristics of obesity and CVD in Japan,7–10 the similar finding of the relationship between MetS and CVD morbidity/mortality across any country is of interest in the understanding of the pathophysiology of MetS and its involvement in CVD.
In terms of the MetS-CVD relationship, the relevance of the component of MetS on CVD morbidity/mortality is a concern. In the current review, not a specific component factor but the accumulated component number of MetS was suggested to increase the risk of CVD.16,17 On the other hand, high blood pressure is a major component of MetS21 and there has been a study showing hypertension as one of the strongest risk components of MetS for CVD.22 Such a detailed concern of the MetS-CVD relationship remains to be studied.
While there were only a few studies16,19,20 regarding stroke in the current study, we noted that stroke mortality could tend to reduce compared to stroke morbidity. In general, people with the development of stroke are not fatal on the instant and receive long-term careful care.23 It can partly explain the weak relevance of MetS on stroke mortality.
In the current review, the predictive value of CVD mortality/morbidity might have been slightly high in women relative to men. The phenomenon has been observed in prior international studies.2–4 Researchers have suggested gender differences in the definition of MetS as a reason for this, although the overall results of the current review for CVD morbidity/mortality did not necessarily depend on the definition of MetS. Only the Japanese definition of MetS originally sets a higher cut-off level of waist circumference for women than for men (i.e. ≥85 cm for men, ≥90 cm for women), in contrast to the definition of MetS set in other countries.24–26 There can be also some other biological reasons affecting the results of gender difference, as gender-specific influences of sex hormones and adipocytokines on CVD in relation to obesity and MetS.27,28 A low-grade systemic inflammation is well known to contribute to the development of CVD.29 Even though the C-reactive protein levels are similar between genders, adiposity is more strongly positively associated with a low-grade systemic inflammation, as reflected in circulating C-reactive protein, in women than in men.30–33 This may be a mechanistic explanation for the gender difference. The presumable gender-related prediction of MetS for CVD outcomes remains an issue to be further examined.
Considering the findings of the current study, preventative strategies of MetS against CVD for general Japanese people must be promoted. Besides drug prescription for metabolic disorders, lifestyle modifications including healthy eating and exercise with weight reduction/maintenance are a basic intervention as a universal approach. Public health check-up screening programs and post-screening health educational systems have already begun in Japan.34 Also, the management of MetS at personalized, organizational and population levels is currently introduced.34 A higher-salt intake is seen in Japan than in Western countries35 and such a high salt intake induces insulin resistance associated with hypertension and MetS.36 Thus, the initiatives of salt reduction may be effective for risk reduction of MetS and related CVD in Japan in particular.
Several limitations associated with the present study warrant mention. Some studies included relatively few participants with CVD outcomes, which is often unavoidable due to the low incidence of CVD in Japan.10 Most studies might not have had a sufficiently long period to observe the development of CVD outcomes, especially mortality, as long-term care for a long lifespan is provided to Japanese people with CVD.11–13 In addition, the confounding factors in the adjusted analyses differed among the reviewed studies.
Conclusion
In this review, MetS was found to be a possibly positive predictor of CVD morbidity/mortality among general Japanese people. Since the available studies are limited, more research is needed for the further establishment of the relationship between MetS and CVD in Japan.
Funding Statement
The authors received no financial support for the research, authorship, and/or publication of this article.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest.
References
- 1.Meigs JB. Invited commentary: insulin resistance syndrome? Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol. 2000;152:908–911. doi: 10.1093/aje/152.10.908 [DOI] [PubMed] [Google Scholar]
- 2.Haslam DW, James WP. Obesity. Lancet 2005; 366: 1197–1209. doi: 10.1016/S0140-6736(05)67483-1 [DOI] [PubMed] [Google Scholar]
- 3.Müller MJ, Lagerpusch M, Enderle J, et al. Beyond the body mass index: tracking body composition in the pathogenesis of obesity and the metabolic syndrome. Obes Rev. 2012;13:6–13. doi: 10.1111/j.1467-789X.2012.01033.x [DOI] [PubMed] [Google Scholar]
- 4.Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119:812–819. doi: 10.1016/j.amjmed.2006.02.031 [DOI] [PubMed] [Google Scholar]
- 5.Gami AS, Witt BJ, Howard DE, et al. Metabolic syndrome and risk of incident cardiovascular events and death: a systematic review and meta-analysis of longitudinal studies. J Am Coll Cardiol. 2007;49:403–414. doi: 10.1016/j.jacc.2006.09.032 [DOI] [PubMed] [Google Scholar]
- 6.Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 2010;56:1113–1132. doi: 10.1016/j.jacc.2010.05.034 [DOI] [PubMed] [Google Scholar]
- 7.Yoshiike N, Miyoshi M. Epidemiological aspects of overweight and obesity in Japan–international comparisons. Nihon Rinsho. 2013;71:207–216. [PubMed] [Google Scholar]
- 8.Yang L, Colditz GA. Prevalence of overweight and obesity in the United States, 2007–2012. JAMA Intern Med. 2015;175:1412–1413. doi: 10.1001/jamainternmed.2015.2405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kivimäki M, Kuosma E, Ferrie JE, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. 2017;2:e277—285. doi: 10.1016/S2468-2667(17)30074-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ueshima H. Explanation for the Japanese paradox: prevention of increase in coronary heart disease and reduction in stroke. J Atheroscler Thromb. 2007;14:278–286. doi: 10.5551/jat.E529 [DOI] [PubMed] [Google Scholar]
- 11.Chen MS, John JM, Chew DP, et al. Bare metal stent restenosis is not a benign clinical entity. Am Heart J. 2006;151:1260–1264. doi: 10.1016/j.ahj.2005.08.011 [DOI] [PubMed] [Google Scholar]
- 12.Yui Y, Hirayama A, Nonogi H, et al. Unstable angina and non-ST elevation acute coronary syndrome: epidemiology and current management in Japan (Japan Multicenter Investigation for Cardiovascular Disease-D (JMIC-D) Committee). Circ J. 2007;71:1335–1347. doi: 10.1253/circj.71.1335 [DOI] [PubMed] [Google Scholar]
- 13.Inohara T, Kohsaka S, Goto M, et al. Hypothesis of long-term outcome after coronary revascularization in Japanese patients compared to multiethnic groups in the US. PLoS One. 2015;10:e0128252. doi: 10.1371/journal.pone.0128252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakajima K, Takeishi Y, Matsuo S, et al. Metabolic syndrome is not a predictor for cardiovascular events in Japanese patients with diabetes mellitus asymptomatic for coronary artery disease: a retrospective analysis of the J-ACCESS-2 study. J Nucl Cardiol. 2013;20:234–241. doi: 10.1007/s12350-012-9656-0 [DOI] [PubMed] [Google Scholar]
- 15.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. John Wiley & Sons; 2011 [Google Scholar]
- 16.Kokubo Y, Okamura T, Yoshimasa Y, et al. Impact of metabolic syndrome components on the incidence of cardiovascular disease in a general urban Japanese population: the Suita study. Hypertens Res. 2008;31:2027–2035. doi: 10.1291/hypres.31.2027 [DOI] [PubMed] [Google Scholar]
- 17.Doi Y, Ninomiya T, Hata J, et al. Proposed criteria for metabolic syndrome in Japanese based on prospective evidence: the Hisayama study. Stroke. 2009;40:1187–1194. doi: 10.1161/STROKEAHA.108.531319 [DOI] [PubMed] [Google Scholar]
- 18.Niwa Y, Ishikawa S, Gotoh T, et al. Metabolic syndrome mortality in a population-based cohort study: Jichi Medical School (JMS) cohort study. J Epidemiol. 2007;17:203–209. doi: 10.2188/jea.17.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saito I, Iso H, Kokubo Y, et al. Metabolic syndrome and all-cause and cardiovascular disease mortality: Japan Public Health Center-based Prospective (JPHC) study. Circ J. 2009;73:878–884. doi: 10.1253/circj.CJ-08-1025 [DOI] [PubMed] [Google Scholar]
- 20.Irie F, Iso H, Noda H, et al. Associations between metabolic syndrome and mortality from cardiovascular disease in Japanese general population, findings on overweight and non-overweight individuals. Ibaraki Prefectural Health Study. Circ J. 2009;73:1635–1642. doi: 10.1253/circj.CJ-08-0442 [DOI] [PubMed] [Google Scholar]
- 21.Yanai H, Tomono Y, Ito K, et al. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr J. 2008;7:10. doi: 10.1186/1475-2891-7-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McNeill AM, Rosamond WD, Girman CJ, et al.. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385 [DOI] [PubMed] [Google Scholar]
- 23.Watanabe J, Kakehi E, Kotani K, et al. High-density lipoprotein cholesterol and risk of stroke subtypes: Jichi Medical School Cohort Study. Asia Pac J Public Health. 2020;32:27–34. doi: 10.1177/1010539519900685 [DOI] [PubMed] [Google Scholar]
- 24.Examination Committee of Criteria for ‘Obesity Disease’ in Japan. Japan Society for the study of obesity. New criteria for ‘obesity disease’ in Japan. Circ J. 2002;66:987–992. doi: 10.1253/circj.66.987 [DOI] [PubMed] [Google Scholar]
- 25.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404 [DOI] [PubMed] [Google Scholar]
- 26.Alberti KG, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366:1059–1062. doi: 10.1016/S0140-6736(05)67402-8 [DOI] [PubMed] [Google Scholar]
- 27.Alehagen U, Vorkapic E, Ljungberg L, et al. Gender difference in adiponectin associated with cardiovascular mortality. BMC Med Genet. 2015;16:37. doi: 10.1186/s12881-015-0187-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glintborg D. Endocrine and metabolic characteristics in polycystic ovary syndrome. Dan Med J. 2016;63:B5232. [PubMed] [Google Scholar]
- 29.Ridker PM, Silvertown JD. Inflammation, C-reactive protein, and atherothrombosis. J Periodontol. 2008;79:1544–1551. doi: 10.1902/jop.2008.080249 [DOI] [PubMed] [Google Scholar]
- 30.Thorand B, Baumert J, Döring A, et al. Sex differences in the relation of body composition to markers of inflammation. Atherosclerosis. 2006;184:216–224. doi: 10.1016/j.atherosclerosis.2005.04.011 [DOI] [PubMed] [Google Scholar]
- 31.Lai MM, Li CI, Kardia SL, et al. Sex difference in the association of metabolic syndrome with high sensitivity C-reactive protein in a Taiwanese population. BMC Public Health. 2010;10:429. doi: 10.1186/1471-2458-10-429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carbone F, Lattanzio MS, Minetti S, et al. Circulating CRP levels are associated with epicardial and visceral fat depots in women with metabolic syndrome criteria. Int J Mol Sci. 2019;20: E5981. doi: 10.3390/ijms20235981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hong GB, Gao PC, Chen YY, et al. High-sensitivity C-reactive protein leads to increased incident metabolic syndrome in women but not in men: a five-year follow-up study in a Chinese population. Diabetes Metab Syndr Obes. 2020;13:581–590. doi: 10.2147/DMSO.S241774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nishizawa H, Shimomura I. Population approaches targeting metabolic syndrome focusing on Japanese trials. Nutrients. 2019;11: E1430. doi: 10.3390/nu11061430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okuda N, Stamler J, Brown IJ, et al. Individual efforts to reduce salt intake in China, Japan, UK, USA: what did people achieve? The INTERMAP population study. J Hypertens. 2014;32:2385–2392. doi: 10.1097/HJH.0000000000000341 [DOI] [PubMed] [Google Scholar]
- 36.Ogihara T, Asano T, Fujita T. Contribution of salt intake to insulin resistance associated with hypertension. Life Sci. 2003;73:509–523. doi: 10.1016/S0024-3205(03)00315-1 [DOI] [PubMed] [Google Scholar]