We couldn't know that severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) would be very different from SARS-CoV or Middle East respiratory syndrome coronavirus (MERS-CoV) even when it was identified as the pathogen of pneumonia of unknown aetiology spreading in China. We initially responded to coronavirus disease 2019 (COVID-19) in the same way as we did against SARS and MERS. The overall case fatality rate of COVID-19 is lower than that of SARS. However, because patients with COVID-19 shed virus at the early stage with mild symptoms, our efforts to contain COVID-19 have failed.
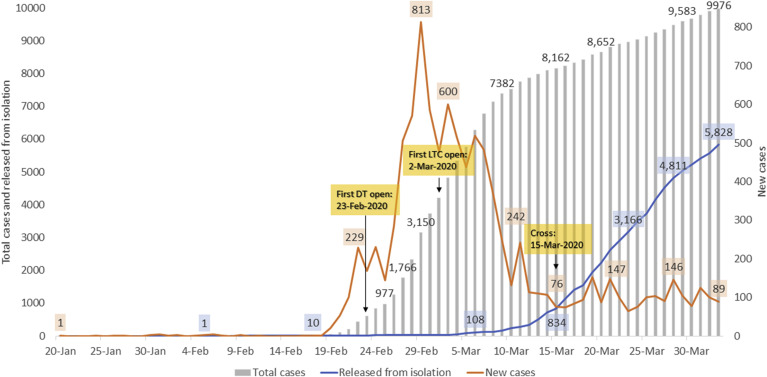
Since the first COVID-19 case was identified in Korea on January 20, 2020, we have experienced an explosive outbreak related to a religious group in the city of Daegu and North Gyeongsang Province [1]. Daegu is Korea's fourth largest city, with a population of 2 500 000, and is surrounded by North Gyeongsang Province. More than 1000 persons of the religious group attended worship services, kneeling on the floor in a relatively small space for the congregation on February 8 and 15. Since February 18, when the first case related to that religious group was identified, the highest number of new cases in a day reached 813 on February 29 (Fig. 1 ) [2]. Since then, the daily number of new cases started to decrease and became <100 on March 15. Remaining concerns are persistent small-cluster outbreaks and an increasing number of imported cases from outside Korea. Currently, many countries in the world are suffering from surging outbreaks. Although principal emergency strategies are common [3], COVID-19 is quite different from other known diseases, and we have to share our experience and knowledge to overcome this COVID-19 pandemic.
Fig. 1.
Timeline of cases with COVID-19 in Korea (modified from [2]). DT, drive-through screening; LTC, Life Treatment Centre.
First, rapid diagnosis and rapid isolation is the key to the prevention of transmission. Korea Centres for Disease Control and Prevention (KCDC) and commercial diagnostic companies started to set up a real-time RT-PCR assay to detect SARS-CoV-2 as soon as the genetic sequences were released. KCDC wanted to boost large-scale DNA analysis capabilities after having experienced the 2015 MERS outbreak. By early March, Korea was capable of running as many as 20 000 tests a day, and a total of 433 211 tests have been performed as of April 3. Rapidly implemented diagnostic techniques enabled proactive screening of contacts and early diagnosis. The relatively shorter period of symptom onset to diagnosis of COVID-19 (7 days in Korea versus 10 days in China) has led to the rapid isolation of patients and a reduction in further transmission [1]. With an increasing number of suspected and/or symptomatic patients to be tested for COVID-19, there has been a need for a safe and efficient screening system. Procedures for obtaining nasopharyngeal swabs, recommended for the detection of SARS-CoV-2, are considered as aerosol-generating procedures, and require specific facilities such as airborne infection isolation rooms (AIIRs) which need disinfection and ventilation between patients. Because very limited numbers of patients could be tested in conventional AIIRs, drive-through (DT) screening centres have been implemented to facilitate specimen collections by hospitals and local authorities [4]. Because the entire procedure takes about 10 min per person, and several persons can be served at different steps at the same time, the testing capacity reaches over 100 samplings per day. DT screening centres contributed to the early diagnosis of masses of patients without delay.
Second, patient triage and prioritization of medical resources are essential for the prevention of a surge during an outbreak. The shortage of healthcare services has become more severe during this COVID-19 pandemic situation. As well as the essential equipment—including hand sanitizers, N95 respirators, and ventilators—hospital beds are lacking. The surge of the outbreak has in many countries led to the breakdown of healthcare systems and an increase in case fatality rates. Although COVID-19 starts with mild symptoms, about 15% of patients with COVID-19 progress to a severe condition, and 5% require ICU care within 5–7 days [5]. They are hospitalized for several weeks until recovery. The hospital beds would quickly be saturated with mild or moderate cases in the early phase of massive outbreak situations. It would be difficult to find beds for patients diagnosed later, and some of them could experience aggravation during home isolation as happened in Daegu [1]. Early diagnosis and adequate initial management are crucial for a better prognosis of COVID-19, because no specific treatment is available. It is less likely that the hospital systems are sufficiently prepared for all the patients with COVID-19, even in the countries with high-performing health systems. The rapidly deteriorating patients will eventually have adverse outcomes if they don't receive appropriate supportive management in time. Therefore, we established the systems to triage patients and prepared facilities for patients with variable disease severity.
Third, the nation should prepare for other types of care centres beyond hospital beds. Moderately or severely ill patients need medical management or intensive care in hospitals, while mildly ill patients can stay at home. Because patients with mild symptoms are shedding high viral loads in the early phase of the disease [6], they can easily transmit the virus to their household contacts. Therefore, these asymptomatic or mild patients should be isolated in isolation-and-care centres. In Korea, accommodation facilities were converted to isolation-and-care facilities and named Life Treatment Centres (LTCs) by the KCDC [7]. The first centre was opened on March 2, and as of March 26 a total of 18 centres could accommodate about 4000 people in Korea. Not only were public facilities utilized, but also private facilities were provided voluntarily and operated by matching hospitals. These types of isolation facilities would be useful to monitor the aggravation of the symptoms of patients and to prevent further transmission to others. Although this could be beneficial for patients' outcomes and disease containment, it might be challenging to operate because human resources, usually lacking in the crisis, are needed. As strategies to reduce the requirement for human resources, information technologies (such as mobile phone applications) were implemented to monitor patients.
Fourth, a contingency plan should be prepared to enhance the capacity for critical care. An enormous number of patients with COVID-19 overwhelmed the capacity of isolation beds and ICU beds since late February, although there were more than 5500 beds in six tertiary-care hospitals in Daegu. Makeshift wards have been dedicated for patients with COVID-19 in hospitals, and public hospitals have been transformed for COVID-19 care only. Temporary AIIRs using mobile machines generating negative air pressure and temporary ICU beds have been prepared. Volunteering doctors and nurses have been taking care of the patients. Military personnel and ambulance workers were sent to Daegu from other regions. In addition, some of the patients were transferred to hospitals in other regions. Hospitals for COVID-19 care have been designated for the efficient use of limited resources.
The continuous communication and collaboration between professional societies with health authorities and local authorities are the important component for the efficient and rapid response to the health crisis. The Korean Society of Infectious Disease formed the committee for COVID-19 response on January 27 and organized the multidisciplinary committee with ten professional societies, including the Korean Society of Epidemiology, the Korean Society of Healthcare-Associated Infection Control and Prevention, the Korean Society of Critical Care Medicine, and the Korean Society of Emergency Medicine on February 4. This multidisciplinary committee have had weekly meetings with the KCDC and Ministry of Health and Welfare. We advised installing a DT system and implementing strategies to triage patients and prepare facilities for patients with variable severity including LTCs. In Korea, from the painful experiences in the 2015 MERS outbreak, the preparedness for emerging infectious diseases (EIDs) has advanced in terms of diagnostic capacities, transparent risk communications, and the cooperation of people. Although we had built more isolation units in hospitals, we now realize that those are not sufficient to overcome this massive epidemic. The threat of EIDs would continue, and we do not know how and when it would come. Singapore, Taiwan and Hong Kong, having experienced the SARS outbreak, are well prepared for EIDs, and are responding efficiently against COVID-19. Investigation into the building of National Hospitals for Infectious Diseases and for specialists to take care of outbreaks should be top priority for our future safety.
Since the first outbreak in China, mankind is suffering, and the loss is devastating. However, we are gathering wisdom, best knowledge, and intellectual reasoning with state-of-the-art science to overcome this outbreak. We may have to live with COVID-19 for some time. While we are responding, we have to prepare the next sustainable strategies along with our lives.
Transparency declaration
There are no potential conflicts of interest relevant to this article. No external funding was received.
Acknowledgement
I greatly appreciate the efforts of all the hospital employees and their families who are working tirelessly during this outbreak. I thank all the members of the Korean Society of Infectious Diseases and Korea Centres for Disease Control and Prevention. I also appreciate the collaboration and productive discussion with Dr Yae-Jean Kim, and Dr Kyung-Ran Kim for her graphic assistance.
Editor: L. Leibovici
References
- 1.Korean Society of Infectious Diseases, Korean Society of Pediatric Infectious Diseases, Korean Society of Epidemiology, Korean Society for Antimicrobial Therapy, Korean Society for Healthcare-associated Infection Control and Prevention, Korea Centers for Disease Control and Prevention Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from january 19 to March 2, 2020. J Korean Med Sci. 2020;35 doi: 10.3346/jkms.2020.35.e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korean Society of Infectious Diseases and Korea Centers for Disease Control and Prevention Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from january 19 to March 10, 2020. J Korean Med Sci. 2020;35 doi: 10.3346/jkms.2020.35.e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huh K., Shin H.S., Peck K.R. Emergent strategies for the next phase of COVID-19. Infect Chemother. 2020;52:105–109. doi: 10.3947/ic.2020.52.1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kwon K.T., Ko J.H., Shin H., Sung M., Kim J.Y. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020;35 doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan W.J., Ni Z.Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X. Clinical Characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.To K.K., Tsang O.T., Leung W.S., Tam A.R., Wu T.C., Lung D.C. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park P.G., Kim C.H., Heo Y., Kim T.S., Park C.W., Kim C.-H. Out-of-hospital cohort treatment of coronavirus disease 2019 patients with mild symptoms in Korea: an experience from a single community treatment center. J Korean Med Sci. 2020;35 doi: 10.3346/jkms.2020.35.e140. [DOI] [PMC free article] [PubMed] [Google Scholar]