Abstract
Background
The soft tissue of the central pretibial area is difficult to reconstruct often requiring free tissue transfer. Especially medically compromised patients are not ideal candidates for free tissue transfer and may benefit from expeditiously harvested local flaps with limited donor site morbidity. As muscle flaps are rare, pedicled flaps based on lateral perforators represent an alternative as the arc of rotation can often be limited to 90°.
Material and Methods
A retrospective analysis of patient data was conducted to identify patients over the age of 60 years with comorbidities that underwent pretibial soft tissue reconstruction with a single-pedicle perforator flap. Patient demographics, size and cause of the defect, flap dimension, arc of rotation and complications were recorded.
Results
Five patients with an average age of 71.4 years were included. The arc of rotation was 69°, all flaps healed. There were two recurrences of osteomyelitis.
Conclusion
Lateral perforators originating from the anterior tibial artery or peroneal artery are adequate source vessels for single pedicled perforator flaps even in medically compromised patients. A perforator located proximal to the defect allows limiting the arc of rotation to less than 90°, which increases the safety of the flap. Patients benefit from a simple procedure without a microvascular anastomosis and a donor site confined to one extremity.
Keywords: Propeller flap, Pedicled perforator flap, Lower extremity reconstruction, Elderly patients
Introduction
Reconstruction of the thin soft envelope over the anterior tibia remains a major challenge for the reconstructive surgeon. The limited mobility and paucity of the skin and subcutaneous tissue combined with the exposure of this region to mechanical stress, causes even small wounds to quickly progress into a complex situation with exposed bone, tendon or metal devices. Due to the lack of adjacent soft tissue, random pattern flaps and local fasciocutaneous flaps often fail.1,2 Pedicled muscle flaps such as the gastrocnemius or anterior tibial muscle flap can adequately reconstruct proximal defects.3 Most commonly, however, soft tissue defects have to be addressed with free tissue transfer. The introduction of pedicled, fasciocutaneous perforator flaps has expanded the armamentarium of the reconstructive surgeon in this area as they are reliable, can be performed expeditiously and preserve muscle and source vessel.4 This is of paramount importance in elderly and/or systemically compromised patients requiring soft tissue reconstruction.2 Pedicled perforator flaps adhere closely to the reconstructive principle of ‘like with like’ and limit donor site morbidity to the injured extremity.2 Proximal musculocutaneous perforators originating from the peroneal and anterior tibial artery are good source vessels due to the size, length and directionality of the perforator.5., 6, 7 Specifically, the peroneal artery represents an ideal source vessel as it is consistent and often least affected by atherosclerosis on the lower extremity.8 The aim of this retrospective study was the evaluation of pedicled perforator flaps based on lateral perforators utilised for the reconstruction of pretibial soft tissue defects in the middle third in elderly, medically compromised patients.
Material and methods
A retrospective analysis of patient data was carried out to identify patients over 60 years of age who underwent soft tissue reconstruction of mid-third pretibial soft tissue defects with laterally based perforator flaps. Patients with at least one medical comorbidity such as peripheral vascular disease, diabetes mellitus, patients immunocompromised by malignant tumours or those with nicotine use were included, while patients in the same age group that received a free tissue transfer were excluded. Five patients could be identified and data were analysed with regard to patient demographics, cause and size of the defect, temporary dressings, flap dimension, arc of rotation, closure of the donor site and complications. The study was approved by the institutional ethics committee.
Surgical technique
Prior to soft tissue reconstruction, all wounds were temporarily dressed with a negative pressure wound therapy following surgical debridement. The preoperative general vascular work up ranged from pulse examination to angiography. Perforators in the proximal lateral region of the lower thigh were mapped preoperatively with a handheld Doppler device (Figure 1). A preliminary flap outline was based on these perforators with the long axis of the flap parallel to the long axis of the leg.
Figure 1.
A 73-year-old male with chronic osteomyelitis after a gunshot wound. A lateral perforator is marked.
All procedures were performed under general anaesthesia in supine position without the use of a tourniquet. After debridement, an exploratory incision along the medial outline of the flap gave access to the subfascial tissue plane to locate perforators. If more than one perforator was available, the largest perforator located slightly proximal to the defect was selected to serve as a source vessel. The flap outline was re-evaluated and adapted accordingly to harvest a flap 1 cm wider and longer than the defect. After intramuscular pedicle dissection under loupe magnification, the flap was elevated completely and rotated into the defect (Figure 2). Care was taken to centre the axis of rotation over the pedicle to avoid any stretch in addition to the torsion of the pedicle. After flap inset, the donor site was grafted with a split thickness skin graft harvested from the same lower extremity.
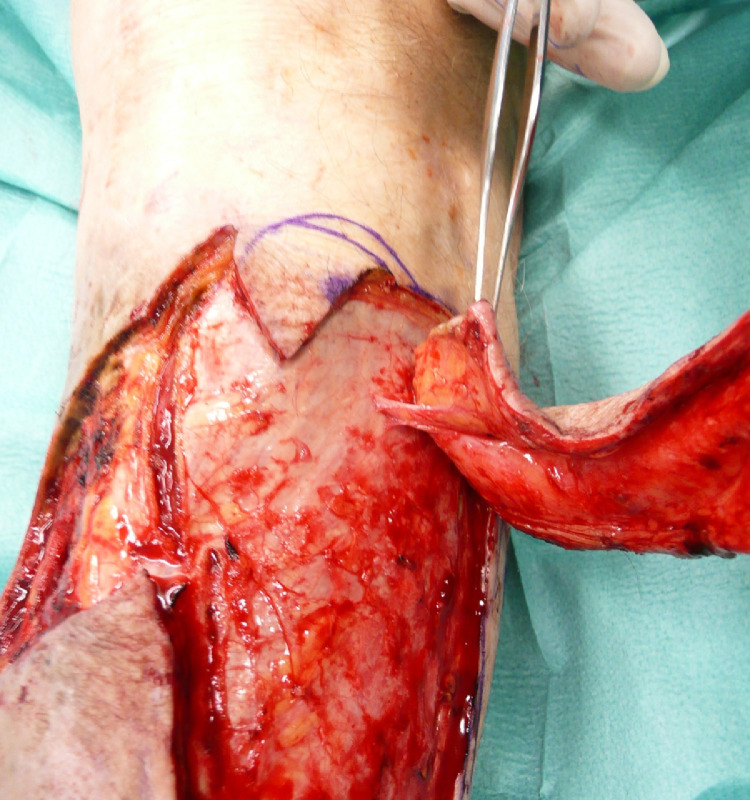
Figure 2.
Intraoperative view of the pedicle.
Results
Five patients were included, four males and one female. The average age was 71.4 years. Comorbidities included severe peripheral vascular disease in two patients, which required vascular intervention in one case (Table 1). The cause of the defect included chronic post-traumatic wounds leading to osteomyelitis in two cases, two cases of minor trauma leading to complex wounds and one case of post-operative wound dehiscence after plating of a tibial fracture. The size of the defect was 33.2 cm², while the average size of the flap was 82.2 cm². The arc of rotation ranged from 45° to 90° with an average of 69° In all cases, a skin-graft was used to close the donor site defect. All flaps survived. In two cases, a fistula formation at the tip of the flap marked the recurrence of osteomyelitis after 5 and 9 months (Figure 3).
Table 1.
Demographic data.
| Age, Gender | Comorbidities | Cause of defect | Size | Prior Vascular surgery | Flap size | Rotation | Donor site closure | Complications |
|---|---|---|---|---|---|---|---|---|
| M, 61 | PVD IV° smoking | Minor Trauma | 12 × 5 cm | TEA groin, pelvis, fem-pop I Bypass | 16 × 8 cm | 45° | skingraft | none |
| M, 73 | IDDM, PVD IV° | Gunshot wound, chronic Osteomyelitis | 6 × 5 cm | Fem Pop I Bypass, PTA | 13 × 6 cm | 80° | skingraft | Recurrence of osteomyelitis |
| F, 67 | IDDM, HTN | open tibia fracture, osteomyelitis, knee arthroplasty | 8 × 5 cm | none | 15 × 9 cm | 90° | skingraft | none |
| M, 86 | HTN, smoking | Chronic osteomyelitis | 4 × 4 cm | none | 8 × 5 cm | 70° | skingraft | Recurrence of osteomyelitis |
| M, 70 | cll, aortic valve replacement, htn, chronic kidney disease | haematoma | 4 × 5 cm | none | 6 × 5 cm | 60° | skingraft | none |
Abbreviations: HTN: Hypertension; IDDM: Insulin-dependent Diabetes mellitus; PVD: peripheral vascular disease; CLL: chronic lymphatic leukaemia; TEA: thromboendarterectomy; PTA: percutaneous transluminal angioplasty.
Figure 3.
Result, 6 months post-operatively. The recurrence of osteomyelitis visible at the inferior flap margin.
Discussion
In the central, pretibial region even small lacerations may progress into complicated soft tissue defects in compromised patients. Whereas local muscle flaps can easily be used in the proximal third, the middle and distal third of the lower thigh, which are traditionally considered free flap territory, as local muscle flaps are scarce. The concept of pedicled perforator flaps has given the reconstructive surgeon an alternative which is applicable to small- and medium size defects otherwise addressed with free flaps.9,10 In this study, flaps based on a single lateral perforator were evaluated. In regard to the source vessel, laterally based flaps are safe as the anterior muscle compartment protects perforators from compression and shearing in trauma cases.2 On the medial side of the tibia crest such a buffer is lacking.5 The size of perforators originating from the anterior tibial and peroneal artery is similar to its counterparts from the posterior tibial artery, while the inter-perforator distance is larger in the vascular territory of the peroneal artery.6 This equates to a larger individual perforasome, which secures perfusion of the flap. Perforators in the lateral region also have a longer intramuscular course than medial perforators.10,11 Pedicle length is essential to evenly distribute the twist induced by the rotation of the flap.9,11,12 Contrary to defects over the lateral knee or fibular head, a rotation of 180° is not required to address ventral defects. In our study, the average degree of rotation was less than 70°. This reduces the risk for kinking and vascular compromise of the flap.12 Especially in the elderly, systemically ill patients included in this study, it seems surgically intuitive to limit rotation as much as possible to increase the safety of the flap. This is achieved by selecting perforators proximal to the level of the defect to reduce the arc of rotation to less than 90°. Proximal perforators enter the fascia perpendicularly, are larger in size and more likely intramuscular than distal perforators.5,7 The lateral donor site longitudinal to the axis of the leg is preferable to a more horizontally placed donor site, as perforasomes along the course of cutaneous nerves often have a direct connection.11,13,14 Therefore, the axis of the flap should be planned longitudinally in the lower extremity.11 As the fibula is covered well with muscle in the middle third, skin grafts are preferred for donor site closure. (Figure 4, Figure 5)
Figure 4.
A 61-year-old smoker.
Figure 5.
Result, 3 weeks post-operatively.
Elderly patients benefit from rapid flap harvest and limited dissection.15 Contrary to muscle flaps, no deep dead space is created. In this study, no complications occurred at the donor site. While the aesthetic appearance of the donor site is inferior to a primary closure, this is of lesser concern in medically compromised patients. In two cases osteomyelitis recurred. This is not considered a flap failure, but attributed to the deep infection present in both cases over decades. Arguably a muscle flap may have been better suited to address the soft tissue defect.
Some points of pedicled perforator flap reconstruction in this specific patient population remain debatable. When flap rotation does not exceed 90°, more than one perforator could be preserved. All flaps in this study were based on a single perforator. Two or more perforators can only be preserved if found in close proximity to each other. As the pivot point of the flap is at the midpoint between the two perforators, the likelihood of vascular compromise through stretching and kinking increases with the distance between the perforators. We thus prefer to base flaps on a single, meticulously dissected perforator, to control the twisting motion of the vessel. It is also debatable if the flap has to be islanded completely when the rotation is less than 90°. An attached proximal base could in theory augment perfusion, especially venous drainage.16,17 In the clinical setting, this regularly creates a large dog ear, which affects flap inset.15 As flap perfusion is reliably secured by a single perforator, islanding the flap improves reach and tension-free closure.15,17 The less than 90° arc of rotation centred over the perforator found at the proximal tip of the flap is not a true propeller flap, which is characterized by two blades almost equal in length. The slight upwards sweep performed with this perforator flap resembles more of a ‘windshield-wiper’ movement. It is therefore debatable whether this flap type should be referred to as a propeller flap. The laterally based perforator flaps are very thin and thus advantageous in the lower extremity reconstruction.18
These perforator-based flaps allow transfer of tissue similar to a free microvascular transfer without the need for lengthy microsurgery. Especially the elderly, medically compromised patient population may benefit from this scale down of the reconstructive ladder.
Declaration of Competing Interest
No conflicts of interest are declared by all authors.
Funding
This publication was supported by the Open Access Publication Fund of the University of Wuerzburg.
References
- 1.Quaba O., Quaba A. Pedicled perforator flaps for the lower limb. Semin Plast Surg. 2006;20:103–111. [Google Scholar]
- 2.Shin I.S., Lee D.W., Rah D.K. Reconstruction of pretibial defect using pedicled perforator flaps. Arch Plast Surg. 2012;39(4):360–366. doi: 10.5999/aps.2012.39.4.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moller-Larsen F., Petersen N.C. Longitudinal split anterior tibial muscle flap with preserved function. Plast Reconstr Surg. 1984;74:398–401. doi: 10.1097/00006534-198409000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Gir P., Cheng A., Oni G. Pedicled perforator (propeller) flaps in lower extremity defects: a systematic review. J Reconstr Microsurg. 2012;28:595–601. doi: 10.1055/s-0032-1315786. [DOI] [PubMed] [Google Scholar]
- 5.Hupkens P., Schijns W., Van Abeelen M. Lateral lower leg perforator flaps: an anatomical study to localize and classify lateral lower leg perforators. Microsurgery. 2015;35(2):140–147. doi: 10.1002/micr.22313. [DOI] [PubMed] [Google Scholar]
- 6.Schaverien M., Saint-Cyr M. Perforators of the lower leg: analysis of perforator locations and clinical application for pedicled perforator flaps. Plast Reconstr Surg. 2008;122:161–170. doi: 10.1097/PRS.0b013e3181774386. [DOI] [PubMed] [Google Scholar]
- 7.Jakubietz R.G., Schmidt K., Zahn R.K. Subfascial directionality of perforators of the distal lower extremity: an anatomic study regarding selection of perforators for 180-degree propeller flaps. Ann Plast Surg. 2012;69(3):307–311. doi: 10.1097/SAP.0b013e31822af8db. [DOI] [PubMed] [Google Scholar]
- 8.Hansen T., Wikström J., Johansson L.O. The prevalence and quantification of atherosclerosis in an elderly population assessed by whole-body magnetic resonance angiography. Arterioscler Thromb Vasc Biol. 2007;27:649–654. doi: 10.1161/01.ATV.0000255310.47940.3b. [DOI] [PubMed] [Google Scholar]
- 9.Jakubietz R.G., Jakubietz M.G., Gruenert J.G. The 180-degree perforator-based propeller flap for soft tissue coverage of the distal, lower extremity: a new method to achieve reliable coverage of the distal lower extremity with a local, fasciocutaneous perforator flap. Ann Plast Surg. 2007;59:667–671. doi: 10.1097/SAP.0b013e31803c9b66. [DOI] [PubMed] [Google Scholar]
- 10.Ha Y., Yeo K.K., Piao Y. Peroneal flap: clinical application and cadaveric study. Arch Plast Surg. 2017;44:136–143. doi: 10.5999/aps.2017.44.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saint-Cyr M., Wong C., Schaverien M. The perforasome theory: vascular anatomy and clinical implications. Plast Reconstr Surg. 2009;124:1529–1544. doi: 10.1097/PRS.0b013e3181b98a6c. [DOI] [PubMed] [Google Scholar]
- 12.Wong C.H., Cui F., Tan B.K. Nonlinear finite element simulations to elucidate the determinants of perforator patency in propeller flaps. Ann Plast Surg. 2007;59:672–678. doi: 10.1097/SAP.0b013e31803df4e9. [DOI] [PubMed] [Google Scholar]
- 13.Chubb D.P., Taylor G.I., Ashton M.W. True and “choke” anastomoses between perforator angiosomes: part II. Dynamic thermographic identification. Plast Reconstr Surg. 2013;132:1457–1464. doi: 10.1097/01.prs.0000434407.73390.82. [DOI] [PubMed] [Google Scholar]
- 14.Deng C., Wu B., Wei Z., Li H. Interperforator flow pattern and clinical application of distal extended peroneal artery perforator flaps. Ann Plast Surg. 2018;80(5):546–552. doi: 10.1097/SAP.0000000000001290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shen L., Liu Y., Zhang C. Peroneal perforator pedicle propeller flap for lower leg soft tissue defect reconstruction: clinical applications and treatment of venous congestion. J Int Med Res. 2017;45(3):1074–1089. doi: 10.1177/0300060516687229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu T.C., Lin C.H., Lin C.H. Versatility of the pedicled peroneal artery perforator flaps for soft-tissue coverage of the lower leg and foot defects. J Plast Reconstr Aesthet Surg. 2011;64:386–393. doi: 10.1016/j.bjps.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 17.John J.R., Tripathy S., Sharma R.K. Peroneal artery perforator-based flaps for reconstruction of middle and lower third post-traumatic defects of the leg. ANZ J Surg. 2015;85:869–872. doi: 10.1111/ans.12556. [DOI] [PubMed] [Google Scholar]
- 18.Jeong H.H., Hong J.P., Suh H.S. Thin elevation: a technique for achieving thin perforator flaps. Arch Plast Surg. 2018;45(4):304–313. doi: 10.5999/aps.2017.01529. [DOI] [PMC free article] [PubMed] [Google Scholar]