Abstract
Disparities in cancer screening and care in rural communities warrant the need to determine effective ways to reach, engage, and educate the community residents. The purpose of this cross-sectional study was to pilot methods to engage rural residents in colorectal cancer (CRC) research and education activities and assess knowledge of CRC guidelines, symptoms, and screening behaviors in this sample. The community-engaged research approach was employed to develop and distribute a CRC knowledge and screening behavior assessment using various methods such as email and community drop boxes placed throughout the community. Bivariate analysis assessed the relationship between age and CRC knowledge items. Three hundred ninety-one surveys were returned with most received from community drop boxes (60%) followed by educational events (23%). The most ineffective method to distribute surveys was through community events. Most individuals were knowledgeable of CRC symptoms (70%) and screening facts (67%). Bivariate analysis showed that individuals 50 years or older had significantly more knowledge of CRC risks and screening than those under the age of 50. This study highlights the potential of community drop boxes as an effective method for engaging rural communities. Further, findings from the survey highlight the need to focus CRC education on younger individuals in which CRC incidence has increased.
Keywords: Colorectal cancer; Rural health, screening; Community engagement
Introduction
Rural residents suffer from higher colorectal cancer (CRC) incidence and mortality rates when compared with their urban counterparts [1, 2]. CRC mortality and incidence rates continue to decline; however, the rates are not declining as quickly for rural residents; therefore the disparities between rural and urban residents persist [3]. Reasons for these disparities are multifaceted, including lack of transportation, long distances to providers, lack of education about screening and treatment, and a deficit of healthcare providers in rural areas [4–8]. Due to the heterogeneity within rural populations that is often overlooked, there are demographic differences, namely age, which serve as predictors of CRC screening. Of CRC screening eligible individuals, older rural residents are more likely to receive screening than their younger counterparts [9–11]. Given the suboptimal screening practices of younger individuals and the unique barriers faced by rural residents, additional effort is needed to understand how to adequately deliver CRC education and screening in rural areas.
Similar to other rural communities in the USA [5, 12, 13], residents residing in rural communities in southern Virginia face CRC disparities (e.g., incidence, mortality). The Pittsylvania/Danville Health District, in particular, has extremely high colorectal cancer (CRC) incidence and mortality rates. Of 35 health districts in the state of Virginia, the Pittsylvania/Danville Health District has some of the worst CRC outcomes ranking 33rd for CRC incidence rates and 35th for CRC mortality rates [14]. CRC incidence and mortality rates for this area exceed those of national rates as well [15]. In 2010, a needs assessment conducted by Massey Cancer Center identified several key barriers to cancer care including limited access to tertiary care and cancer centers, clinician shortages (particularly oncology providers), and minimal community focused cancer education programs [16]. Although not represented in the assessment, understanding CRC knowledge in this population may offer insight into screening behaviors and compliance with screening guidelines [17–20].
The overall goal of this study was to identify education and intervention targets that may improve CRC knowledge and screening behaviors in rural communities. The aims of this study were to (1) pilot a novel method to collect data in previously unengaged rural residents, (2) assess CRC screening behaviors in rural residents, and (3) assess CRC knowledge across multiple domains (e.g., symptoms, screening) in rural residents.
Methods
Setting and Sample
The Pittsylvania/Danville Health District, located in southern Virginia, has a population of approximately 106,561 with the majority of residents living in rural counties. Most residents are Caucasian (66%) and have earned a high school or General Education Diploma (GED) (36.5%). The median household income in this area is $34,624. With only one hospital in the district, many residents travel at least 2 h to seek care in larger academic health centers in Virginia or neighboring North Carolina. There are several cancer screening facilities available to residents; however, there is only one gastroenterology practice.
CRRC Office and Regional Cancer Task Force
This study was conducted by the Cancer Research and Resource Center (CRRC), located in Danville, VA, in close collaboration with a regional cancer task force. The mission of the CRRC, a collaboration between Massey Cancer Center and the Tobacco Region Revitalization Committee, is to provide cancer-related information to and coordinate services (e.g., transportation, financial assistance) for the residents of Danville, Martinsville, and the five surrounding counties. The Center has two full-time and one part-time employees; all staff members earned Bachelor of Science degrees and all received basic life support certification. These individuals are responsible for planning and facilitating educational events and trainings for residents and healthcare providers.
The CRRC staff utilized the community-engaged research approach to design and conduct this study. In 2009, the CRRC staff established partners within and surrounding the Danville community. All partners were aware of the cancer disparities that impacted their communities and were invested in addressing these disparities. As a result of these collaborations, the Regional Cancer Task Force was formed. This group, comprised of area universities, hospitals, Susan G. Komen, the American Cancer Society, and other community groups, immediately went to work creating awareness in their communities (Table 1).
Table 1.
Regional cancer task force organizations
| Organization | Facility type |
|---|---|
| American Cancer Society | Non-profit |
| Averett University | Higher education |
| Cancer Research and Resource Center—Danville | Education |
| Centra Medical Group | Healthcare |
| Cherrystone Missionary Baptist Association | Religious organization |
| Danville Family YMCA | Community/non-profit organization |
| Danville-Pittsylvania Cancer Association | Community/non-profit organization |
| Danville Redevelopment and Housing Authority | Government agency/housing |
| Sovah Health | Healthcare |
| Hargrave Military Academy | Education |
| Susan G. Komen for the Cure and Pittsylvania County Breast Health Ambassador | Non-profit |
| Martinsville Henry County Coalition for Health and Wellness | Community/non-profit organization |
| PATHS, Inc. | Healthcare (federally qualified health center) |
| Tyton BioSciences | Technology/manufacturing |
| Virginia Department Health | State government agency/healthcare |
| Southern Area Agency on Aging | Community/non-profit organization |
| University of Virginia Cancer Center | Higher education |
| Public Libraries—Blue Ridge Regional; Danville; Halifax County South Boston; Pittsylvania County | Government agency |
Data Collection
The Southern Virginia Colorectal Cancer Screening survey was developed in 2017 by the Regional Cancer Task Force. This task force felt that an assessment was necessary in order to understand baseline levels of CRC knowledge and screening behaviors in the community; therefore, they designed a survey to assess rural residents’ knowledge regarding CRC symptoms, screening recommendations, and screening behavior. Items were adapted from questionnaires and information provided by the American Cancer Society, the American Institute for Cancer Research, the National Cancer Institute, and Center for Disease Control’s Screen for Life National Colorectal Cancer Action Campaign. Participants were asked to select the correct responses in each of the educational sections of the survey (e.g., CRC knowledge, CRC symptoms). Screening behaviors for participants over the age of 50 were assessed with three items. We asked if participants have been screened. Follow-up questions asked participants to select reasons why they had (e.g., following screening guidelines, my physician told me to) or had not been screened (e.g., I heard tests were difficult or painful, I am concerned about the costs associated with the tests). Participants were also asked to indicate a preference for receiving follow-up CRC screening information.
The task force was specifically interested in reaching residents who were not usually engaged with community-sponsored events, such as rural community residents. Jointly, the CRRC and the Cancer Task Force developed four strategies to increase community reach to unengaged members: holding educational programs within the community, attending community events of collaborators, strategic placing of community survey boxes throughout the community, and distribution of an online survey. The surveys took approximately 2 min to complete and could be completed using paper and pencil or electronically.
Educational Events
Five educational panel discussions were held specifically for the purpose of discussing colorectal cancer screening, prevention through lifestyle habits, and survivorship issues of patient navigation and treatment options. These were held in public libraries, for nursing students at Averett University, and at a local Section 8 housing facilities. Panelists were task force members representing area cancer-related resource organizations and health care facilities.
Community Events
Surveys were distributed at a broad range of community events including a YMCA-hosted blood pressure educational fair, Bridge 2 Bridge Danville, a local race supporting cancer awareness and survivors, and at a local food bank. An employee of the CRRC or a task force member attended the community events to distribute and collect completed surveys. To increase response, participants were given the option to complete the survey at home and return via mail or call the CRRC and complete the survey with a staff person over the phone.
Survey Boxes
CRRC staff collaborated with community partners to distribute survey “boxes” throughout the community. Task force members identified area organizations that expressed an interest in assisting with survey distribution and collection efforts. Organizations included local libraries, a 24-h gym, and the local housing authorities. A total of 31 survey boxes were placed within these facilities. Each box contained 25 surveys and instructions for survey completion. The local libraries agreed to have a staff person available to read the survey for residents who may require that assistance. Once completed, surveys were returned to the unlocked survey box.
Online
Using an existing list of past attendees to the CRRC or other task force partner events, residents who had previously provided an email address received a Survey Monkey link to complete the survey. The email explained the purpose of the survey and invited residents to click the link and complete the survey.
Survey Items
The only demographic factor collected from residents was age (≥ 50 years old, ˂ 50 years old). Knowledge items were categorized into three domains: screening knowledge, symptoms knowledge, and general CRC knowledge. The three screening items assessed individuals’ knowledge on screening guidelines and methods (e.g., some colorectal tests can be taken at home). CRC symptoms were assessed with eight facts (e.g., many people with colon cancer experience no symptoms in the early stages of the disease). Lastly, general CRC knowledge included four facts (e.g., CRC typically strikes people over the age of 50). Participants were given a list of items and received the following prompt, “Of the FACTS below, check off what you know.” They were instructed that multiple answers were allowed. We totaled the items that were checked for each category to get a total score for each domain.
Individuals who completed the survey and provided sufficient contact information were entered into a drawing to receive one of the six prizes; prizes included gift cards and a gift basket. All procedures were approved by the Institutional Review Board at Virginia Commonwealth University.
Data Analysis
Data were cleaned by Regional Cancer Task Force members and cross-checked by VCU investigators. Descriptive statistics, specifically, frequencies, were performed to summarize survey findings.
Participants were grouped according to whether they were over 50 or under 50 during the time of the survey. We described the associated characteristics of the participants using three domains: screening, symptoms, and general CRC knowledge. Bivariate comparison was conducted using Pearson’s chi-square tests for categorical variables. Statistical analyses were conducted using STATA/MP (version 12.1; StataCorp LP), and 2-sided p values are presented.
Results
Survey Receipt
A total of 391 surveys were returned from participants. Most participants completed the paper-based survey (85%) as opposed to the electronic version. The survey boxes yielded the greatest number (n = 241) of surveys. There was a fairly even distribution across the locations; 39% of surveys were from fitness centers and 12% of surveys were received from community health educators. Figure 1 displays how survey receipt varied across the four data collection methods and highlights survey receipt from the various locations of the survey boxes. There was a total of 13 community events which yielded 39 surveys; 3 events did not yield any surveys. Of the surveys completed, 69% included contact information and those individuals were entered into a drawing for a prize.
Fig. 1.
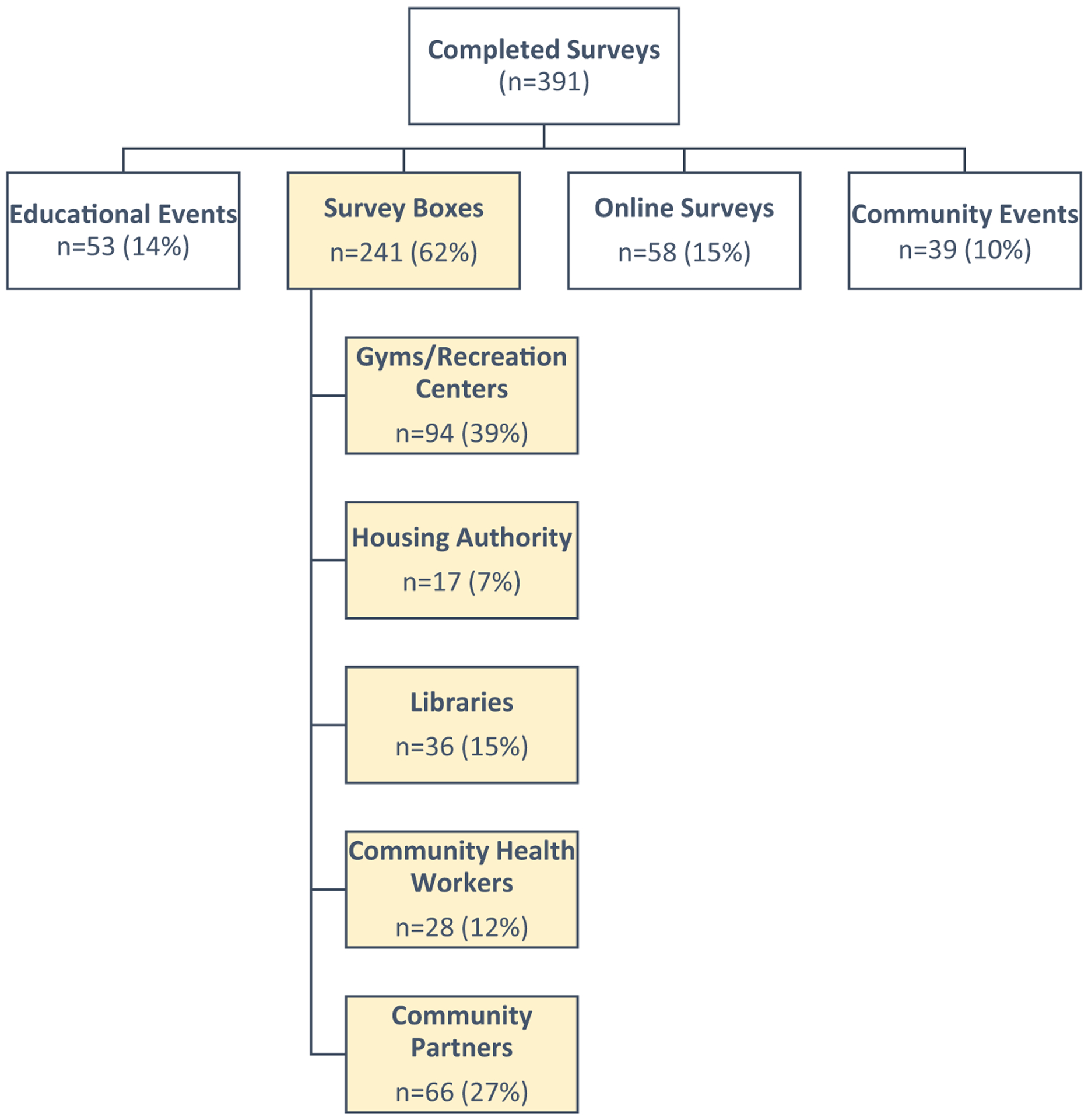
Colorectal cancer survey receipt schema
CRC Knowledge
Of all CRC screening items, approximately 83% of individuals reported that the American Cancer Society suggests that people start colorectal screening at 50 years of age, or younger if at-risk or if African American. However, only 53.4% of participants were aware that some colorectal tests can be taken at home. With regard to CRC symptom knowledge, most individuals were aware that blood in the stool or stool that looks like black tar (89.4%) is a common symptom, while only57.6% reporting know that an individual may feel the need to have a bowel movement that is not relieved by doing so. Lastly, regarding general CRC knowledge, most participants were aware that catching CRC early can save your life and/or greatly reduce associated costs and recovery time (80.4%). The general knowledge fact that individuals selected least was that CRC typically strikes people over the age of 50(56.9%).
In bivariate analysis, individuals over the age of 50 were more knowledgeable about home testing for CRC (63.1%, p = 0.000), ACS screening guidelines with regard to age of screening (86.6%, p = 0.006), and the benefits of high fiber diets for CRC prevention (77.9%, p = 0.046) (Table 2). Older individuals were also more aware than their younger counterparts that CRC is preventable (81.1%, p = 0.000) and that CRC almost always develops from precancerous polyps(74.2%, p = 0.000). There were no significant differences by age with regard to knowledge about CRC symptoms.
Table 2.
Correct responses to survey items by age
| < 50 years of age (%) | ≥ 50 years of age (%) | p value | |
|---|---|---|---|
| CRC screening | |||
| Some CRC tests can be taken at home | 36.8 | 63.1 | 0.000§ |
| ACS recommends screening at age 50 | 75.9 | 86.6 | 0.006‡ |
| Catching CRC early can save your life and/or greatly reduce associated costs and recovery time | 75.3 | 80.6 | 0.202 |
| CRC symptoms | |||
| Change in bowel habits | 73.0 | 79.3 | 0.146 |
| Many people with colon cancer experience no symptoms in the early stages | 60.3 | 67.7 | 0.129 |
| A feeling that you need to have a bowel movement that is not relieved by doing so | 54.0 | 54.4 | 0.944 |
| Blood in the stool or stools that look like black tar | 81.6 | 87.1 | 0.135 |
| Loss of appetite | 56.3 | 55.3 | 0.840 |
| Pain in the belly or a feeling of fullness | 70.7 | 66.4 | 0.361 |
| Unexplained weight loss | 67.8 | 64.5 | 0.494 |
| Constant tiredness, fatigue | 65.5 | 61.3 | 0.389 |
| General CRC knowledge | |||
| CRC is preventable and can be successfully treated if detected early | 64.4 | 81.1 | 0.000§ |
| A diet high in fiber reduces risk of getting CRC | 69.0 | 77.9 | 0.046† |
| CRC typically strikes people over the age of 50 | 52.3 | 58.5 | 0.218 |
| CRC almost always develops from precancerous polyps | 51.7 | 74.2 | 0.000§ |
p < 0.05
p < 0.01
p < 0.001
Screening Behaviors
Of the total sample, 55.5% were at least 50 years of age. Of these study participants, 67% reported that they had received colorectal screening. Key reasons for screening were physician recommendation (72%) followed by individuals reporting that they follow all screening tests guidelines (46%) and family history of cancer.
A substantial proportion of individuals (33%) had not been screened. Reasons for non-adherence to screening guidelines were not having a family history (38%), no physician recommendation (37%), and the belief that screening was for people with symptoms (25%).
All participants were asked if they were interested in receiving follow-up contact from a health professional knowledgeable about cancer; 23% or 90 participants requested information. Many of these individuals were non-screeners. Eight individuals did not provide enough contact information; therefore, CRRC staff could not follow up with these individuals. CRRC staff worked to follow up with respondents and successfully reached 44 individuals. Follow-ups resulted in two gastroenterologist referrals and one referral to the Southern Area Agency on Aging to provide transportation to a colonoscopy appointment.
Discussion
This study provided invaluable insight into effective methods to engage and assess the needs of our community. As distance is always a potential barrier to engaging rural communities, implementing innovative methods, such as the survey boxes, enables and empowers community members to engage in research without the inhibition of such barriers. As survey receipt from survey boxes exceeded other methods, it is evident that the most effective method to get information to our community members is by taking it to them. The survey boxes and the online surveys also allowed participants the opportunity to complete the surveys at their most convenient times. Additionally, regarding our educational events, we recognize the importance of leveraging such events for engagement and research recruitment for future endeavors. The three community events resulted in no survey provision. This may have been due to the nature of these events, as the focus did not pertain to health or health education (e.g., annual race, weekly farmer’s market). Therefore, it may be less beneficial to attempt to engage community members at non-health-related events.
Significant differences were noted between individuals 50 years of age and older and those 49 years of age and younger. Individuals under the age of 50 were not as aware of the recommended screening age as those 50 and over. This is of great importance as the American Cancer Society (ACS) now recommends CRC screening at age 45 [21]. Further, this group was not as aware as their older counterparts that CRC is preventable. These findings highlight a need to target younger populations for CRC education, particularly as individuals are being diagnosed at younger ages [22, 23]. Education efforts targeting younger individuals may also serve to benefit older individuals as studies show positive findings, particularly in parent-child dyads, with regard to younger individuals motivating their older counterparts to seek screening for cancer [24]. A majority of participants were knowledgeable of cancer symptoms and CRC screening guidelines; however, many were unaware of home screening kits. Notably, younger individuals were less knowledgeable of this screening mechanism. Along with educating rural residents about the availability of home screening kits, mailing screening kits and instruction to individuals, particularly those living in rural areas, may increase screening rates [25].
While this study offers a unique approach to engage rural residents in CRC knowledge, there are limitations to note. Although unlikely, it is possible that individuals could complete multiple surveys, particularly those that were completed via survey boxes. The potential of this occurrence was limited by offering participants an opportunity to win a drawing; this required participants to include their name and contact information on the survey.
Findings from this effort highlight the importance of provider recommendations to promote cancer prevention and screening. The high colorectal cancer incidence and mortality rates in the Pittsylvania/Danville health district, like many rural areas, warrant immediate action and attention. While the screening rate for this health district closely mirrors national rates, improvement is warranted [26]. Furthermore, insufficient numbers of providers in rural areas, such as many areas located in the Pittsylvania/Danville Health District, added pressure and burden on providers to educate and treat a large number of patients in such a limited amount of time and with limited resources [27, 28]. More focused efforts to recruit and retain providers are necessary to alleviate such burdens. Additionally, training providers, possibly through brown bag lunch seminars, and supplying provider offices with cancer prevention and screening materials may result in more opportunities for providers to engage in these discussions with patients [29]. Lastly, given the importance of a provider recommendation for screening uptake, there may be opportunities to leverage electronic health records to prompt providers screen their patients on a more consistent basis.
Acknowledgments
We would like to thank the residents of the Pittsylvania/Danville Health District for their participation in our annual assessment. We would also like to thank all of our community partners who dedicated their time, expertise, and resources to develop, distribute, and assess the colorectal screening survey. Services and products in support of the research project were generated by the VCU Massey Cancer Center, supported, in part, with funding from NIH-NCI Cancer Center Support Grant P30 CA016059, NCI 2T32 CA093423, and by the Virginia Tobacco Region Revitalization Commission.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Ethical Approval All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Zahnd WE, James AS, Jenkins WD, Izadi SR, Fogleman AJ, Steward DE, Colditz GA, Brard L (2017) Rural-urban differences in cancer incidence and trends in the United States. Cancer Epidemiol Biomark Prev [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang PS, Mayer JD, Wakefield J, Ko CW (2017) Temporal trends in geographic and sociodemographic disparities in colorectal cancer among medicare patients, 1973–2010. J Rural Health 33(4):361–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henley SJ, Anderson RN, Thomas CC, Massetti GM, Peaker B, Richardson LC (2017) Invasive cancer incidence, 2004–2013, and deaths, 2006–2015, in nonmetropolitan and metropolitan counties-United States. MMWR Surveill Summ 66(14):1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wender RC: Barriers to screening for colorectal cancer. Gastrointestinal endoscopy clinics of North America 2002, 12(1052–5157; 1):145–170. [DOI] [PubMed] [Google Scholar]
- 5.Davis TC, Rademaker A, Bailey SC, Platt D, Esparza J, Wolf MS, Arnold CL (2013) Contrasts in rural and urban barriers to colorectal cancer screening. Am J Health Behav 37(3):289–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolin JN, Bellamy GR, Ferdinand AO, Vuong AM, Kash BA, Schulze A, Helduser JW (2015) Rural healthy people 2020: new decade, same challenges. The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association 31(3):326–333 [DOI] [PubMed] [Google Scholar]
- 7.Petterson SM, Phillips RL Jr., Bazemore AW, Koinis GT: Unequal distribution of the U.S. primary care workforce. Am Fam Physician 2013, 87(11): Online. [PubMed] [Google Scholar]
- 8.The Council of State G: Health care workforce shortages critical in rural America. In. Lexington, KY: Capitol Facts & Figures; 2011. [Google Scholar]
- 9.Crosby RA, Collins T (2017) Correlates of community-based colorectal cancer screening in a rural population: the role of fatalism. J Rural Health 33(4):402–405 [DOI] [PubMed] [Google Scholar]
- 10.Wang H, Qiu F, Gregg A, Chen B, Kim J, Young L, Wan N, Chen LW (2018) Barriers and facilitators of colorectal cancer screening for patients of rural accountable care organization clinics: a multilevel analysis. J Rural Health 34(2):202–212 [DOI] [PubMed] [Google Scholar]
- 11.Wang H, Roy S, Kim J, Farazi PA, Siahpush M, Su D (2019) Barriers of colorectal cancer screening in rural USA: a systematic review. Rural Remote Health 19(3):5181. [DOI] [PubMed] [Google Scholar]
- 12.Cole AM, Jackson JE, Doescher M (2013) Colorectal cancer screening disparities for rural minorities in the United States. J Prim Care Community Health 4(2):106–111 [DOI] [PubMed] [Google Scholar]
- 13.Young WF, McGloin J, Zittleman L, West DR, Westfall JM (2007) Predictors of colorectal screening in rural Colorado: testing to prevent colon cancer in the high plains research network. J Rural Health 23(3):238–245 [DOI] [PubMed] [Google Scholar]
- 14.Cancer in Virginia: overview and selected statistics [http://www.vdh.virginia.gov/content/uploads/sites/27/2016/07/Cancer-in-Virginia-2014_Final.pdf]
- 15.Institute UoWPH: County health rankings key findings. In 2019.
- 16.U.S. Census Bureau, Statistical Abstract of the United States: 2009. In 2010.
- 17.Nelson W, Moser RP, Gaffey A, Waldron W (2009) Adherence to cervical cancer screening guidelines for U.S. women aged 25–64: data from the 2005 Health Information National Trends Survey (HINTS). J Women’s Health (Larchmt) 18(11):1759–1768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee EE, Fogg L, Menon U (2008) Knowledge and beliefs related to cervical cancer and screening among Korean American women. West J Nurs Res 30(8):960–974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graves KD, Huerta E, Cullen J, Kaufman E, Sheppard V, Luta G, Isaacs C, Schwartz MD, Mandelblatt J (2008) Perceived risk of breast cancer among Latinas attending community clinics: risk comprehension and relationship with mammography adherence. Cancer causes & control: CCC 19(10):1373–1382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wall KM, Rocha GM, Salinas-Martinez AM, Baraniuk S, Day RS (2010) Modifiable barriers to cervical cancer screening adherence among working women in Mexico. J Women’s Health (Larchmt) 19(7):1263–1270 [DOI] [PubMed] [Google Scholar]
- 21.Wolf AMD, Fontham ETH, Church TR, Flowers CR, Guerra CE, LaMonte SJ, Etzioni R, McKenna MT, Oeffinger KC, Shih YT, Walter LC, Andrews KS, Brawley OW, Brooks D, Fedewa SA, Manassaram-Baptiste D, Siegel RL, Wender RC, Smith RA (2018) Colorectal cancer screening for average-risk adults: 2018 guideline update from the American Cancer Society. CA Cancer J Clin 68(4):250–281 [DOI] [PubMed] [Google Scholar]
- 22.Siegel R, Desantis C, Jemal A (2014) Colorectal cancer statistics, 2014. CA Cancer J Clin 64(2):104–117 [DOI] [PubMed] [Google Scholar]
- 23.National Cancer Institute Surveillance E, and End Results Program. SEER*Explorer: Colon and rectum. In.
- 24.Mosavel M, Genderson MW (2016) Daughter-initiated cancer screening appeals to mothers. Journal of cancer education: the official journal of the American Association for Cancer Education 31(4):767–775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charlton ME, Mengeling MA, Halfdanarson TR, Makki NM, Malhotra A, Klutts JS, Levy BT, Kaboli PJ (2014) Evaluation of a home-based colorectal cancer screening intervention in a rural state. The Journal of rural health: official journal of the American Rural Health Association and the National Rural Health Care Association 30(3):322–332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American Cancer S (2017) Colorectal cancer facts & figures 2017–2019. In. Atlanta, American Cancer Society [Google Scholar]
- 27.Brems C, Johnson ME, Warner TD, Roberts LW (2006) Barriers to healthcare as reported by rural and urban interprofessional providers. Journal of Interprofessional Care 20(2):105–118 [DOI] [PubMed] [Google Scholar]
- 28.Hart LG, Salsberg E, Phillips DM, Lishner DM (2002) Rural health care providers in the United States. The Journal of rural health: official journal of the American Rural Health Association and the National Rural Health Care Association 18(Suppl):211–232 [DOI] [PubMed] [Google Scholar]
- 29.Shell R, Tudiver F (2004) Barriers to cancer screening by rural Appalachian primary care providers. The Journal of rural health: official journal of the American Rural Health Association and the National Rural Health Care Association 20(4):368–373 [DOI] [PubMed] [Google Scholar]


